MENISCUS TEARS
preservation. This has been driven by an enhanced appreciation of the
contributions of the menisci to reducing articular contact stresses and
to stabilizing the joint in concert with the principal ligaments (1,8,22,32,35,46,52).
Of importance has been refinement of the criteria used to select
appropriate treatment (repair, partial resection, or nonintervention)
for the torn meniscus. Technical advances, including instrumentation
for repair and resection, have facilitated both repair and resection. A
promising potential development is the use of biological scaffolds and
growth factors to enhance repair and stimulate meniscal regeneration (6,11,14,27).
Only the peripheral meniscal rim (the red zone) is richly vascularized,
representing approximately 25% of the entire meniscus. The central
meniscus (the white zone) is completely avascular and without healing
potential. A middle area (the gray zone) is in the transitional area
between the periphery and the central meniscus and has limited
potential for healing. Enhancement of healing beyond the red zone
(peripheral 3–4 mm of the meniscus) has been attempted with a variety
of techniques, including fibrin clot interposition, trephination of the
peripheral rim to encourage vascular ingrowth into avascular regions,
and various suture configurations; it has also been attempted
experimentally by using biological scaffolds, cytokines, and other
growth factors (6,11,12,14,26,29,38,42).
collagen accounts for most of the dry composition, providing tensile
strength (21). Other components include
hydrophilic proteoglycans and elastin. Proteoglycans regulate water
content and, therefore, stiffness of the meniscus. Elastin aids in
recovery from meniscal deformation associated with cyclic loading.
to the circumferential bands. This fiber orientation accounts for the
increased pullout strength of vertical mattress sutures compared to
horizontal mattress sutures (42). The surface layer of the meniscus is composed of randomly oriented fibers, which resist splitting and tearing.
Meniscectomy has been shown to significantly decrease contact area and
increase peak pressures. Under loading conditions, total meniscectomy
can cause a fourfold increase in articular surface stresses, partial
meniscectomy increases forces twofold, and repair can restore normal
contact stresses (8,46).
When compressive force is applied to the knee joint, the anterior and
posterior attachments of the meniscus resist extrusion (49).
This converts compressive force into hoop stress, which the
circumferential orientation of the collagen fibers is ideally suited to
withstand. The radial tie fibers and superficial layer resist shear
stresses that attempt to separate the circumferential bundles, which
would result in a vertical longitudinal tear.
limiting anteroposterior (AP) translation of the tibia relative to the
femur. Although isolated sectioning of the meniscus had no effect on
stability, sectioning it in a knee with a deficient anterior cruciate
ligament (ACL) caused a significant increase in AP translation (32).
The contributions of the medial meniscus to stabilizing the knee exceed
those of the lateral meniscus. Other studies have shown a small but
statistically significant increase in varus–valgus laxity after
meniscectomy (35). These reports confirm the function of the meniscus as a secondary stabilizer.
rotational force applied to the weight-bearing knee that overloads the
meniscus. Degenerative tears occur from repetitive submaximal forces
applied to a meniscus having already undergone attritional wear from an
irregular femoral articular surface; the majority involve the medial
meniscus (39). Concomitant meniscal injury
often accompanies tears of the ACL as well as multiple knee ligament
injuries including dislocation of the knee. Whereas lateral meniscus
injuries are most frequent in acute ACL tears, the medial meniscus is
most often torn in chronic ACL insufficiency. In combined ACL and
medial collateral ligament (MCL) injuries, meniscus tears occur less
frequently with complete MCL tears (grade III) than with partial tears
(grade II) and, in both instances, predominantly affect the lateral
meniscus (48).
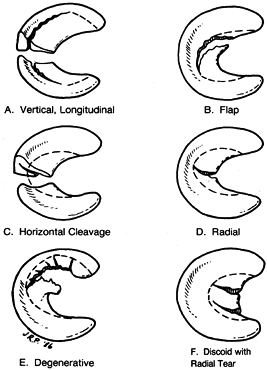
acuity, and location. The most common tears are vertical longitudinal
(bucket-handle), oblique (flap), radial, horizontal cleavage, and
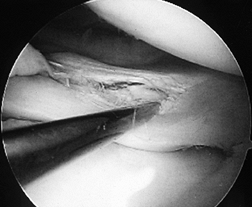
complex (Fig. 85.1). Most tears involve the posterior aspect of the meniscus. Tears are usually
complete, traversing the entire surface of the meniscus, but they may
be incomplete, affecting only the inferior or superior surface of the
meniscus (Fig. 85.2; see also COLOR FIG. 85.2).
 |
|
Figure 85.1. Types of meniscal tears, shown with the typical lines of resection.
|
 |
|
Figure 85.2. (See COLOR FIG. 85.2) Incomplete tear of the superior surface of the lateral meniscus associated with an anterior cruciate ligament tear.
|
loading and rotation of the knee and may be accompanied by mechanical
symptoms of catching, popping, giving-way, swelling, and locking. The
patient may describe relief of symptoms with manual reduction of the
displaced meniscal fragment. In the arthritic knee, it is useful to
distinguish between patients with pain only and those with pain
associated with one or more mechanical symptoms. In the absence of
mechanical symptoms, it is unlikely that resection of a degenerative
tear will give significant pain reduction.
assessment of limb alignment, gait pattern, and hip function,
especially in the older patient who might have hip pain referred to the
medial knee. Fowler and Lubliner delineated predictive criteria for
meniscus tears (25). The most specific findings
of a meniscus tear are a positive McMurray’s test and block to
extension. Unfortunately, the McMurray’s test is the least sensitive
test. Although joint line tenderness is very sensitive for a meniscus
tear, it is the least specific test, especially in the presence of an
acute ACL injury. Some patients will exhibit an effusion, and many will
demonstrate pain with forced knee flexion as well as forced extension
(spring or bounce test).
imaging (MRI) on a case-by-case basis. For patients over the age of 40,
perform AP weight-bearing radiographs in addition to a lateral view of
the knee to exclude degenerative joint disease (DJD), loose bodies,
osteonecrosis, and tumor. Take additional views such as a Merchant view
to evaluate the patellofemoral joint, a notch view to look for loose
bodies, and a weight-bearing PA in 45° of flexion to diagnose early DJD
on an individual basis.
is a tremendous asset, with an overall accuracy approximating 90%. If
cost were not a consideration, MRI would be routine in every patient as
an adjunct to, but not as a substitute for, a thorough physical and
adequate radiographic examination. In this day of managed care, many
patients are referred who have classic symptoms, a confirmatory
physical examination, and an MRI of the knee, but no radiographs. In
our practices, we do not routinely order MRI for patients with a locked
knee, a positive McMurray’s, or symptoms and findings suggestive of a
meniscus tear who have not responded to nonoperative treatment. In our
experience, these patients have sufficient indication for proceeding
directly to arthroscopy.
patients with a type II signal (incomplete tear) have been found to
have complete tears at arthroscopy (23). In
addition, MRI is infrequently helpful in the previously operated
meniscus to assess either healing after repair or reinjury in the
patient with previous partial meniscectomy.
consistent with a meniscus tear, but with no history of locking, a
block to extension, or ACL injury, can be treated nonoperatively with
resolution of symptoms (33). Usual measures
include nonsteroidal anti-inflammatories, a neoprene sleeve,
muscle-strengthening exercises for the lower extremity, and sometimes a
formal course of physical therapy. For patients with continuing
symptoms, arthroscopic intervention is indicated.
partial-thickness tears, incomplete radial tears, and stable vertical
longitudinal tears less than 10 mm in length do not need resection.
Shelbourne has shown that in patients undergoing ACL reconstruction,
these tears remain asymptomatic and do not progress (24).
meniscectomy. The goal of partial meniscectomy is to remove only the
unstable or pathologic portion, leaving as much healthy meniscal tissue
as possible while avoiding an abrupt transition to the remaining
meniscus. Partial meniscectomy is indicated for radial tears not
extending to the periphery, oblique tears, horizontal cleavage tears,
degenerative tears, and irreparable vertical longitudinal tears that
are more than 5 mm from the absolute periphery.
-
See Chapter 84 for the general principles of arthroscopy.
-
Portal placement is of primary importance
in performing partial meniscectomy. With the arthroscope in the
inferolateral portal, use a spinal needle to identify proper placement
of the inferomedial portal and any accessory portals. The inferomedial
portal for medial meniscectomy typically is just inferior to the level
of the inferolateral portal and is made with the knee positioned
P.2302
in
near extension with valgus and external rotation applied to visualize
the posterior third of the meniscus, or in more flexion to visualize
the anterior horn. If the spinal needle cannot be advanced to palpate
the torn meniscus, the portal is not satisfactory. Choose either a more
medial location immediately anterior to the MCL or an inframeniscal
approach. If the posterior horn cannot be exposed without injury to the
femoral condyle, use a posteromedial portal: With the arthroscope in
the posteromedial compartment, pass through the intercondylar notch. -
If a lateral tear is encountered, make
the inferomedial portal with the leg in the figure-four position. This
needs to be at a higher level than the inferolateral portal to allow
instruments to pass freely above the tibial spines. For posterior tears
of the lateral meniscus, instrumentation is usually necessary through
the inferolateral portal because of the tighter radius of curvature of
the lateral meniscus, which limits access from the inferomedial portal. -
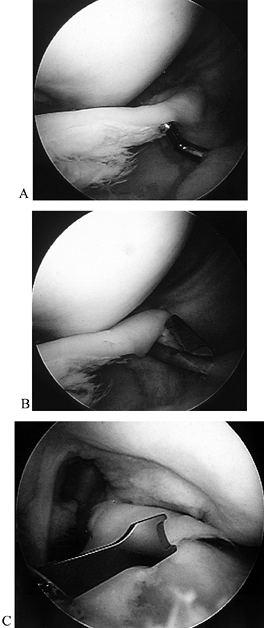
Once appropriate portals are established, resect using a combination of hand instruments and a motorized shaver (Fig. 85.3).
Simple flaps and longitudinal tears can often be excised intact, using
an arthroscopic knife or scissors to detach the segment. Debride most
tears in a piecemeal fashion. A small up-biting punch, straight punch,
right and left 90° punches, and a 4.5 mm full-radius resector will
suffice for resection of most tears.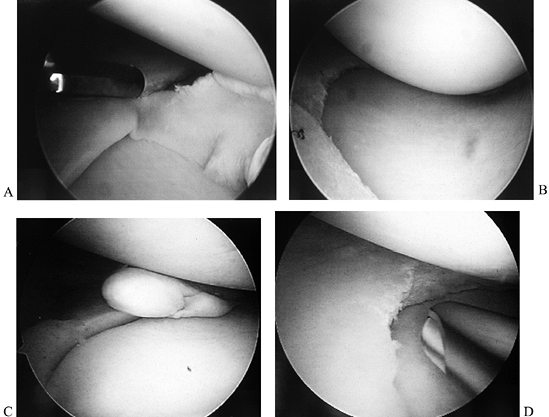 Figure 85.3. A,B: Knife resection of flap tear. C,D: Motorized resection of flap tear.
Figure 85.3. A,B: Knife resection of flap tear. C,D: Motorized resection of flap tear. -
After resecting the meniscal tear, pass
the arthroscope via the notch into the posterior compartments to ensure
that all loose meniscal fragments have been removed. -
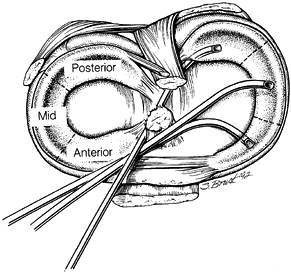
Use a three-portal technique to treat vertical longitudinal (bucket-handle) tears displaced into the notch (Fig. 85.4A; see also COLOR FIG. 85.4).
For a medial meniscus tear, insert the arthroscope in the inferolateral
portal as usual. Establish two inferomedial portals, using a spinal
needle for localization. Place one portal either adjacent to the
patellar tendon or through the patellar tendon. Make a second portal 2
cm medial to the first, taking care to enter just over the rim of the
meniscus so that instruments can reach the posterior horn. Insert
P.2303
an
angled arthroscopic scissors or a curved knife through the second
portal, sectioning the anterior horn attachment in a tapered fashion (Fig. 85.4B).
Switch the arthroscope to the inferomedial portal, and grasp the
meniscus via the inferolateral portal. Now release the posterior extent
of the tear with a small up-biter or meniscal knife through the
anteriormost inferomedial portal or the transtendon portal (Fig. 85.4C).
Smooth the margins using a 4.5 mm motorized shaver. Switch the
arthroscope to the medial side and, with the shaver lateral, trim any
remaining anterior irregularity, if needed.![]() Figure 85.4. (See COLOR FIG. 85.4) A: Displaced bucket-handle tear of the medial meniscus. B: Anterior horn of bucket-handle tear detached. C:
Figure 85.4. (See COLOR FIG. 85.4) A: Displaced bucket-handle tear of the medial meniscus. B: Anterior horn of bucket-handle tear detached. C:
Grasping the resected anterior horn through an inferolateral portal and
arthroscopic meniscotome inserted through a transtendon portal to
resect the posterior attachment (viewed from inferomedial). -
Deal with nondisplaced bucket handle
tears the same way, or via a two-portal technique. If you use the
latter, cut the posterior horn attachment via an ipsilateral portal,
using a small up-biter, and leave a narrow bridge attached. Then divide
the anterior horn attachment from whichever portal affords the best
access. Remove the meniscus by avulsing the small remaining attachment
of the posterior horn. Taper the margins to a smooth contour with
punches and a motorized shaver.
for 24–72 hours postoperatively to minimize swelling and attendant
pain. Implement early isometric quadriceps exercises and range of
motion without load when discomfort permits. Within a few days to 1
week after surgery, begin progression to unaided walking, cycling, and
short-arc quadriceps exercises. Once the incisions are healed, swimming
can be started. Normal activities can usually be resumed within 2–3
weeks but may take as long as 6 weeks. If the tear was complex or
degenerative, defer running, squatting, and other stressful activities
for a minimum of 3–4 weeks. Physical therapy can be beneficial to
achieve an earlier return to activity, but it is not mandatory.
complete or partial meniscectomy remained the treatment of choice of
the vast majority of orthopaedists until the early 1980s. Interest in
repair has been stimulated by DeHaven’s work on open meniscal repair (16,17 and 18) and Henning’s inside-out arthroscopic repair (28,29). Since that time, numerous basic and clinical science reports have validated the concept of meniscal repair (2,20,30,36,37,41,43,44).
Accepted techniques include open repair, inside-out arthroscopic
repair, outside-in arthroscopic repair, and all-inside repair.
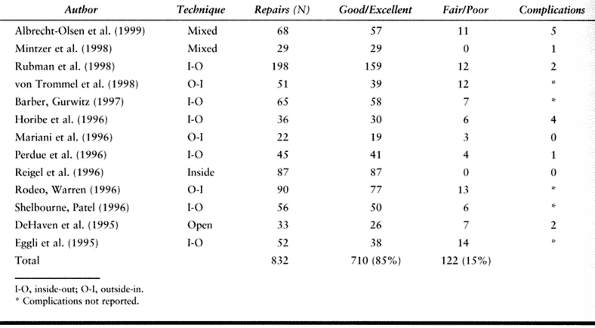
rates of meniscal repair are similar, based on an average of published
reports (2,9,18,20,30,34,36,37,41,43,47,51), with an overall healing rate of nearly 85% (Table 85.1). Interstudy comparisons are difficult due to varied
techniques, as well as differences in types of tears, patient data,
associated injuries, and postoperative assessment criteria. For
instance, clinical success rates based on symptoms and function exceed
anatomic healing rates (34,45).
 |
|
Table 85.1. Results of Meniscal Repair
|
pattern, and age of the tear; quality of meniscal tissue; patient age;
associated injuries; as well as surgical skill.
periphery) and most in the gray zone (3–5 mm from the periphery). We
repair only nonmacerated, nondeformed fragments in the gray zone. While
recent work by Rubman et al. (44) has shown acceptable results from repair of tears in the white zone, this is not yet widely practiced.
Similarly, we treat with partial meniscectomy those chronic tears that
involve a meniscal deformity that precludes a functional repair.
the age of 45 years. Over this age, we do repairs in some patients on a
case-by-case basis, depending primarily on functional activity level,
physiologic age, and willingness to follow a more lengthy and rigorous
postoperative management protocol as contrasted to partial
meniscectomy. Some older patients may elect partial meniscectomy to
allow an earlier return to activity.
technique must be selected. Technical aspects of the two most popular
arthroscopic methods are presented.
placement of sutures while protecting neurovascular structures by
incorporating an accessory incision.
-
Use either a rasp or small shaver to
debride the tear margins to achieve smooth meniscal surfaces and
excoriate the adjacent synovial tissue to produce slight bleeding. -
Make an accessory posteromedial or
posterolateral incision to expose the capsule. For a medial tear,
transilluminate the posteromedial knee through the notch to identify
the saphenous vein, which travels with the nerve. Make a 3 cm
longitudinal incision posterior to the MCL, centered just below the
joint line (to accommodate the needles that will pass from superior to
inferior). Retract the pes tendons posteriorly, along with the
saphenous vein and nerve. Dissect the interval between
P.2305
the
joint capsule and the medial head of the gastrocnemius, and insert a
small vaginal speculum or commercially available specialized retractor
into this interval to expose the posterior capsule while protecting the
posterior neurovascular structures. The retractor will deflect needles
exiting the joint, allowing easy retrieval. -
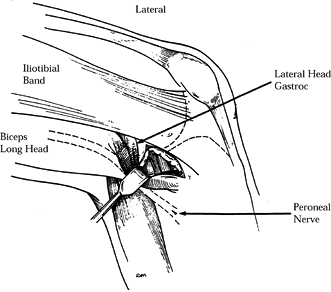
On the lateral side, make the incision along the posterior aspect of the lateral collateral ligament (Fig. 85.5)
with the knee flexed approximately 90°. Develop the interval between
the biceps femoris posteriorly and the iliotibial band anteriorly.
Separate the lateral head of the gastrocnemius from the joint capsule.
Insert the retractor in front of the lateral gastrocnemius to protect
the adjacent peroneal nerve.![]() Figure 85.5.
Figure 85.5.
Exposure of posterolateral capsule. Note that retractor must be placed
in front of the lateral head of the gastrocnemius to protect the
peroneal nerve. -
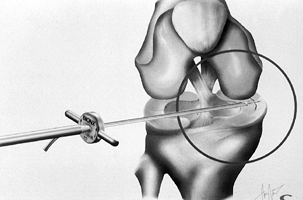
As with an all-inside repair (technique
below), portal placement must allow the cannula to be placed
perpendicular to the tear and horizontal to the joint line. This
usually requires placement of sutures into the meniscus from the
contralateral portal while viewing from the ipsilateral portal.
Placement of the cannula in the contralateral portal also tends to
angle the penetrating needle away from the popliteal region (Fig. 85.6). Because of the curvature of the meniscus, it is helpful to utilize cannulas of various angles (Fig. 85.7). A single cannula is preferable because it allows greater flexibility in placing the second arm of the stitch.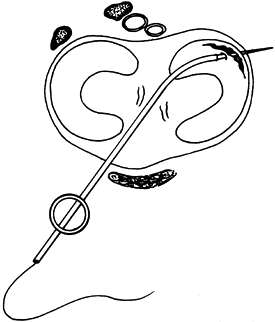 Figure 85.6. A curved cannula inserted through the contralateral portal is used for suturing to avoid popliteal vessels and nerves.
Figure 85.6. A curved cannula inserted through the contralateral portal is used for suturing to avoid popliteal vessels and nerves.![]() Figure 85.7. Zone-specific cannulas for meniscus repair.
Figure 85.7. Zone-specific cannulas for meniscus repair. -
For medial tears, position the knee near
extension to facilitate passage of the needles into the posterior
meniscus and to preserve the posterior capsular fold. For lateral
tears, position the knee in flexion to avoid injury to the peroneal
nerve, and insert a retractor in front of the lateral head of the
gastrocnemius. -
Starting posteriorly, insert the
appropriate curved cannula and advance a 10-inch needle with attached
suture [2-0 nonabsorbable provides sufficient tensile strength (10)]
to engage the torn fragment and reduce it to the margin. With the
posterior retractor in place, push the needle through the meniscus
margin posteriorly. Visualize the needle’s exit before continuing to
push it out of the posterior incision or using a needle driver to grasp
and deliver it. Place the second needle vertically (42)
P.2306
with a 3 mm bridge between arms (Fig. 85.8).
Place as many sutures as necessary, maintaining a 5 mm interval between
sutures. Then tie the sutures directly over the exposed capsule. If
concomitant ACL surgery is being performed, delay tying the sutures
until after the surgery is completed. Release the tourniquet to allow
blood to fill the meniscal repair site and then tie the sutures.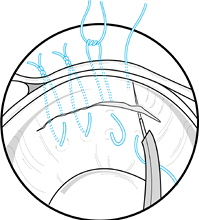 Figure 85.8. Vertical mattress sutures placed through a cannula.
Figure 85.8. Vertical mattress sutures placed through a cannula. -
For tears with an extreme anterior
component, an outside-in suturing technique utilizing commercially
available, modified spinal needles and suture passers can facilitate
repair by allowing more precise needle placement.
decreases operative time and complications; and its healing rates are
similar to those of inside-out repair (2,19).
We use a meniscal arrow system (Bionx Implants, Blue Bell, PA). The
arrow is made of a biodegradable polylactic acid that resorbs over a
3-year period. The implant has a barbed shaft with a 4 mm T-head, and
it comes in 10 mm, 13 mm, and 16 mm lengths (Fig. 85.9).
The barbs are perpendicular to the T-head to obtain maximum purchase in
the circumferential fibers of the meniscal body. Pull-out strength of
the arrow has been shown to be equivalent to horizontal mattress
sutures (2,12). The
instrumentation set contains five different cannulas with varying
curvatures, allowing access to all regions of the meniscus (Fig. 85.10).
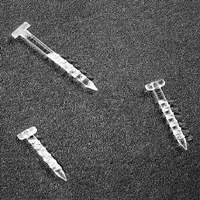 |
|
Figure 85.9. Bionx meniscal arrows. Note that barbs are perpendicular to the T-head.
|
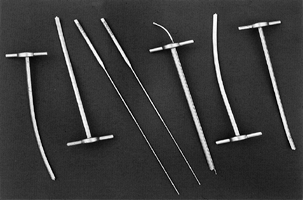 |
|
Figure 85.10. Bionx instrumentation set, including curved cannulas.
|
-
Prepare the tear margins as described
above. Occasionally, it may be necessary to rasp the posterior horn of
the medial meniscus from a posteromedial portal to avoid injuring the
medial femoral condyle. Use a probe to estimate the necessary arrow
length. Whenever possible, use 13 or 16 mm long arrows, because of
their higher pullout strength (12). -
Insert the appropriately curved cannula
parallel to the joint line and perpendicular to the tear to obtain
optimum fixation. Posterior tears are best addressed with the cannula
in the ipsilateral portal, while tears in the midportion require that
the cannula be inserted through the contralateral portal. -
Use the cannula to hold the meniscus in a
reduced position so that the arrow can enter the meniscus 3–4 mm from
the tear. Insert the “spear” into the cannula, pushing it through the
meniscus until its handle is seated, preparing a channel for the arrow (Fig. 85.11).![]() Figure 85.11. Cannula holds the reduction, while a “spear” is used to create a channel for the arrow.
Figure 85.11. Cannula holds the reduction, while a “spear” is used to create a channel for the arrow. -
Remove the spear and insert the
appropriate-length arrow into the cannula. Now push the arrow down the
cannula and across the tear. Be certain to push the inserter all the
way down against the back of the cannula to ensure that the head of the
arrow is countersunk into the meniscus. If removal of an arrow is
necessary,
P.2307
rotate
it 90° with a grasper (T-head perpendicular to tibia) prior to removal.
This will reduce meniscal trauma by disengaging the barbs from the
circumferential fiber bundles. -
For posterior tears, place the most
posterior arrow first, followed by an arrow in the center of the tear.
If the tear is in the midportion of the meniscus, place the first arrow
centrally with subsequent arrows in the anterior and posterior extents
of the tear. Place arrows every 5 mm (Fig. 85.12).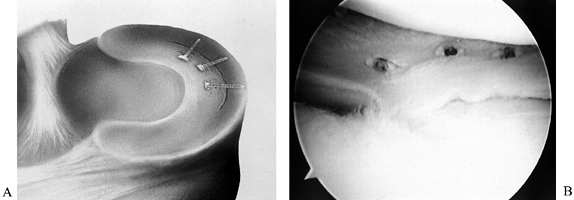 Figure 85.12. Arrows stabilizing a vertical tear.
Figure 85.12. Arrows stabilizing a vertical tear.
motion and no weight bearing for several weeks after surgery, with a
delay of 6 months or more to resume sports (16,29).
Over the past several years, restrictions on patient activities after
meniscal repair have eased considerably. Based on experimental and
clinical studies, postoperative rehabilitation has progressed to early,
full-weight-bearing, unlimited motion without bracing, and return to
sports as soon as normal strength, motion, and flexibility are achieved
(9,47).
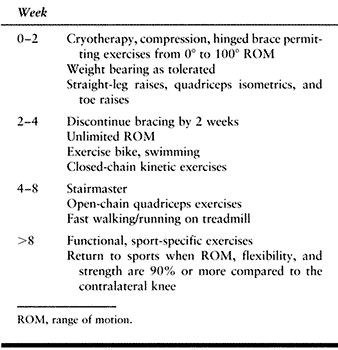
ACL surgery, we follow the rehabilitation program for the cruciate
ligament (see Chapter 89). When isolated
meniscal repair has been performed in an acute tear where satisfactory
apposition and fixation have been achieved, we use a modified
accelerated protocol with a short, initial period of bracing (Table 85.2). Encourage early use of a stationary bicycle and isokinetic exercises, but avoid
squatting and pivoting for 2–3 months. In our experience, return to
full activity usually takes 3–4 months. If a patient develops pain or
effusion, slow down or regress activity until symptoms subside. If
symptoms do not resolve, investigate further (using arthrogram or
arthroscopy) to evaluate the knee.
 |
|
Table 85.2. Postoperative Management for Meniscal Repair
|
block to extension, or associated ACL and meniscus tear can be
associated with articular degeneration (50).
Complications of open or arthroscopic meniscus surgery include failure
to heal or retear after meniscal repair, neurovascular injury,
hemarthrosis, deep vein thrombosis, reflex sympathetic dystrophy,
infection, iatrogenic injury to intraarticular structures, especially
the femoral condyles, osteonecrosis, and DJD (7,31,40).
is knee stability. In knees with concomitant ACL reconstruction,
meniscal healing rates are approximately 90% to 100%. This contrasts
sharply with success rates as low as 30% in the ACL-deficient knee (53).
In isolated meniscal injury, healing rates are less than those observed
in the knee undergoing simultaneous ACL reconstruction, but, as noted
previously, they average 85%.
While permanent injury is rare, a neuroma can occur, producing pain and
numbness. With lateral meniscal repair, the peroneal nerve is at risk
with any inside-out technique. Complications associated with meniscal
arrows include pain secondary to prominent arrow tips, as well as
breakage of arrows during insertion. A recent randomized study with 68
patients compared arrows to inside-out suture repair. Two infections
occurred in the suture group and none in the arrow group; five patients
had saphenous nerve pain in the suture group, compared to two in the
arrow group (2).
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
P, Kristensen G, Burgaard P, et al. The Arrow vs. Horizontal Suture in
Arthroscopic Meniscus Repair. A Prospective Randomized Study with
Arthroscopic Evaluation. Knee Surg Sports Traumatol Arthrosc 1999;7:268.
P, Lind T, Kristensen G, Falkenberg B. Failure Strength of a New
Meniscus Arrow Repair Technique: Biomechanical Comparison with
Horizontal Suture. Arthroscopy 1997;13:183.
ME, Fu FH, Mengato R. Meniscal Tears: The Effects of Meniscectomy and
of Repair on Intraarticular Contact Areas and Stress in the Human Knee:
A Preliminary Report. Am J Sports Med 1986;14:270.
UW, Faber KJ, Ciarelli M, et al. Pull-out Strength and Stiffness of
Meniscal Repair Using Absorbable Arrows or Ti-Cron Vertical and
Horizontal Loop Sutures. Am J Sports Med 1999;27:626.
RD, Shelbourne KD. “Aggressive” Non-treatment of Lateral Meniscal Tears
Seen During Anterior Cruciate Ligament Reconstruction. Am J Sports Med 1995;23:156.
J, Kurosaka M, Yoshiya S, et al. Meniscal Repair Using Fibrin Sealant
and Endothelial Cell Growth Factor: An Experimental Research Study in
Dogs. Am J Sports Med 1992;20:537.
JW, Elliot JS, Lietner T, et al. The Effects of Arthroscopic Partial
Lateral Meniscectomy in an Otherwise Normal Knee: A Retrospective
Review of Functional, Clinical, and Radiographic Results. Arthroscopy 1995;11:29.
PP, Santori N, Adriani E, Mastantuono M. Accelerated Rehabilitation
after Arthroscopic Meniscal Repair: A Clinical and Magnetic Resonance
Imaging Evaluation. Arthroscopy 1996;12:680.
WR, Akers SR, Kish V. Load to Failure of Common Meniscal Repair
Techniques: Effects of Suture Technique and Suture Material. Arthroscopy 1997;13:731.
BB, Hargreaves DJ. Transmission of the Load in the Knee Joint with
Special Reference to the Role of the Menisci. Part II: Experimental
Results, Discussion and Conclusions. Eng Med 1979;8:220.
Trommel MF, Simonian PT, Potter HG, et al. Different Regional Healing
Rates with the Outside-in Technique for Meniscal Repair. Am J Sports Med 1998;26:446.