Femoral Shaft
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > IV – Lower Extremity Fractures and Dislocations > 32 – Femoral Shaft
32
Femoral Shaft
-
A femoral shaft fracture is a fracture of
the femoral diaphysis occurring between 5 cm distal to the lesser
trochanter and 5 cm proximal to the adductor tubercle.
EPIDEMIOLOGY
-
There is an age- and gender-related bimodal distribution of fractures.
-
Femoral shaft fractures occur most frequently in young men after high-energy trauma and elderly women after a low-energy fall.
ANATOMY
-
The femur is the largest tubular bone in
the body and is surrounded by the largest mass of muscle. An important
feature of the femoral shaft is its anterior bow. -
The medial cortex is under compression, whereas the lateral cortex is under tension.
-
The isthmus of the femur is the region
with the smallest intramedullary (IM) diameter; the diameter of the
isthmus affects the size of the IM nail that can be inserted into the
femoral shaft. -
The femoral shaft is subjected to major muscular deforming forces (Fig. 32.1):
-
Abductors (gluteus medius and minimus):
They insert on the greater trochanter and abduct the proximal femur
following subtrochanteric and proximal shaft fractures. -
Iliopsoas: It flexes and externally rotates the proximal fragment by its attachment to the lesser trochanter.
-
Adductors: They span most shaft fractures
and exert a strong axial and varus load to the bone by traction on the
distal fragment. -
Gastrocnemius: It acts on distal shaft fractures and supracondylar fractures by flexing the distal fragment.
-
Fascia lata: It acts as a tension band by resisting the medial angulating forces of the adductors.
-
-
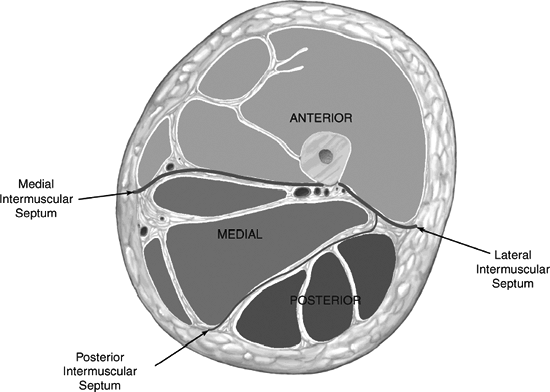
The thigh musculature is divided into three distinct fascial compartments (Fig. 32.2):
-
Anterior compartment: This is composed of
the quadriceps femoris, iliopsoas, sartorius, and pectineus, as well as
the femoral artery, vein, and nerve, and the lateral femoral cutaneous
nerve.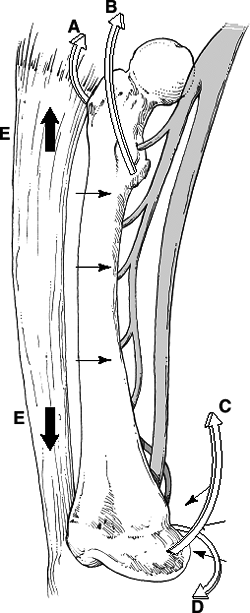 Figure 32.1. Deforming muscle forces on the femur; abductors (A), iliopsoas (B), adductors (C), and gastrocnemius origin (D). The medial angulating forces are resisted by the fascia lata (E).
Figure 32.1. Deforming muscle forces on the femur; abductors (A), iliopsoas (B), adductors (C), and gastrocnemius origin (D). The medial angulating forces are resisted by the fascia lata (E).
Potential sites of vascular injury after fracture are at the adductor
hiatus and the perforating vessels of the profunda femoris.(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)![]() Figure 32.2. Cross-sectional diagram of the thigh demonstrates the three major compartments.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
Figure 32.2. Cross-sectional diagram of the thigh demonstrates the three major compartments.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Medial compartment: This contains the
gracilis, adductor longus, brevis, magnus, and obturator externus
muscles along with the obturator artery, vein, and nerve, and the
profunda femoris artery. -
Posterior compartment: This includes the
biceps femoris, semitendinosus, and semimembranosus, a portion of the
adductor magnus muscle, branches of the profunda femoris artery, the
sciatic nerve, and the posterior femoral cutaneous nerve. -
Because of the large volume of the three
fascial compartments of the thigh, compartment syndromes are much less
common than in the lower leg. -
The vascular supply to the femoral shaft
is derived mainly from the profunda femoral artery. The one to two
nutrient vessels usually enter the bone proximally and posteriorly
along the linea aspera. This artery then arborizes proximally and
distally to provide the endosteal circulation to the shaft. The
periosteal vessels also enter the bone along the linea aspera and
supply blood to the outer one-third of the cortex. The endosteal
vessels supply the inner two-thirds of the cortex. -
Following most femoral shaft fractures,
the endosteal blood supply is disrupted, and the periosteal vessels
proliferate to act as the primary source of blood for healing. The
medullary supply is eventually restored late in the healing process. -
Reaming may further obliterate the endosteal circulation, but it returns fairly rapidly, in 3 to 4 weeks.
-
Femoral shaft fractures heal readily if
the blood supply is not excessively compromised. Therefore, it is
important to avoid excessive periosteal stripping, especially
posteriorly, where the arteries enter the bone at the linea aspera.
P.347P.348 -
MECHANISM OF INJURY
-
Femoral shaft fractures in adults are
almost always the result of high-energy trauma. These fractures result
from motor vehicle accident, gunshot injury, or fall from a height. -
Pathologic fractures, especially in the
elderly, commonly occur at the relatively weak metaphyseal-diaphyseal
junction. Any fracture that is inconsistent with the degree of trauma
should arouse suspicion for pathologic fracture. -
Stress fractures occur mainly in military
recruits or runners. Most patients report a recent increase in training
intensity just before the onset of thigh pain.
CLINICAL EVALUATION
-
Because these fractures tend to be the result of high-energy trauma, a full trauma survey is indicated.
-
The diagnosis of femoral shaft fracture
is usually obvious, with the patient presenting nonambulatory with
pain, variable gross deformity, swelling, and shortening of the
affected extremity. -
A careful neurovascular examination is
essential, although neurovascular injury is uncommonly associated with
femoral shaft fractures. -
Thorough examination of the ipsilateral
hip and knee should be performed, including systematic inspection and
palpation. Range-of-motion or ligamentous testing is often not feasible
in the setting of a femoral shaft fracture and may result in
displacement. Knee ligament injuries are common, however, and need to
be assessed after fracture fixation. -
Major blood loss into the thigh may
occur. The average blood loss in one series was greater than 1200 mL,
and 40% of patients ultimately required transfusions. Therefore, a
careful preoperative assessment of hemodynamic stability is essential,
regardless of the presence or absence of associated injuries.
P.349
ASSOCIATED INJURIES
-
Associated injuries are common and may be
present in up to 5% to 15% of cases, with patients presenting with
multisystem trauma, spine, pelvis, and ipsilateral lower extremity
injuries. -
Ligamentous and meniscal injuries of the ipsilateral knee are present in 50% of patients with closed femoral shaft fractures.
RADIOGRAPHIC EVALUATION
-
Anteroposterior (AP) and lateral views of the femur, hip, and knee as well as an AP view of the pelvis should be obtained.
-
The radiographs should be critically
evaluated to determine the fracture pattern, the bone quality, the
presence of bone loss, associated comminution, the presence of air in
the soft tissues, and the amount of fracture shortening. -
One must evaluate the region of the proximal femur for evidence of an associated femoral neck or intertrochanteric fracture.
-
If a computed tomography scan of the
abdomen and/or pelvis is obtained for other reasons, this should be
reviewed because it may provide evidence of injury to the ipsilateral
acetabulum or femoral neck.
CLASSIFICATION
Descriptive
-
Open versus closed injury
-
Location: proximal, middle, or distal one-third
-
Location: isthmal, infraisthmal or supracondylar
-
Pattern: spiral, oblique, or transverse
-
Comminuted, segmental, or butterfly fragment
-
Angulation or rotational deformity
-
Displacement: shortening or translation
Winquist and Hansen (Fig. 32.3)
-
This is based on fracture comminution.
-
It was used before routine placement of statically locked IM nails.
| Type I: | Minimal or no comminution |
| Type II: | Cortices of both fragments at least 50% intact |
| Type III: | 50% to 100% cortical comminution |
| Type VI: | Circumferential comminution with no cortical contact |
OTA Classification of Femoral Shaft Fractures
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
TREATMENT
Nonoperative
Skeletal Traction
-
Currently, closed management as
definitive treatment for femoral shaft fractures is largely limited to
adult patients with such significant medical comorbidities that
operative management is contraindicated. -
The goal of skeletal traction is to
restore femoral length, limit rotational and angular deformities,
reduce painful spasms, and minimize blood loss into the thigh.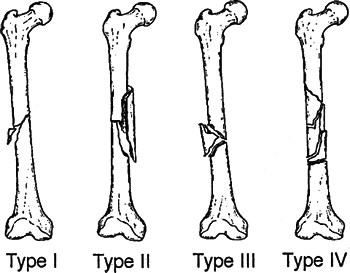 Figure 32.3. Winquist and Hansen classification of femoral shaft fractures.(From Browner BD, Jupiter JB, Levine AM, et al. Skeletal Trauma. Philadelphia: WB Saunders, 1992:1537.)
Figure 32.3. Winquist and Hansen classification of femoral shaft fractures.(From Browner BD, Jupiter JB, Levine AM, et al. Skeletal Trauma. Philadelphia: WB Saunders, 1992:1537.) -
Skeletal traction is usually used as a
temporizing measure before surgery to stabilize the fracture and
prevent fracture shortening. -
Twenty to 40 lb of traction is usually applied and a lateral radiograph checked to assess fracture length.
-
Distal femoral pins should be placed in
an extracapsular location to avoid the possibility of septic arthritis.
Proximal tibia pins are typically positioned at the level of the tibial
tubercle and are placed in a bicortical location. -
Safe pin placement is usually from medial
to lateral at the distal femur (directed away from the femoral artery)
and from lateral to medial at the proximal tibia (directed away from
the peroneal nerve). -
Problems with use of skeletal traction
for definitive fracture treatment include knee stiffness, limb
shortening, prolonged hospitalization, respiratory and skin ailments,
and malunion.
P.350
Operative
-
Operative stabilization is the standard of care for most femoral shaft fractures.
-
Surgical stabilization should occur within 24 hours, if possible.
-
Early stabilization of long bone injuries appears to be particularly important in the multiply injured patient.
Intramedullary (IM) Nailing
-
This is the standard of care for femoral shaft fractures.
-
Its IM location results in lower tensile
and shear stresses on the implant than plate fixation. Benefits of IM
nailing over plate fixation include less extensive exposure and
dissection, lower infection rate, and less quadriceps scarring. -
Closed IM nailing in closed fractures has
the advantage of maintaining both the fracture hematoma and the
attached periosteum. If reaming is performed, these elements provide a
combination of osteoinductive and osteoconductive materials to the site
of the fracture. -
Other advantages include early functional
use of the extremity, restoration of length and alignment with
comminuted fractures, rapid and high union (>95%), and low
refracture rates.
P.351
Antegrade Inserted Intramedullary (IM) Nailing
-
Surgery can be performed on a fracture table or on a radiolucent table with or without skeletal traction.
-
The patient can be positioned supine or
lateral. Supine positioning allows unencumbered access to the entire
patient. Lateral positioning facilitates identification of the
piriformis starting point but may be contraindicated in the presence of
pulmonary compromise. -
One can use either a piriformis fossa or
greater trochanteric starting point. The advantage of a piriformis
starting point is that it is in line with the medullary canal of the
femur. However, it is easier to locate the greater trochanteric
starting point. Use of a greater trochanteric starting point requires
use of a nail with a valgus proximal bow to negotiate the off starting
point axis. -
With the currently available nails, the
placement of large diameter nails with an intimate fit along a long
length of the medullary canal is no longer necessary. -
The role of unreamed IM nailing for the
treatment of femoral shaft fractures remains unclear. The potentially
negative effects of reaming for insertion of IM nails include elevated
IM pressures, elevated pulmonary artery pressures, increased fat
embolism, and increased pulmonary dysfunction. The potential advantages
of reaming rate include the ability to place a larger implant,
increased union, and decreased hardware failure. -
All IM nails should be statically locked
to maintain femoral length and control rotation. The number of distal
interlocking screws necessary to maintain the proper length, alignment,
and rotation of the implant bone construct depends on numerous factors
including fracture comminution, fracture location, implant size,
patient size, bone quality, and patient activity.
Retrograde Inserted Intramedullary (IM) Nailing
-
The major advantage with a retrograde entry portal is the ease in properly identifying the starting point.
-
Relative indications include:
-
Ipsilateral injuries such as femoral neck, pertrochanteric, acetabular, patellar, or tibial shaft fractures.
-
Bilateral femoral shaft fractures.
-
Morbidly obese patient.
-
Pregnant woman.
-
Periprosthetic fracture above a total knee arthroplasty.
-
Ipsilateral through knee amputation in a patient with an associated femoral shaft fracture.
-
-
Contraindications include:
-
Restricted knee motion <60 degrees.
-
Patella baja.
-
The presence of an associated open traumatic wound, secondary to the risk of intraarticular knee sepsis.
-
P.352
External Fixation
-
Use as definitive treatment for femoral shaft fractures has limited indications.
-
Its use is most often provisional.
-
Advantages include the following:
-
The procedure is rapid; A temporary external fixator can be applied in less than 30 minutes.
-
The vascular supply to the femur is minimally damaged during application.
-
No additional foreign material is introduced in the region of the fracture.
-
It allows access to the medullary canal and the surrounding tissues in open fractures with significant contamination.
-
-
Disadvantages: Most are related to use of this technique as a definitive treatment and include:
-
Pin tract infection.
-
Loss of knee motion.
-
Angular malunion and femoral shortening.
-
Limited ability to adequately stabilize the femoral shaft.
-
Potential infection risk associated with conversion to an IM nail.
-
-
Indications for use of external fixation include:
-
Use as a temporary bridge to IM nailing in the severely injured patient.
-
Ipsilateral arterial injury that requires repair.
-
Patients with severe soft tissue contamination in whom a second debridement would be limited by other devices.
-
Plate Fixation
Plate fixation for femoral shaft stabilization has decreased with the use of IM nails.
-
Advantages to plating include:
-
Ability to obtain an anatomic reduction in appropriate fracture patterns.
-
Lack of additional trauma to remote locations such as the femoral neck, the acetabulum, and the distal femur.
-
-
Disadvantages compared with IM nailing include:
-
Need for an extensive surgical approach
with its associated blood loss, risk of infection, and soft tissue
insult. This can result in quadriceps scarring and its effects on knee
motion and quadriceps strength. -
Decreased vascularization beneath the plate and the stress shielding of the bone spanned by the plate.
-
The plate is a load bearing implant; therefore, higher rate of implant failure.
-
-
Indications include:
-
Extremely narrow medullary canal where IM nailing is impossible or difficult.
-
Fractures that occur adjacent to or through a previous malunion.
-
Obliteration of the medullary canal due to infection or previous closed management.
-
Fractures that have associated proximal or distal extension into the pertrochanteric or condylar regions.
-
In patients with an associated vascular
injury, the exposure for the vascular repair frequently involves a wide
exposure of the medial femur. If rapid femoral stabilization is
desired, a plate can be applied quickly through the medial open
exposure.
P.353 -
-
An open or a submuscular technique may be applicable.
-
As the fracture comminution increases, so
should the plate length such that at least four to five screw holes of
plate length are present on each side of the fracture. -
The routine use of cancellous bone
grafting in plated femoral shaft fractures is questionable if indirect
reduction techniques are used.
Femur Fracture in Multiply Injured Patient
-
The impact of femoral nailing and reaming is controversial in the polytrauma patient.
-
In a specific subpopulation of patients
with multiple injuries, early IM nailing is associated with elevation
of certain proinflammatory markers. -
It has been recommended that early
external fixation of long bone fractures followed by delayed IM nailing
may minimize the additional surgical impact in patients at high risk
for developing complications (i.e., patients in extremis or
underresuscitated).
Ipsilateral Fractures of the Proximal or Distal Femur
-
Concomitant femoral neck fractures occur
in 3% to 10% of patients with femoral shaft fractures. Options for
operative fixation include antegrade IM nailing with multiple screw
fixation of the femoral neck, retrograde femoral nailing with multiple
screw fixation of the femoral neck, and compression plating with screw
fixation of the femoral neck. The sequence of surgical stabilization is
controversial. -
Ipsilateral fractures of the distal femur
may exist as a distal extension of the shaft fracture or as a distinct
fracture. Options for fixation include fixation of both fractures with
a single plate, fixation of the shaft and distal femoral fractures with
separate plates, IM nailing of the shaft fracture with plate fixation
of the distal femoral fracture, or interlocked IM nailing spanning both
fractures (high supracondylar fractures).
Open Femoral Shaft Fractures
-
These are typically the result of high-energy trauma.
-
Patients frequently have multiple other orthopaedic injuries and involvement of several organ systems.
-
Treatment is emergency debridement with skeletal stabilization.
-
Stabilization can usually involve placement of a reamed IM nail.
P.354
REHABILITATION
-
Early patient mobilization out of bed is recommended.
-
Early range of knee motion is indicated.
-
Weight bearing on the extremity is guided
by a number of factors including the patient’s associated injuries,
soft tissue status, and the location of the fracture.
COMPLICATIONS
-
Nerve injury: This is uncommon because
the femoral and sciatic nerves are encased in muscle throughout the
length of the thigh. Most injuries occur as a result of traction or
compression during surgery. -
Vascular injury: This may result from tethering of the femoral artery at the adductor hiatus.
-
Compartment syndrome: This occurs only
with significant bleeding. It presents as pain out of proportion, tense
thigh swelling, numbness or paresthesias to medial thigh (saphenous
nerve distribution), or painful passive quadriceps stretch. -
Infection (<1% incidence in closed
fractures): The risk is greater with open versus closed IM nailing.
Grades I, II, and IIIA open fractures carry a low risk of infection
with IM nailing, whereas fractures with gross contamination, exposed
bone, and extensive soft tissue injury (grades IIIB, IIIC) have a
higher risk of infection regardless of treatment method. -
Refracture: Patients are vulnerable
during early callus formation and after hardware removal. It is usually
associated with plate or external fixation. -
Nonunion and delayed union: This is
unusual. Delayed union is defined as healing taking longer than 6
months, usually related to insufficient blood supply (i.e., excessive
periosteal stripping), uncontrolled repetitive stresses, infection, and
heavy smoking. Nonunion is diagnosed once the fracture has no further
potential to unite. -
Malunion: This is usually varus, internal rotation, and/or shortening owing to muscular deforming forces or surgical technique.
-
Fixation device failure: This results from nonunion or “cycling” of device, especially with plate fixation.
-
Heterotopic ossification may occur.