AMPUTATIONS OF THE HAND
Department of Orthopaedic Surgery and Rehabilitation, Loyola University
Chicago Stritch School of Medicine, Maywood, Illinois, 60153.
patient and the surgeon. Nonetheless, a carefully planned and
skillfully executed surgical procedure is essential for early
restoration of pain-free, useful hand function. The ultimate goal of
surgery is the restoration of a hand of acceptable appearance, capable
of the highest degree of function consistent with its remaining
musculoskeletal elements (1,27).
prompt wound healing and joint mobility in digits of maximal length.
The surgeon must take care to preserve sensibility in retained elements
and to prevent formation of painful neuromas.
precision prehension, preservation or restoration of the thumb is of
paramount importance. When the radial fingers are compromised,
precision prehension is impaired, while loss of the ulnar digits
reduces effective power grip (12). Preservation
of length and sensibility is vital to radial digits, whereas
preservation of joint mobility is more important to ulnar digits.
elective, by the mechanism of injury or etiology, or by the anatomic
region of the hand removed. Secondary revision of initially emergent
amputations may be elected to address issues of appearance, function,
or pain.
amputation of portions of the hand. The management of acute traumatic
amputation requires considerable judgment. The surgeon must often
decide which parts should be
retained
by revascularization or replantation, which should be managed with
direct wound closure, and which should be managed primarily by more
proximal surgical amputation.
the likelihood of success with different treatment strategies. Sharp
injuries preserve normal tissues in the proximal part and have a narrow
zone of injury. Distal tissues that may be amenable to reattachment or
revascularization are more likely to be preserved. Crush injuries often
result in a wide zone of injury. Though the skin sleeve may have been
preserved, the profound crushing of underlying bone, joint, and flexor
and extensor tendons may preclude reestablishment of a supple, mobile
digit. Avulsion injuries may result in substantial injury to
neurovascular and tendinous structures proximal to the level of skin
loss or disruption. Examination of amputated parts may aid in
understanding the extent of injury to the residual parts of the hand or
fingers.
easiest, initially, to preserve all viable tissue. Otherwise useless
digits may be converted to fillet flaps for soft-tissue coverage or to
supply digital nerve and bone for graft to be used in other digits.
Although this approach is by design conservative, it will prove
counterproductive if the decision to delete functionless digits is
repeatedly postponed. Retained stiff, insensate, or unstable digits
will compromise the rehabilitation of the remaining, less severely
affected portions of the hand. Also, the original decision to delete
the irreparably compromised digit may be questioned and additional
futile surgeries performed in an attempt to avoid amputation. Early,
appropriate decision making is often difficult: Less experienced
surgeons should seek prompt consultation to establish realistic
expectations for both themselves and their patients.
microvascular or macrovascular disease or a combination of the two.
Microvascular disease, seen commonly in conditions such as scleroderma
and diabetes mellitus, may result in digital ischemia. Irreversible
digital ischemia may also result from macrovascular injury to the
brachial artery after cardiac catheterization in the presence of
systemic atherosclerotic macrovascular and microvascular disease.
amputation. The aim may be either to eliminate a refractory focus of
infection, usually osteomyelitis, or to remove a part whose function
has been irreparably compromised by infection. A painful, swollen
finger rendered immobile after flexor sheath infection may occasionally
be so impaired that the surgeon and patient elect digital amputation.
The histologic character of the tumor and its anatomic location should
be the primary determinants of the level of amputation. The desire to
preserve functional capability must be subservient to the need for
appropriate tumor wound margins (see Chapter 74). Amputation may be confined to a single digit, a ray, or a more major segment of the hand—radial, central, or ulnar.
improved functionally or aesthetically by the amputation of rudimentary
digits. Small, floppy nubbins may be excised when they are insufficient
for reconstruction. When macrodactyly distorts hand form and function,
resection of one or two rays may be indicated. In cases of polydactyly,
amputation of redundant elements must be carefully integrated with
reconstruction of the remaining digits.
Frostbite injury characteristically affects the distal portions of the
fingers. The thumb is less often involved since it is shorter than the
fingers and is often protected by the fingers flexed around it against
the palm. Patients who have experienced severe cold exposure may
experience the effects of ischemia involving all the fingers, both
thumbs, and all toes of both feet, profoundly limiting secondary
reconstruction alternatives. The extent of remaining viable tissue is
often uncertain for a number of days. In selected severe injury, bone
scan or magnetic resonance imaging (MRI) may reveal preservation of
osseous circulation in spite of overlying skin necrosis.
structures, skin, and extensor mechanism without necessitating
amputation. Electrical injury, by contrast, may have a more profound
effect on deep tissues than on the skin. Early resection of the finger
or ray that transmitted the electrical impulse is often necessary.
Residual functional impairment after electrical injury may lead to
secondary amputation.
reconstructive surgical procedures in favor of prosthetic management.
When a hand is painful, deformed, and without function, amputation may
be the most effective reconstructive procedure (2).
-
Design skin incisions and skin flaps to provide sensate skin over the palmar surface of the residual digit.
-
Isolate each digital nerve in the
involved digit. Apply modest traction to the nerve, and sharply divide
the nerve, allowing it to retract proximally into soft tissue. -
Identify transected tendons and draw them
distally into the wound. Sharply divide each tendon and allow it to
retract proximally. Do not sew flexor or extensor
P.1453
tendons
to one another over the end of the amputated digit. To do so will
restrict motion in the residual portion of the digit and severely
compromise tendon excursion and motion in adjacent fingers (see the
discussion of the “quadriga” effect in the section below, Pitfalls and Complications). -
Ligate bleeding vessels at wound margins.
-
Traumatic amputations that create oblique
or jagged distal surfaces may result in a painful digit. Trim bone ends
transversely and free them of palmar prominences.
strength, and length that allow the thumb to carry out its unique range
of activity (13). Motion, sensibility, and appearance are important but less vital attributes of normal thumb function.
role in prehension, preserving thumb length is a priority in the
treatment of traumatic thumb injuries. A well-motored stiff thumb with
basilar mobility and normal length is effective in most functions of
the hand.
the distal phalanx, local flap closure may be required. With
disproportionate palmar skin loss, the Moberg palmar advancement flap
allows preservation of thumb length with advancement of sensate skin
distally (5). The radial nerve–innervated
cross-finger flap from the dorsum of the index finger also brings
sensate skin to the distal phalanx (see Chapter 38).
portion of the proximal phalanx or beyond, satisfactory function may be
achieved if maximal length is preserved with local advancement flaps.
severely compromises prehension. Although thumb length may be
sufficient for buttressing of objects in the palm in power grip, it is
insufficient to reach the tips of adjacent fingers in precision
prehensile activities. Secondary surgical reconstruction is usually
advantageous when amputation occurs proximal to the middle of the
proximal phalanx of the thumb. In such situations, the sacrifice of a
few millimeters of skeletal length to allow direct soft-tissue closure
over bone is usually preferable to extensive primary soft-tissue flap
procedures. Once healing of the amputation has been achieved,
reconstruction will be required to restore at least a portion of the
lost thumb length.
of a thumb that has sustained amputation injury include phalangization,
distraction lengthening, and pollicization, as well as toe-to-hand and
wraparound flap microvascular transfers (see Chapter 34, Chapter 35 and Chapter 36 and Chapter 69).
other digits that could achieve pulp-to-pulp contact with the thumb, it
makes little sense to lengthen the thumb beyond the arc of the
remaining fingers. Phalangization restores primitive prehension to the
hand. To be successful, it requires supple dorsal skin, normal thenar
musculature, and a mobile carpometacarpal joint (24).
-
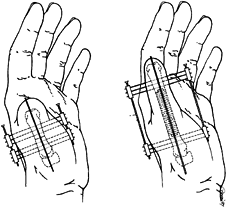
Make a Z-shaped
incision that provides generous web-space exposure and allows flap
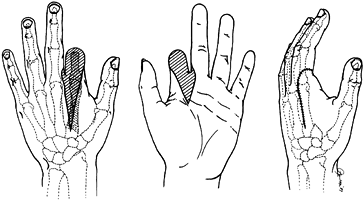
transposition, which shifts the web-space skin margin proximally (Fig. 46.1). Define the adductor pollicis and first dorsal interosseous muscles, and incise and release their investing fascia.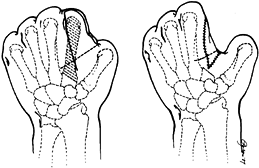 Figure 46.1. Phalangization procedure. A: Resection of the index metacarpal is achieved through Z-plasty flap elevation. B: Z-plasty flap transposition increases the exposed prehensile surface of the thumb.
Figure 46.1. Phalangization procedure. A: Resection of the index metacarpal is achieved through Z-plasty flap elevation. B: Z-plasty flap transposition increases the exposed prehensile surface of the thumb. -
Resect the index metacarpal, taking care
to preserve the proximal attachment of extensor carpi radialis longus
and flexor carpi radialis. Excise the first dorsal and first palmar
interosseous muscles. -
Release the adductor pollicis insertion
from the sesamoid at the metacarpophalangeal (MP) joint level and
reinsert it more proximally on the thumb metacarpal. Transpose skin
flaps. See Hints and Tricks box on the next page.
with good soft-tissue coverage, distraction lengthening is an effective
technique for regaining useful thumb length (8,16).
If proximal joint mobility and thenar musculature are preserved, the
patient should be able to use the thumb effectively for prehensile
activity, although it may be stiff.
-
A simple three-digit prehension pattern
may be recreated by the removal of the ring metacarpal. This procedure
increases the mobility and independence of the little-finger metacarpal. -
Flexion and closing-wedge osteotomy with
radial deviation of the base of the little-finger metacarpal may
improve pinch between the little metacarpal and the thumb metacarpal (6).
-
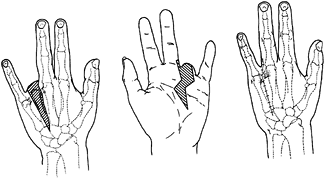
Make a longitudinal skin incision to expose the middle third of the thumb metacarpal (Fig. 46.2)
and incise the periosteum. Bunch up the skin between the pin insertion
sites such that distraction will not put undue pressure on the skin–pin
interface. Insert two parallel groups of pins transversely through the
collapsed distraction apparatus in close proximity to the intended
osteotomy site.![]() Figure 46.2. Thumb distraction lengthening in an adult. A: Place pin groups adjacent to the mid-diaphyseal osteotomy site. B:
Figure 46.2. Thumb distraction lengthening in an adult. A: Place pin groups adjacent to the mid-diaphyseal osteotomy site. B:
Once the desired distraction has been achieved, lock the bone graft
into the medullary canal of the distracted proximal segments. -
Make a transverse osteotomy through the middle third of the metacarpal.
-
Place a longitudinal pin through the
proximal and distal metacarpal segments and across the carpometacarpal
joint. By transfixing the metacarpal to the trapezium, this pin
provides resistance to the tendency of distraction to tighten the
adductor and produce secondary adduction contracture. The longitudinal
pin also prevents subluxation of the base of the thumb metacarpal on
the trapezium with distraction. -
If bone grafting is planned as a second
procedure, circumferentially incise the periosteum at the level of the
osteotomy, and then turn the screws on the distraction device to create
at least 5 mm of immediate distraction at the osteotomy site. -
If distraction osteogenesis is to be
employed, repair the longitudinal incision of the metacarpal periosteum
and then close the skin. Maintain osteotomy coaptation for 7 to 10
days, and then begin distraction of the osteotomy. Over the next 4 to 5
weeks, gradually lengthen the digit by advancing the distraction device
about 1 mm per day; do this four times a day, in ¼ mm increments. The
soft tissues will gradually stretch as the osteotomy gap is widened.
Distraction takes place along the axis provided by the longitudinal
pin. It is often possible to gain up to 3 to 3.5 cm of additional thumb
length with distraction lengthening (8,17). -
Although bone consolidation may occur
spontaneously in young patients, my custom in adults is to electively
add iliac crest bone graft to span the gap between the proximal and
distal metacarpal segments. Keep the device in place until graft
incorporation is radiographically visible. Web-space deepening, as
described above in the section on phalangization, is occasionally helpful as a secondary procedure. -
Alternatively, remove the distraction
device after distraction, and stabilize the bone graft by plate
fixation. Transfer the insertion of the adductor pollicis tendon more
proximally to help diminish the tendency of the lengthened thumb to
adduct. This allows web-space deepening without sacrificing adductor
pollicis strength.
length and mobility, it is often recommended when traumatic thumb
amputation results in basilar joint destruction (3,4,13).
The index finger is usually the digit selected for pollicization. When
the extent of trauma to the thumb has been severe enough to warrant
pollicization, the adjacent index finger is often also compromised, but
this is not necessarily a contraindication to pollicization. An injured
digit with limited mobility may be a liability in the index position
but may substantially enhance function when transposed to the thumb
position.
similar to that of pollicization for the congenitally absent or
hypoplastic thumb with individual modifications (see Chapter 69).
If there is extensive scarring and soft-tissue loss over the radial
border of the hand, preliminary flap coverage may be required.
-
Skin incisions must be individualized
when skin along the radial border of the hand is scarred. Design skin
flaps to bring the best skin—palmar, dorsal, or a combination—into the
web space created between the pollicized digit and the middle finger at
the time of closure.
P.1455
Skin graft is often necessary dorsally and radially but should be avoided in the web space. -
Evaluate digital artery integrity of the
index and middle fingers preoperatively by arteriography when there has
been proximal injury. In some instances, the vascularity to the injured
index finger may be insufficient to support disruption of collateral
flow necessitated by pollicization. In such cases, plan to use a vein
graft from the radial artery in the anatomic snuff box to the digital
arteries of the transposed digit to effect microvascular
revascularization of the digit. -
Identify and preserve the radial and
ulnar index digital nerves and arteries. Preserve the digital nerves by
splitting the common digital nerve to the index and middle fingers.
Mobilize the ulnar proper digital artery to the index by ligating the
radial proper digital artery to the middle finger. -
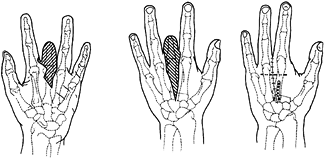
In adult pollicization, reestablish skeletal length by combining remaining thumb and index parts (Fig. 46.3).
The goal is to achieve a reconstructed thumb whose tip extends to about
75% of the length of the proximal phalanx of the middle finger. If the
index is of normal length and the thumb basilar joint is absent, use of
the rotated index metacarpal head as a trapezium will prove most
satisfactory.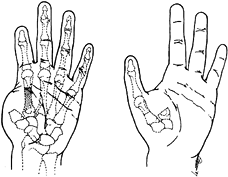 Figure 46.3. Pollicization of a distally amputated index finger. A: The extent of index metacarpal resection depends on the residual length of both the thumb metacarpal and the index finger. B: Fix the transposed index metacarpal to the proximal thumb metacarpal remnant.
Figure 46.3. Pollicization of a distally amputated index finger. A: The extent of index metacarpal resection depends on the residual length of both the thumb metacarpal and the index finger. B: Fix the transposed index metacarpal to the proximal thumb metacarpal remnant. -
When the trapezium and part of the thumb
metacarpal remain, resect the entire index metacarpal and an
appropriate portion of the proximal phalanx. Secure the proximal
phalanx directly on top of the thumb metacarpal remnant. When the
distal portion of the index has been damaged, retain an appropriate
metacarpal length to achieve a composite digit of proper length. Retain
the index metacarpophalangeal joint to provide thumb MP motion, while
the proximal interphalangeal joint of the index will provide an
interphalangeal joint for the reconstructed thumb. -
When the basilar joint and thenar
musculature are absent, carry out a musculotendinous rearrangement as
in pollicization for thumb aplasia. Advance the first dorsal and first
palmar interossei insertions distally on the hood and shorten the
extensor tendons. If the first dorsal interosseous muscle has been
damaged, consider simultaneous opponensplasty tendon transfer. When the
index digit is damaged distally and is merely being moved radialward
without skeletal shortening, extensor tendon shortening may not be
required. -
In adult pollicization, the flexor
tendons to the pollicized digit will not spontaneously shorten and
readapt their optimal resting length as occurs in pediatric
pollicization. Make an incision in the distal forearm and resect a
segment of index flexor tendon consistent with the extent of proximal
transposition of the pollicized index finger.
When amputation occurs at or proximal to the distal interphalangeal
joint, distal flap coverage is rarely indicated. Modest bone shortening
and contouring are usually preferable, unless the potentially
sacrificed bone length is judged critical to preservation of the
functional integrity of the affected finger.
insertion will continue to contribute effectively to grasp activity.
When amputation occurs more proximally (e.g., proximal middle phalanx,
proximal phalanx), the digit will have only limited value in the
little-finger position and will probably be a nuisance in the index
position. When amputation occurs proximal to the superficialis but
distal to the midproximal phalanx, preservation of the digit in the
middle or ring position may help prevent small objects from falling
through the hand, although only limited MP joint flexion will occur
through the pull of the intrinsic muscles.
compromised multiple digits, it is best to preserve all available bone
length. In multidigit degloving injuries, distant flap overage may be
indicated.
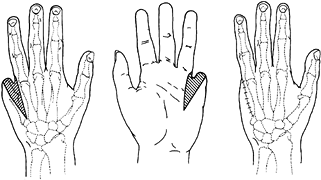
attention to bone as well as to soft tissue to avoid a bulbous distal
contour (Fig. 46.4).
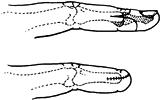 |
|
Figure 46.4. Interphalangeal joint disarticulation amputation. A: Remove palmar condylar prominences. B: The greater length of the palmar flap brings the suture line away from the contact surface.
|
-
Create palmar and dorsal tongue-shaped
flaps by bilateral midlateral incisions. Make the palmar flap slightly
longer, if possible, so that the scar will be dorsal. Pull tendons
distally and divide them sharply. -
Gently divide digital nerves without
applying undue traction, and allow them to retract into proximal soft
tissues. Ligate digital arteries. -
Identify the palmar plate and excise it. Remove the cartilage from the exposed phalangeal articular surface to
P.1456
facilitate bone contouring. Resect the palmar condylar prominences in
line with the palmar cortex of the diaphysis. Shape the remaining flat
condylar surface with a rongeur and rasp to resemble a paddle. Palpate
the bone through the overlying skin to ensure that all prominences have
been relieved. -
Close the skin with interrupted sutures.
Extensive contouring of skin margins is unnecessary, since the skin
contour will gradually model to the underlying bony contour. -
Handle diaphyseal phalangeal amputations in a similar fashion.
manipulate objects. Imperfections of the index finger are, however,
poorly tolerated. When the index finger of an otherwise normal hand is
compromised by loss of length, altered sensibility, or pain, many
patients spontaneously shift to a prehension pattern that ignores the
index finger in preference of a normal middle finger. The greater
length of the middle finger allows it to meet the thumb easily for
precision activity. When a short index finger is being ignored, it is
often held in a hyperextended posture. Amputation of a short index
finger is advised when patterns of disuse become fixed.
either MP joint disarticulation or index ray resection. MP joint
disarticulation preserves the breadth of the palm, which is helpful in
stabilizing objects held with a cylindrical grip but presents an
obtrusive prominence in the web space (18). Ray resection narrows the palm and improves the appearance of the hand by achieving a broad, smooth web-space contour.
If the wedge of skin removed is too large, the distance from thumb to
middle metacarpal will be diminished and thumb abduction may be
limited. Dissect skin flaps from the index digit, taking care to
preserve flap innervation.
 |
|
Figure 46.5. Index ray resection. A: Dorsal view. B: Palmar skin resection. C: Wound closure preserves sensate skin throughout the widened web space.
|
-
Divide the extensor indicis proprius
tendon from its insertion ulnar to the index communis tendon and tag
it. Apply traction to the extensor digitorum communis tendon, divide
it, and allow it to retract. -
Osteotomize the index metacarpal
obliquely through the proximal metaphysis, preserving the insertion of
the extensor carpi radialis longus and flexor carpi radialis tendons. -
Although some authors advocate suturing
the first dorsal interosseous tendon into the second dorsal
interosseous insertion on the middle metacarpal to enhance the strength
of lateral pinch, this transfer is occasionally too strong and may
result in a fixed radial deviation and lumbrical plus (see Pitfalls and Complications, below) posture of the middle finger. -
Divide the deep transverse metacarpal
ligament adjacent to the middle finger. Identify the index flexor
tendons, pull them distally, divide them, and allow them to retract
proximally. Take care in dealing with the digital nerves: The radial
nerve to the index finger must not be extensively mobilized. Sharply
divide digital nerves and allow them to retract into the soft tissue
without tension. The ultimate neuroma end of the nerves must be
distanced from further trauma. -
Remove the index finger. Sew the extensor
indicis proprius into the middle finger extensor digitorum communis
tendon at the level of its insertion to enhance independence of
middle-finger extension. Trim the first dorsal and first palmar
interosseous muscles as necessary to ensure a smooth web-space contour.
Close the skin flaps with the thumb in palmar and radial abduction.
cup small objects in the palm of the hand because of the tendency of such objects to escape from the grasp (Fig. 46.6) (4). Ray resection and reconstruction by either soft-tissue coaptation (Fig. 46.7) or ray transfer (Fig. 46.8) closes this gap and improves the aesthetic appearance of the hand (22,23). Both procedures narrow the palm and thus predictably weaken grasp and cylindrical grip palmar stabilization.
 |
|
Figure 46.6. Absence of either the middle or the ring finger impairs the ability to retain small objects in the palm.
|
 |
|
Figure 46.7. Ring-finger ray resection with soft-tissue coaptation sling. A:
Transverse intermetacarpal ligament and palmar plate continuity is preserved as the ring metacarpal is excised through a dorsal exposure. B: A palmar chevron incision allows resection of redundant palmar skin. C: Interweaving of the transverse intermetacarpal ligament brings the little metacarpal head toward the middle metacarpal, while dorsal skin closure stabilizes rotational alignment. |
 |
|
Figure 46.8. Middle ray resection and index ray resection. A: Converging chevron incisions reduce palmar skin and soft-tissue redundancy. B: Corresponding step-cut osteotomies are fashioned in both the index and middle metacarpal proximal metaphyses. C:
The transposed index finger is fixed to the middle finger with a plate and is further stabilized with Kirschner wire into the ring metacarpal. |
Pronation strength, a measure of grip stabilization by the breath of
the metacarpal, is diminished to 50% of predicted values after index
ray resection (18). Transposition of the index
ray to the middle metacarpal position results in 75% of predicted grip
strength, while transposition of the little-finger ray to the ring
finger metacarpal position results in retention of 85% of predicted
grip strength (7).
effectively brings the relatively mobile little-finger ray into close
approximation to the middle finger but is somewhat less successful in
bringing the relatively fixed index metacarpal alongside the ring
metacarpal (23).
-
Make parallel zigzag incisions on the
palmar surface overlying the metacarpal to be resected. Remove a
generous wedge of dorsal skin. The dorsal skin resection will provide a
dermodesis, which will stabilize the digit and prevent it from rotating
into a position in which the fingers will scissor over one another in
flexion. -
Resect the entire metacarpal
subperiosteally. If the middle metacarpal is excised, preserve the
proximal insertion of the extensor carpi radialis brevis within the
periosteal sleeve, and take care to preserve the origin of the adductor
pollicis muscle. When the ring metacarpal is resected, the entire
metacarpal base may be removed, allowing radial shift of the little
metacarpal on the hamate. -
Avoid injury to the deep motor branch of
the ulnar nerve, which runs just palmar to the metacarpal and is
vulnerable to injury when excising the metacarpal. Identify and ligate
the proper digital arteries. Sharply divide the proper digital nerves
distal to the common digital nerve bifurcation. -
Pull flexor and extensor tendons
distally, divide them, and allow them to retract proximally. Divide the
interosseous and lumbrical tendons. -
Retain a single continuous soft-tissue
band, consisting of the palmar plate and the two adjacent deep
transverse metacarpal ligaments, each of which is firmly attached to
adjacent digits. Press the metacarpal heads together manually. Tightly
secure the digits adjacent to the resected metacarpal to one another by
dividing the
P.1458
ligament–palmar
plate complex and weaving the two segments together. Then securely
suture the shortened ligament–palmar plate complex with interrupted
sutures. -
Close the palmar skin incision first.
Observe the fingers with the wrist in both flexion and extension.
Assess the extent of digital scissoring, if any, as the dorsal skin is
approximated. If residual scissoring persists, excise further dorsal
skin. Circumferential dressing and splinting maintains lateral
metacarpal pressure and protects the ligament repair during the first 3
weeks after reconstruction.
retained digits is facilitated if the skin of a single web space is
preserved and shifted intact to the new web space (10,21).
If possible, base the web-space flap on the digit that is not being
transposed. For example, if the middle finger is being resected and the
index finger is being transposed to the middle-finger position, the
web-space skin of the middle–ring interval is retained based on the
ring finger and is ultimately sewn to the ulnar border of the index
finger.
-
Create palmar zigzag incisions that
converge over the middle third of the metacarpal to be resected. Resect
a dorsal wedge of skin with its apex over the proximal third of the
metacarpal. -
Identify the digital neurovascular
structures. Sharply section the proper digital nerves, and ligate the
proper digital arteries. -
Pull flexor and extensor tendons distally
and divide them. Define the interosseous muscles inserting on the
resected digit distally, dissect them free proximally, isolate them,
and excise them. Divide the lumbrical tendon along the radial aspect of
the digit being resected. -
When the middle metacarpal is resected,
preserve the origin of the adductor pollicis on the middle metacarpal
by subperiosteal dissection. -
Because nonunion of the bone-to-bone
junction between transferred and recipient rays is a common
complication of this procedure, careful planning of the bony osteotomy
and secure internal fixation are essential (10).
Transverse osteotomy through the proximal metaphysis rather than
diaphysis provides maximal cancellous surface area and thus facilitates
union. Alignment of the transferred digit is simplified by applying a T
mini-fragment plate to the intact central metacarpal before osteotomy.
Drill, tap, and secure the proximal screws, taking care to align the
longitudinal limb of the plate with the long axis of the metacarpal to
be removed. Then remove the screws and plate. -
Transversely osteotomize the metaphyseal
base of both the recipient central metacarpal and the metacarpal to be
transferred. Mobilize the transferred ray to allow transfer without
tension. The interosseous muscle origins may need to be released.
Suture the adductor pollicis origin to the ring metacarpal when the
index ray is transposed to the middle position. Precisely fit the
transferred ray onto the recipient base. Resecure the screws and plate
proximally to the central metacarpal. Align the long axis of the
transferred metacarpal to the longitudinal holes of the plate to
reproduce the alignment of the excised metacarpal. Ensure that
rotational alignment has been preserved, that the digit is clinically
straight, and that the fingers do not overlap in flexion. Secure the
shaft of the transferred metacarpal to the plate with additional screws. -
A distal transversely placed Kirschner
wire may be helpful in further stabilizing the transferred digit during
the first weeks following surgery. Approximate the deep transverse
metacarpal ligaments from the adjacent sides of the resected metacarpal. -
Transpose the little-finger metacarpal to
the ring position. The ultimate length discrepancy between the little
and middle fingers may be minimized if the osteotomy is performed more
proximally in the metaphysis of the little finger than in the
metaphysis of the ring-finger metacarpal. This technique may add up to
1.5 cm in length to the shifted little-finger ray.
The hand that has undergone little-finger ray resection has an
excellent cosmetic appearance and acceptance. For this reason, ray
resection is recommended in sedentary patients or those particularly
concerned about cosmesis. In patients who depend on the breadth of the
palm to stabilize a hammer, tennis racket, or other object with a
cylindrical grip, removing the little-finger metacarpal will result in
a significant loss of strength (11).
 |
|
Figure 46.9. Little finger ray resection. A: The extensor carpi ulnaris insertion into the proximal metacarpal is preserved. B: Palmar skin excision. C: Skin closure.
|
-
Make a dorso-ulnar incision to expose the
little-finger metacarpal. Isolate and divide the extensor communis and
extensor quinti tendons. Because the extensor carpi ulnaris inserts on
the base of the little-finger metacarpal, avoid disarticulating the
carpometacarpal joint. Instead, divide the metacarpal obliquely through
the tapering metaphysis. -
Divide the flexor tendons as well as the
third palmar interosseous, lumbrical, and hypothenar muscle tendons.
Trim the hypothenar muscles as necessary to create a smooth contour
along the ulnar border of the hand. -
A third alternative, a compromise between
MP disarticulation and ray resection, involves amputating the
metacarpal head and neck and obliquely contouring the metacarpal
through the distal diaphysis. Although this procedure improves the
appearance of the hand and preserves most of the width of the palm, it
eliminates the firm stabilizing contact surface over the palmar aspect
of the little-finger metacarpal head.
out wrist disarticulation by removing the carpal bones. When the entire
length of the radius and ulna is preserved, forearm rotation is
maximized within a prosthesis. Although fitting a prosthesis is
somewhat simpler with diaphyseal forearm amputations, this advantage is
modest and is outweighed by the advantage of preserving the integrity
of the distal radio-ulnar articulation.
of a pain-free, useful hand. This goal is usually best accomplished by
early active movement of the injured hand. When internal fixation is
used, a firm construct should be designed that will permit digital
motion at the earliest possible time. The hand therapist may help guide
the patient with a recent partial hand amputation to regain useful hand
function. Emotional support should be provided by both the physician
and the therapist to help the patient adapt to the altered body image.
when the free distal end of a transected profundus tendon becomes fixed
distally and cannot move to the proximal extent of its normal excursion
(19,26).
between the profundus tendons at the wrist and distal forearm level,
limitation of motion of a single tendon may have an adverse effect on
the motion of adjacent uninjured digits. Patients who have sustained
amputation may experience limitation of active distal joint flexion in
adjacent digits and may complain of palmar or flexor forearm pain with
attempted forceful flexion. The condition is provoked by sewing the
profundus tendon over the end of a digital amputation stump. It is best
avoided by early active motion of both amputated and adjacent digits.
When quadriga is diagnosed, release of the adherent profundus tendon in
the palm proximal to the lumbrical origin will predictably relieve this
condition.
When amputation occurs through a finger proximal to the insertion of
the profundus tendon but distal to the proximal interphalangeal joint,
the proximal pull of the profundus is transmitted through the lumbrical
into the dorsal hood apparatus, increasing the force of proximal
interphalangeal joint extension. As the patient tries to grip
forcefully, the proximal movement of the profundus results in a posture
of proximal interphalangeal joint extension. This paradoxical digital
motion may be eliminated either by sectioning the profundus proximal to
the lumbrical origin or by releasing the radial lateral band.
skin, all amputations inevitably require transection of sensory nerve
branches. Neuromas occur whenever a nerve is transected and thus are an
inevitable consequence of amputation. With proper surgical and
postoperative management, however, neuromas need not be tender or
painful. When a neuroma is caught in overlying scar or is adherent to a
fixed structure, it often becomes symptomatic. The best approach is
prevention. Many initially tender neuromas improve with local massage
and desensitization activity under the guidance of a therapist. Do not
consider surgical revision of tender neuromas until the wound has
become supple and the skin is no longer adherent to underlying soft
tissue and bone.
distally and tethered by proximal joint motion. In such situations, the
nerve must be freed distally and allowed to migrate proximally. Early
digital motion is encouraged (see Chapter 53).
appearance of the residual hand. Simple procedures tend to be
associated with less residual pain than complex reconstruction.
Encourage early motion. Hand therapy may be invaluable in assisting
patients to regain function.
scheme: *, classic article; #, review article; !, basic research
article; and +, clinical results/outcome study.
E, Alnot J-Y, Coutier C, Cadot B. Résection du Quatrième Rayon pour
Lésions de l’Annulaire les Amputations du Quatrième Rayon de la Main
(Amputation of the fourth ray of the hand). Rev Chir Orthop 1997;83:324.
JF, Carman W, MacKenzie JK. Transmetacarpal Amputation of the Index
Finger: A Clinical Assessment of Hand Strength and Complications. J Hand Surg 1977;2:471.
L, Foucher G. Étude Comparative des Résections Metacarpiennes et des
Translocations après Amputations des Doigts Medians (A comparative
study of metacarpal resection and translocation after amputation of the
middle finger). Ann Chir Main Memb Super 1995;14;74.