SUPRACONDYLAR AND ARTICULAR FRACTURES OF THE DISTAL FEMUR
II – FRACTURES, DISLOCATIONS, NONUNIONS, AND MALUNIONS > Pelvis and
Femur > CHAPTER 21 – SUPRACONDYLAR AND ARTICULAR FRACTURES OF THE
DISTAL FEMUR
the femur) in the adult account for only 7% of all femoral fractures,
but because of our modern lifestyles and high-velocity means of
transportation, these injuries are being seen with increasing
frequency. Fractures of the distal femur are often complex injuries
that present the surgeon with numerous potential complications.
Although there has been an increasing trend toward internal fixation of
fractures of the distal femur, the management of these fractures
remains controversial (4,9,16,26,31,38,40,41,46,51,52,54,55,58,70).
of multiple trauma due to high-velocity, high-energy incidents, such as
motor vehicle accidents or falls from a height. In particular,
motorcycle accidents are a prime cause for these fractures in the 17-
to 30-year-old patient. The elderly patient may present with a fracture
resulting from trivial trauma, such as falling on the flexed knee. Both
groups benefit by early mobilization.
brace immobilization (10,11,42).
Complications associated with the closed management of this fracture
have led to the proposal of a number of alternative methods of internal
fixation. In 1966, Stewart (60) and, in 1967, Neer (45)
and their associates reported large series of distal femur fractures
treated by both open and closed methods. Most of the surgically treated
patients required prolonged supplemental immobilization, negating the
advantages of open reduction and internal fixation. This led both
groups to recommend closed management strongly, despite their findings
that this method results in significant problems—primarily varus and
valgus angulation, internal rotation deformity, and inadequate recovery
of knee motion.
femur fractures frequently gave unacceptably high rates of malunion,
nonunion, and infection, improved techniques of internal fixation have
yielded results far superior to those achieved with nonsurgical
management. Meticulous internal fixation has been shown to yield good
to excellent results in 60% to 80% of cases and allows immediate
mobilization of the patient and the extremity, minimizing the
cardiopulmonary and other multisystem sequelae of long-term immobility (50).
A number of excellent devices are now available that provide improved
techniques for fixation of these fractures. These include, but are not
limited to, the 95° angled blade plate, the 95° condylar screw, the
cloverleaf condylar plate, combined medial/lateral or lateral and
anterior double plates, the antegrade intramedullary (IM) nail, and the
retrograde supracondylar nail.
who have sustained multisystem trauma, usually characterized by
injuries of the head, chest, abdomen, and other parts of the skeletal
system. The immediate objective is to identify and treat
life-threatening problems and initiate protocols to achieve and
maintain cardiovascular and cardiopulmonary stability. Although these
fractures rarely are life-threatening, they do contribute to the
hemodynamic response to trauma and may involve neurovascular structures
to the extent that limb viability is jeopardized. Always include
careful clinical and radiographic assessment of the pelvis and
bilateral lower extremities in the initial trauma workup. Assessment of
the implications of these fractures and planning for surgical
intervention should be done during the early resuscitative period.
Ordinarily, internal fixation can be completed initially and certainly
by the third post-trauma day, depending on the extent of other
injuries. Look for local swelling, painful crepitus with motion, and
deformity of the thigh. Apply hand traction and be gentle when
realigning the deformity before splinting it. Carefully assess the soft
tissues. A small puncture wound over the distal thigh or suprapatellar
pouch area may represent an open fracture. Suspect neurovascular damage
if there is distal coolness, pallor, diminished pulses, or increased
fullness in the popliteal space. Immediate arteriography may be
indicated if evidence of circulatory impairment is present or
neurologic compromise is possibly due to a vascular lesion.
the entire limb and pelvis, if indicated. Identify ipsilateral as well
as contralateral fractures or dislocations of the pelvis, hip, knee,
and lower leg. These associated injuries are often missed in the
initial assessment.
comparing results of various treatments. Developing a workable
classification system for fractures of the distal femur is problematic
because the fractures have an infinite number of configurations and the
injury is always associated with other considerations such as injury of
the soft tissues that play an important role in determining the
approach to treatment and its outcome. I recommend using a combined
system that accommodates both the anatomic characteristics of the
fracture and its “personality.”
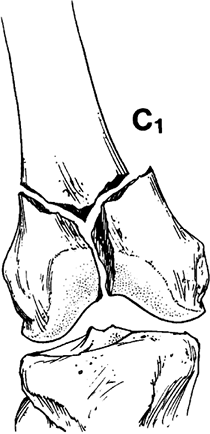
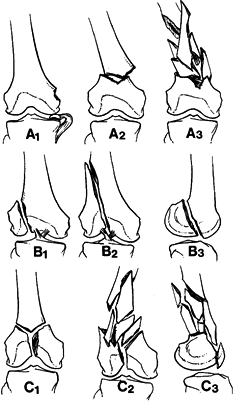
is excellent. A1, A2, and A3 are fractures proximal to the condyles
with the condyles intact. B1, B2, and B3 are variations of a single
condylar fracture. C1, C2, and C3 are the more complex multicondylar
fractures combined with associated supracondylar fractures (Fig. 21.1). Other factors that establish the fracture’s personality include
 |
|
Figure 21.1. Müller’s classification of fractures of the distal femur. (Redrawn from Müller ME, Allgower M, Schneider R, Willenegger H. Manual of Internal Fixation, 2nd ed. New York: Springer-Verlag, 1979, with permission.)
|
-
Degree of displacement.
-
Degree of comminution.
-
Extent and degree of soft-tissue damage (whether open or closed).
-
Associated neurovascular damage.
-
Degree of articular damage.
-
Bone quality (osteopenia).
-
Severity of multisystem injuries.
-
Other fractures.
traction and balanced suspension is almost never used today. This is
discussed in Chapter 10. In 1979, Mooney et al. (42) introduced the ambulatory cast-brace. In 1974, Mays and Neufeld (36)
introduced roller traction, which when combined early with a
cast-brace, allowed early mobilization of the patients and early
restoration of knee motion.
patient with severe, massive comminution or osteopenia, or both; the
rare, nondisplaced fracture; and nonintraarticular fractures in older
children or young adolescents.
shortening, angular and rotational deformities, restriction of joint
motion, incongruity of the articular surface, residual traumatic
arthritis, delayed unions and nonunions (infrequent), and the need for
prolonged hospitalization. Meticulous attention to detail is required
to achieve a satisfactory outcome.
distal femur are anatomic reduction and stable fixation. Numerous
studies support the use of internal fixation in these difficult
fractures (4,9,16,19,20,26,31,38,40,41,46,52,53,54,56,58,70).
Prerequisite to selection of the surgical method is adequate
institutional support, which includes appropriate instrumentation,
skilled and experienced operating room personnel, a knowledgeable
assistant surgeon, and experienced physical therapy support. A
knowledge of closed methods of treatment is essential and should always
be considered as the decision for operative management is weighed.
-
Extraarticular fractures in which acceptable reduction cannot be obtained or maintained.
-
Displaced intraarticular fractures.
Distal femoral fractures combined with ipsilateral (floating knee) or
contralateral fractures to begin early mobilization of the knee and to
facilitate control of the limb. Fix bilateral femoral fractures
internally to facilitate general care. -
Supracondylar femur fractures in patients with multiple system injuries.
-
Obesity. Extremely obese patients are
best managed by internal fixation because of the difficulty in treating
them with skeletal traction or a cast-brace. -
Vascular repair. A distal femur fracture associated with vascular damage should be stabilized to protect the vascular repair.
individualized. Advanced age alone should not be considered a
contraindication to internal fixation. In 1982, Mize et al. showed good
to excellent results in 8 of 11 elderly patients treated with internal
fixation (40). Surgical fixation is preferred
to minimize the hazards of prolonged bed rest. However, in the presence
of osteopenia, obtaining stable fixation is difficult and may be
impossible. Adjunctive methyl methacrylate has been shown to be
effective, and postoperative use of a cast-brace may be indicated (63).
The importance of diligent preoperative planning, meticulous
intraoperative technique, and comprehensive postoperative management is
important. With such care, good to excellent results can be obtained
through surgical intervention.
debridement plus appropriate intravenous antibiotics. Primary internal
fixation is usually advisable in Gustilo grade
I
and II fractures. In grade III fractures, limited internal fixation of
the articular fractures with external fixation of the metaphyseal
component may lower the risk of infection. Later conversion to internal
fixation is often done after the soft tissues have recovered.
of the distal femur are patients with massive, severe comminution;
severe osteopenia; or the presence of infection or severely
contaminated soft tissues that cannot be adequately debrided.
-
Good preoperative planning.
-
Gentle handling of soft tissue.
-
Accurate anatomical reduction.
-
Rigid, stable internal fixation.
-
Bone grafting of any defects.
-
Early, active rehabilitation of the limb and the patient.
AO/ASIF principles are followed. In a classic article in 1979,
Schatzker and Lambert demonstrated the importance of strict adherence
to the basic recommendations (54). They used AO
instruments and implants, and when they evaluated their results, two
distinct groups emerged. When the basic principles of accurate
reduction and stable fixation were followed, good to excellent results
were achieved in 71% of the cases. In the other group, despite using
the same instruments and implants, the basic principles were not
followed, and only 21% of this group showed good to excellent results.
This study revealed that if the requirements of accurate reduction and
stable fixation are met, good results can be achieved in most cases.
Furthermore, this study should serve as a warning of the difficulty of
surgical treatment of distal femur fractures.
limb in balanced suspension with tibial pin traction. Perform surgery
immediately or within 24 to 48 hours after the injury. A radiograph of
the opposite normal femur is helpful for preoperative planning. A
tunnel view of the intercondylar notch is helpful in judging the
displacement of vertical fractures into the joint. Use templates to
draw the outlines of the femur and fracture lines. Determine the type,
size, and position of the implants and the need for a bone graft.
Select all necessary instruments, implants, and back-up devices. The
chief surgeon must review and discuss the procedure step by step with
the assistant surgeons and surgical staff. This type of careful
preoperative planning is important to smooth surgical technique and a
successful outcome.
cancellous screws, a dynamic condylar screw system, a 95° angled blade
plate, a cloverleaf-type condylar plate, combined medial/lateral or
lateral/anterior double plates, an antegrade interlocking IM nail, or a
retrograde supracondylar nail, depending on the type of fracture,
available instrumentation, and the surgeon’s experience and skill. I
prefer the AO/ASIF system.
or similar, screws may suffice for simple stable intra-articular
unicondylar fractures (Müller type B1 or B2). Washers are usually
necessary, and one screw should always be in a buttress position.
used devices in the past for internal fixation of fractures of the
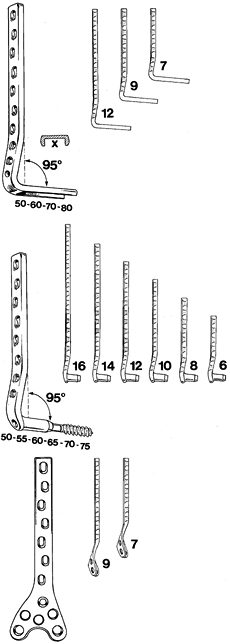
distal femur (Fig. 21.2A). Because of its
one-piece construction and the broad, flat blade, the blade plate
provides stable fixation for most fracture types, but the one-piece
characteristic of the blade plate also accounts for the difficulty in
using it. Precision and correct alignment in all three planes is
required for the insertion of this device.
 |
|
Figure 21.2. A: The ASIF 95° condylar angled blade plate. B: The ASIF 95° dynamic condylar screw and side plate system. C: The ASIF heavy condylar plate designed to fit the lateral side of the distal femur.
|
This two-piece device is more forgiving and allows correction in the
sagittal plane after the lag screw is inserted. Precise seating is also
easier because the channel is precut directly over a guide wire. The
cannulated triple reamer used for cutting the hole for the screw has
less risk of disrupting split condyles than the seating chisel,
especially in young, hard, cancellous bone. The DCS also has an
advantage in that it provides interfragmentary compression of condylar
fragments (37).
through a straight lateral, anterolateral, anteromedial, or straight
medial approach. These surgical approaches are described in Chapter 3.
Complex intraarticular fractures are best exposed through an
anterolateral approach such as that used for total knee arthroplasty,
displacing the patella medially. This approach provides access for
lateral implants and permits access to the articular condyles.
-
To reflect the tibial tubercle, extend
the incision to a point about 15 mm distal to the tuberosity. Extend
the retinacular dissection along the lateral margin of the patellar
tendon. At this point, the tibial tuberosity should be fully exposed so
that the exact center can be identified. -
Make a 3.2 mm drill hole through this
center and continue it carefully through the posterior cortex.
Overdrill the hole in the anterior or near cortex with a 4.4 mm drill.
Measure the distance between the anterior and posterior cortices so the
appropriate-length 6.5 mm cancellous screw can be used later to
stabilize the bone block. -
Tap the near cortical hole with a 6.5 mm tap.
-
Identify the four cortices of the tibial
tuberosity and make a drill hole at each corner through the near part
of the cortex using a 3.2 mm drill. -
Carefully remove a block of cortical and
cancellous bone consisting of the entire tibial tuberosity with the
attached patellar tendon. To accomplish this, connect the four corner
holes by osteotomies made with a narrow, straight osteotome or small
sagittal saw, and lift the block out using ½-inch (1.3 cm) curved
osteotome. The block should be about 1.5 cm thick. -
Reflect the bone block, with attached
tendon and patella, medially to give complete exposure to the anterior
and articular surfaces of the distal femur (Fig. 21.3).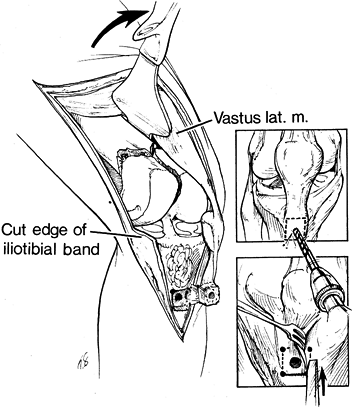 Figure 21.3.
Figure 21.3.
After the tibial tuberosity is elevated, a good exposure of all
components of the fracture is achieved. (Redrawn from Mize RD, Buchloz
RW, Grogan DP. Surgical Treatment of Displaced, Comminuted Fractures of
the Distal Femur. J Bone Joint Surg 64-A:878, 1982, with permission.)
-
Following the surgical exposure, clean
the fracture fragments of hematoma and inspect the entire knee joint.
Then reduce and stabilize the intraarticular condylar fragments. For
purposes of this discussion, the Müller type C1, which is a T or Y
fracture with split condyles, will be used (Fig. 21.4).![]() Figure 21.4. The Müller type C1, the so-called T or Y condylar fracture with split condyles.
Figure 21.4. The Müller type C1, the so-called T or Y condylar fracture with split condyles. -
With the knee flexed at 90°, reduce the
condyles anatomically and restore the articular surface and
patellofemoral groove. Secure the reduction with large sharp pointed
tenaculum bone-holding forceps. Provisionally fix the condyles with
Kirschner wires (K-wires). Do not place the K-wires where they will
interfere with fixation. -
Stabilize the condyles by placing two 6.5 mm cancellous screws with washers (Fig. 21.5).
Choose the sites for screw placement carefully to avoid the entry site
of the condylar lag screw or seating chisel. Insert the screws slightly
proximal to the proposed site of the primary
P.714
fixation device, and posterior and anterior to the middle of the shaft, well away from the anticipated path of the slide plate (Fig. 21.5A, Fig. 21.5B).
The screws need not be parallel, nor should the threads bridge the
fracture lines. Use washers to prevent sinking of the screw heads into
the lateral cortex. Once the condyles are stabilized with accurate
anatomic alignment, remove the temporary K-wires and fix the remainder
of the fracture using either the DCS or the angled blade plate.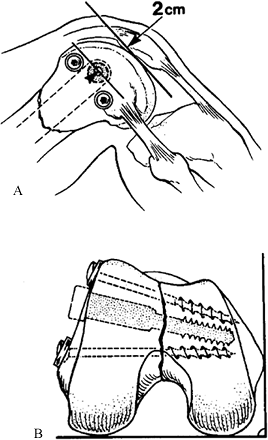 Figure 21.5. A: The articular surface and split condyles have been restored and fixed with two 6.5 mm cancellous screws with washers. B:
Figure 21.5. A: The articular surface and split condyles have been restored and fixed with two 6.5 mm cancellous screws with washers. B:
The screws are inserted slightly proximal to the proposed entry site of
the large condylar screw, and posterior and anterior to the middle of
the shaft, well away from the anticipated path of the side plate. -
Reduce the supracondylar component of the
fracture. When there is minimal comminution in the metaphyseal area,
reduce the condyles directly to the proximal fragment and temporarily
fixed with multiple crossed K-wires or better stabilize with one or
more 4.5 mm cortical lag screws inserted using lag technique. -
When there is comminution in the
metaphyseal area, the side plate of the DCS, blade plate, or similar
device is needed to maintain reduction. In such cases, insert the
condylar lag screw into the distal fragment. Attach the side plate to
the condylar screw, reduce the supracondylar component of the fracture,
and stabilize it with the side plate. The angled blade plate and other
devices can be used in a similar manner.
lateral, or both, particularly of the posterior part, may produce a
Hoffa fragment. This is very difficult to manage because the entire
fragment may be covered by articular cartilage and is devascularized.
These fractures must be recognized, anatomically reduced, and solidly
internally fixed. Fixation usually must be placed through the articular
surface. K-wires and absorbable pins usually are not strong enough, and
4.0 mm cancellous or similar screws are required. Insert these screws
down to the subchondral bone, well beneath the surface of the cartilage.
-
Indirect reduction techniques use tension
on the soft-tissue attachments to the bony fragments to pull and guide
them back into their proper alignment (2,35,47).
This process, also known as ligamentotaxis, has often been equated with
the sails of a ship because the lines are pulled taunt, and wind fills
the sail and holds it in the desired position. This technique is
indicated in severely comminuted intraarticular fractures of the distal
femur, one of the most difficult types to align and stabilize when
traction is between the femur and tibia. The same principles apply to
metaphyseal fractures. -
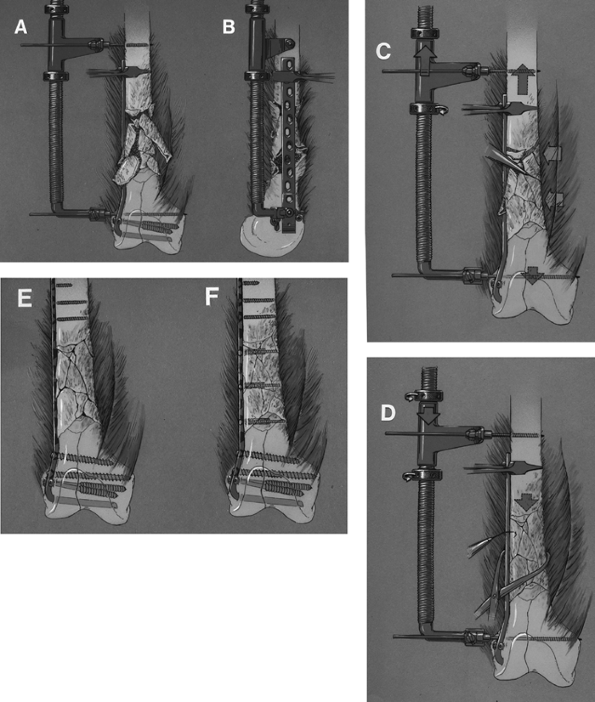
Strip soft tissues only in area where the plate will lie. Next, insert the blade plate or condylar screw (Fig. 21.6A). Insert two Schanz pins, one proximal to the side plate and one into the condyles through the most distal plate hole (Fig. 21.6B).
Through distraction of the soft-tissue attachments, pull and guide the
bony fragments into reasonable alignment. A small periosteal elevator
or dental pick can be helpful to tease and guide fragments. By
overdistracting, it becomes easier to tease fragments into better
alignment (Fig. 21.6C). With the fragments
restored to their proper alignment, turn the nuts on the distractor
counter clockwise to “slightly compress” the comminuted zone (Fig. 21.6D).![]() Figure 21.6. Indirect reduction of a supracondylar fracture of the femur. A. Reduce and fix the intraarticular fracture and insert a blade plate or condylar screw. B. Insert Schanz screws distal and proximal to the fracture and attach the distractor. C. Overdistract the fracture and tease comminuted fragments into position. D. Now slightly compress the comminuted zone to complete the reduction. E,F. Selectively insert screws to complete the fixation.
Figure 21.6. Indirect reduction of a supracondylar fracture of the femur. A. Reduce and fix the intraarticular fracture and insert a blade plate or condylar screw. B. Insert Schanz screws distal and proximal to the fracture and attach the distractor. C. Overdistract the fracture and tease comminuted fragments into position. D. Now slightly compress the comminuted zone to complete the reduction. E,F. Selectively insert screws to complete the fixation. -
After axial and rotational alignment have
been verified, attach the proximal end of the plate to the femoral
shaft, skipping the comminuted zone. Selectively insert lag screws to
increase both the stability and fixation of the construct (Fig. 21.6E, Fig. 21.6F).
With this technique, medial bone grafts are not necessary and are not
recommended because they require stripping of the medial soft tissues
for placement. Maintenance of soft-tissue attachments usually promotes
rapid healing of the fracture because the blood supply to the
comminuted fragments is maintained.
compressing screw. It has a 95° angle between the screw and the side
plate, and both the screw and side plate are available in a variety of
lengths. The condylar screw must be inserted parallel to the knee joint
on the anteroposterior view and on the lateral side of the femoral
condyle so that the plate will lie flat on the lateral midshaft. Proper
alignment may prove difficult until the technique, which involves the
use of K-wires and the available aiming devices, is mastered. With
practice in a motor skills workshop, experience with simple fractures,
and good preoperative planning with close attention to detail, the
technique can be mastered. Determine the position of the condylar screw
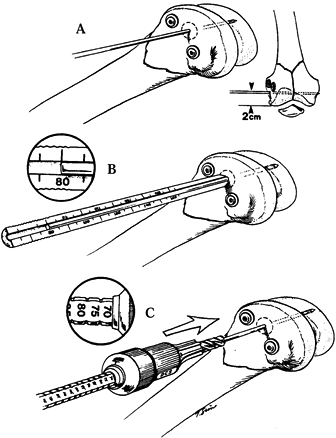
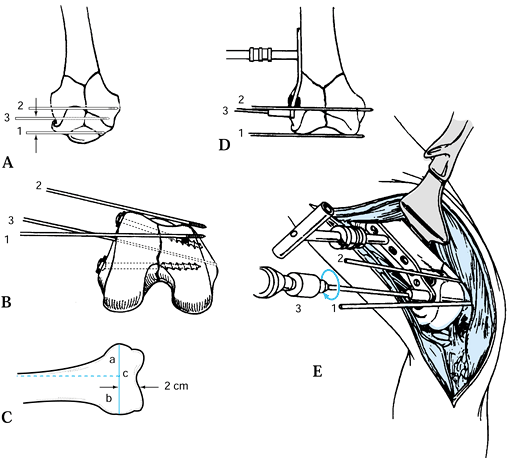
by placing three K-wires (Fig. 21.7A, Fig. 21.7B, Fig. 21.7C, Fig. 21.7D and Fig. 21.7E).
 |
|
Figure 21.7. Placement of the three directional guide wires.
|
-
With the knee bent to 90°, insert a 2 mm
K-wire transversely through the soft tissues of the anterior knee joint
and parallel to the joint axis (Fig. 21.7A, wire 1). Insert a second wire (Fig. 21.7A,
wire 2) anteriorly over the lateral and medial condyles to show the
inclination of the patellofemoral joint. The distal femur is
rhomboid-shaped; therefore, this wire will slope from anterolateral to
posterior medial. -
The location of the site for insertion of
the screw, and for a blade plate as well, must be precise if the side
plate is to lie on the midportion of the lateral aspect of the femoral
shaft. To determine this, measure 2 cm proximal to the articular
surface and draw a line with a marking pen at right angles to the axis
of the femoral shaft (Fig. 21-7C, line a). Then
divide this line in half (line b). Draw a cross line (c) at the halfway
point of the anterior half of line a. This will generally result in
appropriate position of the guide pin for the screw. Verify with direct
visualization. -
The DCS angle guide is a mirror image of the side plate and is used in placing the guide wire through the lateral condyle (Fig. 21.7D, Fig. 21.7E).
Use a standard 9 inch or 230 mm guide wire. The guide pin must be
parallel with the first and second guide wires. It is the definitive
guide for the triple reamer and the subsequent placement of the large
condylar lag screw. Insert it under fluoroscopic visualization until
the medial cortex is reached. When the correct position of the guide
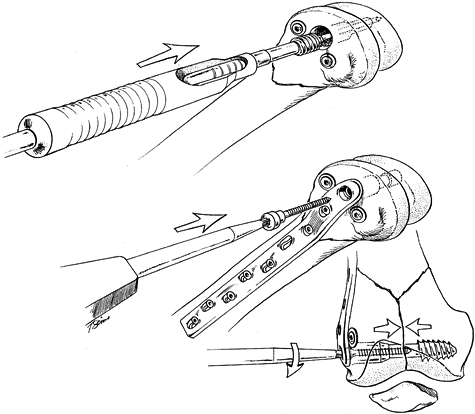
pin has been verified, remove the first and second K-wires (Fig. 21.8A).![]() Figure 21.8. A: Slip the cannulated condylar screw over the guide wire and into the reamed hole. B: Insert the dynamic compressing screw. C: Tighten the compressing screw, resulting in interfragmentary compression between the split condyles.
Figure 21.8. A: Slip the cannulated condylar screw over the guide wire and into the reamed hole. B: Insert the dynamic compressing screw. C: Tighten the compressing screw, resulting in interfragmentary compression between the split condyles. -
Slip the direct measuring device over the
guide wire and read the length of the guide pin that has been inserted
into the femur (Fig. 21.8B). Reverse
calibration on the measuring device allows direct measurement of the
guide pin depth. After taking the measurement, advance the guide wire a
few more millimeters to further engage the medial cortex to help
prevent inadvertent removal of the guide wire with the triple reamer.
Note that because of the rhomboidal shape of the femoral condyles,
P.716P.717P.718
the guide pin should appear short on the AP view (Fig. 21.7B). Overpenetration will result in prominence of the point of the lag screw in the knee joint, which is painful. -
Assemble the triple reamer (Fig. 21.8C),
which allows you to set the depth in 5 mm increments and has a locking
nut to prevent slippage of the depth setting during the reaming
procedure. Always verify that you have the correct triple reamer. To
distinguish the condylar triple reamer from the one used for the hip,
it is labeled DCS. Set the depth setting to about 10 mm less than the
measurement taken from the direct measuring device. The reamed channel
will end about 10 mm from the medial cortex. Slip the cannulated triple
reamer over the guide wire to ream the channel. -
Occasionally, the guide wire will be inadvertently withdrawn with the triple reamer (Fig. 21.9A, Fig. 21.9B, Fig. 21.9C and Fig. 21.9D).
If this happens, reinsert the wire; otherwise, there is a risk of
misplacing the lag screw. This danger is especially great in elderly
patients with osteopenic bone. To reposition the guide pin, first
insert the short centering sleeve and then insert a lag screw backward
into the sleeve (Fig. 21.9C). Reinsert the guide pin through the cannulated lag screw and correctly reposition it (Fig. 21.9D). Verify its correct position on the image intensifier.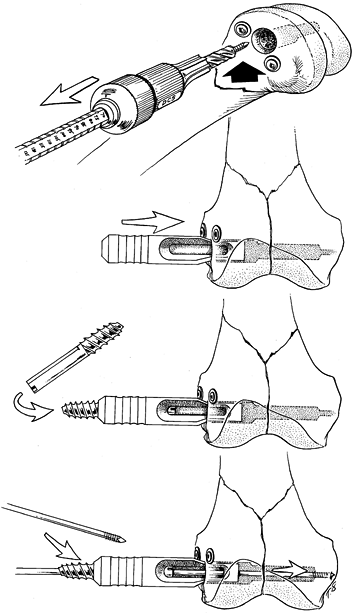 Figure 21.9. A: The guide wire is inadvertently withdrawn with the triple reamer. B: To reinsert the guide wire, first insert the short centering sleeve. C: Next, insert a lag screw backward into the sleeve. D: Insert the guide wire into the cannulated lag screw and position it correctly.
Figure 21.9. A: The guide wire is inadvertently withdrawn with the triple reamer. B: To reinsert the guide wire, first insert the short centering sleeve. C: Next, insert a lag screw backward into the sleeve. D: Insert the guide wire into the cannulated lag screw and position it correctly. -
If the patient has hard cancellous bone,
tap the reamed channel for the lag screw threads. Use the DCS tap with
a short centering sleeve to tap to the same depth as the reamed
channel. Do not pretap the channel in patients with osteopenic bone. -
Assemble the DCS and place it onto the
wrench using the long centering sleeve. Position the assembly over the
guide pin and insert the centering sleeve into the reamed hole (Fig. 21.10A).
Insert the screw until the zero mark on the wrench reaches the lateral
cortex. At this point, the tip of the lag screw is about 10 mm from the
medial cortex, and the proximal end of the lag screw is even with the
lateral cortex. In porotic bone, insert the lag screw to the 5 mm mark,
which allows the tip of the lag screw to cut itself 5 mm beyond the
prereamed channel. With the lag screw properly inserted, the T handle
of the insertion wrench should be parallel with the shaft of the femur,
otherwise, the slide plate cannot be slid onto the lag screw.![]() Figure 21.10. A:
Figure 21.10. A:
Make the point of entry for the condylar lag screw about 2 cm from the
knee joint and in line with the middle of the femoral shaft or slightly
anterior. Place the third wire parallel with the knee joint axis and
with the tip just penetrating the medial cortex. B:
Reverse calibration on the measure device allows direct measurement of
the guide pin depth if a standard 9-inch or 230 mm wire is used. C:
The depth setting of the triple reamer should be 10 mm less than the
measurement from the direct measuring device. The triple reamer is
cannulated. Slip it over the guide wire. -
Remove the wrench with its centering
sleeve and slide the appropriate-length side plate over the lag screw.
Withdraw the guide pin. While an assistant surgeon applies firm
counterpressure medially, use the impactor to seat the side plate
gently. Insert the dynamic condylar compression screw (Fig. 21.10B, Fig. 21.10C).
When fixing a T or Y fracture with split condyles, interfragmentary
compression can be achieved with the compressing screw. Do not compress
with the compression screw in osteopenic bone because the lag screw may
pull out of the bone. -
Achieve supplemental fixation of the side
plate to the distal fragment by inserting one or two 6.5 mm cancellous
screws through the plate immediately proximal to the large condylar lag
screw. Ensure that the proximal component of the fracture is well
reduced. Use a tension device to achieve axial compression. After
tension is applied to the plate, check the reduction and stability of
the fixation. If both are satisfactory, complete screw fixation of the
plate to the femoral shaft.
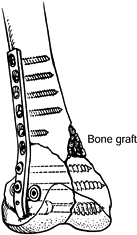
condition of the medial cortex. Stability requires good cortical
contact in compression. I advocate autologous bone grafting of most
fractures of the distal femur that have medial defects (Fig. 21.11):
 |
|
Figure 21.11.
Augment fixation of the condyles by placing two 6.5 mm cancellous screws through the round holes directly above the large condylar screw. Secure the side plate to the shaft with 4.5 mm cortical screws. Fill the medial defect with cancellous bone graft. |
-
Augment fixation of the condyles by
placing two 6.5 mm cancellous screws through the round holes directly
above the large condylar screw. -
Secure the side plate to the shaft with 4.5 mm cortical screws.
-
Fill the medial defect with cancellous bone graft.
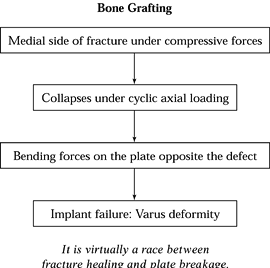
fracture, in which the technique of indirect reduction is used. Out of
68 cases, I have found that bone grafting was necessary in 59 (39).
The medial side of the fracture is subject to compression forces with
activity. If the medial side defect is present because of comminution,
it will collapse under cyclic axial loading and create bending forces
on the plate exactly opposite the defect. If the fracture does not heal
in the usual time, the plate will break, often very quickly if the
forces are great. Use autologous cancellous bone grafting to fill and
buttress the medial defect. Failure to graft these defects can lead to
implant failure, loss of reduction, and delayed union or
nonunion. I prefer the anterior iliac crest as the donor site (Fig. 21.12).
 |
|
Figure 21.12. The progression of a medial instability to varus deformity.
|
with a 95° fixed angle between the blade and the plate. The blade is U
shaped, which contributes to the strength of this device. Owing to its
one-piece construction and broad flat blade, the blade provides stable
fixation for most fracture types. However, the one-piece configuration
of the plate also makes it difficult to use. Precision and correct
alignment in all three planes is required for the insertion of this
device. The technical aspects for the use of this device can be found
in Müller and associates’ Manual of Internal Fixation Technique Recommended by the AO Group (44).
with a heavy proximal side plate configured like the broad dynamic
compression plate and a cloverleaf-shaped distal portion precontoured
to correspond to the lateral condylar surface of the distal end of the
femur (Fig. 21.2C). The distal condylar section
has six round holes to accommodate 6.5 mm cancellous screws. Never
begin surgical fixation of the distal femur without having this implant
or a similar plate for backup. For example, if the lateral condyle is
comminuted or if there are multiple articular fracture lines in both
the sagittal planes and the coronal planes, both the DCS system and the
angled blade plate may be impossible to use. The cloverleaf condylar
plate is an excellent device to salvage a failed DCS system or a 95°
angled blade plate. Although the cloverleaf condylar plate is
technically easier to apply, it should not be used indiscriminately. A
major problem with this device is its lack of rigid interface between
the heads of the screws and the plate; therefore, any deficiency of the
medial cortex usually results in varus malalignment at 4 to 6 weeks
postoperatively. If the fracture is not accurately reduced before this
implant is introduced, distal fragment displacement into valgus
alignment may result. In addition, the cloverleaf plate is not as
strong as either the condylar screw system or the blade plate.
If a lateral approach is used, a separate medial incision is usually
required to apply a medial plate. If an anterolateral approach is used,
a second plate can be applied at right angles to the lateral plate by
placing it on the anterior cortex near the medial side through the same
incision. Always bone graft any defects on the medial side. Sanders et
al. (53) have discussed the use of double
plating for unstable fractures of the distal femur. Some of the
disadvantages to medial/lateral double plating include multiple
surgical exposures, longer operating time, increased stripping of the
soft-tissue attachments with decreased blood supply to bone fragments,
and increased risk of infection. Chapman and Finkemeier (8)
have shown improved results in nonunions using the anterolateral
approach and lateral and anterior plates. The use of indirect reduction
techniques has decreased the indication for double plate fixation.
Antegrade nailing is limited to very specific cases for the distal
femur because at least 10 cm of intact bone above the intercondylar
notch is normally required. Essential to success is the ability to
secure the two distal screws into intact bone. The surgical technique
and indications are discussed in Chapter 20.
medial and lateral condyles. The nail is then anchored to the condyles
with large compression screws. The screws need to engage the opposite
cortex for minimal fixation. In the case of Y or T condylar fractures,
the condyles must be reduced and fixed with lag screws before the
insertion of the nails.
It controls angulation and rotation of the femur but allows axial
impaction. This feature can be desirable in the elderly because it
yields an increased union rate, although it results in some shortening (34,69). It is not suitable for younger patients because of the frequent complications of shortening (34,70). Since the development of retrograde interlocked IM nails, it is little used.
cannulated, single-piece, stainless steel implant that is available in
11 and 12 mm diameters. It was initially designed for the elderly with
a fracture of the distal femur. However, results were so good in the
elderly that they have applied it to younger patients with the same
good results (23,33).
Suggested advantages of the GSH nail include a reduction in operating
time and blood loss, and a reduction of devascularization of fracture
fragments. All of these factors combine to create a lower incidence of
complications (22). This technique is discussed in Chapter 20.
-
Insert tubes for suction drainage to
prevent the formation of a hematoma. Close the synovial tissue and
iliotibial band subcutaneous fat and skin in layers. If an
anterolateral approach is used, a meticulously layered closure is
important to prevent adhesions and to permit early vigorous knee
motion. Do not suture the vastus lateralis to the intermuscular septum;
doing so may retard knee motion. Meticulous closure of the skin is
recommended. Apply a sterile dressing and splint the knee. -
As soon as the drains are removed, begin
knee rehabilitation. Continuous passive emotion (CPM) is helpful to
regain knee motion in the immediate postoperative period. The AO group
advocates positioning the limb on a frame, with the hip and knee flexed
90°. This position, combined with CPM, prevents quadriceps contraction,
helps decrease swelling, and enhances knee motion if the patient can
tolerate it. Continue CPM full-time until gait training is initiated
and then intermittently after gait training is started. If CPM is
unavailable, maintain the limb in the 90°/90° position for 4 to 6 days.
While the limb is on the frame, begin gentle, active, assisted
range-of-motion exercises. Because of the risk of a flexion
contracture, many surgeons prefer that the rest position be in full
extension. -
If the fracture has been fixed rigidly,
the patient may begin immediate partial weight bearing of about 10 kg.
The patient who remains completely non-weight bearing with the hip and
knee flexed may developed circulatory stasis and rapid disuse
osteopenia. -
Maintain weight bearing to the weight of
the lag using two crutches until there is clinical and radiographic
evidence of healing of the fracture, which usually requires 12 to 16
weeks, at which time progress gradually to full weight bearing.
Supplemental external support is usually not required, but a functional
cast-brace may be desirable for the elderly patient with tenuous
fixation, the patient with marked comminution, or the unreliable
patient.
definitive treatment of supracondylar fractures of the femur because
the transfixation pins tend to tie down the quadriceps mechanism and
interfere with regaining knee motion (59). The
primary indication for external fixation today is high-energy type II,
IIIB, and C open supracondylar fractures of the femur, in which initial
primary internal fixation of the metaphyseal portion of the fracture is
thought to be too risky because of the potential for infection, or the
fracture has occurred in the presence of other severe multiple injuries
and the time required for definitive internal fixation is inadequate.
In the instance in which the fracture has occurred along with other
injuries, a simple anterior single bar frame, bridging from the femur
to the tibia to provide temporary stability and alignment of the
extremity until definitive internal fixation can be done, may be
indicated. This can be a life-saving procedure because it stabilizes
the limb and allows early mobilization of the patient.
being hit by the bumper of a high-speed vehicle, the soft-tissue
envelope may be severely compromised and reconstruction may require a
local or free flap, particularly if the injury extends across the knee
joint into the tibial plateaus. In these cases, many surgeons prefer to
perform limited internal fixation of the articular surface of the femur
with lag screws and wires. The metaphyseal portion of the fracture is
then managed with an external fixator from the shaft of the femur to
the reassembled condyles or bridging to the tibia. When only the femur
is fixed, use a hybrid circular fixator using tensioned wires in the
articular fragments and half pins in the shaft.
quality allows, most trauma surgeons today convert to plate fixation
after the condition of the soft tissues has stabilized and the risk of
infection has been minimized (see Chapter 32).
fractures of the distal femur include neurovascular injury,
thromboembolic disease, delayed union or nonunion, malunion, infection,
joint contracture, knee instability, posttraumatic arthritis, implant
failure, refracture after removal of the implant, and others. Although
many of these problems cannot be avoided, the occurrence of some can be
diminished by recognizing potential pitfalls in the various phases of
treatment.
suspicion for associated injuries to the head, chest, abdomen, and
spine. Carefully evaluate the pelvis and all extremities for possible
occult injuries. Ligamentous instability of the knee can occur with
fracture of the distal femur and often cannot be determined until after
the fracture is stabilized. Carefully evaluate the neurovascular
function; if vascular injury is suspected, arteriography is indicated.
many of the intraoperative and postoperative complications. During this
planning phase, determine the best surgical approach; the type,
approximate size, and position of the implants; and the possible need
for a bone graft. Making these decisions before surgery allows
preparation of the appropriate instrumentation and implants, and a
smoother surgical procedure with less wound exposure time.
stripping, accurate anatomic reduction, stable fixation, and grafting
of any bony defects cannot be overemphasized. Strict adherence to these
principles will decrease the incidence of infection, implant failure,
malunion, delayed wound and fracture healing, and nonunion. Accurate
reconstruction of the articular surfaces is essential.
plate or the DCS is failure to appreciate the rhomboid shape of the
distal femur. The blade or condylar screw must be directed somewhat
posteriorly and be of proper length to avoid penetration of the
anterior surface of the medial femoral condyle.
fractures with severe osteopenia or comminution. Occasionally, these
fractures are impossible to stabilize surgically with any type of
implant and surgery may not be indicated.
rehabilitation will serve to decrease swelling, avoid muscle
contracture, enhance knee motion, and diminish the incidence of
thromboembolic disease. During this phase, stress patient education.
Early excessive weight bearing can lead to implant failure, resulting
in deformity or delayed healing and the need for repeat surgery.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
RW, Ross SE, Lawrence KL. Fatigue of the Interlocking Nail in the
Treatment of Fractures of the Distal Part of the Femoral Shaft. J Bone Joint Surg 1987;69-A:1391.
MS, Brumback RJ, Ellison TS, et al. Interlocking Intrameduallary
Nailing for Ipsilateral Fractures of the Femoral Shaft and Distal Part
of the Femur. J Bone Joint Surg 1991;73-A:1492.
PS, Luchetti WT, Campbell JT, Vresilovic EJ. Supracondylar Femur
Fracture Above a Mature Knee Fusion Treated with a Long Locked
Intramedullary Rod. Am J Orthop 1997;26:630.
JF, Dehne E, LaFollette B. Closed Reduction and Early Cast-Brace
Ambulation in the Treatment of Femoral Fractures. Part II: Results in
143 Fractures. J Bone Joint Surg 1973;55-A:1581.
JF, King P. Closed Reduction and Early Cast-Brace Ambulation in the
Treatment of Femoral Fractures. Part I: An In-Viro Quantitative
Analysis of Immobilization in Skeletal Traction and Cast Brace. J Bone Joint Surg 1973;55-A:1559.
MB, Caucci D, Zecher SB, Covall DJ. Treatment of Intercondylar and
Supracondylar Distal Femur Fractures Using the GSH Supracondylar Nail. Am J Orthop 1995;24:684.
I, Moro RE, De Pedro Moro JA, Cebrian Para JL, Lopez-Duran Stern L.
Antegrade Nailing for Fractures of the Distal Femur. Clin Orthop 1998;350:74.
K, Behzadi K, DeCoster TA, et al. Mechanics of Retrograde Nail Versus
Plate Fixation for Supracondylar Femur Fractures. J Orthop Trauma 1995;9:152.
CJ, Lindsay RW, Noble PC, et al. Optimal Location of a Single Distal
Interlocking Screw in Intermedullary Nailing of Distal Third Femoral
Shaft Fractures. J Orthop Trauma 1998;12:267.
JB, DeLee JC, Heckman JD, Keever JE. Supracondylar and Intercondylar
Fractures of the Femur Treated with a Supracondylar Plate and Lag
Screw. J Bone Joint Surg 1982;64-A:864.
JA, Londy F, Saltzman CL, et al. Interlocking Intramedullary Nails—An
Improved Method of Screw Placement Combining Image Intensification and
Laser Light. Clin Orthop 1992;281:199.
SL, Trager S, Green S, Seligson D. Management of Supracondylar
Fractures of the Femur with the GSH Intramedullary Nail: Preliminary
Report. Contemp Orthop 1991;22:631.
SL, et al. Management of Supracondylar Fractures of the Femur with the
GSH Supracondylar Nail: The Percutaneous Technique. Tech Orthop 1994;9:189.
WM, Bennett FS, DeLong WG Jr, et al. Intitial Experience with the
Treatment of Supracondylar Femoral Fractures Using the Supracondylar
Intramedullary Nail: A Preliminary Report. J Orthop Trauma 1994;8:322.
H, Stockman B, Van Damme G, et al. The Retrograde Intramedullary
Supracondylar Nail: An Alternative in the Treatment of Distal Femoral
Fractures in the Elderly. Arch Orthop Trauma Surg 1991;118:92.
C, Konemann B, Miclau T, et al. A New Mechanical Aiming Device for the
Placement of Distal Interlocking Screws in Femoral Nails. Arch Orthop Trauma Surg 1998;117:147.
RF, Schaffhausen JM, Bechtold JE. Biomechanical Characteristics of
Interlocking Femoral Nails in the Treatment of Complex Femoral
Fractures. Clin Orthop 1991;267:169.
KS, Shen WY, So WS, et al. Interlocking Intramedullary Nailing for
Supracondylar and Intercondylar Fractures of the Distal Part of the
Femur. J Bone Joint Surg 1991;73-A:332.
SE, Seligson D, Henry SL. Intramedullary Supracondylar Nailing of
Femoral Fractures. A Preliminary Report of the GSH Supracondylar Nail. Clin Orthop 1993;296:200.
DS, Isbister ES, Porter KM. Zickel Supracondylar Nail for Supracondylar
Femoral Fractures in Elderly or Infirm Patients. A Review of 33 Cases. J Bone Joint Surg 1994;76-B:596.
EC, Maestu PR, Blanco RP. Blade-plating of Closed Displaced
Supracondylar Fractures of the Distal Femur with the AO/ASIF System. J Trauma 1992;32:174.
R, Regazzoni P, Reudi TP. Treatment of Supracondylar-Intercondylar
Fractures of the Femur Using the Dynamic Condylar Screw. J Orthop Trauma 1989;3:214.
P 3rd. The Treatment of Femoral Shaft Fractures Using Intramedullary
Interlocked Nails with and without Intramedullary Reaming: A
Preliminary Report. J Orthop Trauma 1997;11:89.
PR, McCarty EC, Shyr Y, Johnson D. Length of Operative Procedures:
Reamed Femoral Intramedullary Nailing Performed with and without a
Fracture Table. J Orthop Trauma 1998;12:485.