Distal Femur
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > IV – Lower Extremity Fractures and Dislocations > 33 – Distal Femur
33
Distal Femur
EPIDEMIOLOGY
-
Distal femoral fractures account for about 7% of all femur fractures.
-
If hip fractures are excluded, one-third of femur fractures involve the distal portion.
-
A bimodal age distribution exists, with a
high incidence in young adults from high-energy trauma, such as motor
vehicle or motorcycle accidents or falls from a height, and a second
peak in the elderly from minor falls. -
Open fractures occur in 5% to 10% of all distal femur fractures.
ANATOMY
-
The distal femur includes both the supracondylar and condylar regions (Fig. 33.1).
-
The supracondylar area of the femur is
the zone between the femoral condyles and the junction of the
metaphysis with the femoral shaft. This area comprises the distal 10 to
15 cm of the femur. -
The distal femur broadens from the cylindric shaft to form two curved condyles separated by an intercondylar groove.
-
The medial condyle extends more distally
and is more convex than the lateral femoral condyle. This accounts for
the physiologic valgus of the femur. -
When viewing the lateral femur, the femoral shaft is aligned with the anterior half of the lateral condyle (Fig. 33.2).
-
When viewing the distal surface of the femur end on, the condyles are wider posteriorly, thus forming a trapezoid.
-
Normally, the knee joint is parallel to
the ground. On average, the anatomic axis (the angle between the shaft
of the femur and the knee joint) has a valgus angulation of 9 degrees
(range, 7 to 11 degrees) (Fig. 33.3). -
Deforming forces from muscular attachments cause characteristic displacement patterns (Fig. 33.4).
-
Gastrocnemius: This flexes the distal fragment, causing posterior displacement and angulation.
-
Quadriceps and hamstrings: They exert proximal traction, resulting in shortening of the lower extremity.
-
MECHANISM OF INJURY
-
Most distal femur fractures are the result of a severe axial load with a varus, valgus, or rotational force.
-
In young adults, this force is typically the result of high-energy trauma such as motor vehicle collision or fall from a height.
-
In the elderly, the force may result from a minor slip or fall onto a flexed knee.
CLINICAL EVALUATION
-
Patients typically are unable to ambulate with pain, swelling, and variable deformity in the lower thigh and knee.
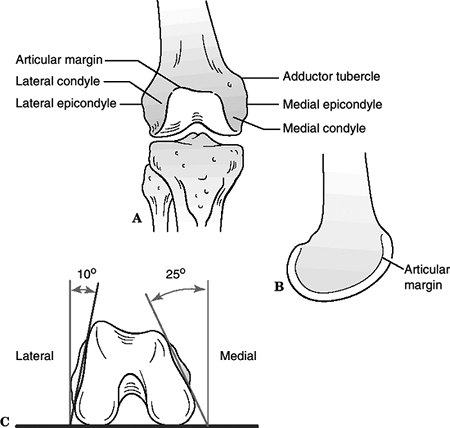
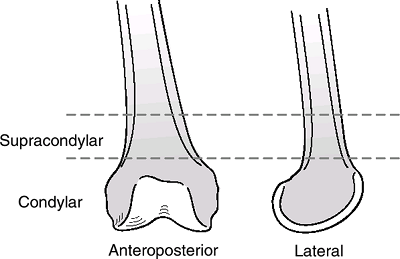 Figure 33.1. Schematic drawing of the distal femur.(Adapted from Wiss D. Master Techniques in Orthopaedic Surgery. Philadelphia: Lippincott-Raven, 1998.)
Figure 33.1. Schematic drawing of the distal femur.(Adapted from Wiss D. Master Techniques in Orthopaedic Surgery. Philadelphia: Lippincott-Raven, 1998.)![]() Figure
Figure
33.2. Anatomy of the distal femur. (A) Anterior view. (B) Lateral view.
The shaft of the femur is aligned with the anterior half of the lateral
condyle. (C) Axial view. The distal femur is trapezoidal. The anterior
surface slopes downward from lateral to medial, the lateral wall
inclines 10 degrees, and the medial wall inclines 25 degrees.(Adapted from Wiss D, Watson JT, Johnson EE. Fractures of the knee. In: Rockwood CA, Green DP, Bucholz RW, et al., eds. Rockwood and Green’s Fractures in Adults, 4th ed. Philadelphia: Lippincott-Raven, 1996.) -
Assessment of neurovascular status is
mandatory. The proximity of the neurovascular structures to the
fracture area is an important consideration. Unusual and tense swelling
in the popliteal area and the usual signs of pallor and lack of pulse
suggest rupture of a major vessel.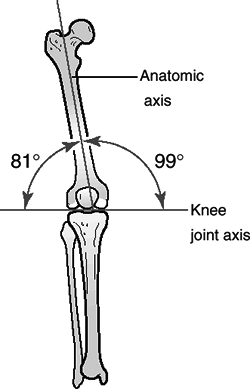 Figure
Figure
33.3. Alignment of the lower extremity. The knee joint is parallel to
the ground. The knee joint is in 9 degree valgus to the knee joint.(Adapted from Browner BD, Levine AM, Jupiter JB. Skeletal Trauma: Fractures, Dislocations, Ligamentous Injuries, 2nd ed. Philadelphia: WB Saunders, 1997.) -
Compartment syndrome of the thigh is uncommon and is associated with major bleeding into the thigh.
-
Examination of the ipsilateral hip, knee, leg, and ankle is essential, especially in the obtunded or polytraumatized patient.
P.356
P.357
 |
|
Figure
33.4. Lateral view showing muscle attachments and resulting deforming forces. These result in posterior displacement and angulation at the fracture site. (Adapted from Browner BD, Levine AM, Jupiter JB. Skeletal Trauma: Fractures, Dislocations, Ligamentous Injuries, 2nd ed. Philadelphia: WB Saunders, 1997.)
|
RADIOGRAPHIC EVALUATION
-
Anteroposterior, lateral, and two 45-degree oblique radiographs of the distal femur should be obtained.
-
Radiographic evaluation should include the entire femur.
-
Traction views may be helpful to better determine the fracture pattern.
-
Contralateral views may be helpful for comparison and serve as a template for preoperative planning.
-
Complex intraarticular fractures and
osteochondral lesions may require additional imaging with computed
tomography to assist in completing the diagnostic assessment and
preoperative planning. -
Magnetic resonance imaging may be of value in evaluating associated injuries to ligamentous or meniscal structures.
-
Arteriography may be indicated with
dislocation of the knee, because 40% of dislocations are associated
with vascular disruption. The reason is that the popliteal vascular
bundle is tethered proximally at the adductor hiatus and distally at
the soleus arch. By contrast, the incidence of vascular disruption with
isolated supracondylar fractures is between 2% and 3%.
CLASSIFICATION
Descriptive
-
Open versus closed
-
Location: supracondylar, intercondylar, condylar
-
Pattern: spiral, oblique, or transverse
-
Articular involvement
-
Comminuted, segmental, or butterfly fragment
-
Angulation or rotational deformity
-
Displacement: shortening or translation
OTA Classification of Distal Femoral Fractures
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
TREATMENT
Nonoperative
-
Indications include nondisplaced or
incomplete fractures, impacted stable fractures in elderly patients,
severe osteopenia, advanced underlying medical conditions, or select
gunshot injuries. -
In stable, nondisplaced fractures,
treatment is mobilization of the extremity in a hinged knee brace, with
partial weight bearing. -
In displaced fractures, nonoperative
treatment entails a 6- to 12-week period of skeletal traction followed
by bracing. The objective is not absolute anatomic reduction, but
restoration of the knee joint axis to a normal relationship with the
hip and ankle. Potential drawbacks include varus and internal rotation
deformity, knee stiffness, and the necessity for prolonged
hospitalization and bed rest.
P.359
Operative
-
Most displaced distal femur fractures are best treated with operative stabilization.
-
If surgery is to be delayed more than 8 hours, tibial pin traction should be considered.
-
Articular fractures require anatomic reconstruction of the joint surface and fixation with interfragmentary lag screws.
-
The articular segment is then reattached
to the proximal segment, with an effort to restore the normal anatomic
relationships. These should encompass all angular, translational, and
rotational relationships. -
In patients with severe osteopenia or contralateral amputation, length may be sacrificed for fracture stability.
-
With the advent of more biologic techniques of fracture stabilization, the necessity for bone grafting has diminished.
-
Polymethylmethacrylate cement may be necessary in extremely osteoporotic bone to increase the fixation capability of screws.
Implants
-
Screws: In most cases, they are used in
addition to other fixation devices. In noncomminuted, unicondylar
fractures in young adults with good bone stock, interfragmentary screws
alone can provide adequate fixation. -
Plates: To control alignment
(particularly varus and valgus) of the relatively short distal
articular segment, a fixed angle implant is frequently necessary.-
A 95-degree condylar blade plate: This provides excellent fracture control but is technically demanding.
-
Dynamic condylar screw (DCS): This is
technically easier to insert than a condylar blade plate, and
interfragmentary compression is also possible through its lag screw
design. Disadvantages of the DCS are the bulkiness of the device and
the poorer rotational control than with the blade plate. -
Nonlocking periarticular plates (condylar
buttress plates): These are used with extensive comminution or multiple
intraarticular fractures. Screws may toggle within the plate holes;
therefore, these plates have no inherent varus or valgus stability.
This stability must therefore be provided by additional fixation
devices such as a second medial plate or by the inherent stability of
the bone after fixation of the fracture. -
Locking plates (with fixed angle screws):
The development of locking plates made the nonlocking periarticular
plate relatively obsolete. Locking plates are an alternative to the DCS
and blade plate. Like the DCS and the blade plate, locking plates are
fixed-angle devices. The screws lock to the plate and therefore provide
angular stability to the construct.
-
-
Intramedullary (IM) nails
-
Antegrade inserted IM nail: It has
limited use owing to the distal nature of the fracture. It is best used
in supracondylar type fractures with a large distal segment. -
Retrograde inserted IM nail: It has the
advantage of improved distal fixation. The disadvantages are the
further insult to the knee joint and the potential of knee sepsis if
the nailing is complicated by infection.
-
-
External fixation
-
In patients whose medical condition
requires rapid fracture stabilization or in patients with major soft
tissue lesions, spanning external fixation allows for rapid fracture
stabilization while still allowing access to the limb and patient
mobilization. -
Definitive external fixation, although rarely used, can be in the form of a unilateral half-pin fixator or a hybrid frame.
-
Problems include pin tract infection, quadriceps scarring, delayed or nonunion, and loss of reduction after device removal.
-
P.360
Associated Vascular Injury
-
The incidence is estimated to be about 2%.
-
If arterial reconstruction is necessary, it should be done before definitive skeletal stabilization.
-
Reduction of the fracture and temporary
fixation with an external fixator or femoral distractor before vascular
repair should be considered. -
Definitive fracture management can proceed after the vascular procedure if the patient’s condition allows.
-
Fasciotomy of the lower leg should be performed in all cases.
Supracondylar Fractures after Total Knee Replacement
-
These are rare and are related to
osteopenia, rheumatoid arthritis, prolonged corticosteroid usage,
anterior notching of the femur, and revision arthroplasty. -
Treatment is based on the status of the arthroplasty implants (well fixed or loose) and the patient’s preinjury function.
-
In displaced fractures, options include long-stem revision, IM nailing, and plate fixation.
Postoperative Management
-
The injured extremity is typically placed
on a continuous passive motion device in the immediate postoperative
period if the skin and soft tissues will tolerate. -
Physical therapy consists of active
range-of-motion exercises and partial weight bearing with crutches 2 to
3 days after stable fixation. -
A cast brace may be used if fixation is tenuous.
-
Weight bearing may be advanced with radiographic evidence of healing (6 to 12 weeks).
COMPLICATIONS
-
Fixation failure: This is usually a
result of one of the following: poor bone stock, patient noncompliance
with postoperative care, or inadequate surgical planning and execution. -
Malunion: This usually results from
unstable fixation or infection. Varus is the most common deformity.
Malunion with the articular surface in extension may result in relative
hyperextension of the knee, whereas malunion in flexion may result in a
functional loss of full extension. Malunion resulting in functional
disability may be addressed with osteotomy. -
Nonunion: This is infrequent because of the rich vascular supply to this region and the predominance of cancellous bone.
-
Posttraumatic osteoarthritis: This may
result as a failure to restore articular congruity, especially in
younger patients. It also may reflect chondral injury at the time of
trauma. -
Infection: Open fractures require
meticulous debridement and copious irrigation (serial, if necessary)
with intravenous antibiotics. Open injuries contiguous with the knee
necessitate formal irrigation and debridement to prevent knee sepsis. -
Loss of knee motion: This is the most
common complication as a result of scarring, quadriceps damage, or
articular disruption during injury. If significant, it may require
lysis of adhesions or quadricepsplasty for restoration of joint motion.
It is best prevented by early range of motion and adequate pain control.
P.361