Surgical Reconstruction of the Lateral Collateral Ligament
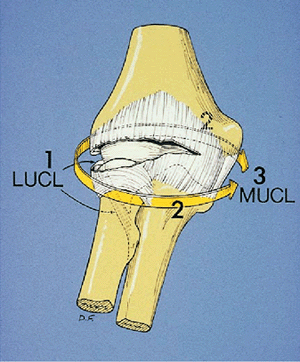
involve a common pathway that begins as a posterolateral rotatory
subluxation. In virtually all cases of complete dislocation, the
essential lesion is disruption of the ulnar part of the lateral
collateral ligament (6,8,9,10).
The medial collateral ligament may be intact. The annular ligament
remains unaffected. This pattern of instability involves rotatory
ulnohumeral subluxation accompanied by posterolateral subluxation or
dislocation of the radiohumeral joint, with the ulna and radius
rotating off the humerus together as a unit (Fig. 15-1).
We have now come to recognize that possibly the most common clinical
expression of lateral ulnar collateral ligament (LUCL) deficiency
relates to exposure and treatment of radial head pathology associated
with elbow distraction.
instability. We are not aware of any nonsurgical means of treating this
condition once established except for the permanent use of an elbow
brace. This is cumbersome and not always effective, especially in obese
patients. Osborne and Cotterill (11) suggested
that the lax tissues around the elbows of young children with
instability might tighten with growth and prevent recurrences of their
instability. We have no data to substantiate this thought, although it
is an attractive proposition.
reconstruction. There are several relative ones. Children with open
epiphyseal plates should not have their ligaments reconstructed with
tendon grafts that cross the physis. Instead, the existing lateral
collateral ligament (LCL) tissues are imbricated and reattached to bone
isometrically. Our youngest patient,
who
was 4 years old at the time of surgery, was the victim of child abuse
and repeatedly injured herself by falling. Her repair has failed and
her parent has been advised that she should not be reoperated until her
mental development and family circumstances improve. The absence of a
radial head adversely affects the prognosis but is not a
contraindication to surgery.
 |
|
Figure 15-1. We have now come to recognize that the spectrum of elbow ligament/capsule disruption is imitated by description of the LCL.
|
the lateral ligament of the elbow involves assessment of the findings
on history and physical examination but is based first on the
prerequisite understanding of the functional anatomy as well as the
pathoanatomy and etiology of elbow instability.
an explanation of the anatomy and pathology is appropriate here. On the
lateral side of the elbow, an ulnar insertion has been variably
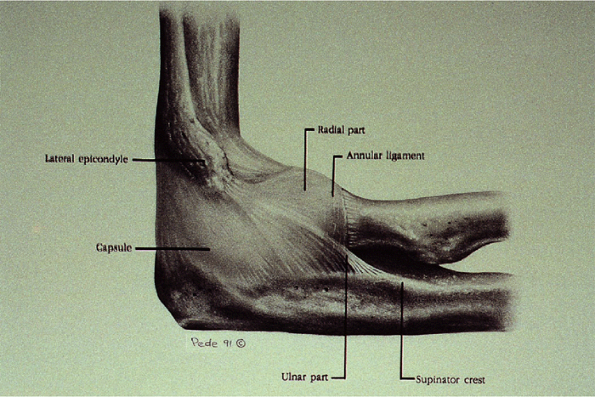
illustrated in the anatomy literature (1,3,4,5,7,14). We identified this ligament as part of the lateral capsuloligamentous complex in 17 of 17 fresh-frozen cadaver elbows (Fig. 15-2) (9).
Lack of awareness in the past is probably due to the fact that it
blends with the fibers of the lateral collateral complex from which it
is indistinguishable (7). It originates from
the lateral epicondyle. As it courses superficially over the annular
ligament it blends with it and then curves posteriorly and ulnarward to
insert on the tubercle of the supinator crest of the ulna (4,14).
Its fibers are distinct at its insertion but are hidden beneath the
fascia covering the supinator and the extensor carpi ulnaris muscles.
It can be palpated at its insertion by applying a varus or supination
moment to the elbow.
usually posttraumatic, with about one-half of patients having a history
of a documented dislocation requiring reduction (6).
The remainder of the posttraumatic cases have experienced injuries such
as “sprains” or fractures of the radial head or coronoid. Finally, this
condition can also be iatrogenic, caused by violation of the ulnar part
of the LCL during lateral release for lateral epicondylitis or radial
head excision (6,8). It should be noted that the ulnar part of the LCL passes around
the radial head, which augments tension in the ligament (7). Removal of the radial head can cause slight laxity.
 |
|
Figure 15-2.
The lateral collateral ligament (LCL) is a complex of fibers consisting of the radial part, the ulnar part, and the annular ligament, all of which blend together. The ulnar part is indistinct at its origin on the lateral epicondyle. In fact, the common extensor origin also blends with this but has been excised for the purpose of this illustration. The ulnar part of the LCL arches over the annular ligament, with which it is closely integrated. It is most distinct along its anterior border as it inserts on the tubercle of the supinator crest. There is an additional fan-shaped insertion posterior to this, along the base of the annular ligament and just proximal to it. This gradually thins out until only the capsule remains. (Reprinted from O’Driscoll SW, Horii E, Morrey BF, et al. Anatomy of the ulnar part of the lateral collateral ligament of the elbow. Clin Anat 1992;5:296–303
, with permission.) |
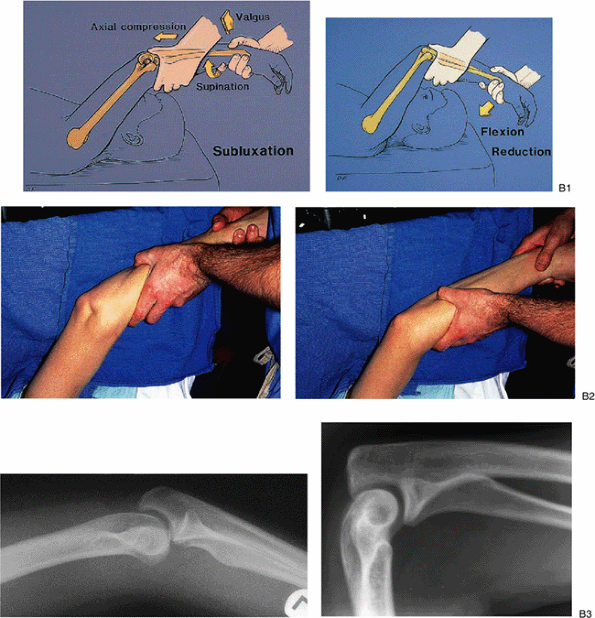
catching or locking of the elbow. Careful interrogation reveals that
this occurs in the extension half of the arc of motion with the forearm
in supination. The physical examination may be unremarkable. Valgus
stress may show some laxity. However, the classic physical finding is
that of a positive pivot shift maneuver (8) (Fig. 15-3).
The elbow is supinated by applying torque at the wrist, and a valgus
moment is applied to the elbow during flexion. This results in a
typical apprehension response with reproduction of the patient’s
symptoms and a sense that the elbow is about to dislocate. Reproducing
the actual subluxation and the clunk that occurs with reduction can
usually be accomplished only with the patient under general anesthetic
or occasionally after
injecting
local anesthetic into the elbow joint. The lateral pivot shift test
performed in that manner results in subluxation of the radius and ulna
off the humerus, which causes a prominence posterolaterally over the
radial head and a dimple between the radial head and the capitellum. As
the elbow is flexed past approximately 40 to 60 degrees, reduction of
the ulna and radius together on the humerus occurs suddenly with a
palpable visible clunk. It is the reduction that is apparent. It should
be emphasized that the lateral pivot-shift test for posterolateral
rotatory instability is not easy to learn or teach and is readily
demonstrable only in the extreme case.
 |
|
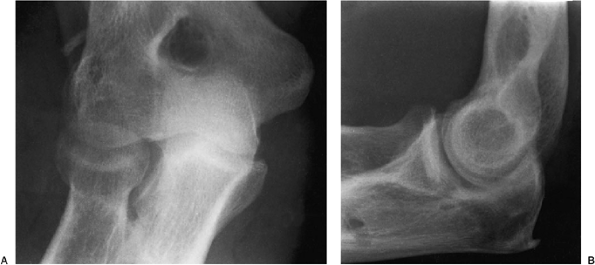
Figure 15-3. The lateral pivot-shift test of the elbow. A:
The lateral pivot-shift test is most easily performed with the arm overhead. (We now use this method routinely.) Full external rotation of the shoulder provides a counterforce for the forearm supination and leaves one hand free to control valgus. The posterolateral dislocation of the radiohumeral joint produces a bony prominence and an obvious dimple, where the skin is “sucked in” just proximal to the dislocated radial head. On the lateral radiograph the radiohumeral joint is dislocated posterolaterally and there is a rotatory subluxation of the ulnohumeral joint; the semilunar notch of the ulna is rotated away from the trochlea. B: Reduction occurs with elbow flexion or sometimes simply with forearm pronation. The dimple disappears laterally and the lateral radiograph is normal. |
subtle instability is insufficient to demonstrate with the pivot-shift
test. In those patients with symptoms strongly suggestive of recurrent
subluxations, arthroscopy reveals an excessive degree of widening of
the ulnohumeral articulation with forced supination or widening of the
lateral ulnohumeral joints.
prepped and draped from the tourniquet on the upper arm distally to
include the hand. If no palmaris longus is present, the leg is prepped
and draped to permit access to the knee region for obtaining the
semitendinosus tendon. The elbow is operated on with the arm on the
patient’s chest.
avulsed lateral ulnar collateral ligament or reconstructing it with a
tendon graft. Avulsion has been observed in children and in a few cases
of acute fracture-subluxations of the elbow. Repair of the lateral
complex must be meticulously performed when closing the capsule after
treating the radial head in the fracture dislocation. In general, one
can safely assume that in chronic cases the damaged ligament will be
attenuated and require substitution with a graft. Our first choice is
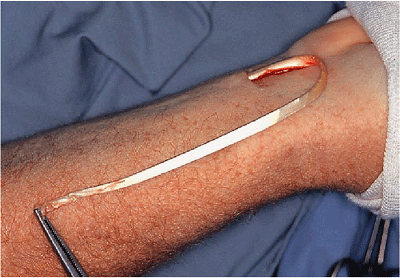
the ipsilateral palmaris longus, which is obtained through a 1-cm
transverse incision in the wrist crease, using a long tendon stripper.
At least 20 cm of length is required for the tendon reconstruction. If
the patient does not have a palmaris longus, the semitendinosus or
plantaris can be used. The larger tendons can be split to reconstruct
both the medial and lateral ligaments when necessary.
addressed surgically for a variety of pathologic states of variable
extent when the lateral collateral ligament is released. This occurs
usually by reflection from the humerus. The inadequate or inconsistent
repair of this structure is one of the most common reasons for lateral
collateral ligament insufficiency, which frequently leads to subtle
clinical presentation of posterolateral rotatory instability.
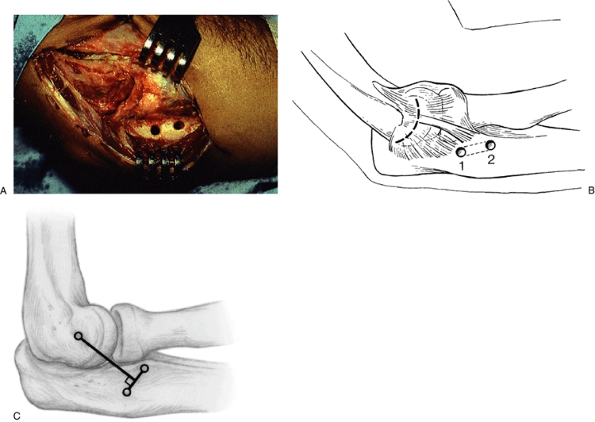
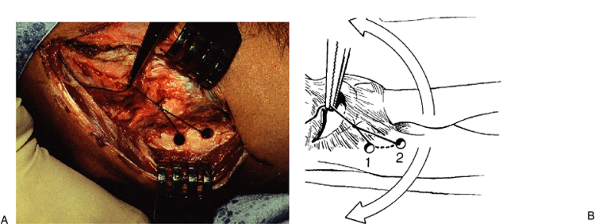
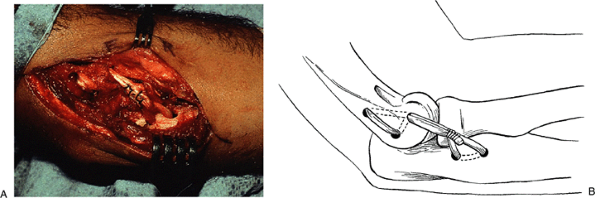
drill hole is placed in the midportion of the lateral epicondyle, which
is the center of the projected curvature of the capitellum and is
coincident with the origin of the lateral collateral ligament. A No. 2
or No. 5 Mersilene suture is employed in a running locked fashion
distally to the tubercle of the supinator crest. The purchase in the
ulna is through a drill hole at that site or through the remnant of the
ligament as it attaches to the tubercle. The suture is then brought
proximally through a second drill hole again in the anatomic origin of
the lateral collateral ligament (Fig. 15-4). The forearm is pronated and is immobilized between 60 and 90 degrees of flexion.
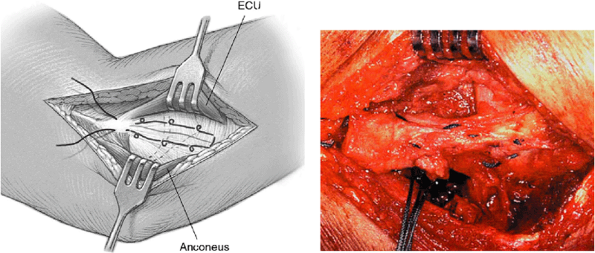
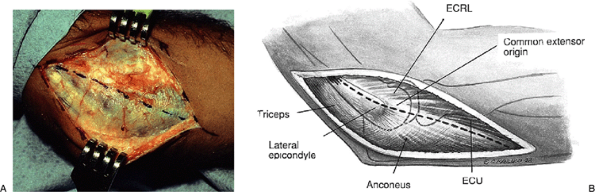
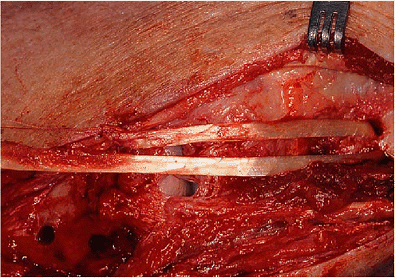
The deep fascia is incised along the supracondylar ridge and distally
between the anconeus and extensor carpi ulnaris muscles (Fig. 15-6).
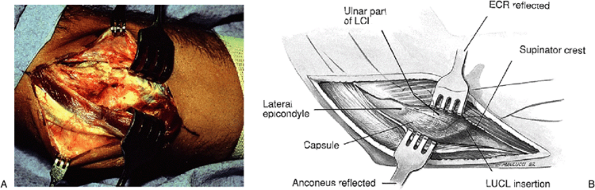
The triceps is reflected off the posterolateral aspect of the distal
humerus in continuity with the anconeus, which is reflected off the
lateral side of the ulna and capsule (Fig. 15-7).
The common extensor origin is partially reflected to expose the
capsule. Capsuloligamentous attenuation is assessed and laxity is
confirmed. This is usually proximal to the annular ligament, and the
capsular laxity is best appreciated by varus stress or performing the
pivot-shift maneuver.
 |
|
Figure 15-4.
Insufficient LUCL is repaired by a suture placed through a bone tunnel at the lateral epicondyle. A running locked (Krachow) stitch is used to repair/reconstruct this deficiency. The proximal suture is also placed through a bone hole. |
 |
|
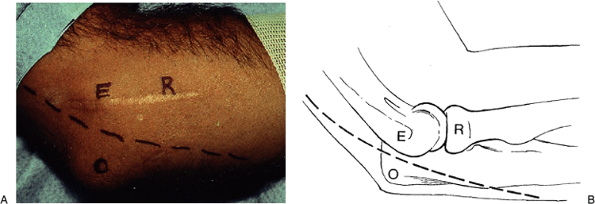
Figure 15-5. A,B: A 10-cm Kocher-type skin incision is used, passing between the epicondylar and olecranon.
|
 |
|
Figure 15-6. A,B:
The deep fascia is incised along the supracondylar ridge and distally between the anconeus and extensor carpi ulnaris muscles. The interval is best identified by palpation. |
 |
|
Figure 15-7. A,B:
The triceps and anconeus are reflected in continuity off the posterior humerus and capsule, exposing the lateral side of the ulna. The common extensor origin is partially reflected to expose the capsule. Capsuloligamentous attenuation is assessed and laxity confirmed. |
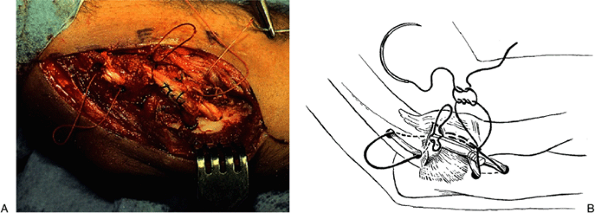
An alternative is to open the capsule either posterior or anterior to
be in line with the flow of the ligament. The insertion site for the
tendon graft is then prepared by creating 3- to 4-mm drill holes in the
ulna, one near the tubercle
on
the supinator crest, which is easily palpated just distal to the
annular ligament attachment on the ulna. The other is 1 cm
posterior/proximal to the first and on a line perpendicular to the line
of the graft (Fig. 15-8C). The underlying bone is channeled with a curved awl or curette.
 |
|
Figure 15-8. A,B:
The capsule is opened along the capitellum in an arc to permit inspection of the joint and later imbrication of the capsule. An alternative approach is to open the capsule obliquely from the epicondyle to just posterior to the annular ligament. The insertion site for the tendon graft is then prepared by creating two drill holes in the ulna, one near the tubercle on the supinator crest (which is felt by stressing the elbow in varus or supination) and the other 1.25 cm proximally at the base of the annular ligament. The underlying bone is channeled with a curved awl from the Bankart set of instruments. C: The ulnar holes are sometimes made so the line connecting these holes is perpendicular to the line of the collateral ligament. |
center of the capitellum (viewed from the lateral side). A No. 1 suture
is passed through these two holes and grasped with a hemostat at the
estimated isometric center of rotation of the elbow (Fig. 15-9).
The isometric ligament origin is then determined by flexing and
extending the elbow to see if the suture moves. No movement occurs if
the suture and hemostat are on the isometric point. The entry site for
the graft, hole No. 3, is then burred into the humerus at that point.
Two technical points are worth noting. First, since the instability is
most noted in extension, the ligament must be tight in extension. Hence
if there is any question, the hole is made more anterior than expected.
Finally, once the starting point is identified, it should be expanded
to be about 5 to 6 mm. This enlargement takes place superior/anterior, not posterior/distal (Fig. 15-10).
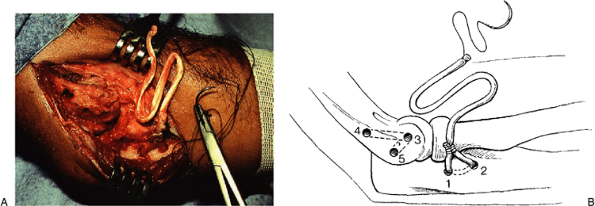
An exit site, hole No. 4, is created with the bur just posterior to the
supracondylar ridge about 1.5 cm proximally and a tunnel created
between the two with the curved awls or curettes (Fig. 15-10).
A reentry site, hole No. 5, is created with the bur distally so that a
bridge of bone, 1.25 cm, spans the two holes, and a tunnel is created
from this site to the original entry site at the epicondyle, where the
tendon will exit again.
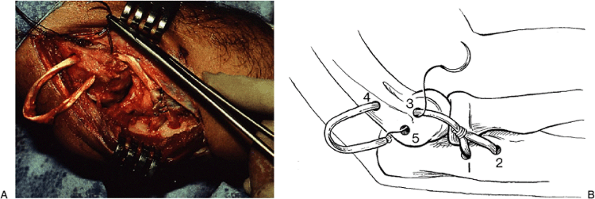
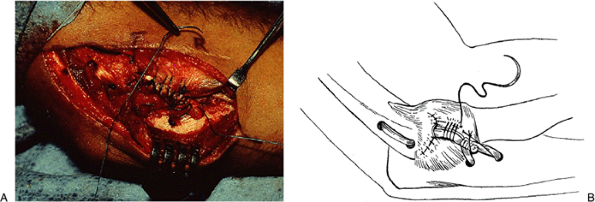
It is then passed into the entry site, hole No. 3, in the lateral
epicondyle, which represents the isometric origin of the ligament being
reconstructed, out through the exit site, hole No. 4, proximally, down
the posterior surface of the distal humerus, back into the bone through
the reentry site, hole No. 5, to emerge at the isometric origin at hole
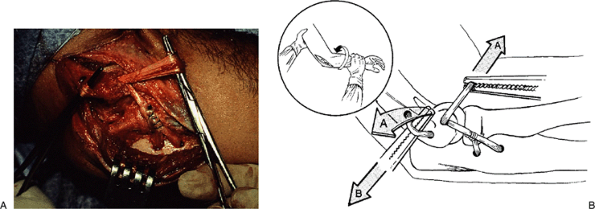
No. 3 (Fig. 15-11). It is tensioned (Fig. 15-12) and sutured down to itself with the elbow in 30 to 40 degrees of flexion and forced pronation (Fig. 15-13). The
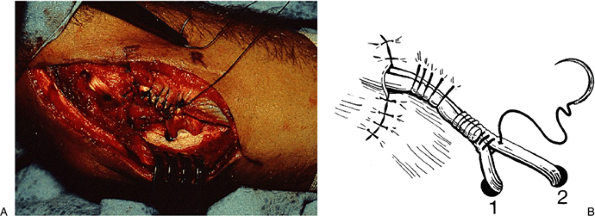
reconstruction can be augmented by passing a heavy No. 2 absorbable (Dexon) suture through the same course as the tendon graft (Fig. 15-14).
If the capsule has been opened longitudinally, the suture should be
woven through the capsule in an arch and not permitted to fall deep to
the capsule because it will rub on the side of the capitellum and
radial head. The capsule is closed and plicated, and the original arch
of the ulnar part of the LCL is restored by pulling the graft
anteriorly and suturing it to the capsule (Fig. 15-15).
This also prevents the graft from slipping posterior to the radial head
and permits optimum testing. The capsule must be closed under the graft
to prevent it from rubbing on the radial head or capitellum. If further
tension is desirable, this can be accomplished by closing the distal
triangular gap between the two limbs of the graft (Fig. 15-16).
 |
|
Figure 15-9. A,B:
A No. 1 suture is passed through these two holes and grasped with a hemostat at the estimated isometric center of rotation of the elbow. The isometric ligament insertion is then determined by flexing and extending the elbow to see if the suture moves. No movement occurs if the suture and hemostat are on the isometric point. This point is usually more anterior than might be thought. |
 |
|
Figure 15-10. A,B:
An entry site for the graft, hole No. 3, is then burred into the humerus at that point. Since the hole is bigger than the tip of the hemostat, one should make the hole posterior and proximal to the hemostat point (Fig. 15-8B inset). If it is placed distal or posterior, the tendon graft will be lax in extension and tight in flexion or vice versa. An exit site, hole No. 4, is created with the bur just posterior to the supracondylar ridge about 1.5 cm proximally and a tunnel created between the two with the curved and straight awls. A reentry site, hole No. 5, is created with the bur distally so that a bridge of bone, 1.25 cm, spans the two holes, and a tunnel is created from this site to the original entry site at the epicondyle where the tendon will exit again (hole No. 3). The tendon graft is then brought through the first two holes in the ulna, holes 1 and 2, and sutured to itself. |
 |
|
Figure 15-11. A,B:
The graft is then passed into the entry site, hole 3, in the lateral epicondyle, which represents the isometric origin of the ligament being reconstructed, out through the exit site, proximally, hole 4, down the posterior surface of the distal humerus, back into the bone through reentry site, hole 5, to emerge at the isometric origin at hole 3. |
 |
|
Figure 15-12. A,B: The graft is tensioned by pulling the proximal loop with a hemostat while pulling on the free end.
|
 |
|
Figure 15-13. A,B: The free end is sutured to the remainder of the graft with the elbow in 40 degrees of flexion and forced pronation.
|
in some patients is to make a minimal arthrotomy in line with the ulnar
part of the LCL but just near the epicondyle. This provides access to
the origin of the LCL where the graft must be attached to the humerus
but minimizes the dissection and arthrotomy. The rest of the procedure
is the same except the capsule is plicated only from anterior to
posterior, rather than from distal to proximal. The advantage of this
modification is that it obviates the tedious task of closing the
capsule
beneath
the graft, and it is quicker. The former is necessary to prevent the
graft from rubbing on the joint margins or slipping posterior to the
radial head.
 |
|
Figure 15-14. A,B:
The reconstruction can be augmented by passing a heavy No. 2 absorbable (Dexon) suture through the same course as the tendon graft. If this is done, the suture should be woven through the capsule in an arch and not permitted to fall deep to the capsule. This is particularly important when a longitudinal arthrotomy is used because the tendon will rub on the side of the capitellum and radial head. |
 |
|
Figure 15-15. A,B:
The capsule is closed and plicated, and the original arch of the ulnar part of the LCL is restored by pulling the graft anteriorly and suturing it to the capsule. This also prevents the graft from slipping posterior to the radial head. The capsule must be closed under the graft to prevent it from rubbing on the radial head or capitellum. |
 |
|
Figure 15-16. A,B:
If further tension is desirable, this can be accomplished by closing the distal triangular opening between the two limbs of the graft. The closure is routine and the forearm is held pronated until the limb is immobilized. |
 |
|
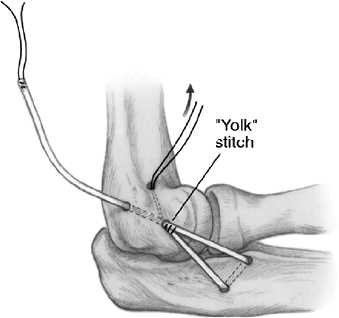
Figure 15-17. The short arm of the graft is secured to the long arm with a “yolk” stitch so both enter the isometric hole.
|
 |
|
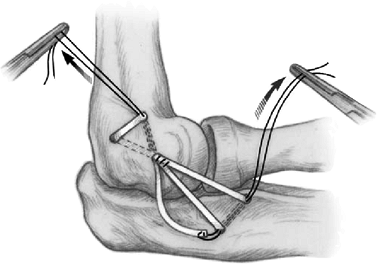
Figure 15-18.
The long arm is looped through the humeral tunnels. Tension is maintained on the “yolk” stitch, which is drawn through the humeral hole for this purpose. If length allows and clinical goals require a third “arm,” the graft is brought back through the ulnar tunnel. |
Proximally, we have also been making hole No. 5 the distal posterior
hole on the humerus anterior to the supracondylar ridge. This permits
wrapping the tendon over the strong bone in the supracondylar ridge.
Finally, we have also been employing a yolk stitch. By suturing the end
of the ligament to the rest of the graft so both “arms” of the
reconstruction enter the isometric hole, tension is placed on the
suture that is not yet cut, as well as on the long arm of the graft (Fig. 15-17). The long end is then wrapped around the supracondylar ridge and then distally to enter the ulna tunnel (Fig. 15-18).
is routine and the forearm is kept in full pronation to protect the
repair until the limb is immobilized.
cross the physis, so we do not do this operation. Instead the LCL is
elevated from its origin, tightened, and resutured to the isometric
point on the lateral epicondyle with heavy sutures that pass through
bone but not through the physis. The method is similar to that
described by Osborne and Cotterill (11).
locked hinge brace in full pronation for about 10 days. Then protected
motion is allowed in the brace with a 30-degree extension block for 3
to 6 weeks. The period of immobilization and bracing varies depending
on the degree of generalized laxity of the patient, the security of the
repair, the history of previous episodes of immobilization (and whether
or not they caused stiffness), and the attitude of the surgeon about
the appropriateness of immobilizing an elbow. We have varied this quite
a bit ourselves, ranging from immediate motion in a brace for 6 weeks
to immobilization for 6 weeks followed by bracing for up to 3 months.
In general, 10 days of immobilization and 6 weeks of protected motion
are used. Children and those patients who have previously undergone
prolonged immobilization for up to 6 weeks without developing
contractures are thought to be at less risk of developing contractures
and are immobilized for 3 to 6 weeks. As our experience and follow-up
accumulate, these guidelines will certainly change.
reported that eight patients treated for recurrent elbow dislocations
during a 4-year period by imbrication and reattachment of the LCL did
not experience any recurrences. Our initial experience with
reconstruction in patients ranging from 4 to 49 years of age has just
been recently updated by Sanchez-Sotelo et al. In the group of 42
patients, stability was restored in about 90%, and excellent results
(no pain, no loss of motion, no instability) occur in about 60% (6).
As noted in the original report, the update confirms that. If arthritis
was present or the radial head had been excised, the outcome was less
predictable (6,12). The
other 40% complain of either some pain or loss of motion, although this
could be related to the fact that they typically have had one or more
previous operations. In the primary case of untreated instability, the
results are highly successful.
of the palmaris longus tendon during harvesting, one case in which the
length of tendon harvested was suboptimal (the repair was not as
secure, although the patient’s instability has not yet recurred), one
saphenous nerve neuroma from the semitendinosus donor site, and one
deep vein thrombosis (DVT) in a patient with a prior history of DVTs.
There has been one instance of fracture of the humeral tunnel site.
years earlier. She had been immobilized for almost 3 weeks. Her
presenting complaint was that the elbow slipped out of joint with
certain stress, especially when the elbow was extended and supinated.
The lateral rotatory stress test showed posterior lateral rotatory
instability, as did the varus stress test (Fig. 15-19). A palmaris longus tendon was harvested (Fig. 15-20) and the lateral complex was reconstructed as described earlier (Fig. 15-21). One year later her motion was normal and the joint was stable (Fig. 15-22).
 |
|
Figure 15-19. A,B: Stress radiographs reveal a deficiency of the lateral collateral ligament with varus and posterolateral rotary stress.
|
 |
|
Figure 15-20. The ipsilateral palmaris longus tendon has been harvested.
|
 |
|
Figure 15-21. The graft is placed in the isometric position as described in Fig. 15-9.
|
 |
|
Figure 15-22. A,B: One year later the joint is painless and stable.
|
