Ankle Fractures: Open Reduction Internal Fixation
injuries. Nondisplaced fractures can almost always be successfully
treated nonoperatively with close follow-up. Most displaced bimalleolar
fractures benefit from operative reduction and fixation if no surgical
contraindications exist.
closed reduction, and if successful, carefully followed to union with
nonoperative treatment. Isolated, distal, fibula fractures without
mortise widening or talar shift can usually be successfully managed
nonoperatively if the fibular displacement is less than 2 mm. These
patients must be differentiated from individuals who also have an
obvious or occult injury to the medial side of the ankle. While the
decision for operative versus nonoperative treatment is frequently
clear, for a group of patients, the treatment decision is more
difficult; for these patients, reduction may be borderline acceptable
or follow-up x-rays suggest some loss of reduction.
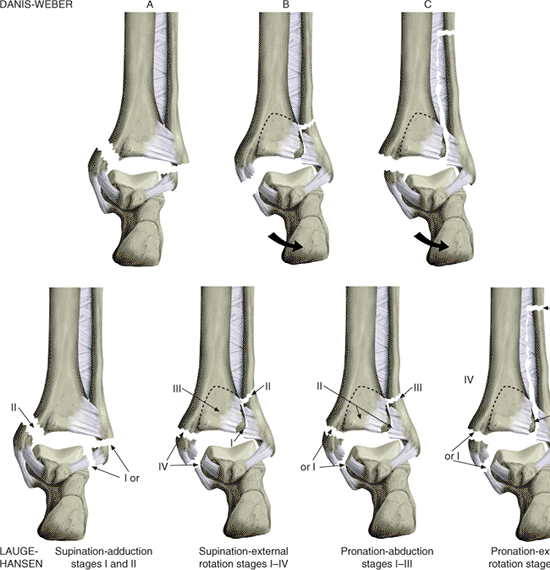
commonly used. Lauge-Hansen described a classification based on the
foot position (supination or pronation) at the time of injury and the
direction of the injury force (external rotation, adduction, or
abduction) on the foot (Fig. 33.1). The
Danis-Weber classification is based on the location of the fibula
fracture with respect to the ankle joint. In Danis-Weber injuries, the
fibula fracture is distal to the ankle joint and is usually the
equivalent to Lauge-Hansen supination-adduction injuries. In
Danis-Weber B injuries, the fibula fracture is at the level of the
ankle joint and can be either a supination–external rotation or
pronation-abduction injury. Type C Danis-Weber fractures are
characterized by a fibula fracture proximal to the ankle joint and are
usually the equivalent of the Lauge-Hansen pronation–external rotation
injury.
the most common fracture pattern. In this injury, the supinated foot is
subjected to an external rotation force that may cause a varying degree
of soft-tissue and bony damage. The first structure to be injured is
the anterior tibiofibular ligament (stage I). As the external rotation
force continues, the
fibula
is fractured (stage II). Further force results in rupture of the
posterior tibiofibular ligament or a fracture of the posterior
malleolus (stage III). Finally, the deltoid ligament is ruptured or the
medial malleolus is fractured (stage IV). Because of their clinical
significance, stage II injuries must be differentiated from stage IV
supination–external rotation injuries. Stage II injuries can be managed
nonoperatively because the deltoid ligament is intact, stabilizing the
talus in the mortise. However, in stage IV injuries, the ankle is
unstable, and surgical management is usually recommended (1).
 |
|
Figure 33.1.
The Danis-Weber (AO/ASIF) classification system is based on the level of the fibula fracture. The Lauge-Hansen system is based on experimentally verified injury mechanisms. Type A Danis-Weber injuries are usually Lauge-Hansen supination-adduction injuries. Type B can be either supination–external rotation or pronation-abduction injuries. Type C injuries are usually pronation–external rotation injuries. |
ankle is palpated have been used as clinical indicators for occult
injury to the medial deltoid ligament. Recent studies have shown that
these traditional signs are not sensitive for predicting deltoid
ligament incompetence (1,2).
Stress radiographs should routinely be obtained in patients with
isolated fibula fractures that are classified as supination–external
rotation injuries (Danis-Weber type B) so the physician can identify
occult injury to the deltoid ligament. Several different methods for
obtaining stress radiographs have been described and include the use of
gravity, valgus stress, or external rotation (2,3).
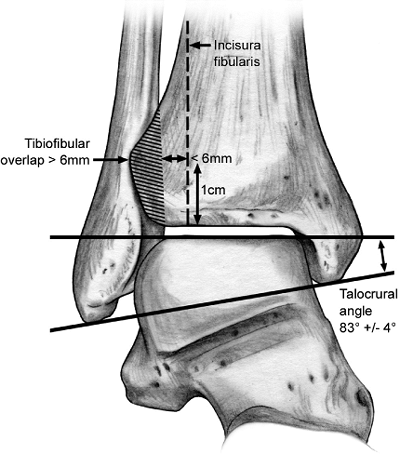
x-rays in the absence of plaster, which may obscure important findings.
Occasionally, contralateral radiographs are useful to evaluate unusual
abnormalities. The physician must understand the normal radiographic
landmarks and relationship of the fibula with the distal tibia. Equal
medial, lateral, and superior joint space should be seen surrounding
the talus on the mortise view. The position of the distal fibula with
respect to the incisura should be carefully evaluated. This is measured
1 cm proximal to the tibial plafond. Specific measurements may vary
depending on the ankle rotation and angle of the x-ray beam. The
distance between the medial border of the fibula and the incisura
should be less than 6 mm on both the anteroposterior (AP) and mortise
view. On the AP view, the fibula should overlap the tibia by 6 mm, or
42 % of the fibular width, and there should be at least 1 mm of overlap
between the fibula and tibia on the mortise view. Finally, the length
of the fibula is assessed by evaluating the talocrural angle, which on
average should measure 83 ±4 degrees and can be compared with the
contralateral ankle (Fig. 33.2). In addition,
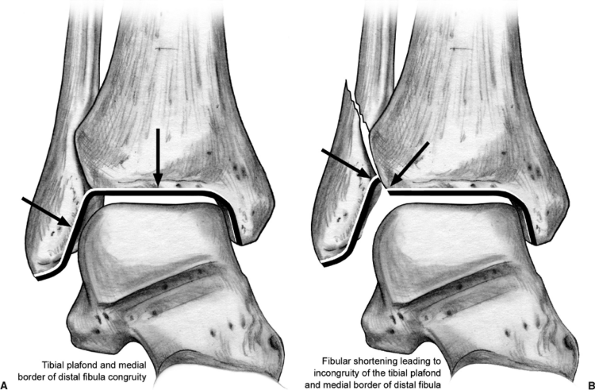
fibular shortening will lead to incongruity in a line drawn along the
tibial plafond and the medial border of the distal fibula (Fig. 33.3).
 |
|
Figure 33.2.
Radiographic projection of fibula on tibia in standard AP radiograph. When measured 1-cm proximal to the ankle joint, the distance between the medial border of the fibula and the incisura should be less than 6 mm on any view. On the AP view, the fibula should generally overlap the tibia (shaded area) by greater than 6 mm or more than 42% of the fibular width; however, individual variation and beam angle may effect individual measurements. There should be more than 1 mm of overlap of the tibia and fibula on any view. |
whether operative or nonoperative, is to maintain anatomic reduction of
the tibiotalar joint. Lateral displacement of the talus will reduce
ankle joint contact, resulting in joint-contact stress alterations that
may predispose the patient to posttraumatic osteoarthritis (4,5,6).
 |
|
Figure 33.3.
Normally, there is congruity in a line drawn along the tibial plafond and the medial border of the fibula. When the fibula is shorted, incongruity is observed at the junction of the tibia and fibula. |
fracture management. The majority of rotational ankle fractures will
require little more than longitudinal traction and internal rotation
reduction to be achieved. A well-padded, posterior, plaster splint with
the ankle at neutral dorsiflexion will provide comfort and
immobilization and allow for soft-tissue swelling. In general,
immediate circumferential casting should be avoided, even if this is
eventually chosen as the definitive treatment method, as ongoing
swelling can lead to dangerous constriction and exacerbation of the
soft-tissue injury. Edema control with judicious elevation is a
well-accepted approach to early management if compromised vascular
inflow is not an issue. Cryotherapy may reduce swelling and may have
analgesic benefit. More recently, intermittent compression devices have
been utilized to help control swelling both preoperatively and
postoperatively (7,8).
soft-tissue injuries or those with large, posterior, malleolar
fractures that cause persistent talar subluxation, the surgeon may find
that temporary external fixation is required. External fixation
provides fracture and soft-tissue stability, allows for free access and
easy evaluation of the soft tissues, and optimizes patient mobilization.
internal fixation can be addressed with immediate surgery. However if
soft-tissue swelling is a concern, the operation is delayed and the
limb is immobilized and elevated. Examination of the skin should be
performed preoperatively
to
insure that the soft tissues can safely permit operative treatment.
This requires removal of the splint or cast prior to the induction of
anesthesia. The “wrinkle sign” is often used to assess the readiness of
soft tissues for surgical intervention. The ankle is dorsiflexed to the
neutral position and the anterior ankle skin is observed for the
presence of wrinkles. Absence of wrinkles suggests excessive
soft-tissue swelling and edema.
most ankle fractures is straightforward, care should be exercised to
avoid unexpected findings. A careful review of high-quality plain
radiographs (without obscuring plaster) should be performed. A
preoperative plan or surgical tactic, while often neglected for this
“simple” fracture, may provide mental preparation and avoid unnecessary
mistakes. Forging ahead, assuming the case is a simple straightforward
ankle fracture, can lead to suboptimal outcomes when unusual fracture
variations are encountered.
or spinal anesthetic is administered. Prophylactic intravenous
antibiotics are administered prior to surgery. A first-generation
cephalosporin is used unless there is an allergic contraindication, in
which case an alternative antibiotic is chosen. A towel roll is placed
beneath the ipsilateral buttock to provide easier access to the fibula (Fig. 33.4).
As is routine, a pneumatic tourniquet is applied to the upper thigh.
The leg is sterilely prepped. A sterile sheet is then placed beneath
the leg to prevent inadvertent contamination of surgical gowns during
the draping process. A stockinette is applied to the leg, and the leg
is draped free. The toes are sealed with a plastic adhesive drape and
the stockinette is removed to the midcalf.
trimalleolar ankle fractures with a large, displaced, posterior,
malleolar fragment that will be fixed through a posterolateral
approach. Reduction and fixation of the medial malleolus in the prone
position may be easiest performed after the knee is flexed.
 |
|
Figure 33.4.
Before prepping and draping the patient, a roll is placed beneath the ipsilateral buttock to facilitate easier access to the fibula. A tourniquet and occlusive drape may be placed around the upper thigh. |
the fracture can also be marked based on palpation and radiographic
review. We generally perform surgery under tourniquet control to
minimize blood loss, to maximize visualization, and to speed the
surgical procedure. After confirming that preoperative prophylactic
antibiotics have been administered, we exsanguinate the extremity with
an elastic (Esmarch) bandage and inflate the tourniquet to the
appropriate level.
dictates whether the medial malleolus or the fibula is fixed first. In
cases of osteopenia, we prefer to fix the medial malleolus first
because it may aid the subsequent reduction of the fibula. Care must be
exercised when using reduction clamps on osteopenic bone. Excessive
pressure with reduction clamps may easily cause iatrogenic comminution
of the fibula. In addition, the ankle joint can usually be visualized
through the medial malleolar fracture site in most circumstances. This
allows inspection of the articular surface and removal of any
intra-articular debris. While joint inspection and irrigation can be
performed either before or after fixation of the fibula, we often do
this prior to rigid fixation of the fibula.
with the long axis of the tibia. This incision should also be placed
slightly anterior to the midcoronal axis to allow inspection of the
anterior aspect of the ankle joint. Other surgeons prefer a slightly
angled incision, but too much, distal, anterior angulation may make
difficult the access to the screw insertion site. The saphenous vein
and its accompanying saphenous nerve branches should be preserved
whenever possible (Fig. 33.5).
reduction. This can best be confirmed by visualizing the anterior
aspect of the fracture. Because of the orientation of the fracture
plane, anterior or posterior malreduction may not always be appreciated
when looking at the lateral surface.
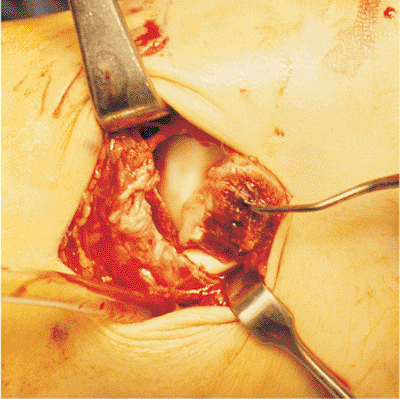
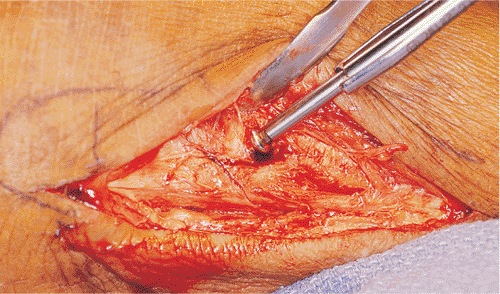
irrigation and thorough inspection of the articular surface of the
tibia and talus (Fig. 33.6). Any
osteocartilaginous debris should be removed. Articular damage to either
the tibia or talus should be noted in the operative report.
edges of the fracture. A 2.5-mm drill is used to perforate the medial
tibial cortex to allow anchorage of a bone tenaculum. A small, pointed,
bone tenaculum can be placed on the medial malleolar-fracture fragment
from anterior to posterior and used to guide the reduction. A second
small or large, pointed, bone tenaculum is then used to achieve
compression of the reduction. One tine is placed in the tibial
metaphyseal drill hole and the other is placed around the distal aspect
of the
medial malleolus. (Fig. 33.7).
 |
|
Figure 33.5.
A relatively straight incision is used for the medial malleolus. Excessive, distal, anterior angulation may interfere with the necessary screw-insertion angle. The saphenous vein and nerve should be visualized and protected during the medial approach to the ankle. |
 |
|
Figure 33.6. Retraction of the medial malleolar fragment distally allows inspection and irrigation of the ankle joint.
|
 |
|
Figure 33.7.
A pointed reduction tenaculum is used to provide provisional reduction of the medial malleolus. One tine is placed in a drill hole placed in the medial tibial metaphysis and the other tine is placed around the distal aspect of the medial malleolus. Partially threaded, cancellous, lag screws are inserted anterior and posterior to the tenaculum. |
usually secured with two 4.0-mm, partially threaded, cancellous screws.
With the tenaculum centered on the fragment, one screw is placed
anteriorly and one is placed posteriorly to the tenaculum. A scalpel is
used to split the superficial deltoid ligament in line with the fibers
to facilitate placement of the drill against bone. With the hind foot
slightly everted, a 2.5-mm drill bit is then drilled across the
fracture site in line with the long axis of the tibia. A second drill
bit or Kirschner (K) wire may be placed to avoid rotational forces
during the screw insertion. We routinely use a 40-mm cancellous screw
because the nonthreaded portion is usually long enough so that the
threads are positioned beyond the fracture site and engage the denser,
distal-tibial, cancellous bone. For optimal results, the threads should
be placed in the denser distal-tibial metaphysis, especially in
patients with osteoporosis. A second 4.0-mm cancellous screw is then
inserted parallel to the first screw.
fragment size to avoid iatrogenic comminution and malreduction. The use
of 4.0-mm cancellous screws may not be advisable if the medial
malleolus-fracture fragment is very small or comminuted. Other options
for small-fragment fixation include the use of a single lag screw with
a K wire, small diameter screws, or tension band wiring. Extra-long
2.0- and 2.7-mm screws are available; although they may not be stocked
on standard sets, they are useful for very small medial-malleolar
fragments. Tension band fixation is performed by inserting 1.6-mm K
wires in a direction similar to the standard screw fixation.
Eighteen-gauge wire or no. 5 suture is then passed around the K wires
and crossed in figure-of-eight fashion around a screw placed in the
tibial metaphysis. The ends of the K wires are then bent and impacted.
supination-adduction type injuries should be fixed either with
horizontal screws (placed at right angles to the fracture) or with a
short, low-profile, medial, buttress plate. Washers may be required in
osteoporotic patients to prevent the screw from sinking through the
thin metaphyseal cortex. This fracture pattern may also be associated
with marginal impaction of the tibial plafond. Reduction of the tibial
plafond and support with bone graft or bone graft substitute may be
required prior to medial malleolar reduction (Fig. 33.8).
fracture and the planned position of fixation. Adjustments may be
needed due to associated soft-tissue abrasions or healed blisters. The
fibula is generally approached through a relatively straight
incision (Fig. 33.9).
Angling the distal portion of this incision slightly anteriorly will
allow access to the anterolateral corner of the ankle. This will allow
access to the anterolateral aspect of the ankle joint and permit
fixation of a Chaput-Tillaux fragment, which is an avulsion of the
anterior, inferior, tibiofibular ligament. A more posterior incision
may be used if a posterior antiglide plate is planned. Care should be
taken to preserve the
superficial
peroneal nerve, which may cross the surgical approach at a subcutaneous
or fascial level, to avoid painful neuroma formation.
 |
|
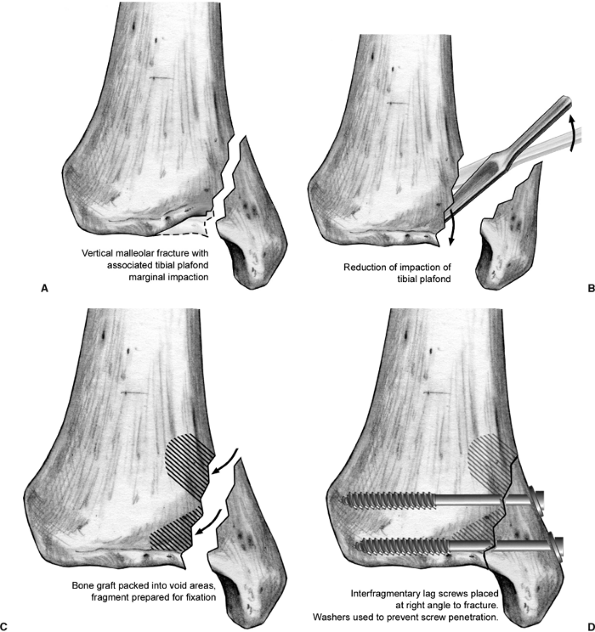
Figure 33.8.
Impaction of the medial, distal, tibial-articular surface may be seen in supination-adduction injuries. Following reduction, this segment may be buttressed with either local metaphyseal bone, allograft bone, or bone graft substitutes. Because of the vertical orientation of the fracture plane, the interfragmentary lag screws are usually placed parallel to the ankle joint. |
 |
|
Figure 33.9.
A straight lateral incision may be used for fixation of the fibula. The incision may be adjusted anteriorly or posteriorly depending on the fracture patterns and the planned fixation. |
elevated, but further periosteal stripping is kept to a minimum,
especially in comminuted fractures. Care must be exercised when
reducing the fibular fracture to avoid iatrogenic comminution. This
precaution is especially critical in older patients with osteoporosis.
Fracture reduction can be achieved by using one or more of the
following techniques: Traction and rotation can be applied to the hind
foot to assist with fracture reduction; a bone tenaculum may be
attached to the distal fragment and used to manually reduce the distal
fragment; the tines of a bone tenaculum may be placed at right angles
to the fracture plane and used to obtain and secure the fracture
reduction. Fracture reduction is usually fairly easy immediately after
injury but may be more difficult in delayed cases with fibular
shortening.
and fixed with an interfragmentary lag screw and a neutralization
plate. Occasionally, long oblique fractures can be adequately fixed
with only interfragmentary lag screws (9).
While we usually use a 3.5-mm cortical screw for the lag screw
fixation, in smaller fragments it is occasionally advantageous to use a
smaller diameter screw, such as a 2.7-mm or 2.0-mm cortical screw (Fig. 33.10).
 |
|
Figure 33.10. For oblique fibular fractures, a 3.5-mm cortical screw is placed in lag fashion perpendicular to the fracture plane.
|
fixation is not feasible, plate fixation is applied in a bridging mode
such that the comminuted fracture area is bypassed. For many fractures,
simple one-third tibular plates are adequate, but for very distal
fractures we prefer to use a bone-specific, custom, fibula plate
(Zimmer, Warsaw, IN) that allows a larger number of distal screws (Fig. 33.11).
As an alternative approach, a small-fragment locking plate could also
be used to provide improved fixation stability in a small, distal,
fracture fragment. When no bony keys are available to determine
reduction, the distal fragment may be reduced to the talus
provisionally with K wires. After visual and radiographic confirmation
of the reduction, the surgeon can apply a plate in a bridging mode.
 |
|
Figure 33.11.
This fibular peri-articular plate allows placement of additional distal-screw fixation, which may be particularly useful for obtaining additional screw fixation in very distal fractures. |
the medial incision. However, in selected circumstances, visualization
of the anterior ankle joint can also be performed by dissecting
anterior to the fibular and retracting the soft tissues with a small
right-ankle retractor (Fig. 33.12). This
exposure may also be used to reduce and internally fix avulsion
fractures involving the anterior tibiofibular ligament (Chaput-Tillaux
fragments).
throughout the procedure, especially during wound closure when
excessive skin-edge manipulation with forceps can traumatize the
tissue. We typically close incisions in an interrupted fashion with no.
3-0 or 4-0 nylon
sutures
via an Allgöwer-Donnatti technique. Because of the limited deep tissue,
a two-layer closure is usually not feasible; however, deep absorbable
sutures may help align the incision and relieve tension for the skin
closure.
 |
|
Figure 33.12.
Exposure of the anterolateral ankle joint may be performed by dissecting anterior to the fibula and retracting soft tissues with a small right-angle retractor. |
posterior malleolar involvement have a higher incidence of
posttraumatic osteoarthritis than do bimalleolar ankle fractures.
Simulated, posterior, malleolar fractures have shown a modest increase
in ankle contact stresses in static mechanical-loading studies.
Development of arthrosis may also be due to associated chondral damage
and joint instability. Rather than significantly increasing contact
joint stress, a pronounced anterior shift in the location of the
articular contact area was found in a recent study in which dynamic
ankle motion was examined in a simulated, posterior, malleolus fracture
(4). The authors postulated that this shift in
location produced substantial loading of articular cartilage not
accustomed to bearing stress and thus initiated the arthrosis.
greatly in their size. Small fragments are often extra-articular. These
small fragments are attached to the posterior, inferior, tibiofibular
ligament and are usually adequately reduced with anatomic reduction of
the fibula. However, larger, posterior, malleolar fragments may
comprise a significant portion of the articular surface, and anatomic
reduction is probably essential for good long-term function.
size is limited with plain radiographs and is better evaluated with a
computed tomography (CT) scan (10). If a CT
scan is unavailable, then a 50-degree external-rotation view may better
allow assessment of the posterior fragment size (11,12).
fixed should ideally be made preoperatively based on the size of the
fragment. Most authors recommend fixation of posterior malleolar
fractures that comprise more than 25% of the articular surface. Closed
reduction with dorsiflexion of the ankle and percutaneous
anterior-to-posterior fixation has been described as an alternative
treatment for nondisplaced or minimally displaced, posterior, malleolar
fractures. However, the accuracy of this method may not always result
in an anatomic position. Our preference for treatment of large,
posterior, malleolar fractures requiring fixation is to reduce and
stabilize these fractures prior to fixation of the fibula because the
application of a plate on the fibula usually obscures lateral
radiographic visualization of the articular surface. A large pointed
tenaculum may be inserted posteriorly through the fibular incision. A
small incision is made over the anterior tibia and blunt dissection
carried down to the bone to allow placement of the anterior tine (Fig. 33.13). Minor manipulation of the fragment can be achieved with dorsiflexion of the ankle and
rotational torque of the tenaculum. Anterior to posterior fixation of
the fragment is then achieved with either standard screws or cannulated
screws placed through one or more percutaneous incisions.
 |
|
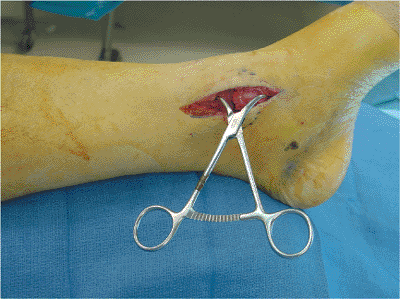
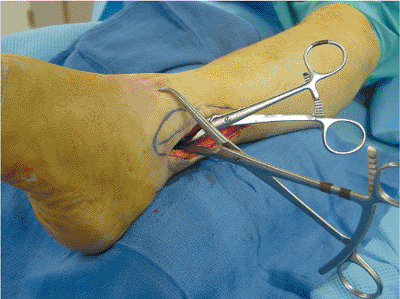
Figure 33.13.
A large bone tenaculum is placed around the fibula and can be used to manipulate and reduce the posterior malleolus. The small tenaculum in this photo is maintaining reduction of the fibula fracture. |
 |
|
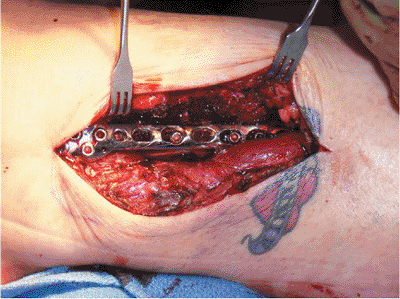
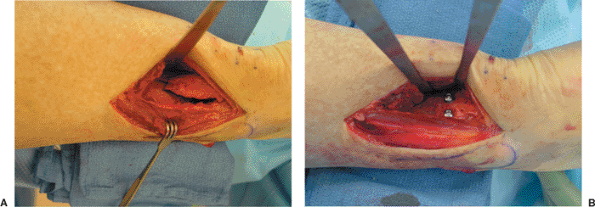
Figure 33.14. A.
This large, posterior, malleolus fragment was exposed through a posterolateral approach along the lateral border of the Achilles tendon. B. Following direct reduction of the fracture fragment, posterior-to-anterior lag-screw fixation with 4.0-mm cancellous screws and washers. After posterior malleolus fixation, fibula fixation can be achieved using a posteriorly placed antiglide plate. |
fragments, fixation may be achieved through an open posterior approach.
The patient is positioned prone and a posterolateral approach to the
fragment is performed along the lateral border of the Achilles tendon (Fig. 33.14).
This allows accurate fragment reduction via visualization of the
fragment at the posterior tibial metaphysis. The fracture fragment is
internally fixed with two or three posterior-to-anterior screws.
Washers are often used to prevent penetration of the screw heads
through the thin tibial cortex. In an alternative, a short, two- or
three-hole, one-third, tubular plate may be applied in an antiglide
mode to the posterior tibia.
medially based, or in which there is metaphyseal cortical comminution
that may not provide an adequate reduction key, reduction of the
posterior malleolar fragment may be obtained through the medial
approach prior to reduction of the medial malleolus. This approach will
allow direct visualization of the articular surface. The flexor tendons
are retracted posteriorly with a small Homan retractor, and a small
bone hook or pointed tenaculum is used to obtain fragment reduction.
Fixation is then achieved with anterior-to-posterior lag screws
inserted through small stab incisions.
with type-C ankle fractures; however, transsyndesmotic fixation may not
be required in all cases. Anatomic reduction and stable fracture
fixation may restore adequate syndesmotic stability. More distal fibula
fractures secured with rigid plate fixation may offer sufficient
stability to obviate the need for transsyndesmotic fixation (13,14).
If the deep deltoid ligament is intact, rigid fixation of the medial
malleolus will also provide an additional stabilizing force that
prevents talar subluxation.
the rigidity of the fracture fixation, we recommend careful assessment
of the syndesmosis in all ankle fractures. Traditionally, syndesmotic
stability in ankle fractures has been assessed by pulling the fibula
laterally in the coronal plane either with a clamp or bone hook (i.e.,
the “Hook test”). The distal tibiofibular syndesmosis consists of the
anterior tibiofibular, posterior tibiofibular, and the interosseous
ligaments. Additional stability is provided by the interosseous
membrane and the medial deltoid ligament, both of which may have been
injured to varying degrees.
stressing the fibula anteriorly and posteriorly in the sagittal plane.
Disruption of the syndesmosis will produce significant instability of
the fibula that may be best appreciated in the sagittal plane. The
improved sensitivity of this testing method was recently described in a
cadaveric study (15).
syndesmotic fracture fixation. These issues include screw diameter,
number of screws, number of cortices engaged, timing of weight bearing,
and the need and timing of screw removal.
syndesmotic fixation because of its increased strength and its ease of
removal. However, it requires availability of an additional implant
set. The larger head can be easily palpated at the time of removal and
there is no risk of incorrectly removing one of the small-fragment
screws. We generally engage only three cortices except in cases of
severe osteopenia, in which case it may be advantageous to place a
screw across the far tibial cortex to improve purchase. The use of
three cortices allows some angular freedom of the screw and may prevent
mechanical screw fracture. Except in cases of very proximal fibular
fractures (Maissoneuve injury), we only use a single syndesmotic screw.
We generally allow patients to weight bear on their syndesmotic screws
after 6 weeks and plan removal of the syndesmotic screw at 3 months.
This can usually been done in the office under local anesthesia.
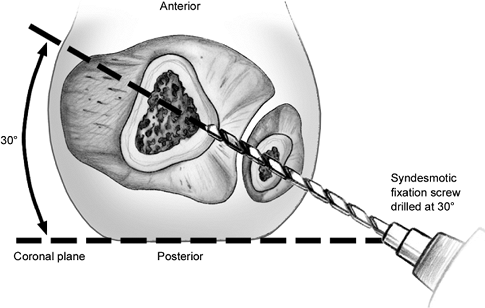
-
Elevate the heel on a towel roll to allow
the surgeon room to position the drill to direct the screw correctly.
Because the fibula is located at the posterior border of the tibia,
syndesmotic screws should be angled anteriorly approximately 30 degrees
from the coronal axis. -
Position the ankle in neutral
dorsiflexion. Because the talar dome is wider anteriorly than
posteriorly, fixation with the ankle plantarflexed may, in theory,
overtighten the mortise. -
Reduce the syndesmosis. The syndesmotic
reduction can usually be held manually with light pressure, although
temporary K-wire fixation may also be used. Caution should be exercised
in using any type of clamp because if the clamp is not perfectly
centered its use may create unappreciated malrotation or translation of
the fibula. -
A 3.2-mm drill hole is made approximately
2 cm above the ankle joint. This should be parallel to the ankle joint
and directed anteriorly approximately 30 degrees (Fig. 33.15).
 |
|
Figure 33.15. Syndesmotic fixation screws should be directed approximately 30 degrees anterior to the coronal plane.
|
total length with a depth gauge. In most cases, we choose a screw
approximately 1 cm shorter than the measured length so the far cortex
is not engaged. In cases of severe osteopenia, we choose to engage the
far cortex. The fibula and near cortex is then tapped with a 4.5-mm tap
and the screw is inserted. Accurate reduction is then confirmed with
bi-planar fluoroscopic views of plain radiographs.
fracture is not internally fixed, we manually reduce the syndesmosis
and secure it provisionally with one or more K wires. After the
reduction is confirmed with bi-planar fluoroscopic imaging, we place
two 4.5-mm screws as described above.
In addition to evaluation of fracture reduction and hardware position,
we look for radiographic parameters of anatomic syndesmotic reduction.
With the AP and mortise views, we verify adequate tibiofibular overlap.
We also examine the position of the fibula with respect to the
incisura. While specific measurements may vary based on the x-ray beam
ankle, on the AP view the fibula and tibia should overlap by at least 6
mm, and the distance between the medial border of the fibula and the
incisura should be less than 6 mm on any view. Equivocal findings merit
comparison to the contralateral-ankle stress radiographs. If there are
equivocal findings following syndesmotic ORIF, then we recommend CT to
evaluate proper position of the fibula within the tibial incisura.
Finally the length of the fibula is assessed by evaluating the
talocrural angle, which on average should measure 83 (±4) degrees (see Fig. 33.2).
who underwent ORIF, significant improvements in all domains of the
SF-36 Health Survey, except for general health, were seen between 4 and
20 months after the operation. However, after 20 months their physical
functioning scores remained below those of the US population norm (16).
patients undergoing operative treatment of displaced Danis-Weber type-B
ankle fractures. At 24 months, the authors noted significantly lower
SF-36 physical function and role physical scores compared to the US
norms (17).
applied to the wounds and held in position with sterile cast padding.
With the ankle held in neutral dorsiflexion, additional cast padding is
applied followed by a short-leg, posterior, stirrup splint. The splint
is maintained until the patient can comfortably dorsiflex the injured
ankle and thus prevent equinus contracture. The leg is elevated
postoperatively to minimize swelling. Patients with sufficient
home-care assistance may be discharged directly home, but many patients
require overnight observation.
and 14 days after surgery. The splint is removed and if adequate wound
healing is evident, the sutures are removed. Radiographs are checked to
confirm maintenance of reduction. Reliable patients are instructed in
active ankle and subtalar range-of-motion exercises. Patients are
placed in a removable short-leg orthotic.
postoperatively. Repeat x-rays are obtained at 6 weeks, and patient
weight bearing is advanced at this time. If necessary, physical therapy
is initiated to assist with regaining range of motion, proprioception,
and strengthening.
months and may require use of compression stockings or elastic wraps.
Patients are cautioned against returning to sports until they have
regained adequate strength and agility. Return to driving is left to
the patient’s judgment, although a recent study has shown that
simulated braking time returned to normal at 9 weeks following internal
fixation (1).
appreciate initially the complexity of the ankle fracture pattern.
While many ankle fractures are simple standard fractures that can be
easily fixed with anticipation of an excellent outcome, other fractures
will be more complex and anatomic reduction may be difficult. The
physician’s failure to appreciate the size of a posterior malleolar
fragment, the presence of articular impaction, or intra-articular
fragments will likely predispose the patient to a suboptimal outcome (18).
problematic following ankle fracture. If independent range-of-motion
exercises and stretching is not rapidly successful in restoring a
functional range of motion, early referral should be made to physical
therapy. Rarely, a posterior, soft-tissue, capsular release along with
lengthening of the Achilles and other flexor tendons may be indicated
to improve severely restricted ankle dorsiflexion.
severe osteopenia. Newly developed locked-screw plate constructs may be
considered to improve stability in certain circumstances. The use of
injectable one-graft substitute pastes that harden in situ has been
shown to improve screw purchase in patients with severe osteopenia.
Insertion of intramedullary K wires to cross thread with the fibular
plate screws has also been said to improve fixation in both
biomechanical and clinical studies (19).
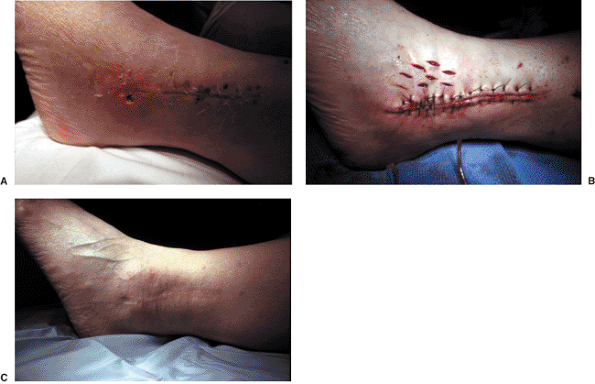
drainage or wound breakdown with accompanying erythema. Operative
debridement and culture-specific antibiotics are usually required.
Because of the risk of ankle joint involvement, ankle aspiration
through a noncellulitic area is also suggested. Once the infection is
under control and the soft tissues are healthy, delayed tension-free
closure can be performed. Tension relief using a “pie-crust” technique
may be helpful to obtain a tension free closure (Fig. 33.16). Small stab wounds are placed in the skin and allowed to heal by secondary intention.
fractures is not known. While it is generally thought to be low, few
reported long-term follow-up studies are available. A higher percentage
of poorer results have been seen with studies reporting relatively
long-term follow-up (20). Posttraumatic
arthritis can be anticipated in cases where there has been significant
articular cartilage damage, such as may seen in supination-adduction
fracture patterns, and where malreduction is followed by talar
subluxation. Factors reported to be associated with the development of
posttraumatic arthritis include a shortened fibula, a widened ankle
mortise, and Danis-Weber type-B fractures.
Patients with nonunion usually present with persistent pain localized
to the fracture site. Shortening and malrotation of the fibula can
frequently occur after both operative and nonoperative management of
malleolar fractures (21,22).
This can lead to ankle valgus and disruption of talocrural mechanics.
Various lengthening osteotomies for the fibula that can restore normal
joint mechanics and alleviate clinical symptoms have been described (23).
 |
|
Figure 33.16. A. Breakdown of distal fibula wound with exposed screw head. B. After excision of the affected area, the pie-crust technique was used to permit skin closure. C. The small pie-crust stab wounds heal by secondary intention.
|
following ankle fracture fixation due to the subcutaneous location of
the hardware (24). This most commonly involves
lateral fibular plates and screws. Symptomatic relief can usually be
obtained with outpatient hardware removal after the fracture is
adequately healed. We normally encourage patients to wait 1 year from
the time of surgery before removing their hardware. Patients are
permitted full weight bearing after hardware removal but are cautioned
against activities that could cause significant torsional force for 6
to 12 weeks following hardware removal.
overlying their fracture hardware. Of the 22 patients with
hardware-related pain who had undergone hardware removal, only one half
had improvement in their lateral ankle pain following hardware removal.
In addition, functional outcome scores were poorer for patients with
pain overlying lateral-ankle hardware than in those with no pain at
this location; this poorer outcome seems to be independent of whether
the hardware had been removed.
KA, Amirtharage M, Tejwani NC, et al. Ankle stress test for predicting
the need for surgical fixation of isolated fibular fractures. J Bone Joint Surg 2004;86:2393–2398.
DC, Otto JK, McKinley TO, et al. Kinematic and contact stress analysis
of posterior malleolus fractures of the ankle. J Orthop Trauma 2004;18:271–278.
DB, Motamed S, Hedman T, et al. The effect of fibular malreduction on
contact pressures in an ankle fracture malunion model. J Bone Joint Surg Am 1997;79:1809–1815.
J, Blagg S, Bishay M. The efficacy of the A-V impulse system in the
treatment of posttraumatic swelling following ankle fracture: a
prospective randomized controlled study. J Orthop Trauma 2004;18:596–601.
DB, Ghalambor N, Perlman M. Intermittent pneumatic pedal compression
and edema resolution after acute ankle fracture: a prospective,
randomized study. Foot Ankle Int 1997;18:347–350.
JS, DeCoster TA, Firoozbakhsk KK, et al. Plain radiographic
interpretation in trimalleolar ankle fractures poorly assesses
posterior fragment size. J Orthop Trauma 1994;8:328–331.
KA, Sheikhazadeh A, Mogatederi S, et al. Lower-extremity function for
driving an automobile after operative treatment of ankle fracture. J Bone Joint Surg 2003;85:1185–1189.
K, Martin CH, Boden SD, et al. Operative treatment of syndesmotic
disruptions without the use of a syndesmotic screw: a prospective
clinical study. Foot Ankle Int 1994;15:407–414.
JJ, Burrow D, Bromage S, et al. Instability of the tibio-fibular
syndesmosis: have we been pulling in the wrong direction? Injury, Int J Care Injured 2004;35:814–818.
WT, Dirschl DR, Crowther JD, et al. Change over time of SF-36
functional outcomes for operatively treated unstable ankle fractures. J Orthop Trauma 2002;16:30–33.
M, Sprague S, Hanson B, et al. Health-related quality of life following
operative treatment of unstable ankle fractures: a prospective
observational study. J Orthop Trauma 2004;18:338–345.
GS, Hoiness PR, Skraamm I, et al. Use of a synthetic bone void filler
to augment screws in osteopenic ankle fracture fixation. Arch Orthop Trauma Surg 2004;124:161–165.
KJ, Petraco DM, Kummer FJ, et al. A new technique for complex fibula
fracture fixation in the elderly: a clinical and biomechanical
evaluation. J Orthop Trauma 1997;11:28–33.
A. The role of fibular length and the width of the ankle mortise in
post-traumatic osteoarthritis after malleolar fracture. Int Orthop 1998; 22:357–360.
OL, Dirschl DR, Obremskey WT. Incidence of hardware-related pain and
its effect on functional outcomes after open reduction and internal
fixation of ankle fractures. J Orthop Trauma 2001;15:271–274.
