Nerve Stimulators and Insulated Needles
locate the brachial plexus was recorded by Perthes in 1912. However,
the acceptance of this method to aid in performance of peripheral nerve
blocks was not realized until the 1960s when electronic advances and
the consequent introduction of more convenient solid-state units were
made. Greenblatt and Denson demonstrated that motor nerves can be
stimulated without eliciting pain and that the current required to
stimulate the nerve depends on the distance between the needle and the
target nerve. In the last two decades, peripheral nerve stimulation
techniques have largely replaced paresthesia techniques for most major
conduction blocks, particularly in lower extremity blockade. This
approach is well accepted and is associated with favorable success
rates. It is important to realize that nerve stimulators are not used
as a replacement for the sound knowledge of anatomy, but to help to
position the needle in closer proximity to the nerve without a required
contact with the nerve (paresthesia) and with less discomfort to the
patient.
threshold stimulus must be applied to the nerve. The ability to
stimulate a nerve depends on the intensity of the current applied and
the duration of the current. In mixed nerves it is possible to
stimulate the motor component without eliciting pain by limiting the
current intensity and duration. To stimulate motor fibers, a current of
shorter duration (0.05 to 0.2 ms) is typically used. The use of a
shorter pulse duration increases the likelihood of an increased
proximity between the nerve fibers and the unshielded tip of the
needle, but makes the localization of the nerve more challenging.
Consequently, the nerve stimulator is usually set up with a current of
1 to 1.5 mA and a pulse duration of 0.1 to 0.3 ms. The intensity of the
current is decreased along with the pulse duration to adjust the
position of the needle. In contrast, the stimulation of sensory fibers
requires longer pulse duration time (0.3 to 1.0 ms) than do motor
fibers (0.05 to 0.1 ms). With such a setup it is possible to locate
sensory nerves such as the radial nerve at the wrist, the lateral
femoral cutaneous nerve, and the saphenous nerve by eliciting
electrical paresthesia. The use of longer pulse duration is appropriate
in patients with peripheral neuropathy, including diabetic patients. In
these patients it is often necessary to
stimulate
with a pulse duration time of 0.3 to 1.0 ms to elicit a motor response.
The access to multiple pulse duration times represents a major
improvement of the nerve stimulator presently available. An important
principle of peripheral nerve stimulation is the preferential “cathodal
stimulation.” In other words, when the nerve is stimulated by an
electrode, significantly less current is required to obtain a response
to a nerve stimulation when the cathode (negative) rather than the
anode (positive) is adjacent to the nerve. This principle has
significant clinical applications, and it requires that clinicians pay
particular attention to the polarity of the electrodes. Another
fundamental principle is that the current intensity required to
stimulate the nerve is in relationship to the distance of the needle
from the nerve. As the stimulating tip moves away from the nerve, the
relationship between the current and the distance from the nerve is
governed by Coulombs law:
the needle–nerve distance. This principle is used to estimate
needle–nerve distance by employing a stimulus of known intensity and
pulse duration. It should be noted that this relationship is not
linear, which means that as the needle–nerve distance increases, a
current of substantially greater intensity is required to stimulate the
nerve.
stimulator-assisted nerve block techniques assume that nerve
stimulators are accurate and user-friendly to maneuver during block
performance. Skin resistance, electrode surface resistance, and gel
conductivity can vary widely. For these reasons, nerve stimulators for
use in regional anesthesia should be specifically engineered for that
application, rather than be an “all-purpose” unit with neuromuscular
block monitoring capabilities. A plethora of features present on some
units does little to facilitate their use and adds to the complexity of
their operation. Some of the desirable characteristics of nerve
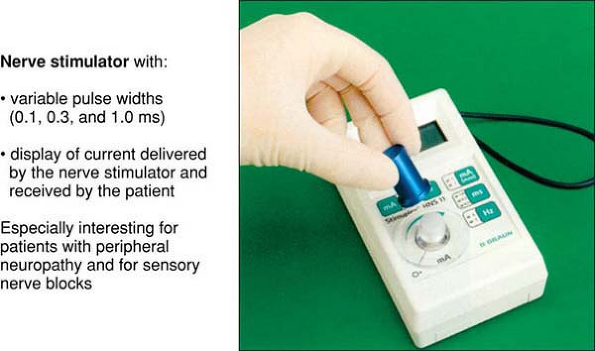
stimulators for regional blocks are outlined here (Fig. 2-1).
 |
|
Figure 2-1.
HNS-12 Nerve Stimulator. Variable pulse widths of 0.1, 0.3, and 1.0 ms. Displays current delivered by the nerve stimulator and received by the patient. Especially interesting for use on patients with peripheral neuropathy and for sensory nerve blocks. |
-
Current intensity—It is important that the nerve stimulator deliver accurate current over a range of 0 to 5 mA.
-
Variable pulse duration time—To
allow for stimulation of motor as well as sensory nerves in patients
with normal nerve conduction and peripheral neuropathy, the nerve pulse
duration time should be variable rather than fixed. -
Constant current output—This
feature allows for an automatic compensation of the voltage output when
tissue or connection impedance changes during nerve stimulation,
ensuring accurate delivery of the specified current. -
Current meter—It
is important that the current display indicates both the current
delivered by the nerve stimulator and the actual current delivered to
the patient. The currents should be similar. -
Current intensity control—Whatever
means to control the current are used, it is important that the current
can be easily and conveniently adjusted during block performance. Some
newer units, which incorporate a remote control of the current, are
also being introduced. This feature allows a single operator to perform
the block by controlling the intensity of the current using a foot
pedal or a hand-controlled device. -
2-Hz stimulating frequency—While
many nerve stimulators currently in clinical use feature 1-Hz
stimulation, 2-Hz stimulation is clinically much more advantageous,
since it allows faster manipulation of the needle. -
Disconnect indicator—This feature alerts the operator when the stimulus is not being delivered due to a disconnection or unit problem.
-
Digital display—This
feature allows the operator to monitor the intensity of the current
delivered by the nerve stimulator to the patient, and the frequency and
the pulse duration used.
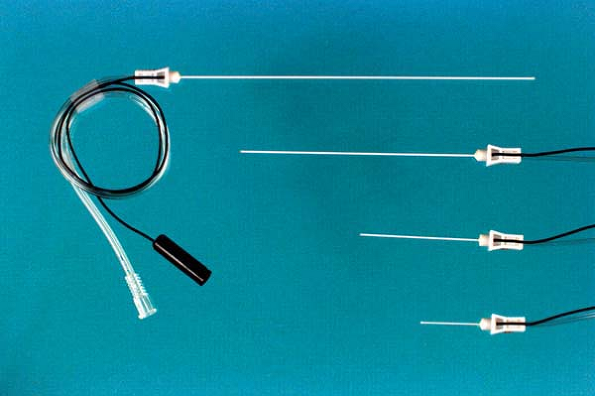
The negative electrode of the nerve stimulator is connected to the
insulated needle while the positive electrode of the nerve stimulator
is connected to an electrocardiogram electrode serving as a ground
electrode. There are different sizes of needles and, for some sizes,
different gauges. Although the most appropriate angle at the tip
remains the object of some debate (15° vs. 30°), the size and the gauge
of the needle for a given block should be chosen according to the
approach and the patient population (e.g., adult vs. pediatric, larger
patients vs. smaller patients). Thus a 22-gauge, 2.5-cm needle is
indicated for an interscalene block in adults, whereas in children a
25-gauge, 2.5-cm
needle
is preferred for the same block. The use of a longer needle (up to 5
cm) may also be indicated in morbidly obese or very muscular patients.
Although some experts prefer the use of a 5-cm needle to perform an
interscalene block, as a rule of thumb, for less-experienced
practitioners, the shortest recommended needle is generally safest and
should be preferred. Insulated needles are usually available in lengths
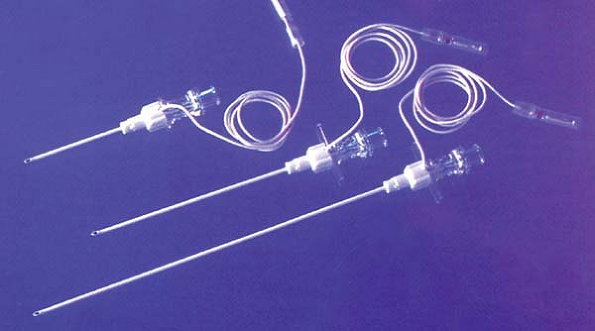
from 2.5 to 15 cm. In addition, for the placement of perineural
catheters for continuous nerve block techniques the use of an insulated
introducer Tuohy needle is frequently preferred (Fig. 2-3).
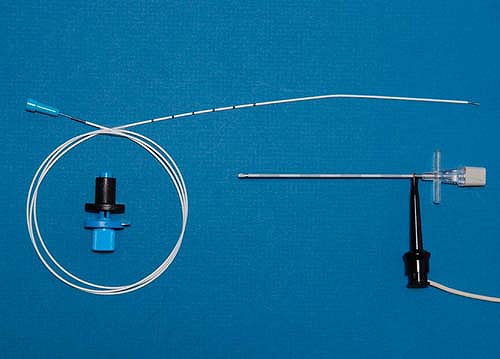
Although the use of a stimulating stylet for the placement of a
perineural catheter was described as early as 1951, the use of a
stimulating catheter (Fig. 2-4) has only recently been introduced clinically.
 |
|
Figure 2-2. Insulated beveled needles commonly used in combination with a nerve stimulator for single nerve blocks.
|
 |
|
Figure 2-3. Insulated introducer Tuohy needle.
|
needles to perform peripheral nerve blocks, including transarterial
(axillary) and paresthesia techniques (interscalene and axillary), and
field blocks (median and radial nerve blocks at the wrist and fascia
iliaca block). For the fascia iliaca block, the use of a Tuohy needle
in adult patients facilitates the performance of the block by allowing
a better feeling of the needle going through the fasciae lata and
iliaca.
 |
|
Figure 2-4. Stimulating catheter.
|
C, Raj P, Ford D. The use of peripheral nerve stimulators for regional
anesthesia: a review of experimental characteristics, technique, and
clinical applications. Reg Anesth 1985;10:49–58.
