Ulnar Nerve Transposition
is a very common disorder. It usually occurs as a consequence of
fibrosis in the region of the medial epicondyle, which inhibits gliding
of the nerve, and because the cubital tunnel narrows when the elbow is
flexed. The typical symptoms include pain, paresthesia or numbness of
the little and ring fingers, and weakness of pinch and grip. Relief can
usually be obtained by restricting elbow flexion and avoiding pressure
on the medial aspect of the elbow. If the symptoms cannot be controlled
in this manner or if there is marked loss of sensibility or weakness,
surgery is recommended. Many operative procedures have been described,
which include neurolysis, epicondylectomy, and anterior transposition.
This chapter describes the various potential sites of compression of
the ulnar nerve at the elbow and the technique of submuscular anterior
transposition.
the medial cord of the brachial plexus, which then divides into the
ulnar nerve and the medial cutaneous nerves of the arm and forearm. In
the midportion of the arm the ulnar nerve lies anterior to the medial
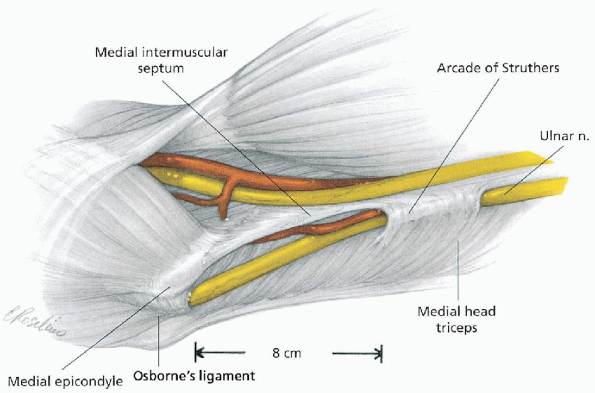
head of the triceps and posterior to the medial intermuscular septum (Fig. 9-1).
In 70% of extremities a medial musculofascial arcade, as described by
Struthers, covers the nerve. This arcade is located approximately 8 cm
proximal to the medial epicondyle and is composed of the deep fascia of
the arm, superficial fibers of the triceps, and the internal brachial
ligament arising from the coracobrachialis tendon. The nerve then
passes into a fibroosseous groove that is bordered anteriorly by the
medial epicondyle, posterior and laterally by the olecranon and ulnar
humeral ligament, and medially by a fibroaponeurotic band. In this
region numerous branches of the superior and inferior collateral and
posterior ulnar recurrent arteries, as well as several veins, accompany
the nerve. Also at this level, a small articular branch leaves the
ulnar nerve to innervate the joint capsule. Occasionally, an anomalous
muscle called the anconeus epitrochlearis is encountered covering the
ulnar nerve. This muscle arises from the medial border of the olecranon
and inserts onto the medial epicondyle.
 |
|
FIGURE 9-1. Anatomy of ulnar nerve and potential sites of compression. (From Doyle JR. Arm. In: Doyle JR, Botte MJ, eds. Surgical anatomy of the hand and upper extremity. Philadelphia: Lippincott Williams & Wilkins, 2003:389, with permission.)
|
travels between the humeral and ulnar heads of the flexor carpi
ulnaris. Osborne described a fibrous band that begins at the
fibroaponeurosis of the epicondylar groove and continues to the flexor
carpi ulnaris. It is often very thick and is a common cause of ulnar
nerve compression. (Synonyms for the ligament described by Osborne are
the triangular ligament, the arcuate ligament, and humeral ulnar arch.)
In this region the medial collateral ligament of the elbow lies
posterior to the ulnar nerve. While lying within the muscle of the
flexor carpi ulnaris, the ulnar nerve gives off motor branches to this
wrist flexor. Traveling distally, the nerve pierces the flexor pronator
fascia and then lies between the flexor digitorum superficialis (FDS)
and the flexor digitorum profundus (FDP).
there are more than three patterns of ulnar neuropathy. Therefore, I
use the schema outlined in Table 9-1.
elbow include local tenderness; alteration in the sensibility of the
hypothenar eminence, the entire small finger, and the dorsal and ulnar
palmar aspects of the ring finger; and weakness of the FDP of the ring
and small fingers, the abductor digiti quinti, the interossei, and the
adductor pollicis. Nonoperative treatment is usually effective and
involves reduction in activity, avoidance of external compression and
elbow flexion, nonsteroidal antiinflammatory medications, and elbow
pads and splints that inhibit elbow flexion.
|
TABLE 9-1. ALTERNATEa CLASSIFICATION OF ULNAR NERVE NEUROPATHY
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||
there is evidence of chronic sensory and/or major dysfunction, surgery
is recommended. Because cervical radiculopathy, thoracic outlet
syndrome, compression within Guyon’s canal, and polyneuropathy can
mimic ulnar nerve compression at the elbow, electrodiagnostic studies
are often performed before surgery.
-
Hand table
-
Calibrated tourniquet
-
Bipolar coagulator
-
Vessel loops or small Penrose drains
-
Army/Navy retractors
-
Power drill with 2-mm bit or 0.045-inch Kirschner wire
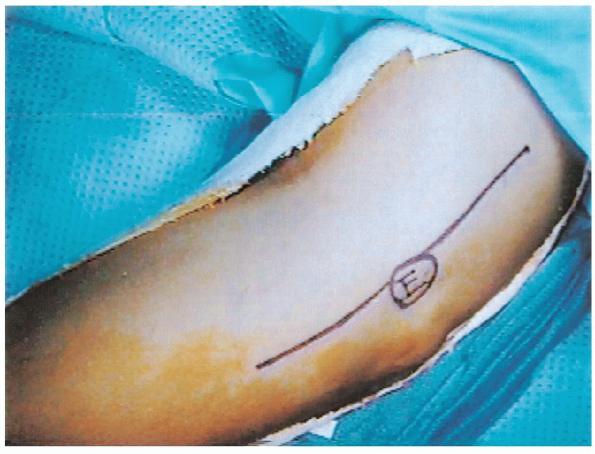
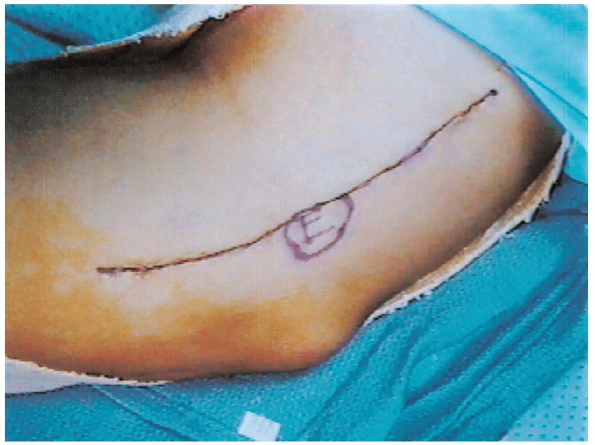
medial aspect of the elbow region. The incision extends approximately
10 cm proximal to the medial epicondyle, passing 2 cm anterior to the
epicondyle, and continuing 8 cm distally (Fig. 9-3).
 |
|
FIGURE 9-2. The patient’s arm is abducted 90 degrees and rests on a padded hand table.
|

close to the axilla as possible. The upper extremity is then prepared
and draped. The tourniquet is applied after exsanguination and the skin
incision outlined with a marking pencil (Fig. 9-3).
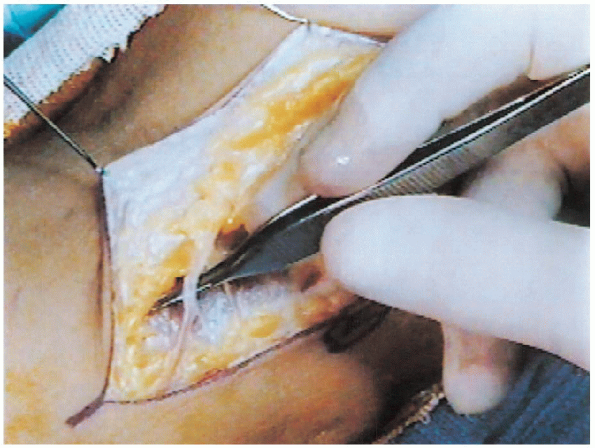
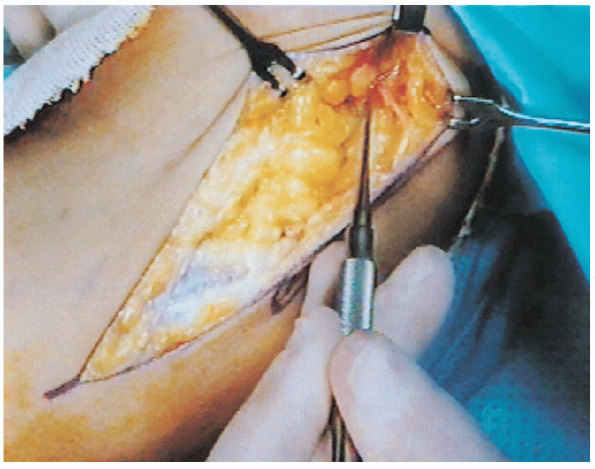
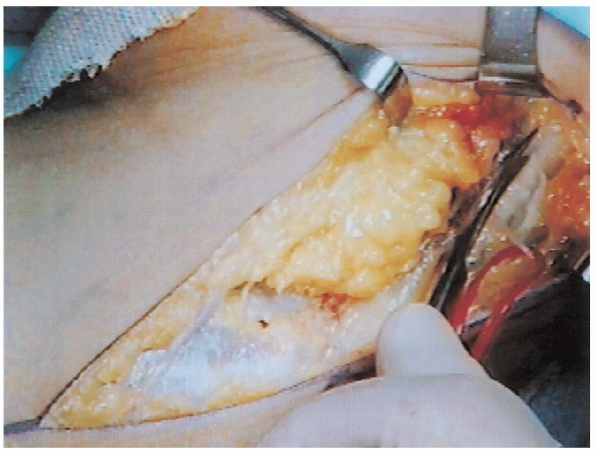
Subsequent to the skin incision, the dissection is continued through
the adipose tissue with scissors. Numerous veins require coagulation or
ligation. At this time, the medial cutaneous nerves should be
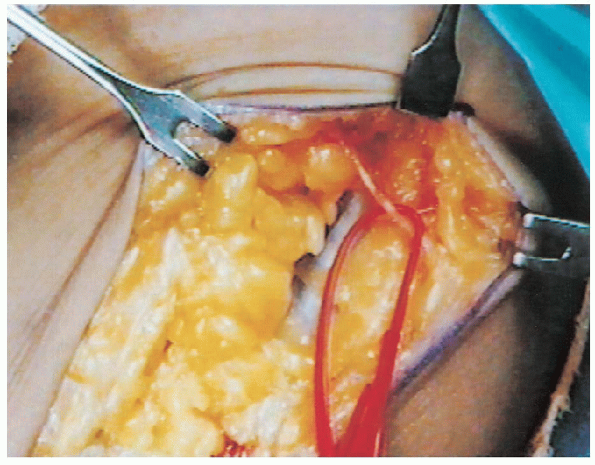
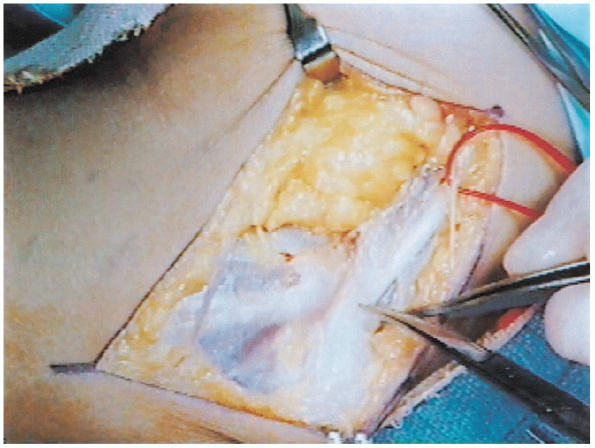
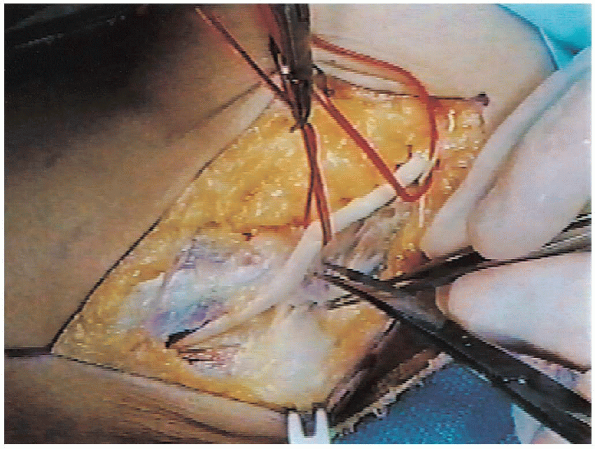
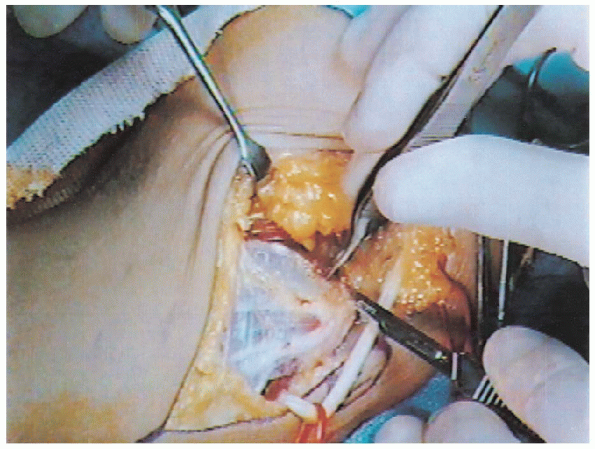
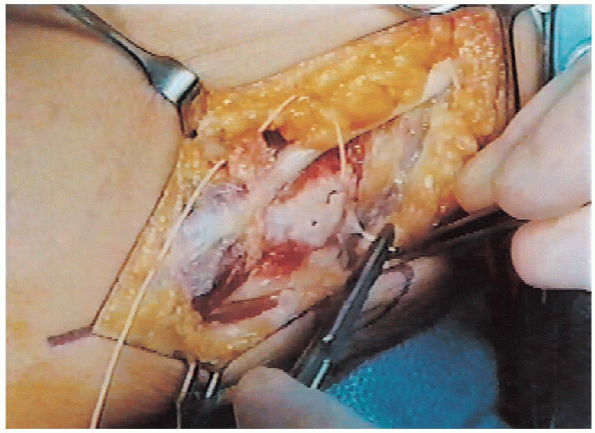
identified and mobilized (Figs. 9-4 and 9-5). Colored
vessel loops are placed around these nerves to both remind the surgeon
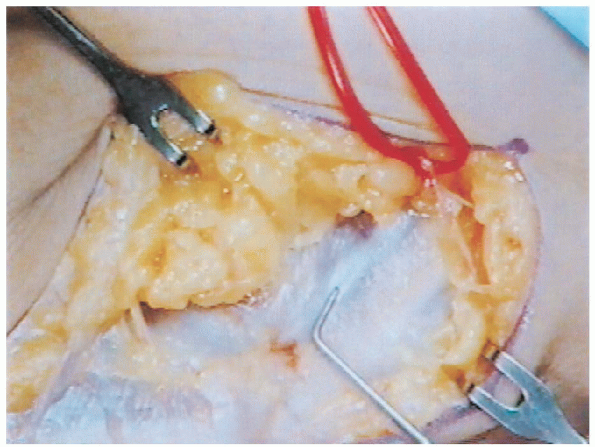
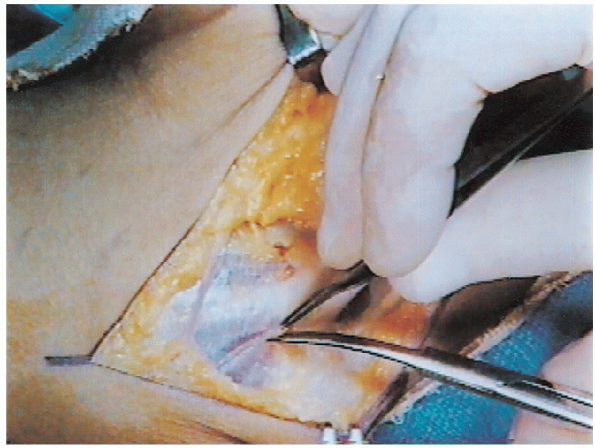
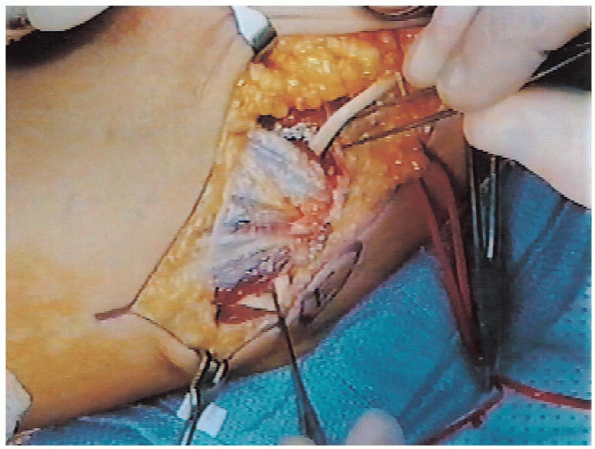
of their presence and to aid in their gentle retraction (Fig. 9-6). Next, the ulnar nerve is located posterior to the medial intermuscular septum (Fig. 9-7), and the fascia is incised from the upper arm to the epicondyle (Figs. 9-8 and 9-9).
Using Army/Navy retractors, the proximal subcutaneous tissue is
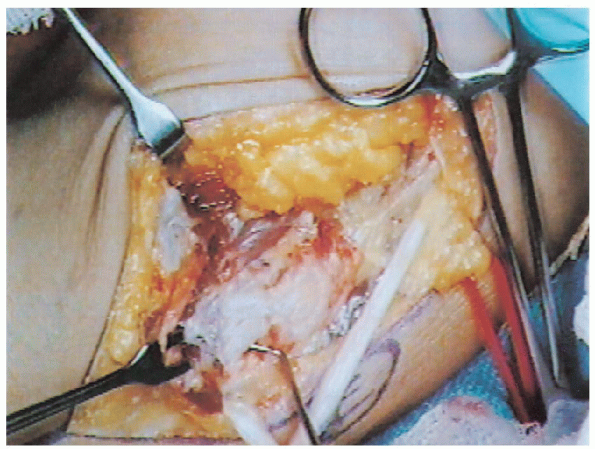
retracted, and with blunt scissors the arcade of Struthers is released (Fig. 9-10). If the arcade is not fully released, it may cause an iatrogenic compression of the ulnar nerve
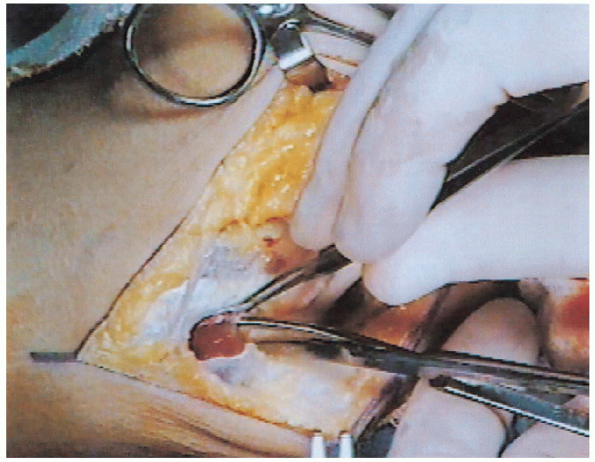
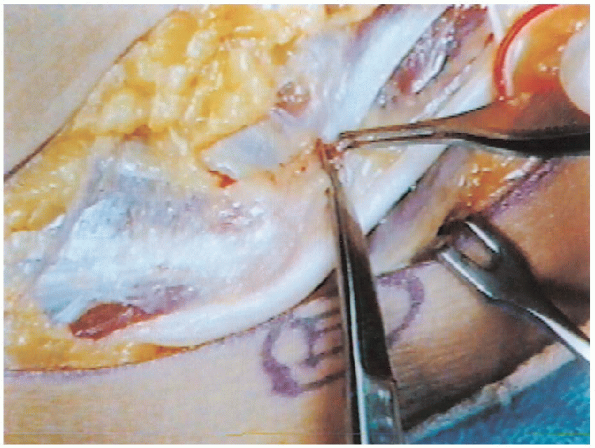
subsequent to the anterior transposition. Next, the retrocondylar fascia is divided (Fig. 9-11), and exposure of the nerve is continued in a proximal-to-distal direction by dividing Osborne’s ligament (Fig. 9-12) and separating the two heads of the flexor carpi ulnaris muscle (Fig. 9-13).
 |
|
FIGURE 9-3. Incision marked. E, medial epicondyle.
|
 |
|
FIGURE 9-4. Medial cutaneous nerve of forearm.
|
 |
|
FIGURE 9-5. Medial cutaneous nerve of arm.
|
 |
|
FIGURE 9-6. Vessel loop around medial cutaneous nerve of arm.
|
 |
|
FIGURE 9-7. Probe at medial intermuscular septum.
|
 |
|
FIGURE 9-8. Exposure of ulnar nerve proximal to epicondyle.
|
 |
|
FIGURE 9-9. Division of fascia surrounding ulnar nerve.
|
 |
|
FIGURE 9-10. Incision of arcade of Struthers.
|
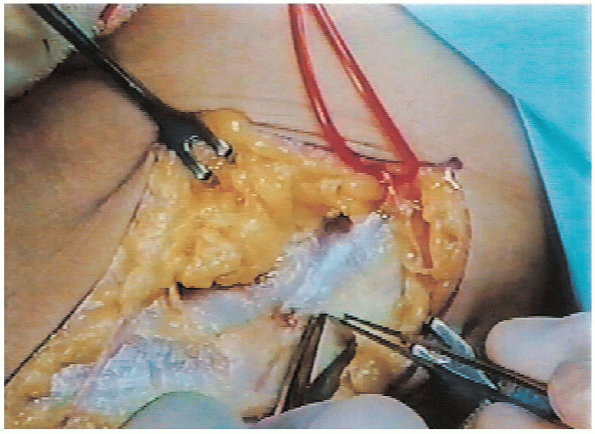
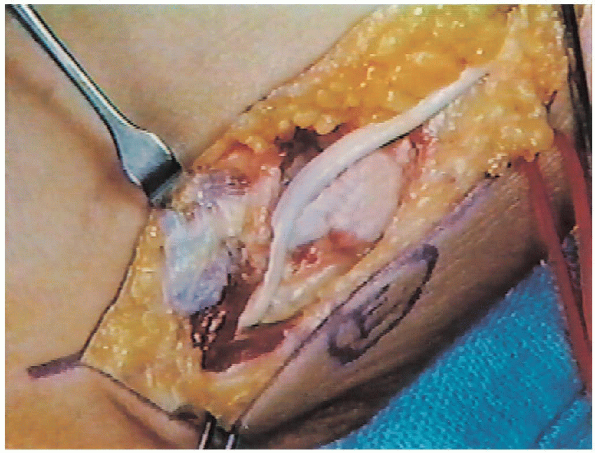
The nerve should be carefully dissected away from its bed with as much
preservation as possible of any blood vessels that accompany the nerve;
however, vessels can be coagulated to permit anterior transposition.
During the neurolysis, the nerve is retracted gently with either vessel
loops or small Penrose drains. The small articular branches require division, but injury to the flexor carpi ulnaris motor branches should be avoided (Fig. 9-16); these are located distal to the epicondyle. Subsequent to the neurolysis and with the elbow flexed, the nerve often subluxes anteriorly (Fig. 9-17). The elbow should be placed in
full flexion to ensure that the tendon of the
medial head of triceps does not translate over the epicondyle. If this
tendon does translate, it must be incised; otherwise, the patient will
complain of persistent painful snapping despite surgery.
 |
|
FIGURE 9-11. Division of retrocondylar fascia.
|
 |
|
FIGURE 9-12. Release of Osborne’s ligament.
|
 |
|
FIGURE 9-13. Separation of the two heads of the flexor carpi ulnaris.
|
 |
|
FIGURE 9-14. Neurolysis of the ulnar nerve. Vessel loops retract nerve.
|
 |
|
FIGURE 9-15. Excision of intermuscular septum.
|
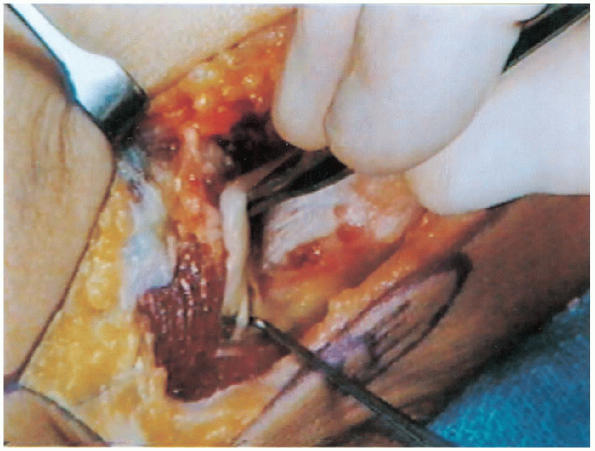
for any severe fibrosis, and, if the epineurium is fibrotic, a limited
epineurotomy is performed until a good fascicular pattern can be
observed. Next, the origin of the flexor-pronator is sharply incised
from the medial epicondyle, and the muscle group reflected off the
anterior medial aspect of the elbow (Fig. 9-18).
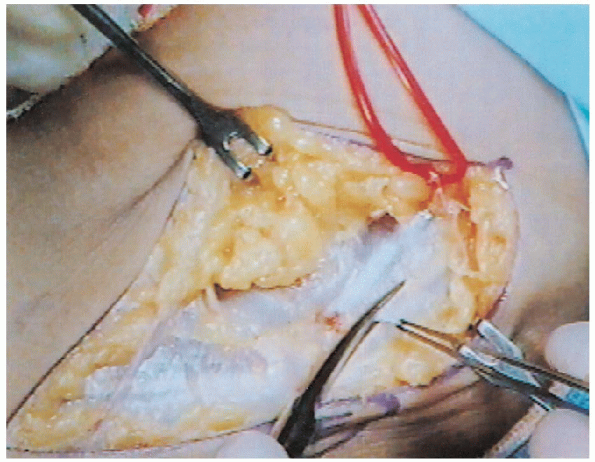
During this mobilization, the median nerve and brachial artery may be
encountered, because they lie medial to the flexor-pronator muscle
group. During the dissection of the humeral head
of the flexor carpi ulnaris muscle, one should be careful not to injure
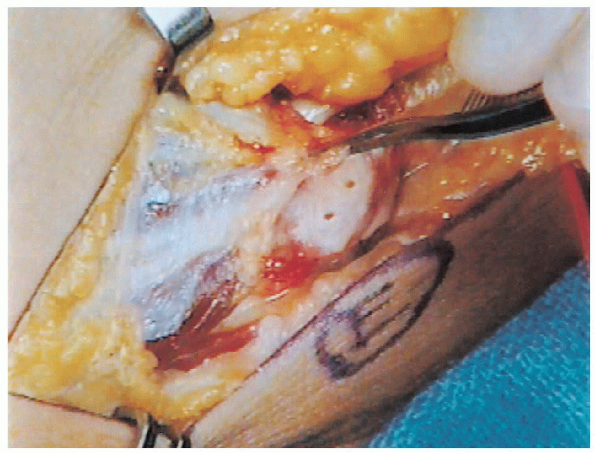
the medial collateral ligament (Fig. 9-19). Once the muscle mobilization
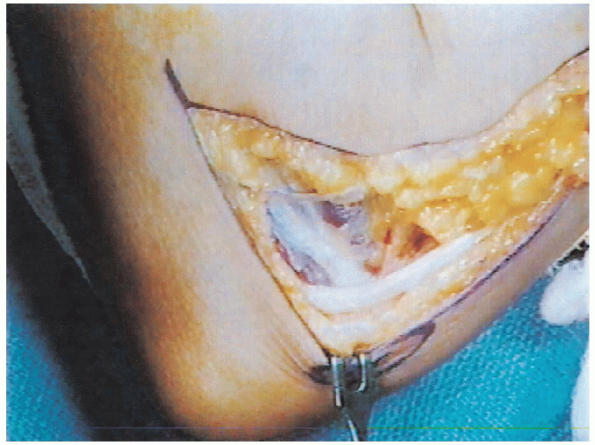
has been completed, the ulnar nerve is transposed anteriorly and the
surgeon must make sure that it lies in a straight path without kinking
or impingement (Fig. 9-20). Three holes are drilled into the tip of the medial epicondyle (Fig. 9-21), and, with the elbow in full extension, the flexor pronator tendon is reattached with 2-0 sutures (Fig. 9-22). Once
the submuscular anterior transposition has been completed, the nerve is
reevaluated to ensure that it glides easily beneath its new muscular
cover (Fig. 9-23). Although many
surgeons prefer to release the tourniquet before skin closure, this has
not been found necessary provided that careful hemostasis has been
obtained throughout the procedure.
 |
|
FIGURE 9-16. Probe at motor branch of the flexor carpal ulnaris muscle.
|
 |
|
FIGURE 9-17. On flexion of the elbow, the ulnar nerve undergoes anterior subluxation.
|
 |
|
FIGURE 9-18. Dissection of the flexor pronator muscle group from its epicondylar origin.
|
 |
|
FIGURE 9-19. Probe at the medial collateral ligament.
|
 |
|
FIGURE 9-20. Anterior transposition of ulnar nerve.
|
sutures, which is followed by a subcuticular closure also using an
absorbable suture (Fig. 9-24). The elbow is
then splinted in 90 degrees of flexion for 10 days. Active range of
motion is begun at that time with intermittent protection
provided by a sling or removable splint for an additional 2 weeks.
 |
|
FIGURE 9-21. Holes have been drilled into epicondyle for reattachment of flexor pronator tendon, which is being held by forceps.
|
 |
|
FIGURE 9-22. Suture placed through flexor pronator tendon and hole drilled into epicondyle.
|
exercises can be started if adequate mobility has not been obtained.
Progressive strengthening can also be instituted at this time. Several
months of scar massage with a thick cream such as cocoa butter and the
application of silastic skin cover are effective means of minimizing
the surgical scar.
 |
|
FIGURE 9-23. The gliding of the ulna nerve is tested subsequent to anterior transposition and reattachment of the flexor pronator muscle.
|
 |
|
FIGURE 9-24. Subarticular closure of incision.
|
