Postoperative Treatment Adjuncts
postsurgical stiffness, continuous passive motion (CPM) is useful in
maintaining motion and preventing stiffness.
bleeding and edema occurring within minutes after surgery or trauma,
and since motion has been shown to negate these changes (4,9), this treatment should commence as soon as possible following surgery, ideally in the recovery room (2,4). However, this is not always practical.
motion obtained at the time of surgery following intraarticular
fracture fixation, contracture release, synovectomy, and excision of
heterotopic ossification. It may also be useful following the
replacement of arthritic joints that were stiff preoperatively or in
any setting in which swelling and motion restriction are anticipated.
presence of ligamentous insufficiency if the elbow is unstable or if
fracture fixation is not rigid or is tenuous. The most common
contraindication is poor-quality soft tissue and concern about wound
dehiscence.
-
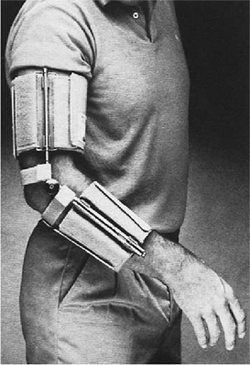
Access to an effectively designed device for inpatient and outpatient use (Figs. 9-1 and 9-2).
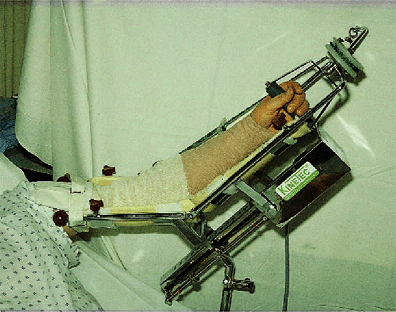 Figure 9-1. Bedside-based CPM machine.
Figure 9-1. Bedside-based CPM machine.![]() Figure 9-2. A,B: Portable CPM unit.
Figure 9-2. A,B: Portable CPM unit. -
A nursing staff knowledgeable in the applications of CPM.
-
A compliant patient.
-
Physician understanding and commitment and communication with patient and nursing staff.
-
Until motion is started, it is preferable
to elevate the limb with the elbow in full extension and wrapped in a
compressive Jones dressing to minimize swelling. -
A drain is usually useful to prevent periarticular accumulation of blood.
-
Before starting CPM, all circumferential
wrapping (Jones, cling, etc.) should be removed and replaced with a
single elastic sleeve.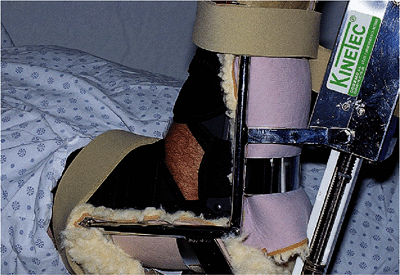 Figure 9-3. Proper position with elbow and device flexion axis coincident. In this instance the elbow is also protected in a brace.
Figure 9-3. Proper position with elbow and device flexion axis coincident. In this instance the elbow is also protected in a brace. -
The arm is carefully positioned in the
CPM device and the elbow flexion axis, or brace hinge aligned with the
flexion axis of the device (Fig. 9-3). -
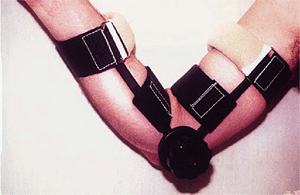
The hand and forearm are secured with well-padded supports (Fig. 9-4), especially if a brachial plexus block is being used.
-
The wound is examined to ensure that its integrity is not compromised during elbow flexion.
 |
|
Figure 9-4. The hand and forearm are secured and carefully padded if sensory changes exist due to the brachial plexus block.
|
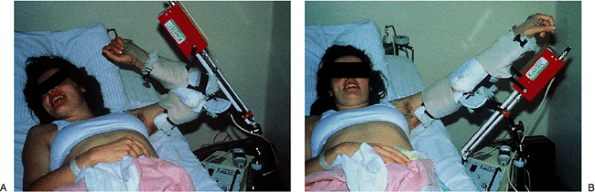
postoperative period. Once CPM is started, it is necessary that the
full range of motion be utilized (Fig. 9-5).
The tissues are being “squeezed” alternately in flexion and extension,
as CPM causes a sinusoidal oscillation in intraarticular pressure. This
not only rids the joint and tissue of excess blood and fluid, but
prevents further edema from accumulating (4).
In the first 24 hours, swelling can develop in minutes (as a result of
bleeding), so CPM should be applied early and be continuous. Only
bathroom privileges are allowed.
requires close supervision by someone skilled with its use, so it is
mandatory that the patient and family be involved and educated from the
beginning regarding the principles of use and how to monitor the limb.
Frequent checking and slight adjustments of position prevent
pressure-related problems. The arm tends to slip out of the machine, so
it must frequently be readjusted. If the full flexion arc cannot be
immediately attained, the physician must increase the adjustments as
rapidly as tolerated by the soft tissue.
amount of time required for swelling to develop increases also, so that
longer periods out of the machine are permitted.
CPM treatment at home should be used long enough to get the patient
through the period during which he or she will be unable to accomplish
the full range of motion independent of assistance. This can be several
days to several weeks, usually a month.
This permits a range from analgesia to anesthesia by varying the dose
of bupivocaine, a long-acting local anesthetic. In many cases, the dose
employed initially is sufficient to cause a complete or nearly complete
motor and sensory block. Motor blockade requires splinting of the wrist
to protect it. Moderate or complete anesthesia, as opposed to analgesia
with minimal anesthesia, requires careful attention to the status of
the limb overall, as the patient’s protective pain response is no
longer present and impending complications such as compartment syndrome
can be missed.
hospital, then removed. At that time the patient is generally able to
maintain the same range of motion with oral analgesics. The
goal is to have the patient leave the hospital capable of moving the elbow from about 10 to 135 degrees of motion actively.
 |
|
Figure 9-5. A,B: The range of motion on CPM should be full. This permits the tissues to be squeezed alternately in flexion and extension.
|
 |
|
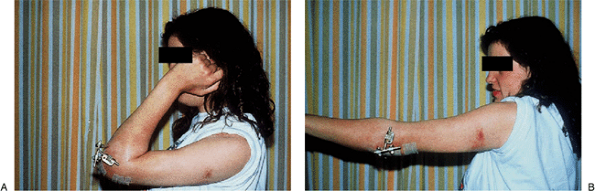
Figure 9-6. A,B:
Typical range of motion seen at 3 weeks following a distraction interposition arthroplasty treated postoperatively using continuous passive motion. |
has also been used effectively if a brachial plexus block is
contraindicated, unsuccessful, or unavailable.
require a transfusion. Excessive wound or incision pressure at full
flexion is the greatest concern. The incision must be visible to the
surgeon in the early stages of CPM treatment. If wound compromise
occurs, CPM is discontinued. Excessive pressure from an improperly
applied or padded device is particularly possible in limbs rendered
arthritic by the brachial block. Hematomas are drained surgically.
basis for its utility, there is little clinical evidence that clearly
documents its effectiveness compared with a control population (3). Nonetheless, it is the authors’ opinion, shared by others, that this is a valuable modality in selected patients (1) (Fig. 9-6).
arthritic conditions is stiffness. The accepted principle to avoid this
after a fracture is rigid fixation. Early motion has also been used to
decrease this sequelae after fractures and injury at the elbow (see the
preceding section, “Continuous Passive Motion”). In spite of these
measures, because of limitations imposed by the injury or in executing
the ideal treatment, and due to the inherent biology and response to
injury, stiffness of the elbow is a common problem (7).
Unfortunately, aggressive physical therapy to address posttraumatic
stiffness is not always successful and, in fact, may contribute to
making the contracture worse.
response to insult. The goal of splint treatment is to stretch the soft
tissues, thus maintaining the length of the capsule and ligaments.
The
question then arises as to the best method of providing a force to
stretch the periarticular soft tissues: dynamic or static adjustable
splinting. The selection of one program over the other is dependent on
one’s philosophy and interpretation of the concepts and goals of splint
usage (8,9,10).
 |
|
Figure 9-7. Commercially available dynamic splint. The tension and excursion may be adjusted by the patient.
|
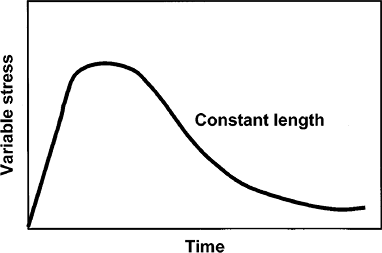
treating impending or developing stiffness, probably because dynamic
splints are readily available (Fig. 9-7). The
rationale of dynamic splinting is based on considering the elbow
capsule as a viscoelastic tissue. The response of such a tissue to a
constant force is shown in Fig. 9-8. The response in
the soft tissue to a persistent force is a deformation, which is called creep (10).
However, the constant force may cause irritation of the soft tissue;
hence inflammation is commonly associated with dynamic splinting.
Nonetheless this type splinting remains a commonly employed option for
many (8).
 |
|
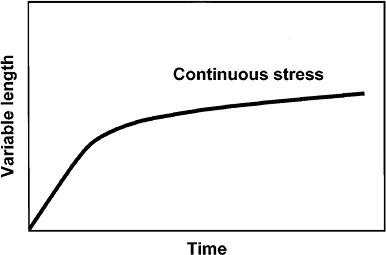
Figure 9-9. Tissue response to a single discrete force results in stress relaxation of the viscoelastic tissue over time.
|
 |
|
Figure 9-8.
Viscoelastic tissue response to a constant force resulting in gradual stretching of the tissue. However, the potential for inflammation is not demonstrated by this curve but is possible if the force is constantly present, which is the case in dynamic loading. |
applied to the elbow, which results in a discrete stress being imparted
to the tissue. However, since the splint position is not further
altered, the soft tissue is allowed to undergo a process called stress
relaxation that occurs over a period of time in response to the fixed
position (Fig. 9-9). It is felt that stress
relaxation lessens the likelihood of tissue irritation and of
inflammation. Thus the elbow is more amenable to this type of load
application and splint philosophy, since it is inflammation that breeds
additional swelling and scarring.
of a flexion or extension contracture that is amenable to stretch
deformation. Experimental data (6) and clinical experience suggest tissue is amenable to this type of therapy in three stages as follows (9):
I, onset to 3 months from injury, highly effective; II, 3 to 6 months,
moderately successful; III, 6 to 12 months, variably effective. A
stable articulation and articular surface is a prerequisite for splint
therapy to be effective in any of these stages.
not tolerate the constant forces from the splint. Excessive or
increasing swelling can also cause the development of neural symptoms
that require splint discontinuance or program alteration as follows:
sensory—alter the pressure points; motor—alter basic program or
discontinue.
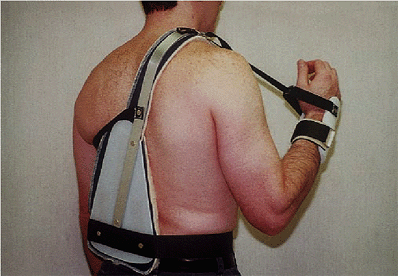
With traditional humeral-based support, the soft tissue tends to “bunch
up” in the brace in flexion, and this tendency limits further flexion.
The hyperflexion brace is stabilized at the shoulder, and the elbow is
flexed through a mechanism applied to the wrist with an adjustable
strap.
 |
|
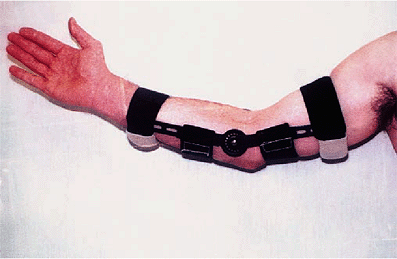
Figure 9-10. A static adjustable splint currently used by the author in which the force is directly applied to the axis of rotation.
|
 |
|
Figure 9-11. The same splint shown in Fig. 9-10 but reversed and being used in the flexion mode. Hence the splint is called the universal splint in our practice.
|
 |
|
Figure 9-12.
To avoid soft-tissue impingement associated with straps supporting braces about the elbow, a hyperflexion splint that frees the elbow of any encumbrance is based at the shoulder and flexion across the elbow by way of the wrist. |
the elbow flexion axis. The brace should have broad surfaces for force
application at the wrist and forearm, and the support at the brachium
should not cause soft-tissue constriction. The precise use is described
later in a format designed to be individualized and given to the
patient.
static adjustable splint may be modified, depending on individual needs
and progress.
-
General goals.
To attain improved motion of the elbow, inflammation must be avoided.
This is done with the use of the anti-inflammatory agents, heat and ice
and education of the patient to the signs of inflammation. -
Cardinal signs of inflammation.
Increased soreness, increased discomfort with use, swelling or,
commonly, a progressive loss of motion rather than improvement from day
to day. -
Treatment of inflammation.
Avoid the causative factor. Be less vigorous with static adjustable
splint, adhere to the heat/ice program, and take antiinflammatory
agents as prescribed. If it seems inadequate, the program may need to
be modified. Check with your doctor. -
Direction of improvement.
Often both increased elbow flexion and extension are being sought. In
general, the motion which is needed most is addressed at night as well
as during the day. The opposite motion is encouraged during the day. -
Typical splint program (20-hour program, 0 to 3 weeks from injury or surgery) (Fig. 9-13).
-
Morning. Upon
rising in the morning the splint is removed. Gently flex and extend the
elbow while taking a hot bath or shower for approximately 15 minutes.
Take antiinflammatory agent. -
Apply the splint in the opposite
direction as that which was used at night. Apply it to the point where
it is recognized that the elbow is being stressed but pain is not
extreme or intolerable. -
Noon. The
splint may be removed for 1 hour in the morning, 1 hour in the
afternoon, and 1 hour in the evening. Reapply the splint in the
opposite direction after these rest periods.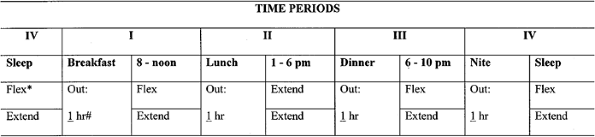 Figure 9-13.
Figure 9-13.
Flexion and extention visual splint (20 hours and 3 weeks). The hours
are changed for the Phase II/6 hour program. *Circle direction of
splinting: extension or flexion; write in duration out of splint. A
sample of the “20-hour” daily program given to the patient at the time
of splint prescription. A visual prescription of the splint usage
program is provided to those undergoing splint therapy. -
Evening. Use
the elbow when out of the splint as able during these periods and in
the evening. While out of the splint if the elbow is sore or seems
inflamed, apply ice for 15 minutes before bedtime. If not inflamed but
stiff, apply heat for 15 minutes, gently working the joint in flexion
and extension. -
Night. Before
going to bed at night apply the splint in the direction needed most.
Application should be sufficient to be aware that the elbow is being
stressed and a person should be able to sleep comfortably for about 6
hours without being awakened by elbow pain.
P.169 -
that disappears when the splint is removed, it is acceptable to
continue the program but to alter it to minimize nerve symptoms. If the
numbness does not resolve or motor symptoms develop, discontinue the
splint and call your doctor.
-
Sleep in direction needed most.
-
In the morning, do a 15-minute warm-up.
Take antiinflammatory; use extremity as tolerated for 2 hours. Then
apply splint in opposite direction to that used during sleep. -
At noon, remove the splint for 2 hours. Reapply same splint used at night.
-
At dinnertime, remove the splint for 2 hours. Reapply in the evening in opposite direction to that used at night.
-
At night, apply ice if sore and inflamed.
Apply heat if stiff. Remove splint 1 hour before bedtime, then apply it
in the direction in which motion is needed most. -
Reassess after 3 weeks. Alter the program further as needed.
approximately 360 braces for patients with various expressions of stiff
elbow. We estimate an overall success rate of the
splinting
program as about 80%. That is, the splint was considered a beneficial
adjunct. It is not a panacea. It is this experience that has resulted
in the program that is currently employed. These splints are now
commercially available (Prosthetic Laboratories of Rochester, Inc.; 201
1st Ave. S.W.; Rochester, MN 55902). This experience has also led to
the further development of effective splints by Air Cast and other
commercial vendors.
explaining the rationale of brace management and specifically
discussing the program based on the specific goals of treatment.
SW, Kumar A, Salter RB. The effect of continuous passive motion on the
clearance of a hemarthrosis from a synovial joint: an experimental
investigation in the rabbit. Clin Orthop 1983;176:305–311.
LJ, Lennon R, Adams R, et al. The technique and efficacy of axillary
catheter analgesia as an adjunct to distraction elbow arthroplasty: a
prospective study. J Shoulder Elbow Surg 1993;2:182–189.
RE, Russell PS. Studies on wound healing, with special reference to the
phenomenon of contracture in experimental wounds in rabbits’ skin. Ann Surg 1956;144:961–981.

