Acetabulum
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > IV – Lower Extremity Fractures and Dislocations > 26 – Acetabulum
26
Acetabulum
ANATOMY
-
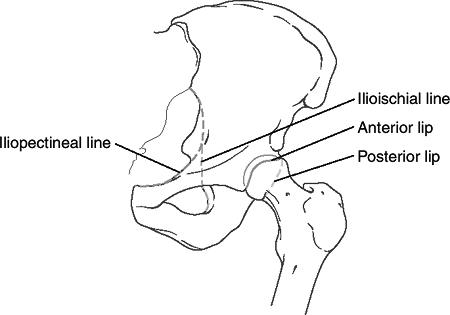
From the lateral aspect of the pelvis,
the innominate osseous structural support of the acetabulum may be
conceptualized as a two-columned construct (Judet and Letournel)
forming an inverted Y (Fig. 26.1). -
Anterior column (iliopubic component):
This extends from the iliac crest to the symphysis pubis and includes
the anterior wall of the acetabulum. -
Posterior column (ilioischial component):
This extends from the superior gluteal notch to the ischial tuberosity
and includes the posterior wall of the acetabulum. -
Acetabular dome: This is the superior
weight-bearing portion of the acetabulum at the junction of the
anterior and posterior columns, including contributions from each. -
Corona mortis
-
A vascular communication between the external iliac or deep inferior epigastric artery and the obturator artery
-
Present in up to 85% of patients
-
May extend over the superior pubic ramus; average distance from the symphysis to corona, 6 cm
-
-
Ascending branch of medial circumflex
-
Main blood supply to femoral head
-
Deep to quadratus femoris
-
-
Superior gluteal neurovascular bundle
-
Emerges from the greater sciatic notch
-
MECHANISM OF INJURY
-
Like pelvis fractures, these injuries are
mainly caused by high-energy trauma secondary to a motor vehicle,
motorcycle accident, or fall from a height. -
The fracture pattern depends on the
position of the femoral head at the time of injury, the magnitude of
force, and the age of the patient. -
Direct impact to the greater trochanter
with the hip in neutral position can cause a transverse type of
acetabular fracture (an abducted hip causes a low transverse fracture,
whereas an adducted hip a high transverse fracture). An externally
rotated and abducted hip causes anterior column injury. An internally
rotated hip causes posterior column injury. -
With indirect trauma, (e.g., a
“dashboard”-type injury to the flexed knee), as the degree of hip
flexion increases, the posterior wall is fractured in an increasingly
inferior position. Similarly, as the degree of hip flexion decreases,
the superior portion of the posterior wall is more likely to be
involved.
CLINICAL EVALUATION
-
Trauma evaluation is usually necessary,
with attention to airway, breathing, circulation, disability and
exposure, depending on the mechanism of injury.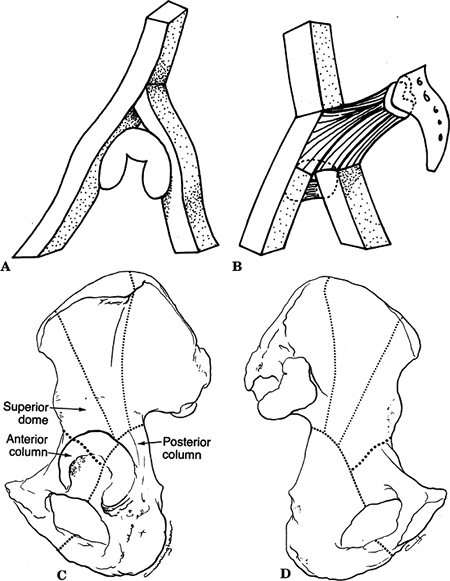 Figure
Figure
26.1. (A) A diagram of the two columns as an inverted Y supporting the
acetabulum. (B) The two columns are linked to the sacral bone by the
“sciatic buttress.” (C) Lateral aspect of the hemipelvis and
acetabulum. The posterior column is characterized by the dense bone at
the greater sciatic notch and follows the dotted line
distally through the center of the acetabulum, the obturator foramen,
and the inferior pubic ramus. The anterior column extends from the
iliac crest to the symphysis pubis and includes the entire anterior
wall of the acetabulum. Fractures involving the anterior column
commonly exit below the anterior-inferior iliac spine as shown by the heavy dotted line.
(D) The hemipelvis from its medial aspect, showing the columns from the
quadrilateral plate. The area between the posterior column and the heavy dotted line, representing a fracture through the anterior column, is often considered the superior dome fragment.(From Letournel E, Judet R. Fractures of the Acetabulum. New York: Springer-Verlag, 1964.) -
Patient factors, such as patient age,
degree of trauma, presence of associated injuries, and general medical
condition are important because they affect treatment decisions as well
as prognosis. -
Careful assessment of neurovascular
status is necessary, because sciatic nerve injury may be present in up
to 40% of posterior column disruptions. Femoral nerve involvement with
anterior column injury is rare, although compromise of the femoral
artery by a fractured anterior column has been described. -
The presence of associated ipsilateral
injuries must be ruled out, with particular attention to the
ipsilateral knee in which posterior instability and patellar fractures
are common. -
Soft tissue injuries (e.g., abrasions,
contusions, presence of subcutaneous hemorrhage) may provide insight
into the mechanism of injury.
P.290
P.291
RADIOGRAPHIC EVALUATION
-
An anteroposterior (AP) and two Judet views (iliac and obturator oblique views) should be obtained.
-
AP view: Anatomic landmarks include the
iliopectineal line (limit of anterior column), the ilioischial line
(limit of posterior column), the anterior lip, the posterior lip, and
the line depicting the superior weight-bearing surface of the
acetabulum terminating as the medial teardrop (Fig. 26.2). -
Iliac oblique radiograph (45-degree
external rotation view): This best demonstrates the posterior column
(ilioischial line), the iliac wing, and the anterior wall of the
acetabulum (Fig. 26.3).![]() Figure
Figure
26.2. Diagram outlining the major landmarks: the iliopectineal line
(anterior column), the ilioischial line (posterior column), the
anterior lip of the acetabulum, and the posterior lip of the acetabulum.(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.) -
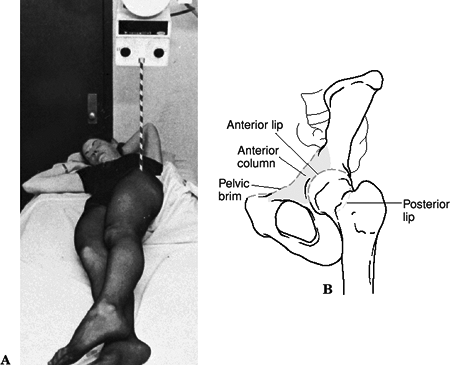
Obturator oblique view (45-degree
internal rotation view): This is best for evaluating the anterior
column and posterior wall of the acetabulum (Fig. 26.4).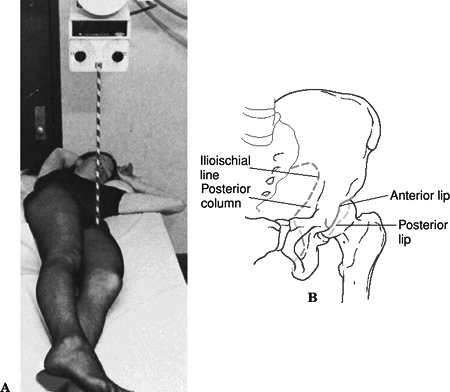 Figure
Figure
26.3. Iliac oblique view (A) This view is taken by rotating the patient
into 45 degrees of external rotation by elevating the uninjured side on
a wedge. (B) Diagram of the anatomic landmarks of the left hemipelvis
on the iliac oblique view. This view best demonstrates the posterior
column of the acetabulum, outlined by the ilioischial line, the iliac
crest, and the anterior lip of the acetabulum.(From Tile M. Fractures of the Pelvis and Acetabulum, 2nd ed. Baltimore: Williams & Wilkins, 1995.) -
Computed tomography (CT): This provides
additional information regarding size and position of column fractures,
impacted fractures of the acetabular wall, retained bone fragments in
the joint, degree of comminution, and sacroiliac joint disruption.
Three-dimensional reconstruction allows for digital subtraction of the
femoral head, resulting in full delineation of the acetabular surface.
P.292
CLASSIFICATION
Judet-Letournel (Fig. 26.5)
Based on degree of columnar damage, there are ten fracture patterns, five “elementary” and five “associated:”
| Elementary Fractures | Associated Fractures |
| Posterior wall | T-shaped |
| Posterior column | Posterior column and posterior wall |
| Anterior wall | Transverse and posterior wall |
| Anterior wall | Transverse and posterior wall |
| Anterior column | Anterior column/posterior hemitransverse |
| Transverse | Both-column |
P.293
Elementary Fractures
 |
|
Figure
26.4. Obterator oblique view (A) This view is taken by elevating the affected hip 45 degrees to the horizontal by means of a wedge and directing the beam through the hip joint with a 15-degree upward tilt. (B) Diagram of the anatomy of the pelvis on the obturator oblique view. (From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)
|
-
Posterior wall fracture
-
This involves a separation of posterior articular surface.
-
Most of the posterior column is undisturbed.
-
It is often associated with posterior femoral head dislocation.
-
The posterior wall fragment is best visualized on the obturator oblique view.
-
“Marginal impaction” is often present in
posterior fracture-dislocations (articular cartilage impacted into
underlying cancellous bone).-
In a series by Brumback, marginal
impaction was identified in 23% of posterior fracture-dislocations
requiring open reduction. This was best appreciated on CT scan.
-
-
-
Posterior column fracture
-
The ischium is disrupted.
-
The fracture line originates at the
greater sciatic notch, travels across the retroacetabular surface,
exits at the obturator foramen.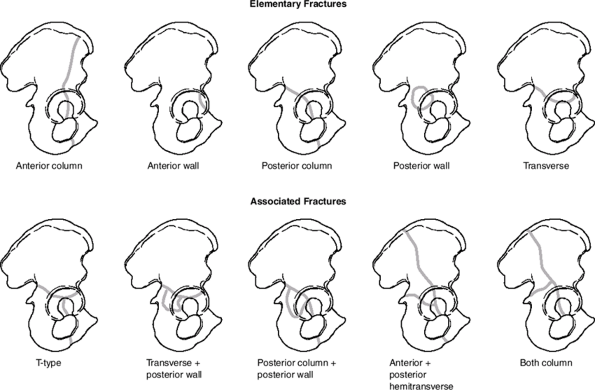 Figure 26.5. Letournel classification of acetabular fractures.
Figure 26.5. Letournel classification of acetabular fractures. -
The ischiopubic ramus is fractured.
-
Medial displacement of the femoral head can occur.
P.294P.295 -
-
Anterior wall fracture
-
Disruption of a small portion of the anterior roof and acetabulum occurs.
-
Much of anterior column is undisturbed.
-
The ischiopubic ramus is not fractured.
-
The teardrop is often displaced medially with respect to the ilioischial line.
-
-
Anterior column fracture
-
This is associated with disruption of the iliopectineal line.
-
It is often associated with anteromedial displacement of the femoral head.
-
It is classified according to the level
at which the superior margin of the fracture line divides the
innominate bone: low, intermediate, or high pattern. -
The more superiorly the fracture line ascends, the greater the involvement of the weight-bearing aspect of the acetabulum.
-
CT may be helpful in delineating the degree of articular surface involvement.
-
-
Transverse fracture
-
The innominate bone is separated into two fragments, dividing the acetabular articular surface in one of three ways:
-
Transtectal: through the acetabular dome.
-
Juxtatectal: through the junction of the acetabular dome and fossa acetabuli.
-
Infratectal: through the fossa acetabuli.
-
-
The more superior the fracture line, the greater the displacement of the acetabular dome will be.
-
The femoral head follows the inferior ischiopubic fragment and may dislocate centrally.
-
The ilioischial line and teardrop maintain a normal relationship.
-
CT typically demonstrates an AP fracture line.
-
Associated Fractures
-
Associated posterior column and posterior wall fracture
-
Two elementary fracture patterns are
present. The posterior wall is usually markedly displaced/rotated in
relation to the posterior column. This injury represents one pattern of
posterior hip dislocation that is frequently accompanied by injury to
the sciatic nerve.
-
-
T-shaped fracture
-
This combines a transverse fracture of
any type (transtectal, juxtatectal, or infratectal) with an additional
vertical fracture line that divides the ischiopubic fragment into two
parts. The vertical component, or stem, may exit anteriorly,
inferiorly, or posteriorly depending on the vector of the injurious
force. The vertical component is best seen on the obturator oblique
view.
-
-
Associated transverse and posterior wall fracture
-
Marginal impaction may exist; this is best evaluated by CT.
-
Associated anterior column and posterior hemitransverse fracture
-
This combines an anterior wall or
anterior column fracture (of any type) with a fracture line that
divides the posterior column exactly as it would a transverse fracture.
It is termed a hemitransverse because the “transverse” component
involves only one column. -
Importantly, in this fracture a piece of
acetabular articular surface remains nondisplaced and is the key for
operative reduction of other fragments.
-
-
Both-column fracture
-
This is the most complex type of acetabular fracture, formerly called a “central acetabular fracture.”
-
Both columns are separated from each other and from the axial skeleton, resulting in a “floating” acetabulum.
-
The “spur” sign above the acetabulum on an obturator oblique radiograph is diagnostic.
-
OTA Classification of Acetabular Fractures
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
TREATMENT
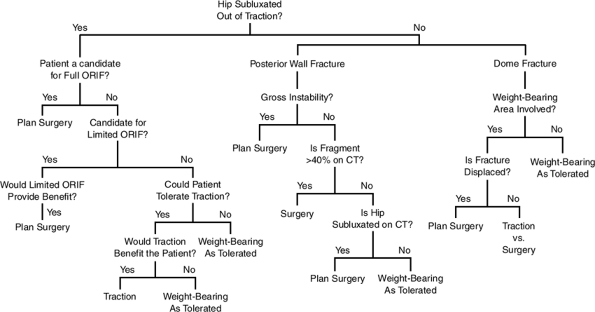
The goal of treatment is anatomic restoration of the articular surface to prevent posttraumatic arthritis (Fig. 26.6).
Initial Management
The patient is usually placed in skeletal traction to
allow for initial soft tissue healing, allow associated injuries to be
addressed, maintain the length of the limb, and maintain femoral head
reduction within the acetabulum.
allow for initial soft tissue healing, allow associated injuries to be
addressed, maintain the length of the limb, and maintain femoral head
reduction within the acetabulum.
Nonoperative
-
A system for roughly quantifying the
acetabular dome following fracture can be employed using three
measurements: the medial, anterior, and posterior roof arcs, measured
on the AP, obturator oblique, and the iliac oblique views, respectively.-
The roof arc is formed by the angle
between two lines, one drawn vertically through the geometric center of
the acetabulum, the other from the fracture line to the geometric
center. -
Roof arc angles are of limited utility for evaluation of both column fractures and posterior wall fractures.
-
-
Nonoperative treatment may be appropriate in:
-
Displacement of less than 2 to 5 mm in
the dome, depending on the location of the fracture and patient
factors, with maintenance of femoral head congruency out of traction,
and an absence of intraarticular osseous fragments. -
Distal anterior column or transverse
(infratectal) fractures in which femoral head congruency is maintained
by the remaining medial buttress. -
Maintenance of the medial, anterior, and the posterior roof arcs greater than 45 degrees.
-
 |
|
Figure 26.6. Treatment algorithm for acetabular fractures.
(From Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 5th ed. Baltimore: Lippincott Williams & Wilkins, 2002.)
|
P.297
P.298
Operative
-
Surgical treatment is indicated for:
-
Displaced acetabular fractures (>2 to 3 mm).
-
Inability to maintain a congruent joint out of traction.
-
Large posterior wall fragment.
-
Removal of an interposed intraarticular loose fragment.
-
A fracture-dislocation that is irreducible by closed methods.
-
-
Surgical timing
-
Surgery should be performed within 2 weeks of injury.
-
It requires
-
A well-resuscitated patient.
-
An appropriate radiologic workup.
-
An appropriate understanding of the fracture pattern.
-
An appropriate operative team.
-
-
Surgical emergencies include:
-
Open acetabular fracture.
-
New-onset sciatic nerve palsy after closed reduction of hip dislocation.
-
Irreducible posterior hip dislocation.
-
Medial dislocation of femoral head against cancellous bone surface of intact ilium.
-
-
-
Morel-Lavallé Lesion (Skin Degloving Injury)
-
This is infected in one-third of cases.
-
This requires thorough debridement before definitive fracture surgery.
-
-
Not been shown to be predictive of clinical outcome
-
Fracture pattern
-
Posterior dislocation
-
Initial displacement
-
Presence of intraarticular fragments
-
Presence of acetabular impaction
-
-
Has been shown to be predictive of clinical outcome
-
Injury to cartilage or bone of femoral head
-
Damage: 60% good/excellent result
-
No damage: 80% good/excellent result
-
-
Anatomic reduction
-
Age of patient: predictive of the ability to achieve an anatomic reduction
-
Stability
-
Instability is most common in posterior
fracture types but may be present when large fractures of the
quadrilateral plate allow central subluxation of the femoral head or
anterior with major anterior wall fractures. -
Central instability results when a
quadrilateral plate fracture is of sufficient size to allow for central
subluxation of the femoral head. A medial buttress with a spring plate
or cerclage wire is necessary to restore stability. -
Anterior instability results from a large
anterior wall fracture or as part of an anterior type fracture with
posterior hemitransverse fracture.
Congruity
-
Displaced dome fractures rarely reduce
with traction; surgery is usually necessary for adequate restoration of
the weight-bearing surface. -
High transverse or T-type fractures are
shearing injuries that are grossly unstable when they involve the
superior, weight-bearing dome. Nonoperative reduction is virtually
impossible, whereas operative reduction can be extremely difficult. -
Displaced both-column fractures (floating
acetabulum): Surgery is indicated for restoration of congruence if the
roof fragment is displaced and secondary congruence cannot be obtained
or if the posterior column is grossly displaced. -
Retained osseous fragments may result in
incongruity or an inability to maintain concentric reduction of the
femoral head. Avulsions of the ligamentum teres need not be removed
unless they are of substantial size. -
Femoral head fractures generally require open reduction and internal fixation to maintain sphericity and congruity.
-
Soft tissue interposition may necessitate operative removal of the interposed tissues.
-
Assessment of reduction includes:
-
Restoration of pelvic lines.
-
Concentric reduction on all three views.
-
The goal of anatomic reduction.
-
Surgical Approaches
Approaches to the acetabulum include the
Kocher-Langenbach ilioinguinal and extended iliofemoral. No single
approach provides ideal exposure of all fracture types. Proper
preoperative classification of the fracture configuration is essential
to selecting the best surgical approach.
Kocher-Langenbach ilioinguinal and extended iliofemoral. No single
approach provides ideal exposure of all fracture types. Proper
preoperative classification of the fracture configuration is essential
to selecting the best surgical approach.
-
Kocher-Langenbach
-
Indications
-
Posterior wall fractures
-
Posterior column fractures
-
Posterior column/posterior wall fractures
-
Juxtatectal/infratectal transverse or transverse with posterior wall fractures
-
Some T-type fractures
-
-
Access
-
Entire posterior column
-
Greater and lesser sciatic notches
-
Ischial spine
-
Retroacetabular surface
-
Ischial tuberosity
-
Ischiopubic ramus
-
-
Limitations
-
Superior acetabular region
-
Anterior column
-
Fractures high in greater sciatic notch
-
-
Complications
-
-
Ilioinguinal
-
Indications
-
Anterior wall
-
Anterior column
-
Transverse with significant anterior displacement
-
Anterior column/posterior hemitransverse
-
Both-column
-
-
Access
-
Sacroiliac joint
-
Internal iliac fossa
-
Pelvic brim
-
Quadrilateral surface
-
Superior pubic ramus
-
Limited access to external iliac wing
-
-
Complications
-
Direct hernia: 1%
-
Significant lateral femoral circumflex artery nerve numbness: 23%
-
External iliac artery thrombosis: 1%
-
Hematoma: 5%
-
Infection: 2%
-
-
-
Extended iliofemoral
-
Indications
-
Transtectal transverse plus posterior wall or T-shaped fractures
-
Transverse fractures with extended posterior wall
-
T-shaped fractures with wide separations of the vertical stem of the “T” or those with associated pubic symphysis dislocations
-
Certain associated both column fractures
-
Associated fracture patterns or transverse fractures operated on more than 21 days following injury
-
-
Access
-
External aspect of the ilium
-
Anterior column as far medial as the iliopectineal eminence
-
Posterior column to the upper ischial tuberosity
-
-
Complications
-
Infection: 2% to 5%
-
Sciatic nerve palsy: 3% to 5%
-
Heterotopic ossification: 20% to 50% without prophylaxis
-
-
Postoperative Care
-
Indomethacin or irradiation is indicated for heterotopic ossification prophylaxis.
-
Chemical prophylaxis, sequential compression devices, and compressive stockings for thromboembolic prophylaxis are recommended.
-
Mobilization out of bed is indicated as associated injuries allow, with pulmonary toilet and incentive spirometry.
-
Full weight bearing on the affected
extremity should be withheld until radiographic signs of union are
present, generally by 8 to 12 weeks postoperatively.
P.301
COMPLICATIONS
-
Surgical wound infection: The risk is
increased secondary to the presence of associated abdominal and pelvic
visceral injuries. Local soft tissue injury from the original impact
force may cause closed degloving or local abrasions. Postoperative
hematoma formation occurs frequently, further contributing to potential
wound infection. -
Nerve injury
-
Sciatic nerve: The Kocher-Langenbach
approach with prolonged or forceful traction can cause sciatic nerve
palsy (most often the peroneal branch; incidence, 16% to 33%). The use
of somatosensory-evoked potentials may decrease the risk of sciatic
injury in posterior approaches. -
Femoral nerve: The ilioinguinal approach
may result in traction injury to the femoral nerve. Rarely, the femoral
nerve may be lacerated by an anterior column fracture. -
Superior gluteal nerve: This is most
vulnerable in the greater sciatic notch. Injury to this nerve during
trauma or surgery may result in paralysis of the hip abductors, often
causing severe disability.
-
-
Heterotopic ossification: The incidence
ranges from 3% to 69%, highest with the extended iliofemoral approach
and second highest with the Kocher-Langenbach. The highest risk is a
young male patient undergoing a posterolateral extensile approach in
which muscle is removed. The lowest risk is with use of the
ilioinguinal approach. Both indomethacin and low-dose radiation have
been helpful in reducing the incidence of this complication. -
Avascular necrosis: This devastating
complication occurs in 6.6% of cases, mostly with posterior types
associated with high-energy injuries. -
Chondrolysis: This may occur with
nonoperative or operative treatment, resulting in posttraumatic
osteoarthritis. Concentric reduction with restoration of articular
congruity may minimize this complication.