Talus
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > IV – Lower Extremity Fractures and Dislocations > 40 – Talus
40
Talus
EPIDEMIOLOGY
-
These are second in frequency among all tarsal fractures.
-
Two percent of all lower extremity injuries and 5% to 7% of foot injuries involve fractures of the talus.
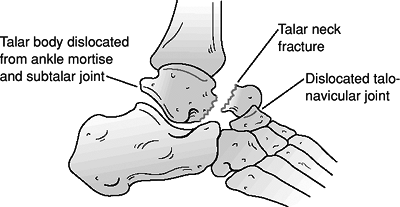
ANATOMY (FIG. 40.1)
-
The body of the talus is covered
superiorly by articular surface through which a person’s body weight is
transmitted. The anterior aspect is wider than the posterior aspect,
which confers intrinsic stability to the ankle. -
Medially and laterally, the articular
cartilage extends plantar to articulate with the medial and lateral
malleoli, respectively. The inferior surface of the body forms the
articulation with the posterior facet of the calcaneus. -
The neck of the talus is roughened by
ligamentous attachments and vascular foramina. It deviates medially 15
to 25 degrees and is the most vulnerable to fracture. -
The talar head has continuous articular
facets for the navicular anteriorly, the spring ligament inferiorly,
the sustentaculum tali posteroinferiorly, and the deltoid ligament
medially. -
There are two bony processes. The lateral
process is wedge shaped and articulates with the posterior calcaneal
facet inferomedially and the lateral malleolus superolaterally. The
posterior process has a medial and lateral tubercle separated by a
groove for the flexor hallucis longus tendon. -
An os trigonum is present in up to 50% of
normal feet. It arises from a separate ossification center just
posterior to the lateral tubercle of the posterior talar process. -
Sixty percent of the talus is covered by
articular cartilage. No muscles originate from or insert onto the
talus. The vascular supply is dependent on fascial structures to reach
the talus; therefore, capsular disruptions may result in osteonecrosis. -
The vascular supply to the talus consists of:
-
Arteries to the sinus tarsi (peroneal and dorsalis pedis arteries).
-
An artery of the tarsal canal (posterior tibial artery).
-
The deltoid artery (posterior tibial artery), which supplies the medial body.
-
Capsular and ligamentous vessels and intraosseous anastomoses.
-
MECHANISM OF INJURY
-
Most commonly associated with a motor
vehicle accident or a fall from a height with a component of
hyperdorsiflexion of the ankle. The talar neck fractures as it impacts
the anterior margin of the tibia. -
“Aviator’s astragalus”: This historical
term refers to the rudder bar of a crashing airplane impacting the
plantar aspect of the foot, resulting in a talar neck fracture.
P.436
 |
|
Figure 40.1. Superior and inferior views of the talus (stippling indicates the posterior and lateral processes).
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
CLINICAL EVALUATION
-
Patients typically present with foot pain.
-
Range of foot motion is typically painful and may elicit crepitus.
-
Diffuse swelling of the hindfoot may be present, with tenderness to palpation of the talus and subtalar joint.
-
Associated fractures of the foot and ankle are commonly seen with fractures of the talar neck and body.
RADIOGRAPHIC EVALUATION
-
Anteroposterior (AP), mortise, and
lateral radiographs of the ankle, as well as AP, lateral, and oblique
views of the foot are obtained. -
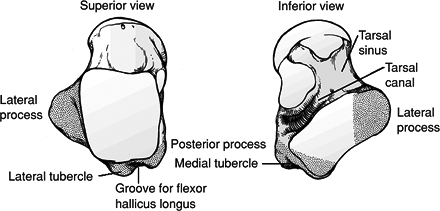
Canale view: This provides an optimum
view of the talar neck. Taken with the ankle in maximum equinus, the
foot is placed on a cassette, pronated 15 degrees, and the radiographic
source is directed cephalad 15 degrees from the vertical (Fig. 40.2). -
Computed tomography (CT) is helpful to
characterize fracture pattern and displacement further and to assess
articular involvement. -
Technetium bone scans or magnetic resonance imaging (MRI) may be useful in evaluating possible occult talar fractures.
CLASSIFICATION
Anatomic
-
Lateral process fractures
-
Posterior process fractures
-
Talar head fractures
-
Talar body fractures
-
Talar neck fractures
P.437
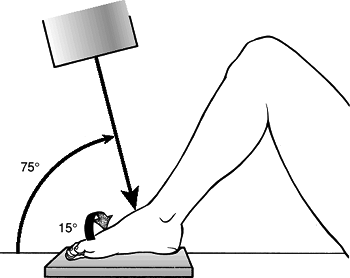
Hawkins Classification of Talar Neck Fractures (Figs. 40.3 and 40.4)
 |
|
Figure 40.2. Canale and Kelly view of the foot. The correct position of the foot for x-ray evaluation of the foot is shown.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
| Type I: | Nondisplaced |
| Type II: | Associated subtalar subluxation or dislocation |
| Type III: | Associated subtalar and ankle dislocation |
| Type IV: | (Canale and Kelley): type III with associated talonavicular subluxation or dislocation |
OTA Classification of Talar Fractures
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
TREATMENT
Fractures of the Talar Neck and Body
These represent a continuum and are considered together.
Nondisplaced Fractures (Hawkins Type I)
-
Fractures that appear nondisplaced on
plain radiographs may show unrecognized comminution or articular
step-off on CT scan. Fractures must truly be nondisplaced with no
evidence of subtalar incongruity to be considered a type I fracture. -
Treatment consists of a short leg cast or
boot for 8 to 12 weeks. The patient should remain non–weight bearing
for 6 weeks until clinical and radiographic evidence of fracture
healing is present.
Displaced Fractures (Hawkins Types II to IV)
-
Immediate closed reduction is indicated,
with emergency open reduction and internal fixation (ORIF) for all open
or irreducible fractures.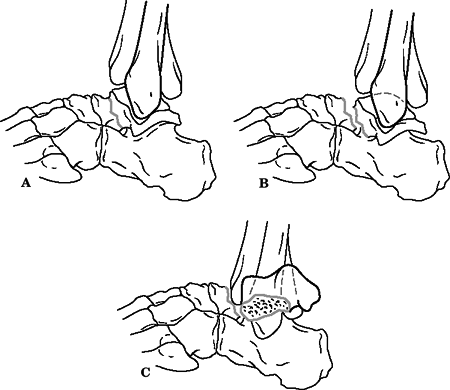 Figure
Figure
40.3. The three patterns of talar neck fractures as described by
Hawkins. Note that type I fractures are nondisplaced. (A) Type I talar
neck fractures with no displacement. (B) Type II talar neck fractures
with displacement and subluxation of subtalar joint. (C) Type III talar
neck fracture with displacement and dislocation of both ankle and
subtalar joints.(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)![]() Figure
Figure
40.4. Type IV fracture of the talar neck with subluxation of the
subtalar joint and dislocation of the talonavicular joint.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
If anatomic reduction is obtained and
confirmed by CT scan, the patient should be placed in a short leg cast,
with treatment as for nondisplaced fractures. -
If open reduction is necessary, all major fragments should be salvaged. Primary arthrodesis should be avoided.
-
Surgical approaches include:
-
Anteromedial: This approach may be
extended from a limited capsulotomy to a wide exposure with malleolar
osteotomy. The internal is just medial to the anterior tibial tendon.
This approach allows visualization of the talar neck and body. Care
must be taken to preserve the saphenous vein and nerve and, more
importantly, the deltoid artery. -
Posterolateral: This approach provides
access to posterior process and talar body. The interval is between the
peroneus brevis and the flexor hallucis longus. The sural nerve must be
protected. It is usually necessary to displace the flexor hallucis
longus from its groove in the posterior process to facilitate exposure. -
Anterolateral: This approach allows
visualization of the sinus tarsi, lateral talar neck, and subtalar
joint. Inadvertent damage to the artery of the tarsal sinus can occur
through this approach. -
Combined anteromedial-anterolateral: This is often used to allow maximum visualization of the talar neck.
-
P.438
P.439
-
Internal fixation: Two interfragmentary
lag screws or headless screws are placed perpendicular to the fracture
line. The screws can be inserted in antegrade or retrograde fashion.
Posterior-to-anterior directed screws have been demonstrated to be
biomechanically stronger. -
Use of titanium screws allows better visualization with MRI for evaluation of subsequent osteonecrosis.
-
Areas of significant comminution and bone loss should be grafted.
-
A plate can be used to buttress areas of comminution.
-
A short leg cast or removable boot should
be placed postoperatively for 8 to 12 weeks, and the patient should be
kept non–weight bearing. -
Hawkins sign: Subchondral osteopenia
(seen on the AP ankle radiograph) in the talus at 6 to 8 weeks tends to
indicate talar viability. However, the presence of this sign does not
rule out osteonecrosis; its absence is also not diagnostic for
osteonecrosis.
Lateral Process Fractures
These are intraarticular fractures of the subtalar or
ankle joint that occur most frequently when the foot is dorsiflexed and
inverted. There has been an increase in incidence with the rise in
popularity of snowboarding.
ankle joint that occur most frequently when the foot is dorsiflexed and
inverted. There has been an increase in incidence with the rise in
popularity of snowboarding.
-
Lateral process fractures are often missed on initial patient presentation. Fracture is misinterpreted as a severe ankle sprain.
-
Because of the difficulty in detecting
and defining the extent of a lateral process fracture, a CT scan is
frequently necessary to fully appreciate the extent of injury. -
Less 2 mm displacement: Patients should
have a short leg cast or boot for 6 weeks and be non–weight bearing for
at least 4 weeks. -
More than 2 mm displacement: ORIF is performed using lag screws or wires through a lateral approach.
-
Comminuted fractures: Nonviable fragments are excised.
P.440
Posterior Process Fractures
These involve the posterior 25% of the articular surface
and include the medial and lateral tubercles. Fractures may occur in a
severe ankle inversion injury whereby the posterior talofibular
ligament avulses the lateral tubercle or by forced equinus and direct
compression.
and include the medial and lateral tubercles. Fractures may occur in a
severe ankle inversion injury whereby the posterior talofibular
ligament avulses the lateral tubercle or by forced equinus and direct
compression.
-
Diagnosis of fractures of the posterior
process of the talus can be difficult, in part relating to the presence
of an os trigonum. -
Nondisplaced or minimally displaced:
Patients should have a short leg cast for 6 weeks and be non–weight
bearing for at least 4 weeks. -
Displaced: ORIF is recommended if the
fragment is large; primary excision is performed if the fragment is
small; a posterolateral approach may be used.
Talar Head Fractures
These fractures result from plantarflexion and
longitudinal compression along the axis of the forefoot. Comminution is
common; one must also suspect navicular injury and talonavicular
disruption.
longitudinal compression along the axis of the forefoot. Comminution is
common; one must also suspect navicular injury and talonavicular
disruption.
-
Nondisplaced fractures: Patients should
be placed in a short leg cast molded to preserve the longitudinal arch
and should be partially weight bearing for 6 weeks. An arch support is
worn in the shoe to splint the talonavicular articulation for 3 to 6
months. -
Displaced fractures: ORIF is indicated, with primary excision of small fragments through an anterior or anteromedial approach.
COMPLICATIONS
-
Infection: The risk may be minimized by
early ORIF with soft tissue coverage for open injuries or waiting until
swelling has decreased. -
Osteonecrosis: The rate of osteonecrosis is related to initial fracture displacement:
Hawkins I: 0% to 15% Hawkins II: 20% to 50% Hawkins III: 20% to 100% Hawkins IV: 100% -
Posttraumatic arthritis: This occurs in
40% to 90% of cases, typically related to articular incongruity or
chondral injury at the time of fracture. This may be evident in either
the ankle or subtalar joints. The rates of arthritis in the subtalar
joint, ankle joint, or both joints are 50%, 30%, and 25%, respectively. -
Delayed union and nonunion: Delayed union
(>6 months) may occur in up to 15% of cases. It may be treated by
open reduction and bone grafting. -
Malunion: Commonly varus, this is related
to initial fracture reduction associated with dorsomedial comminution.
Malunion results in subtalar stiffness and excessive weight bearing on
the lateral side of the foot; malunion is frequently painful. -
Open fracture: This complicates up to 15%
to 25% of injuries and reflects the often high-energy mechanism that
produces these fractures. Copious irrigation and meticulous debridement
are necessary to prevent infectious complications. The reported
infection rate for open talus fractures is 35% to 40%. -
Skin slough: This may occur secondary to
prolonged dislocation, with pressure necrosis on the overlying soft
tissues. When severe, it may result in pressure erosion, compromising
soft tissue integrity and resulting in possible infection. -
Interposition of long flexor tendons: This may prevent adequate closed reduction and necessitate ORIF.
-
Foot compartment syndrome: Rare. However,
pain on passive extension of the toes must raise clinical suspicion of
possible evolving or present compartment syndrome of the foot,
particularly in a patient in whom symptoms are out of proportion to the
apparent injury. Emergency fasciotomy is indicated.
P.441 -
Subtalar Dislocation
-
Subtalar dislocation, also known as
peritalar dislocation, refers to the simultaneous dislocation of the
distal articulations of the talus at the talocalcaneal and
talonavicular joints. -
It most commonly occurs in young men.
-
Inversion of the foot results in a medial subtalar dislocation, whereas eversion produces a lateral subtalar dislocation.
-
Up to 85% of dislocations are medial.
-
Lateral dislocations are often associated
with a higher-energy mechanism and a worse long-term prognosis compared
with medial subtalar dislocations.
-
-
All subtalar dislocations require gentle and timely reduction.
-
Reduction involves sufficient analgesia
with knee flexion and longitudinal foot traction. Accentuation of the
deformity is often necessary to “unlock” the calcaneus. Once the
calcaneus is unlocked, reversal of the deformity can be applied.
Reduction is usually accompanied by a satisfying clunk. -
In many cases, a subtalar dislocation is stable following closed reduction.
-
CT scan is useful after closed reduction
to determine whether associated fractures are present and to detect
possible talocalcaneal subluxation. -
A variety of bone and soft tissue
structures may become entrapped, resulting in a block to closed
reduction. With medial dislocations, the talar head can become trapped
by the capsule of the talonavicular joint, the extensor retinaculum or
extensor tendons, or the extensor digitorum brevis muscle. With a
lateral dislocation, the posterior tibial tendon when entrapped
P.442
may present a substantial barrier even to open reduction (Fig. 40.5).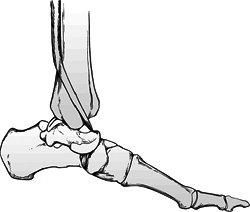 Figure 40.5. Lateral subtalar dislocation with interposed posterior tibial tendon preventing closed reduction.(Adapted from Leitner B. Obstacles to reduction in subtalar dislocations. J Bone Joint Surg Am 1954;36:299.)
Figure 40.5. Lateral subtalar dislocation with interposed posterior tibial tendon preventing closed reduction.(Adapted from Leitner B. Obstacles to reduction in subtalar dislocations. J Bone Joint Surg Am 1954;36:299.) -
Open reduction, when necessary, is
usually performed through a longitudinal anteromedial incision for
medial dislocations and a sustentaculum tali approach for lateral
dislocations. -
Following a short period of immobilization, physical therapy is instituted to regain subtalar and midtarsal mobility.
Total Dislocation of the Talus
-
Total dislocation of the talus is a rare injury, resulting from an extension of the forces causing a subtalar dislocation.
-
Most injuries are open.
-
Initial treatment is directed to the soft tissues.
-
In general, open reduction of the completely dislocated talus is required.
-
Results may be complicated by infection, osteonecrosis, and posttraumatic arthritis.