DISLOCATIONS AND MULTIPLE LIGAMENTOUS INJURIES OF THE KNEE
IV – SPORTS MEDICINE > Knee > CHAPTER 91 – DISLOCATIONS AND
MULTIPLE LIGAMENTOUS INJURIES OF THE KNEE
with extensive capsular, meniscal, chondral, and extraarticular tendon
injury comprises a potentially devastating condition. The spectrum of
injury can range from multiplanar laxity to frank dislocation of the
knee. Of foremost concern is the potential for neurovascular injury.
Popliteal artery injury requires emergent multidisciplinary evaluation
and treatment. Once perfusion of the limb has been assured, the
orthopaedic surgeon faces a major task to stabilize the joint, restore
a functional range of motion,
and minimize, if not prevent, future degenerative changes of the joint.
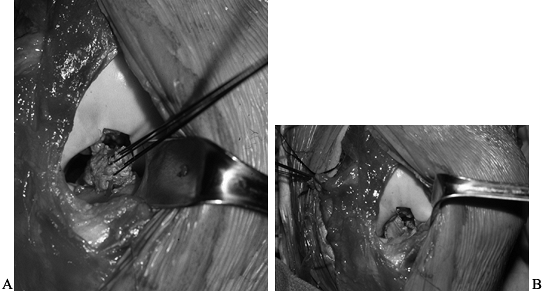
adductor hiatus and distally by the fibrous arch of the soleus,
traverses the popliteal fossa adjacent to the posterior capsule of the
knee (Fig. 91.1). These attachments create a
bow string effect, rendering the artery susceptible to injury whenever
the knee dislocates or even whenever multiple ligaments are torn (4,10,21,22,25,34).
Approximately one third of knee dislocations have associated arterial
injury, with anterior and posterior dislocations having the highest
incidence, approaching 40% (7). Posterior knee
dislocation, in which the tibia is driven posteriorly into the
popliteal fossa, can directly contuse or lacerate the artery, whereas
anterior dislocation, a result of excessive knee hyperextension, can
result in complete arterial rupture or injury confined to the intimal
lining, producing immediate or delayed thrombosis (10,21,22,25).
Occlusion or rupture of the popliteal artery jeopardizes perfusion of
the lower extremity in the vast majority of patients because of the
inadequate collateral circulation about the knee (2,3).
 |
|
Figure 91.1. Anterior and posterior views of the popliteal artery with its collateral circulation.
|
the popliteal fossa are less rigidly fixed than the artery. This may
account for a slightly lower incidence (approximately 25% overall) of
nerve trauma in reported series (9,10,17,18,30,31,32 and 33). Injury is most likely to involve the peroneal nerve, although injury of the posterior tibial nerve can occur (36).
Kennedy found that as little as 15° of hyperextension caused stretching
of the peroneal nerve because of the cam-like effect of the lateral
femoral condyle against the closely positioned nerve (10). Complete disruption or severe stretching with the nerve remaining macroscopically intact can occur. Good and Johnson (6)
have reported the natural history of nerve injuries based on published
series to be as follows: 60% no improvement, 32% complete recovery, and
8% incomplete recovery (9,10,17,18,30,31,32 and 33).
cruciate ligaments and one collateral ligament. Occasionally, knee
dislocation can occur with one of the cruciates remaining intact (1,10,17,29,30).
Typically, a dislocation causes extensive capsular injury as well as
injury to the menisci, articular cartilage, extensor mechanism, and
other structures including the iliotibial band as well as popliteus,
biceps, and pes anserina tendons. After dislocation, the tibiofemoral
joint may spontaneously reduce and be normally aligned or may remain
subluxated or dislocated.
injuries occur, many of which also have extensive capsular injury.
These patterns include:
-
ACL1 + MCL.
-
ACL + MCL + medial capsule.
-
ACL + posterolateral complex (LCL, popliteus, arcuate complex).
-
PCL + posterolateral complex.
-
PCL + MCL + medial capsule.
such as motor-vehicle accidents, pedestrians being hit by cars, or
contact sports (24,28,30,32);
however, high-energy forces are not a prerequisite for knee
dislocation, as lower-energy trauma from a fall or stationary
hyperextension can cause dislocation (10).
 |
|
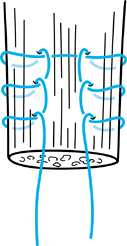
Figure 91.2. Classification of knee dislocations.
|
is produced by knee hyperextension with anterior displacement of the
tibia relative to the femur. Kennedy observed tearing of the posterior
capsule and PCL at an average of 30° of hyperextension. Continued
hyperextension to 50° caused popliteal artery injury. Girgis observed
that PCL injury occurred only following ACL rupture, which is
consistent with clinical experience (5).
 |
|
Figure 91.3. Lateral radiograph of an anterior dislocation.
|
results from a posteriorly directed force applied to the anterior tibia
of the flexed knee (dashboard injury). Experimentally, posterior
dislocation has been produced by the application of 75 to 100 in.-lb of
torque to the tibia with the knee in 20° of flexion (10).
Kennedy found this injury difficult to reproduce in cadaveric
experiments because of the tethering effect of the extensor mechanism
that blocked displacement. He noted that patellar tendon rupture was
associated with experimentally produced posterior knee dislocation.
Clinically, a direct blow to the anterior tibia with the knee flexed
nearly 90° is the mechanism responsible for most posterior dislocations.
 |
|
Figure 91.4. Lateral radiograph of a posterior dislocation.
|
direct valgus or varus forces applied to the proximal tibia. Kennedy
noted that experimental reproduction was commonly associated with
tibial plateau and supracondylar femur fractures. Clinically, medial
and lateral dislocations have been observed in heavy laborers or
victims of motor-vehicle
accidents, mining accidents, and crush injuries (10).
component. This occurs when one element of the supporting structures
remains intact, allowing the tibia to angulate and rotate relative to
the femur. Of the rotatory types of injuries, posterolateral
dislocation is important to recognize because it is often irreducible
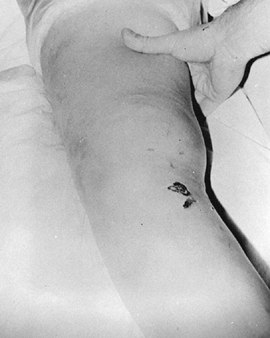
by closed methods (8,23) (Fig. 91.5A, Fig. 91.5B).
Reduction of this dislocation can be blocked by a buttonhole tear in
the medial capsule, trapping the medial femoral condyle (Fig. 91.5C, Fig. 91.5D). This can result in a medial cutaneous skin furrow (35).
This sign is an indication for immediate open reduction; delay may
result in skin necrosis or further neurovascular compromise.
 |
|
Figure 91.5. A: Anteroposterior radiograph of a posterolateral dislocation with marginal patellar fracture. B: Lateral radiograph of a posterolateral dislocation. C: Appearance of knee before reduction. D: Medial femoral condyle buttonholed through medial capsule, blocking closed reduction.
|
diagnosis may not be suspected because there is normal alignment and
lack of excessive swelling. Diagnosis requires clinical demonstration
of cruciate and collateral ligamentous injuries. A knee dislocation
that has spontaneously reduced may demonstrate one or more of the
following (34):
-
Greater than 30°dg recurvatum (indicates PCL and posterior capsule disruption).
-
Greater than 1 cm of anteroposterior (AP) excursion (indicates ACL and PCL tears), with soft endpoints.
-
Lateral capsular sign (indicates ACL and lateral complex disruption).
-
Large hemarthrosis or hematoma.
the mechanism of injury and applying reversing forces to effect closed
reduction, a more useful classification identifies the structures that
are torn and will need repair or reconstruction. Modified from Schenck
to include associated capsular injury, the following are patterns of
dislocation most often encountered (26):
-
ACL + PCL torn; MCL + LCL + capsule intact.
-
ACL + PCL + MCL + medial capsule torn; LCL + posterolateral intact.
-
ACL + PCL + LCL + posterolateral complex torn; MCL intact.
-
ACL + PCL + MCL + medial capsule + LCL + posterolateral complex torn.
 |
|
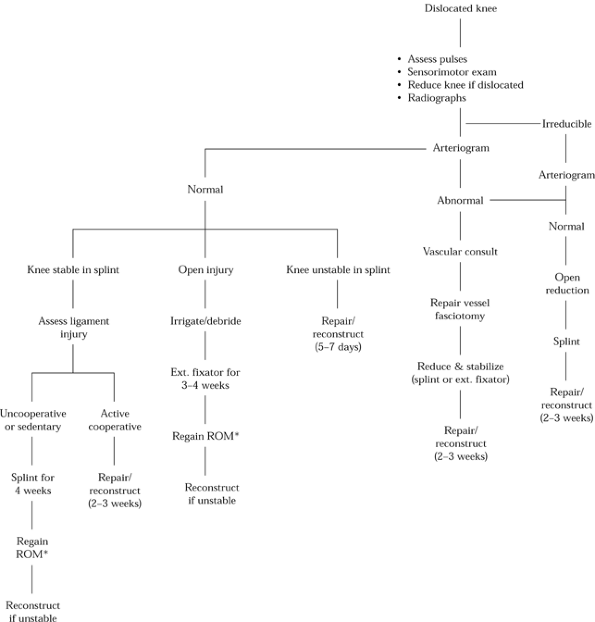
Figure 91.6. Algorithm for management of the dislocated knee. ROM, range of motion.
|
immediate vascular and neurologic assessment of the limb, followed by
gentle closed reduction. Because fractures of the distal femur and
proximal tibia as well as knee dislocation can cause gross deformity,
gentle reduction is similarly beneficial in improving circulation in
these conditions.
Gentle
longitudinal traction is usually sufficient to effect reduction or at a
minimum improve alignment. Lifting the femur anteriorly in addition to
longitudinal traction is helpful to avoid further trauma to the
popliteal structures in the instance of an anterior dislocation. At
this point, reassess the pedal pulses and repeat the neurologic exam.
If pulses are present and bilaterally symmetric, splint the knee in 5°
of flexion, avoiding hyperextension, and obtain radiographs. Once this
is completed, methodically and gently assess the knee for ligamentous
laxity (Fig. 91.7 , Fig. 91.8 and Fig. 91.9).
Apply AP stress at 30° of flexion. Check varus–valgus laxity at 0° and
30° of flexion. If significant ligamentous injury has occurred, there
will be abnormal tibial excursion and soft endpoints. If the collateral
ligaments are intact but stretched (grade II sprain), return of
intrinsic varus–valgus stability will be noted after reduction of the
dislocation. Have the patient attempt to actively extend the knee even
with some assistance while you palpate anteriorly for any defect in the
extensor mechanism. An arteriogram (Fig. 91.10)
in the radiology suite is necessary to exclude complete thrombosis, a
small laceration, or an intimal injury. Obtain immediate consultation
from a vascular surgeon if any abnormality is noted (see below). Admit
the patient for observation of peripheral circulation and potential
compartment syndrome and formulate the plan for surgical repair.
 |
|
Figure 91.7. Gentle valgus stress testing in extension reveals medial complex injury.
|
 |
|
Figure 91.8. Gentle varus stress testing in extension indicates lateral complex injury.
|
 |
|
Figure 91.9. Recurvatum of involved extremity, as compared to the contralateral extremity, indicates posterior laxity.
|
 |
|
Figure 91.10. Postreduction arteriogram reveals popliteal artery disruption.
|
after attempted reduction, fullness in the popliteal area, open injury,
or irreducible dislocation. Arteriography is usually performed in the
operating room in expectation of popliteal exploration. This saves
valuable time, as opposed to obtaining the arteriogram in the radiology
suite. The return of distal pulses following reduction does not negate
the urgency of further vascular evaluation. Return of distal pulses
following closed reduction has been reported in the presence of
complete popliteal artery disruption (9,16,22,25).
It has been shown that after this time interval, irreversible muscle
damage and gangrene occur, even if blood flow is reestablished (19). When revascularization is performed within 8 h, there is an 87% limb survival rate (7). Conversely, treatment of a popliteal vascular injury after 8 h has been reported to have an amputation rate as high as 85% (7).
successful and timely repair does not guarantee limb survival. Other
factors such as age, the presence of an open wound, associated crush
injuries, fractures, and extent of damage to the collateral circulation
may affect the results. Delayed revascularization may be successful on
occasion. Because ischemic tolerance is variable, delayed
revascularization (from 36 h up to 4 days after injury) has led to limb
survival (3,12).
Therefore, the need for amputation should be evaluated on an individual
basis and not performed prematurely if there is any potential for
revascularization.
interpositional saphenous vein graft, harvested from the contralateral
limb. On completion of revascularization, a full four-compartment
fasciotomy must be performed (4), followed by
maintenance of the reduction of the knee. This requires cooperation
between the orthopaedic and vascular surgeons to ensure protection of
the vascular repair while facilitating treatment of the knee
instability.
have sustained a knee dislocation. These injuries have a similar
incidence of neurovascular complications as do knees that present with
gross deformity. Therefore, perform an examination as described above
for the dislocated knee with intact circulation. We routinely obtain
arteriograms for these patients, although satisfactory assessment using
Doppler pressure measurements (ankle/arm pressure ratios) has been
reported (34).
and the collateral ligament(s) is usually obvious. It is crucial to
establish whether there is accompanying injury to either the
posterolateral complex (PLS) or the medial complex [medial capsule and
posterior oblique ligament (POL)]. Although ACL + MCL is a common
injury pattern and does well with initial nonoperative treatment for
the MCL followed by ACL reconstruction alone, untreated injury to the
other medial structures (capsule and POL) can compromise an ACL
reconstruction. Extensive injury to the medial capsular–ligament
complex is indicated by:
-
Greater than 5 mm valgus opening in full knee extension.
-
Increased external tibial rotation at 30°dg of knee flexion.
-
An increased anterior drawer test at 90°dg of flexion while in external rotation.
-
Increased (>10°dg side to side) external tibial rotation at 30°dg of flexion.
-
Varus opening 5 mm in full extension.
-
Anterior tibial translation in full extension greater than when in flexion (when ACL torn).
injuries, use a well-padded Robert-Jones (R-J) dressing incorporating
medial and lateral splints with the knee in 5° of flexion. This is
superior to a knee immobilizer. Subtle
peroneal nerve injury (in situ
injury) may accompany posterolateral disruptions. Although motor
function can be difficult to grade accurately in the acute setting,
decreased sensation in the first dorsal web space may be a clue to such
injury. Monitor the patient in hospital for at least 24 h for possible
vascular injury and remain alert to the potential for compartment
syndrome. Early primary repair of a capsular injury typically has an
outcome superior to reconstruction performed for chronic instability.
Ideally, undertake surgical repair by 14 days, although surgery can
still be successful as late as 3 weeks postinjury.
minimum, an AP and a lateral in extension are necessary to determine if
tibiofemoral alignment has been restored and can be maintained in a
splint. Posterior subluxation can be difficult to detect, and,
especially if nonoperative treatment is considered, a comparison view
with the normal knee can be helpful. Oblique and tunnel views may
demonstrate subtle avulsions and fractures. Stress radiographs are not
routinely performed in acute cases but can be used to document
instability in chronic cases.
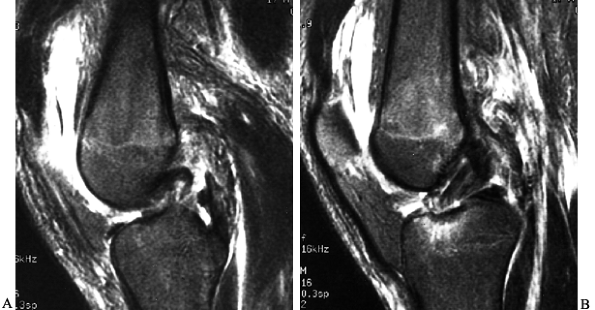
the articular cartilage and menisci as well as subtle posterolateral
complex injury because the popliteus tendon and other lateral
structures can be well visualized. Often MRI will show the type of
cruciate injury (avulsion vs. midsubstance) that is helpful in
preoperative planning of the type of repair or reconstruction (Fig. 91.11).
 |
|
Figure 91.11. Magnetic resonance image demonstrating midsubstance PCL rupture (A) and ACL tibial avulsion (B).
|
-
Ensure perfusion of the lower limb.
-
Stabilize the knee joint while restoring functional range of motion (ROM).
-
Minimize the development of posttraumatic joint degeneration.
by primarily repairing or reconstructing torn structures.
Immobilization choices include casting, casting supplemented with
transarticular Steinmann pins transfixing the tibia to the femur, and
external fixation bridging the knee joint. Another method is
“olecranization” of the patella, which transfixes the patella to the
tibia, preventing posterior tibial subluxation while allowing limited
motion of the knee. All of these methods rely on indirect healing of
ligaments, capsule, and muscles supplemented by scar formation during a
period of immobilization. Methods that promote mobilization of the knee
and limb involve surgical repair with limited or comprehensive
reconstruction.
of flexion using a well-padded R-J dressing incorporating splints,
extending from the proximal thigh to include the foot. Elevate the
extremity, monitor the patient for 24 to
48
h in hospital, and then apply a groin-to-toes long leg cast in 5° of
flexion or properly fit a long leg functional brace. Obtain radiographs
to ensure that alignment is normal. Continue immobilization for 4 weeks
and then begin range-of-motion exercises. This method is suitable for
patients who are inactive or uncooperative either because of other
injuries or personality or who decline surgical treatment.
reduce the knee under regional or general anesthesia and insert a
single large-diameter Steinmann pin into the upper tibia starting
medial to the tibial tuberosity and under fluoroscopic control advance
it into the intercondylar notch to engage the lateral part of the
distal femur in the metaphyseal region. The knee must be reduced before
the pin is seated in the femur; perform a lateral radiograph if the
fluoroscopic image is not clear. Use supplemental casting as described
above. Disadvantages of this technique include the need for removal of
the pin and the possibility of pin breakage with motion.
Steinmann pins from the superior pole of the patella to exit the
inferior pole and engage the anteriormost portion of the intercondylar
eminence on the tibia. This prevents posterior subluxation; however,
with excessive motion of the knee, the pins can break or erode through
the articular surface of the patella. Therefore, we rarely use this
method of stabilization.
unstable knee that does not rely on hardware traversing the interior of
the joint. Its major indication is to treat the open dislocation where
repeated wound procedures are necessary. The major disadvantage is that
motion is sacrificed, and because of the passage of pins into the
anterior or lateral femur, quadriceps adhesions are likely to develop.
We prefer to remove the fixator at 3 to 4 weeks if wound healing is
satisfactory, and, provided the knee is stable, start motion in a
hinged brace. If the knee is unstable, then once motion is regained,
perform arthroscopic assisted ACL and PCL reconstruction as described
in Chapter 89 and Chapter 90.
and irreducible dislocations. Relative indications include a
redislocating or subluxating knee despite splinting and a knee
dislocation or multiple ligament injuries in an active patient. Surgery
is contraindicated in uncooperative patients and in patients likely to
be unable to successfully rehabilitate the knee after surgery (e.g.,
patients with concomitant head trauma or severe polytrauma). Treat this
group by immobilizing the knee initially, followed by reconstructive
surgery if needed at the time their other injuries have resolved.
-
When to perform surgery?
-
What type of skin incision(s) to use?
-
How to treat cruciate and collateral ligament, and capsular tears?
-
What to do with the nerve injury?
-
What is the role of arthroscopy?
postinjury phase (up to 21 days), or months later. The advantages of
performing surgery within a 21-day period is that structures can be
discretely identified and repaired; once stability is achieved, motion
of the knee at least on a limited basis can be initiated; and articular
injuries can be precisely identified, which can be helpful in
prognosticating outcome as well as guiding rehabilitation. Unless
otherwise indicated (see below), there is no advantage in surgery
performed immediately versus 7 to 21 days postinjury. This short delay
allows ample preoperative monitoring of limb perfusion, promotes
resolution of soft-tissue swelling, and allows the surgeon to put
together a well-thought-out operative plan. Usually after a 48-h period
of observation, the patient can be discharged home with the knee
splinted. Forewarn the patient about the signs of delayed thrombosis
and the possible need for urgent readmission, and schedule elective
repair of the knee ligaments about 14 days after injury.
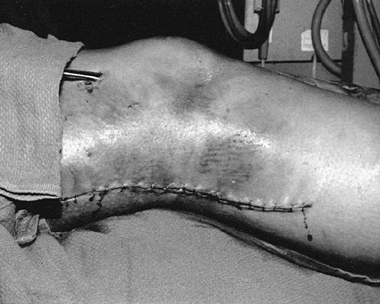
irreducible dislocations, and dislocations redislocating or subluxating
after splinting. Immediate surgery is performed in instances of
dislocations associated with open injuries and irreducible
dislocations. For open dislocations, irrigate and debride the wounds
and joint as for an open fracture and then apply an external fixator to
maintain reduction. For irreducible dislocations, perform open
reduction, close the wound, and splint the knee. We prefer to wait 10
to 14 days before performing definitive surgical repair. If vascular
repair is necessary, ligament surgery can be delayed up to 3 weeks if
needed. This is because the extreme medial incision used by vascular
surgeons does not allow adequate exposure of the joint without the
mobilization of a large subcutaneous flap. In the face of compromised
circulation, this can impair wound
healing. Perform surgery within 5 to 7 days for dislocations that subluxate despite proper splinting.
peroneal nerve is injured, use a midlateral incision for exposing these
structures together with a medial parapatellar skin incision for any
medial knee and cruciate injuries, maintaining at least a 7 cm bridge
of skin between the two incisions (Fig. 91.12 and Fig. 91.13).
If the lateral structures are intact, then a longitudinal midline
anterior incision can be used to expose the posteromedial corner,
medial side, as well as the intercondylar region and remainder of the
interior of the joint.
 |
|
Figure 91.12. Anteromedial incision.
|
 |
|
Figure 91.13. Lateral incision.
|
is avulsed from the femur, by advancing the ligament stump into its
bony attachment. Treat midsubstance PCL tears by primary reconstruction
with a patellar tendon bone (PTB) graft and midsubstance ACL tears with
doubled semitendinosis and gracilis grafts. An alternate method
advocated by Shelbourne et al. is to reconstruct only the PCL, leaving
the ACL to be reconstructed on a delayed basis in the hope of
minimizing postoperative stiffness (28). In our
experience it is difficult to tension the PCL adequately while
maintaining normal tibiofemoral alignment in the absence of the ACL. We
utilize Clancy’s method of simultaneously tensioning both ACL and PCL
at 20° of knee flexion to achieve neutral positioning of the knee (see Chapter 90).
midsubstance tears with nonabsorbable suture. Repair of the capsule is
crucial for protecting the cruciate repairs. The capsule is often
avulsed from one side of the joint. Drill holes placed in the AP plane
are satisfactory for posterior capsule avulsions. Fix the capsular and
collateral ligament repairs with the knee in 30° of flexion; secure the
posterior capsule with the knee at no greater than 15° of flexion to
avoid limitation of knee extension.
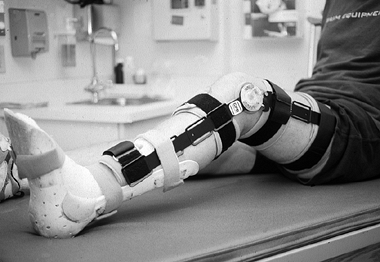
decompress any external fascial bands, as there is approximately a 40%
chance of spontaneous partial or complete recovery (9,10,17,30,31,32 and 33). Postoperatively, incorporate an ankle–foot orthosis (AFO) into the hinged knee brace (Fig. 91.14). If the nerve is disrupted (Fig. 91.15),
tag the ends for later grafting. Unlike transection injuries, the
extent of damage cannot be accurately assessed immediately because of
proximal and distal hemorrhage. Satisfactory results have been reported
when surgery was delayed for 3 months (37).
 |
|
Figure 91.14.
Hinged knee brace incorporating AFO to maintain ankle in neutral position in patient with knee dislocation and complete peroneal nerve palsy. |
 |
|
Figure 91.15. Stretch-and-tear injury to the common peroneal nerve results in “mop ends” that are difficult to reapproximate.
|
arthroscopy can be used to identify associated articular and meniscal
injuries. Arthroscopic inspection of the knee usually requires less
than 5 min, provided that gravity inflow is used, and therefore poses
little risk of fluid extravasation into the calf. Although arthroscopic
cruciate reconstruction can be performed in selected cases when the ACL
and PCL ligaments are torn and the capsule and the collaterals are for
the most part intact, most knee dislocations
involve
significant capsular and collateral tears that require open surgery. In
these cases, we prefer to use arthroscopy for diagnosis only and
perform repairs and reconstructions using open technique utilizing
arthroscopic guides and instruments as described below.
-
Repeat the ligamentous examination of the
knee to confirm the preoperative assessment. Administer a prophylactic
antibiotic (cefazolin). Prep and drape both lower extremities free to
determine correct AP postioning using lateral radiographs and
observation of the normal knee’s tibial plateau to femoral condyle
relationship. Tourniquet use should be cleared by the vascular surgeon
in cases with arterial injury and repair. Inflate the tourniquet no
higher than 275 mm Hg. -
With the knee slightly flexed, start the
incision 5 cm above the patella, extending it over the medial border of
the patella, parallel to the medial aspect of the patellar tendon, and
ending at the border of the pes anserinus, about 6 cm below the medial
joint line. Open the medial retinaculum incorporating any tears,
beginning at the superior border of the pes anserina tendons near the
tibial tubercle. Identify the MCL and its site of rupture (usually from
the medial femoral epicondyle or midsubstance) and continue to open the
retinaculum along the sartorius toward the posterior corner of the knee
to the vastus medialis muscle. -
At this point, swing the retinacular
incision proximally toward the adductor tubercle in the interval
between the medial gastrocnemius and the posterior oblique ligament.
Open the joint anteriorly alongside the medial border of the patellar
tendon. Retract the fat pad inferiorly, the MCL and medial capsule
medially, and the patellar ligament and patella laterally to inspect
the notch. It may be necessary to extend the capsular incision
proximally to the midpoint of the patella. -
Remove any chondral debris and inspect
the medial meniscus. To visualize the lateral meniscus, flex the hip to
90° and position the knee in the figure-of-four position. -
If the ACL is avulsed from the tibia or
femur, place at least two sutures (#2 nonabsorbable) through the
avulsed end of the ligament. For a tibial avulsion, pass the sutures
through parallel drill holes placed in the curetted central bed of the
tibial ACL attachment, using a tibial aiming device (Fig. 91.16). If the ACL is avulsed from the femur, maximally flex the knee and similarly place sutures in the torn end.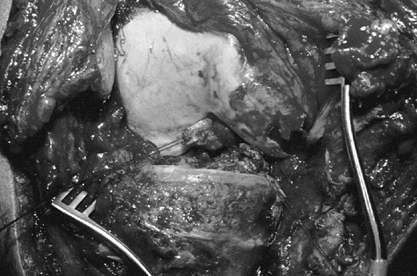 Figure 91.16. Avulsion of ACL from tibia held with #2 nonabsorbable suture. Notice anteromedial capsular stripping, exposing proximal tibia.
Figure 91.16. Avulsion of ACL from tibia held with #2 nonabsorbable suture. Notice anteromedial capsular stripping, exposing proximal tibia. -
Expose the distal lateral femur by
subcutaneous dissection through the prepatellar bursa and incise the
iliotibial band at its midpoint, proximal to the flare of the lateral
metaphysis, staying above the intermuscular septum. Elevate the vastus
lateralis from the femur and retract it anteriorly. -
For femoral avulsions of the ACL, use a
drill guide to insert, from outside in, parallel 3 mm Kirschner wires
at the femoral insertion of the ACL (at the junction of the roof and
wall of the notch, 2 to 3 mm anterior to the over-the-top position).
Using a suture hook, deliver the sutures previously placed in the torn
ligament to the lateral femur. -
If the ACL is a mop-end or midsubstance tear, reconstruct it with doubled hamstring tendons (Chapter 89). Do not fix the ACL repair or graft until the PCL is addressed.
-
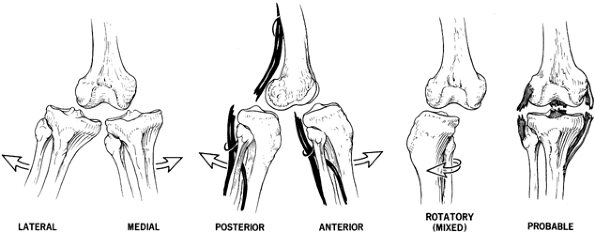
If the PCL is avulsed from the femur (Fig. 91.17A),
place multiple sutures, similar to the ACL, in the torn end and pass
them through parallel drill holes 8 mm posterior to the articular
cartilage and at the 10:30 (L knee) or 1:30 (R knee) position on the
medial femoral condyle (Fig. 91.17B).![]() Figure 91.17. A: Avulsion of PCL from femur with long stump of ligament remaining intact. B: Avulsed PCL after repair through bony tunnel with sutures tied over 14 mm button.
Figure 91.17. A: Avulsion of PCL from femur with long stump of ligament remaining intact. B: Avulsed PCL after repair through bony tunnel with sutures tied over 14 mm button. -
If tibial avulsion of the PCL has
occurred, enter the joint through the usual tear or make an incision in
the posteromedial capsule. Incise the inferior aspect of the
posteromedial capsule along the upper tibia and identify the PCL bed.
Place a tibial aiming device for the PCL through the notch into the
tibial attachment site, staying on the lateral edge, and drill a 3 mm
Kirschner wire to this point from the anteromedial tibia, starting
immediately below the tibial tubercle. Make sure that there is
sufficient spread between tibial tunnels for the PCL and an ACL graft
to avoid convergence or fracture. Protect the contents of the popliteal
fossa with a retractor or fingertip through the posteromedial incision.
Overream the guide wire with a 6 mm cannulated drill and deliver the
sutures placed in the torn end of the PCL through this tunnel with a
suture-passer. -
Reconstruct a midsubstance rupture of the PCL with an autogenous patellar tendon bone graft as described in Chapter 90.
-
Provisionally tension and fix the
cruciate repairs/reconstructions simultaneously using an assistant.
Position the knee in 20° of flexion to restore the normal tibiofemoral
relationship. Lateral radiography of the injured and uninjured knees
may be needed. -
Sutures around posts or tied over buttons
allow repeated tensioning and graft retightening as needed to restore
normal AP tibiofemoral position. -
After the cruciate ligaments have been
provisionally addressed, repair the medial structures. Avulsion of the
posteromedial capsule is usually from the tibia. Repair with sutures
(#2 nonabsorbable) placed from anterior to posterior along the upper
medial tibial plateau. If needed, reflect the retinacular layer from
posterior to anterior to expose the MCL at the level of the medial
femoral epicondyle and the joint. Gentle distal retraction of the pes
tendons permits inspection of the MCL tibial attachment. -
Inspect the medial capsule and ascertain
the status of the medial meniscus from inside the joint, using both the
anteromedial and posteromedial capsular incisions. Repair the meniscus
to the medial capsule (coronary ligaments) with vertical mattress
sutures (#1 nonabsorbable). -
Fix MCL avulsions from the tibia or femur
with a 6.5 mm cancellous screw and a soft-tissue spiked washer. Repair
midsubstance injuries with whipstitch sutures (#2 nonabsorbable).
Repair the posteromedial capsule incision or injury in vest-over-pants
fashion using horizontal mattress sutures (#2 nonabsorbable) in 15° of
flexion. -
Release the tourniquet before final
closure. Close the iliotibial band, medial retinacular layer, and
anteromedial capsular incision with absorbable sutures. Place drains in
the subcutaneous layer. Reapproximate the subcutaneous layer with
minimal sutures, and close the skin.
-
Use positioning, draping, and tourniquet as described above.
-
Make two incisions—midlateral and
anteromedial—separated by more than 7 cm. Make the lateral incision
first, starting 7 cm proximal to the lateral femoral epicondyle in line
with the posterior edge of the ilial–tibial band (ITB). With the knee
flexed to 90°, curve the incision distally to pass over the anterior
portion of the fibular head. -
With blunt dissection, elevate the
posterior subcutaneous flap in the proximal part of the incision.
Identify the peroneal nerve as it exits under the biceps; distally, the
ITB and biceps insertion are frequently avulsed or torn (Fig. 91.18).
Follow the peroneal nerve distally. If it is stretched, divide the
fascial roof at its entrance into the anterolateral leg near the
fibula. If it is torn, tag the ends for delayed reconstruction.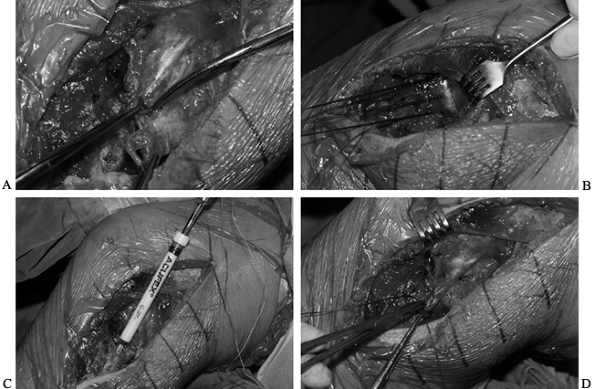 Figure 91.18. Extensive disruption of lateral structures. A: Avulsion of biceps (bottom clamp) and avulsion of FCL from fibular head (upper clamp). B:
Figure 91.18. Extensive disruption of lateral structures. A: Avulsion of biceps (bottom clamp) and avulsion of FCL from fibular head (upper clamp). B:
Insertion of three suture anchors in upper lateral tibia to repair
tibial coronary ligament and lateral capsule (retracted to show lateral
meniscus rim and joint). C: Inserting suture anchor in fibular head. D: Lateral capsule repaired; inserting suture in avulsed end of FCL. -
Identify tears in the lateral capsule.
This often is avulsed as a single sheet from one side of the joint. If
not avulsed, open the capsule behind the FCL, which is avulsed or torn
in its midsubstance. Repair the meniscus using vertical mattress
sutures (#1 nonabsorbable). -
Find and repair the popliteus. It may be
necessary to make an anterolateral capsular incision if the popliteus
is torn from its femoral attachment. When opening the thin layer of
capsule overlying the popliteus, avoid injury to it. Repair the
popliteus and capsule with suture anchors (#2 nonabsorbable). -
Approach the medial knee as previously
described using a curved skin incision centered over the medial femoral
epicondyle and extending along the midmedial leg, maintaining at least
7 cm between the two incisions.
-
Perform surgery as described above using two incisions.
-
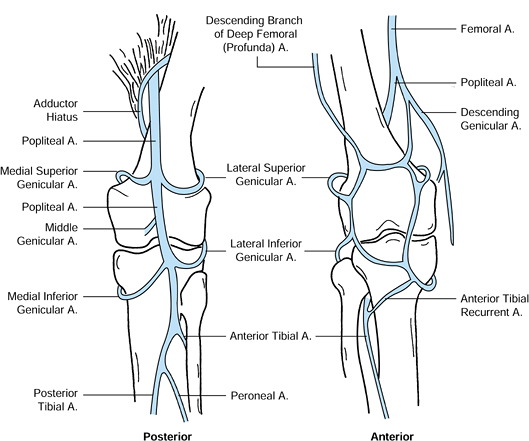
In this injury expect to find the
extensor mechanism torn. Inspect the patellar tendon using gentle
subcutaneous dissection from the anteromedial incision. Repair
midsubstance rupture of the patellar tendon with interrupted
whipstitches (#2 nonabsorbable) reinforced by two or more interlocking,
horizontal weaving (Krackow) sutures (#2 nonabsorbable) placed through
drill holes in the patella or tibial tubercle, depending on where the
tear is located (Fig. 91.19) (11).
Repair avulsion injuries with similar interlocking sutures passed
through drill holes in the respective bony attachment. Tighten all
repairs to allow knee flexion to 60°. Do not use cerclage sutures.![]() Figure 91.19.
Figure 91.19.
Ligament fixation. Placement of the suture in a tendon. (Redrawn from
Krackow KA, Thomas SC, Jones LC. A Stitch for Ligament–Tendon Fixation.
J Bone Joint Surg [Am] 1986;68:764.)
-
This injury is not operated early. After
motion has been regained (>120°), perform open or arthroscopic
assisted reconstruction of both ligaments. -
These procedures are described in detail in Chapter 89 and Chapter 90. A few technical aspects deserve emphasis, however.
-
For the PCL, use autogenous PTB, allograft PTB, or Achilles.
-
For the ACL, use autogenous hamstrings,
allograft PTB, or an achilles tendon graft. We prefer autogenous PTB
for the PCL and doubled hamstrings for the ACL. -
Position the tibial tunnels carefully to
avoid convergence. Place the PCL tibial tunnel inferior to the tibial
tuberosity in the midline and the ACL tibial tunnel medial, midway
between the posteromedial tibial brim and the tibial tuberosity. -
Pass the PCL graft first. Tension the
grafts simultaneously with the knee at 20° of flexion. By using suture
fixation around a post or over a 14-mm button, readjustment of graft
tension is easy to accomplish. Simultaneous tensioning of the grafts
aids in defining the neutral position of the tibia in relation to the
femur.
-
At the completion of surgery, position
the knee in near extension, avoiding hyperextension and using splints
incorporated into a bulky R-J dressing from foot to groin. Elevate the
extremity for 48 h, monitoring the neurovascular condition of the limb
and remaining alert to the potential for compartment syndrome. -
Remove the drains by 48 h and replace the
bulky dressing with a well-fitting, adjustable-hinged knee brace that
is locked at 0° but allows motion from 0° to 45° during exercises. Do
not allow the knee to hyperextend. -
At 2 to 3 days, start continuous passive
motion (CPM) for 2-h sessions four times daily. Flexion in this range
does not significantly increase strain in the PCL. If possible,
continue CPM for at least 72 h in the hospital and preferably for an
additional week at home. -
At 10 to 14 days, increase passive
flexion to 60°. Use passive heel slides for flexion, but active
extension can be performed from 60° to 0°. -
At 3 weeks start intermittent passive flexion to 90°, but restrict active flexion to 60°.
-
Keep the brace locked in extension at all
other times for the first 6 weeks, during which partial weight bearing
is allowed. During this 6 weeks, use electrical stimulation, isometric
quadriceps exercises, and straight-leg raises. -
At 6 weeks unlock the brace for unlimited
motion and ambulation if the patient can control the knee with the
quadriceps. At 6 weeks the brace is not necessary for sleeping or
sitting in a safe environment. -
Continue bracing for another 2 to 3 weeks
or longer, depending on patient preference. Thereafter, perform
exercises in accordance with the protocol(s) for cruciate ligament
injuries (Chapter 89 and Chapter 90).
of the knee until 6 weeks. Delay resistive quadriceps exercises until 3
months.
weeks to minimize distraction of the lateral compartment with weight
bearing. Use passive knee flexion only for the first 6 weeks, and no
resistive hamstring exercises should be performed until 3 months after
surgery.
the results of the different methods of treating ligamentous injuries
in the dislocated knee. The long-term incidence of degenerative
arthritis remains unknown. Historically, a stable knee with 85° of
flexion was considered a good result, and 105° was regarded as an
excellent result. More recent studies have demonstrated improved
results with early surgical repair/reconstruction and immediate motion (4,20,26,27,31).
near dislocations, we have observed acceptable short- and midterm
results (2 to 10 years) following early surgical repair/reconstruction
of all torn ligaments combined with early motion of the knee in
cooperative, active patients. With this regimen, 80% of operated
patients can be expected to have 1 + or less total AP laxity and only
trace to 1 + medial–lateral knee laxity with an arc of motion of 120°.
This has allowed return to activity in nearly 75% of patients, although
only 50% are able to resume preinjury activity levels without symptoms.
amputation acutely and the development of chronic claudication if
perfusion is incompletely restored. Nerve injury frequently results in
sensory and motor abnormalities of the leg and foot. As previously
noted, the majority of patients (60%) do not experience any improvement
over time. Weakness or absent peroneal nerve function leaves the
patient with a foot drop that usually requires an AFO, although tendon
transfers or hindfoot arthrodesis may be used in certain cases.
and degenerative joint disease are the major problems the orthopaedic
surgeon must be prepared to deal with after initial injury and
treatment. Although early motion minimizes the risk of stiffness, the
intense fibroblastic response to injury may not be held in check. As
many as 30% to 50% of patients may require treatment intervention to
regain motion (20,27,31).
If loss of extension is 10° or more at 4 weeks, and/or flexion is less
than 90° and not improving at 6 weeks, then arthroscopic release of
adhesions and gentle manipulation should be tried. Delay in treatment
of limited motion in the postoperative period makes later treatment
more difficult and often requires extensive soft-tissue releases.
cruciate ligaments and repair and reefing of the capsule and collateral
ligaments. When repair is not possible, perform Clancy’s biceps
tenodesis for posterolateral instability (14) and reconstruct the MCL with a free hamstring or PTB graft in cases of chronic medial laxity (13). Progression of degenerative changes may require osteotomy or even joint replacement at a later time.
a multidisciplinary approach. After satisfactory stabilization of the
patient and treatment of any associated vascular injury, obtaining a
stable knee with functional motion is the next goal. This requires
accurate clinical assessment and good imaging to formulate an operative
plan. It is important that the patient understand that a normal knee is
not expected following such a severe injury. With technically
well-performed surgical repair and/or reconstruction, early motion can
be initiated, which is crucial in reducing postoperative stiffness. In
our experience this provides the best short-term results. Nonetheless,
the patient remains at risk for developing degenerative changes over
time.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
DE, Speer KP, Wickiewicz TL, et al. Complete Knee Dislocation without
Posterior Cruciate Ligament Disruption. A Report of Four Cases and
Review of the Literature. Clin Orthop 1992;284:228.
FG, Marshall JL, al Monajem ARS. The Cruciate Ligament of the Knee
Joint: Anatomical, Functional and Experimental Analysis. Clin Orthop 1975;106:216.
JD, Gillham NR. Injury to the Popliteal Artery Associated with
Dislocation of the Knee: Palpable Pulses Do Not Negate the Requirement
for Arteriography. Injury 1989;20:307.
MH, Moore TM, Harvey JP Jr. Follow-up Notes on Articles Previously
Published in the Journal: Traumatic Dislocation of the Knee Joint. J Bone Joint Surg [Am] 1975;57:430.
MS, Freedman EL. Allograft Reconstruction of the Anterior and Posterior
Cruciate Ligaments after Traumatic Knee Dislocation. Am J Sports Med 1995;23:580.
A, Arden P, Rainey HA. Traumatic Dislocation of the Knee. A Report of
40 Cases, 3 Cases with Special Reference to Conservative Treatment. J Bone Joint Surg [Br] 1972;54:96.
ACL, anterior cruciate ligament; MCL, medial collateral ligament; LCL,
lateral collateral ligament; PCL, posterior cruciate ligament.