Fractures and Dislocations of the Midfoot and Forefoot
overall health, activity, and emotional status of patients. A recent
study looking at the outcomes of multiple trauma patients with and
without foot involvement found a significant worsening of the outcome
in the presence of a foot injury.110
Their conclusion is that more attention and aggressive management need
to be given to foot injuries to improve the outcome of multiply injured
patients.
diagnose. Its unique function to provide a stable platform for weight
transference as well as adapt to various irregular surfaces place
specific, significant demands on its component parts. To adequately
diagnose and treat foot injuries, it is important to understand these
unique features. Attention to detail is important for accurate
diagnosis. Previous chapters have covered the treatment of the hindfoot
structures, the talus and calcaneus; now the discussion will turn to
the midfoot and forefoot.
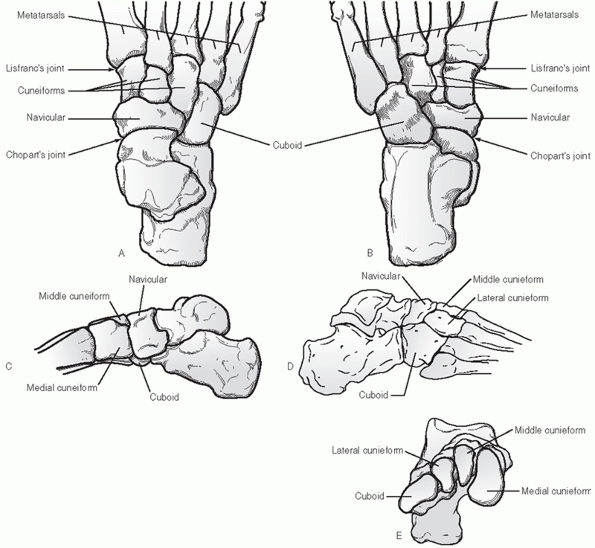
distal to Chopart joint line and proximal to Lisfranc joint line. Five
bones compose the midfoot: the navicular, cuboid, and medial, middle,
and lateral cuneiforms (Fig. 60-1). This anatomic unit plays a distinct role in the normal mechanics of foot function.100
There is no bony weight-bearing contact with the ground in this area in
the normal foot structure. Despite the presence of many large, broad,
flat articular surfaces, this collection of bones is also relatively
immobile compared with the rotatory and accommodative functions of the
hindfoot and forefoot.
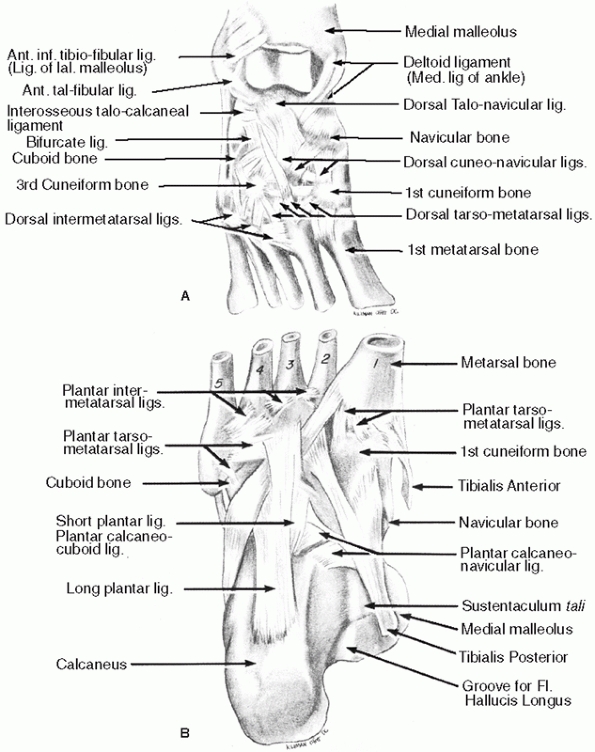
clearly related to its anatomic structure. The stability or resistance
to movement in these articulations is caused in large part to the
numerous dense plantar ligaments, which tightly bind the osseous
structures in the midfoot together (Fig. 60-2). These ligaments also carry over to the hindfoot and medial forefoot,
providing strong mechanical links between the three sections of the
foot. The fact that the normal arch shape of the weight-bearing foot
can be maintained without the need for muscle action demonstrates the
inherent stability supplied by these dense ligamentous structures.
Mechanically, this section of the foot can be represented as a
multisegmented beam. The strength and stability of the whole structure
are dependent on the tensile strength of the plantar-based
intersegmental ties between the osseous structures. The only motor unit
to completely insert into the midfoot is the tibialis posterior. Its
multiple insertions on the plantar surface of the midfoot bones are
intertwined with the plantar ligamentous structures to provide dynamic
support and mechanical overload protection. There are minor variable
insertions of the tibialis anterior and the peroneus longus onto the
plantar aspect of the medial cuneiform, but the posterior tibial muscle
is effectively the only motor unit to control movement in the midfoot.
Its attachment to all five bones of the midfoot ensures movement as a
unit.
 |
|
FIGURE 60-1 Bony anatomy of the midfoot. A. Dorsal view. B. Plantar view. C. Medial view. D. Lateral view. E. Coronal view.
|
function. The medial arch provides a protective conduit and alcove for
the neurovascular structures and intrinsic musculature of the plantar
aspect of the foot. These muscles are extremely important to the
function and stability of the weight-bearing surfaces of the forefoot.
As a rigid beam, the midfoot solidly binds the forefoot to the hindfoot
through the full arc of subtalar motion. During weight bearing, the
midfoot acts as a mechanical actuator transmitting the rotational
motion of the hindfoot complex to the forefoot.100
The midfoot, because of its axial rigidity, is also responsible for the
weight-bearing relationship of the hindfoot to the forefoot. Relative
changes in the position of the medial and lateral aspects of the
midfoot can lead to significant distortions in forefoot/hindfoot
alignment.
move, and cadaveric studies show that motion does occur between the
individual bones of the midfoot.85 This motion is small compared with the motion of the subtalar complex and metatarsophalangeal
joints, but it plays a role in shock absorption during weight bearing.
The functional descriptive is that of a leaf spring that provides
essential dampening and recoil of repetitive loading forces.
 |
|
FIGURE 60-2 Ligamentous structure of the midfoot. A. The dorsal view shows extensive overlap of the interosseous ligaments. B.
The plantar ligaments are thicker than their dorsal counterparts and are dynamically reinforced by the tibialis anterior, tibialis posterior, and peroneus longus tendons. Note the extensive attachments of the tibialis posterior throughout the midfoot bones. |
the various functions of this section of the foot should be considered.
Stability is of paramount importance. The structural integrity of the
five bones and their positional relationship to each other are key to
retaining midfoot function. Second, maintenance of the normal
relationship of the weight-bearing surfaces of the hindfoot to the
forefoot should be considered. This requires attention to the
maintenance of talonavicular, calcaneocuboid, and fifth tarsometatarsal
joint motions. The least important consideration is to maintain the
articular integrity of the surfaces between these five bones. They
should be readily sacrificed for the restoration of bony stability and
the preservation of the major end articular surfaces. An important tool
in determining the presence of instability is the weight-bearing
radiograph. Regular views of the foot while the patient is applying
full single-limb weight can be very instructive in displaying the
relative stability of the foot articulations. This does not substitute
for a computed tomography (CT) scan, which is vital to fully appreciate
the extent of bony injury both stable and unstable.89
position or ability to glide over the talus, can greatly impair foot
function. Both direct and indirect forces have a role in disruption of
the normal navicular architecture. A direct blow, although uncommon,
can cause avulsions to the periphery or crush injury in the
dorsal-plantar plane. More often, indirect forces of axial loading
either directly along the long axis of the foot or obliquely cause
navicular injury. Injury may be sports related, secondary to a fall
from a height, or to the result of a motor vehicle collision.66,96,99 Because of the cross interaction of the surrounding
bony and soft tissue structures, injury to adjacent structures is
likely and must be carefully ruled out where a navicular injury is
found. Significant injury to the cuboid or intercuneiform structures
can occur with relatively low-level oblique loads. These collateral
injuries must also be recognized and treated accordingly.27
of a direct blow but also can serve as a subtle marker for significant
collateral injury to the midfoot from either a ligamentous or a bony
standpoint. Dorsal rim fractures are the most common. Careful
evaluation of the foot clinically and with stress radiographs should be
done to rule out other potential injuries. Tuberosity fractures are
usually the result of forced eversion of the foot resisted by the pull
of the tibialis posterior tendon. A direct blow can also be responsible
for a tuberosity fracture. They rarely displace because of the thick
surrounding ligamentous support but can cause significant long-term
pain and disability if neglected.
midfoot deformity and loss of function to subtle chronic pain and local
tenderness. The contour of two thirds of the navicular is readily
palpable in the foot. Following injury, local tenderness to palpation,
ecchymosis, or local edema warrants further investigation. Passive
motion through the subtalar joint complex should be smooth and
comparable to the contralateral side. As with any foot injury,
anteroposterior (AP), lateral, medial oblique, and lateral oblique
views should be obtained to ascertain the extent of injury to the
navicular as well as rule out collateral damage. If the patient is
ambulatory, the initial films should be weight-bearing, single-leg
stance if possible, to fully appreciate any ligamentous instability.
Medial and lateral oblique radiographs of the midfoot will aid in
assessing the lateral pole of the navicular as well as the medial
tuberosity.
talonavicular joint surface. Because of the concave shape of this
structure, an accurate assessment of congruity is difficult on plain
radiographs. The joint surface is best viewed with anterior-posterior
and medial-lateral cuts of the navicular in the longitudinal plane of
the foot using CT. This study is also helpful for suspected stress
injury,6 which can be differentiated
from acute trauma by the history of prodromal symptoms of pain with
weight-bearing activity over a period of time, minimal repetitive
trauma, and local tenderness over the medial third of the navicular
with perhaps subtle or no visible changes on plain radiographs. These
studies may help visualize the injury pattern as well as the presence
of sclerotic margins.
presence of an accessory navicular, may require magnetic resonance
imaging (MRI) to show the extent of injury to the posterior tibialis
attachment or the synchondrosis located between the accessory and the
navicular tubercle proper. A focused bone scan can also localize the
injury if MRI or CT is not readily available.
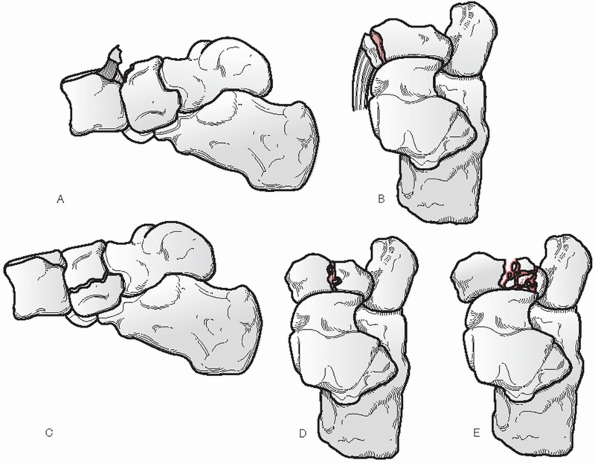
in the literature, which categorize navicular injuries based on injury
pattern. The most commonly used classification has been to categorize
the recognized injuries as tuberosity fractures, cortical avulsion
fractures, stress fractures, and body fractures. Body fractures are the
result of a significant axial load driving the talar head into the
navicular. Body fractures have been further divided into Type I, II, or
III based on proposed mechanism of injury99 (Fig. 60-3).
Although this system does not differentiate treatment needs, it did
correlate well with outcome. The more disruptive the injury, the less
successful is the result.
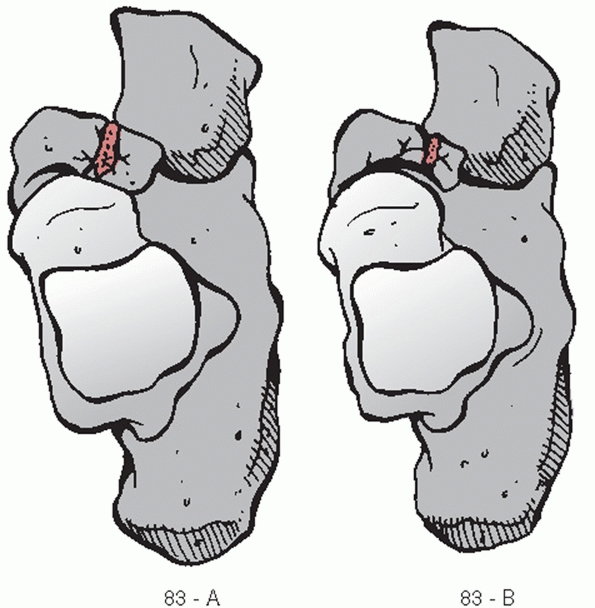
the initially extensive fracture classification for navicular fractures
under the major heading of 83.71 This classification greatly simplifies previously cumbersome variables to grade the fractures as either simple or comminuted (Fig. 60-4).
The designation of navicular fractures under this system observes the
format: (83-_). The subclassification A denotes a simple noncomminuted
fracture. Subclassification B denotes comminution. There is no longer a
subclassification for fracture position, displacement, or joint
involvement. Unfortunately, these issues are important for deciding on
appropriate treatment options and make this classification of little
use except for general classification.
It is wider dorsally and medially than plantar and laterally. This
medial prominence known as the navicular tuberosity provides the
interim attachment point for the posterior tibialis on its medial
inferior surface. Proximally, the articular surface is concave and
articulates with the talus. This joint enjoys a significant arc of
motion and serves to transmit the motion of the subtalar joint to the
forefoot. It is classically the point from which forefoot inversion and
eversion are initiated. The distal articular surfaces of the navicular
have three separate broad facets that articulate with each of the three
cuneiforms. These joints provide little motion as they play mainly a
role in the dissipation of loading stresses. Laterally, the navicular
appears to rest on the dorsal medial aspect of the cuboid with a
variable articular surface.
ligaments plantar and dorsally support the naviculocuneiform joints.
The spring and superficial deltoid ligaments provide strong support to
the plantar and medial aspects of the talonavicular joint. These are
aided by the navicular and calcaneonavicular ligaments dorsally and
laterally. There are also strong ligamentous connections between the
cuboid and navicular laterally and posteriorly.
a radial distribution in the plane of the talonavicular articulation.
The dorsalis pedis and the medial plantar artery feed these perforating
vessels from the dorsal and plantar surfaces, respectively. Perfusion
is abundant along the periphery, but it is relatively avascular
centrally.108 The watershed area is
located in the central third of the navicular body and is the site for
the majority of navicular stress fractures.
navicular involve the shape of the tuberosity and the presence of an
accessory navicular (os tibiale externum). These are present up to 25%
of the time and bilateral in 90%.100
Clinically, the accessory navicular can be seen as a medial prominence
on the foot. It can be present in one of these forms: a fused
elongation of the normal tuberosity, a bone island with a flat
synchrondritic joint separating it from the navicular tuberosity
proper, or a true os
separated completely from the navicular (Fig. 60-5). All three variants are completely within the substance of the posterior tibialis tendon.
 |
|
FIGURE 60-3
The present popular classification of navicular fractures is composed of three basic types with a subclassification for body fractures suggested by Sangeorzan. A. Avulsion-type fracture can involve either the talonavicular or naviculocuneiform ligaments. B. Tuberosity fractures are usually traction-type injuries with disruption of the tibialis posterior insertion without joint surface disruption. C. A type I body fracture splits the navicular into dorsal and plantar segments. D. A type II body fracture cleaves into medial and lateral segments. The location of the split usually follows either of the two intercuneiform joint lines. Stress fractures are usually be included in this group. E. A type III body fracture is distinguished by comminution of the fragments and significant displacement of the medial and lateral poles. |
 |
|
FIGURE 60-4 The OTA classification for navicular fractures.83 Type A denotes a simple fracture. Type B denotes comminuted fracture.
|
not on the pattern of fracture but on the effect it has on the position
of the navicular in the midfoot and the congruity of the talonavicular
joint. It is important to emphasize again that damage to adjacent
structures is not unusual and that careful assessment of the whole foot
needs to be undertaken before treatment is instituted.46,66
The two criteria most important in obtaining a satisfactory outcome are
maintenance or restoration of (a) the medial column length and (b) the
articular congruity of the talonavicular joint. Regardless of the
pattern produced, all isolated nondisplaced fractures of the navicular
should be treated in a short leg cast with non-weight bearing for 6 to
8 weeks6,78 (Table 60-1).
These patients should be followed frequently initially. Late evidence
of instability may be seen once the initial swelling recedes. Repeat
weight-bearing radiographs out of plaster should be done at 10 to 14
days after the initial injury to confirm the absence of bony or soft
tissue instability. If instability appears or other injuries become
apparent, appropriate surgical intervention should be considered. Even
chronic stress
fractures have been seen to do well, treated in a casted non-weight-bearing manner for 8 weeks.6,55
The term “nondisplaced” refers to both the position of the navicular in
the midfoot and the talonavicular joint integrity. The issue of soft
tissue instability is also important. Any loss of naviculocuneiform
integrity or navicular-cuboid stability should be addressed surgically.
Also if other injuries are present in the foot that require surgical
attention, consideration may be given to stabilizing this fracture with
some form of fixation.
 |
|
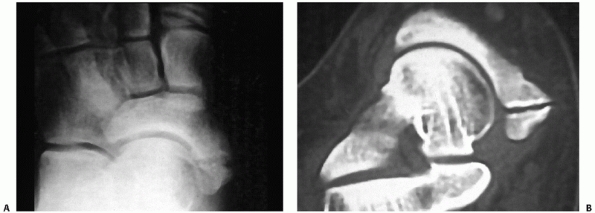
FIGURE 60-5 Accessory navicular. A. Anteroposterior radiograph. B. CT scan showing synchondrosis between the accessory navicular and the navicular proper.
|
unstable injury or fracture resulting in loss of position or loss of
articular congruity. Because the joint is concave in shape, 2 mm of
separation in any plane is considered to represent incongruity. Authors
agree these injuries need to be managed aggressively with surgery.78,96,99
Cortical avulsion fractures found to involve more than the cortical rim
of the weight-bearing surface of the navicular body should be
considered for anatomic restoration. Stabilization of individual
fragments appears to be best accomplished with either 2.7-, 3.5-, or
4.0-mm screw fixation. Immediate use of autogenous cancellous bone
graft should be considered for any area displaying a component of crush
injury. If anatomic restoration to 60% or more of the talonavicular
surface can be accomplished, every effort should be made to salvage the
joint.96,99
If, however, greater than 40% of the articular surface cannot be
reconstructed, an acute talonavicular fusion should be done to preserve
foot alignment.
|
TABLE 60-1 Closed Management of Navicular Fractures
|
|
|---|---|
|
understanding of the fracture pattern and the associated injuries. The
incision should be made in the longitudinal plane with minimal
dissection to prevent significant damage to the vascular supply. The
goal in treating injuries involving the talonavicular joint is direct
visualization of the articular surface to ensure an anatomic reduction.
This is best obtained through a dorsal longitudinal incision over the
area in question (Fig. 60-6). If the fracture
is in the dorsal-plantar plane, the incision should be directly over
the fracture. During the approach, great care should be taken to avoid
injury to the dorsalis pedis artery and the superficial and deep
peroneal nerves, which invariably infringe on the operative
field. Fixation for fractures involving the body and the talonavicular surface should be introduced percutaneously.
 |
|
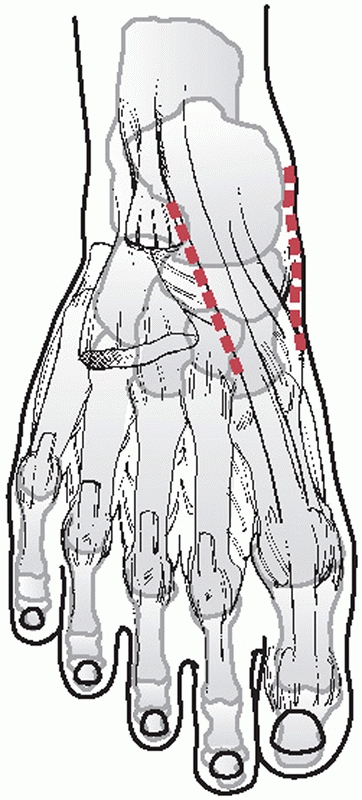
FIGURE 60-6
Surgical approaches to the navicular. The medial incision is between the tibialis anterior and posterior tendons. The dorsal incision is just lateral to the dorsalis pedis artery and medial to the extensor tendons. |
a medial column external fixator can be applied or internal plating can
be used to protect the reduction. The use of a long 2.7- or 3.5-mm
plate to bridge multiple joints temporarily will also halt excess joint
motion until the fracture stabilizes.103
truly stable and nondisplaced along the talonavicular joint should be
treated in a closed manner. A short leg cast is worn without weight
bearing for at least 6 weeks. A repeat full weight-bearing radiograph
of the fracture pattern should be done in the first 2 weeks after
injury to ensure stability and rule out collateral injury. After 6
weeks, progression to weight bearing is allowed only after the patient
is asymptomatic to manual manipulation. Full weight bearing in a cast
or brace is encouraged until the patient is pain free before allowing
unprotected activity. I do not recommend the initial use of
off-the-shelf removable casts because of their inability to hold and
support the foot in a neutral position.
inclination is to protect the fracture in a well-molded cast until they
are completely asymptomatic with full weight bearing. No weight bearing
is allowed for a minimum of 6 weeks, and it should only permitted when
there is no discomfort to manual manipulation. If after 3 months
symptoms are not resolved, reassessment of the fracture should be
undertaken by CT. If no evidence of healing is noted, open bone
grafting of the fracture site should be undertaken along with
compression screw fixation.38 This
usually requires an extra-articular cortical osteotomy over the
fracture site, removal of the fibrous tissue, and placement of bone
graft, followed by lag screw fixation perpendicular to the fracture
line.
or a tuberosity nonunion that has failed casting is best handled with
open reduction and internal fixation to provide compression across the
fracture site. The synchondrosis or fibrous nonunion site should be
completely debrided to expose healthy bone on both sides. Lag screw
fixation with a soft tissue washer to anchor the tibialis posterior
insertion is used. Great care should be taken during the dissection to
minimize disturbance of the tibialis posterior insertion onto the
proximal tuberosity fragment.
The goal is to achieve anatomic reduction of the talonavicular
articular surface and restoration of the supporting position of the
navicular in the midfoot. In the presence of suspected unstable or
incongruent fractures, I find a CT scan oriented perpendicular to the
longitudinal axis of the foot with cuts reconstructed in the sagittal
and transverse planes helpful in assessing talonavicular joint
congruity. Any displacement more than 2 mm should be considered a sign
of instability and aggressively pursued. Also, one should look for
areas of articular incongruity with the talar head, which may represent
an area of joint impaction. The order of importance in achieving a
functional, plantigrade foot should be, first, restoration of navicular
position (including the tuberosity), followed by restoration of
talonavicular congruity. The naviculocuneiform and navicular-cuboid
articulations can be readily sacrificed to achieve these goals.
joint impaction or significant comminution, reduction can be easily
obtained with percutaneous use of a large bone reduction clamp while
the surgeon visually insures reduction of the talonavicular joint.
Percutaneous lag screw fixation perpendicular to the fracture is best
to hold the reduction (Fig. 60-8). In the case
of small medial or lateral fragments or multiple fragments,
continuation of the screw fixation into the surrounding cuneiform
joints or cuboid should be done to obtain a stable construct. To
adequately visualize the talonavicular joint and assist in the
reduction of any fracture diastasis, I routinely use a medially based
small external fixator to obtain and maintain the reduction until
fixation is in place. Pins are usually placed in the talar neck and the
cuneiforms and distracted to restore the normal space for the navicular
to reside. When doing so, however, one must be aware of any instability
in the intercuneiform joints. Their proximal articular surfaces should
align smoothly with one another. Failure to maintain this relationship
can make stable anatomic reduction difficult (Table 60-2).
reduction remain the same. Every effort should be made to restore the
talonavicular joint congruity. Once the joint is restored, any
remaining void in the body of the navicular should be filled with
corticocancellous autograft. Stabilization in these instances is
obtained by placing screws into the adjacent bones (Fig. 60-9).
Significant disruption of any naviculocuneiform joint should be
addressed with removal of the remaining articular surface and immediate
fusion. These three joints are more valuable to foot function when
stable rather than mobile.
60% of the articular contour of the talonavicular joint, an acute
talonavicular fusion should be done. This situation can occur with
severe central or lateral crush of the joint surface. At this point,
preservation of overall foot alignment takes precedence over
talonavicular function. In this case, an appropriately sized
tricortical iliac crest graft should be used to fill the comminution
void between the talus and cuneiforms. A complete fusion of all
naviculocuneiform joints and the talonavicular joint should be the
goal. It is critical to maintain the normal medial column length and
arch contour during grafting and fixation. In the absence of other
injuries to the foot requiring a more extensive fusion, I would not
recommend a double or triple arthrodesis as the initial procedure.
should be placed in a well-molded plaster cast with the foot in a
plantigrade position. Again, I do not recommend off-the-shelf braces
because they do not provide full stable contact to the foot for the
first 6 weeks. Non-weight bearing should be maintained for a full 3
months to allow for both bony and associated soft tissue healing. If
restoration of the talonavicular joint is achieved, non-weight-bearing
patient-directed range-of-motion exercises of the subtalar joint
complex begin at 6 weeks. The patient is kept in a protective removable
cast boot at all other times. Progressive weight bearing as tolerated
is instituted at 8 weeks and advanced only as the patient’s symptoms
permit. The patient remains in a supportive brace until pain-free full
weight bearing is achieved.
 |
|
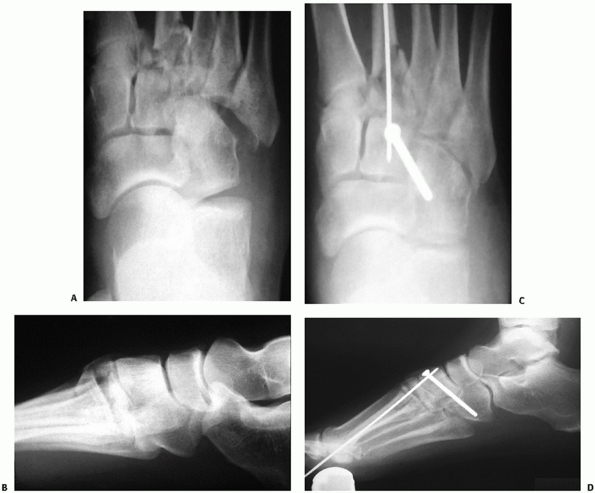
FIGURE 60-7 Displaced closed navicular fracture. A,B. Anteroposterior and lateral films of comminuted fracture of the navicular with disruption of the articular body. C. Preoperative CT scan showing extent of injury to navicular. D,E. Postoperative anteroposterior and lateral with navicular reduced and stabilized with two 3.5-mm lag screws.
|
 |
|
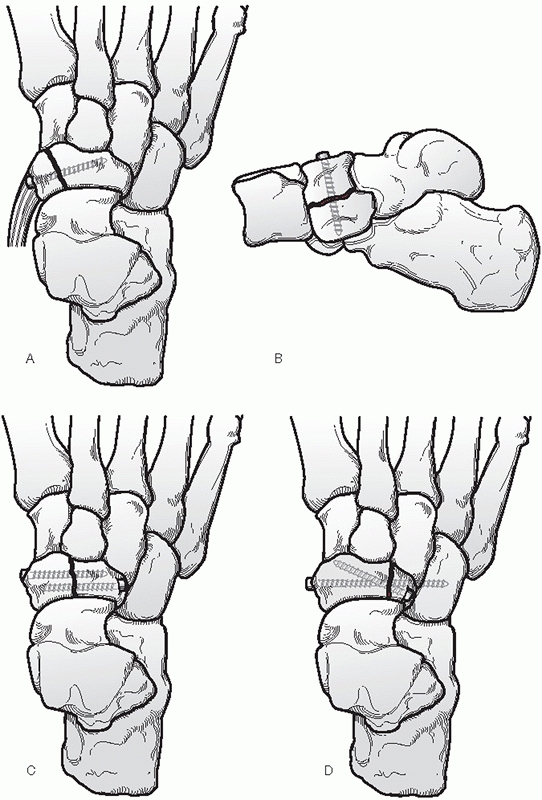
FIGURE 60-8 Suggested fixation methods for simple navicular fractures. A. Tuberosity fracture repaired with a 3.5-mm cortical lag screw and a soft tissue washer. B.
Type I body fracture. The joint reduction is observed through a medial incision and lag screws are placed percutaneously dorsal to plantar. C. Type II body fractures are reduced with direct visualization of the fracture from a dorsal incision with percutaneous lag screws placed from either medial or lateral position. D. In the event that the lateral fragment is too small for stable fixation, the screws should be carried into the cuboid to ensure stability. |
|
TABLE 60-2 Operative Management of Navicular Fractures
|
||||
|---|---|---|---|---|
|
include nonunion of the fracture fragments, arthritic degeneration,
late instability, loss of normal foot alignment through bony resorption
or collapse, and avascular necrosis. Avascular necrosis can be evident
as early as 8 weeks from injury and is usually centrally located in the
navicular. Without subsequent osseous collapse, it is usually
asymptomatic. There is no evidence to suggest that avoiding normal
weight bearing in the presence of avascular necrosis once the fracture
has completely healed will prevent subsequent collapse. In treating
these complications, the principle
of
restoring and maintaining normal bony alignment should remain the
primary goal. Collapse of the body without disruption of the
talonavicular joint should be addressed with corticocancellous grafting
and fusion of the naviculocuneiform joints to restore medial column
position. Loss of the talonavicular articular surface requires a
talonavicular fusion with bone graft as needed to replace avascular
bone and restore column length.
 |
|
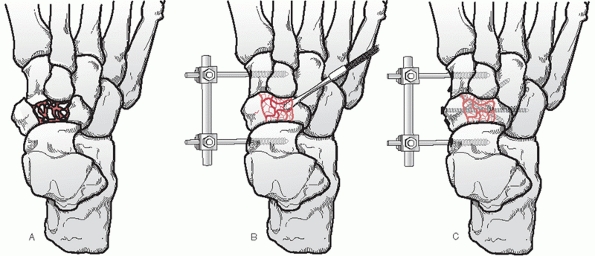
FIGURE 60-9 Reduction and fixation technique for comminuted or displaced navicular fractures. A. Typical fracture pattern with middle to lateral talonavicular disruption. B.
Placement and use of an external fixator aids in restoration of length and maintenance of position for fixation. The talonavicular joint is restored and bone graft placed behind it to fill any void. C. Fixation screws are placed into the cuneiforms or cuboid to secure fracture. |
spring ligament can cause weight-bearing pain and a loss of normal
talonavicular alignment when weight bearing. The picture is similar to
that seen with posterior tibial insufficiency but the pain can be
localized to the area under and just proximal to the navicular
tuberosity. If recognized early enough, surgical reconstruction of the
spring ligament can eliminate the pain and correct the deformity.
subluxation of the navicular is rare. Most cases are noted to be part
of a significant complex disruption involving most, if not all of the
midfoot. When it does occur, the navicular can be found either medial
and plantar to its normal position in the case of neuropathic
instability or dorsal as occurs with acute trauma. The trauma mechanism
appears to be an initial hyperplantarflexion of the forefoot with
subsequent axial loading. The ligamentous disruptions involve the
dorsal naviculocuneiform ligaments first, followed by the plantar
naviculocuneiform ligaments. The plantar talonavicular supporting
ligaments fail last.86 Dislocation
in the neuropathic foot appears to be the result of motor pull with
ligamentous failure. The tibialis posterior pulls the navicular plantar
and medial relative to the foot with the tibialis anterior and peroneus
longus taking the foot dorsally and laterally. The deformity is
progressive, creating a large plantar medial bony prominence and the
likelihood of ulceration.
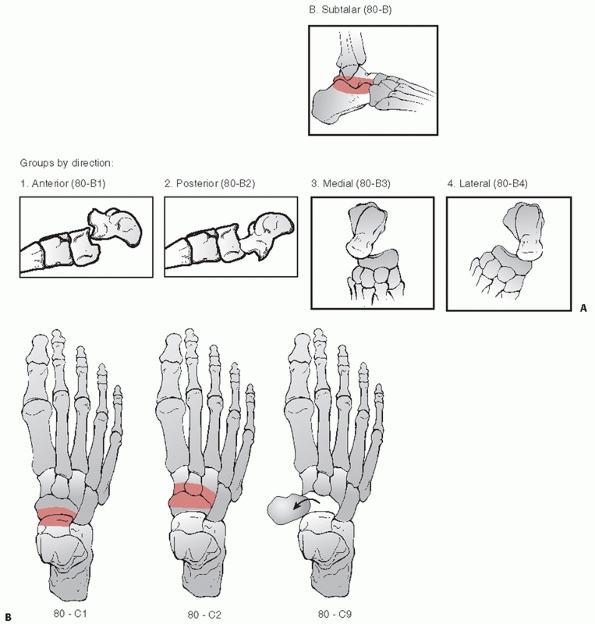
dislocations have not usually been classified. With the recent revision
to the fracture compendium, navicular dislocations are included in the
classification under the general heading of 80 for dislocations in the
foot.71 If the dislocation is
isolated to the talonavicular joint only, the dislocation is designated
80-C1 where the subheading C denotes midfoot and 1 designates
navicular. If the navicular-cuneiform joints are involved, the
designation is 80-C3. Involvement of both joints would fall under the
multiple classification of 80-C9. If the dislocation of the
talonavicular joint is in conjunction with instability of the whole
subtalar complex, then the classification falls under the involvement
of the more proximal joint, the subtalar joint. The designation in this
case is 80-B_, where B denotes the subtalar joint as the primary
dislocation. These dislocations are further subdivided by the direction
of the dislocation and thereby the dislocated position of the
talonavicular joint. The numeric designation for the fourth heading
ranges from 1 to 5 and specifically relates the position of the
navicular bone to the talus (Fig. 60-10).
fracture management. To maintain proper midfoot alignment, anatomic
reduction and stabilization are required. Open reduction is usually
necessary to restore both navicular position and articular congruity. I
find the dorsal approach to the talonavicular joint most useful. It
allows visualization of both the talonavicular and naviculocuneiform
articular surfaces. A small external fixator applied to the medial
aspect of the talar head and cuneiforms greatly facilitates reduction.
Reports in the literature have cited the use of wires and screws to
maintain reduction.29,86,111 Wires
can be used to cross both the talonavicular and the naviculocuneiform
joints. Screws should only be used across the naviculocuneiform joints.
Once reduced, the talonavicular articulation is stable (Fig. 60-11).
 |
|
FIGURE 60-10 Classification of navicular dislocations. A.
When the dislocation of the talonavicular joint occurs with talar-calcaneal disruption, the designation is 80-B. A fourth place numeral is used to designate position of the distal bone: 1 for anterior, 2 for posterior, 3 for medial, 4 for lateral, and 5 for other. B. If the dislocation is in isolation, the designation is 80-C for midfoot dislocation. Here, the fourth digit is used to designate the joint involved. The position scheme described above could be used as a fifth digit but is not part of the official designation. 80-C9 denotes multiple joint involvement in the midfoot. |
collapse of the medial column is a rare but major complication of
navicular dislocation. Significant weight-bearing deformity can occur
with loss of the normal medial midfoot architecture. Treatment would
require a fusion of the involved joints after restoration of the normal
architecture with structural bone graft being used to fill all voids.
Prolonged non-weight bearing is advised until a solid fusion is
obtained.
is usually seen in association with injuries to the talonavicular
joint, with other midfoot structures, or in conjunction with complex
Lisfranc joint injuries.27,28,66,96,97
A small medial or dorsal avulsion fracture of the navicular is
considered a sign of a possible cuboid injury. Without careful
scrutiny, these injuries can be dismissed initially as a lateral ankle
sprain. A cuboid injury can be quite subtle but the long-term
consequences to the lateral column of the foot can cause significant
mechanical problems.28,47
These structural changes include loss of bony arch support, shortening
of the lateral column of the foot, forefoot abduction, and plantar bony
prominence. All of these can distort the normal weight-bearing position
of the foot.
an ankle twist or as part of a high-energy multitrauma event. As with
any foot injury, cuboid fracture can occur with a direct blow. This
type of injury rarely causes articular disruption or axial
shortening.
More commonly, the mechanism of injury is forced plantarflexion and
abduction, causing a compressive load along the long axis of the
cuboid. The resulting injury has been termed a “nutcracker” fracture.47 Variable amounts of axial loading through the fourth and fifth metatarsals add to the variability of the fracture pattern (Fig. 60-12).
 |
|
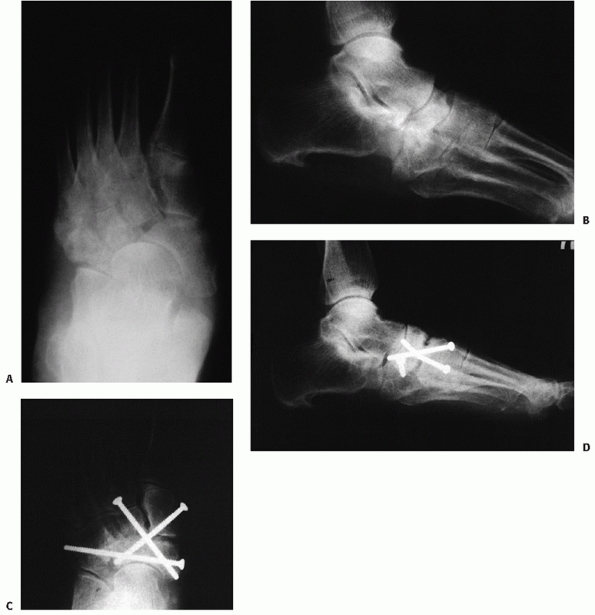
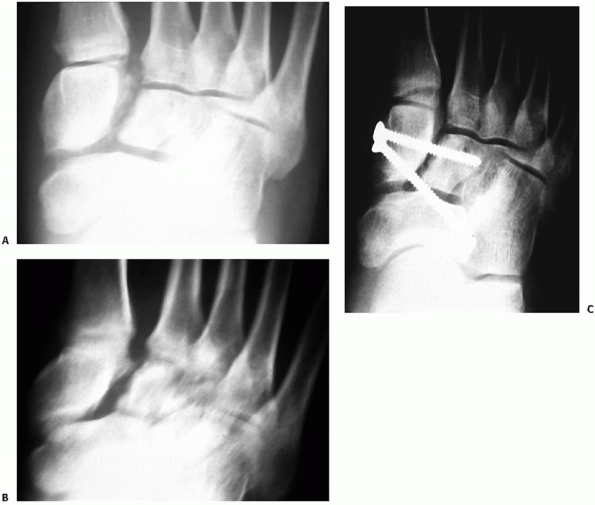
FIGURE 60-11 Neuropathic dislocation of the navicular. A. Anteroposterior radiograph with medial deviation of the navicular. B. Lateral radiograph showing plantar migration. C,D. Fixation post reduction for fusion of the naviculocuneiform joints.
|
severe distortion of the foot anatomy. Dorsolateral pain swelling and
ecchymosis over the lateral midfoot should raise suspicion of a cuboid
injury. In the presence of other injuries to the midfoot such as the
navicular or cuneiforms or tarsometatarsal region, careful inspection
of the cuboid and its articulations is warranted to rule out subtle
instability or injury.
be extremely helpful in assessing cuboid injury. Multiple medial
oblique radiographic views may be needed to see the articular outlines
of both the calcaneocuboid and cuboid-metatarsal joints. As with other
potential midfoot problems, weight-bearing or stress views should be
obtained to rule out interosseous instability of the surrounding
structures. Loss of structural stability can have just as severe an
impact on foot function as a fracture. If injury to the cuboid is
suspected or detected on plain films, a detailed CT scan with
longitudinal and coronal cuts is necessary to assess the extent of
injury and instability. As with other midfoot injuries, loss of
structural integrity and stability are of foremost importance, followed
closely by tarso-metatarsal articular congruity and calcaneocuboid
congruity.
frank dislocation can occur but it is rare. Painful subluxation termed
“cuboid syndrome” has a reported incidence of up to 9% among
high-performance athletes and up to 17% for professional ballet dancers.36,72
Symptoms include lateral foot pain radiating to the anterior ankle,
fourth ray, or plantar aspect of the midfoot. Usually the patient
complains of weakness with forefoot push off. Typically, the finding
for “cuboid syndrome” includes a reduction in dorsolateral to plantar
medial mobility through the calcaneocuboid joint, peroneus longus
spasm, and pain with pressure applied to the plantar aspect of the
cuboid. Similar to
more
severe injuries to the cuboid, the mechanism appears to be forced
pronation of the midfoot in relation to the hindfoot in the presence of
axial loading. This twisting force through the saddle shaped
calcaneocuboid joint can produce incongruity. The presence of the
peroneus longus in its fibrous tunnel on the plantar and lateral aspect
of the cuboid appears to assist in maintaining the incongruity.
 |
|
FIGURE 60-12 Cuboid fracture patterns. A.
Oblique foot radiograph with cuboid impaction fracture at the tarsometatarsal joint. There is also an associated third metatarsal fracture. B,C. Anteroposterior and lateral radiograph of cuboid with calcaneal cuboid impaction. D. Oblique radiograph of cuboid crush with both calcaneal and metatarsal joint involvement. |
most likely the result of a direct medially applied force followed by
axial loading or abduction of the foot. When present, it is usually in
conjunction with other complex injuries to the hindfoot and forefoot.
The position of the dislocated cuboid is always plantar and medial.
Anteroposterior and lateral radiographs that show medial deviation of
the cuboid from the lateral border of the calcaneus suggest instability.
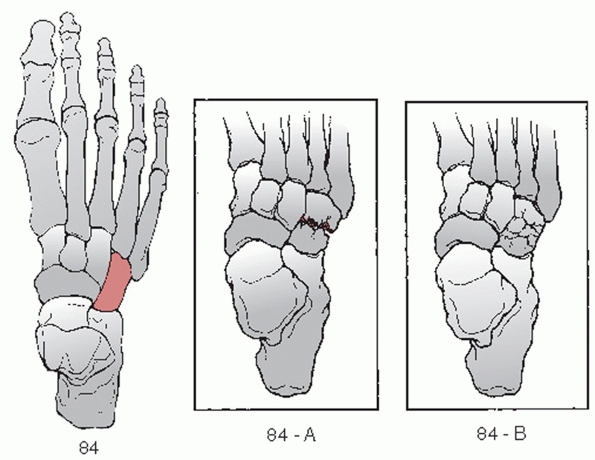
there is no commonly used classification for isolated cuboid fractures.
The Orthopedic Trauma Association (OTA) has revised a general
classification system for cuboid fractures and designated them
numerically as 84 (Fig. 60-13).71 This updated classification
greatly simplifies the cataloging of these fractures. Instead of an
exhaustive list of subheadings, the new system groups all cuboid
fractures as simple (A) or comminuted (B). Unfortunately, the updated
nomenclature does not take into account the joint involvement or
whether there is any shortening of the axial length, two criteria that
are important for determining treatment.
 |
|
FIGURE 60-13 OTA classification of cuboid fractures.84 Type A describes simple fractures. Type B denotes comminuted fracture. There is no subclassification for joint involvement.
|
account structural integrity and interosseous stability. It is perhaps
more helpful to categorize the injuries as nondisplaced, unstable, or
crush for the purposes of management.
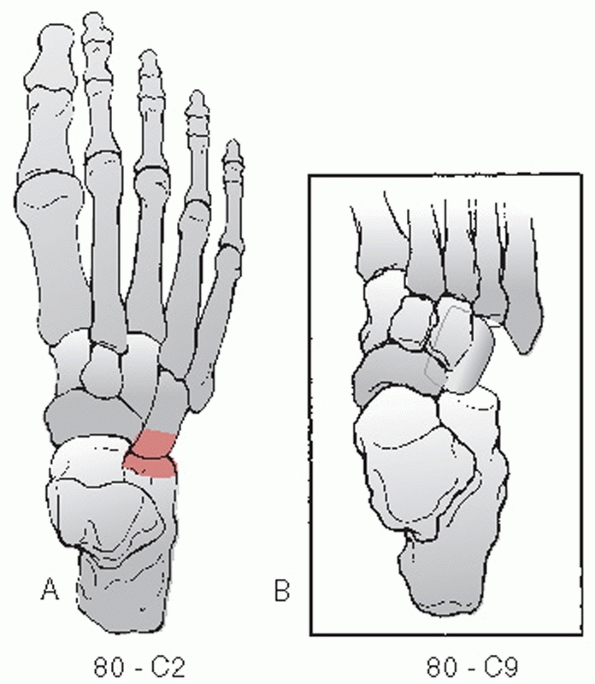
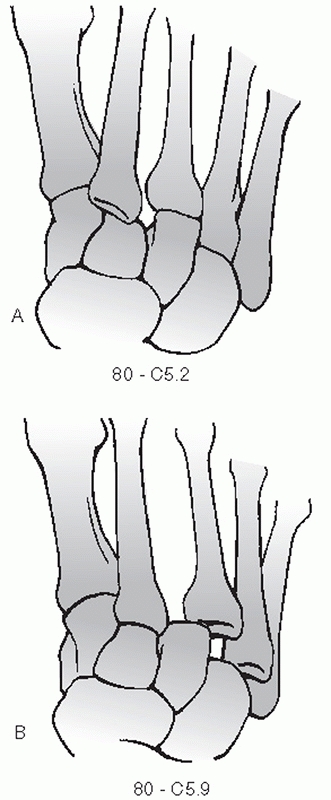
compendium identifies these injuries as 80-C2 when it involves the
calcaneocuboid joint. If the cuboid lateral cuneiform joint is
involved, the designation is 80-C4. And for involvement of the cuboid
metatarsal joints, the designation would be 80-C5.4 for the fourth
metatarsal or 80-C5.5 for the fifth metatarsal if they occurred in
isolation. With both metatarsal tarsal joints involved, the designation
would be 80-C5.9. A true dislocation of the cuboid where it involves
all the joints would be designated 80-C9 (Fig. 60-14).
Its saddleshaped articulation with the calcaneus acts as a stress valve
for the imperfectly matched movements of the talonavicular and subtalar
joints. The dorsal calcaneal tuberosity and medial cuboid tuberosity
are fashioned to provide bony stability to the joint and prevent dorsal
or lateral migration of the cuboid in a weight-bearing situation. Thick
plantar and medial ligaments support those respective areas of the
articulation. Distally, the cuboid provides separate articular facets
for each of the fourth and fifth metatarsals. There are variable
articular surfaces on the dorsomedial aspect of the cuboid where the
navicular and lateral cuneiform come into contact with the cuboid. The
thick, broad, longitudinal plantar ligament provides support along the
plantar and medial borders of the calcaneocuboid joint. A variable
pattern of plantar and dorsal ligaments provides loose support at the
tarsometatarsal joints. It is important to realize that the
cuboid-metatarsal articulations are more important to overall foot
function than the calcaneocuboid articulation. These tarsometatarsal
joints provide for nearly all of the dorsal and plantar motion of the
lateral column of the foot. Studies have shown up to three times as
much available motion at these two joints compared with the medial
three tarsometatarsal joints.85 The
peroneus longus courses along the lateral and plantar surfaces of the
cuboid on its way to the base of the first metatarsal. The importance
of the cuboid in the overall function of the foot lies primarily in its
structural position as a lateral column spacer, followed by the
function of the fourth and fifth tarsometatarsal joints and then by
calcaneocuboid joint motion.
 |
|
FIGURE 60-14 OTA Classification of cuboid dislocations (80-C). A.
Isolated calcaneal cuboid dislocation. Isolated cuboid metatarsal dislocations are classified as a tarsometatarsal dislocation. B. True complete cuboid dislocation. |
the cuboid with no evidence of loss of bony length or interosseous
instability can be treated without operative management. A well-molded
cast and an initial period of non-weight bearing for 4 to 6 weeks is
recommended.78 Again, it is
important to follow these injuries frequently. Weight-bearing stress
radiographs should be obtained 10 to 14 days after the initial
assessment to ensure the absence of occult injuries as the swelling
subsides (Table 60-3). With the reduction of
pain on clinical examination, progressive weight bearing can be
instituted. True cortical avulsion injuries of the cuboid can be
allowed to bear weight as tolerated immediately in an off-the-shelf
short leg walker until asymptomatic. Again, frequent follow-up is
needed to rule out late instability.
should be taken to restore lateral column function and length. Isolated
cuboid-metatarsal instability without cuboid fracture denotes a
Lisfranc-type injury and will be covered under that section (see p. 2136).
sedation to allow the joint to “unlock.” The patient is placed in the
prone position and the hindfoot is fully plantarflexed. With relaxation
of the peroneal spasm, dorsally directed pressure is placed on the
plantar aspect of the cuboid. At the same time, the forefoot is further
plantarflexed. Another reduction method can be performed with the
patient lying supine and the foot suspended by longitudinal traction
applied to the fourth toe and with the forefoot in slight
plantarflexion. Vigorous activity post reduction should be avoided for
24 to 48 hours.
|
TABLE 60-3 Closed Management of Cuboid Injuries
|
|
|---|---|
|
significant disruption of the plantar support structures of the
midfoot. Anatomic reduction and prolonged immobilization are necessary
to preserve midfoot stability. Open reduction is recommended along with
K-wire fixation across the calcaneocuboid joint to hold the reduction.33,49
At 4 weeks, the wires are removed and gentle non-weight-bearing motion
is begun. Weight bearing usually has to wait for adequate healing of
other associated injuries to the foot.
the cuboid should proceed first followed by the other injuries as the
cuboid provides plantar support as well as determines lateral column
length for the remainder of the midfoot. Stabilization of the reduction
can wait until all reductions are complete.
as the results of individual series are difficult to evaluate due to
their small numbers.47,66,96,97
Once disruption of the cortical integrity of the cuboid occurs,
significant compaction of bony length and disruption of articular
surfaces can occur. Nonoperative care in the face of structural
distortion leads to poor results because of late deformity of the foot.
The goals of operative management are to restore the lateral column
length and plantar support of the midfoot first, preserve the mobility
of the tarso-metatarsal joints second, and restore articular integrity
to the calcaneocuboid joint last. Liberal use of autogenous cancellous
bone graft is recommended along with some form of internal and/or
external fixation to maintain and protect the reduction.114
believe it is important to reduce and rigidly fix all compressed or
articularly distorted cuboid fractures. In the case of significant
injury to other parts of the foot, even minimally displaced stable
fractures should be internally fixed to provide support for the other
injured structures. Simple longitudinal fractures are easily fixed with
2.7- or 3.5-mm cortical lag screws across the fracture plane. Fixation
of these fractures should provide increased stability for restoration
of the rest of the foot.
openly if there is more than 2 mm of joint surface disruption, loss of
normal smooth joint motion at either the calcanealcuboid or cuboid
metatarsal articulations, or any evidence of longitudinal compression.
Inevitably, I find the amount of lost lateral column length and
instability is greater than would be expected by preoperative studies.
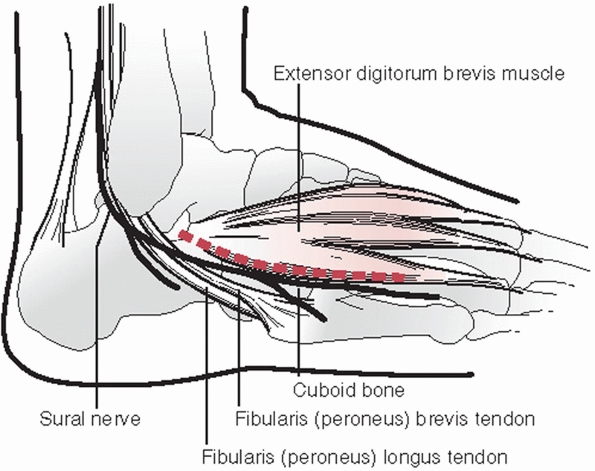
incision over the cuboid at the lateral border of the extensor brevis
muscle (Fig. 60-15). The skin incision extends
from the sinus tarsi distal to the base of the fourth metatarsal. Great
care is taken to identify and protect the sural nerve during this
dissection. Once exposed, a small fixator is used to restore lateral
column length. Two pins are placed in the distal calcaneus and one pin
each in the fourth and fifth metatarsal bases. It is important to be
sure that the articular surfaces of the fourth and fifth metatarsals
are flush in their alignment. With restoration of cuboid position and
articular congruity, abundant cancellous graft is used to fill any
defect (Fig. 60-16). The majority of these
crush injuries have a relatively intact cortical surface with impaction
of one or the other articular surface. Reduction of the ends of the
cuboid allows replacement of the cortex as a buttress behind the
subchondral bone. It is then fixed with 2.7-mm cortical screws. In
other cases, the use of a 3.5-mm tubular plate can be employed as an
internal buttress with screws engaging the medial cortex to secure its
position. Screws or wires into the navicular, cuneiform, and/or
calcaneus can be used if instability is detected in their articulations
with the cuboid. Only smooth K-wires should be used to stabilize the
fourth and fifth tarsometatarsal joints (Fig. 60-17).
 |
|
FIGURE 60-15
Surgical approach to the cuboid. Palpable landmarks are the sinus tarsi and the fourth tarsometatarsal joint. The incision should be dorsal to the sural nerve and plantar to the extensor brevis muscle. |
 |
|
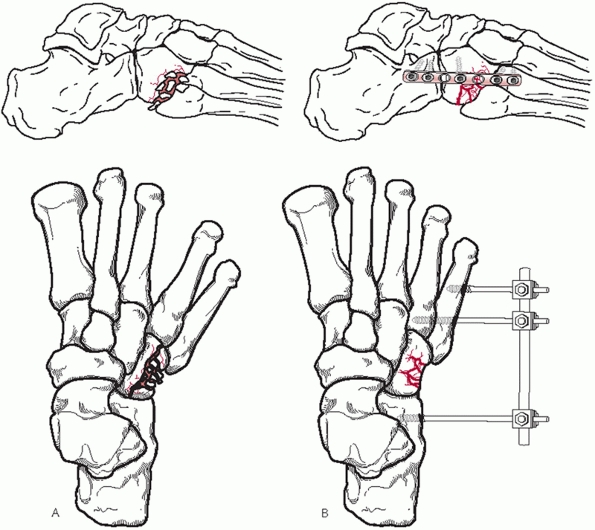
FIGURE 60-16 Restoration of nutcracker fracture of cuboid. A. Typical fracture appearance in anteroposterior and lateral planes. B. Placement of external fixator to restore normal anatomy. Any defect should be filled with cancellous graft. C. Internal stabilization is possible with a 3.5-mm tubular plate to maintain reduction and position of cuboid.
|
compressive stability of the repaired cuboid. If there is any question
of instability, the small fixator is left in place for 6 to 8 weeks to
protect the cuboid from natural compressive forces and to allow time
for bony healing (Fig. 60-18). Regardless of
the amount of articular comminution at either joint surface, I do not
believe there is a role for immediate fusion of the calcaneocuboid or
the cuboid-metatarsal joints.
significant midfoot injury, is best treated with open reduction. A
small external fixator should be used between the calcaneus and fifth
metatarsal to recreate the space for the cuboid. The cuboid can be
easily manipulated back into place with the aid of a threaded K-wire or
small external fixator pin placed through the longitudinal midpoint of
the bone. This “joy stick” can then be used to pull the cuboid
laterally back into its reduced position. A possible block to reduction
can occur if the peroneus longus tendon becomes displaced into the
cuboid-fifth metatarsal joint.31
Once reduction is obtained, it should be maintained with a fixation
screw placed from the lateral cuneiform into the cuboid as well as a
fixation screw or smooth K-wire across the calcaneocuboid joint and or
cuboid-metatarsal joint to maintain reduction56 (Fig. 60-19).
extremity should not be allowed to bear weight until bony and
ligamentous stability is evident clinically. If there is no external
fixation present postoperatively, then a short leg cast with the foot
held in neutral, plantigrade position is used to minimize compressive
forces across the cuboid for 6 weeks. With external fixation present,
some form of plantigrade splint should be used to support the foot and
toes in a neutral, plantigrade position. Any reduction pins including
the external fixator are removed at 6 weeks. After 6 weeks,
non-weight-bearing, self-directed range-of-motion exercises of the foot
through the ankle and subtalar joint should begin with the foot being
protected in a removable cast or plantigrade splint. Weight bearing may
begin at 10 weeks and progress as comfort allows in a removable short
leg walker.
continued or late instability between the cuboid and adjacent
structures, loss of lateral column length, or arthritic degeneration.27,28,47
Any alteration of normal cuboid position can have a profound effect on
the stability of the whole foot. Abduction of the forefoot and midfoot
instability both place the foot at
a
mechanical disadvantage during weight bearing, causing a significant
alteration of gait and pain. Loss of lateral column length would
require a bone graft to restore length with either fusion of the
calcaneocuboid joint or opening wedge osteotomy of the cuboid. Even in
the presence of significant arthropathy in the fifth tarsometatarsal
joint, fusion in this area produces uniformly bad results.
Interpositional arthroplasty of the symptomatic fifth tarsometatarsal
joint can provide pain relief with continued motion.8
 |
|
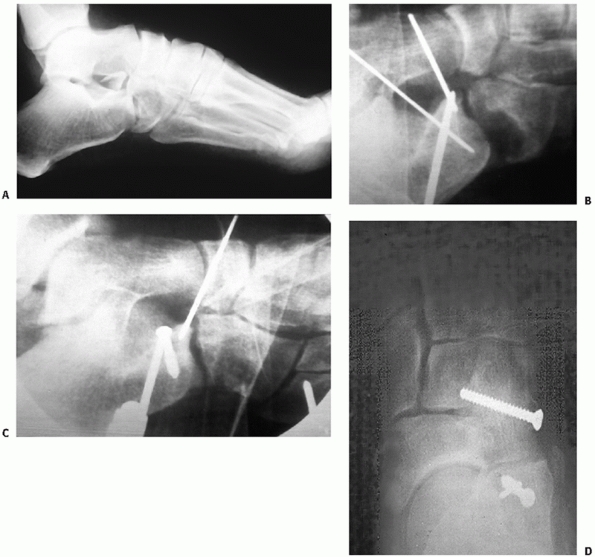
FIGURE 60-17 Cuboid fracture involving the calcaneocuboid joint. A.
Preoperative lateral radiograph of injury at the calcaneocuboid joint. Note the fracture of the anterior process of the calcaneus contributing to the instability. B. Placement of the external fixator allows restoration of anatomic position. C. The articular surface is reduced and the void is filled with cancellous graft. D. The intact cortex is then reduced under the subchondral lip and held in place with screws secured to the medial wall of the cuboid. |
substance of the peroneus longus tendon. It can be found at the level
of the cuboid tunnel where the peroneus longus tendon passes under the
cuboid or at the level of the calcaneocuboid joint. It is present in 5%
to 14% of the population and the majority are bilateral and symmetric.46
Injury to this bone can be caused by a direct blow or supination and
plantarflexion forces, which can place a tensile load across the
structure (Fig. 60-20). Fracture of this sesamoid bone can occur with or without disruption of the tendon.87
Patients usually present with lateral ankle pain on weight bearing
resistant to conservative measures. Tenderness can be localized to the
plantar lateral aspect of the foot proximal to the base of the fifth
metatarsal. Resistance to peroneus longus motion also causes pain. A
medial oblique radiograph will usually reveal the presence of the os
peroneum.
minimum of 6 weeks followed by progressive weight bearing in a cast
until asymptomatic. Despite these measures, a painful fibrous union can
occur, which is best treated with excision of the bone fragments.87
Wide displacement of the fragments indicates disruption of the peroneus
longus tendon. Confirmation of the disruption can be seen on an MRI
study of the tendon. When the treatment fails immobilization or the
fragments require removal, the peroneus longus tendon should be
anastomosed to the peroneus brevis tendon to prevent continued pull on
the plantar scar tissue. This is best accomplished by an incision
posterior to the fibular and proximal to the peroneal retinaculum. Here
a simple side-to-side anastomosis is performed to stop independent
function of the peroneus longus at the plantar aspect of the foot. The
simple technique is very effective in relieving any chronic discomfort
from the injury.
 |
|
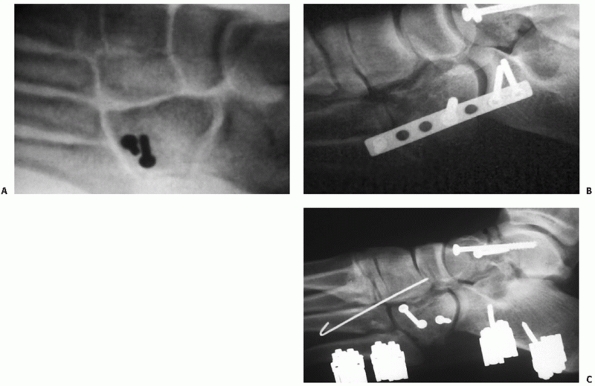
FIGURE 60-18 Alternative methods of stabilizing cuboid fracture repair. A. Interfragmentary screws are best when the outer cortex is relatively intact and resistant to compression. B.
Internal bracing can be done with a neutralization plate spanning both joints to hold anatomic alignment. This will have to be removed within 3 months of weight bearing. C. Continued external fixation is also useful to maintain lateral column length while awaiting bony healing. |
Isolated cuneiform dislocations do occur but are more often associated
with plantar-based fractures of the bone rather than disruption of the
thick plantar ligamentous structure. Commonly, cuneiform injuries are
seen in conjunction with tarsometatarsal joint injuries. Whether injury
to the cuneiform results in a fracture or fracture dislocation, it is
usually the result of indirect axial loading of the bone. The extent of
damage is dependent on the presence of concurrent forces acting on the
foot in a direction perpendicular to the axial load. Plantar flexion
can lead to dorsal dislocation. Dorsiflexion can cause significant
fracture comminution and shortening. Fracture or fracture dislocation
of these bones usually requires significant force and can be a signal
of severe ligamentous injury to the whole of the midfoot.
seemingly minimal energy. A twisting injury to the forefoot during
sports or a fall can cause shortening of the medial ray due to
ligamentous disruption of the intercuneiform ligaments96 (Fig. 60-21).
Clinically, a noticeable increase in the size of the first web space
has been reported for isolated medial cuneiform injuries. This gap sign
is particularly visible when the foot is subjected to full
weight-bearing forces.26
careful close examination of the injured foot. Localized tenderness
over the cuneiform region, pain in the midfoot with weight bearing, or
discomfort with motion through the tarsometatarsal joints can signify
injury to these bones. Anteroposterior, lateral, and oblique
radiographic views should be obtained to assess the extent of injury
and check for injury to adjacent structures. These should be obtained
with single-leg weight bearing if possible; otherwise, manual stress
views with forefoot inversion and eversion are needed to look for
subtle signs of instability. Coronal and longitudinal CT scans of the
midfoot can be used to more clearly define the extent of the injury.
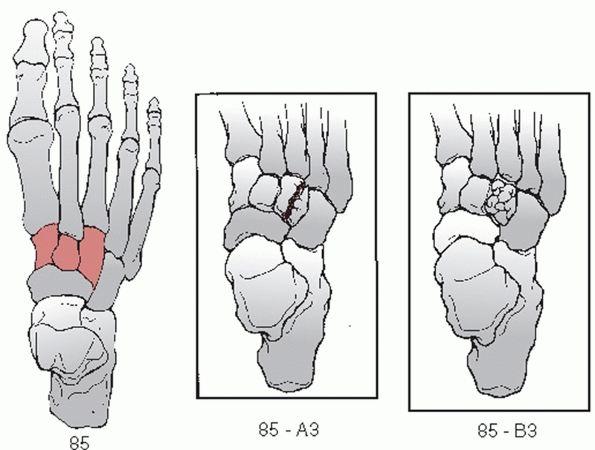
Fractures listed as 85-A are simple fractures and those listed as 85-B
are comminuted. There is a further subclassification to denote which
cuneiform is involved: 1 for medial, 2 for middle, and 3 for lateral.
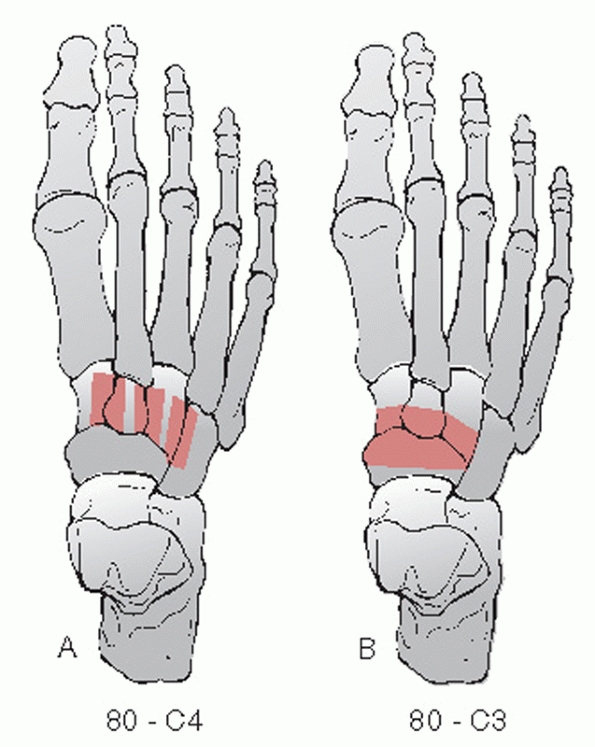
classifications depending on the joint involved. Naviculocuneiform
dislocation is designated by 80-C3. Intercuneiform dislocation is
designated 80-C4, and cuneiform metatarsal dislocation is designated
80-C5. With a cuneiform metatarsal dislocation, there is a numeric
subclassification to denote the metatarsal involved (Fig. 60-23).
There is no specific classification for a complete cuneiform
dislocation; they are simply designated as 80-C9 for multiple midfoot
dislocations.
determination of treatment or outcome is not yet possible by this
system. Treatment should be based not on the pattern of the fracture
but rather on the presence of instability or shortening.
 |
|
FIGURE 60-19 Cuboid dislocation. A. Anteroposterior view of foot showing medial migration of cuboid. B. Lateral film showing plantar migration. C,D. After reduction and fixation with a 3.5-mm screw from the lateral cuneiform into the cuboid.
|
medial column of the foot and provide the rigid support for the medial
longitudinal arch. They constitute the apex of the transverse arch that
provides a stable conduit for the plantar musculotendinous and
neurovascular structures.100 All are
wedge shaped along the axial axis. The medial cuneiform has a plantar
base and a dorsal crest. The middle and lateral cuneiforms are reversed
with dorsal bases and plantar crests. Proximally, each cuneiform
articulates with approximately one third of the distal navicular. Each
cuneiform articulates with its respective metatarsal distally. The
third cuneiform rests atop the cuboid laterally and shares a variable
articular surface with that bone. There are numerous ligamentous
attachments between these three bones and the surrounding structures.
Between each of the two cuneiform pairs, there are three distinct
connecting ligaments. The weakest link structurally is the medial
cuneiform with its sloping proximal articulation with the navicular and
relative paucity of ligamentous attachments to other structures. Of
importance also is the fact that there are no ligamentous connections
between the first and second metatarsal to stabilize the first ray and
dissipate any rotatory forces. Isolated loading of the first metatarsal
is resisted only by the strength of the medial cuneiform attachments.
instability or the loss of position of the individual bones that
requires aggressive treatment. It is the relative stability of the
cuneiforms that is most important for proper foot function. Anatomic
restoration and maintenance of position are required for satisfactory
outcome in these injuries.
dorsal dislocation of the middle and lateral cuneiforms when there is
no evidence of adjacent injury (Table 60-4).
Ankle block anesthesia is used to provide relaxation and pain relief
for closed reduction and manipulation. Longitudinal traction is applied
to the affected ray, and with direct dorsal pressure, a reduction is
attempted.
Successful stable, anatomic reduction can be treated with a
non-weight-bearing short leg cast holding the foot in a neutral,
plantigrade position.84
Off-the-shelf removable walkers should not be used because they permit
too much early motion about the injury site and can lead to late
instability. Careful follow-up is needed to ensure continued reduction.
Percutaneous pins or screw fixation can be used to help maintain
position.
 |
|
FIGURE 60-20 Fracture of the os peroneum. A. Lateral radiograph of acute os peroneum fracture while running. B,C. Three-month follow-up with proximal migration of peroneal fragment up the peroneal tunnel. D. Lateral radiograph of foot after excision of fragments and side-to-side anastomosis of peroneus longus to brevis.
|
treated with open reduction and pin or screw fixation into adjacent
stable structures. Any loss of structural position due to bony crush
should be corrected with cancellous or corticocancellous bone grafting.
Instability of the medial cuneiform requires internal fixation even if
closed anatomic reduction is obtained through traction.64,67 There has been a report of the tibialis anterior tendon blocking reduction of a medial cuneiform dislocation.22
stability, my preference is to treat only stable nondisplaced cuneiform
fractures without surgery. Structural displacement or instability can
be easily and decisively treated with open reduction through a dorsal
longitudinal approach combined with rigid internal fixation. The
incision is based over the cuneiform in question. Care needs to be
taken to identify and protect the neurovascular structures in this area
during dissection. My goal is to preserve structural integrity, and I
strive for intercuneiform and naviculocuneiform fusion of all unstable
articulations. If more than 50% of the articular surface of the
affected tarsometatarsal joint is disrupted, I will consider an acute
fusion of the involved tarsometatarsal joint. Autogenous cancellous
bone graft is used in all cases where anatomic reduction shows evidence
of bone loss. The 2.7- or 3.5-mm cortical screws are used to secure
fixation of the unstable bone into adjacent stable structures (Fig. 60-24).
cuneiform instabilities. Nonunion has been reported for medial
cuneiform fracture and has been treated successfully with open
reduction and internal fixation.15
It appears the only complications are from missed diagnosis or
incomplete reductions whereby pain and instability of the midfoot are
noted.
stable sprains to clinically apparent, grossly unstable deformities.
Regardless of the presentation, any injury of the Lisfranc complex can
result in prolonged recovery and significant long-term morbidity. It is
important to recognize and treat these injuries early and aggressively
for best results. Retrospective studies have found up to 20% of these
injuries go initially unrecognized and can have significant long-term
consequences. High suspicion for this type of injury should be present
following motor vehicle trauma. Significant disruptions can occur and
undergo spontaneous reduction masking the underlying gross instability.
 |
|
FIGURE 60-21 Isolated medial ray instability caused by disruption of the intercuneiform ligaments. A. Initial non-weight-bearing anteroposterior view showing irregularities in the first to second intercuneiform joint. B. Stress view showing instability. Note there is no instability of the tarsometatarsal joints. C. Open reduction through a dorsal approach with percutaneous fixation to reduce and stabilize the medial ray.
|
 |
|
FIGURE 60-22 OTA classification of cuneiform fractures.85
To designate the cuneiform involved, a number corresponding to that cuneiform is placed at the end of the fracture designation. The numeral 1 is for medial, 2 for middle, and 3 for lateral. Type A designates a simple fracture. Type B denotes comminution. |
 |
|
FIGURE 60-23 OTA classification for cuneiform dislocations (80-C). A. The designation for intercuneiform joint disruption. B. The designation for naviculocuneiform dislocations.
|
|
TABLE 60-4 Closed Management of Cuneiform Injuries
|
|
|---|---|
|
 |
|
FIGURE 60-24 Middle cuneiform fracture dislocation. A. Lateral radiograph of a dorsal fracture dislocation of the second cuneiform with a fracture of the third. B. CT scan of bony destruction in the midfoot. C. Complete dislocation of second cuneiform on opening the skin. D.
Rigid internal fixation with 3.5-mm lag screws in attempt to fuse the middle cuneiform to the medial and lateral cuneiforms. The navicular screw was to stabilize an associated body fracture. |
through a wide range of insults. Subtle injury to the ligamentous
structure can occur through sports or other low-impact trauma. More
significant bony injury and instability usually occur from high-energy
trauma such as a fall from a height or a motor vehicle collision. Two
mechanisms of injury are described.109,113,117
A direct loading of the joint complex along the dorsal surface in the
manner of a crush injury or an object falling on a stationary foot can
result in ligamentous or bony disruption anywhere along the joint line.
The pattern will vary depending on the point of application of the
force. Significant soft tissue damage can occur with this type of
injury and hamper subsequent treatment.
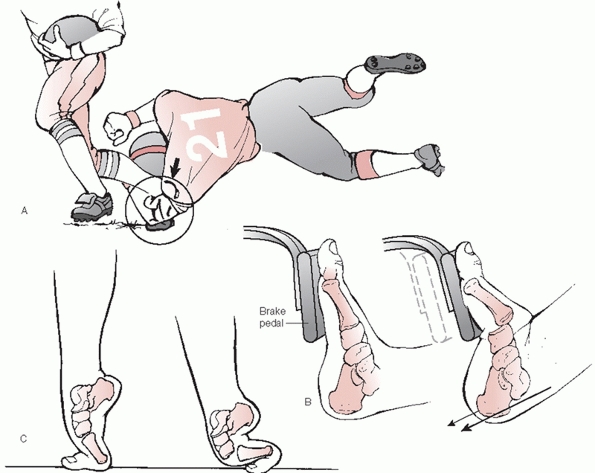
significant disruption of the whole complex. It is characterized by longitudinal loading of a plantarflexed foot.24,37,76,80,113
This causes hyperplantarflexion across the long axis of the foot,
disrupting first the dorsal ligaments and then the plantar ligaments
with a variable extent of bony injury. The resulting pattern again is
dependent on the amount of force and the presence of secondary forces
acting about the long axis of the foot. This is the most common
mechanism for sports injuries (Fig. 60-25).
There can be a significant amount of collateral injury as well with
these injuries. Fractures of the cuneiforms, cuboid, and or metatarsals
are common. The second metatarsal is the most frequently fractured.
Ligamentous disruptions involving the intercuneiform joints or cuboid
stability have also been recorded. Again their presence is dependent on
the amount of loading force and the presence of secondary forces.
Published studies to date do not show any true relationship between
mechanism of injury and the resultant pattern.
of the foot in question. In the case of isolated injury, pain anywhere
over the tarsometatarsal joint complex is significant for a possible
injury. Passive dorsiflexion and plantarflexion of individual
metatarsal heads will elicit pain at the proximal articulations. Pain
at the midfoot with attempted single-limb heel lift also points to a
potential Lisfranc injury. The presence of plantar ecchymosis is also
suggestive of ligamentous injury.
 |
|
FIGURE 60-25 Indirect injury to the tarsometatarsal joints. A. Axial load to the foot in fixed equinus as in football. B. Axial loading in the presence of descending stairs or operating a brake pedal C. Axial loading resulting from a fall from a height.
|
treatment of this injury. It is used to assess the stability of the
joint as well as to catalog the presence of collateral injuries. If
possible at the time of presentation weight-bearing films of the foot
in an AP, lateral, and 30-degree medial oblique position should be
obtained. Because of the possibility of spontaneous reduction in these
injuries non-weight-bearing films provide no loading of the ligaments
to test their integrity.37
Weigh-bearing films provide a readymade stress film of the joint
complex. If the patient is unable to bear weight due to pain or the
presence of other injuries, non-weight-bearing films are still useful
as a preliminary evaluation. On each of the three views, the observer
is looking for a disruption of the normal in line arrangement between
the metatarsal base and the opposing tarsal bone. The AP view allows
assessment of the alignment of the lateral border of the first
cuneiform with the first metatarsal base and the medial border of the
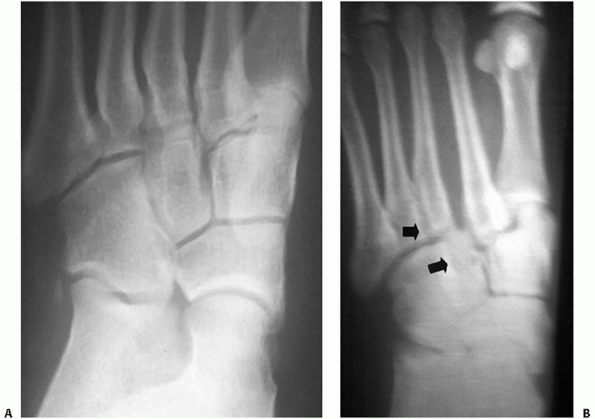
second metatarsal base with the second cuneiform (Fig. 60-26).
The 30-degree oblique view shows the alignment of the medial border of
the third metatarsal with the lateral cuneiform and the medial border
of the fourth metatarsal base with the medial border of the cuboid (Fig. 60-27).
The lateral view allows a rough assessment of the alignment of the
dorsum of the second metatarsal with the middle cuneiform. The position
of the second metatarsal on the AP view and the position of the fourth
metatarsal on the oblique are the most consistent indicators for
unstable injuries.
 |
|
FIGURE 60-26 Anteroposterior view of the tarsometatarsal joint. A. Normal joint alignment on weight-bearing view. B.
Manual stress view of tarsometatarsal injury with lateral migration of first and second metatarsals while foot is non-weight bearing. |
 |
|
FIGURE 60-27 Medial oblique view of the tarsometatarsal joint. A. Normal fourth tarsometatarsal joint alignment on weight-bearing view. B.
Non-weight-bearing view of tarsometatarsal injury with lateral displacement of fourth metatarsal in relation to the medial border of the cuboid (shown by arrows). |
for injury remains high, stress views of the joint complex should be
obtained as soon as possible. These are best obtained with anesthesia
to minimize pain and muscle guarding. If the patient’s injury permits,
a simple ankle block using 0.25% plain Marcaine can provide sufficient
anesthesia to perform an adequate stress test. Using a fluoroscopic
C-arm, the joint complex should be viewed in both the AP and oblique
planes with the hindfoot held stable and a supination-pronation or an
adduction-abduction stress applied to the forefoot. Any displacement of
normal joint contours greater than 2 mm denotes ligamentous instability
(Fig. 60-28). Recently, the assessment of the
medial column line formed by the medial border of the navicular and
medial cuneiform in the AP stress radiograph has been shown as a
possible predictor of joint instability.23 Intersection of this line with the first metatarsal base indicates stability of the first tarsometatarsal joint.
in a Lisfranc injury and to further investigate radiographically stable
injuries, a CT scan can be obtained. As a preoperative screening tool,
a CT scan can be very helpful in identifying collateral occult
fractures or dislocations that may also require attention to preserve
the stability and function of the foot.62)
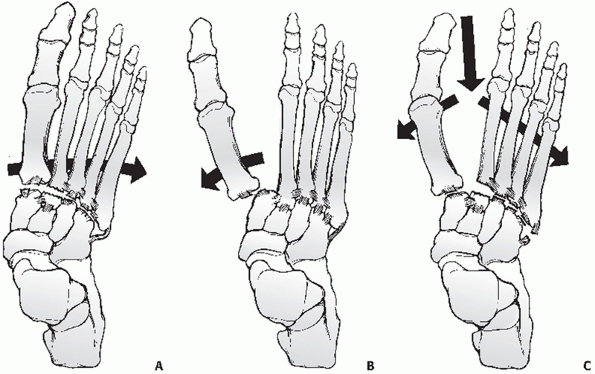
proposed to describe the resultant instability of severe injuries.
Quenu and Kuss91 first proposed the classification used by many today (Fig. 60-29).
It essentially divides these injuries into three types based on the
resultant pattern. The revised OTA classification designates the
dislocation aspect of this injury as (80-C5._). The last place
designates in this classification scheme denotes the metatarsal
involved 1 through 5. The number 9 is used to designate multiple
dislocations71 (Fig. 60-30).
Lisfranc variants involving intercuneiform instabilities are designated
by the designation of the joint involved and are listed in a previous
section. Fractures that commonly occur with this injury are classified
according to the metatarsal and location involved. A further discussion
of that classification can be found in the section on metatarsal
fractures.
 |
|
FIGURE 60-28 The use of stress films to identify unstable injuries is important. A. Non-weight-bearing radiograph of midfoot pain. B. A weight-bearing stress view of the same foot showing widening between the first and second rays.
|
found to aid in determining appropriate treatment or for predicting
outcome in these injuries. No classification system presently accounts
for the nondisplaced injury or the incidence of associated fractures.
transition between the midfoot and forefoot. It consists of the three
cuneiform-metatarsal articulations and the two cuboid-metatarsal
articulations of the fourth and fifth rays.100 The alignment and stability of this joint line are critical for normal function of the foot (Fig. 60-31).
The medial-to-lateral cascade of the distal articular surfaces of the
cuneiforms and cuboid provide for the transverse arch of the foot. The
metatarsals, with the distal heads placed for forefoot weight bearing,
comprise the distal half of the longitudinal arch. The rigid arch
complex provides the plantar structures with an area free from constant
compressive forces
that
can compromise neurovascular structures. Of greater importance is the
concept of a rigid lever arm in gait. This arch stiffness permits the
smooth transfer of the center of motion during weight bearing from the
ankle to the forefoot. This rigidity allows for smooth heel lift and
weight transfer to the opposite leg.
 |
|
FIGURE 60-29 The common classification devised by Quenu and Kuss. A.
Depicts homolateral disruption where all metatarsals travel in the same direction. This group can be subdivided into medial or lateral to denote the direction of disruption. B. Partial disruption involves only the first metatarsal or all the lesser rays. C. Divergent dislocation occurs when there is complete disruption of the tarsometatarsal joints but the first ray and the lesser rays displace in opposite directions. |
 |
|
FIGURE 60-30 The OTA classification scheme for tarsometatarsal dislocation (80-C5._). A. Example of isolated tarsometatarsal dislocation classification. The fifth digit is used to designate the metatarsal involved. B. Classification for multiple metatarsal involvement. The number of metatarsals and direction are not classified.
|
individual articulations of this complex allows the forefoot to
fine-tune individual metatarsal head positions to accommodate uneven
ground. The normal foot should exhibit an equal weight distribution
pattern across the six weight-bearing surfaces of the forefoot —two
sesamoids under the first metatarsal head and four lesser metatarsal
heads, each surface with an equal load. Motion studies about these
joints have shown two distinct components —the medial column (which is
a continuation of the talus, navicular, the three cuneiforms, and their
respective metatarsals) and the lateral column represented by the
calcaneus, cuboid, and the lateral two metatarsals. These can be
thought of as the two sides of a closed triangle with the transverse
metatarsal ligament as the base structure uniting the two columns. At
the level of the tarsometatarsal joints there is a distinct difference
in the amount of motion available. The medial three joints have less
than one third the available mobility of the two articulations that
comprise the lateral column.85 The
relative medial stiffness is to the result of the importance of
structural integrity over mobility. The talonavicular articulation is
the major point of mobility in that column. By contrast, the fourth and
fifth tarso-metatarsal joints represent the major point of mobility in
the lateral column, and the need for mobility there is crucial to
normal foot motion.
tarsometatarsal joints. They can be further subdivided into a medial
and a middle leg (the lateral column represents the lateral leg). The
motion of the first tarsometatarsal joint is, again, three times that
of the second and third tarsometatarsal joints. This mobility at the
first tarsometatarsal joint allows the insertions of the powerful
tibialis anterior and peroneus longus muscles to affect first ray
position and adjust the first metatarsal head to allow even
weight
distribution over uneven ground. The middle leg with its intrinsic
stability provides the true rigid lever arm about which the other two
legs adjust. The lateral leg also has powerful extrinsic motor
insertions. The peroneus brevis and peroneus tertius affect positioning
and stability of the lateral leg through their insertion on the base of
the fifth metatarsal.
 |
|
FIGURE 60-31 The anatomy of the tarsometatarsal joints. A. Proximal view of the cuneiform and cuboid articular surfaces. B. Distal view of the corresponding articular surfaces of the metatarsals. C.
Schematic representation of the contour of the tarso-metatarsal joint line. Note the keying in place of the base of the second metatarsal. |
to understand for treatment considerations. The first articulation is a
broad surface, usually 3 cm deep, and with a broad plantar base and
dorsal apex. The second and third are much smaller and triangular in
shape with the apex plantar. The second is recessed from the first by
approximately 1 cm and from the third by 0.5 cm. The fourth and fifth
are again more trapezoidal in shape and lie in a separate plane plantar
and lateral to the joints of the medial column. The inherent stability
of this region is the result in part to the recessed second metatarsal
base but even to a greater degree to the numerous strong ligamentous
attachments across each tarsometatarsal joint and between each ray.
There is a significant amount of variability in the position and
strength of individual ligaments across many of these joints. The
important characteristics to note are (a) the plantar ligaments are
significantly stronger than the dorsal ligaments, (b) the multiple
ligaments overlap among the joints of the lesser four tarsometatarsal
joints, and (c) the Lisfranc ligament, which is the largest and
strongest ligament of this joint complex, represents the only
ligamentous support between the medial leg and the middle and lateral
legs in the forefoot. The Lisfranc ligament originates from the plantar
lateral aspect of the medial cuneiform just below the plantar extent of
the second tarsometatarsal joint and inserts on the plantar and medial
aspect of the second metatarsal base. At best it is an indirect link
between the first and second metatarsals. There is no interligamentous
connection between the first and second metatarsal.
are important for management are stability and associated fracture
management. Extra-articular fractures, which appear with these
injuries, should be treated as described elsewhere in this text to
preserve that structure’s role in foot function. Intra-articular
fractures of the tarsometatarsal joints should be handled in the
context of the treatment of the joint complex.
with metatarsal motion, and tenderness to palpation but fail to exhibit
any instability should be considered a sprain. In addition to the
normal concept of rest, ice, compression, and elevation (RICE) for
treating sprains, the need for immobilization is important. These
injuries can be severely debilitating and require a long recovery
period.24,76
Nondisplaced ligamentous injuries with or without small plantar
avulsion fractures of the metatarsal or tarsal bones should be placed
in a well-molded short-leg walking cast (Table 60-5).
Initially, the patient is kept non-weight bearing with crutches and
only permitted to bear weight as comfort allows. Once full weight
bearing can be accomplished in a cast, the patient is tested for
weight-bearing comfort without support. The ability to perform a
single-limb heel rise without pain is a good indicator. Only when the
patient is pain free out of the cast should rehabilitative therapy
begin.
The definition of instability presently is defined as a greater than
2-mm shift in normal joint position. Closed manipulation under
anesthesia with casting as a definitive
treatment
has been shown to be a poor choice because maintenance of the reduction
is too difficult and residual deformity can lead to significant
morbidity. An initial closed reduction should be done for complete
dislocations to reduce the tensile pressure on the overlying skin and
protect the soft tissues from further compromise. Splinting of the foot
in a reduced position should be done until definitive treatment can be
performed. Mechanical blocks to reduction include joint surface
impaction, interposition of capsule or avulsion fracture fragments or
the interposition of the tibialis anterior at the first-second
interspace.
|
TABLE 60-5 Closed Management of Tarsometatarsal Injuries
|
|
|---|---|
|
The only variable that appears to determine outcome in these injuries
is the accuracy of the reduction. Recent studies also tend to show that
injuries that are purely ligamentous have a tendency toward chronic
pain and instability even with initial anatomic reduction and stable
fixation.58 More recently, Coetzee and Ly21
advocated that this subgroup of tarsometatarsal injury without fracture
may best be treated with acute fusion to hold the anatomic reduction.
The optimal method of fixation and the postoperative management of
these patients are not as clear. There are advocates for both closed
and open K-wire fixation after either closed or open anatomic
reduction. The pins are left in for 6 weeks. Others advocate the use of
screw fixation to stabilize the disrupted joints, leaving them across
the joints for 3 to 6 months. From the standpoint of stability of
fixation, screws appear to be superior at holding a reduction over
multiple K-wires in mechanical tests, but the optimal site of screw
placement and the need to stabilize the lateral tarsometatarsal joints
are in dispute.61
visualization across the whole joint complex. The most common approach
is using two longitudinal incisions44,102 (Fig. 60-32).
The first is centered over the first to second intermetatarsal space,
allowing identification of the neurovascular bundle and access to the
medial two tarsometatarsal joints. A second longitudinal incision is
made over the fourth metatarsal. Because of the vertical overlapping of
the lateral three metatarsals, this incision allows direct
visualization of these tarsometatarsal joints. Variations of these
standard incisions may be necessary depending on associated injuries to
the cuneiforms, cuboid, metatarsals, and navicular and their
articulations. Both of these incisions should be full thickness to the
bony surface with a minimum of undermining. Medial or lateral migration
in the wound should only be done through subperiosteal dissection to
preserve the integrity of the soft tissue envelope.
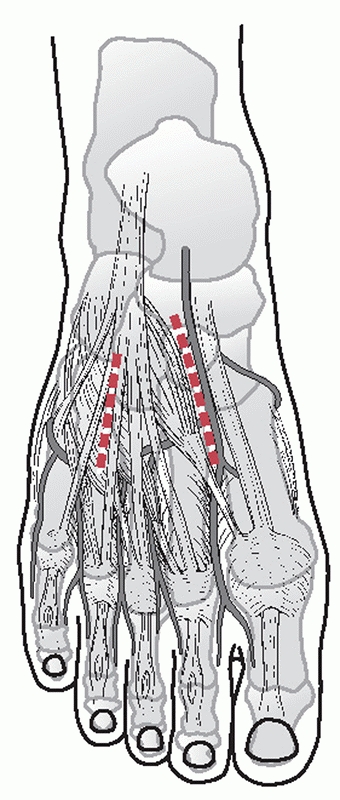 |
|
FIGURE 60-32
The surgical approach to the tarsometatarsal joints of the foot. The medial incision is along the first web space. The lateral incision is over the medial aspect of the fourth metatarsal. This will allow visualization of all joints. |
performed before reduction is attempted. Because of the ligamentous
interconnection of the lesser metatarsals, they must all be free from
any restraints to reduction and their joints free of fracture debris or
capsular interposition before any one of them can be accurately
reduced. Once reduction is accomplished, fixation is performed using
either fixation screws or K-wires to hold the joints stable (Fig. 60-33).
screws should remain in place after reconstruction. Opinions range from
removal before weight bearing begins to leaving the screws in place at
least 12 months or until symptomatic.58
The present trend is to leave them in at least until full weight
bearing has been achieved, although many trauma surgeons leave the
screws in place for the first 3 months after weight bearing.
on the presence of joint instability. Stable injuries are treated in a
well-molded cast with progressive weight bearing as tolerated after an
initial 3-week period of non-weight bearing. Because of the occasional
appearance of late instability, I usually obtain single-leg
weight-bearing AP and oblique
radiograph views of the injured foot at 10 to 14 days from the injury, to ensure anatomic alignment.102
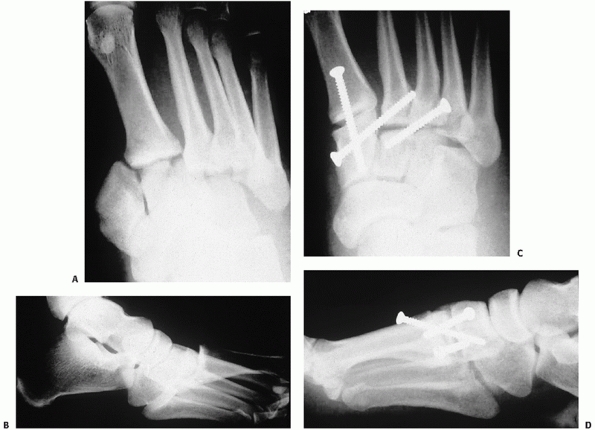 |
|
FIGURE 60-33 A,B.
Homolateral dislocation of the tarsometatarsal joints. This amount of displacement requires immediate reduction to minimize further damage to the soft tissue. C,D. Reduction and internal fixation of the tarsometatarsal joints with small fragment screws. |
open reduction and internal fixation. Before surgery, a routine CT scan
of the midfoot is obtained to assess the surrounding structures for
fracture or signs of ligamentous instability that may alter the
surgical plan. Also, in the case of tarsometatarsal articular
fractures, a rough assessment of the amount of comminution can be made
using the CT scan.
structural or ligamentous instability present in the cuneiforms is
addressed first with anatomic realignment and percutaneous screw
fixation (Fig. 60-34). Likewise, any injury to
the cuboid is addressed before reduction and fixation of the Lisfranc
complex. With the use of a large Weber clamp, reduction of the second
tarsometatarsal joint is obtained and held. Under direct visualization,
a 3.5-mm fixation screw is used to stabilize the joint (Fig. 60-35).
The remaining lateral joints are then assessed for stability. Screw
fixation is used for the third in the presence of instability. Because
of the importance of motion in the lateral two joints, any regional
instability is treated with percutaneous K-wire fixation. The fourth is
assessed and treated first before the fifth. The interligamentous
connections will usually hold the fifth in a reduced position once the
third and fourth are reduced, negating the need for further fixation.
The first is reduced only after anatomic reduction of the lesser
metatarsals, and it is fixed with a 3.5-mm screw.
surface should be reduced and stabilized before joint reduction. In the
case of simple fractures affecting 25% or more of the joint surface,
anatomic reduction and fixation with a K-wire or a mini fragment lag
screw is done. If the fragments are too small for fixation, they are
débrided. In the rare case where there is significant articular
comminution of the medial tarsometatarsal joints either individually or
as a group, consideration should be given to primary fusion.
Destruction of greater than 50% of the articular surface should undergo
a primary fusion at the time of reduction. Any void left by debridement
of fragments is filled with cancellous bone graft. Lag screws are used
across the joints to be fused. If the is no cortical abutment to
maintain metatarsal position, a small plate and screws should be used
to secure the metatarsal in a reduced position. The lateral two
articulations should never undergo fusion regardless of the amount of
initial injury. This area requires mobility and does poorly if fused.
 |
|
FIGURE 60-34 Presentation of an atypical Lisfranc injury. A,B.
Initial radiographs show disruption of the tarsometatarsal joints with evidence of interarticular fracture and fracture of the medial cuneiform. C. CT scan showing the longitudinal fracture of the medial cuneiform and comminution of the second and third cuneiforms. D,E. Reduction and fixation of the tarsometatarsal joints is accomplished with only medial column fixation. The medial cuneiform is fixed first with a lag screw followed by the tarsometatarsal joints. The first joint was stable. The lateral column required no fixation after reduction of the medial column. |
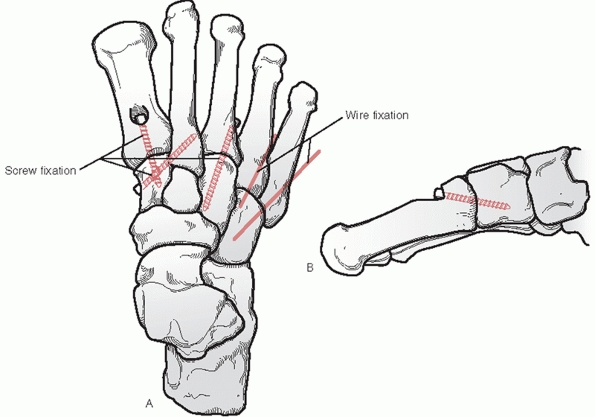 |
|
FIGURE 60-35 Suggested fixation placement for stabilizing tarsometatarsal injuries. A.
The 3.5-mm fixation screws are used to stabilize the medial column. The usual order is to restore the position of the second followed by the third with the first going last. The lateral column should be stabilized with percutaneous K-wires only if necessary. B. Longitudinal cross section at the first tarsometatarsal joint showing the recommended notching of the metatarsal base to avoid fracturing the cortex. |
for acute fusion of the treatment of the truly ligamentous injury. In
those patients who have only a ligamentous injury and are more than 275
pounds in weight or are involved in significant manual labor, acute
fusion provides them with the stabilization they need without the
incidence of chronic pain or late subsidence. The first second and
third tarsometatarsal joints are stripped of cartilage reduced
anatomically and fixed with two lag screws per joint in a manner
similar to that described for the acute stabilization.
plantigrade cast for 6 to 8 weeks. Progressive weight bearing is then
permitted as comfort allows. Advancement out of cast immobilization is
done once pain-free full weight bearing is achieved. Internally placed
hardware is removed from across the joints at 6 to 9 months after
initial treatment.
disruption, or radiographic evidence of joint degeneration, the best
results are dependent only on the ability to obtain and maintain an
anatomic reduction of the joint complex.80,109,113
Reduction not only refers to the position of the tarsometatarsal joints
but also to the restoration of the arch and the return of midfoot
stability. The major complications of this fracture complex are
incomplete reduction, loss of reduction, or post traumatic arthropathy.45,52
The radiographic appearance of degeneration of the joint is not unusual
with this injury and does not correlate well with clinical symptoms.
Anatomic reduction of the joint complex with medial column arthrodesis
is the treatment of choice for symptomatic arthropathy.52,68,98
diagnosis with these injuries. If the injury is recognized within 6
weeks of onset, anatomic reduction and stabilization is the treatment
of choice. After 6 weeks, anatomic reduction is difficult and the
results are poor.45 These injuries are best treated with medial column fusion when the patient is symptomatic (Fig. 60-36).
Realignment of a long displaced joint can be difficult due to the soft
tissue contractures. Before attempting reduction, complete soft tissue
release of all malaligned joints should be done to allow movement as a
unit. Resistance to realigning the lesser metatarsals can come from
contracture of the peroneus brevis muscle. This muscle can be
lengthened in the sheath posterior to the distal fibula, allowing
easier reduction of the lesser joints. Again, fusion of the fourth and
fifth tarsometatarsal joints should be avoided if at all possible.
it provides a broad plantar surface for load sharing. Weight-bearing
studies show that the two sesamoids and the four lesser metatarsal
heads share an equal amount of the forefoot load in normal
gait.
The platform is structured to also be mobile in the sagittal plane.
This provides the forefoot with the ability to alter the position of
the individual metatarsal heads to accommodate uneven ground. This
ability to alter position allows the forefoot to maintain a relatively
even pressure distribution on the plantar skin, protecting it from
local injury. Although the forefoot appears to work as a single unit,
it parts are distinctly different and need to be treated accordingly in
the case of injury.100
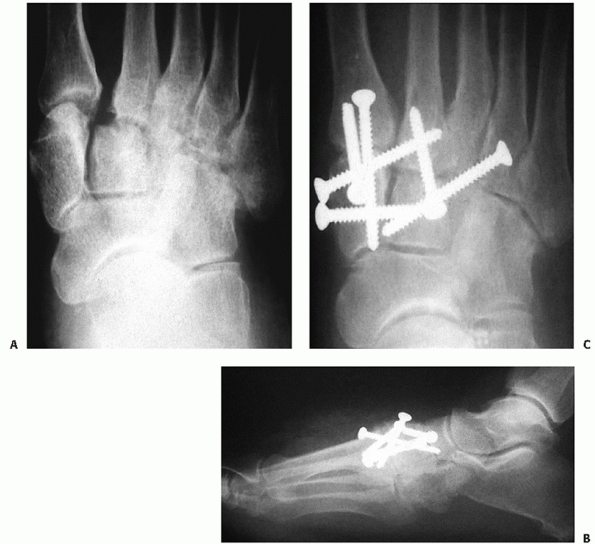 |
|
FIGURE 60-36 Late tarsometatarsal injury. A.
Weight-bearing radiograph of midfoot pain now 5 months from injury. Note the displacement of the joints and the loss of definition. B,C. Realignment and fusion of the medial column using a screw pattern similar to acute stabilization. Note the satisfactory restoration of the lateral joint space. |
result from the direct blow of a heavy object dropped onto the
forefoot. Such a direct force can result in the fracture of any
metatarsal at any point. Indirect forces, particularly twisting the
body with the toes fixed (as when a person catches the toe of the shoe
in a narrow opening), apply torque to the foot, producing fractures of
the metatarsal shafts, particularly spiral fractures of the middle
three metatarsals. Avulsion fractures, particularly the base of the
fifth metatarsal, are common. Stress fractures also occur commonly in
the metatarsals, particularly at the second and third metatarsal necks
and at the proximal portion of the shaft of the fifth. Despite the
relative insignificance usually relegated to metatarsal injuries they
can lead to significant limitations if ignored.54,102,104
is relatively easy if it is looked for. The advantage is that there is
no significant soft tissue envelope surrounding these bones to hide any
deformity or swelling. The presence of pinpoint tenderness, palpable
nonpitting edema, crepitance, or deformity is readily apparent. The
patient usually complains of pain in the dorsum of the foot, which
increases with weight bearing. The dorsum of the foot is usually
swollen and ecchymotic. In the first few hours after injury, it is
usually easy to find point tenderness over the fracture site. One
should be wary of closed crush injuries to the forefoot. Significant
swelling or soft tissue tightness should lead one to suspect a
compartment syndrome. If it is suspected, it is imperative that
operative decompression of the plantar and interosseous compartments be
done on an emergency basis. The fractures can be stabilized
percutaneously at that time.
weight-bearing films should be obtained in the AP and lateral planes.
Except in the case of an isolated direct blow, initial films should
include the whole foot to rule out other potential collateral injuries
that may also require attention. In the absence of other injuries,
repeat films specifically of the forefoot should be obtained to better
define the pathology. Whole foot radiography tends to overexpose the
forefoot and metatarsal head region, making radiographic evaluation
difficult. A lateral radiograph of the metatarsals is important for
judging sagittal plane displacement of the head. Other studies are
rarely needed to evaluate acute fractures. With evidence of a proximal
intra-articular fracture of any metatarsal, it is important to rule out
disruption of the tarsometatarsal joints and instability of the
Lisfranc joint.
is important to find the underlying cause of the stress fracture. They
occur individually as a response to locally high repetitive loads that
exceed the body’s reparative mechanism. The underlying cause can range
from local changes in the sagittal position of adjacent metatarsal
heads, to a tight gastrocnemius, to underlying metabolic bone disease
causing osteopenia. Any mechanical reason for the overload should be
addressed at the same time as the fracture. As with traumatic injuries,
any significant displacement of the metatarsal head from its normal
position should be addressed with reduction and stabilization. Failure
to treat the cause as well as the deformity may doom the other lesser
metatarsals to the same fate as the local force load is transferred
from one metatarsal to the next (Fig. 60-37).
a detailed description of the fracture pattern of each bone but does
not offer any insight into overall stability or treatment. The
designation of metatarsal fractures under this system observes the
format: (87( )-_ _._) in a fashion similar to the metacarpals of the
hand. To denote which metatarsal the classification refers to, an alpha
identifier should be placed beside the major designation: first
metatarsal (T), second metatarsal (I), third metatarsal (L), fourth
metatarsal (R), fifth metatarsal (S). The alpha designation to the
right of the hyphen refers to the amount of articular involvement and
or midshaft comminution. Extra-articular simple fractures are
designated A. The letter B denotes partial articular involvement or
wedge fracture of the shaft. And C denotes complete articular
involvement and or comminuted shaft fractures. Further
subclassification is given to accurately place the fracture: proximal,
central, or distal. Each of these groups is further divided by the
final description of the fracture71 (Fig. 60-38).
groups: the first and fifth metatarsals because of their location and
unique functions and the central metatarsals because of their
interconnectivity.
 |
|
FIGURE 60-37
Stress fractures of the metatarsal bones. These two radiographs show the progression of fractures from medial to lateral along the metatarsals in an insensate individual. |
metatarsal were referred to as Jones fractures. We now recognize that
there are probably three distinct fracture patterns that occur here60,92 (Fig. 60-39).
A true Jones fracture is acute in nature and occurs in zone 2 at the
metaphyseal diaphyseal junction. The relative frequency of these
fractures was shown in a busy general orthopedic practice to be
approximately 93% zone 1, 4% zone 2, and 3% zone 3.25
in many ways. Its configuration is shorter and wider than the lesser
four metatarsals. The lack of interconnecting ligaments between the
first and second metatarsal bones allows independent motion. Strong
thick ligaments that make up the capsule of the first tarsometatarsal
joint support its resting position. There are two powerful motor
attachments to its base. The anterior tibialis inserts on the plantar
medial aspect of the first metatarsal base and the peroneus longus
attaches onto the plantar lateral base of the first metatarsal. These
two muscles exert significant influence on the position of the first
metatarsal head. The tibialis anterior serves to elevate the first
metatarsal and the peroneus longus acts to plantarflex the head. The
first metatarsal head supports two sesamoid bones, which provide two of
the six contact points of the forefoot. This translates to the first
ray essentially supporting one third of the forefoot weight at any one
time.100
metatarsal to some degree depends on the configuration of the fracture.
For simple avulsions at the metatarsal base, an incision directly over
the fracture may be best for direct vision of reduction. For the
majority of proximal and midshaft fractures, a dorsal-lateral approach
through the first second intermetatarsal space is adequate
for
visualization of reduction and fixation. This incision can be extended
distally and proximally to allow access for a bridging plate if needed.
The approach should be done carefully to avoid unnecessary disruption
of tissue planes. In this area of the forefoot lie the dorsalis pedis
artery and the deep peroneal nerve. Branches of the superficial
peroneal nerve can be found overlying the deeper structures. These
structures need to be identified and protected during the surgical
dissection and closure.
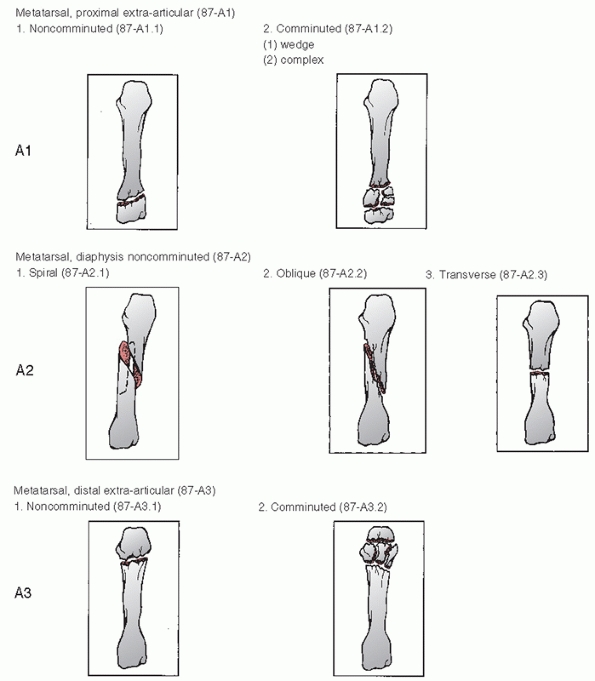 |
|
FIGURE 60-38
OTA Classification for metatarsal fractures (87-_). Modifiers are used to specify the metatarsal involved and follow the classification number: T, great toe; I, index toe; L, long toe; R, ring toe; S, small toe. A. Subclassification fracture patterns for type A extra-articular metaphyseal and simple diaphyseal. |
the first metatarsal during gait and it is therefore important to
maintain its normal position in relation to the foot. The best way to
determine operative or nonoperative treatment is with stress
radiographs. Manual displacement of the position of the first
metatarsal through the joint or fracture site represents an instability
that requires fixation. If no evidence of instability can be seen on
stress films of the fracture, and no other injury of the midfoot or
metatarsals is evident, isolated first metatarsal fractures can be
adequately treated in a short leg cast with weight bearing as tolerated
for 4 to 6 weeks (Table 60-6). It is important
when casting this injury to position the foot in a plantigrade position
yet without placing dorsally directed pressure on the first metatarsal.
The best way to apply the cast is with the patient in the prone
position with knee of the affected limb flexed to 90 degrees, placing
gentle pressure on the lesser metatarsals to obtain a plantigrade
position. Activities are then advanced as
tolerated
in a walking cast until there is comfortable full weight bearing before
advancing to regular shoes or increased activity. Any evidence of
instability or loss of normal position of the metatarsal head should be
treated with operative stabilization. The goal is to restore and
maintain the normal position of the first metatarsal head in relation
to the others.44,104
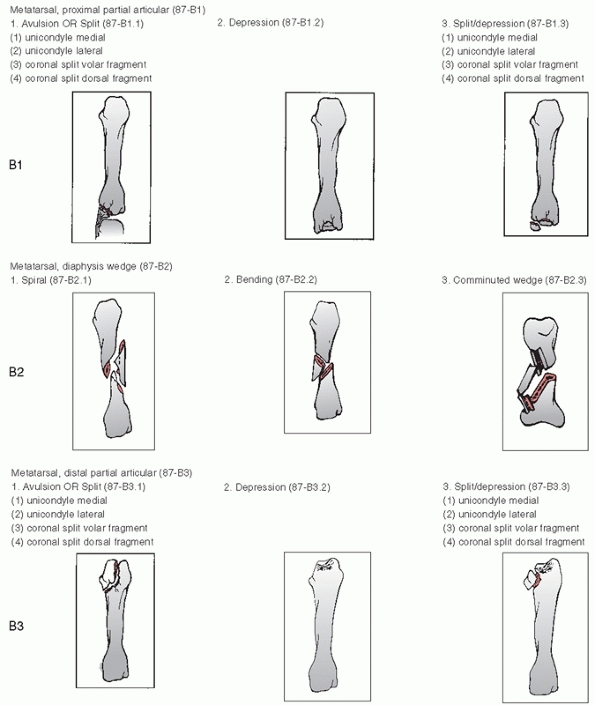 |
|
FIGURE 60-38 (continued) B. Fracture pattern subclassification for type B, partial articular fractures or wedged diaphyseal fractures.
|
configuration. Simple fractures of the shaft or either articular
surface can be fixed with percutaneous smooth wires or by open
reduction and screw fixation. Plate and screw fixation should be used
for transverse or minimally comminuted fractures where inadequate
fixation will occur with screws or wires alone. External fixation
should be considered with severe midshaft or head comminution or open
injuries. The fixator is used to restore first metatarsal axial length
and alignment with the forefoot without further compromise to the soft
tissue.
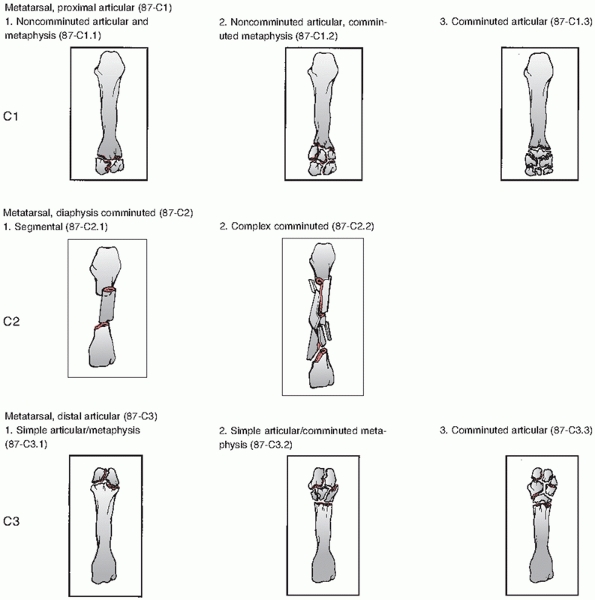 |
|
FIGURE 60-38 (continued) C. Subclassification of fractures with complete articular or comminuted diaphyseal involvement.
|
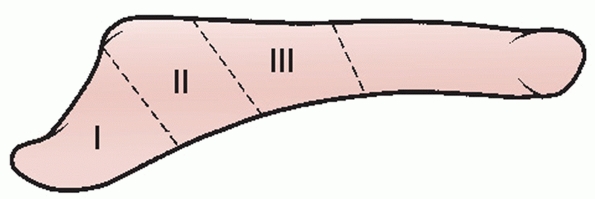 |
|
FIGURE 60-39
Three zones of proximal fifth metatarsal fracture. Zone 1: Avulsion fracture. Zone 2: Fracture at the metaphyseal-diaphyseal junction. Zone 3: Proximal shaft stress fracture. |
|
TABLE 60-6 Closed Management of First Metatarsal Fractures
|
|
|---|---|
|
based on the desire to maintain the position of the first metatarsal
head in the normal cascade of the forefoot. Preservation of the
metatarsophalangeal joint function is vital for normal function.
Preservation of the tarsometatarsal joint is desirable but may be
sacrificed for ray stability and position with little detrimental
effect on forefoot function. Therefore, the criteria for intervention
are based on the stability of the fracture and the adjacent joint. One
should remember there are no ligamentous supports for this metatarsal
to adjacent structures so any fracture displacement is likely to
represent an unstable fracture.
should be addressed aggressively with surgical stabilization. 44,46
Simple fractures, whether diaphyseal or intra-articular, are best
treated with lag screw fixation with 2.7-mm screws after open reduction
(Fig. 60-40). With stabilization of the
fracture, reassessment of the stability of the tarso-metatarsal joint
should be performed. If the joint is thought to be unstable, a 3.5-mm
fixation screw can be placed across the joint similar to the manner
used to stabilize the first tarsometatarsal joint in a Lisfranc injury
if the fracture pattern permits. More commonly because of the fracture
pattern, this joint instability is treated with a contoured one-third
tubular plate and 3.5-mm screws. The plate extends from the medial
cuneiform to the distal intact aspect of the shaft to obtain proper
purchase (Fig. 60-41).
more comminuted fractures when lag screw fixation is not possible. The
determining factor is whether there is enough intact bone distally to
obtain a secure fixation of the plate. Fracture patterns involving
severe comminution of the proximal half of the metatarsal are amenable
to this type of fixation.
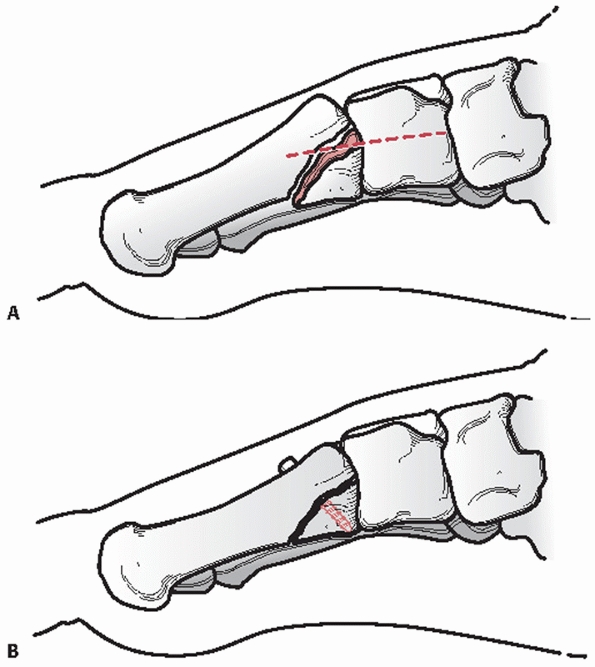 |
|
FIGURE 60-40 A. Unstable intraarticular first metatarsal fracture. B. Reduction and placement of lag screw fixation.
|
with inadequate intact bone to support a plate are best handled by
external fixation (Fig. 60-42). These fracture
patterns usually have significant soft tissue damage associated with
them and should be stabilized without creating further soft tissue
trauma. Fixator pins can find purchase in the intact midfoot and
proximal phalanx to establish length and position. Secondary pins can
be used to secure intact segments of the metatarsal to further control
alignment. If the proximal phalanx is used to stabilize the fracture,
care should be taken in the final positioning. The external fixator
should be placed such that the proximal phalanx is at minimum in a
plantigrade position but it should be slightly dorsiflexed if possible.
This is to prevent problems of toe position in the event of joint
stiffness post injury.
treated to preserve articular function. Disruptions of the articular
surface should be openly restored and stabilized, using cancellous bone
graft behind the subchondral bone for support if needed. All displaced
fractures of the first metatarsal head and neck region should be
anatomically reduced and pinned with smooth wires (Fig. 60-43).
Large intra-articular fragments should be fixed with smooth wires or
mini-screws. In the presence of comminution of the neck or head,
external fixation is required to restore length and hold position. The
fixator should incorporate the proximal phalanx of the great toe.
around the health of the soft tissues and the rate or evidence of bony
healing. Non-weight-bearing status is maintained for 8 to 10 weeks.
Those fractures internally fixed are placed in a short leg cast. In the
presence of external fixation, a removable molded splint is used to
maintain the foot in a plantigrade position. Active and passive motion
of the great toe are encouraged in the early postoperative period if it
is not included in the fixation. Once bridging callus is identified on
radiography, the external fixator is removed, and the patient is
allowed to advance weight bearing in a removable walker as tolerated.
Internal fixation that is bridging the tarsometatarsal joint is left in
place for up to 6 months before being removed. Progression of activity
is based on patient comfort. A full-length in-shoe orthotic device with
medial support for the first metatarsal arch is used for up to 1 year.
degeneration of the tarsometatarsal and metatarsophalangeal joints are
all possible complications of first metatarsal fractures. Transfer
metatarsalgia to the lesser toes can occur with shortening of the first
metatarsal length. Secondary surgery may be necessary to realign or
bone graft the fracture.
There are significant ligamentous structures that link each of the
bones to their adjacent neighbors. At the base of each of these bones
is a series of three ligaments (dorsal, central, and plantar), which
act to stabilize and support each with their neighbor. The central
three have no extrinsic motor insertions. Their role is for structural
support. They do provide for the origin of dorsal and plantar
interossei muscles. The plantar muscles insert into the medial aspect
of the associated proximal phalanx. The tendon of the dorsal muscle,
however, inserts into the plantar aspect of the proximal phalanx of its
medial neighbor. Finally, there is the thick transverse metatarsal
ligament distally that connects the metatarsals indirectly by linking
the plantar plates of the adjacent metatarsophalangeal joints. There is
also a cascade of allowable increase in motion through the
tarsometatarsal joints beginning at the second metatarsal and going out
to the fifth. It is this increase in motion in the sagittal plane that
allows for significant adaptability to terrain by the metatarsal heads.
It is also the relative resistance to motion at the second and third
tarsometatarsal joints that causes stress fractures to be seen more
commonly in these two metatarsals.
 |
|
FIGURE 60-41 Comminuted fracture of first metatarsal. A,B. Anteroposterior and lateral radiographs of injury. C-E. The 2-year postinjury weight-bearing films show maintenance of the joint line. The bridging plate was removed at 6 months.
|
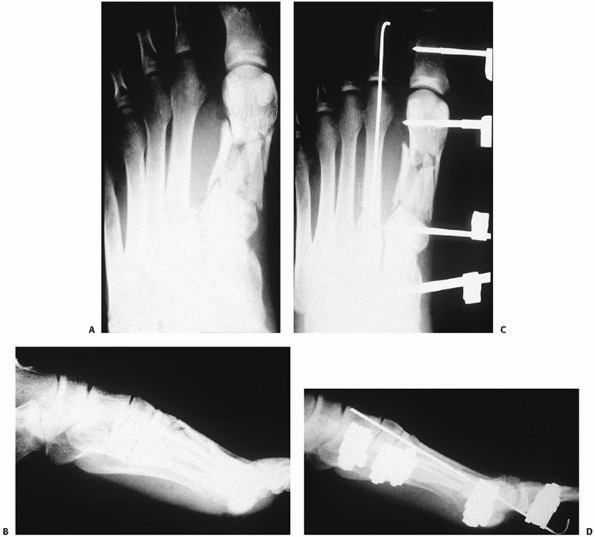 |
|
FIGURE 60-42 The use of the external fixator for severe first metatarsal fractures. A,B. Injury films showing significant disruption of the metatarsal shaft. C,D. Placement of an external fixator with restoration of metatarsal length and alignment.
|
more common than first metatarsal fractures and can be isolated or part
of a more significant injury pattern.2,104
As with the first metatarsal, the emphasis is on the resulting position
of the metatarsal head. Although there is little in the literature
documenting specific criteria for unacceptable position, the problems
of transfer metatarsalgia and shoe wear are well known in fractures
that allow significant changes in the normal position of the
metatarsal head (Table 60-7).
The criterion most often mentioned is that any fracture displaying more
than 10 degrees of deviation in the dorsal plantar plane or 3 to 4 mm
of translation in any plane should be actively corrected104 (Fig. 60-44).
 |
|
FIGURE 60-43 Displaced first metatarsal head fracture. A. Injury film showing disruption of all metatarsal heads. B. The use of two smooth wires to stabilize the reduction of the first metatarsal head.
|
That is not to mean they should be ignored. Isolated midshaft
fractures, whether comminuted or simple, are usually quite stable with
little shortening and can be managed adequately with hard sole or stiff
shoes and progressive weight bearing as tolerated. Any appreciable
deviation in metatarsal head position should be addressed with
reduction and possibly pinning to maintain normal forefoot alignment.
|
TABLE 60-7 Closed Management of Central Metatarsal Fractures
|
|
|---|---|
|
deviate either dorsally or plantar in the sagittal plane are treated
with closed reduction using finger trap distraction to restore
alignment. These patients are also then allowed to begin weight bearing
as tolerated in a hard-sole shoe. Progression to full activities is
dependent solely on the reduction of symptoms. Pin fixation is rarely
needed with the isolated injury because of the surrounding soft tissue
stability at the metatarsophalangeal joint.
fracture requires further investigation to ensure there is no
instability along the Lisfranc joint. Weight-bearing stress radiographs
are recommended to confirm tarsometatarsal stability. If instability is
present, the fracture should be treated within the context of the
Lisfranc instability. A stable base fracture of the third or fourth
metatarsal can be reduced closed without fixation. A base fracture of
the second should be stressed to see if it has any tendency to displace
laterally. Because there are no stabilizing ligaments between the first
and second metatarsals, limited open reduction and intramedullary
pinning of the second metatarsal can be done to maintain proper
position if it has a tendency to shift laterally.
metatarsal fractures or there is significant comminution. The inherent
stability provided by adjacent structures now tends to accentuate any
deformity. Closed reduction can be attempted but it is usually
unstable. In this situation it is easier to open the fracture, reduce
it, and secure it with an intramedullary K-wire or 2.7-mm screw and
plate fixation. The choice of fixation is dependent more on the
condition of
the
surrounding soft tissue than on the fracture pattern or location. If
there is significant soft tissue injury or open wound, I prefer to use
intramedullary K-wire fixation (Fig. 60-45).
Great care must be taken during the reduction to avoid dorsiflexion or
plantarflexion of the distal fragment causing a malalignment of the
metatarsal head with its neighbors. Use of the K-wire for fixation is
also effective if there is severe comminution of the shaft. One must be
careful not to shorten the position of the head in relation to its
neighbors.
 |
|
FIGURE 60-44 A. Displaced fractures of the second, third, and fourth metatarsal shafts. B. Lateral radiograph shows unacceptable plantar angulation of 30 degrees. C. Anatomic closed reduction and percutaneous pin fixation. D,E. Anteroporsterior and lateral radiographs at 6 weeks showing early healing of all three fractures in good alignment.
|
hard to control. Many times apparently simple neck fractures from acute
trauma actually extend into the head and metatarsophalangeal joint.
These fractures are difficult to treat by open means, running the risk
of devascularization of the head and losing any remaining stability
with disruption of the soft tissue attachments. Closed reduction with
traction and local anesthesia is the preferred method of treatment. The
goal is to bring what is usually a plantarflexed head back to a neutral
position and impale the head on the neck of the metatarsal. Realignment
can be supplemented by percutaneous pin fixation. The pin should
incorporate both the metatarsal shaft and the base of the proximal
phalanx to ensure stable fixation. If a pin is used to maintain the
reduction, I recommend entering the base of the proximal phalanx or
metatarsal head from the lateral aspect and aim to bend the pin down
the medial wall of the shaft. This elastic bend in the K-wire will
exert a medially directed force to balance the natural tendency for
these fractures to drift laterally.
metatarsals, a combination of procedures should be done. The proximal
fracture should be exposed and control of the segmental fragment
achieved with an intramedullary K-wire. Then a closed reduction of the
distal fracture should be done. The
metatarsophalangeal
joint is aligned, and the pin is passed across the distal fracture and
the metatarsophalangeal joint. Finally, the proximal fracture is
reduced and the wire is advanced across it in a retrograde fashion.
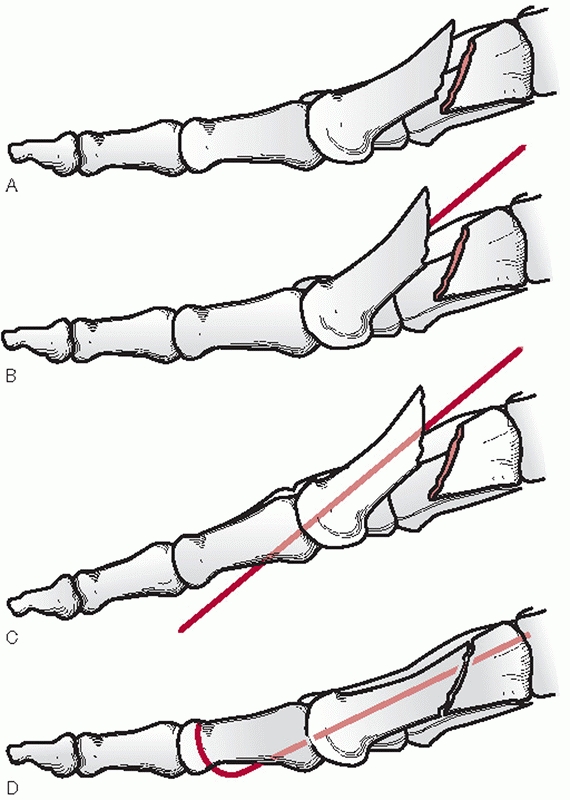 |
|
FIGURE 60-45 Central metatarsal fracture stabilization. A. Typical fracture pattern. B. The fracture site is surgically exposed and a smooth wire placed distally down the shaft. C. The proximal phalanx of the toe is held in a reduced position so the pin engages the plantar cortex of the phalanx. D. The fracture is then reduced and the wire fed through the proximal portion of the metatarsal.
|
the patient in a short leg cast for 2 weeks with the foot in a
plantigrade position to allow soft tissue healing. The patient is
permitted to bear weight through the heel during this time. With
removal of the sutures a removable cast is used to maintain normal foot
position until the patient is comfortable to bear weight, usually 4 to
6 weeks. The pins are removed at 4 weeks unless they are bridging a
bony gap. In that case, cancellous bone grafting is done at that time
and the pin remains until radiographic evidence of bony consolidation
is seen or the patient is weight bearing without pain.
metatarsal fractures usually stem from incomplete restoration of
plantar anatomy.2 This is not
possible in some cases no matter how diligent one is. Also, just
because there is a recognizable deformity once bony healing has
occurred does not guarantee that a patient will have clinical symptoms.
In those patients who are symptomatic upon restoration of bone stock
and healing of soft tissues, simple osteotomies can usually correct the
symptomatic deformity. Other causes of a poor outcome are more related
to the energy of the initial trauma. Fracture comminution, soft tissue
injury, and open injuries were noted to lead to late symptoms of pain
and stiffness regardless of the type of intervention.2
discussed separately from the other metatarsals because of the
different venues where these injuries are seen. Although injury to this
area does occur with motor vehicle collisions, the majority of injuries
are related to sporting or athletic activities. These fractures are
separated roughly into two groups: proximal base fractures and distal
spiral or dancer’s fractures. Proximal fifth metatarsal fractures are
further divided by the location of the fracture and the presence of
prodromal symptoms1,25,40,92,95,107,116 (Fig. 60-46).
fifth metatarsal usually occurs from an indirect load. Sudden inversion
of the hindfoot with weight on the lateral metatarsal places tension
along the insertion of the lateral band of the plantar aponeurosis
which inserts into the proximal base of the fifth metatarsal causing
disruption of the bony cortex. The peroneus brevis appears to have
little effect on this fracture pattern. This same mechanism can also
produce lateral ligament injury at the ankle, and therefore it must be
ruled out in patients who complain of lateral ankle pain after a
twisting injury. This is easily done by directly palpating the bone and
resisting active eversion of the foot. Both will produce pain if injury
is present. A direct blow to the tuberosity area can also produce an
avulsion-type injury but usually exhibits more comminution and
involvement of the fifth tarsometatarsal joint. The fragment size may
vary from a small fleck to a fragment encompassing almost the entire
tuberosity. Only rarely is the articulation of the fifth
tarsometatarsal joint involved. The fracture is usually minimally
displaced and stable because of its attachment to the plantar
aponeurosis.
an acute injury cause by adduction of the forefoot resulting in a
fracture at the proximal metaphyseal-diaphyseal junction of the bone.
The fracture propagates from the lateral aspect of the proximal
metatarsal toward the four to five articular surface. It can progress
proximally into the metatarsal-cuboid joint and exhibit comminution. It
is a fracture due mainly to tensile stress along the lateral border of
the metatarsal.
metatarsal is now referred to as a proximal diaphyseal stress fracture.
These are relatively rare and seen mainly in athletes. It occurs in the
proximal 1.5 cm of the shaft of the metatarsal. Repetitive cyclic loads
as seen in high-level athletics appear to be the underlying mechanism
for these injuries. The fracture is induced by tensile forces resulting
in microfractures at the lateral cortex. Continued loading propagates
the fracture medially. The presence of clinical symptoms before the
radiographic visualization of the fracture is classic in this pattern.
Weeks to months of pain with exertion at the lateral border of the
proximal metaphysis can be seen. Radiographic examination reveals a
variable fracture length with sclerotic margins and variable callus.
to proximal-medial. The mechanism of injury a rotational force being
applied to the foot while it is axially loaded in a plantarflexed
position. The usual method is by rolling over the outer border of the
foot.
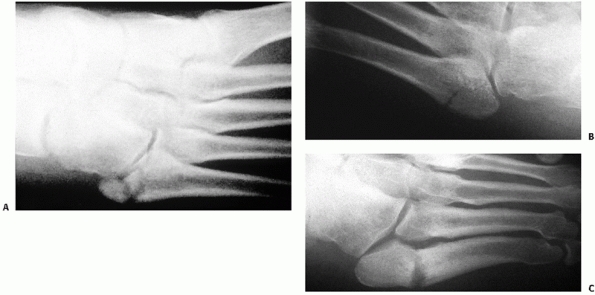 |
|
FIGURE 60-46 Fracture of the fifth metatarsal base. A. Zone 1 injury with comminution. B. Zone 2 injury. C. Zone 3 injury with 6-month history of pain.
|
distinguished from the other lesser metatarsals in that it does have
major motor insertions at its base. The peroneus brevis attaches on the
dorsal aspect of the tubercle of the fifth metatarsal and the peroneus
tertius attaches on the dorsal aspect at the proximal metaphyseal
diaphyseal junction. Functionally, the peroneus tertius acts as a
balancing force to forefoot dorsiflexion counteracting the natural
inversion tendency of the tibialis anterior. The peroneus brevis serves
as more of an antagonist to posterior tibialis function to maintain the
position of the foot under the talus. There is also a strong attachment
of the plantar fascia to the plantar aspect of the tubercle.
A fracture would not have the smooth radiolucent line parallel to the
metatarsal shaft. Also in this area are two sesamoid bones, which
should not be mistaken for a displaced fracture. The os peroneum is
located within the tendon of the peroneus longus and can be found on
the lateral border of the cuboid. The os vesalianum is found just
proximal to the base of the fifth metatarsal medial to the insertion of
the peroneus brevis. Its smooth contours, in contrast to a fracture,
should distinguish it from an acute injury.100
studied in depth in an attempt to understand the problem with proximal
metatarsal nonunion. It is similar to the other metatarsals in that a
single nutrient artery enters from the medial cortex at the junction of
the proximal and middle third of the diaphysis and supplies the shaft.
Secondary epiphyseal and metaphyseal arteries supply the base and
tuberosity.100
to the proximal tuberosity is necessary, great care should be taken
during the approach. The sural nerve, the insertion of the peroneus
brevis, and the insertion of the peroneus tertius, as well as the
lateral anchor for the extensor retinaculum, are all within the
surgical margins.32 Damage to these
structures should be avoided. If there is a need to access the fracture
directly through one of the tendon insertions, it appears to be better
to make a “z” cut transsection of the structure and repair it than to
remove it from its bony insertion.
looking at various treatment aspects for the variety of fractures seen
in the fifth metatarsal4,82,92,116 (Table 60-8).
The conclusion is that zone 1 injuries as well as distal fractures can
be treated quite well by closed means. Avulsion fractures and dancer’s
fractures do well if treated symptomatically.82,83,116
A soft Jones dressing, a stiff-soled shoe, and casts have been shown to
be equally effective. Symptoms can last for 6 to 8 weeks but usually
heal fully. In adolescents, whether pain in this area is from a true
fracture or from apophysitis, the treatment is the same.
|
TABLE 60-8 Closed Management of Fifth Metatarsal Fracture
|
|
|---|---|
|
diaphysis, zone 2, is controversial. Part of the problem appears to be
the mixing of acute and chronic injuries in earlier series. These act
as two different fracture populations where those with prodromal
symptoms are more likely to have difficulty healing and should be
considered as zone 3 injuries. Looking specifically at acute zone 2
injuries, treatments ranging from symptomatic protection to short leg
casting or surgery have been reviewed.4,82,92
Short leg casting with weight-bearing progression as tolerated appears
to give the best results. The cast is left on for 8 to 10 weeks.
proximal tuberosity and present with prodromal symptoms before complete
fracture. It is this particular entity that poses problems because of
its tendency toward nonunion.82
Successful treatment of this fracture pattern requires more aggressive
treatment than that used for other fracture patterns in the fifth
metatarsal. Initial treatment is between casted non-weight bearing for up to 3 months versus surgical intervention with grafting and internal compression.92,107
In the fractures with a short period of localized pain with activity
before diagnosis, non-weight-bearing casting offers results comparable
to surgery.1,57,88
nonunion that occurs mainly with a zone 3 injury. Best results are
obtained with open debridement of the nonunion site and cancellous bone
grafting. Rigid intramedullary compression of the fracture is used to
stabilize the injury. The approach is along the lateral border of the
fifth metatarsal just above the adductor minimi muscle (Fig. 60-47).
The proximal tip of the tuberosity is identified as well as the
nonunion site. The fracture site should be completely opened with
osteotomes or a rongeur. The medullary canal should be cleared of any
sclerotic debris. The void created by the debridement needs to be
completely filled with autograft. Axial compression can be obtained
with a cortical or cannulated screw 3.5 mm or larger to tightly fit the
metatarsal canal. Using fluoroscopic imaging the screw is introduced
through the proximal tuberosity across the fracture. According to
cadaveric studies, the insertion point for intramedullary fixation is
1cm dorsal to the palpable inferior margin of the proximal tuberosity
and just medial to the peroneus brevis insertion. The drill, or guide
pin, should proceed in a plantar direction at an angle 7 degrees off
the plantar surface of the foot with the ankle in neutral.53
The sural nerve is only 5 mm or so dorsal to the insertion site and
should be shielded from injury. The screw should engage the cortical
bone of the distal fragment without distorting metatarsal alignment for
best results. Surgical stabilization does not permit early return to
activity with these fractures. Short leg casting and protected weight
bearing similar to the treatment of early zone 3 injuries arenecessary
to have the best chance of healing.40
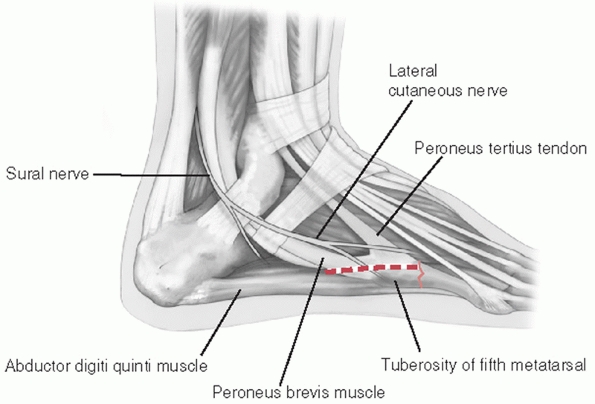 |
|
FIGURE 60-47
Surgical approach to the base of the fifth metatarsal. Structures to identify and protect include the sural nerve, the digiti quinti tendon, and the peroneus brevis tendon. |
shaft fractures, and nondisplaced direct blow injuries in a removable
walker and permit them to bear weight on the leg as tolerated. Crutches
and mild, oral pain medication are supplied initially to aid the
patient. The patient is allowed to progress to weight bearing as
comfort permits without the further use of pain medication and
essentially walk themselves out of the boot.
the fifth tarsometatarsal joint is evident, consideration should be
given to restoring the joint surface alignment with open reduction. I
have on occasion found articular fragments rotated 90 to 180 degrees
within the joint. Open reduction and stabilization of these injuries
has been very satisfying (Fig. 60-48). The
reduced fragments can be held in place with mini fragment screws that
do not cross the joint or K-wires that can cross the joint. Those with
severe comminution should be treated closed. If the fragments are too
small or too numerous to obtain adequate fixation, there is nothing to
be gained by opening the fracture and further disrupting the blood
supply to the area. I routinely place these in a short leg cast to more
securely stabilize the foot for the first 4 weeks. Weight bearing is
still permitted as comfort allows.
same whether the injury is truly acute or has a history of prodromal
symptoms. Both are placed in short leg non-weight-bearing casts for 6
weeks. The presence of prodromal symptoms will
determine
when weight-bearing activities are allowed. At 6 weeks, acute injuries
(no prodromal symptoms) are changed to a removable short leg walker and
weight bearing is allowed to progress as tolerated. When full
asymptomatic weight bearing occurs, physical therapy can begin as well
as a return to sporting activities. This takes up to 10 weeks in most
cases. Those fractures that present after a history of localized pain
with activity (stress fractures) are left in a non-weight-bearing cast
for 8 weeks. Reexamination of the fracture is done to look for clinical
and radiographic signs of healing. Radiographically, dissolution of the
sclerotic margins of the fracture and reconstitution of the medullary
canal are signs of active healing. Lack of pain with direct palpation
of the fracture site and with motion of the distal metatarsal can be
seen clinically as healing occurs. Non-weight-bearing casting is
usually continued for a full 3 months.
 |
|
FIGURE 60-48 Fixation options for fifth metatarsal base fractures. A,B.
Anteroposterior and lateral radiographs of single screw fixation to hold the reduction. It is important to contact the opposite cortex. C,D. Anteroposterior and lateral radiographs of minifragment plate and screw construct to hold fragmented base intact. |
all patients to use a soft accommodative arch support to try and reduce
the lateral sheering forces on the fifth metatarsal. In the high-level
athlete or high-demand employee, I will consider surgical grafting and
fixation to ensure healing. This step is taken carefully because it
does not lead to a quicker recovery. This course of treatment will take
up to 3 months to reduce symptoms enough to allow a return to activity.
The only advantage to surgery occurs in that group of patients in whom
I am convinced the fracture will go on to a nonunion because of long
prodromal symptoms and failure of previous immobilization.
time of presentation or failure of nonoperative management, operative
reduction and fixation is advocated. This is done usually through a
percutaneous approach with the patient in the lateral decubitus
position. Lag screw fixation is introduced through the tuberosity into
the distal medullary canal using fluoroscopy. The screw size should be
determined by the distal diaphyseal bone canal size (Fig. 60-49). A 4.5-mm
cortical screw is fine for a normal size canal, but larger feet may
require a 6.5-mm screw to obtain adequate intramedullary purchase.
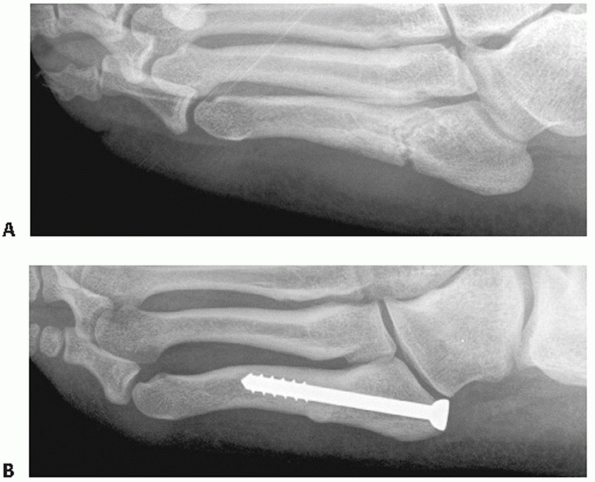 |
|
FIGURE 60-49 Fifth metatarsal chronic stress fracture. A. Presentation oblique radiograph with sclerotic margins at metaphyseal diaphyseal junction. B. Oblique radiograph 3 months postplacement intramedullary compression screw. Note complete healing of fracture.
|
properly are rare. For zone 1 fractures, nonunion can occur but is
usually asymptomatic and require no intervention. There are reported
incidences of pain from sural nerve entrapment or tarsometatarsal joint
pain with nonunion.41 In these
instances, these fracture fragments should be excised. If the
symptomatic nonunion is large enough to involve the insertion of the
peroneus brevis, it is large enough for fixation and cancellous bone
grafting using a 3.5-mm or 4.0-mm lag screw.
injuries is more the result of the method of treatment. These fractures
need a period of immobilized non-weight bearing
to minimize complications. Surgical failures are a factor of resuming
activity too soon, inadequate grafting, and/or incomplete debridement
of the sclerotic medullary canal.40
occur in isolation as well as be a small part of a high-energy
multipleinjury trauma.11,46
It occurs most commonly at the first metatarsophalangeal joint complex
during sports but can also be an isolated injury to a lesser
metatarsophalangeal joint. The importance of first metatarsophalangeal
joint stability should not be underestimated. It provides for stable
load sharing between the metatarsal head and the distal pad of the
respective toe. Dorsiflexion motion provides for a smooth transition
between heel off and toe off during weight-bearing gait. It is
important to be aware of the potential for injury to this joint with
any form of loading trauma to the foot because of the significant
long-term problems of pain and instability if left untreated.
metatarsophalangeal joint is composed of a cam-shaped metatarsal head
and a matched concave articulation on the proximal phalanx. These
contours contribute little to the overall stability of the joint.
Stability is provided by the complex structure of the joint capsule and
ligaments. The capsule is normally thin and weak dorsally. The plantar
capsule is a thick, weight-bearing structure with strong attachments to
the base of the proximal phalanx. There is a thinner, more flexible
attachment to the plantar aspect of the metatarsal head proximally.
Imbedded in this plantar structure are two bones known as sesamoids,
which articulate directly with the metatarsal head. It is the medial
and lateral sesamoid that are the two ground contact points for weight
bearing through the first metatarsal. Between these two sesamoids and
plantar to the intersesamoid ligament runs the flexor hallucis longus
tendon.
intrinsic motor insertions that exert significant control over the
stability and position of the joint. Medially, the medial head of the
flexor hallucis brevis inserts directly into the proximal aspect of the
medial sesamoid. The adductor hallucis partially inserts along the
medial border of the medial sesamoid but also continues distally to
insert on the medial plantar tubercle of the proximal phalanx and the
transverse lamina of the extensor aponeurosis. This motor complex
provides dynamic resistance to valgus stress on the great toe. The
lateral head of the flexor hallucis brevis inserts on the proximal
aspect of the lateral sesamoid. The oblique and transverse heads of the
adductor hallucis muscle insert mainly along the lateral border of the
sesamoid but have extensions into the lateral plantar tubercle of the
proximal phalanx, the lateral capsular complex, and the tunnel of the
flexor hallucis longus. This motor complex resists varus stress applied
to the great toe. There are no tendinous insertions present on the
metatarsal head (Fig. 60-50).
attachments of the metatarsal head to the joint complex. The better
known sets of ligaments are the medial and lateral collateral ligaments
extending from the metatarsal head to the medial and lateral base of
the proximal phalanx. The second set is known as the medial and lateral
metatarsosesamoid ligaments. They form a strong attachment between the
medial and lateral edges of the respective sesamoids and the medial and
lateral sides of the metatarsal head.
longitudinal quadrants. Dorsal medially, sensation is supplied by the
medial dorsal cutaneous branch of the superficial peroneal nerve. The
dorsal lateral aspect is usually a continuation of the first web space
innervation by the terminal branches of the deep peroneal nerve.
Plantar, the medial and lateral plantar hallucal nerves from the medial
branch of the posterior tibial nerve provide sensation to the great
toe. These nerves run just medial and lateral to their respective
sesamoids and can be easily injured by traumatic or iatrogenic means.100
It is behind only knee and ankle injuries in importance for time lost
from athletic activity. The spectrum of involvement is wide, from minor
sprain to frank dislocation or disruption of the complex.13,51 The mechanism of injury can be quite variable, making the diagnosis in
multiple trauma difficult. Hyperdorsiflexion (turf toe),12,20 plantarflexion (sand toe),39
and valgus and varus stresses have all been described for this injury.
In all instances, there is simultaneous axial loading of the joint. The
amount and rate of force application determine the extent of the injury.
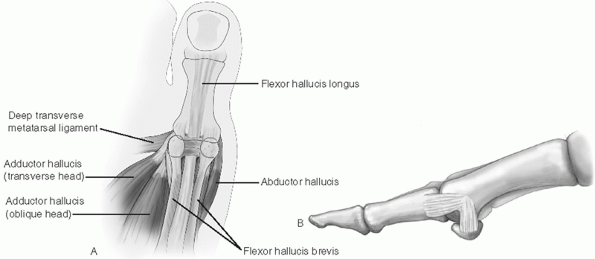 |
|
FIGURE 60-50 Functional anatomy of the first metatarsophalangeal joint. A. Dorsal view of plantar ligamentous structure of the volar plate. B. Lateral view depicting the ligamentous attachments between the metatarsal head and the volar plate and proximal phalanx.
|
the examiner and close physical examination. A simple avulsion fracture
from the metatarsophalangeal joint may be a sign of traumatic joint
instability.20 Pain with weight
bearing or exertional activities may be the only clue to an isolated
mild injury. Ecchymosis and swelling are not always present initially.
The presence of deformity such as the loss of the normal parabolic
cascade of the toes is evidence of a possible injury. Besides close
palpation to determine the point of tenderness, it is important to
discern the structures involved. The presence of passive and active
stability is important to note. Both the range of joint motion and
relative stability in all planes should be checked and compared with
the contralateral joint to assess for subtle differences. Acute
instability in any plane denotes a significant injury.11 Another useful tool to assess stability is the dorsoplantar translation test (Fig. 60-51). Increased translation relative to the contralateral side denotes significant instability of the capsular-ligamentous complex.20
and lateral examinations of the forefoot to clearly define the area in
question and prevent overexposure. Also, both medial and lateral
oblique views, as well as a sesamoid view, are needed to fully assess
the joint. Even in the case of frank persistent dislocation, plain
films should be obtained before attempted reduction to determine the
position and condition of the sesamoids. The radiographs may reveal the
presence of intra- or extra-articular fractures, avulsion injuries of
the medial or lateral collateral ligaments, or displacement of the
sesamoid structures. Proximal, distal, or divergent migration of the
sesamoids either together or separately may occur. A sesamoid fracture
or separation through a bipartite synchondrosis is possible. A
comparable view of the contralateral side may be helpful in discerning
any changes in the sesamoid complex position. On the AP view, the
distance between the base of the proximal phalanx and the distal pole
of either sesamoid should be within 3 mm of the same distance on the
contralateral foot.90 If a partite
sesamoid is present, the normal distance between the proximal
phalangeal base and the distal pole of the sesamoid should be less than
10
mm for the tibial sesamoid and 13 mm for the fibular sesamoid. Greater distances denote possible plantar plate disruption.90
Care must be taken in the presence of bipartite sesamoids because the
incidence of bilateral fragments is quite variable. The two factors
most important in determining a treatment plan are, first, the presence
of a dislocation and, second, the joint stability once reduced.
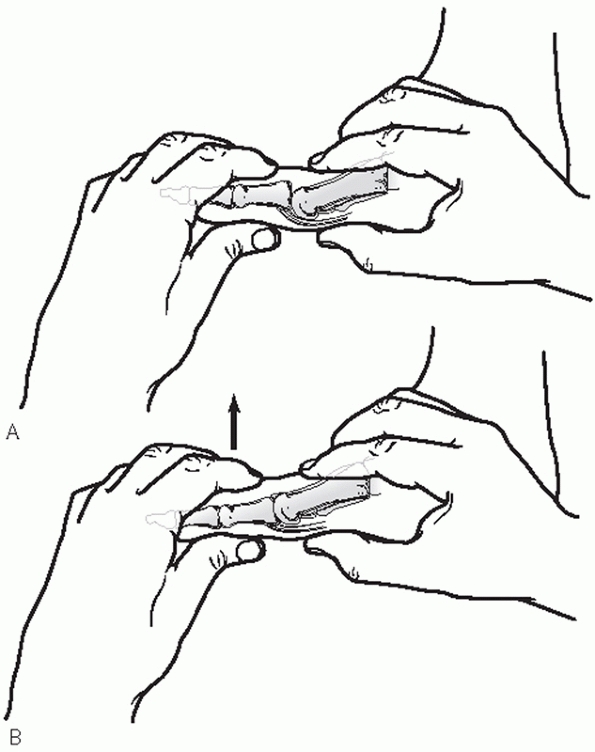 |
|
FIGURE 60-51 Stability test for metatarsophalangeal joint. A. Position of hands to test dorsal plantar stability of volar complex. B. Direction of motion.
|
encompasses the full spectrum of injury possible at the first
metatarsophalangeal joint. Sprains or nondisplaced injuries (turf toe)
have been classified into grades I, II, and III based on pain and
instability20 (Table 60-9).
Treatment and outcome for these injuries correlate well with the
initial grade. Dislocations were first classified by Jahss and later
modified as other variations on the general pattern were reported (Fig. 60-52).
In general, type I dislocations involve an intact plantar plate. Type
II dislocations involve partial disruption of the plantar plate in some
manner. Jahss type III dislocations have a complete dissociation of the
plantar plate from the base of the proximal phalanx. The OTA system
classifies the dislocation of all joints involving the toes under the
80-D heading. Dislocation of the first metatarsal phalangeal joint is
designated 80-D1.1, where the 1.1 denotes the metatarsal- phalangeal
joint of the first toe.71 There is no sub-classification for position or sesamoid involvement. Sesamoid dislocation has a separate code: 80-D4.
first metatarsophalangeal, two factors determine treatment: the ease of
joint reduction and the resultant stability. The term turf toe12,20 is generally used to discuss injuries without a history of dislocation to the great toe. Sand toe39
is a more recent term used to describe specifically an injury to the
dorsal capsule of any toe. Treatment for these injuries is akin to
treating sprains in other joints with a period of rest and
immobilization dependent on the severity of the injury.12,20,39
Rest, ice (slurry baths), compressive wraps, and immobilization or
protected weight bearing are used to aid in recovery of the joint.
Stiff-soled shoes or rigid inserts are used initially for weight
bearing to minimize capsular stretch. Activity is advanced as symptoms
abate. Operative intervention is rarely indicated except in cases of
intra-articular fractures or significant discrete instability.12
The presence of avulsion fragments in the face of significant valgus
instability may need to be addressed by open reduction and internal
fixation or debridement and ligamentous repair.20 Displaced intra-articular fractures or osteochondral lesions should be fixed or debrided depending on their size.
|
TABLE 60-9 Classification of Turf Toe Injuries
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
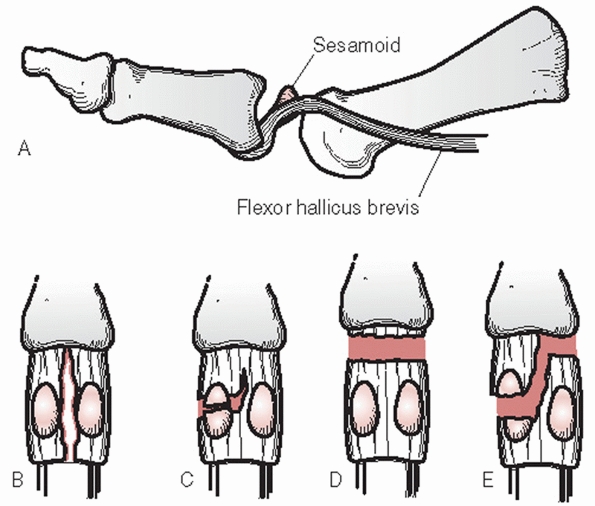 |
|
FIGURE 60-52 Modified Jahss classification of first metatarsophalangeal dislocations. A. Type I: Dorsal dislocation without disruption of sesamoid complex. Usually not reducible closed. B.
Type IIA: Dislocation with longitudinal disruption of volar plate and intersesamoid ligament, noted by increased distance between sesamoids. C. Type IIB: Partial disruption of volar plate with disruption of either medial or lateral sesamoid. D. Type IIIA: Complete soft tissue disruption of the volar complex from the proximal phalanx. E. Type IIIB: Complete volar plate disruption including disruption of one sesamoid. |
acute dislocations is sparse. All agree that dislocations of the first
metatarsophalangeal joint should be immediately reduced to minimize any
further compromise to the soft tissues. Initial reduction can be
obtained with gravity traction using finger
traps
attached to the first toe to suspend the heel off the ground. An easy
reduction usually denotes a significant injury of the plantar plate and
has no inherent stability once reduced.13,43,51,81
In the case of an intact plantar plate, the initial dislocation is
usually not reducible by closed means. Associated fractures of the
metatarsal or disruption of the tarsometatarsal joint can make closed
reduction of the dislocated metatarsophalangeal joint possible. In
these cases, reduction of the joint should be done before achieving
bony stabilization proximally.13
Many dislocations that occur due to high-energy trauma have plantar
wounds. In the rare instance when a closed reduction is obtained and no
further instability is noted, conservative treatment measures are
instituted for the joint as described for sprains.
unstable joint, operative intervention becomes necessary to restore
stability and function. The irreducible joint is usually due to the
intact plantar plate resting dorsal to the metatarsal head (Jahss type
I). Apparent irreducibility can also occur with a longitudinal split of
the plantar plate that allows the metatarsal head to button-hole
through (Jahss type IIA). The difference between these two types can
easily be discerned on the AP radiograph by the wide dissociation of
the sesamoids in the Type II pattern.13
The difference is important for planning the operative approach. A
dislocation with an intact plantar plate can be approached either
plantar or dorsally. If the surgical approach is not limited by soft
tissue injury, the dorsal approach appears to be the more acceptable
way and eliminates the potential of iatrogenic injury to the plantar
hallucal nerves.13
plantar directed pressure on the plantar plate to reduce it around the
end of the metatarsal head. Due to the significant disruption of the
collateral ligaments, the reduced joint should be immobilized in a
rigid dressing until tenderness on examination is diminished
sufficiently to begin active motion and weight bearing. Then the
regimen for sprain care should be followed.
 |
|
FIGURE 60-53 Radiograph of Type IIA dislocation of the first metatarsophalangeal joint. A. Anteroposterior view with loss of joint space and widening of the intersesamoid space. B. Lateral view with sesamoid noted behind metatarsal head and complete dislocation of joint.
|
usually results in significant residual instability of the joint.
Disruption can manifest itself in any number of ways, including
complete disruption of the plate from the proximal phalanx, a
longitudinal split, or some combination involving disruption of either
the medial or lateral sesamoid (Fig. 60-53).
This disruption presents as either a fracture of the sesamoid or
separation of a bipartite synchondrosis. Either way, it denotes a
significant disruption of the stabilizing mechanism of this joint.
Treatment and surgical approach are based on the goal of restoring
structural integrity to the joint. To reduce and repair the plantar
plate, it is best to use a medial longitudinal approach to be able to
access both the dorsum of the joint for reduction and the plantar
aspect for plantar plate repair. Avulsion of the plantar plate from the
proximal phalanx should be repaired with sutures through drill holes
from the plantar aspect to the dorsum of the proximal phalanx.
Disruption of the intersesamoid ligament is sutured together. Great
care should be taken not to include the flexor hallucis longus in the
repair. Free movement of the tendon should be visualized with isolated
motion of the interphalangeal joint after the repair is complete.
Sesamoid fracture or separation should be reduced and held with
cerclage, soft tissue sutures, or mini fragment screw. In the case of
severe comminution, unilateral removal of the sesamoid with repair of
the resulting defect can be considered. The repaired plantar structure
is protected from dorsiflexion for up to 6 weeks before starting
non-weight-bearing motion and then progressed along the same guidelines
as for sprain care.
stiffness and disruption of the normal weight-bearing position of the
great toe can lead to permanent changes in gait mechanics and a
reduction in activities due to pain. The development of hallux rigidus
may be in part a result of recurrent injury to this joint. Valgus
instability can lead to hallux valgus deformity. Late instability or
the appearance of osteochondral fragments should be watched for closely
and treated aggressively by surgical repair of the disrupted
structures. Sesamoid nonunions, fibrous unions, or arthropathy can also
appear with these injuries. Treatment of these complications should
follow those outlined for care of the isolated injury. Complications
appear to be minimized with aggressive stabilization and rehabilitation
of the joint.
section, are an integral part of the capsular-ligamentous structure of
the first metatarsophalangeal joint. They function within the joint
complex as both shock absorbers and fulcrums in supporting the
weight-bearing function of the first toe. Their position on either side
of the flexor hallucis longus forms a bony tunnel to protect the tendon.7
The medial plantar branch of the posterior tibial artery provides the
vascular supply to the sesamoids. Medial and lateral branches enter
each sesamoid respectively at the proximal pole. Secondary vessels
enter the sesamoids from the plantar surface. Lesser vessels about the
periphery do not appear to pierce the outer cortex of the sesamoid to
add to the osseous circulation.18,105
ossification centers, which may not unite. This gives rise to partite
sesamoids. The medial sesamoid exhibits a partite appearance 10 times
more often than the fibular sesamoid. The problem is the variability in
their presence. There is a reported incidence of anywhere from 5% to
30% in the general population. The reported incidence of bilaterally
also varies between 25% and 85%.19,50 Both these variables make using contralateral views to rule out a fracture difficult.
with the sesamoids, with diagnoses ranging from sesamoiditis to stress
fracture, to acute fracture.7,46
The mechanism of injury varies with the diagnosis. Direct blows such as
a fall from a height or a simple landing from a jump as in ballet can
cause an acute fracture. Acute fractures can also occur with the
hyperpronation and axial loading seen with joint dislocations.
Repetitive loading from improper running usually gives rise to the more
insidious stress fracture. The major fracture pattern is transverse in
nature and seen with indirect or repetitive injuries. Comminuted or
stellate patterns are noted in cases of direct loading. The medial
sesamoid is more often injured.
diagnosis, usually presents itself as a localized pain on the plantar
aspect of the joint directly under the sesamoid involved. The presence
of a soft tissue callus under the sesamoid denotes a chronic process.
Active or passive dorsiflexion of the metatarsophalangeal joint can
initiate or exacerbate the pain. Swelling is occasionally seen.
radiographic views should be obtained of the first metatarsophalangeal
area in all cases. Because normal foot films tend to overexpose and
obscure the bony anatomy of the forefoot, it is important to specify
coned down views to get the best exposure to visualize this area. The
sesamoid view should be adjusted to allow visualization of the
metatarsal-sesamoid joint surface. In the case of partite sesamoids, a
similar view of the contralateral side can be helpful but need not be
taken routinely because the variability in the presence of bilateral
partite sesamoids makes comparison difficult. The absence of bilateral
partite sesamoids does not confirm the presence of a fracture.90,100
best way to discern between a partite sesamoid and an injury. Partite
sesamoids have smooth sclerotic edges and the sum of its parts makes a
sesamoid larger than a normal one. In contrast, with a fracture:
-
A fracture margin on a sesamoid is rough and irregular.
-
Because of the tight support of the plantar plate, there is minimal separation unless the plate is torn.
-
The sum of the fracture fragments should equal a normal sesamoid size.
-
Fracture callus is usually apparent on subsequent follow-up.
with a partite sesamoid also. If clinical symptoms point to an acute
injury of a partite sesamoid, stress views of the joint are recommended
to rule out disruption of the synchondrosis. This is done by taking AP
views of the sesamoids with the toe dorsiflexed and comparing it to an
unstressed view. Varus or valgus stress can be added to place further
tension on the side of suspected injury. Significant separation
indicates at least partial disruption of the plantar plate and may
denote plantar plate instability.43,94
injury has been touted in the past as a useful tool. Recent studies of
its reliability show a low specificity in identifying sesamoid injuries.19 Focused CT scans or MRI studies may aid in the diagnosis of these injuries.9,10
There is no recognized classification system for fracture of the
sesamoid. The OTA compendium provides a code for noting any sesamoid
dislocation, 80-D4.71
Cast immobilization with a toe plate provided to prevent dorsiflexion
of the metatarsophalangeal joint as well as a midfoot ridge to minimize
forefoot weight bearing should be used for a period of 4 to 6 weeks.
The longer period appears to be needed for stress-related injuries. As
symptoms abate, treatment is progressed to a stiff-soled shoe to
restrict dorsiflexion for a further 4 to 6 weeks. This time period is
based on the
patient’s
clinical response. Accommodative inserts that unweight the injured
sesamoid can also be used at this time. Complete relief of symptoms can
take as long as 6 months.74,112,115
In cases of significant displacement suggesting plantar plate injury,
treatment should follow the guidelines for joint dislocation with plate
disruption as described earlier (see p. 2155).
|
TABLE 60-10 Closed Management of Sesamoid Fractures
|
|
|---|---|
|
either excision of the sesamoid or bone grafting of the ununited defect
should be done. Complete excision has been the treatment of choice but
is not without complications.101 If
the articular surface of the sesamoid is intact and the cartilage is
healthy, an attempt at bone grafting of the defect should be undertaken.3
The joint is inspected for articular congruity. Whether grafting or
excising, great care must be taken to maintain the integrity of the
plantar complex. For grafting, the sesamoid should be approached just
plantar to the insertion of the abductor hallucis tendon and only the
medial wall exposed. No further plantar or proximal dissection should
be done to minimize damage to the sesamoid blood supply. The cortex is
disrupted by drill holes and the void filled with cancellous graft. A
circumferential cerclage stitch of nonabsorbable suture can be placed
around the sesamoid parallel to the articular surface and in the
substance of the plantar plate to provide some stability and
compression, or a mini fragment screw can be used to provide
compression (Fig. 60-55). In the case of
sesamoid excision, the sesamoid should be carefully shelled out from
the plantar plate. Sutures should be placed across the void to maintain
plate continuity and reconstruct the short flexor mechanism. The
abductor hallucis tendon should be advanced into the distal capsule to
enhance the repair.
dorsal and plantar approaches have been described. Both go through the
first intermetatarsal space. The dorsal incision appears to be the
better approach for isolated sesamoid pathology. Direct visualization
of the joint surface and minimal disruption of the blood supply occurs
with this route. This approach is more difficult if there is an
associated disruption of the plantar plate, which may be better
addressed through a plantar incision. Either way, great care must be
taken not to injury the lateral plantar nerve just lateral to the
lateral sesamoid (Fig. 60-56). The actual
approach to the sesamoid whether grafting or excising should be
directly lateral through the plantar plate. The plantar incision can be
expanded by curving the distal end through the proximal plantar crease
to expose the plantar plate insertion. Great care again should be taken
to minimize any disruption to the plate. In the case of sesamoid
excision, the adductor tendon should be advanced into the distal aspect
of the plantar plate to strengthen the defect left by the sesamoid
removal.
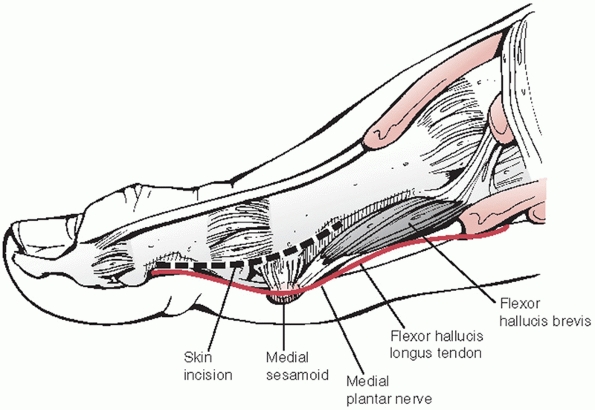 |
|
FIGURE 60-54
Surgical approach to the medial sesamoid. The incision is medially based along the metatarsophalangeal joint to allow both intra-articular and extra-articular access to the tibial sesamoid. It is important to identify and protect the plantarmedial nerve lying medial to the sesamoid. Careful dissection along the plantar plate will expose the medial sesamoid for excision or fixation. |
involved, every effort should be made to not excise both. Significant
disruption of the plantar plate integrity and function occurs with the
loss of both.
postoperative course should mirror the initial conservative course in
treatment. Long-term use of orthotic inserts with arch support and
protection of the injured sesamoid should be routinely considered. With
chronic sesamoiditis, the use of devices such as a full-length, carbon
fiber insert to help restrict metatarsophalangeal dorsiflexion may also
be helpful in reducing recurrence.
unrecognized fractures can lead to significant pain and restriction of
activity. Chronic pain despite appropriate treatment is also a problem.
The treatment of last resort, surgical excision, also can lead to
significant problems. Late deformities resulting from the imbalance in
the dynamic mechanism caused by the loss of a sesamoid or damage during
surgery to plantar plate complex integrity can lead to hallux varus or
hallux valgus deformities as well as a cock-up toe. Transfer
metatarsalgia onto the remaining sesamoid or to other metatarsals may
occur. These problems are best minimized by meticulous attention to
detail during surgery and the use of orthotics to improve load sharing
along the forefoot.
 |
|
FIGURE 60-55 Medial sesamoid fracture with plantar plate disruption. A. Preoperative radiograph showing separation of medial sesamoid as well as proximal migration of lateral sesamoid. B,C. Six-week postoperative radiographs showing mini fragment screw in sesamoid.
|
toes are much like the great toe in that their stability comes from the
ligamentous attachments and position of the plantar plate. In the case
of the lesser toes, the plantar plate is actually an intra-articular
portion of the transverse intermetatarsal ligament connecting all the
lesser toe metatarsophalangeal joints. It is attached to each
metatarsal by medial and lateral metatarsal-phalangeal ligaments.
Medial and lateral metatarsal-phalangeal collateral ligaments attach
between the metatarsal head and the base of the articulating phalanx.
There are no motor attachments directly into this complex. Positional
response is due to the dynamic position of the distal segments of the
toes.
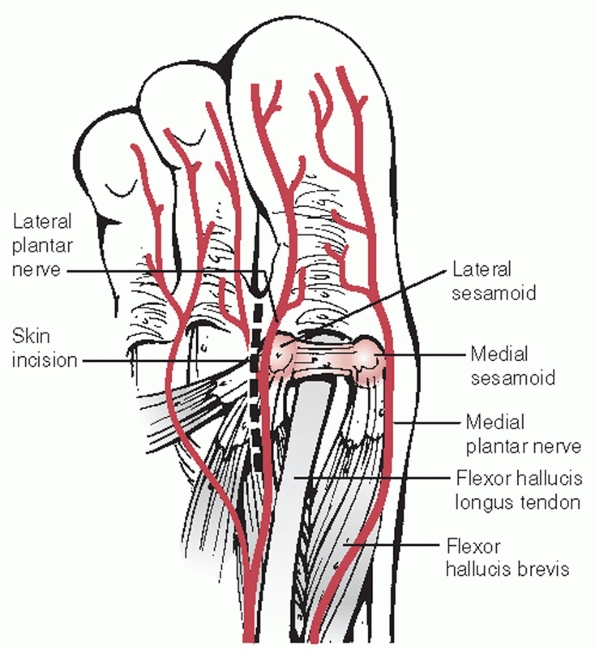 |
|
FIGURE 60-56
Surgical approach to the lateral sesamoid. The incision is plantar, based between the palpable second metatarsal head and the lateral sesamoid. Careful dissection is needed to identify and protect the lateral plantar nerve just lateral to the sesamoid. From this approach, the sesamoid and lateral tendinous insertions are visualized. |
lesser metatarsophalangeal joints are rare. The literature describes
only two types of traumatic injuries: hyperdorsiflexion and
hyperplantarflexion with axial loading.14,39,46
Isolated hyperdorsiflexion injuries without dislocation are not
mentioned in the literature. Hyperflexion injuries of the lesser toe
are only mentioned in the presence of the sand toe type39
injury of the first metatarsophalangeal joint. Dislocations of the
lesser toes do occur with forced dorsiflexion and axial loading and are
reported as a part of multiple trauma in motor vehicle collisions.
Lateral, medial, or plantar displacement forces have also resulted in
dislocations at these joints.
about the joint in question. Disruption of the normal parabolic cascade
of the toes is visible in the plane of the deformity (Fig. 60-57).
In dorsal dislocations, the metatarsal head is prominent plantar and
the toe appears hyperextended. Radiographs of the forefoot in the AP,
lateral, and oblique planes will aid in the diagnosis and help to rule
out associated fractures and disruptions of surrounding joints.
Ipsilateral foot fractures and dislocations are often associated with
these injuries.
classification method for metatarsal-phalangeal dislocations, the
recent OTA compendium creates a system to catalog these injuries.71
The major designation for metatarsal-phalangeal joint dislocations is
80-D1._. The classification is further divided by the metatarsal
involved. The added designation, 80-D1.2, represents a dislocation of the second metatarsal-phalangeal joint (Fig. 60-58).
There is no further subclassification to designate direction. Multiple
dislocation of the metatarsal-phalangeal joint is designated 80-D1.9.
 |
|
FIGURE 60-57 Lesser toe dislocation at the metatarsophalangeal joint. A.
Clinical view of widened web space and individual clawing of involved toes from recent trauma. The clinical scar is from previous trauma. B. Radiograph of the involved joints shows unreduced dislocations of the second and third joints. |
attempted for a lesser toe metatarsophalangeal dislocation. Usually a
circumferential ankle block with 0.25% Marcaine can be used to reduce
discomfort and relax the patient after a thorough examination of the
foot. Finger traps to the affected toe(s) are used for gravitational
traction to stretch out the joint tissues. The toe is then
hyperdorsiflexed at the dislocated joint, and the phalanx is pushed
distally beyond the end of the metatarsal and then brought into
plantarflexion. This closed technique is successful about half of the
time.14
reduction is performed through a dorsal approach. In almost all cases
the pathology preventing reduction has been found to be the plantar
plate.14 One case report found the flexor digitorum longus to be a block to reduction for a fifth metatarsophalangeal dislocation.48 Once reduced, the joint should be assessed for residual stability. Temporary pinning to stabilize the joint is recommended.
Post reduction AP radiographs should be obtained and checked closely
for any asymmetry between the joint spaces of the lesser
metatarsophalangeal joints. Widening of a single joint space may be due
to an incarcerated plantar plate.
for lesser joint injuries is similar to that from great toe injuries.
Weight bearing and progression of activities are dependent on symptoms.
Pins used to stabilize joints initially should be removed at 3 weeks.
these injuries early. Problems with residual pain and stiffness are
most often related to a missed diagnosis or late or recurrent
instability. The presence of other injuries to the ipsilateral foot
also has a dramatic effect on outcome. Isolated injuries treated with
early reduction and rehabilitation has the best outcome.
forefoot. The proximal phalanx of the fifth toe is the one most often
involved.46 In fact, fracture of the proximal phalanx of any toe is much more common than fracture of the middle or terminal phalanx.
majority of phalangeal fractures. A direct blow such as a heavy object
dropped onto the foot usually causes a transverse or comminuted
fracture. The second or stubbing injury is the result of axial loading
with secondary varus or valgus force resulting in a spiral or oblique
fracture pattern.44,46 This mechanism is most likely to produce clinical deformity.
signs and symptoms with these injuries. Also, difficulty with shoe wear
and pain with ambulating bare foot or with supple shoes are common.
Occasionally, the patient will relate a history of acute deformity with
spontaneous or manipulated reduction.
Radiographic
examination is important in differentiating between a sprain,
dislocation, and/or fracture. Standard AP and lateral films of the
forefoot should be obtained.
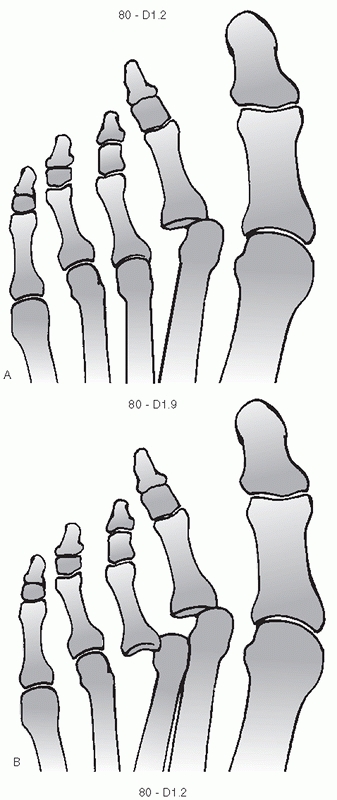 |
|
FIGURE 60-58 OTA classification for metatarsal phalangeal dislocation (80-D1. _). The last place denotes the metatarsal involved. A. Example of second metatarsal phalangeal dislocation. B. Designation for multiple dislocations.
|
only classification that allows an accurate description of the fracture
pattern involved.71 The designation
of phalangeal fractures under this system observes the format (88( )-_
_._) in a fashion similar to the metatarsals of the foot. To denote
which ray the classification refers to, an alpha numeric identifier
should be placed in parentheses beside the major designation: first toe
(T1/2), second toe (N1/2/3), third toe (M1/2/3), fourth toe (R1/2/3),
fifth toe (L1/2/3). The second numeric designation denotes whether it
is the proximal (1), middle (2), or distal (3) phalanx that is involved.
represents fracture complexity while the numeric subgroupings denote
fracture position and pattern. Group A denotes extra-articular and
simple diaphyseal fractures. Group B involves partial articular and
diaphyseal wedge fractures. Group C involves complex articular or
diaphyseal shaft fractures. The first numeric sub grouping denotes area
of involvement: proximal metaphyseal (1), diaphyseal (2), and distal
metaphyseal (3). The second designation is for fracture pattern
designation and can vary depending on the group and first numeric
designation (Fig. 60-59). There are no data to show its effectiveness with determining care and predicting outcome with these fractures.
painful and usually require modified shoe wear and analgesic medication
for 2 to 3 weeks. All nondisplaced fractures, regardless of their
articular involvement, can be treated with stiff-soled shoes and
protected weight bearing with advancement as tolerated. The use of a
buddy taping technique between adjacent toes may improve pain relief
and help stabilize potentially unstable fracture patterns44,46 (Table 60-11).
With the great toe, stabilizing the proximal fragment for reduction is
usually no problem. For the lesser toes, the use of a pen or pencil in
the web space adjacent to the apex of the fracture can provide the
rigid surface to allow three-point bending pressure against the
fracture (Fig. 60-61). With extra-articular
fractures, axial alignment and rotation are important in fracture
reduction. Axial shortening does not adversely affect function. With
extra-articular fractures, the adequacy of the reduction is determined
by the clinical appearance of the toe in relation to its neighbors and
not its radiographic appearance. The nail bed should be rotated into a
position similar to adjacent toes and the toe’s axial position should
be aligned with the normal cascade of the other toes. Once satisfactory
clinical alignment is obtained, the toe can be buddy taped to its
neighbor for added stability. Lamb’s wool or other soft nonabsorbant
material should be placed in the web space to minimize maceration of
the soft tissues. Sometimes with the great toe, short-term
immobilization in a plaster splint may be necessary to hold the
reduction.
where gross instability or persistent intra-articular discontinuity is
present (Fig. 60-62). This problem usually
arises when there is an intra-articular fracture of the proximal
phalanx of the great toe or multiple fractures of lesser toes. A
grossly unstable fracture of the proximal phalanx of the first toe
should be reduced and can be fixed with percutaneous K-wires or mini
fragment screws. Unstable intra-articular fractures of any joint
despite adequate reduction should be reduced and percutaneously pinned
in place to avoid late malalignment (Fig. 60-63).
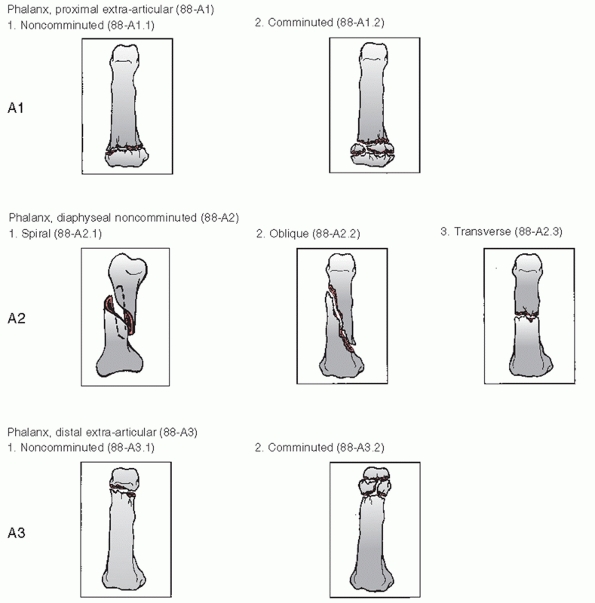 |
|
FIGURE 60-59
OTA classification for phalangeal fractures (88-__._). Modifiers to designate phalanx and toe involved: T1/T2 for great toe, N1/N2/N3 for index toe, M1/M2/M3 for middle toe, R1/R2/R3 for ring toe, and L1/L2/L3 for little toe. A. Classification scheme for type A phalangeal fractures. |
shoes as soon as tolerated. Percutaneous fixation is usually removed at
4 weeks and buddy taping begun until the appendage is asymptomatic with
full weight bearing.
in the form of continued abnormal alignment. This can provide problems
with shoe fit and wear as well as soft corn lesions between toes caused
by bony prominences. The most frequent cause I have seen is missed
diagnosis. Rotational deformities will cause abnormal joint function
and can result in progressive deformity. Late deformities, if
symptomatic, should be treated with refracture and pinning.
The majority occur in the proximal joint, are dorsal in direction, and
occur to exposed, unprotected toes. This type of injury may be
clinically indistinguishable from a phalangeal fracture. Pain or
stiffness with motion and dorsal-plantar thickening of the toe to
palpation are seen clinically. AP and lateral radiographs of the toes
should be viewed carefully for subtle joint differences. Especially
with the interphalangeal joint of the hallux, partial spontaneous
reduction with interposition of the plantar plate or sesamoid will
cause a subtle widening of the joint on radiography. Complete reduction
is required to restore normal function.
classification for these injuries in the literature. The revised OTA
compendium has established a means to code the dislocations of the
interphalangeal joints for reporting and discussion purposes.71
The designation for proximal interphalangeal joint dislocation is
80-D2. Designation of distal interphalangeal dislocation is denoted as
80-D3. As with the metatarsals, there is a subclassification available
to denote which toe is affected using the values 1 to 5 numbering from
medial to lateral (Fig. 60-64). The presence of
multiple dislocation is designated by 80-D9. There is no means to
classify the position of dislocation or the presence of other injury.
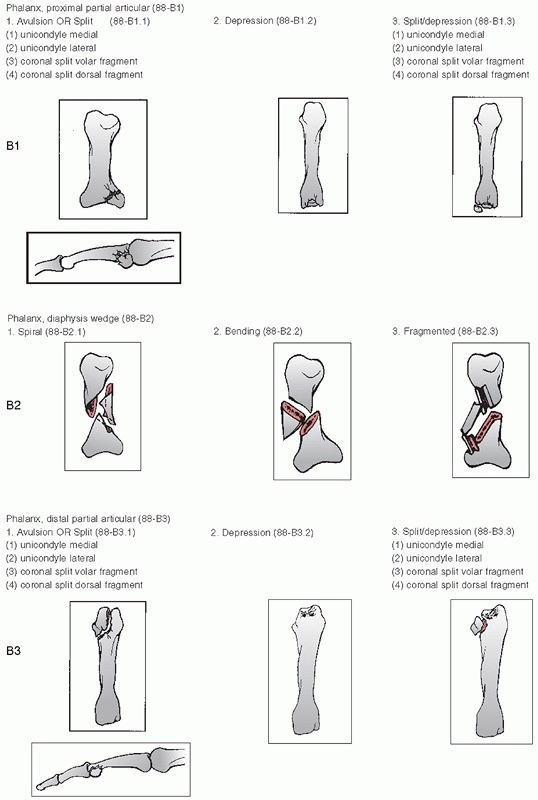 |
|
FIGURE 60-59 (continued) B. Classification scheme for type B phalangeal fractures.
|
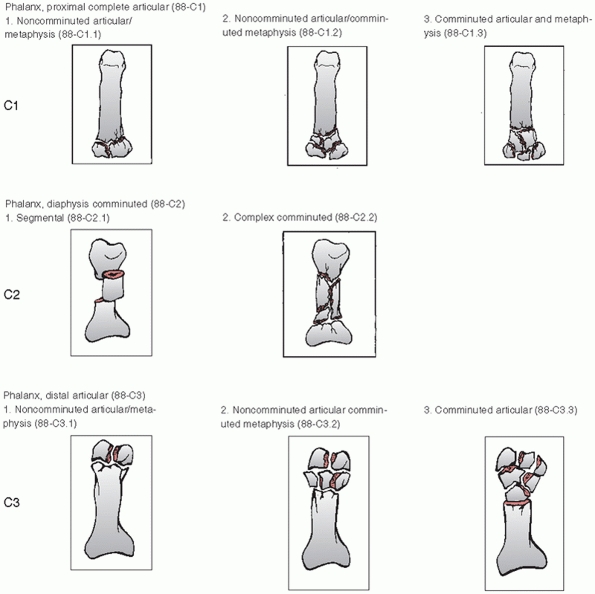 |
|
FIGURE 60-59 (continued) C. Classification scheme for type C phalangeal fractures.
|
|
TABLE 60-11 Closed Management of Toe Fractures
|
||
|---|---|---|
|
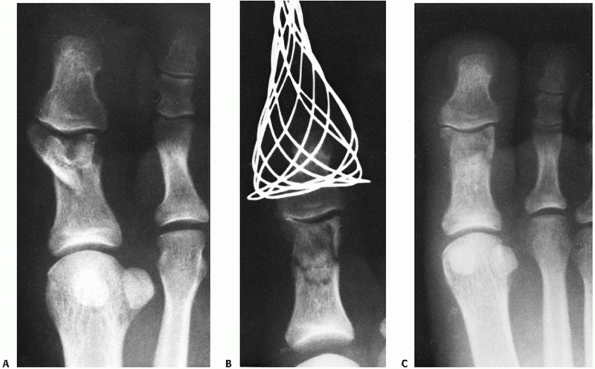 |
|
FIGURE 60-60 A. Displaced intra-articular fracture of the interphalangeal joint of the great toe. B. After the application of longitudinal traction, stable acceptable alignment is achieved. C. One year later, the fracture is healed and the patient is asymptomatic.
|
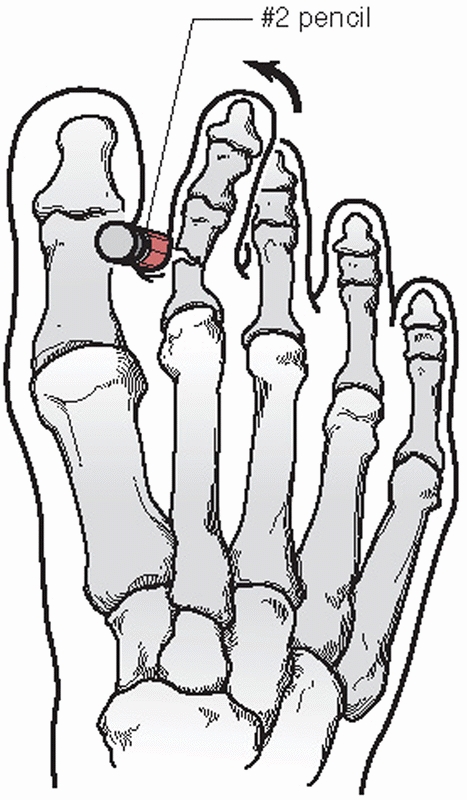 |
|
FIGURE 60-61
A method of closed reduction for displaced proximal phalanx fractures. A hard object, like a pencil, is placed in the adjacent web space and used as a fulcrum for reduction. |
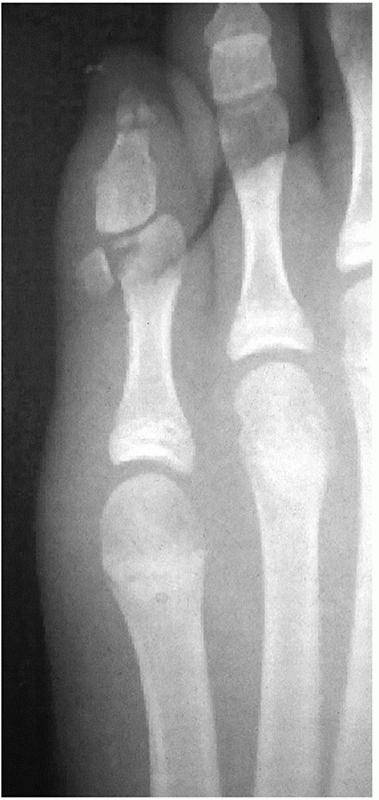 |
|
FIGURE 60-62
Radiograph showing an irreducible intra-articular fracture of the fifth phalanx. This would require open reduction and percutaneous pinning. |
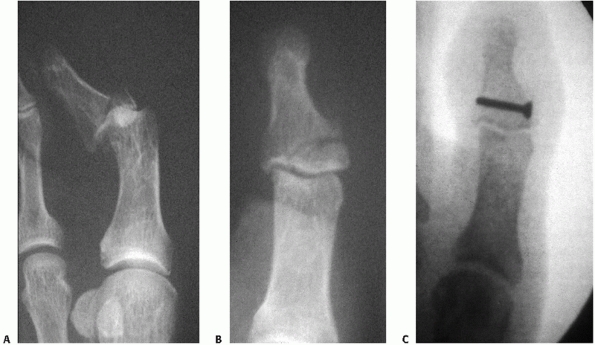 |
|
FIGURE 60-63 Unstable fracture dislocation of the first distal phalanx. A. Anteroposterior view of the initial instability. B. Initial reduction with continued incongruence of the joint and continued instability on movement. C. Internal fixation with 2.7-mm screw to reduce the joint and provide stability for motion.
|
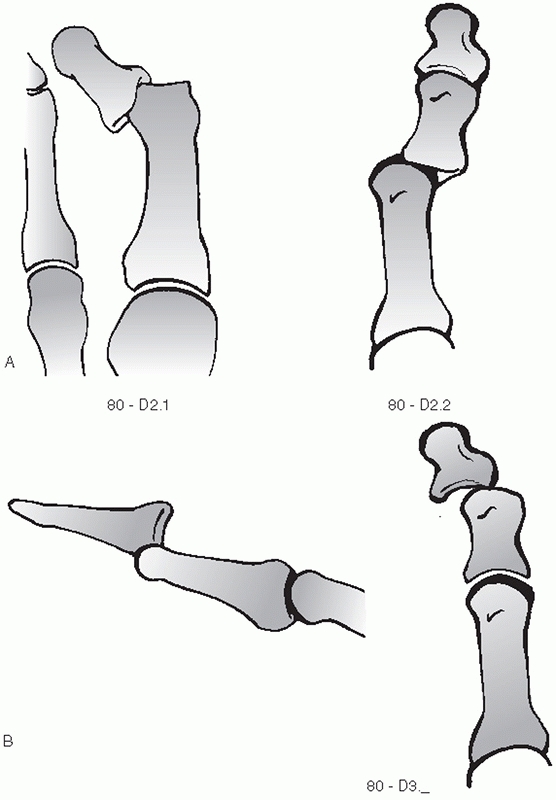 |
|
FIGURE 60-64
OTA classification of interphalangeal dislocations (80- D_._). The last place denotes the toe involved (1 through 5 for first through fifth toes). A. Designation for proximal interphalangeal joint dislocation. B. Classification scheme for distal interphalangeal joint involvement. |
longitudinal traction represent the treatment of choice for these
injuries. Opinions as to the ease with which reduction can be obtained
vary in the literature. In all cases of difficult reduction, the
dorsally displaced plantar plate has been described as the block to
reduction.14 In my personal
experience, I find longitudinal traction followed by plantarflexion can
help with closed reduction. A dorsal surgical approach to the joint is
recommended if closed reduction fails. This allows easy reduction of
the displaced plantar plate. Once reduced, the interphalangeal joint is
stable and can be adequately treated with buddy taping and progressive
activity as tolerated.
few complications. The problems stem from either missed dislocations or
recurrent instability. This problem is seen mainly with the fifth toe.
Treatment involves resection arthroplasty to restore toe alignment and
stability.
trauma to the foot, whenever a violent force is applied to the foot,
the extent of the injury may be greater than initially appreciated.
Great care in determining the full extent of the injury is crucial to
determining proper care. Accurate, timely assessments of the soft
tissue viability and bony and ligamentous stability are the keys to
treating a multiply injured foot.
open injury. Regardless of the mechanism of injury, all open wounds in
the foot should be thoroughly debrided as soon as feasible. Complete
surgical débridement of all contaminated and necrotic tissue is the
most important step in wound management. Often with injuries to the
foot, multiple debridements are required to ensure a clean wound before
closure is attempted. As with all open wounds, tetanus prophylaxis
should be given at the time of presentation and short-term,
prophylactic, broad-spectrum antibiotic coverage should used until
closure. Unless infection supervenes, antibiotics are usually stopped
within 24 hours of wound closure to minimize the risk of nosocomial
infection. Aggressive soft tissue management is important and closure
of wounds either directly or with transferred tissue should be done
when the wound is clean and stable and within 1 week of presentation.77
patients because of the extent of injury to the foot as well as other
areas. Occult fractures and instabilities, if left untreated, can
significantly affect the patient’s outcome. Stress radiographs are
essential to elicit ligamentous and bony instability not readily
apparent otherwise. CT scan of the area in question along longitudinal
and coronal planes can reveal individually nondisplaced fractures,
which together may result in significant instability of the foot.
usually follows closely the suggested treatment of each individual
injury. The overall objective is to preserve circulation and sensation.
This may require modification of normal surgical approaches to reach
all injuries with a minimum of dissection. Preservation of the plantar
skin and fat pads is essential. For proper foot function, maintenance
of a plantigrade position and bony stability are priorities. Preserving
gross motion is desirable and should focus on the talonavicular,
calcaneocuboid, cuboid-metatarsal, and metatarsophalangeal joints. The
remainder can be considered expendable if necessary to achieve overall
foot stability.
performed at the time of presentation to minimize further soft tissue
trauma. In the presence of open injuries, temporary bony stability
should be achieved with K-wires or external fixation at the time of
initial debridement. Definitive fixation should be reserved for the
time of final debridement and wound closure whether by local tissue or
free muscle flap.93 Bony stability
facilitates soft tissue healing. With multiple adjacent, apparently
individually stable fractures, percutaneous fixation is still
recommended to ensure maintenance of overall foot stability and allow
earlier motion of adjacent critical joints. Postoperative care is based
on the specific injuries present and the treatment given.
upper and lower extremities is well recognized in the treatment of
trauma, compartment syndrome of the foot is still an underrecognized
condition. The last 20 years have seen a dramatic increase in the
recognition and treatment of this entity. There are a number of
different types of injuries that in particular have been associated
with foot compartment syndrome. While crush injuries have a high
incidence of probability of causing a compartment syndrome (up to 27%),77
the presence of multiple forefoot fractures, a Lisfranc
fracture-dislocation, or a calcaneal fracture can produce dangerously
high foot compartment pressures, too.
requires a careful examination. The usual signs used in other areas
(increased pain, decreased sensation, or pain with passive motion) are
unreliable in the foot. The injury alone is usually sufficient to cause
significant pain. The most important factor in identifying a
compartment syndrome is a high index of suspicion. Marked swelling of
the foot or multiple significant structural disruptions with intact
skin should arouse suspicion. The best objective means of determining
the presence of compartment syndrome is to measure the compartment
pressures with invasive catheterization. The threshold should be a
measured pressure that is less than 30 mm Hg below the patient’s
diastolic blood pressure. This threshold takes into account the
possibility that the patient may present in a hypotensive state.
Multiple reading sites as well as rechecks over a period of hours may
be necessary to rule out the presence of increased compartment
pressures. It is important to attempt to reach the calcaneal
compartment for pressure reading as it appears to be the most sensitive.69
The medial compartment contains the abductor hallucis and flexor
hallucis brevis muscles and is located plantar and medial to the first
metatarsal. The lateral compartment contains the abductor digiti minimi
and the flexor digiti minimi brevis and is found on the inferolateral
surface of the fifth metatarsal.
The
central compartment is divided into superficial and deep portions. The
deep or calcaneal compartment contains the quadratus plantae muscle.
The superficial portion contains the flexor digitorum longus and brevis
muscles. Dorsally, between each of the metatarsals lie the dorsal and
plantar interosseous muscles, which appear to lie in a separate
compartment defined by each intermetatarsal space. In the plantar
aspect of the forefoot distal and deep to the quadratus plantae is the
oblique head of the adductor hallucis, which also appears to have its
own fascial compartment.
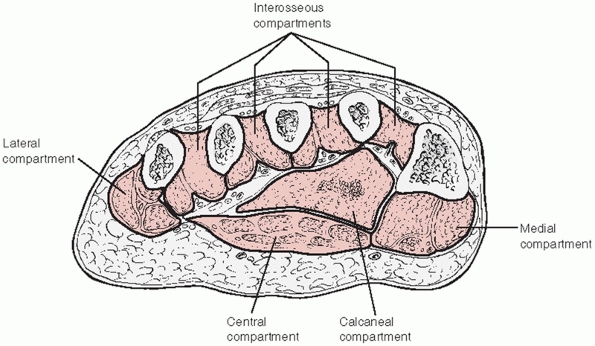 |
|
FIGURE 60-65
Schematic cross section of the foot at the proximal metatarsal level. The major compartments are outlined in their approximate position. The quadratus plantae and adductor hallucis compartments share the space defined as the deep central compartment but have separate fascial boundaries. |
invasive pressure measurements can conclusively show normal compartment
pressures), release of the foot compartments should be done. Presently
the most reliable way to decompress all compartments including the deep
calcaneal is through a three-incision approach69 (Fig. 60-66).
The two dorsal incisions are placed one medial to the second metatarsal
shaft and one lateral to the fourth metatarsal shaft. Blunt dissection
is done between the interosseous muscles and the fascia to the deep
compartments. The lateral compartment is reached by releasing the
fascia attached to the inferolateral aspect of the fifth metatarsal
through the lateral incision. The third, medial incision is used to
access the medial and central compartments more fully. The incision is
within the arch of the foot along the muscle body of the abductor
hallucis. Dissection is carried both dorsal and plantar to this muscle,
freeing it up from the plantar fascia and the attachment to the bony
structures dorsally. This will also disrupt the superficial and deep
components of the central compartment and allow access to the adductor
muscle belly. The medial dissection carries the greatest risk. The
lateral plantar nerve and vessels lie on the quadratus muscle and can
be seen with the release of the compartment. The wounds should be
closed in a secondary fashion 5 to 7 days later.
or without timely treatment. A missed compartment syndrome usually
results in fixed clawing of the toes, requiring surgical release and
realignment due to pain and poor shoe fit. Reports of communication
between the compartments of the foot and the deep compartment of the
leg resulting in adjacent compartment pressure elevation can further
complicate treatment.69 Fasciotomy
also has its risks. Loss of the dorsal skin bridge is possible with the
two-dorsal-incision approach, but this complication appears to be more
the result of the initial tissue trauma than of the surgical procedure.
Damage to plantar structures can occur if careful dissection is not
done.
progressive destruction of joint integrity affecting one or more
peripheral articulations. This process appears to result from the
disturbance of normal pain and proprioceptive sensation in the foot. In
systemic diseases such as diabetes, associated metabolic abnormalities
such as the glycolization of collagen may also contribute to the
destructive process. The interposition of glucose molecules within the
collagen fibers disrupts the interstrand binding and can significantly
weaken the strength and integrity of tendons and ligaments. The end
result is a complete disruption of normal mechanical function and shape
in the foot, which can lead to significant morbidity in the affected
patient.
process has revealed important data for the clinical management of
these patients. This process of joint destruction is progressive in
nature. Animal studies have shown that the appearance of a Charcot
process is caused by repetitive trauma that goes unrecognized or
unchecked. The longer the destructive forces are present, the greater
are the destruction and resultant deformity. These in vivo studies also
showed that an initial fracture must be present before the cascade of
bony destruction and resorption could occur; ligamentous disruption by
itself does not initiate
the
process. Of greatest importance, though, is the information that if the
initial injury is recognized and protected from further trauma, the
fracture will heal and not go on to Charcot destruction.34,35,59,73
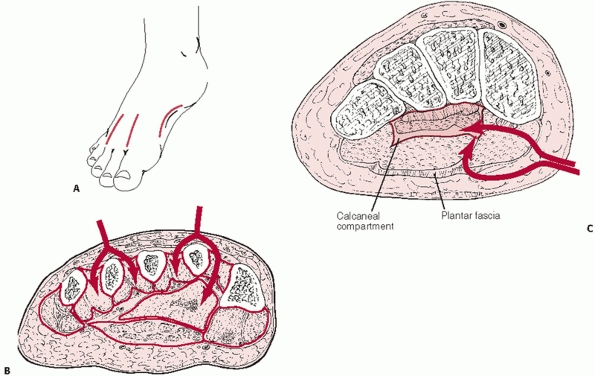 |
|
FIGURE 60-66 Recommended method of foot fasciotomy. A. Relative incision locations on the foot surface. B. Path of blunt dissection through the dorsum of the forefoot. C. The position and direction of the medial incision to reach the calcaneal and oblique adductor hallucis compartments.
|
both the nature of the injury and the loss of protective sensation. The
types of injuries encountered are no different than those of normal
sensate individuals and they exhibit the same underlying mechanisms of
injury. The differences, when present, are usually noticed in the
decreased amount of force present to cause the injury or the relative
lack of discomfort in the patient for the injury noted. Many of these
patients do complain of pain but this appears to be more the result of
the soft tissue edema than of the underlying osseous injury.
systemic condition and their ability to heal is of paramount importance
in deciding treatment for their injury. Consideration of such factors
as the level of their glucose control, nutritional status, and
vascularity all relate directly to their ability to recover from
injury. Diabetic patients with poor glucose control can exhibit
decreased collagen synthesis, impaired cellular proliferation, and
decreased granulocyte function, all of which can have profound effects
on wound healing. Tight control of glucose concentrations can to some
degree reverse these problems.65,106 Serum glycohemoglobin can be used as a measure of a patient’s recent past glucose control.42,106
Over the 120-day life of the red blood cell, glucose enters at a
concentration dependent on the amount of free glucose in the blood. In
a nonenzymatic reaction, it irreversibly binds to hemoglobin, forming
glycosylated hemoglobin. This amount of glycosylated hemoglobin is
directly proportional to the average concentration of free glucose seen
by the cell over its life. Nondiabetic individuals have a
glycohemoglobin level of between 4% and 6%. Ideally, a glycohemoglobin
level less than 8.5% for a diabetic patient denotes tight control of
his or her daily blood sugar.106
problems in diabetics. Adequate healing has been obtained with serum
albumin levels greater than 3.5 g/dL and a total lymphocyte count of at
least 1500.30,42,73
paramount importance in treating these injuries. Without an adequate
vascular supply, healing of damaged tissues will not occur regardless
of the treatment option chosen. Every patient should have the vascular
status of the injured limb documented as soon as the initial edema
recedes. Both arterial Doppler and transcutaneous oxygen pressure
techniques are recommended to assess the limb for adequate healing
potential.34,35,59,63,73
For midfoot and forefoot injuries, arterial toe pressures greater than
40 mm Hg appear to signal adequate vascular supply for healing. In the
face of vascular compromise, assessment by a vascular surgeon should be
done before definitive treatment to determine if improving vascular
flow is an option.
be to minimize deformity, maximize stability, and protect the skin from
subsequent pressure abnormalities. The question of surgical versus
nonsurgical treatment is not yet completely resolved. In the face of an
ongoing Charcot process, with a warm, erythematous, edematous foot with
significant bony destruction, conservative management is advocated. By
definition, this is not an acute injury but rather a situation that has
been developing
over
weeks or even months. It requires prolonged total contact casting and
non-weight bearing to attempt to control the deformity and stop the
repetitive trauma in time for the process to burn itself out. There is
no place for surgical management in the face of an active Charcot
process.
truly acute injury in a diabetic patient before significant bony
destruction occurs. Initially, all neuropathic patients should undergo
immediate immobilization and elevation with strict non-weight bearing
of the extremity. This is done to reduce the acute edema and protect
the appendage from further injury. Radiographic examination is
performed to determine the exact extent and stability of the injury.
The studies should mirror those for similar injuries in nonneuropathic
patients. Stress films are important to completely assess underlying
bony stability.
injuries in the midfoot and forefoot. The treatment of ankle injuries
in diabetics by nonoperative means has shown uniformly poor results,
pointing to the need for stabilization to achieve healing of these
fractures. One of the major fears in operatively managing these
patients is the problem of wound complications caused by the surgery.
This is not to be taken lightly. Great care should be taken to minimize
trauma to the tissues during both the surgical approach and wound
retraction. The literature suggests that, with such careful attention,
diabetic wounds will heal without problems if an adequate vascular
supply is present.
acute injuries in a neuropathic foot as you would with an otherwise
normal individual. Closed treatment should be considered if the injury
is isolated and stable. Prolonged immobilization in a
non-weight-bearing posture is recommended. Weight bearing should only
be allowed after clear radiographic evidence of healing is present. One
should remember that these patients have compromised protective
sensation and may not be able to protect incompletely healed fractures.
Therefore, they have the potential to initiate a Charcot process with
repetitive loading without even knowing it.
individuals who present with unstable injuries without evidence of bony
reaction. Any nontraumatic bony fragmentation or periosteal reaction is
an absolute contraindication to surgery, and then injuries should be
treated as an early Charcot foot with immobilization. The truly acute
unstable injury can be approached in the same manner that the injury
would be cared for in the nonneuropathic patient. Open reduction and
internal fixation has been shown to give these patients the best chance
for a stable foot.
should be immediately immobilized and elevated and placed in a strict
non-weight-bearing status. Stable injuries are treated closed with
immobilization and strict non-weight bearing until healed. Ligamentous
disruptions or unstable bony injury patterns are treated operatively
provided the patient meets the criteria outlined for adequate wound
healing. In the case of ligamentous instability of the midfoot area, I
believe that operative reduction and immediate fusion is the preferred
course. Every attempt is made to preserve the articulation of the
talonavicular, the fifth tarsometatarsal, and the metatarsophalangeal
joints, but the overriding goal is to achieve bony stabilization to
preserve foot position. The surgical technique used is the same
presented in the earlier sections of this chapter. Multiple fractures,
even if they appear stable initially, should be at least percutaneously
stabilized and perhaps even formally fused to adjacent structures to
ensure a stable construct. I find that isolated metatarsal fractures
are best treated with closed reduction when the edema subsides and then
with prolonged non-weight bearing. Multiple fractures should be
realigned, pinned, and protected until healed.
heel cord for signs of contracture limiting the patient’s passive
dorsiflexion. Restricted dorsiflexion in the neuropathic patient can
lead to significant midfoot and forefoot deforming forces leading to
future problems with foot position once healing is complete (Table 60-12).
Any resistance to full dorsiflexion with the knee both flexed and
extended should be addressed with a percutaneous heel cord lengthening
at the time of surgery.5 All
operatively treated feet should be rigidly immobilized in at least a
plantigrade weight-bearing position if not slight dorsiflexion and kept
strictly non-weight bearing until complete healing is seen
radiographically.
protective pressure, position, and/or vibratory sensation does not
allow them the ability to self-assess the amount or effect of weight
bearing or motion on the injury. Without exception, these patients
should be kept strictly non-weight bearing and immobilized until the
foot is cool without evidence of edema and complete radiographic
healing is evident. The use of a well-molded total contact cast is
preferred to protect foot alignment and prevent skin breakdown. The
immobilization period is prolonged and as a rule of thumb should be at
least twice as long as one would do for a normal injury; 3 to 6 months
is not unusual. Once healing is evident radiographically, the return to
normal weight bearing in a diabetic shoe should be gradual. Initial
weight bearing should be done with a cast and advanced to proper shoe
wear only after full weight bearing in the cast is obtained without any
disruption or swelling of the foot. This usually takes a further 4 to 6
weeks to allow the bone to adjust to the increased pressure of weight
bearing.
|
TABLE 60-12 Management of Neuropathic Fractures
|
||||||||
|---|---|---|---|---|---|---|---|---|
|
all the potential complications associated with treating similar
injuries in a nonneuropathic patient. Nonunion, malunion, hardware
failure, and avascular necrosis can occur. Neuropathic arthropathy can
also occur. In the face of early weight bearing or late instability,
repetitive injury can restart the process of bony destruction and
resorption. That is why it is very important to closely monitor and
advise this population of patients on the need for prolonged protection
and personal vigilance in caring for these injuries.
J, Drez D. Nonoperative treatment of stress fractures of the proximal
shaft of the fifth metatarsal. Foot Ankle Int 1986;7:152-154.
D, Stacpoole-Shea S, Nguyen H, et al. Lengthening of the Achilles
tendon in diabetic patients who are at high risk for ulceration of the
foot. J Bone Jone Surg Am 1999;81A:535-543.
D, Saltzman C. Disorders of the hallucal sesamoids. In: Adela-ar R, ed.
Disorders of the Great Toe. Rosemont: American Academy of Orthopedic
Surgeons, 1997: 33-41.
M. Athletic injuries of the Great Toe metatarsophalangeal joint. In:
Adela-ar R, ed. Disorders of the Great Toe. Rosemont: American Academy
of Orthopedic Surgeons, 1997:1-22.
B, Briggs P. Surgical management of acute tarsometatarsal fracture
dislocation in the adult. Clin Orthop Relat Res 1998;353:125-133.
P, Rodgers M, Iiboshi A. Pressure distribution under symptom-free feet
during barefoot standing. Foot Ankle Int 1987;7:262-267.
J, Ly T. Treatment of primarily ligamentous Lisfranc joint injuries:
primary arthrodesis compared with open reduction and internal fixation.
J Bone Joint Surg Am 2006;88A:514-520.
H, Manos R, Buoncristiani A, et al. Abduction stress and AP
weight-bearing radiography of purely ligamentous injury in the
tarsometatarsal joint. Foot Ankle Int 1998; 19:537-541.
T. Fractures of the proximal fifth metatarsal: selecting the best
treatment option. J Am Acad Orthop Surg 1995;3:110-114.
S, De Lee J, Page C. Nutritional status: importance in predicting wound
healing after amputation. J Bone Jone Surg Am 1984;66A:71-75.
M, Crawford H, Saltzman C. Peroneus longus tendon obstructing reduction
of cuboid dislocation. J Bone Jone Surg Am 2001;83A:1387-1391.
B, McCollum M, Murphy G, et al. Risk of sural nerve injury with
intramedullary screw fixation of fifth metatarsal fractures: a cadaver
study. Foot Ankle Int 1999;20: 182-184.
K, Blackwell J, Gilmour W. Operation for nonunion of stress fracture of
the tarsal navicular. J Bone Jone Surg Br 1989;71B:105-110.
M, Naranja R, Glasgow S, et al. Analysis of failed surgical management
of fractures of the base of the fifth metatarsal distal to the
tuberosity: the Jones fracture. Foot Ankle Int 1996;17:449-457.
N, Trevino S. Sural nerve entrapment by avulsion fracture of the base
of the fifth metatarsal bone. Foot Ankle Int 1981;2:154-155.
G, Chrzan J, Giurini J. Reconstructive foot surgery for the diabetic
patient. In: Kozak G, Campbell D, Frykberg R, eds. Management of
Diabetic Foot Problems. Philadelphia: WB Saunders, 1995.
R, Saxby T, Vandemark R. A new type of dislocation of the first
metatarsophalangeal joint: a case report. Foot Ankle Int
1992;13:540-545.
S. Foot Injuries. In: Browner B, Jupiter J, Levine A, Trafton P, eds.
Skeletal Trauma. 2nd ed. Philadelphia: WB Saunders, 1998:2405-2438.
P, Reschauer R, Kutscha-Lissberg E. Injuries to the tarsometatarsal
joint: incidence, classification, and treatment. J Bone Jone Surg Br
1982;64B:349-356.
J. Fractues and dislocations of the foot. In: Rockwood C, Green D,
Bucholz R, Heckman J, eds. Fractures in Adults. 4th ed. Philadelphia:
Lippincott-Raven, 1996.
J, Labib S, Fowler R. Intramedullary screw fixation of the fifth
metatarsal: an anatomic study and improved technique. Foot Ankle Int
2004;25:274-277.
K, Fuller P, Brukner P, et al. Outcome of conservative and surgical
management of navicular stress fracture in athletes. Am J Sports Med
1992;20:657-666.
K, Menger A, Retzlaff S. Nonoperative treatment of fifth metatarsal
fractures in an orthopaedic suburban private multispecialty practice.
Foot Ankle Int 2005;26: 704-707.
R, Tejwani N, DiGiovanni C, et al. Outcome after open reduction and
internal fixation of Lisfranc joint injuries. J Bone Jone Surg Am
2000;82A:1609-1618.
C, Birkedal J, Dickerson E, et al. Stabilization of Lisfranc joint
injuries: a biomechanical study. Foot Ankle Int 2004;25:365-370.
L, v d Werken C. Fracture-dislocations of the tarsometatarsal joint, a
combined anatomical and computed tomographic study. Injury
1992;23:51-55.
P, Maurer R. Talonavicular dislocations and midfoot arthropathy in
neuropathic diabetic feet: natural course and principles of treatment.
Clin Orthop Relat Res 1989: 226-231.
B, Stoppacher R, Kristiansen T. Plantar lateral dislocation of the
medial cuneiform: a case report. Foot Ankle Int 1998;19:118-119.
R, DeGnore LT. Isolated dislocation of the middle cuneiform in a
farmer: a case report and review of the literature. Foot Ankle Int
1997;18:735-738.
R, Prieskorn D, Sobel M. Midtarsal and tarsometatarsal arthrodesis for
primary degenerative osteoarthritis or osteoarthritis after trauma. J
Bone Jone Surg 1996;78: 1376-1385.
A, Weber T. Fasciotomy of the foot: an anatomical study with special
reference to the release of the calcaneal compartment. Foot Ankle Int
1990;10:267-275.
J, Slongo T, Agel J, et al. Fracture and dislocation classification
compendium: 2007. J Orthop Trauma 2007;21(10 suppl):S1-S128.
C, Winter W, Bucknell A, et al. Injuries to the midtarsal joint and
lesser tarsal bones. J Am Acad Orthop Surg 1998;6:249-258.
M, Fisher R, Burgess A, et al. Fracture dislocations of the
tarsometatarsal joints: end results correlated with pathology and
treatment. Foot Ankle Int 1986;6: 225-242.
R, Mendicino S, Rockett M. Isolated medial cuneiform fracture: review
of the literature and report of two cases. Foot Ankle Int
2000;21:150-153.
M, Rosenstein A, Bjorkengren A, et al. Isolated dislocation of the
tarsal navicular: a case repost. Foot Ankle Int 1988;9:146-149.
D, Stinson W. Excision of the fractured os perineum: a report on five
patients and review of the literature. Foot Ankle Int 1992;13:277-281.
K, Peicha G, Lajtai G, et al. Conventional radiography, CT, and MRI
imaging in patients with hyperflexion injuries of the foot: diagnostic
accuracy in the detection of bony and ligamentous changes. AJR Am J
Roentgenol 1999;173:1673-1677.
E, Kuss G. Etude sur les luxutations du metatarse (luxations
metatarso-tarsiennes) du diastasis entre le 1. et le 2. metatarsien.
Rev Chir Paris 1909;39:281-336.
M, Wippermann C, Krettek C, et al. Fractures and fracture dislocations
of the midfoot: occurrence, causes, and long-term results. Foot Ankle
Int 2001;22:392-398.
S, Warren N, O’Brien S, et al. Diastasis of bipartite sesamoids of the
first metatarsophalangeal joint. Foot Ankle Int 1993;14:425.
B, Mayo K, Hansen S. Intra-articular fractures of the foot: talus and
lesser tarsals. Clin Orthop Relat Res 1993:135-141.
BJ, Benirschke SK, Mosca V, et al. Displaced intra-articular fractures
of the tarsal navicular. J Bone Jone Surg Am 1989;71A:1504-1510.
A, Krisdakumtorn T. Return to activity after sesamoidectomy in
athletically active individuals. Foot Ankle Int 2003;24:415-419.
R, Heckman J. Fractures and dislocations of the forefoot: operative and
nonoperative treatment. J Am Acad Orthop Surg 1995;3:70-78.
T, Nork S, Sangeorzan B. Temporary bridging of the medial column in
severe midfoot injuries. J Orthop Trauma 2003;17:513-520.
R, Austen D, Tuttleman M. Diagnosis and monitoring of diabetes mellitus
and diabetic complications. In: Moore W, Eastman R, eds. Diagnostic
Endocrinology. 2nd ed. St. Louis: Mosby-Year Book, 1996:250-254.
J, Balduini F, Zelko R, et al. Fractures of the base of the fifth
metatarsal distal to the tuberosity. J Bone Jone Surg Am
1984;66A:209-214.
D, Schemitsch E, McKee M, et al. Do foot injuries significantly affect
the functional outcome of multiply injured patients? J Orthop Trauma
1999;13:1-4.
M, Locher S. Reconstruction of the cuboid in compression fractures:
short- to midterm results in 12 patients. Foot Ankle Int
2002;23:1008-1013.
B, Linder J, Giattini J. Treatment of fractures of the fifth
metatarsal: a prospective study. Foot Ankle Int 1997;18:267-269.
