Pelvis
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > IV – Lower Extremity Fractures and Dislocations > 25 – Pelvis
25
Pelvis
ANATOMY
-
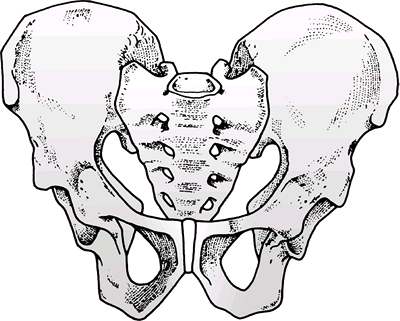
The pelvic ring
is composed of the sacrum and two innominate bones joined anteriorly at
the symphysis and posteriorly at the paired sacroiliac joints (Figs. 25.1 and 25.2). -
The innominate
bone is formed at maturity by the fusion of three ossification centers:
the ilium, the ischium, and the pubis through the triradiate cartilage
at the dome of the acetabulum. -
The pelvic brim
is formed by the arcuate lines that join the sacral promontory
posteriorly and the superior pubis anteriorly. Below this is the true or lesser pelvis, in which are contained the pelvic viscera. Above this is the false or greater pelvis that represents the inferior aspect of the abdominal cavity. -
Inherent stability of the pelvis is
conferred by ligamentous structures. These may be divided into two
groups according to the ligamentous attachments:-
Sacrum to ilium: The strongest and most
important ligamentous structures occur in the posterior aspect of the
pelvis connecting the sacrum to the innominate bones.-
The sacroiliac ligamentous complex is divided into posterior (short and long) and anterior ligaments. Posterior ligaments provide most of the stability.
-
The sacrotuberous ligament
runs from the posterolateral aspect of the sacrum and the dorsal aspect
of the posterior iliac spine to the ischial tuberosity. This ligament,
in association with the posterior sacroiliac ligaments, is especially
important in helping maintain vertical stability of the pelvis. -
The sacrospinous ligament
is triangular, running from the lateral margins of the sacrum and
coccyx and inserting on the ischial spine. It is more important in
maintaining rotational control of the pelvis if the posterior
sacroiliac ligaments are intact.
-
-
Pubis to pubis: This is the symphysis pubis.
-
-
Additional stability is conferred by ligamentous attachments between the lumbar spine and the pelvic ring:
-
The iliolumbar ligaments originate from the L4 and L5 transverse processes and insert on the posterior iliac crest.
-
The lumbosacral ligaments originate from the transverse process of L5 to the ala of the sacrum.
-
-
The transversely placed ligaments resist
rotational forces and include the short posterior sacroiliac, anterior
sacroiliac, iliolumbar, and sacrospinous ligaments. -
The vertically placed ligaments resist
vertical shear (VS) and include the long posterior sacroiliac,
sacrotuberous, and lateral lumbosacral ligaments.
P.276
PELVIC STABILITY
 |
|
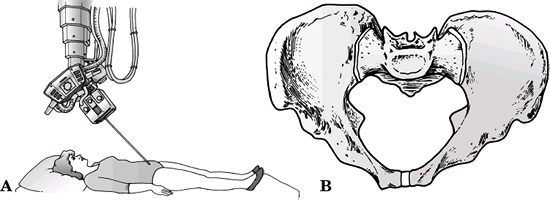
Figure 25.1. Lateral projection of the left innominate bone. Note the muscular attachments to the ilium, ischium, and pubis.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
A stable injury is defined as one that can withstand normal physiologic forces without abnormal deformation.
-
Penetrating trauma infrequently results in pelvic ring destabilization.
-
An unstable injury may be characterized by the type of displacement as:
-
Rotationally unstable (open and externally rotated, or compressed and internally rotated).
-
Vertically unstable.
-
McBroom and Tile
Sectioned ligaments of the pelvis determine relative
contributions to pelvic stability (these included bony equivalents to
ligamentous disruptions):
contributions to pelvic stability (these included bony equivalents to
ligamentous disruptions):
-
Symphysis: pubic diastasis <2.5 cm
-
Symphysis and sacrospinous ligaments:
>2.5 cm of pubic diastasis (note that these are rotational movements
and not vertical or posterior displacements) -
Symphysis, sacrospinous, sacrotuberous, and posterior sacroiliac: unstable vertically, posteriorly, and rotationally
P.277
MECHANISM OF INJURY
 |
|
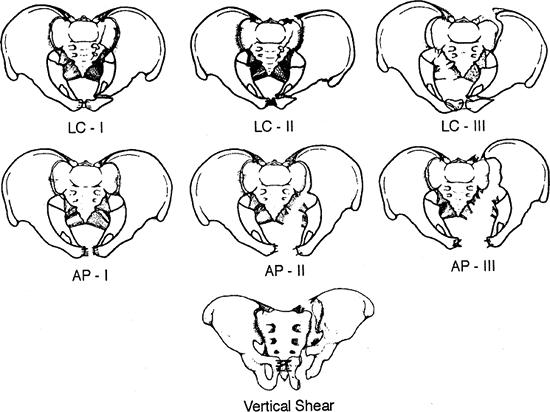
Figure 25.2. Medial projection of the left innominate bone with muscle attachments and outline of the sacroiliac joint surface.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
These may be divided into low-energy
injuries, which typically result in fractures of individual bones, or
high-energy fractures, which may result in pelvic ring disruption.-
Low-energy injuries may result from
sudden muscular contractions in young athletes that cause an avulsion
injury, a low-energy fall, or a straddle-type injury. -
High-energy injuries typically result
from a motor vehicle accident, pedestrian-struck mechanism, motorcycle
accident, fall from heights, or crush mechanism.
-
-
Impact injuries result when a moving
victim strikes a stationary object or vice versa. Direction, magnitude,
and nature of the force all contribute to the type of fracture. -
Crush injuries occur when a victim is
trapped between the injurious force, such as motor vehicle, and an
unyielding environment, such as the ground or pavement. In addition to
those factors mentioned previously, the position of the victim, the
duration of the crush, and whether the force was direct or a “rollover”
(resulting in a changing force vector) are important to understanding
the fracture pattern. -
Specific injury patterns vary by the direction of force application:
-
Anteroposterior (AP) force
-
This results in external rotation of the hemipelvis.
-
The pelvis springs open, hinging on the intact posterior ligaments.
-
-
Lateral compression (LC) force: This is
most common and results in impaction of cancellous bone through the
sacroiliac joint and sacrum. The injury pattern depends on location of
force application:-
Posterior half of the ilium: This is classic LC with minimal soft tissue disruption. This is often a stable configuration.
-
Anterior half of the iliac wing: This
rotates the hemipelvis inward. It may disrupt the posterior sacroiliac
ligamentous complex. If this force continues to push the hemipelvis
across to the contralateral side, it will push the contralateral
hemipelvis out into external rotation, producing LC on the ipsilateral
side and an external rotation injury on the contralateral side. -
Greater trochanteric region: This may be associated with a transverse acetabular fracture.
-
External rotation abduction force: This is common in motorcycle accidents.
-
Force application occurs through the femoral shafts and head when the leg is externally rotated and abducted.
-
This tends to tear the hemipelvis from the sacrum.
-
-
Shear force
-
This leads to a completely unstable
fracture with triplanar instability secondary to disruption of the
sacrospinous, sacrotuberous, and sacroiliac ligaments. -
In the elderly individual, bone strength will be less than ligamentous strength and will fail first.
-
In a young individual, bone strength is greater, and thus ligamentous disruptions usually occur.
-
-
P.278
CLINICAL EVALUATION
-
Perform patient primary assessment
(ABCDE): airway, breathing, circulation, disability, and exposure. This
should include a full trauma evaluation. -
Initiate resuscitation: Address life-threatening injuries.
-
Evaluate injuries to head, chest, abdomen, and spine.
-
Identify all injuries to extremities and pelvis, with careful assessment of distal neurovascular status.
-
Pelvic instability may result in a
leg-length discrepancy involving shortening on the involved side or a
markedly internally or externally rotated lower extremity. -
The AP-LC test for pelvic instability should be performed once only and involves rotating the pelvis internally and externally.
-
“The first clot is the best clot.” Once
disrupted, subsequent thrombus formation of a retroperitoneal
hemorrhage is difficult because of hemodilution by administered
intravenous fluid and exhaustion of the body’s coagulation factors by
the original thrombus.
-
-
Massive flank or buttock contusions and swelling with hemorrhage are indicative of significant bleeding.
-
Palpation of the posterior aspect of the
pelvis may reveal a large hematoma, a defect representing the fracture,
or a dislocation of the sacroiliac joint. Palpation of the symphysis
may also reveal a defect. -
The perineum must be carefully inspected for the presence of a lesion representing an open fracture.
P.279
HEMODYNAMIC STATUS
Retroperitoneal hemorrhage may be associated with
massive intravascular volume loss. The usual cause of retroperitoneal
hemorrhage secondary to pelvic fracture is a disruption of the venous
plexus in the posterior pelvis. It may also be caused by a large-vessel
injury, such as external or internal iliac disruption. Large-vessel
injury causes rapid, massive hemorrhage with frequent loss of the
distal pulse and marked hemodynamic instability. This often
necessitates immediate surgical exploration to gain proximal control of
the vessel before repair. The superior gluteal artery is occasionally
injured and can be managed with rapid fluid resuscitation, appropriate
stabilization of the pelvic ring, and embolization.
massive intravascular volume loss. The usual cause of retroperitoneal
hemorrhage secondary to pelvic fracture is a disruption of the venous
plexus in the posterior pelvis. It may also be caused by a large-vessel
injury, such as external or internal iliac disruption. Large-vessel
injury causes rapid, massive hemorrhage with frequent loss of the
distal pulse and marked hemodynamic instability. This often
necessitates immediate surgical exploration to gain proximal control of
the vessel before repair. The superior gluteal artery is occasionally
injured and can be managed with rapid fluid resuscitation, appropriate
stabilization of the pelvic ring, and embolization.
-
Options for immediate hemorrhage control include:
-
Application of military antishock trousers (MAST). This is typically performed in the field.
-
Application of an anterior external fixator.
-
Wrapping of a pelvic binder circumferentially around the pelvis (or sheet if a binder is not available).
-
Application of a pelvic C-clamp.
-
Open reduction and internal fixation
(ORIF): This may be undertaken if the patient is undergoing emergency
laparotomy for other indications; it is frequently contraindicated by
itself because loss of the tamponade effect may encourage further
hemorrhage. -
Consider angiography or embolization if hemorrhage continues despite closing of the pelvic volume.
-
NEUROLOGIC INJURY
-
Lumbosacral plexus and nerve root injuries may be present, but they may not be apparent in an unconscious patient.
GENITOURINARY AND GASTROINTESTINAL INJURY
-
Bladder injury: 20% incidence occurs with pelvic trauma.
-
Urethral injury: 10% incidence occurs with pelvic fractures, in male patients much more frequently than in female patients.
-
Examine for blood at the urethral meatus or blood on catheterization.
-
Examine for a high-riding or “floating” prostate on rectal examination.
-
Clinical suspicion should be followed by a retrograde urethrogram.
-
Bowel Injury
Perforations in the rectum or anus owing to osseous fragments are technically open injuries and should be treated as such.
P.280
Infrequently, entrapment of bowel in the fracture site with
gastrointestinal obstruction may occur. If either is present, the
patient should undergo diverting colostomy.
 |
|
Figure 25.3. Anteroposterior view of the pelvis.
(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
RADIOGRAPHIC EVALUATION
Standard trauma radiographs include an AP view of the chest, a lateral view of the cervical spine, and an AP view of the pelvis.
-
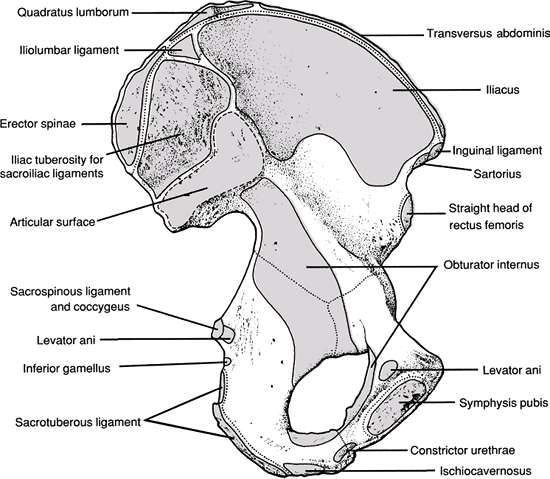
AP of the pelvis (Fig. 25.3):
-
Anterior lesions: pubic rami fractures and symphysis displacement
-
Sacroiliac joint and sacral fractures
-
Iliac fractures
-
L5 transverse process fractures
-
-
Special views of the pelvis include:
-
Obturator and iliac oblique views: They may be utilized in suspected acetabular fractures (see Chapter 26).
-
Inlet radiograph (Fig. 25.4): This is taken with the patient supine with the tube directed 60 degrees caudally, perpendicular to the pelvic brim.
-
This is useful for determining anterior or posterior displacement of the sacroiliac joint, sacrum, or iliac wing.
-
It may determine internal rotation deformities of the ilium and sacral impaction injuries.
-
-
Outlet radiograph (Fig. 25.5): This is taken with the patient supine with the tube directed 45 degrees cephalad.
-
This is useful for determination of vertical displacement of the hemipelvis.
-
It may allow for visualization of subtle
signs of pelvic disruption, such as a slightly widened sacroiliac
joint, discontinuity of the sacral borders, nondisplaced sacral
fractures, or disruption of the sacral foramina.![]() Figure 25.4. Inlet view of the pelvis: technique (A) and artist’s sketch (B).(Modified from Tile M. Fractures of the Pelvis and Acetabulum, 2nd ed. Baltimore: Williams & Wilkins; 1995.)
Figure 25.4. Inlet view of the pelvis: technique (A) and artist’s sketch (B).(Modified from Tile M. Fractures of the Pelvis and Acetabulum, 2nd ed. Baltimore: Williams & Wilkins; 1995.)
P.281 -
-
-
Computed tomography: This is excellent for assessing the posterior pelvis, including the sacrum and sacroiliac joints.
-
Magnetic resonance imaging: It has
limited clinical utility owing to restricted access to a critically
injured patient, prolonged duration of imaging, and equipment
constraints. However, it may provide superior imaging of genitourinary
and pelvic vascular structures. -
Stress views: Push-pull radiographs are performed while the patient is under general anesthesia to assess vertical stability.
-
Tile defined instability as ≥0.5 cm of motion.
-
Bucholz, Kellam, and Browner consider ≥1 cm of vertical displacement unstable.
-
-
Radiographic signs of instability include:
-
Sacroiliac displacement of 5 mm in any plane.
-
Posterior fracture gap (rather than impaction).
-
Avulsion of the fifth lumbar transverse
process, the lateral border of the sacrum (sacrotuberous ligament), or
the ischial spine (sacrospinous ligament).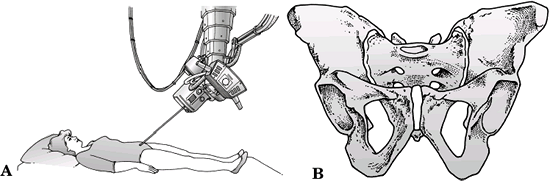 Figure 25.5. Outlet view of the pelvis: technique (A) and artist’s sketch (B).(Modified from Tile M. Fractures of the Pelvis and Acetabulum, 2nd ed. Baltimore: Williams & Wilkins; 1995.)
Figure 25.5. Outlet view of the pelvis: technique (A) and artist’s sketch (B).(Modified from Tile M. Fractures of the Pelvis and Acetabulum, 2nd ed. Baltimore: Williams & Wilkins; 1995.)
-
P.282
|
Table 25.1. Injury classification keys according to the Young and Burgess system
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
CLASSIFICATION
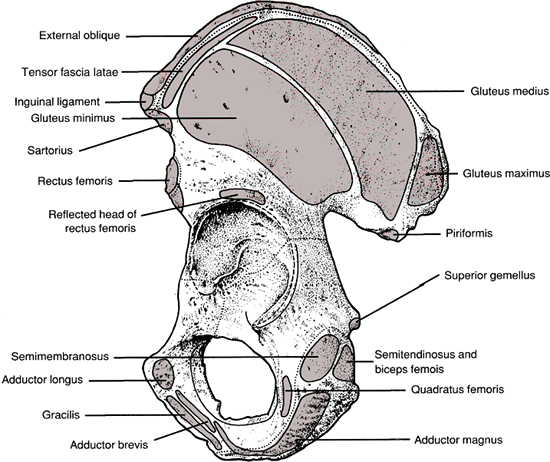
Young and Burgess (Table 25.1 and Fig. 25.6)
This system is based on the mechanism of injury.
-
LC: This is an implosion of the pelvis
secondary to laterally applied force that shortens the anterior
sacroiliac, sacrospinous, and sacrotuberous ligaments. One may see
oblique fractures of the pubic rami, ipsilateral or contralateral to
the posterior injury.Type I: Sacral impaction on the side of impact. Transverse fractures of the pubic rami are stable. Type II: Posterior iliac wing fracture
(crescent) on the side of impact with variable disruption of the
posterior ligamentous structures resulting in variable mobility of the
anterior fragment to internal rotation stress. It maintains vertical
stability and may be associated with an anterior sacral crush injury.Type III: LC-I or LC-II injury on the
side of impact; force continued to contralateral hemipelvis to produce
an external rotation injury (“windswept pelvis”) owing to sacroiliac,
sacrotuberous, and sacrospinous ligamentous disruption. Instability may
result with hemorrhage and neurologic injury secondary to traction
injury on the side of sacroiliac injury. -
AP compression (APC): This is anteriorly
applied force from direct impact or indirectly transferred via the
lower extremities or ischial tuberosities resulting in external
rotation injuries, symphyseal diastasis, or longitudinal rami fractures.![]() Figure 25.6. Young and Burgess classification of pelvic ring fractures.(From Young JWR, Burgess AR. Radiologic Management of Pelvic Ring Fractures. Baltimore: Urban & Schwarzenberg, 1987, with permission.)
Figure 25.6. Young and Burgess classification of pelvic ring fractures.(From Young JWR, Burgess AR. Radiologic Management of Pelvic Ring Fractures. Baltimore: Urban & Schwarzenberg, 1987, with permission.)Type I: Less than 2.5 cm of symphyseal diastasis. Vertical fractures of one or both pubic rami occur, with intact posterior ligaments. Type II: More than 2.5 cm of symphyseal
diastasis; widening of sacroiliac joints; caused by anterior sacroiliac
ligament disruption. Disruption of the sacrotuberous, sacrospinous, and
symphyseal ligaments with intact posterior sacroiliac ligaments results
in an “open book” injury with internal and external rotational
instability; vertical stability is maintained.Type III: Complete disruption of the
symphysis, sacrotuberous, sacrospinous, and sacroiliac ligaments
resulting in extreme rotational instability and lateral displacement;
no cephaloposterior displacement. It is completely unstable with the
highest rate of associated vascular injuries and blood loss. -
VS: vertically or longitudinally applied
forces caused by falls onto an extended lower extremity, impacts from
above, or motor vehicle accidents with an extended lower extremity
against the floorboard or dashboard. These injuries are typically
associated with complete disruption of the symphysis, sacrotuberous,
sacrospinous, and sacroiliac ligaments and result in extreme
instability, most commonly in a cephaloposterior direction because of
the inclination of the pelvis. They have a highly associated incidence
of neurovascular injury and hemorrhage. -
Combined mechanical (CM): combination of injuries often resulting from crush mechanisms. The most common are VS and LC.
P.283
P.284
Tile Classification
| Type A | Stable |
| A1: | Fractures of the pelvis not involving the ring; avulsion injuries |
| A2: | Stable, minimal displacement of the ring |
| Type B: | Rotationally unstable, vertically stable |
| B1: | External rotation instability; open-book injury |
| B2: | LC injury; internal rotation instability; ipsilateral only |
| B3: | LC injury; bilateral rotational instability (bucket handle) |
| Type C: | Rotationally, and vertically unstable |
| C1: | Unilateral injury |
| C2: | Bilateral injury, one side rotationally unstable, with the contralateral side vertically unstable |
| C3: | Bilateral injury, both sides rotationally and vertically unstable with an associated acetabular fracture |
OTA Classification of Pelvic Fractures
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
FACTORS INCREASING MORTALITY
-
Type of pelvic ring injury
-
Posterior disruption is associated with higher mortality (APC III, VS, LC III)
-
-
High Injury Severity Score (Tile, 1980, McMurty, 1980)
-
Associated injuries
-
Head and abdominal, 50% mortality
-
-
Hemorrhagic shock on admission (Gilliland, 1982)
-
Requirement for large quantities of blood
-
24 U versus 7 U (McMurty, 1980)
-
-
Perineal lacerations, open fractures (Hanson, 1991)
-
Increased age (Looser, 1976)
P.285
Morel-Lavallé Lesion (Skin Degloving Injury)
-
Infected in one-third of cases
-
Requires thorough debridement before definitive surgery
TREATMENT
-
The recommended management of pelvic
fractures varies from institution to institution, a finding
highlighting that these are difficult injuries to treat.
Nonoperative
Fractures amenable to nonoperative treatment include:
-
Lateral impaction type injuries with minimal (<1.5 cm) displacement.
-
Pubic rami fractures with no posterior displacement.
-
Gapping of pubic symphysis <2.5 cm.
-
Rehabilitation:
-
Protect weight bearing typically with a walker or crutches initially.
-
Serial radiographs are required after mobilization has begun to monitor for subsequent displacement.
-
If displacement of the posterior ring
>1 cm is noted, weight bearing should be stopped. Operative
treatment should be considered for gross displacement.
-
Tile: Stabilization Options
-
Stable (A1, A2): Stable, minimally
displaced fractures with minimal disruption of the bony and ligamentous
stability of the pelvic ring may successfully be treated with protected
weight bearing and symptomatic treatment. -
Open-book (B1)
-
Symphyseal diastasis <2 cm: Protected weightbearing and symptomatic treatment are indicated.
-
Symphyseal diastasis >2 cm: External
fixation or symphyseal plate is performed (ORIF preferred if laparotomy
for associated injuries and no open injury), with possible fixation for
the posterior injury.
-
-
LC (B2, B3)
-
Ipsilateral only: Elastic recoil may improve pelvic anatomy. No stabilization is necessary.
-
Contralateral (bucket-handle): The posterior sacral complex is commonly compressed.
-
Leg-length discrepancy <1.5 cm: No stabilization is necessary.
-
Leg-length discrepancy >1.5 cm: The choice is external fixation versus ORIF.
-
-
-
Rotationally and vertically unstable (C1, C2, C3): External fixation with or without skeletal traction and ORIF are options.
P.286
Operative Techniques
-
External fixation: This can be applied as
a construct mounted on two to three 5-mm pins spaced 1 cm apart along
the anterior iliac crest, or with the use of single pins placed in the
supraacetabular area in an AP direction (Hanover frame).-
External fixation is a resuscitative
fixation and can only be used for definitive fixation of anterior
pelvis injuries; it cannot be used as definitive fixation of
posteriorly unstable injuries.
-
-
Internal fixation: This significantly increases the forces resisted by the pelvic ring compared with external fixation.
-
Iliac wing fractures: Open reduction and stable internal fixation are performed using lag screws and neutralization plates.
-
Diastasis of the pubic symphysis: Plate fixation is used if no open injury or cystostomy tube is present.
-
Sacral fractures: Transiliac bar fixation
may be inadequate or may cause compressive neurologic injury; in these
cases, plate fixation or sacroiliac screw fixation may be indicated. -
Unilateral sacroiliac dislocation: Direct fixation with cancellous screws or anterior sacroiliac plate fixation is used.
-
Bilateral posterior unstable disruptions:
Fixation of the displaced portion of the pelvis to the sacral body may
be accomplished by posterior screw fixation.
-
Special Considerations
-
Open fractures: In addition to fracture
stabilization, hemorrhage control, and resuscitation, priority must be
given to evaluation of the anus, rectum, vagina, and genitourinary
system.-
Anterior and lateral wounds generally are protected by muscle and are not contaminated by internal sources.
-
Posterior and perineal wounds may be contaminated by rectal and vaginal tears and genitourinary injuries.
-
Colostomy may be necessary for large bowel perforations or injuries to the anorectal region.
-
Colostomy is indicated for any open injury where the fecal stream will contact the open area.
-
-
Urologic injury
-
The incidence is 15%.
-
Blood at the meatus or a high-riding prostate may be noted.
-
Eventual swelling of the scrotum and labia (occasional bleeding artery requiring surgery) may occur.
-
Retrograde urethrogram is indicated in
patients with suspicion of urologic injury, but one should ensure
hemodynamic stability as embolization may be difficult because of dye
extravasation. -
Intra peritoneal bladder ruptures are repaired. Extra peritoneal ruptures may be observed.
-
Urethral injuries are repaired on a delayed basis.
-
-
Neurologic injury
-
L2 to S4 are possible.
-
L5 and S1 are most common.
-
Neurologic injury depends on the location of the fracture and the amount of displacement.
-
Sacral fractures: neurologic injury
-
Decompression of sacral foramen may be indicated if progressive loss of neural function occurs.
-
It may take up to 3 years for recovery.
-
-
Hypovolemic shock: origin
-
Intrathoracic bleeding
-
Intraperitoneal bleeding
-
Diagnostic tables
-
Ultrasound
-
Peritoneal tap
-
Computed tomography
-
-
Retroperitoneal bleeding
-
Blood loss from open wounds
-
Bleeding from multiple extremity fractures
-
-
Average blood replacement (Burgess, J Trauma 1990)
-
LC = 3.6 U
-
AP = 14.8 U
-
VS = 9.2 U
-
CM = 8.5 U
-
-
Mortality (Burgess, J Trauma 1990)
-
Hemodynamically stable patients 3%
-
Unstable patients 38%
-
LC: head injury major cause of death
-
APC: pelvic and visceral injury major cause of death
-
LC1 and LC2 → 50% brain injury
-
LC3 (windswept pelvis: rollover/crush)
-
60% retroperitoneal hematoma
-
20% bowel injury
-
-
AP3 (comprehensive posterior instability)
-
67% shock
-
59% sepsis
-
37% death
-
18.5% adult respiratory distress syndrome (ARDS)
-
-
VS
-
63% shock
-
56% brain injury
-
25% splenic injury
-
25% death
-
23% lung injury
-
-
-
Postoperative management: In general, early mobilization is desired.
-
Aggressive pulmonary toilet should be
pursued with incentive spirometry, early mobilization, encouraged deep
inspirations and coughing, and suctioning or chest physical therapy if
necessary. -
Prophylaxis against thromboembolic
phenomena should be undertaken, with a combination of elastic
stockings, sequential compression devices, and chemoprophylaxis if
hemodynamic status allows. Duplex ultrasound examinations may be
necessary. Thrombus formation may necessitate anticoagulation and/or
vena caval filter placement. -
Weight-bearing status may be advanced as follows:
-
Full weight bearing on the uninvolved lower extremity occurs within several days.
-
Partial weight bearing on the involved lower extremity is recommended for at least 6 weeks.
-
Full weight bearing on the affected extremity without crutches is indicated by 12 weeks.
-
Patients with bilateral unstable pelvic
fractures should be mobilized from bed to chair with aggressive
pulmonary toilet until radiographic evidence of fracture healing is
noted. Partial weight bearing on the less injured side is generally
tolerated by 12 weeks.
-
P.288 -
COMPLICATIONS
-
Infection: The incidence is variable,
ranging from 0% to 25%, although the presence of wound infection does
not preclude a successful result. The presence of contusion or shear
injuries to soft tissues is a risk factor for infection if a posterior
approach is used. This risk is minimized by a percutaneous posterior
ring fixation. -
Thromboembolism: Disruption of the pelvic
venous vasculature and immobilization constitute major risk factors for
the development of deep venous thromboses. -
Malunion: Significant disability may
result, with complications including chronic pain, limb length
inequalities, gait disturbances, sitting difficulties, low back pain,
and pelvic outlet obstruction. -
Nonunion: This is rare, although it tends
to occur more in younger patients (average age 35 years) with possible
sequelae of pain, gait abnormalities, and nerve root compression or
irritation. Stable fixation and bone grafting are usually necessary for
union.