The Role of the Orthopaedic Surgeon in Diagnosing Child Abuse
part of human social interactions transcending time and cultures.
Recorded history indicates that violence toward children has been
condoned and even accepted. The nature of the abuse has encompassed a
broad spectrum of injuries inflicted on children and the neglect of
children by those who are responsible for their well-being. The notion
of children’s rights is relatively modern. Historically, paternal power
was absolute, including the right to abandon, abuse, and even kill
one’s child. Correction and discipline was limited only by the father’s
conscience. This right was extended to anyone involved in rearing the
child.
during the Industrial Revolution. Reaction to this practice was partly
responsible for the development during the 19th century of social
groups dedicated to the prevention of child abuse, and many societies
began to recognize child abuse as a problem that should not be ignored.
The Society for the Prevention of Cruelty to Children was established
in the mid-1800s. In 1860, Ambrose Tardieu reported 32 cases with the
physical signs that are typical of abuse, which included cutaneous
lesions, fractures (before x-ray films were available), subdural
hematomas described as “thickening of blood on the surface of the
brain,” and death. His report also addressed the social aspects of the
relationship between the abused and the abuser.
community’s attention on this problem with his publication in 1946
describing the association between long-bone fractures and subdural
hematomas. In 1962, approximately 100 years after Tardieu’s first
report, the term “battered child syndrome” was coined by C. Henry Kempe
(2). It reported one of the most dramatic
manifestations of family violence and implied that children are injured
by being struck by or thrown against something. When first described,
it was suggested that battered child syndrome “should be considered in
any child with a combination of multiple fractures, subdural hematoma,
failure to thrive, and soft-tissue swellings or skin bruising; when
sudden, unexplained death occurred; and in situations in which the type
and degree of injury were inconsistent with the history.”
an important figure in formulating the concept of “unrecognized trauma
in infants.” He advocated the term “syndrome of Ambroise Tardieu” in
recognition of the French physician’s pioneering work. The “Child Abuse
Prevention Act” in 1974 and the subsequent development of state
reporting laws in the United States followed the publication of Kempe’s
and Silverman’s articles (4).
The popular term “battered child” was recognized as inadequate at that
time, but it had an impact. Since then, the concept of child abuse has
been broadened to include the entire spectrum of childhood injuries
including physical and emotional neglect as well as physical,
psychological, and sexual abuse. “Manifestations of the Battered-Child
Syndrome,” by Akbarnia et al., (6) was one of the early reports on this topic in orthopaedic literature. It appeared in the Journal of Bone and Joint Surgery in 1974 and alerted orthopaedists to the existence and prevalence of this problem.
nonaccidental injury (NAI). Defining a condition by what it is not is
unsatisfactory. The adoption of this terminology not only requires an
acceptable definition of what constitutes an accident, but also
suggests that any injury that does not fit that definition is child
abuse. In addition, it diminishes the gravity of the active infliction
of harm by the abuser and thereby deflects attention from the
perpetrator.
intent to cause harm? Although the definition must include the fact
that the act was willful (otherwise, it would truly be accidental), the
assailant may not be aware of the consequences of his or her actions.
Therefore, premeditation is not required to diagnose abuse. The type of
handling and magnitude of the force involved is on the opposite end of
the spectrum of the reasonableness with which parents and caregivers
should gently, tenderly, and lovingly care for children. Some
understanding of behavior patterns that are typical of those
responsible for the care of a child must be considered when determining
if an act constitutes abuse. In addition, the definition must be
comprehensive to include the spectrum of childhood injuries. Defining
it with precision remains a challenge even for experts.
must be able to encompass the scope of the problems that must be
included in the spectrum of child abuse. We recognize today that child
abuse fits in the spectrum of family violence (7).
Most people now consider abuse ônot as a discrete illness entities or
syndromes, but as symptoms of different issues and risks for particular
children in individual families’ (8).
“Child abuse consists of any act of commission or omission that
endangers or impairs a child’s physical or emotional health and
development. Child abuse includes any damage done to a child which
cannot be reasonably explained and which is often represented by an
injury or series of injuries appearing to be nonaccidental in nature” (9). Included are forms of physical, sexual, and emotional abuse as well as neglect. The Child Abuse Prevention and Treatment Act
(CAPTA) defines child abuse and neglect as “at a minimum, any act or
failure to act resulting in imminent risk of serious harm, death,
serious physical or emotional harm, sexual abuse, or exploitation of a
child by a parent or caretaker who is responsible for the child’s
welfare.”
orthopaedic aspects of this spectrum. Several good reviews of this
topic are available, and the reader is referred to them (10,11). The chapter on child abuse in the previous edition of this text is also excellent (4).
United States Department of Health and Human Services (HHS) to
establish a national data collection and analysis program to make
available information on child abuse and neglect that is reported at
the state level. The department responded by establishing the National
Child Abuse and Neglect Data System (NCANDS). NCANDS is a federally
sponsored effort that collects and analyzes annual data on child abuse
and neglect submitted voluntarily by all the States and the District of
Columbia.
releases its most current child abuse statistics, as reported by the
states, in April of each year. The statistics reported in the following
text were released in April 2004 and represent an analysis of the data
for calendar year 2002 (US Department of Health and Human Services,
Administration for Children and Families. Child Maltreatment 2004:
Reports from the States to the National Child Abuse and Neglect Data
System). This was accessed by the present author on November 21, 2004
at http://www.acf.dhhs.gov/programs/cb/stats/ncands/. The results are available in a publication called Child Maltreatment 2002 (12).
of abuse and neglect (an increase from 826,000 just 2 years earlier).
An estimated 2.6 million referrals of abuse or neglect concerning
approximately 4.5 million children were received by child protective
service agencies. More than two-thirds of those referrals were accepted
for investigation or assessment (most others were unsubstantiated).
annually, making child abuse more common than developmental dysplasia
of the hip and 30 times the incidence of new cases of myelomeningocele.
It is widely held that child abuse is significantly underreported (13).
The actual incidence of abuse and neglect is estimated to be three
times the number that is reported to authorities. All statistics should
be considered suspect, as they represent only the tip of the iceberg.
neglect were made by such professionals as educators, law enforcement
and legal personnel, social services personnel, medical personnel,
mental health personnel, child daycare providers, and foster care
providers. Educators made 16.1% of all reports, whereas law enforcement
made 15.7%, and social services personnel made 12.6%. Only 7.8% of
reports were made by medical personnel. Such nonprofessionals as
friends, neighbors, and relatives submitted approximately 43.6% of
reports.
African Americans had the highest rates of victimization. While the
rate of white victims of child abuse or neglect was 10.7 per 1000, the
rate among Native Americans or natives of Alaska was 21.7 per 1000
children, and for African Americans, it was 20.2 per 1000 children.
Half of all victims were white.
neglect (including medical neglect), approximately 20% were physically
abused, approximately 10% were sexually abused, and 6.5% were
emotionally or psychologically maltreated. In 2002, an estimated 1400
children died of abuse or neglect (more than three children per day)—a
rate of 1.98 per 100,000 children nationally. This is a significant
increase from an estimated 1300 children who died in 2001. Most (84.5%)
of the children who die are younger than 6 years. Forty-one percent of
the fatalities were in children under the age of 1 year. Three out of
four fatalities occur in children younger than 4 years. Abuse of girls
is slightly more common than abuse of boys (48% male; 51.5% female; the
victim’s sex was not reported in 0.5% of cases.) Most victims were
abused by a parent (81%), although reported sexual abuse by a parent
occurs in the minority. The median age of the perpetrators was 31 years
for women and 34 years for men.
Fractures are the second most common presentation in child abuse (skin
lesions are the most common). More detailed analysis of the nature and
frequency of abusive fractures will be provided in the subsequent
section on fractures.
maltreatment are available at the National Clearinghouse on Child Abuse
and Neglect Information at 1-800-394-3366, or http://nccanch.acf.hhs.gov/index.cfm.
promoted the thinking that child abuse is a culmination of a series of
stresses that impinge on parents and children. This idea is based on
Helfer and Kempe’s three elements that contribute to the propensity for
abuse: a child with qualities that are provocative; a parent with the
psychological predisposition; and a stressful event that triggers a
violent reaction (5). In Bittner and
Newberger’s model, there are social and cultural factors that provide a
background in which a family develops. Family stresses (caused by the
child, by the parent, and by social/situational factors) provide an
environment in which a triggering situation can lead to maltreatment of
the child. How the risk for child abuse may operate in any individual
family must be assessed clinically. They proposed that the team of
clinicians must understand the social, familial, psychological, and
physiologic concomitants of child abuse in order to assess the
situation and subsequently develop a comprehensive management plan.
regarded it as a constitutional predisposition to violence, the signs
of which appear only in the presence of an environmental stressor. This
is analogous to someone with a dust allergy who does not respond with
an allergic reaction unless placed in a dusty environment.
from different sources will likely lead to different risk profiles,
incidence, ratios of physical abuse to sexual abuse to neglect, and so
on.
|
TABLE 34.1 RISK FACTORS FOR CHILD ABUSE
|
|
|---|---|
|
NCANDS) and reviews of records from medical data gathered through
hospital systems will almost certainly differ. Interpreting these data
can be misleading and must be done with care. Underreporting in certain
segments of the population may also skew the results. Notable areas of
concern are risk profiles that identify minorities or ethnic groups and
those in the lower socioeconomic class as being more likely to abuse
their children.
for child abuse can help society to focus limited resources for its
prevention and detection on situations that present a high risk. One
might also believe that health care providers with a knowledge of risk
factors will pay closer attention to an injured child whose social
situation is characterized by numerous risk factors for child abuse.
However, because abuse can affect children in all environments,
dismissing the injuries of a white child from a more advantaged
background as not being caused by abuse, without adequate
investigation, is a disservice to that child. Health care providers
have a moral and legal obligation to maintain a high index of suspicion
to avoid underdiagnosis of vulnerable individuals.
plausible history. This fact emphasizes why orthopaedic expertise
regarding fracture mechanisms is required. Understanding the
antecedents of the child’s injury and assessing the plausibility of the
history are two of the initial goals of history taking. For example,
the body mass of a child younger than 12 months typically will not
generate sufficient force to fracture a normal bone in a fall from a
bed, crib, or couch. One must suspect abuse when a nonambulatory child
presents with a fracture. Of course, an insufficiency fracture through
pathologic bone is another possibility in the differential. Because
injuries of any kind are rare in nonabused infants, age is one of the
most important factors in making the diagnosis of child abuse.
impossible, and even with older children it is typically brief and
consists of asking the child how the injury occurred and, in the case
of apparent abuse, who inflicted the injury. The interviewer should
assess the child’s affect and developmental status, and observe the
child’s verbal and behavioral interactions with family members and
other adults. Interviews of caretakers should be more detailed and must
be done separately. Thorough medical and developmental histories must
be obtained.
than healthy developing children. Indications of abuse are the same in
both groups. Behavioral indicators in a child with a disability may not
be recognized or may be attributed to the underlying condition. Risk
factors include increased demands for care, chronic stress on the care
providers, parental attachment problems, parental isolation,
unrealistic expectations, aggressive behavior in the child,
communication limitations leading to decreased ability to report
information about the abuse, inability to communicate specific needs
resulting in neglect, and increased dependency on many caretakers (17).
Children with severe disabilities may be at increased risk of
malnutrition and failure to thrive. Malnutrition is sometimes accepted
as part of the disability, but it can be viewed as neglect to provide a
basic bodily need (18,19).
Some children’s developmental disorders are due to abuse, for example,
shaken baby syndrome can lead to cerebral palsy. There is a lack of
adequate studies regarding the incidence and nature of abuse in
children with disabilities, but these children certainly represent a
vulnerable population. Awareness of the uncommon Munchausen syndrome by
proxy (20) will help avoid missing this complicated form of abuse.
response to potential maltreatment. Cooperation and liaison with
official community agencies such as the child protection service (CPS),
law enforcement, and prosecutors is crucial and legally mandated. Open,
good-faith exchange with these agencies is legal and protected. It is
not restricted by the Privacy Rule of the Health Insurance Portability
Accountability Act (HIPAA).
document a description of the injury. Whether that is the orthopaedist
or another member of the health care team depends on the local medical
community and the situation of the particular case. Use quotations when
possible, identify “players,” control information exchange, do not
suggest a mechanism of injury, and avoid confrontation, accusation, and
prejudicial statements. Document everything including parental behavior
and the presence of visitors. The interviewer should keep in mind that
questioning does not equal blaming. Immediately address the concern
that the injuries may have been inflicted. What has happened cannot be
changed, what is happening currently can be stopped, and abuse that
could occur in the future can be prevented. The needs of the child and
provision of medical care to the child are the primary concerns and
should be given priority over the child abuse workup. Family-centered
care may have to take a back seat. The parents’ right to know needs to
be balanced against possible threats (direct or indirect) to the
child’s safety. Obtaining and documenting adequate information to rule
out inflicted injury is crucial, but these efforts are often
inadequate. Oral et al. (21) retrospectively
reviewed emergency room charts and orthopaedic office notes. In a large
percentage of cases, they found that documentation was insufficient to
explain the cause of fractures and thereby rule out inflicted trauma.
They advocated the use of forms, protocols, and periodic chart review
to help ensure
compliance (see the section of this chapter entitled “Author’s Preferred Treatment”).
required. Again, the environment will determine which professional is
primarily responsible for this. If the child is seen in the emergency
room of an urban children’s hospital, an emergency room physician or
pediatrician will be accountable. If it is a more rural or isolated
environment, the orthopaedist may need to take a more active role. In
addition, the orthopaedist’s role will vary depending on whether the
cause of the injuries has already been identified as abuse at the time
of consultation. If so, the role will be to ensure that all
musculoskeletal injuries are found and to document their nature and
severity. If abuse is not known or suspected, then only professional
awareness and a high degree of suspicion will identify the cause of the
injury.
that soft-tissue injuries were present in 92% of children suspected of
being victims of child abuse (14). A child’s
age, the pattern and location of soft-tissue injury(s), the number of
injuries, and the age of the lesion(s) are all important to consider.
The classic soft-tissue lesions such as cigarette burns, bite marks, or
multiple linear ecchymoses in the shape of an electrical cord leave
little doubt that abuse occurred, but in McMahon’s report these were
uncommon. Therefore, these findings are quite specific, but not
sensitive. The examiner must be careful to identify subtle signs of
abuse, because the “classic” findings may be present in only some
abused children, typically in the more severe cases.
pain on movement of the injured extremity, swelling at the fracture
site, and deformity. Dos Santos et al. (22)
found that less swelling was present on presentation in children with
long bone fractures caused by abuse than similar fractures that
occurred because of accidents. The history and the reported time when
the injury occurred are often unreliable in cases of child abuse.
Frequently, delays in seeking care for these children allow resolution
of these acute signs and symptoms. The absence of the typical acute
findings of fractures in abused children is one of the reasons that
screening for fractures in suspected cases of abuse includes skeletal
surveys and bone scans (see the section in this chapter entitled “Other Imaging Studies”).
is suspicious and indicates possible abuse. Soft-tissue injuries of the
head and face are much more common in abused children and are rare in
the absence of abuse. Ecchymoses are common, but may not be of the
suspicious pattern (14). Soft-tissue injuries are less common after accidental injury, but do occur frequently in approximately 37% of cases (23).
Therefore, the mere presence of a soft-tissue injury does not clearly
imply that the injury was a result of abusive force. Location is
important, because toddlers commonly have bruises over the shins,
knees, elbows, and brow. They may have a few old cuts or scars around
the eyes or cheekbones because of normal collisions. However, bruising
of the buttocks, perineum, trunk, back of the legs, and especially the
head or neck suggests inflicted trauma.
signs of multiple fractures in various stages of healing, the same is
true for skin lesions. Wilson (24) has
suggested the following guidelines for estimating the age of a bruise
from its color: from 0 to 3 days after injury, a bruise usually is red,
blue, or purple; from 3 to 7 days, it is green or green-yellow; and
from 8 to 28 days, it is yellow or yellow-brown.
These lesions can be scalding injuries, cigarette burns, or burns
caused by flames. Burns are most common among children between birth
and 2 years of age (14). The pattern of
deliberate immersion burns often is symmetric, with sharp lines between
the burned and unburned skin. Accidental scald burns usually are
distributed asymmetrically (25).
be invaluable in cases of child abuse. It is best to obtain more than
one view, with different lighting. Many centers have protocols in place
for obtaining satisfactory and complete photographs.
classic article in 1946 reported the association between long-bone
fractures and subdural hematomas. Typically, one of two histories is
provided: (i) a fall from a short height or a similar minor, blunt
traumatic episode is described, or (ii) the baby is brought for medical
attention due to the development of symptoms including poor feeding,
irritability, vomiting, seizures, lethargy, breathing difficulties, and
unresponsiveness (26). The head is the most
vulnerable part of the body for accidental injury and child abuse
because of its relatively large size, the weak neck muscles, and the
less dense bone with open sutures in younger children. The type of
skull fracture is not specific for identifying cases of child abuse, as
similar fractures may occur in different settings (27).
due to child abuse. Essentially, all the injuries that are known to be
caused by blunt trauma can be seen in victims of child abuse. Death due
to child abuse can be caused by internal hemorrhage because of the
rupture of abdominal organs after punches or kicks. The death rate from
these injuries can be high and is attributable to both the severity of
the trauma and the delay in diagnosis. Delays can result from lack of
timely diagnosis in the emergency room or delays on the part of the
abuser in seeking medical attention for the child. Hematuria can be one
sign of blunt internal injury. It is often the recognition of other
signs of abuse, however, along with a high index of suspicion for
associated abdominal trauma, that is required to identify this
potentially life-threatening type of injury.
conjunctival hemorrhage and orbital swelling. Retinal hemorrhages in
infancy are almost invariably caused by shaking and are seen in shaken
baby syndrome (28).
ortho-paedists if all abusive fractures had a typical appearance.
Although there are some patterns of fractures that are distinctive,
many of the patterns are also seen in cases of accidental trauma (Table 34.2). There is some debate as to which patterns are most common. Loder and Bookout (29)
noted that suspicious fracture patterns include metaphyseal corner
fractures, lower extremity fractures in nonambulatory children,
bilateral acute fractures, rib fractures, spine fractures, and physeal
fractures in young children. Kleinman (13)
stated that the most likely fracture in an abused infant is a long bone
metaphyseal lesion, followed by rib, skull, and long bone shaft
fractures. Kleinman et al. subsequently reported on the challenges of
dating the characteristic metaphyseal fracture (30). Blakemore et al. (31)
reported that single, fresh, long bone diaphyseal fractures are most
common. It is likely that there is a sampling bias that explains some
of these discrepancies, but different standards for radiographic
technique and the frequency with which skeletal surveys, follow-up
skeletal surveys, and bone scans are done may also lead to variations
in the reported rates (13).
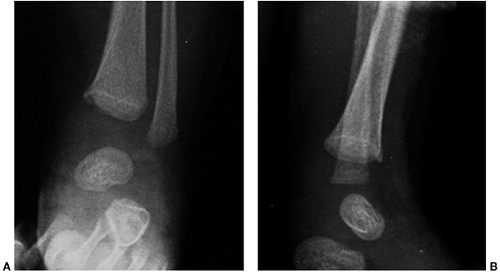
being inflicted by abusive trauma. Metaphyseal “bucket-handle” or
“corner” fractures often form the basis for the diagnosis of abuse (Fig. 34.1) and are considered pathognomonic for abusive trauma. They have highly distinctive radiographic characteristics (32)
that result from the isolation of a mineralized disc (or a part
thereof) that can be seen radiographically. Depending on its size and
the orientation and angle of the radiograph, one will see a
bucket-handle lesion, corner fracture, or metaphyseal lucency. The
metaphyseal lesion may be difficult to identify on plain radiographs.
High-detail imaging may be needed. Kleinman (13) prefers the term classic metaphyseal lesion (CML) to describe this type of injury because it represents a radiologic alteration that most
closely satisfies the need for an objective finding that “regardless of
history in an otherwise normal patient, can be viewed as a highly
specific inflicted injury.” He states that it is rarely seen as an
isolated finding in a healthy infant for whom a plausible accidental
event is available to explain the injury, and it is invariably due to
severe indirect forces. Most injuries due to child abuse “occur by
indirect forces which develop as the child is grabbed by an extremity,
shaken, slammed, or hurled into a solid object” (13).
They occur because of avulsive forces applied to the periosteal
attachment to the surface of the metaphysis. The periosteum serves as
the anchor for the epiphyseal cartilage to the metaphysis. Failure of
the bone in this area results in a corner fracture. The bucket-handle
fracture results from the same type of indirect force, but represents a
separation of a crescentic fragment from the zone of provisional
calcification that is tipped into an oblique plane (33).
|
TABLE 34.2 SPECIFICITY OF RADIOLOGIC FINDINGS
|
||
|---|---|---|
|
 |
|
Figure 34.1 Classic metaphyseal lesion of the distal tibia in a 2-week-old infant. A: Anteroposterior ankle. (B:) Lateral ankle. This finding is pathognomonic for child abuse.
|
be difficult to diagnose due to the various sutures, synchondroses, and
fissures that may be present throughout the development of a child.
Diagnosing these variants as a fracture is a common pitfall. Fractures
appear as radiolucent, sharply etched lines that may or may not branch
but finally taper and become indistinct. Sutures, on the other hand,
have a serpiginous appearance, symmetry, sclerotic edges, and typical
anatomic positions (34). Vascular markings are
more linear, have a near constant anatomic branching pattern, and
involve only the inner table. Other radiographic views or computed
tomography (CT) scan of the head can assist in cases that are
confusing. As mentioned previously, the type of skull fracture is not
specific for identifying child abuse. Similar fractures can occur in
different settings (27).
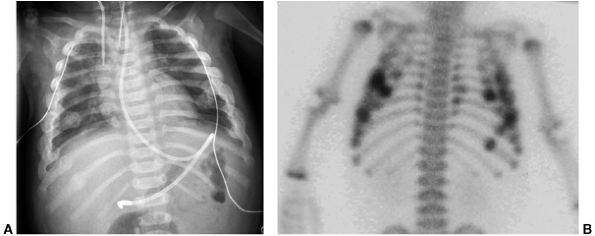
multiple rib fractures in children younger than 2 years) are highly
suggestive of intentional injury (Figs. 34.2 and 34.3).
The amount of force required to inflict them makes these injuries very
unlikely to be accidental. Rib fractures (especially posterior) may be
difficult to detect, but are not uncommon in children who are abused.
In a study of 62 children younger than 3 years with rib fractures (316
collectively), the finding of a rib fracture had a positive predictive
value of 95% for the diagnosis of abuse. The positive predictive value
rose to 100% after the exclusion of children with a defined history of
accident or disease (35).
 |
|
Figure 34.2
Acute skull fracture in a 5-month-old abused child. This fracture could be consistent with accidental injury if there were a documented history of significant trauma (a fall or auto accident). |
 |
|
Figure 34.3 Multiple healing rib fractures seen on chest x-ray film (CXR) (A) and on bone scan (B) in the same child as in Figure 34.2. The findings of multiple healing rib fractures (including posterior) and the acute skull fracture (Fig. 34.2) clearly indicate child abuse.
|
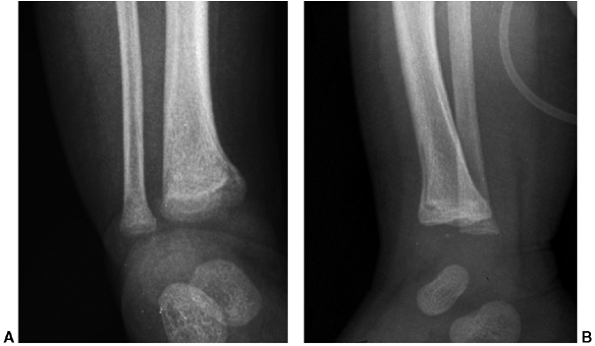
radiologist arises when the radiographic appearance of a fracture
resulting from abuse is not characteristic. Many of the fracture
patterns caused by abuse can also be seen after accidental trauma (Fig. 34.4).
In this situation, making the correct diagnosis is more difficult. In
such cases, age is one of the most important factors in differentiating
accidental from abusive trauma (31,36).
Some fractures that would not raise suspicion in ambulatory children
(because they are common and accidental) do not occur in infants unless
excessive force is applied and therefore are highly suspicious for
abuse in this age-group. For example, a spiral fracture of
the humerus in a young child is particularly indicative for abuse. Strait et al. (37)
reported that abuse was rare (1 of 99 cases) in children older than 15
months presenting with humeral fractures, but these fractures in 9 of
25 children younger than 15 months were diagnosed as having been caused
by abuse.
 |
|
Figure 34.4 Metaphyseal fracture of distal femur in a 13-month-old child. A: Anteroposterior view. B:
Lateral view. Was this fracture caused by abuse, or was it accidental? This fracture pattern could be seen in either situation. If the child were 4 months old, the fracture would be very suspicious for abuse. At 13 months of age, and if the child is ambulatory, it could be accidental. |
tibia or femur are common accidental injuries in toddlers, but are
suspicious if the child is preambulatory (31).
There is no diaphyseal fracture pattern that is specific for abuse.
Twisting injury to an extremity causes spiral fractures. In the
ambulatory child, the twists associated with falls while walking,
running, climbing, or falling down stairs are sufficient to cause
fractures (38). It is impossible for a
preambulatory child, however, to sustain this level of trauma unless it
is applied to him/her directly. Transverse or oblique long bone
fractures, on the other hand, are more common with abusive injury than
are spiral fractures. The peak incidence of pediatric femur fractures
is between 2 and 3 years of age (39). Femur fractures can result from low-energy falls and are two to three times more common in boys than in girls (40). King et al. (41)
found that approximately half of the 189 abused children in their
retrospective study had a single fracture and that a transverse
fracture was the most common type (as was the case for the child
illustrated in Fig. 34.4).
vast majority (13 of 14) of nonaccidental femur fractures occurred in
children younger than 1 year. Comparing them with 33 femoral fractures
known to be caused by accident, the authors concluded that there is no
specific radiographic site or fracture pattern that allows
differentiation between accidental and nonaccidental femoral fractures.
Blakemore et al. (31) also felt that age is the
most important factor in diagnosing abuse, because isolated femur
fractures are commonly seen in children who are 1 to 5 years of age.
Some authors would suggest that the incidence of long-bone fractures
caused by abuse in ambulatory children is relatively low (31,36). Dalton et al. (43)
recommended that because 31% of 138 femoral fractures in children
younger than 3 years were due to abuse, and only 10% (one third of the
total abuse cases) were identified as abuse at admission, a high index
of suspicion must be maintained even in the ambulatory child. They
recommended that although the “cause of isolated shaft fractures in
young children is low, the clinician should still have a high degree of
vigilance and have the circumstance investigated when the history and
physical findings are disturbing.” Only 18% of 34 humerus shaft
fractures in children younger than 3 years were classified as probably
caused by abuse in the review by Shaw et al. (44).
The history and physical findings (not the fracture pattern itself)
were critical in establishing cause. Neither age nor fracture pattern
is pathognomonic of abuse, so suspicion should remain high.
had skeletal surveys. In addition, for any fracture to be categorized
as abuse, its cause had to be confirmed at a legal hearing. Therefore,
interpretation of the scope of the results of this study seems to be
limited, because inclusion in the category of abuse was quite
restricted (some abused children may have been placed in the accidental
injury group) and screening for fractures was not highly sensitive
(some fractures may have been missed). Maintaining a high degree of
suspicion may even uncover abuse when an isolated long bone fracture in
an infant caused by a legitimate injury mechanism is investigated
further (45). In the review by Strait et al. (37), 18.5% of 124 humerus fractures were indeterminate in children younger than 15 months.
that isolated fractures of the femur are analogous to the toddler’s
fracture of the tibia. Like other authors, they concluded that the
ability to walk was the strongest predictor of abuse. Ten (42%) of 24
children
not old enough to walk had been abused, whereas only 3 of 115 toddlers
had been. Although child protective services were frequently consulted,
the authors felt that it may have been unnecessary in 42% to 63% of
cases. They felt that unless other evidence of abuse such as an
inconsistent history, bruises, or other fractures was present, abuse
was very unlikely in the child old enough to walk.
but occur in the minority of abused children. Only 17% of the 904
abused children in the report of Merten et al. (46) had fractures. McMahon et al. (14)
in their review of 371 abused children found that most did not show the
classic signs of child abuse that we, as orthopaedists, expect to see.
Although only 9% had fractures identifiable on x-ray film, 92% had
soft-tissue injuries (ecchymosis was most common). The metaphyseal
lesion was not seen, and long bone fractures tended to be diaphyseal.
Although the McMahon article is very enlightening regarding abused
children who do not present with the classic findings, only 10% of the
children included in the report actually had radiographs taken! One can
only speculate as to the number and type of fractures that may have
been found if full skeletal surveys had been performed. The rate of
fractures reported by different authors depends on the source of the
information (social service agencies vs. orthopaedists offices vs.
emergency rooms, etc.) and the methods employed to identify fractures.
Because neglect is the most common form of abuse, and neglected
children do not commonly have fractures, it is likely that few victims
of abuse have fractures. However, orthopaedists are typically not
involved in many cases of neglect; therefore, from our vantage point,
it can be presumed that a substantial percentage of the young patients
we see with fractures have been abused. Approximately 30% of fractures
in children younger than 3 years (27) and 56% of fractures in children younger than 1 year have been found to be nonaccidental (16).
Although corner fractures, fractures at different stages of healing,
and injuries at multiple sites may be more specific, the clinician must
remember that all types of fractures at all locations can be seen in
children who have been abused (Table 34.2).
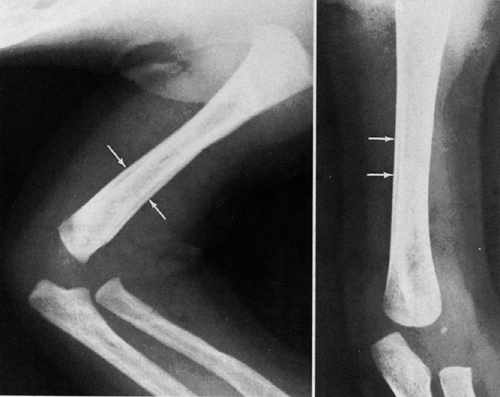
stages of healing can be important in identifying abuse, it is
extremely important to be able to identify the ages of fractures based
on their radiographic appearance (47,48) (Table 34.3).
Soft-tissue swelling may be the only radiographic finding for recent
fractures. The orthopaedist is accustomed to identifying this finding
on x-ray films of acute fractures. Because care for abused children is
frequently delayed, this finding may be absent on the initial
radiographs. The earliest sign of bone healing is subperiosteal new
bone formation (SPNBF). SPNBF will not be seen until at least 5 days
after injury. This finding has low specificity as there are multiple
etiologies (see “Differential Diagnosis”
section), and it must be distinguished from the many other conditions
that can lead to this radiographic appearance. Indistinctness of the
fracture line is the next finding that helps to date the fracture
between approximately 10 days to 2 weeks (Fig. 34.5). Soft callous formation and
indistinctness of the fracture line date fractures to similar
ages—between 2 and 3 weeks. Numerous factors (age of the child,
mechanism of injury, fracture stability, and fracture location)
determine whether either or both are seen. The subsequent stages of
hard callous formation and remodeling are even more variable, but are
typically distinct from the early findings. It would likely be
impossible to distinguish a fracture that is 4 weeks old from one that
is 6 weeks old. Subsequent growth that separates a physeal fracture
from the physis (Salter-Harris growth arrest line) helps identify older
fractures (Fig. 34.6).
One should remember that not all fractures heal at the same rate. For
example, an ulnar diaphyseal fracture will heal more slowly than a
coexisting distal radial metaphyseal fracture (a common combination
seen when both bones of the forearm fracture). During healing they can
have the radiographic appearance of fractures of different ages. One
should be aware of such possibilities.
|
TABLE 34.3 TIMETABLE OF RADIOLOGIC CHANGES IN CHILDREN’S FRACTURESa
|
||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||
 |
|
Figure 34.5
Subperiosteal new bone formation (SPNBF). Lateral x-ray film of the humerus showing a healing fracture and typical SPNBF in an 11-week-old infant. Although this fracture pattern itself is not very troubling, the finding of a long bone fracture in an infant is very suspicious for abusive trauma. |
 |
|
Figure 34.6 Healing classic metaphyseal lesion (CML). A: Antero-posterior view. B: Lateral view. This is the same patient who also had the humeral shaft fracture shown in Figure 34.5. This fracture pattern along with the findings in Figure 34.5 clearly indicates that these fractures were caused by abuse.
|
scans is that many fractures from abuse are not apparent on physical
examination. Accurate diagnosis of abusive injury can be reached in
most cases by careful appraisal of the social and family history,
combined with painstaking clinical radiographic and other imaging
evaluations.
It is necessary for two primary reasons. As mentioned, the typical
physical findings of fractures (pain with movement of the injured
extremity, swelling at the fracture site, and deformity) may be absent
in abused children (22). In addition,
identifying multiple fractures can be crucial to the diagnosis of child
abuse. The additional information may prove invaluable during a
subsequent investigation and prosecution. American Academy of
Pediatrics guidelines state that a skeletal survey should be mandatory
in all cases of suspected physical abuse in children younger than 2
years (49). In children older than 5 years,
skeletal survey and bone scan have little value as screening tools.
Injuries in children in the 2 to 5 year age-group should be handled
individually (Table 34.4).
vary from one source to another, but the American College of Radiology
has published standards for skeletal survey imaging in cases of
suspected abuse (50) (Table 34.5).
Additional views may be included in some hospitals. For example at one
of the local hospitals in the author’s community, lateral views of both
arms and lower extremities, five views of the skull (anteroposterior,
both laterals, Towne, Waters), and cone down views of tibia and fibula,
with internal rotation if the child is ambulatory, are included in the
routine skeletal survey to assess child abuse. “Babygrams” do not
provide sufficient radiographic detail. They are inadequate for
screening for abuse and should not be accepted.
Quality
and adequacy of the skeletal survey images must be assured by a
radiologist. With the trend to convert to digital radiographic
techniques, digital image quality must be comparable to high-detail
film screen radiography before it replaces the standard techniques.
|
TABLE 34.5 STANDARD SKELETAL SURVEY
|
||
|---|---|---|
|
skeletal survey versus bone scan in screening for child abuse. Bone
scans are particularly sensitive for detecting rib fractures, subtle
shaft fractures, and early periosteal elevation (51).
Bone scans can help identify unsuspected sites of skeletal injury or
occult or subtle lesions seen on plain radiographs. The bone scan can
be negative acutely. There is also concern that the bone scan may miss
subtle spine fractures and CMLs due to the typical increased level of
activity seen at the growth plate on bone scans. Both fulfill the need
for screening children who are too young to localize pain for the
examiner. Bone scans lack specificity, are more expensive, and expose
the child to a radionuclide. Any lesions identified on the bone scan
must be followed up with radiographs. Conventional radiographs have the
advantages that they are easy to perform, can be interpreted in
minutes, can differentiate from other pathologies such as tumor and
infection, can show different stages of healing, and are less
expensive. Both modalities are felt to be sensitive. The specificity is
high for skeletal survey and low for bone scintigraphy.
found that radiographs were positive in 105 cases and false-negative in
32. Bone scans were positive in 120 and false-negative in 2. The
authors concluded that scintigraphy should be the screening procedure
of choice in cases of suspected abuse. Mandelstam et al. (53)
found that 20% of children with inflicted injuries were identified on
bone scan only. Like other authors, they also found that the CML can be
missed on bone scan (only 35% were identified). The authors concluded
that neither a bone scan nor a skeletal survey is ideal, but they
provide complementary information to one another. Therefore, they
recommended that both studies be done in suspected cases of physical
abuse. Flynn et al. (40) suggest a bone scan
when abuse is suspected and the skeletal survey is negative or
equivocal. Follow-up skeletal survey 2 weeks later has been shown to
increase the diagnostic yield and should be considered when abuse is
strongly suspected, but not confirmed initially (54).
The American Academy of Pediatrics Section on Radiology states that if
the child is in a safe environment, a follow-up skeletal survey in 2
weeks could be considered instead of initial bone scan. Bone scan does
not obviate the need for a second skeletal survey (49).
adequate with plain radiographs, particularly in cases of nonossified
epiphyses. The proximal femur and the elbow are common examples. Repeat
close-up views in proper alignment that are centered over the physis in
question may be sufficient when coupled with a good knowledge of normal
anatomy and consideration of comparison views to the contralateral
side. If not, ultrasonography, magnetic resonance imaging (MRI), or
arthrography can be considered for further imaging of these challenging
anatomical areas.
and children with suspected intracranial injury. These studies are not
considered standard components of the evaluation in all suspected abuse
cases. They should be considered for a child younger than 1 year who
presents with a history of serious trauma, brutality, or shaking, or a
child who presents with serious bruising or trauma, abdominal trauma,
or a positive skeletal survey (34). CT scan of
the head may not clearly document subdural bleeding, but it does
provide diagnostic and clinical information needed for immediate
management of the child. CT scan is better than MRI for evaluation of
acute hemorrhage and can detect cranial and facial fractures. Delayed
MRI (5 to 7 days) is recommended because acute hemorrhage may not be
detected initially. It offers very high sensitivity and specificity in
subacute and chronic situations. In a few days, hemorrhagic areas
become bright on T2-weighted images as fresh blood turns to
methemoglobin.
spinal injury resulting in paralysis will have negative radiographs
[spinal cord injury without radiographic abnormality (SCIWORA)]. MRI of
the spine is the imaging modality of choice. Thoracoabdominal trauma
can be evaluated with a CT scan if the child is stable. Evaluation and
management are similar to those in cases of accidental trauma.
presents with any signs of bruising, so coagulation studies must be
obtained.
ophthalmology consultation must be obtained. Shaking is a key element
in creating hemorrhagic retinopathy (28).
Certain patterns of hemorrhagic retinopathy are particularly indicative
of shaking, with a very narrow differential diagnosis.
osteogenesis imperfecta (OI), and several less common skeletal diseases
must be considered in the differential diagnosis of fractures caused by
abuse. The skeletal diseases in the differential for child abuse are
listed in Table 34.6. They receive little or
no mention in this text as they are listed in the table, and more
information is available in the excellent work by Brill et al. (55).
The more common challenge that the orthopaedist will face is
distinguishing abusive injuries from accidental and obstetric trauma,
normal variants, and OI.
that extends from the cortical surface to the endosteal margin. They
result from vessels that course through dense cortical bone. Normal
metaphyseal variants, including beaking, step-offs, and spurs, must be
distinguished from the CML (56). The absence of
a fracture line or its presence bilaterally can help differentiate
these from abuse. The typical finding of metaphyseal beaking of the
proximal tibia in toddlers (Fig. 34.7) could be mistaken for the CML of child abuse, especially during healing (Fig. 34.6B).
Physio-logic SPNBF is a recognized normal variant in the long bones of
infants between 1 and 6 months of age and most commonly involves the
femur, humerus, and tibia (Fig. 34.8). It is not uncommon and has been reported to be present 30% to 50% of the time (57).
It is radiographically indistinguishable from other conditions that
cause SPNBF, such as diaphyseal fractures, osteomyelitis, and
congenital syphilis.
radiographic appearance of long-bone fracture patterns, it should be
clear that differentiating accidental from abusive trauma represents
the most common challenge for the orthopaedist. Falling down the stairs
or from a height can result in fracture patterns that are similar to
fractures caused by abuse. Parents and caretakers may not be
aware
of the risks associated with a child’s attainment of new developmental
milestones (climbing up on objects, climbing down stairs, falling
down). As mentioned earlier, age and attainment of toddlerhood is a
primary consideration when trying to determine whether a fracture was
accidental or not (31,36,37,38,40,42,43,44). The amount of soft-tissue swelling may be a helpful sign. Dos Santos et al. (22)
found that less swelling was present initially in long bone fractures
caused by abuse than similar fractures that were accidental. The
authors concluded that the history and the time of the injury may not
be reliable in suspected cases of abuse.
|
TABLE 34.6 DIFFERENTIAL DIAGNOSIS OF SKELETAL DISEASES
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
|
Figure 34.7 Normal metaphyseal beaking of the proximal tibia in a toddler. (From Keats TE, Atlas of normal roentgen variants that may simulate disease 6th ed. St. Louis: Mosby Year Book, 1996:564.)
|
and multiple rib fractures. Even this constellation of findings is not
specific for abuse, as injuries due to motor vehicle accidents can
result in the same findings (27).
classic differential diagnostic challenges that the orthopaedist and
radiologist can face. Claiming that their child has OI can be a common
defense used by an abusive family in legal defenses. The classification
of Sillence (58,59) is
well known. For the purposes of this discussion, only a brief summary
will be offered. The reader is referred for further details of this
condition to Chapter 8. OI is a rare disorder
of type I collagen (incidence of approximately 1 in 25,000 live
births). OI type I is mild and is typically distinguished by distinctly
blue sclerae (however, some children with OI type I do not have blue
sclerae). OI type II is lethal in the perinatal period. OI type III is
severe and causes progressive deformity. OI type IV is typically a
milder form, with normal sclerae. Of the two subtypes, type IVA has no
dentinogenesis imperfecta. OI is either dominantly inherited or occurs
sporadically as a consequence of a new mutation. However, mosaicism has
been reported and could explain the occurrence of more than one
affected child to apparently “unaffected” parents. The only types that
represent a practical differential challenge of abuse are the unusual
type I OI without blue sclerae and type IVA OI.
 |
|
Figure 34.8 Normal subperiosteal new bone formation (SPNBF) in an infant with no history of trauma or fracture. (From Keats TE, Atlas of normal roentgen variants that may simulate disease 6th ed. St. Louis: Mosby Year Book, 1996:422.)
|
instrumental in confirming cases of OI when abuse is otherwise
considered to be the cause (60). If testing is
indicated, a skin biopsy for cultured dermal fibroblasts can detect
approximately 85% of OI cases. Collagen analysis to exclude type IV OI
is recommended only in rare cases in
which the diagnosis of child abuse remains in doubt after thorough
evaluation by clinicians in consultation with experienced radiologists (61). When faced with making this distinction, clinicians can rely on several helpful points (40).
Child abuse is much more common than OI (3 in 100 vs. 1 in 25,000).
Typically, a family history is present in OI. Common abusive injuries
(skull and rib fractures, subdural hematomas, retinal hemorrhages, and
metaphyseal corner fractures) are not associated with OI. Although
normal infants younger than 4 months may have blue sclerae, they do not
have the dental findings, osteopenia, or wormian bones on skull
radiographs seen in children with OI. If there is a reliable reporter
and a history of multiple fractures with minimal trauma, OI is likely.
Smith offered these guidelines (62):
-
In suspicious circumstances, suspect child abuse.
-
Consider collagen testing if
-
bruises or burns are not seen
-
the reported injury seems too minor to have caused a fracture
-
fractures occur in different environments
-
placed in protective custody. In such an environment, a child with OI
type IVA will still fracture. The fractures will likely cease to occur
in the abused child. Children with OI can also be victims of abuse (63).
Collagen synthesis testing is rarely required to rule out OI, as the
diagnosis would have already been strongly suspected in most cases (64).
measurements to differentiate between abuse and OI is unknown, as
values for BMD are not available for either typically developing
children younger than 2 years or for children with OI.
techniques. Clavicular fractures are most common and occur not only
with difficult deliveries but also with uneventful deliveries of large
babies. They can be associated with brachial plexus palsies. Some are
only noted incidentally on subsequent x-ray films, so they may be more
common than reported in the literature. Humerus fractures occur with
breech deliveries and have become much less common with the increased
utilization of cesarean section. Sonography can help with
identification of proximal humeral physeal fractures. Absence of SPNBF
at 11 days of age is compelling evidence against a birth injury (65).
Subdural hematoma can be caused by obstetric trauma. Evaluation of
obstetric injuries has provided useful insight into the biomechanics
and imaging characteristics of inflicted skeletal injuries.
following their review of 39 children younger than 1 year with
fractures. They felt that these infants had a “self-limiting variant of
OI” due to a transient defect in collagen formation. Since its
introduction in 1990, this condition has stirred intense controversy. A
number of medical authors and legal proceedings have challenged the
findings of this paper. It has been pointed out that none of the
authors was a radiologist, thereby bringing into question the accuracy
of their findings. Most of the radiographic features of this condition
are the same as those seen in child abuse (68). Paterson et al. (66,67)
reported that some fractures developed after hospitalization. Although
they concluded that this was consistent with the transient osteopenic
state, it is well documented that some abusive fractures occurring
before hospitalization become evident only on follow-up studies. Ablin
and Sane (61) stated that “until clinical
research scientifically establishes the existence of temporary brittle
bone disease, it should remain strictly a hypothetical entity and not
an acceptable medical diagnosis,” and Albin states, it “remains a
medical hypothesis lacking the support of sound scientific data” (69).
Legal proceedings involving testimony by Paterson have cast doubts on
his findings. The possibility of temporary brittle bone disease may
“compromise or obstruct protection of a child” and that by being aware
of and referring others to relevant law reports, pediatricians can help
keep the issues in perspective (70).
indicated that there were approximately 20 cases reported in the world
literature, and fractures as late sequelae of copper deficiency have
never been reported. British courts have sought to define what is
acceptable opinion versus untried hypothesis. “Untested and
unacceptable views should not be put forward—advice American courts
should take note of in this age of ôpseudoscience’ in the courtroom” (70).
injury caused by abuse is the same as traumatic fractures and
soft-tissue injuries due to other causes. The pathoanatomy of the CML
is pathognomonic for abuse. It has been described in detail by Kleinman
et al. (32) in a classic article that received
the Society for Pediatric Radiology John Caffey Award. The authors
studied four children who died because of their injuries. The
histopathology of their lesions was correlated with fracture patterns
on pre- and postmortem radiographs and anatomy from autopsy specimens.
The CML is due to a series of subepiphyseal planar fractures through
the most immature part of the metaphyseal bone. The separation occurs
in the region of transition from the zone of calcified cartilage to the
primary spongiosa. If the injury extends to the periphery of the bone,
it undermines and isolates a peripheral fragment of bone encompassing
the periosteal collar. The periosteum serves as the anchor for the
epiphyseal cartilage to the metaphysis. The CML occurs because of
avulsive
forces
applied to the periosteal attachment to the surface of the metaphysis.
The result is the isolation of a mineralized disc (or a part thereof)
that can be seen radiographically.
documents thickening of the zone of hypertrophic cartilage, with some
cases showing extension of the growth plate into the metaphysis.
Because estimating the age of CMLs is difficult, the authors suggested
that the extent of healing may be helpful in dating these fractures.
abuse and death. It is accepted and well known that a high percentage
of children will be reinjured and some will die if they are returned to
the abusive environment. Therefore, abuse must be diagnosed, and either
some intervention or removal of the child from the abusive environment
must be enforced.
trickiest aspects of managing this condition. Kleinman writes that, as
with other clinical situations, “the most effective approach to
diagnosis is one based on thoughtful and measured acquisition of data
that is carefully analyzed in the light of one’s knowledge and
experience” (13). Managing fractures due to
abuse is typically not difficult or challenging. Identifying all
fractures, making the diagnosis, and instituting the process to protect
the child from reinjury are the challenging aspects of child abuse.
easy. To feel angry is human. As professionals, controlling our
emotional response is essential in carrying out our responsibility to
care for and protect the child. Particularly in cases that are less
clear, the physician should try to form a relationship with the family
which will foster their participation in the subsequent diagnostic and
therapeutic workup. One must also explain the case report and aspects
of the protective service process to the family.
advise that all children younger than 1 year with a fracture be
admitted to the hospital and referred to a pediatrician for child
protection assessment. Management should be multidisciplinary, with the
key being recognition because of the risk to the abused child (11).
Such teams and resources are available in most, if not all,
institutions. The importance of diagnosing abuse and intervening on
behalf of the vulnerable child cannot be overemphasized.
the potential disincentives for a practitioner to initiate an
investigation or to make the diagnosis. Advance preparation and
knowledge about the process may help minimize this potential
disincentive. Physicians have certain rights that they should expect to
be able to exercise when they testify (72).
-
The right not to know
-
The right to understand the question
-
The right to ask for a question to be repeated
-
The right not to be confused
-
The right to refresh one’s memory
-
The right to ask if a factual statement or an opinion is being requested.
-
Factual information about the child’s fractures
-
Possible mechanism of injury
-
Amount of force/energy needed to cause the fractures
-
Dating fractures
-
Judge information based on reasonable medical certainty
-
Potential for future fractures
chapter on child abuse in the previous edition of this book has an
extensive section on medicolegal issues for the orthopaedist. It is
excellent and recommended for the reader interested in more
information. Further insights to diffuse these concerns are addressed
in the following text.
many fractures. We should ask ourselves if we recognize abusive
fractures when we see them. The reported maltreatment rate is 1% to
1.5% annually. Given the widely held belief that child abuse is
significantly underreported, this incidence is likely to be lower than
the actual rate of occurrence. Fractures are the second most common
presentation in child abuse. These statistics should cause us to pause
and wonder whether we recognize the etiology of abusive fractures often
enough. Some are obvious; diagnosing the rest is where the challenge
lies.
is essential for the orthopaedist to consider two key issues. The first
is that we must have a high index of suspicion.
Without it, we will not recognize abuse often enough. Many of us also
care for children with disabilities, and must remember that they are
particularly vulnerable. Not only are they at increased risk of
physical injury; medical neglect in the form of lack of provision of
adequate nutrition by the caregiver is not uncommon. We should
recognize this when it is present, and ask our pediatrician colleagues
to assess and intervene.
insidiously erode our willingness to report suspicious fractures and
institute the process. The clinician may also feel psychosocial
pressure to not report cases that are of concern. We may want to avoid
putting a family through the embarrassment of filing a report and
completing an investigation. Methods to minimize these disincentives
are addressed later in this section.
becoming overzealous. One must remember that ambulatory status is a
very strong predictor of likely abuse. Child Protective Services may be
consulted unnecessarily in some cases (36).
Unless other evidence of abuse such as an inconsistent story, bruises,
or other fractures is present, abuse of the toddler (who might, for
example, have a toddler’s fracture of the tibia) is much less likely
than abuse of the infant. Of course, there are enthusiasts on both
sides. Physicians and other professionals practicing in this field may
seek to simplify matters, taking extreme positions that reflect either
an overly passionate approach to diagnosing abuse or an unwillingness
to consider abuse in all but the most flagrant cases. Financial rewards
for legal counsel may increase the zealousness with which cases are
pursued.
effective and safe care. The following resources are those that I have
found to be particularly useful. Paul Kleinman’s multiauthored book Diagnostic Imaging of Child Abuse 2nd ed. (13)
is an essential reference for all centers. Dr. Kleinman is a
radiologist with a worldwide reputation for his expertise in the field
of child abuse. During his career, he has been active in research and
education.
auspices of the Pediatric Orthopaedic Society of North America Trauma
Committee (Chairman: Peter Pizzutillo, M.D.) in 2002 (40).
It is a very useful, quick-glance guide that is also handy for
residents’ education. It is available by emailing John M. Flynn, M.D.
at the Children’s Hospital of Philadelphia-Flynnj@email.CHOP.edu.
contains reviews of recent peer-reviewed articles on the diagnosis,
prevention, and treatment of child abuse and neglect. Medical, legal,
mental health, and social work professionals known for their expertise
and experience summarize the articles which are chosen from more than
1000 medical journals. The reviewers offer opinions about the validity
and significance of the research findings.
|
TABLE 34.7 AVOIDING PITFALLS
|
||
|---|---|---|
|
“child protective services is unlikely to do anything” is a self-fulfilling prophecy and should not happen (72).
Consulting the physicians and staff of referral centers that specialize
in the management of child maltreatment removes at least some of the
disincentive to reporting. Many physicians are uncomfortable in the
courtroom. Much of the legal work can be handled by expert physicians
who work in referral centers. In this case, the orthopaedist may not be
needed as often in court. If disincentives are removed, we can be
appropriately suspicious. The radiologist and members of the referral
center staff can be more objective and more detached from psychological
pressures to not report. These centers are typically referred to as
children’s advocacy centers [the local center in my community is the
Midwest Children’s Resource Center (MCRC) in St. Paul, Minnesota,
United States]. They typically utilize the multidisciplinary team (MDT)
approach for the treatment or prevention of child abuse and neglect in
their respective communities. Many provide 24-hour coordination of
suspected child abuse and neglect (SCAN) cases, integrating hospital
services with outside community agencies. They can formulate and
provide many of the necessary protocols mentioned in the preceding
text. They partner pediatric subspecialty consultants (hospital MDTs)
with providers in the community (community MDTs). A hospital MDT
includes physicians, nurses, social workers, and risk managers. A
community MDT includes law enforcement, child protection investigators,
and county attorneys. Child abuse consultants provide expertise in
diagnosis of inflicted trauma. The medical care team is therefore more
free to first and foremost provide medical care.
consultation for case reviews, telephone consultation, and expert
testimony. They are also active in education for both health care and
community providers, often supporting combined, multidisciplinary
interaction and education. They typically offer both medical and
psychological assessments. The National Association of Children’s
Hospitals and Related Institutions (NACHRI) is considering designating
qualifying programs as centers of excellence. They provide training
supported by a national grant from the Department of Justice. The
American Academy of Pediatrics Section on Child Abuse and Neglect
(SOCAN) maintains a listing of these centers across the United States
and Canada. This can be accessed at http://www.aap.org/sections/scan/ and the link “State Child Abuse Programs.” Numerous policy statements are available on this website as well.
enforcement to the teams at referral centers. Those in law enforcement
add expertise in acquisition of information and the ability to evaluate
and photograph the scene of the injury. They can provide an evaluation
and report on conditions in the home, the number of calls for domestic
disputes that have been made, and whether there is any prior history of
intervention. The initial report to the appropriate police department
is oral and is followed by a written report.
was organized to support individuals and organizations working to
protect children from abuse and neglect worldwide. Founded in 1977, it
is the only multidisciplinary international organization that brings
together a worldwide cross section of committed professionals to work
toward the prevention and treatment of child abuse, neglect, and
exploitation globally. ISPCAN’s mission is “to prevent cruelty to
children in every nation, in every form: physical abuse, sexual abuse,
neglect, street children, child fatalities, child prostitution,
children of war, emotional abuse, and child labor. ISPCAN is committed
to increasing public awareness of all forms of violence against
children, developing activities to prevent such violence, and promoting
the rights of children in all regions of the world.” The organization’s
journal, Child Abuse and Neglect: The International Journal is published by Elsevier Science (http://www.elsevier.com).
ISPCAN partners with numerous national organizations such as American
Professional Society on the Abuse of Children (APSAC) in the United
States.
consultation only, or one may consider referring a child to a tertiary
referral center for assessment and management. These referrals may be
helpful because such centers have the equipment and expertise to
perform the necessary studies and interpret them appropriately.
Although it is impractical to restrict evaluations to specialized
centers, the scope of services they offer may be helpful to the
orthopaedist. Alternatively, developing connections to access the
consultative services of a pediatric radiologist with expertise in the
field could be valuable to the orthopaedist without ready access to a
specialized center in his or her local area.
Academy of Pediatrics Committee on Child Abuse and Neglect and
Committee on Children with Disabilities. Assessment of maltreatment of
children with disabilities. Pediatrics 2001; 108(2):508–512.
R, Blum KL, Johnson C. Fractures in young children: are physicians in
the emergency department and orthopedic clinics adequately screening
for possible abuse? Pediatr Emerg Care 2003;19(3):148–153.
DM, Barbor P, Hull D. Unusual injury? Recent injury in normal children
and children with suspected non-accidental injury. Br Med J 1982;285:1399–1401.
AC, Partington MD. Overview and clinical presentation of inflicted head
injury in infants. In: Adelson PD, Partington MD, guest eds. Neurosurgery clinics of North America. Philadelphia, PA: WB Saunders, 2002;13(2):149–154.
PK, Marks SC, Spevak MR, et al. Extension of growth-plate cartilage
into the metaphysis: a sign of healing fracture in abused infants. AJR Am J Roentgenol 1991;156:775–779.
LC, Loder RT, Hensinger RN. Role of intentional abuse in children 1 to
5 years old with isolated femoral shaft fractures. J Pediatr Orthop 1996;16(5):585–588.
KA, Char E, Bensard DD, et al. The positive predictive value of rib
fractures as an indicator of nonaccidental trauma in children. J Trauma 2003;54:1107–1110.
RT, Siegel RM, Shapiro RA. Humeral fractures without obvious etiologies
in children less than 3 years of age. When is it abuse? Pediatrics 1995;96:667–671.
SA, Rosenfield NS, Leventhal JM, et al. Long-bone fractures in young
children: distinguishing accidental injuries from child abuse. Pediatrics 1991;88(3):471–476.
the POSNA Trauma Committee, 2002 Chairman: Peter Pizzutillo, MD, John
M. Flynn, MD at the Children’s Hospital of Philadelphia, Flynnj@email.CHOP.edu.
SA, Cook D, Fitzgerald M, et al. Complementary use of radiological
skeletal survey and bone scintigraphy in detection of bony injuries in
suspected child abuse. Arch Dis Child 2003;88:387–389.
RD, Pepin M, Byers PH. Studies of collagen synthesis and structure in
the differentiation of child abuse from osteogenesis imperfecta. J Pediatr 1996;128:542–547.
CR, Burns J, McAllion SJ. Osteogenesis imperfecta: The distinction from
child abuse and the recognition of a variant form. Am J Med Genet 1993;45:187–192.
PA, Scotland TR, Myerscough EJ. Fractures in children younger than age
1 year: importance of collaboration with child protection services. J Pediatr Orthop 2002;22(6):740–744.
