Closed Reduction and Percutaneous Pinning of Supracondylar Fractures of the Distal Humerus in the Child
Trauma > 3 – Closed Reduction and Percutaneous Pinning of
Supracondylar Fractures of the Distal Humerus in the Child
common and problematic elbow fracture that occurs in children. This
fracture represents between 55% and 80% of all children’s elbow
fractures. It occurs from a fall usually from a height greater than 2
feet. In a review of 391 supracondylar fractures admitted to Children’s
Hospital in San Diego over an 8-year period, 29% of the injuries
occurred in falls from school playground equipment (5) (Fig. 3-1).
fracture. Extension-type supracondylar fractures of the humerus have
been classified into three types. We have subcategorized these types as
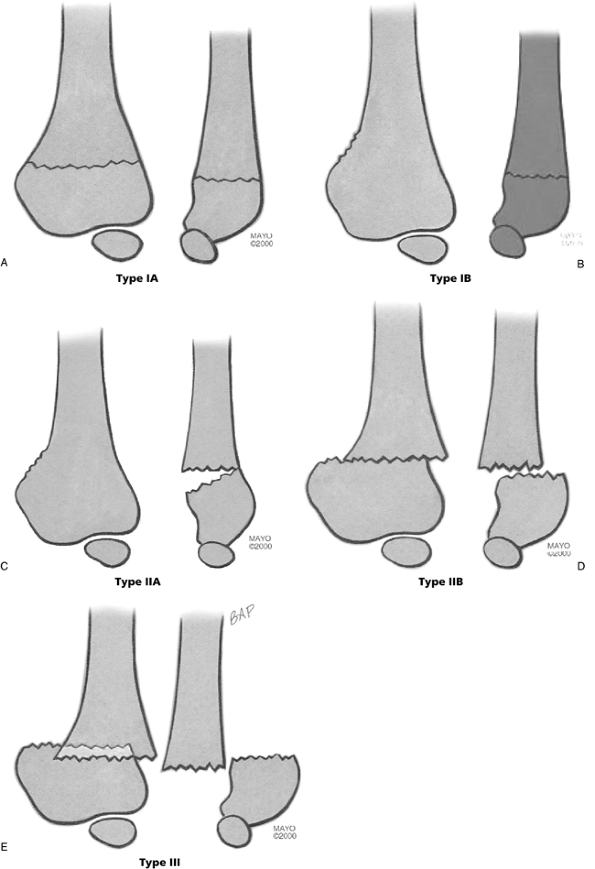
follows (Fig. 3-2).
diagnosis of nondisplaced fracture is made by the clinical examination,
which reveals tenderness, both medially and laterally, over the distal
humeral condyles. Though radiographs may show no cortical disruption, a
posterior fat pad sign is often present (16).
With this fracture the diagnosis may not be confirmed until 3 weeks
after injury, when radiographs will show callus formation. The
preferred treatment of a nondisplaced supracondylar fracture of the
humerus is a long-arm cast, elbow flexed to 90 degrees for 3 weeks.
 |
|
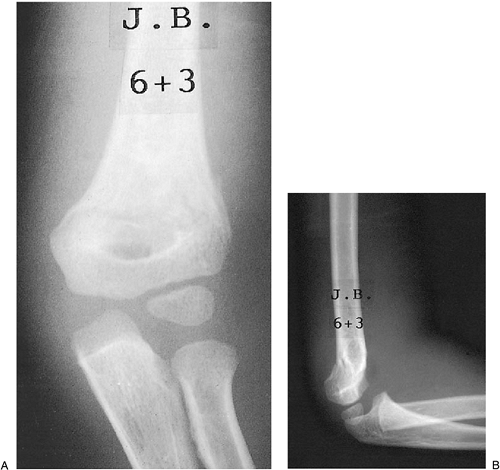
Figure 3-1. Etiology of 393 displaced supracondylar fractures treated at Children’s Hospital, San Diego, 1984 to 1992.
|
carefully to avoid underestimating the degree of deformity, which can
lead to subsequent cubitus varus (4). If the
radiographs reveal compression (torus) or collapse of the medial
column, closed reduction may be required. The carrying angle of the
contralateral, uninvolved elbow should be carefully checked. Children
with little physiologic valgus (10 degrees or less; i.e., cubitus
rectus) are at particular risk for developing an unsightly cubitus
varus deformity.
should be evaluated further. Because of pain and guarding, the child’s
elbow cannot be fully extended and the carrying angle of the injured
side cannot be determined without a general anesthetic. In the
operating room, these minimally angulated fractures can be more fully
examined, and, if necessary, a closed reduction and percutaneous
pinning using one or two 0.062 smooth K-wires via a lateral approach
can be performed (Fig. 3-3).
the humeral/capitellar relationship of more than 20 degrees will
require reduction (Fig. 3-4). Again, clinical
evaluation of the uninjured elbow, especially noting
hyperextensibility, will help define the need for further examination
of the child’s injured arm under anesthesia.
demonstrates both rotational and hyperextension deformity
radiographically, but some cortical contact remains, usually on the
posterior side.
need general anesthesia and closed reduction in the operating room.
Type IIB is more difficult to reduce than IIA and requires correction
of the angulation and rotation. If there is minimal swelling and a
normal neurocirculatory status, this can be done semielectively if the
child has recently eaten. Closed reduction and percutaneous pinning
using two lateral pins is our treatment of choice for type II fractures
(Fig. 3-5).
are an extension type, with the proximal fragment anterior to the
distal fragment. Only 2% are the flexion type with anterior
displacement of the distal fragment (12). In 70% of the cases, the distal fragment is displaced posteromedially with respect to the proximal fragment (12). Medially displaced fractures, when incompletely reduced, will lead to cubitus varus deformity.
reduction and percutaneous pinning, which offers advantages in types II
and III injuries as well as in type IB injuries with medial collapse:
-
It provides immediate stability of the fracture fragments.
![]() Figure 3-2. Classification of supracondylar fractures. A: Type IA—nondisplaced AP (left), lateral (right) appearance. B: Type IB—minimally displaced/medial compression AP (left), lateral (right) appearance. C: Type IIA—hyperextension posterior cortex intact AP (left), lateral (right) appearance. D: Type IIB—displaced/angulated with osseous contact AP (left), lateral (right) appearance. E: Type III—completely displaced AP (left), lateral (right) appearance.
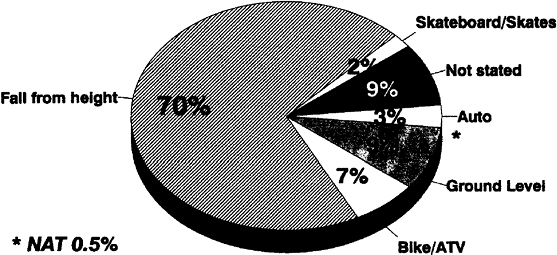
Figure 3-2. Classification of supracondylar fractures. A: Type IA—nondisplaced AP (left), lateral (right) appearance. B: Type IB—minimally displaced/medial compression AP (left), lateral (right) appearance. C: Type IIA—hyperextension posterior cortex intact AP (left), lateral (right) appearance. D: Type IIB—displaced/angulated with osseous contact AP (left), lateral (right) appearance. E: Type III—completely displaced AP (left), lateral (right) appearance. Figure 3-3. Supracondylar fracture IB: medial compression. Examination in the operating room confirmed the varus alignment (A).
Figure 3-3. Supracondylar fracture IB: medial compression. Examination in the operating room confirmed the varus alignment (A).
Closed reduction and percutaneous pinning with a single K-wire from the
lateral approach was utilized to maintain the reduction (B).![]() Figure 3-4. Supracondylar fracture IIA. The AP view shows only the slightest suggestion of a fracture line (A). The lateral view shows extension of the humeral/capitellar relationship of more than 20 degrees (B).
Figure 3-4. Supracondylar fracture IIA. The AP view shows only the slightest suggestion of a fracture line (A). The lateral view shows extension of the humeral/capitellar relationship of more than 20 degrees (B).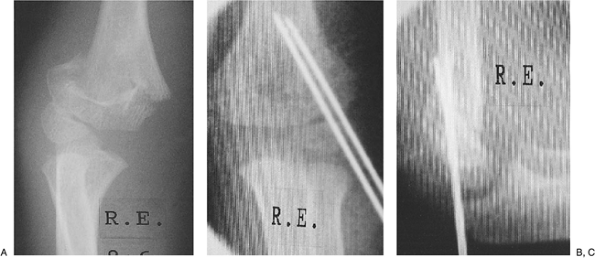 Figure 3-5. Supracondylar fracture IIB. Displaced, angulated, and rotated fracture (A). Closed reduction and percutaneous pinning with two K-wires from the lateral approach were performed (B). Lateral radiograph demonstrates reduction of the humeral/capitellar relationship (C).
Figure 3-5. Supracondylar fracture IIB. Displaced, angulated, and rotated fracture (A). Closed reduction and percutaneous pinning with two K-wires from the lateral approach were performed (B). Lateral radiograph demonstrates reduction of the humeral/capitellar relationship (C). -
It allows evaluation of the carrying
angle after reduction and pinning. Any varus component can be
appreciated immediately and corrected. This is difficult to do with
traction or casting techniques. -
It is simple and cost-effective. The hospital stay is less than 24 hours.
-
It addresses concerns about vascular
safety. If there are difficulties with arterial occlusion, closed
reduction and stabilization of the fracture fragment will restore the
pulse in nearly 90% of cases (15). In the rare
case of significant arterial injury, vascular exploration and repair
are greatly facilitated by immediate fracture stabilization.
-
Severe swelling.
If the swelling is so severe that adequate reduction is impossible by
closed means, then open reduction and pin fixation are performed. -
Open fracture.
Usually, the proximal fragment will perforate the skin anteriorly
through the brachialis muscle, creating a grade I open fracture. These
are best treated by an anterior debridement of the fracture fragment,
with reduction and internal fixation of the fracture fragments. Care
must be taken not to injure the anterior neurovascular structures
during the fracture reduction and stabilization. -
Irreducible fracture.
In markedly displaced type III fractures, the proximal humeral shaft
will occasionally buttonhole into the brachialis muscle and even dimple
the skin anteriorly in the cubital fossa (2).
Closed reduction may not be possible because of interposed periosteum
and muscle, and open reduction is necessary. We prefer an initial
lateral approach but will not hesitate to add a medial incision to
facilitate gentle reduction of the fracture fragments and then pinning
with 0.062 smooth K-wires. -
Late diagnosis or loss of reduction.
If the fracture is more than a week old, callus formation will usually
preclude closed reduction and percutaneous pinning. Open reduction and
internal fixation are generally required. We will perform this on
displaced fractures that are more than 6 weeks old, as it is possible
to define the fracture margins, remove the callus, and then obtain a
near anatomic reduction. Late valgus osteotomy of the distal humerus is
reserved for significant cases of cubitus varus and is used as a
reconstructive procedure.
-
Anesthesia.
If the child cannot undergo general anesthesia because of having
recently eaten or having experienced multiple injuries, temporary
splinting is utilized until the following day. -
Technical difficulty.
Percutaneous pinning of the distal humerus in a child can be difficult,
even in a stable type IB minimally angulated fracture. The technique
should be done by one with expertise using this procedure. By treating
supracondylar fractures by this protocol, experience may be rapidly
gained on the more stable patterns so that the more difficult type III
fractures can also be handled. -
Concern about nerve function.
Iatrogenic ulnar nerve palsy can occur following pinning, so concern
about the status of this nerve must be resolved before the technique is
performed.
perform a careful neurocirculatory evaluation before multiple
examinations by other physicians or attempts at blood drawing have
occurred. Examine the uninjured arm to assess the carrying angle and
hyperextension. Assess the radial pulse, capillary refill, and volar
and dorsal compartments. Pinprick examination for sensation is poorly
tolerated by most children and is rarely used. We prefer light touch
and two-point discrimination to evaluate sensation. The most common
nerve injured with a displaced extension-type supracondylar fracture is
the anterior interosseous nerve. This purely motor branch of the median
nerve is best evaluated by active flexion on the distal interphalangeal
joint of the index and thumb.
elbow should include anteroposterior (AP), lateral, and both oblique
views of the distal humerus. AP and lateral views of the contralateral,
uninjured elbow are essential for evaluating Baumann’s angle and to
recognize minimal displacement of an ossific center. Clinical and
radiographic evaluation of the entire forearm on the injured side is
essential, as there was a 6% incidence of ipsilateral distal radius
fractures with displaced supracondylar fractures in our series (5).
pulses, prompt closed reduction will usually restore the vascular
integrity. After reduction, if the pulses remain absent to palpation
and Doppler evaluation, and the forearm appears ischemic, percutaneous
stabilization is performed before surgical exploration of the brachial
artery. Preoperative angiography is not utilized, as it simply prolongs
the time to the operating room and can increase the period of vascular
compromise and ischemia (10,15).
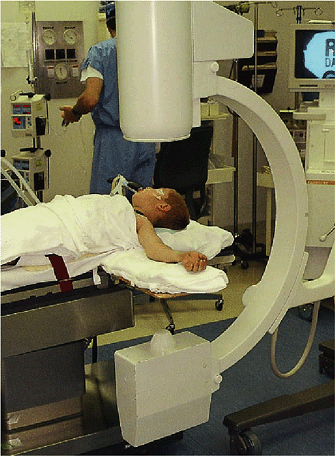
is under general anesthesia and is positioned on the operating table
with the injured arm placed on a radiolucent arm board. A bed sheet is
positioned around the child’s torso, so that the anesthesiologist can
provide countertraction when reduction of the extremity is carried out
by the orthopaedic surgeon. The child’s head needs to be braced with
tape or a bolster to prevent it from moving off the operating table
when traction is applied (Fig. 3-6).
with the films of the contralateral elbow, are evaluated. If an
adequate AP radiograph has not been obtained because of the marked
displacement and overriding of the fracture fragments, a traction AP
and lateral radiograph can be obtained once the child is asleep to more
fully evaluate the fracture pattern and to rule out intraarticular
involvement (T-condylar fracture pattern).
operating table so that the C-arm is free to rotate under the arm board
in both an AP and a lateral position without rotating the patient’s arm
(Fig. 3-6).
and operative personnel use protective lead aprons and sterile gowns.
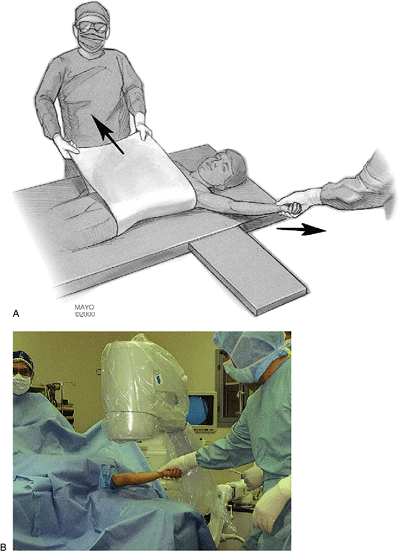
Longitudinal traction is first applied by the orthopaedic surgeon and
countertraction is provided by the anesthesiologist with the previously
placed sheet about the patient’s trunk (Fig. 3-7).
The image is viewed in the AP projection and any translation of the
distal fragment is corrected by varus or valgus manipulation (Fig. 3-8).
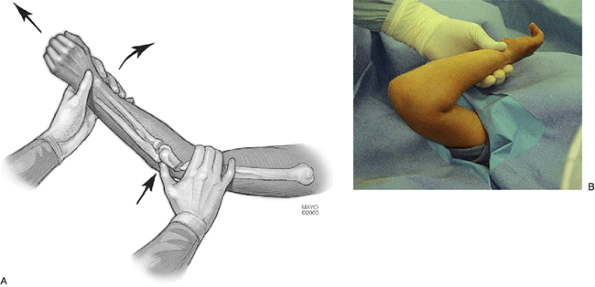
Once adequate length and alignment have been obtained on the AP view,
the traction is continued while gentle pressure is applied posteriorly
over the olecranon and the elbow is gradually flexed. This pressure is
increased at 30 to 40 degrees of flexion to reduce the distal fragment
onto the anterior fragment. The elbow is hyperflexed to approximately
130 degrees and held in about neutral to slight pronation, while the
image intensifier is rotated to obtain a lateral view of the elbow (Fig. 3-9).
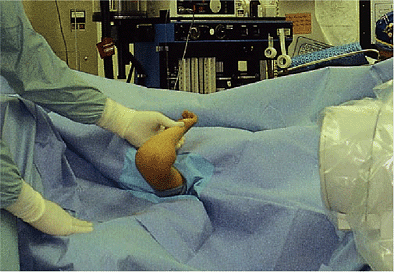
humeral-to-capitellar relationship obtained, percutaneous pinning can
be carried out (Fig. 3-10). If an oblique spike
of bone is viewed, a rotational malalignment is present and
re-reduction may be necessary. Next, while maintaining the elbow in the
hyperflexed position, two smooth 0.062 K-wires are inserted through the
capitellum (lateral approach) across the fracture site (Fig. 3-11).
Even in a minimally displaced fracture, this may be a difficult task in
the hands of an inexperienced surgeon. When combined with an unstable
fracture and marked soft-tissue swelling, this maneuver may be
extremely difficult and frustrating. After the first pin is inserted,
the lateral image will demonstrate its placement across the distal
humerus. A second K-wire is added for stability through the lateral
condyle.
projection, the elbow can safely be extended and an AP view can be
obtained to demonstrate satisfactory reduction and correct positioning
of the pins (Fig. 3-12). It is imperative that
both of these pins engage the far cortex. If the reduction is not
acceptable at this point, pin removal and repeat closed reduction are
necessary. An excellent lateral view of the distal humerus can now be
obtained
by externally rotating the arm, with the image intensifier still maintained in the AP position (Fig. 3-13).
If one attempts to do this before pin fixation of the fracture
fragments, rotational malalignment can occur. At this point, a medial
pin can be inserted for a type III supracondylar fracture. The
orthopaedic surgeon should massage the swelling out of the medial side
around the epicondyle and place his thumb over the ulnar nerve to
protect it while inserting the 0.062 K-wire. Extending the elbow to
about 50 degrees will reduce the likelihood of the ulnar nerve
subluxing anteriorly, which sometimes occurs with hyperflexion. A 5-mm
incision over the medial epicondyle with blunt dissection down to
bone/cartilage will allow direct visualization if the surgeon is unable
to palpate the nerve due to swelling or inexperience.
 |
|
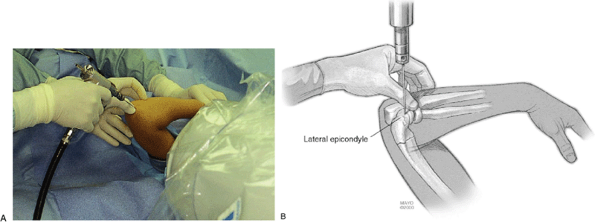
Figure 3-6.
Under general anesthesia, the patient is positioned on the operating room (OR) table with a wooden arm board and a sheet is placed under the patient’s axilla for the anesthesiologist to provide countertraction. The image intensifier is placed at the head of the OR table. In this position, a lateral image can be obtained without rotating the arm. |
 |
|
Figure 3-7.
The arm is prepped and draped. Longitudinal traction is applied by the operating surgeon and countertraction from the anesthesiologist utilizing the previously placed sheet in the patient’s axilla (A). The image is brought into position for an AP view (B). |
 |
|
Figure 3-8. Under image control, any translation is corrected by varus or valgus pressure.
|
 |
|
Figure 3-9.
Once adequate length and alignment have been obtained on the AP view, the traction is continued while gentle pressure is applied posteriorly over the olecranon and the elbow is gradually flexed (A). The elbow is held in maximum flexion of around 130 degrees and in neutral to slight pronation (B). |
 |
|
Figure 3-10.
A lateral image is now obtained. If the reduction has been accomplished and a normal humeral-to-capitellar relationship obtained, percutaneous pinning can be carried out. |
 |
|
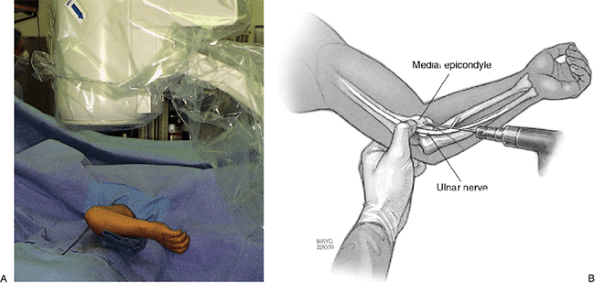
Figure 3-11. While maintaining the elbow in the hyperflexed position (A). Two K-wires (0.062) are inserted through the capitellum (lateral approach) across the fracture site under image control (B).
|
on the previously placed lateral pins. The medial pin will provide
greater stability and prevent loss of the reduction
while the cast is being applied (18).
For types I and II fractures, we use only the two parallel or divergent
lateral pins. This avoids the risk to the ulnar nerve. These inherently
more stable fracture patterns do not require the medial pin. The
K-wires are carefully bent to 90 degrees outside of the skin (Fig. 3-14).
We leave 1 inch of K-wire extending out to prevent pin migration under
the skin and to facilitate removal in the outpatient clinic 3 weeks
later.
 |
|
Figure 3-12.
Once the two K-wires are across the fracture on the lateral projection, the elbow can safely be extended and an AP view obtained to demonstrate satisfactory reduction and correct positioning of the K-wires. If reduction is unsatisfactory, pin removal and closed reduction must be reattempted. |
 |
|
Figure 3-13. An excellent lateral view can be obtained by externally rotating the arm at this point (A).
A medial pin can be inserted for type III supracondylar fractures. The surgeon extends the patient’s elbow and inserts the pin while protecting the ulnar nerve with the surgeon’s thumb (B). The surgeon triangulates on the previously placed lateral pins when inserting this third K-wire. This K-wire will prevent loss of reduction for these more unstable fractures. For type II fractures, we use only the two lateral parallel or divergent K-wires. |
 |
|
Figure 3-14.
The pins are bent to a 90-degree angle, leaving 1 inch extending to prevent migration under the skin. Felt, soft roll, and a long-arm cast that is split are then applied. The patient is observed in the hospital for 24 hours. The patient will be rechecked in 1 week and the pins removed with radiographs out of plaster at 3 weeks. |
fracture, closed reduction and single cross-pin fixation through the
radial styloid before closed reduction and pinning of the supracondylar
fracture provide the most effective treatment in our experience.
before cast application. The patient is then placed in a long-arm
fiberglass cast, which is positioned at approximately 80 degrees of
elbow flexion. The cast is univalved and spread, and the patient is
observed in the hospital overnight before being discharged.
using this extremity. Dangling the extremity with the elbow casted in
this position (i.e., less than 90 degrees flexion) may result in
movement of the cast that can cause the pins to be pulled out
prematurely and the fracture reduction to be lost. For this reason the
patient is seen 1 week after discharge for clinical as well as
radiographic evaluation. At 3 weeks following injury, the cast is
removed for radiographs. In nearly all cases, there is sufficient
callus formation to allow for pin removal and gentle mobilization of
the elbow. A light dressing is applied to the pin sites, and the
patient utilizes a sling for about a week. Bathing is permitted at this
time to encourage early range of motion and prevent stiffness.
evaluation and at 6 and 12 months for clinical and radiographic
evaluation. Very occasionally, growth plate injury can occur with this
fracture, and it is important to recognize this problem early. Physical
therapy has not been necessary in any of our patients when mobilization
was begun 3 weeks after the injury.
type III injuries are treated by the preceding protocol. The results
have been extremely satisfying, with nearly anatomic reduction in all
cases and perioperative hospital stays of less than 24 hours. Range of
motion returns to normal in 95% of the children within 3 months.
Cubitus varus has rarely occurred and is usually of minimal magnitude.
Only one child originally treated by this protocol has required
subsequent valgus osteotomy.
of the distal humerus are well recognized. Acute vascular compromise
with subsequent compartment syndrome can result in Volkmann’s
contracture if not treated appropriately. The most common late
complication is fracture malunion leading to a cubitus varus deformity.
The most commonly injured nerve in a displaced supracondylar fracture
is the anterior interosseous branch of the median nerve. Some series do
not recognize this because this nerve is often not assessed
preoperatively. After injury to the median nerve, the most likely
nerves injured, in decreasing frequency, are the radial and ulnar
nerves. On the other hand, in our experience, most ulnar neuropathies
are iatrogenic, secondary to pin placement. Also, in all our cases and
in those reviewed in the literature, the ulnar neuropathy cleared from
1 to 6 months after pin removal (6,12,17). If an ulnar neuropathy is first
appreciated after reduction and a three-pin technique has been
utilized, we recommend immediate removal of the medial pin. With a
two-cross-pin technique, we would not recommend removal of the medial
pin until 3 weeks after the injury to avoid loss of reduction.
supracondylar fracture, the radial pulse will be absent at
presentation. In greater than 90% of these cases (10,15), the pulse will return with closed reduction and pinning of the fracture under general anesthesia.
fracture should be reduced and stabilized by percutaneous pinning or,
if necessary, even open reduction and fixation. At this point, nearly
all authors recommend in the presence of an absent radial pulse and
with forearm and hand ischemia exploration of the artery at the
fracture site. Shaw et al. explored three cases and documented intimal
tears with thrombus obstructing the brachial artery lumen. In two
patients, the injured segment was excised and replaced by a saphenous
bone graft; prophylactic fasciotomy was also performed. One patient
that was explored was noted to have brachial artery entrapment that was
treated by appropriate release. Schoenecker et al. recommend brachial
artery exploration if Dopplerable pulses did not return within 30
minutes after fracture reduction (14). They
would consult a vascular surgeon to aid their exploration. Three of
seven patients explored demonstrated interluminal damage or
transsection and required saphenous bone graft. Four others
demonstrated kinked or entrapped artery at the fracture site,
necessitating mobilization of the vessel with reestablishment of the
pulses. Garbuz et al. explored five radial arteries and found a similar
ratio of luminal damage or laceration and kinking of the brachial
arteries (7). The one patient who was treated
with ligation had symptoms of long-term claudication. Eight of eleven
patients who initially had an absent pulse developed a return of the
pulse after the closed reduction. In three children the radial pulse
did not return, but no further treatment was required, as the forearm
and hand remained pink without any further neurologic deficits.
hand in 13 patients following closed reduction and percutaneous pinning
of the supracondylar fracture (13). They
recommended, as noted earlier, segmental pressure monitoring, color
flow duplex scanning, and magnetic resonance angiography (MRA) as a
noninvasive, safe technique for evaluating brachial artery patency and
collateral circulation around the elbow. The vascular injuries were
found in all 13 patients studied. Four patients had thrombus and/or
intimal tear. These patients underwent vein patch graft angioplasty.
Urokinase infusion was used intraarteriorly in four patients, and open
thrombectomy was used in one. However, at follow-up study with MRA,
these patients showed a high rate of asymptomatic reocculsion and
residual stenosis of the brachial artery. Thus they called into
question the need for vascular reconstruction of intimal tears when the
patient has a pink hand and MRA or other studies demonstrate adequate
collateral circulation. They strongly recommend that these patients be
observed with a vascular surgeon.
complication, since the popularization of immediate closed reduction
and percutaneous pinning by Flynn et al. (6).
In the review from our institution, only one compartment syndrome has
been encountered, and this was recognized early and treated
appropriately by volar compartment fasciotomy at the time of reduction
and pinning (5).
determined to be tense, intracompartmental pressures should be obtained
for the volar, dorsal, and hand compartments (8).
If the pressures are elevated above 30 mm Hg, fasciotomy should be
carried out. The brachial, radial, and ulnar arteries should be
explored at the time of decompression.
decompression of the volar forearm. This incision allows an easy
approach to the antebrachial fascia and the transverse carpal ligament
as well as to the neurovascular structures of the forearm and the
mobile wad. The incision is nearly identical to McConnell’s combined
exposure of the median and ulnar neurovascular bundles, as described by
Henry (9). A straight longitudinal incision is used for the dorsal compartment of the forearm.
removed at 3 weeks. Oral antibiotics are often used if there is
drainage or hypertropic granulation at the pin sites.
adequate reduction and pinning of supracondylar fracture of the
humerus. When it does occur, this deformity causes cosmetic concerns
and may result in secondary fractures and late ulnar nerve palsy (1,3,11).
fracture, the patient should be taken immediately to the operating room
for a closed reduction and percutaneous pinning.
circulation should be reassessed. If the forearm and hand are ischemic
and there are no palpable pulses by Doppler, a vascular surgeon should
be notified, and exploration of the artery and fracture should be
performed as previously noted by multiple authors. In nearly one-third
of the cases explored, as documented in the literature, the artery is
kinked around the fracture site and can be freed up. Often there is
associated spasm that may respond to local treatment. The majority of
the pathology noted in such cases, however, requires repair of the
brachial artery, repair of the damaged lumen, removal of thrombus, and
possible saphenous vein graft. All attempts should be made to restore
that circulation rather than ligating the brachial vessel.
pulse is present, the patient should be observed very closely, and no
exploration is recommended. In most cases, the Dopplerable pulse will
return in the first 12 hours. If no pulse returns and there is no
associated nerve injury, we would observe the patient rather than
undergo further studies and possible exploration. However, if there is
an overlying median nerve injury that may mask forearm and hand
ischemia of the compartments, consideration should be made for further
noninvasive vascular studies, MRA, and possible brachial artery
exploration with the aid of a vascular surgeon.
surgeons) are the most helpful in exploring and repairing the small
vessel of the child’s brachial artery. In these circumstances after
brachial artery repair if the period of ischemia is more than 4 hours,
prophylactic fasciotomy of the forearm should be considered.
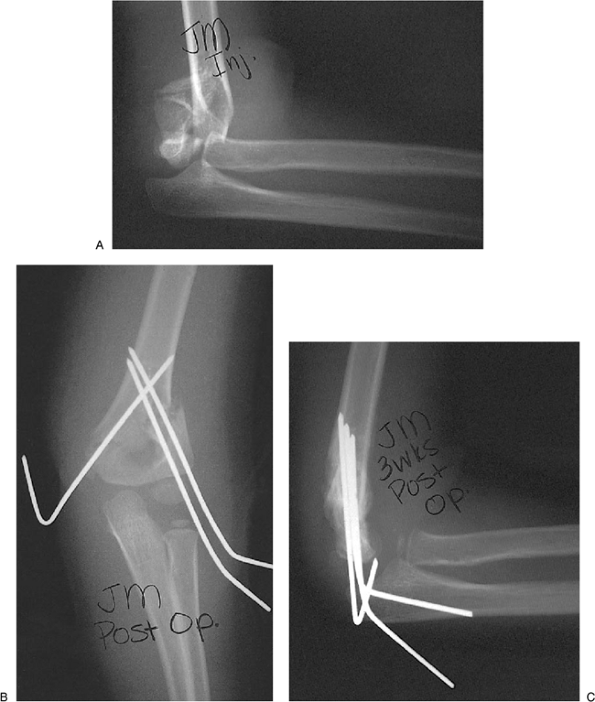
severely displaced type III fracture. Radiographs showed posterior
translation and soft-tissue swelling (Fig. 3-15A).
Using the technique described earlier, a closed reduction and
percutaneous pinning were successfully performed using two lateral pins
and one medial pin (Fig. 3-15B). Three weeks later, maintenance of the reduction is confirmed (Fig. 3-15C) and the pins were removed.
 |
|
Figure 3-15. Completely displaced supracondylar type III fracture (A); AP view (B), and lateral view (C) after two lateral pins and one medial pin were inserted (at the time of pin removal 3 weeks postoperatively).
|
MJ, Scott SM, Peters CL. Brachialis muscle entrapment in displaced
supracondylar humerus fractures: a technique of closed reduction and
report of initial results. J Pediatr Orthop 1997;17:298–302.
JL, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar
fractures of the humerus in children: sixteen years experience with
long-term follow-up. J Bone Joint Surg 1974;56A:263–272.
MB, Singer IJ, Hall JE. Supracondylar fracture of the humerus in
children: further experience with a study in orthopedic
decision-making. Clin Orthop 1984;188:90–97.
S, Tredwell SJ, Beauchamp RD, et al. Management of pulseless pink hand
in pediatric supracondylar fractures of the humerus. J Pediatr Orthop 1997;17:303–310.
BA, Kasser JR, Emans JB. Management of vascular injuries in displaced
supracondylar humerus fractures without arteriography. J Orthop Trauma 1990;4:25–29.
LE, McKellop HA, Hathaway R. Torsional strength of pin configurations
used to fix supracondylar fractures of the humerus in children. J Bone Joint Surg 1994;76A:253–256.