Retrobulbar Block
II – Single-Injection Peripheral Blocks > C – Miscellaneous Blocks
> 18 – Retrobulbar Block
Anesthesia for the majority of surgical procedures in and around the
eye (e.g., cataract extraction, glaucoma filtering procedures, iris
surgery, trans-par-plana vitrectomy, or orbital exploration [combined
with second injection in the superior nasal quadrant]).
The proper technique begins with the patient’s arrival for surgery.
Apprehension in anticipation of eye surgery is common and should be
expected. The concept of a needle being stuck behind the eye is
frightening; therefore, sedation should be given upon arrival and not
delayed until just before administration of the retrobulbar injection.
Patients need to have their fears allayed during the preparation and
waiting period and not so much at the actual time of the injection,
which if done properly causes little pain.
and strict attention to detail minimizes the risk for complications.
Instruct the patient to keep both eyes open and to look straight ahead.
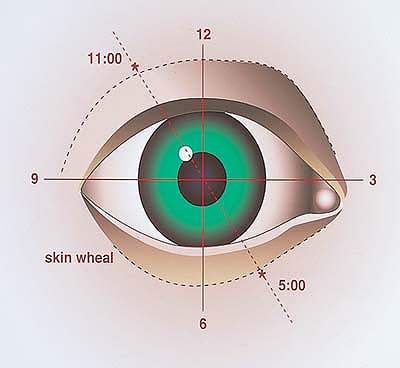
Visualize the globe and orbit as divided into four quadrants (Fig. 18-1).
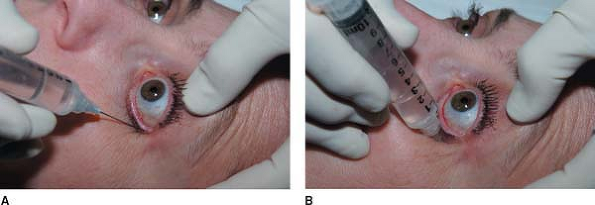
Using a 30-gauge short needle and a 10-cc syringe containing the
anesthetic agent, raise a skin wheal 8 to 10 mm posterior to the lid
margin so as to be inferior to the tarsal plate and in the center of
the inferior temporal quadrant (Fig. 18-2A).
Without being withdrawn, the needle is turned and directed through the
skin, posteriorly toward the back of the orbit without angulation. It
is inserted to the hilt, and with the laxity of the lid and further
posterior pressure, the hilt indents the lid, thereby advancing the
needle tip past the equator of the globe and into the retrobulbar
space. During insertion of the needle, approximately 2 mL of anesthetic
agent is injected, and the needle is then withdrawn. Moderate digital
pressure
is applied to the globe and orbit through the closed lid for
approximately 3 to 5 minutes. A 27-gauge, 31-mm disposable needle is
placed on the same syringe, and the lower lid is immobilized by the
needle tip so that it is at the level of the equator of the globe prior
to penetrating the skin (Fig. 18-2B).
The needle is guided along the previously anesthetized tract, angulated
only slightly toward the apex of the orbit, and advanced carefully to
the hilt and into retrobulbar space. After negative aspiration for
blood, 5 to 7 mL of the local anesthetic mixture is injected. In the
case of trans-par-plana vitrectomy or orbital exploration, a complete
akinesia of the extraocular muscles and total anesthesia is indicated.
This may require a supplemental injection in the superior nasal
quadrant. For that purpose, the same 27-gauge, 31-mm needle is
introduced at the level of the skin of the upper lid just below the
superior orbital rim at the 1:30 position (Fig. 18-3). The needle is
directed posteriorly along the roof of the orbit to a depth of 2.5 cm,
where an additional 2 to 3 mL of anesthetic solution is injected. It is
important not to slant the needle toward the apex of the orbit since
the optic nerve is nasally located in the orbit and may be damaged.
 |
|
Figure 18-1. Visually partition the globe and orbit into four quadrants.
|
 |
|
Figure 18-2. A:
Using a 30-gauge needle and a 10-cc syringe containing the anesthetic agent, raise a skin wheal 8 to 10 mm posterior to the lid margin so as to be inferior to the tarsal plate and in the center of the inferior temporal quadrant. B: A 27-gauge, 31-mm disposable needle is placed on the same syringe, and the lower lid is immobilized by the needle tip so that it is at the level of the equator of the globe prior to penetrating the skin. |
 |
|
Figure 18-3. Supplemental injection at the superior nasal quadrant.
|
-
In addition to sedation to alleviate fear
and apprehension, calm discussion and authoritative reassurance on the
part of the person administrating the anesthesia is most helpful.
Touching the patient (e.g., holding the hand or shoulder) during this
preinjection talk adds to the bonding and trust, which is an important
aspect of reassurance. The syringe and needle should be concealed from
view and not brandished in front of the patient’s face. Words like
“stick,” “hurt,” “pain,” and “sting” should be avoided. Nonspecific
terminology should be used, such as, “I’m going to give you a little
medicine now,” or, “You may feel this for a few seconds,” or “You may
feel some burning here.” A steady stream of conversation in a low, calm
voice is most effective in allaying fear. Use phrases and ask questions
such as, “How are you doing?”; “Do you need anything?”; “You’re doing
fine”; “Can I do anything for you?”; “How did you sleep last night?”;
“Do you have any questions?”; and “We’re going to take good care of
you.” -
The skin wheal burns for approximately 5 seconds and requires vocal reassurance, such as “it only burns for a few seconds.”
-
The skin wheal must be in the proper
position so that the 30-gauge needle, which is advanced posteriorly,
passes below the tarsal plate. -
For short procedures of less than 30
minutes, lidocaine is satisfactory. For longer procedures, a mixture of
50% lidocaine and 50% bupivacaine will prolong anesthesia. -
The addition of epinephrine also prolongs the duration of the block.
-
The addition of hyaluronidase shortens the onset of the block and enhances the spread of the agent through the tissue.
-
Neither hyaluronidase nor epinephrine is necessary in most cases.
-
The use of sedation at the time of
injection is rarely necessary, especially if sedation has been used
earlier and the technique described is followed. -
Fentanyl and other opioids may be used if
the patient experiences pain during the procedure, but it is rarely
necessary and should not be used systematically. -
The most serious complications are
penetration of the globe during injection, intra-optic nerve sheath
injection with direct effect on the central nervous system, and
retrobulbar hemorrhage. -
Perforation of the globe is always
possible, particularly with large myopic eyes; therefore, the operator
should be alerted to this possibility and follow the technique as
described. If resistance to the passage of the needle is felt, the
globe should be carefully observed for movement and for motions of the
needle. Motion indicates the needle tip is impaling the sclera, and the
needle should be retracted slightly and redirected until no motion is
seen before thrusting the needle to the hilt and injecting. Tucking the
lid with the needle tip also is a safeguard against penetrating the
globe. -
Intra-optic nerve sheath injection can be
minimized by using a shorter needle (31 mm rather than 38 mm). However,
intra-optic nerve sheath injection may still occur without the
operator’s knowledge. Therefore, it is important to monitor the
patient’s vital signs prior to and after the performance of the block.
Because patients can develop respiratory or cardiac arrest up to 1 hour
after the injection, the placement of an intravenous line and immediate
access to cardiopulmonary resuscitation (CPR) equipment is critical. -
Retrobulbar hemorrhage is not uncommon
following retrobulbar injection. The hemorrhage is usually mild and
rarely causes a problem. Occasionally, a retrobulbar hemorrhage may be
severe causing proptosis, increased intraocular pressure, and a frozen
orbit. In these cases, it is best to cancel surgery and carefully
monitor the intraocular pressure. If sufficient pressure is exerted by
the retrobulbar hemorrhage to potentially exceed the arterial systolic
pressure and close the central retinal artery, a lateral canthotomy is
indicated to relieve the pressure of the lids on the globe. This is
rarely necessary, but everyone should be alerted to and prepared for
the possibility.
DC, Sturgess DA, Pemberton CJ, et al. Peribulbar and retrobulbar
anesthesia with prilocaine: a comparison of two methods of local ocular
anesthesia. Ophthal Surg 1993;24:842–845.
