Tumors
is used to describe any abnormal mass, or neoplastic growth or erosion,
involving soft tissue or bone that may be present in the hand or wrist.
Thus, benign soft tissue growths such as ganglion cysts, giant cell
tumors of the tendon sheath, pyogenic granulomas, gouty deposits, and
aneurysms will be discussed, along with malignant lesions of soft
tissue such as melanoma, squamous cell carcinoma, and sarcomas of soft
tissue and bone.
broad definition that a tumor is any swelling, tumefaction, or erosive
lesion of skin, soft tissue, or bone. The tumors that will be discussed
are representative of many of the lesions that may be commonly
encountered. But this does not represent a comprehensive compilation.
benign, but the wise practitioner will always be aware of the need to
consider all possibilities. This chapter will be divided into benign
and malignant categories, including lesions of the skin, soft tissue,
and bone, as well as tumor-like conditions.
section on the basic principles of diagnosis, including imaging
techniques, tumor classification, biopsy, and staging of soft tissue
sarcomas.
-
Tumors that present with a history of
rapid enlargement, aching discomfort, or exceed 3 to 4 cm in size,
warrant a careful evaluation of the mass and overlying skin, and
require palpation for enlarged lymph nodes in the epitrochlear and
axillary regions. -
A plain radiograph is an appropriate
initial study to obtain. For suspicious soft tissue tumors, magnetic
resonance imaging (MRI) is advised with T1, T2, and short tau inversion
recovery (STIR).-
T1 images are useful for anatomic detail.
-
T2 images show fluid collections, such as purulent material and hematomas.
-
Gadolinium contrast may enhance the appearance of soft tissue tumors.
-
-
If a malignancy is diagnosed, the workup
should include a chest radiograph and total-body scintigraphy
(radioisotope scans) to rule in or out metastatic spread. -
Computed axial tomography (CT) of the
chest, abdomen, and pelvis is also utilized, along with routine
hematology, chemistry panel, and coagulation studies. -
A medical oncologist and radiation therapist may be used as indicated.
adopted by the Musculoskeletal Tumor Society is based on the location
(site) and extent of the lesion, and the histologic grade. The site of
the lesion can be either intracompartmental (T1) or extracompartmental
(T2). The extent of the tumor refers to the presence or absence of
metastatic lesions. The histologic grade may be benign (G0), low grade
(G1), or high grade (G2).
the institution where subsequent treatment will be given, as studies
have suggested that this increases the ultimate survival. Four
dissection methods have been employed for biopsy and are given in Table 3-2. All biopsies should be carefully planned, and open biopsies are preferred over needle biopsies.
-
The biopsy is performed under tourniquet control, and the limb is elevated but not exsanguinated with an Esmarch bandage prior to inflation of the tourniquet.
-
The resultant biopsy tract becomes a
contaminated tract of tumor cells, and will require removal en bloc if
the lesion is malignant. -
Thus, the biopsy incision should be
placed in such a way that it facilitates future surgery. In general,
longitudinal incisions are preferred over transverse incisions.P.38Table 3-1 Enneking System for Staging of Soft Tissue Sarcoma and Sarcoma of the BoneStage Grade Site Metastases IA G1 T1 M0 IB G1 T2 M0 IIA G2 T1 M0 IIB G2 T2 M0 IIIA G1–G2 T1–T2 M1 IIIB G1–G2 T1–T2 M1 Characteristics Grade (G) G1 Low G2 High Site (T) T1 Intracompartmental T2 Extracompartmental Metastases (M) M0 No regional or distant metastases M1 Regional or distant metastases present Taken
from Enneking WF, Spanier SS, Goodman MA. A system for the surgical
staging of musculoskeletal sarcoma. Clin Orthop Rel Res
1980;153:106–120. -
Frozen sections may be used to determine
that adequate tissue has been removed for study, or for determining
margins. However, permanent sections are required for definitive
treatment.
to introduce the reader to some current concepts regarding treatment
options.
especially to malignant tumors and those tumors that are benign but
behave aggressively, such as giant cell tumor of the bone.
|
Table 3-2 Musculoskeletal Tumor Dissection Method
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
-
The treatment options are not inclusive of all recommended treatments, and are intended as an introduction to the subject.
-
The treatment options may change as further experience and knowledge are applied to a given tumor.
-
A team approach is ideal, and may include
surgical specialists, pathologists, diagnostic and therapeutic
radiologists, and oncologists. -
In suspicious lesions, referral of the
patient to a team or center of experience for evaluation and treatment,
even before a biopsy is performed, may be considered.
-
Ganglion cysts are probably the most commonly encountered benign soft tissue tumor in the wrist and hand.
-
They occur most commonly over the dorsal
aspect of the wrist, the palmar and radial aspects of the wrist, the
flexor tendon sheath in the region of the A-1 pulley, and over the
distal interphalangeal (DIP) joint of the fingers and the
interphalangeal (IP) joint of the thumb. -
In the flexor tendon sheath, they are
termed volar retinacular ganglia. Over the DIP joint of the digits and
IP joint of the thumb, they are termed mucous cysts. -
Less common sites are about the PIP
joint, the carpal and ulnar canal, in the substance of extensor
tendons, from the extensor retinaculum, and in carpal bones.
-
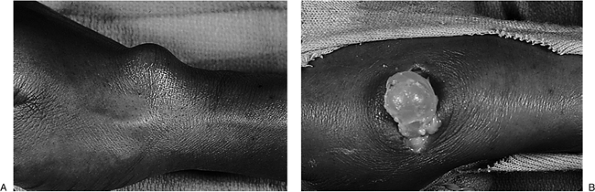
At the wrist, ganglion cysts may present as a firm, nontender mass that can be up to several centimeters in diameter (Figure 3-1). These cysts may transilluminate when a bright light source, such as a penlight, is pressed against them.
-
The size of the cyst may vary from time to time, and may be related to physical activities.
-
The lesions are fixed to the underlying structures, and do not move with flexion or extension of the wrist or digits.
-
At the wrist, the diagnosis may be confirmed by aspiration that yields a thick, jelly-like material that has no color.
-
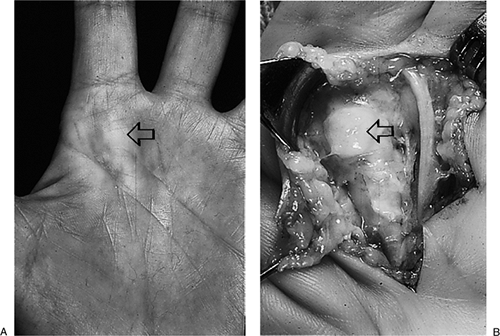
At the radial and palmar aspects of the
wrist, the ganglion cyst may lie beneath the radial artery and push it
up beneath the skin into a more prominent position. This displacement
of the radial artery must be remembered if the ganglion cyst is treated
by aspiration or excision (Figure 3-2). -
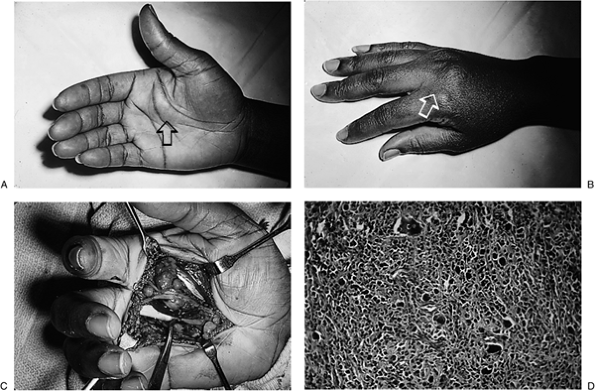
In the flexor sheath, they present as
firm masses in the palm at the level of the metacarpophalangeal joint,
and become more prominent with hyperextension of the fingers (Figure 3-3). -
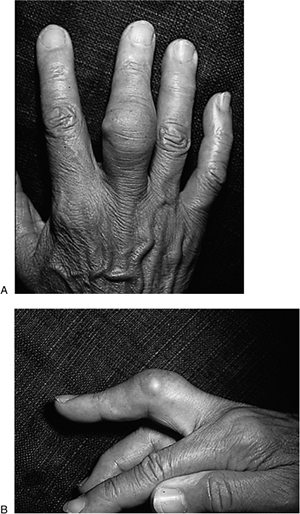
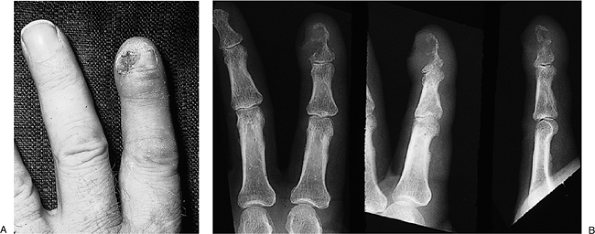
In the digits, they may be seen as thin
walled cysts that overlie the DIP and IP joints and may often be
associated with osteoarthritis (Figure 3-4 and Figure 3-5). -
Examples of a ganglion cyst in the carpal canal and in the substance of the extensor tendon, respectively, are seen in Figure 3-6 and Figure 3-7.
 |
|
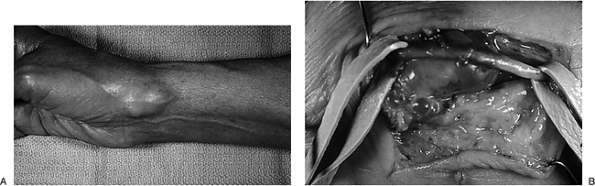
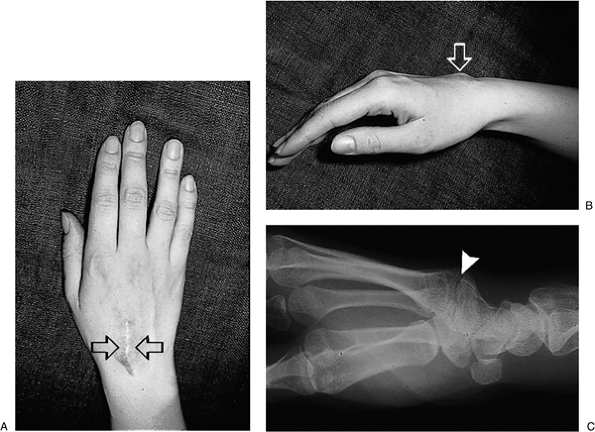
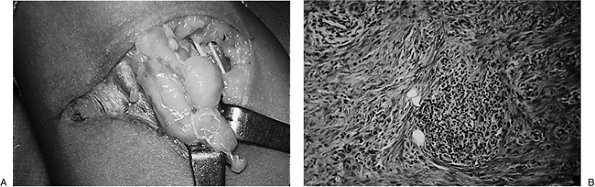
Figure 3-1 (A) View of the dorsal aspect of the right wrist, showing a large cystic mass. (B)
The mass had the characteristic appearance of a ganglion cyst and was removed, along with a suitable portion of the dorsal capsule. |
-
At the dorsal aspect of the wrist, the
ganglion should not be confused with a carpal boss, rheumatoid
synovitis, or an accessory muscle called the extensor digitorum brevis
manus (EDBM). -
The correct diagnosis is aided by noting
that a carpal boss occurs at the base of the middle finger metacarpal
and the adjacent capitate, is hard like bone, and is more distal than
the dorsal carpal ganglion that arises from the region of the
scapholunate capsule (Figure 3-8). For a complete discussion of a carpal boss, see the section on benign bone tumors. -
Rheumatoid synovitis is usually softer to
palpation than the ganglion, and moves distal and proximal as the
fingers are flexed and extended. It flattens out when a complete fist
is made and presents with a “tuck sign” when the fingers are extended (Figure 3-9).![]() Figure 3-2 (A) View of the radial and palmar aspect of the right wrist showing a prominent mass. (B)
Figure 3-2 (A) View of the radial and palmar aspect of the right wrist showing a prominent mass. (B)
The mass arose beneath the radial artery; rubber bands have been placed
about the artery proximal and distal, to retract the artery out of
harms way so that the ganglion may be excised. Remember that the radial
artery may be misidentified as a vein. It should be protected and
preserved. -
The EDBM is a fusiform-shaped mass that
occurs over the metacarpals, does not transilluminate, and maintains
its shape with finger flexion and extension (Figure 3-10). -
An intratendinous ganglion of an extensor
tendon may occur over the wrist and hand, and is diagnosed by the fact
that it moves with flexion and extension of the fingers and maintains
its shape. Rheumatoid synovitis, however, does not (see Figure 3-7 and Figure 3-9).
observation, aspiration (with or without an injection of cortisone),
multiple puncture technique, or surgical excision. While the specifics
of treatment are beyond the scope of this text, note that for surgical
intervention of the ganglion, current
conventional wisdom recommends excision of a small portion of the wrist capsule along with the cyst.
 |
|
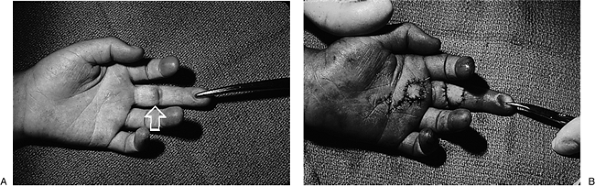
Figure 3-3 (A) Mass (arrow) at the base of the left index finger ray. (B) The volar retinacular ganglion cyst (arrow) is arising from the first annular pulley and will be excised along with a small portion of the pulley.
|
-
Excision of a recurrent or multilocular
cyst may be aided by careful injection of a dilute solution of
methylene blue into the cavity of the cyst using a 30-gauge needle.-
The dye provides for excellent contrast of the cyst from the surrounding structures, and aids in its complete removal (Figure 3-11).
-
-
The intratendinous ganglion can usually
be removed from the substance of the extensor by longitudinally
splitting its fibers and shelling out the cyst (see Figure 3-7). -
A word of caution is warranted when aspirating or removing a volar carpal ganglion:
-
The radial artery is in close proximity, and is often applied to the wall of the ganglion.
-
A preoperative assessment of the status
of the radial and ulnar arteries with an Allen’s test and/or Doppler
device will allow you to make appropriate decisions should the radial
artery be injured during the procedure.
-
-
These lesions have no malignant
potential, and may be observed. Cosmetic rather than functional
factors, or concerns about cancer, may play a significant role in the
patient’s decision to remove a large cyst from the wrist. -
In contrast, the volar retinacular cyst
may interfere with grip, and one or two punctures of the cyst often
result in its disappearance. -
Patients may try to needle a mucous cyst
at home, and should be cautioned against this. Because the lesion
connects to the joint, any resulting infection may be difficult to
treat.
-
The diagnosis is seldom in doubt, based
on the clinical appearance and microscopic demonstration of a fibrous
capsule. That structure is often lined with a flattened layer of
epithelial-like cells and contains a mucinous material that usually
stains a pale blue on hematoxylin and eosin sections.
-
Aside from the ganglion cyst, this is probably the most common benign soft tissue tumor encountered in the upper extremity.
-
Giant cell tumor may not be a suitable
term for this lesion, because it does not always contain giant cells
and is not always associated with the tendon sheath. This lesion has
also been called a fibrous tissue xanthoma. -
It is the most common tumor in the palm
and digits, and appears to have a propensity for the radial three
digits and the DIP joint region. -
It is usually on the palmar surface of the hand and fingers, but may occur dorsally.
-
These tumors are slow growing, firm, nodular, and nontender.P.41
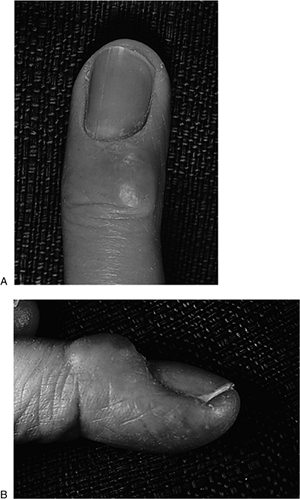
![]() Figure 3-4 Characteristic appearance of the ganglion cyst (mucous cyst) at the distal interphalangeal joint.
Figure 3-4 Characteristic appearance of the ganglion cyst (mucous cyst) at the distal interphalangeal joint. -
They are brown-yellow. In some instances,
portions of the lesion may lie just beneath the skin; a hint of this
color may show through in a thin-skinned patient. -
In contrast to the ganglion, they do not transilluminate.
-
They may occur as compound multinodular lesions.
-
Radiographs may demonstrate a soft tissue
mass. In some instances there may be erosion of the adjacent osseous
phalanx, or extension into the joint space.
-
Treatment is surgical through an appropriate incision.
-
Because of their slow growth, these
lesions may wrap around nerves and other vital structures, and care
must be exercised in their removal. Figure 3-12 shows the preoperative, intraoperative, and microscopic appearance of such a lesion. -
At surgery, the lesions are moderately easy to remove.
-
Failure to identify all satellite
extensions or discover an extension into the joint space, however, may
be associated with a higher than normal recurrence rate. The same
comments would apply if the tumor has invaded the flexor tendon sheath.
 |
|
Figure 3-5
Ganglion cyst arising from the PIP joint. Radiographs (not shown) demonstrated significant degenerative arthritis in this joint. |
-
The microscopic appearance often, but not
always, reveals collections of giant cells in a dense and cellular
fibrous tissue matrix. -
Hemosiderin collections are prominent, and may explain the coloration of these lesions (Figure 3-12D).
-
These cysts are found most commonly in
the distal phalanx, most often in males. They may be found following
amputation or injury of the fingertip.P.42![]() Figure 3-6
Figure 3-6
This large ganglion cyst arose from the volar aspect of the carpal
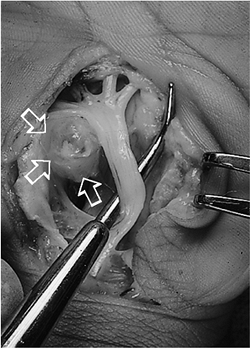
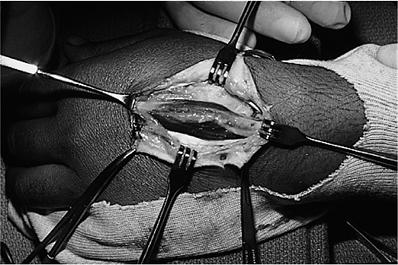
canal, and caused median nerve complaints. The ganglion is to the left (arrows) and the probe is deflecting the median nerve.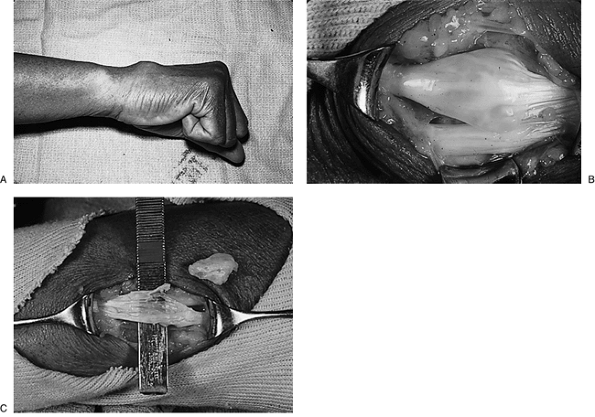 Figure 3-7 (A)
Figure 3-7 (A)
Ganglions may arise in the substance of extensor tendons, and present
as a mass that moves distally with flexion of the fingers. (B) The ganglion cyst is fusiform in shape. (C) It can be removed without loss of integrity of the extensor tendon. -
They are most commonly found on the
palmar surface of the digits, in contrast to sebaceous cysts (due to
obstructed sebaceous glands) that occur on the dorsal aspect of the
hand. Epidermal inclusion cysts are believed to result from the
traumatic implantation of epithelial cells into the underlying soft
tissue.
-
These slow-growing masses in the distal phalanx of the fingers or thumb are firm and slightly moveable.
-
They are thick-walled white lesions that contain a white, thick, “cheesy” material.
-
A history of trauma is not always present.
-
If the cyst has been present for a long
time, it may produce a pressure defect on the adjacent osseous phalanx
that is visible on radiograph. -
The typical appearance is shown in Figure 3-13.
-
Epidermal inclusion cysts are easily removed from the surrounding soft tissue.
-
They may often recur, and some surgeons
have claimed a lower recurrence rate by excising an ellipse of skin
over the cyst that may contain the site of the original traumatic
implantation.
 |
|
Figure 3-8 The carpal boss is often mistaken for a ganglion cyst. (A–B) Prominent mass and scar (arrows) following an attempted removal of a “ganglion.” (C) A radiograph clearly demonstrates the true nature of this mass.
|
 |
|
Figure 3-9
This patient with rheumatoid synovitis demonstrates the fact that synovial lesions “bunch-up” and become more prominent when the fingers are extended (A), and flatten out when a fist is made (B). |
 |
|
Figure 3-10
This anomalous muscle called the extensor digitorum brevis manus (EDBM) may also mimic the ganglion cyst; it is distal to the typical ganglion location, and is more fusiform in shape. |
-
They have a wall of fibrous tissue on microscopic section, and the white, “cheesy” material is keratin.
-
These lesions have no malignant potential.
-
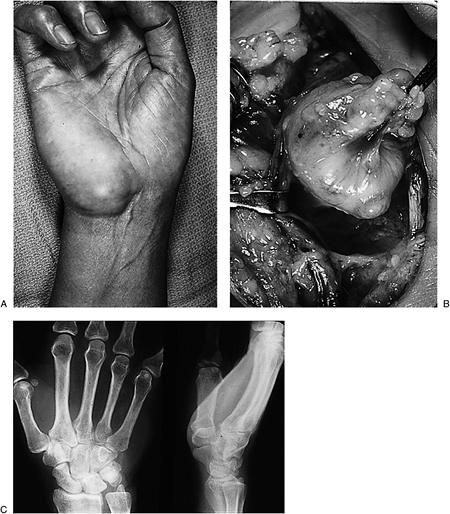
Although lipoma is the most common benign soft tissue tumor in the body, it is relatively uncommon in the wrist or hand.
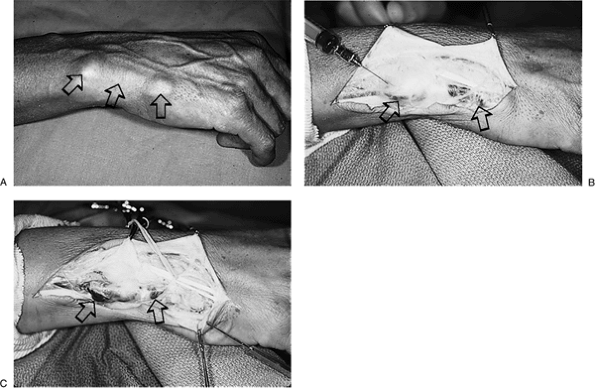 Figure 3-11 (A) This elongated compound ganglion cyst spanned a considerable distance across the wrist and hand (arrows). (B) An injection with a dilute solution of methylene blue demonstrated its true extent. (C) That made its complete removal easier.
Figure 3-11 (A) This elongated compound ganglion cyst spanned a considerable distance across the wrist and hand (arrows). (B) An injection with a dilute solution of methylene blue demonstrated its true extent. (C) That made its complete removal easier. -
It may occur in any location in the hand
and wrist, including Guyon’s canal or the carpal tunnel—where it may
produce nerve symptoms.
-
The typical lipoma is represented by a soft to firm nontender mass that does not transilluminate.
-
It may be firm if it has been growing for a long time in a confined anatomic space.
-
It may be diagnosed on radiograph by its comparatively diminished density (it appears darker) than the surrounding tissues.
-
This finding, called Bufalini’s sign, demonstrates the comparative diminished radio-density of fatty tissue.
-
-
Figure 3-14 demonstrates the preoperative, intraoperative, and x-ray appearance of a large lipoma in the hand.
-
Lipomas are well demarcated and easily removed, and recurrence is unusual.
-
Typical fat cells are seen on the histological sections, with minimal amounts of fibrous tissue.
-
There is no malignant potential.
-
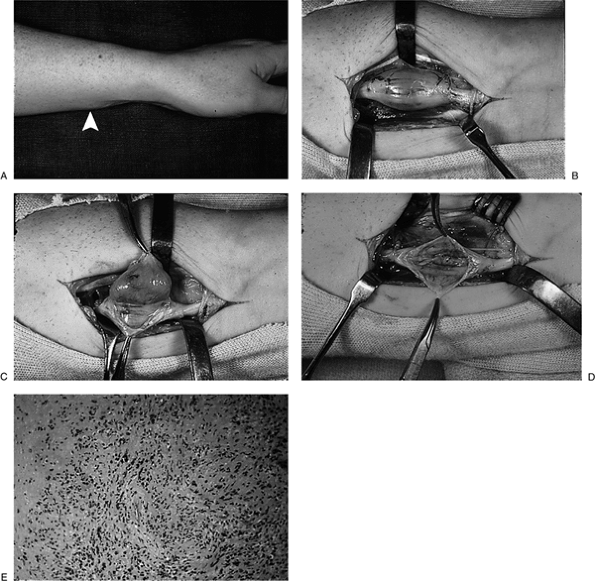
Neurilemmoma is the most common benign nerve tumor of the hand and wrist, and most often involves the median nerve at the wrist.
-
It is most often seen in the 4th to 6th decades.
 |
|
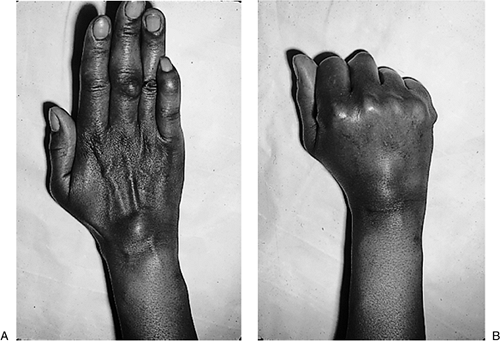
Figure 3-12 (A) This compound giant cell tumor of the tendon sheath presented as a palmar hand lesion (arrow). (B) It also presented as dorsally. (C) It was associated with several vital structures in the palm, and invaded the metacarpophalangeal joint of the middle finger. (D)
The characteristic histologic features of giant cells in a cellular matrix with scattered hemosiderin deposits are noted. (Hematoxylin and eosin, original magnification × 160.) |
-
Most often, patients present with a pain free mass on the flexor side of the wrist.
-
Percussion over the mass may produce some distal paresthesias.
-
The mass is mobile side-to-side, but not longitudinally. It does not transilluminate.
-
It is more medial in the wrist than the usual volar carpal ganglion.
-
This lesion is easily differentiated from
other nerve tumors by the fact that it may be removed from the nerve
involved by shelling it out of the nerve. -
The nerve fibers are separated longitudinally, and the mass is removed (Figure 3-15A-D).
-
It is surprising to note that little or no nerve deficit is present following its removal.
-
The histological appearance in Figure 3-15E is characteristic, and recurrence is uncommon.
-
Neurofibromas are benign nerve lesions that arise from nerve fasciculi.
-
They may be single or multiple, and are most common in neurofibromatosis (von Recklinghausen’s disease).
-
They may present as subcutaneous masses about the hand and wrist.
-
These lesions may be associated with café-au-lait spots seen in neurofibromatosis.
-
The typical appearance of this lesion in a patient with neurofibromatosis is shown in Figure 3-16.
-
In contrast to the neurilemmoma, these
lesions have a nerve that enters and exits the mass, and that cannot be
freed from the mass.P.46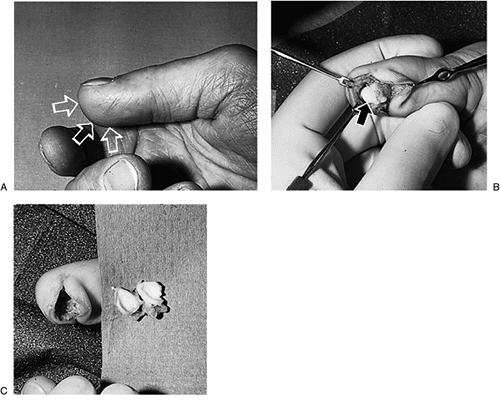 Figure 3-13 (A) The enlarged terminal phalanx (arrows) of this carpenters thumb revealed a thick-walled cyst. (B) It was filled with keratin material. (C) It was easily shelled out of the pulp of the terminal phalanx.
Figure 3-13 (A) The enlarged terminal phalanx (arrows) of this carpenters thumb revealed a thick-walled cyst. (B) It was filled with keratin material. (C) It was easily shelled out of the pulp of the terminal phalanx. -
If a small sensory nerve is involved, it
may be excised along with the lesion—and little or no residuals will be
encountered. Note the afferent and efferent nerve fibers from the
neurofibroma in Figure 3-16C. -
Progressively enlarging lesions that are symptomatic may require removal.
-
The characteristic histology is demonstrated in Figure 3-16D.
-
Malignant degeneration is possible in patients with neurofibromatosis.
-
This is a benign but very aggressive
lesion that occurs almost exclusively in the fingers and toes of
children before the age of one year. -
In the hand, it is most often seen in the region of the IP joint.
-
These lesions present as small raised masses that are nontender.
-
With growth, joint contracture and deformity may be seen.
-
The lesions may grow at an alarming rate, and may mimic a malignancy (Figure 3-17).
-
Treatment may include observation, limited and wide excision, and amputation.
-
Observation is indicated because spontaneous resolution may occur. Progressive deformity may require surgical intervention.
-
Wide excision and skin grafting may give the best local control but recurrence is high (Figure 3-18).
-
Intracytoplasmic inclusion bodies are present in the histologic section, which suggests a viral or myofibroblast origin.
-
This childhood and adolescent condition is a benign but aggressive lesion seen most often in the palm.
-
The lesion presents as a small, pain free mass that may be closely applied to the underlying vital structures in the palm.
 |
|
Figure 3-14 (A) This patient presented with a slow-growing, pain-free mass in the palm of her right hand. (B) It was a classic lipoma. (C) The diagnosis was made preoperatively, based on the radiolucent nature of the lesion on a radiograph (Bufalini’s sign).
|
-
Wide excision with sparing of the
associated vital structures is the treatment of choice. Use skin grafts
or flap coverage as needed.
-
The histologic appearance resembles fibrosarcoma; the recurrence rate may be 50% or more.
-
This condition is also known as
pseudosarcomatous fasciitis, subcutaneous pseudosarcomatous
fibromatosis, and infiltrative fasciitis. -
The lesion begins as a small nodule in the forearm or hand.
-
The lesion is characterized by a small but rapidly growing nodule that was only recently noted.
-
Figure 3-19 shows the intraoperative and histologic appearance of this lesion.
-
The natural history of this lesion appears to be self-limited, and even partially excised lesions do not reoccur.
-
The key to treatment of this lesion is to
differentiate it from a soft tissue sarcoma, and to avoid inappropriate
and aggressive treatment.
 |
|
Figure 3-15 (A) This patient presented with a slightly tender mass (arrow) on the palmar side of her left forearm. (B) It was found to be a large tumor involving the substance of the median nerve. (C) The lesion was “shelled-out” under loupe magnification. (D) No residual nerve deficits were noted following excision of this schwannoma. (E)
Microscopic view of the schwannoma. Note the dense and irregular cellular pattern. (Hematoxylin and eosin, original magnification × 160.) |
-
Its histologic appearance may resemble that of a fibrosarcoma and myxoid liposarcoma.
-
These lesions most often involve the contact surface of the digits.
-
These lesions present as dark red,
raised, and small spherical masses that are often associated with a
history of injury to the site of presentation. -
They may appear to be sessile, but are usually pedunculated and bleed easily.
-
Figure 3-20 shows two examples of pyogenic granuloma.
-
In most cases, the condition is cured by
severing the stalk or pedicle flush with the skin, followed by applying
silver nitrate to the base of the pedicle on the digit. -
Some have suggested that a small ellipse of skin be excised with the lesion, but this may not be necessary.
-
This condition represents “run-away”
angiogenesis, and has no malignant potential. The histologic sections
reveal a collection of blood vessels.
 |
|
Figure 3-16 (A) This woman, age 24, presented with a small subcutaneous mass in the hypothenar eminence of the left hand (arrow), which was associated with a café-au-lait spot on the dorsum of the opposite hand (arrow). (B–C)
The lesion was a neurofibroma that arose from a small sensory fiber, and complete removal was possible without significant deficit. (D) Histologic appearance of the neurofibroma, demonstrating a moderately cellular matrix. (Hematoxylin and eosin, original magnification × 400.) |
-
This is a relatively uncommon lesion that occurs in the distal phalanx and often under the fingernail.
-
It represents a neoplastic proliferation
of the smooth muscle cells of the normally occurring glomus, which is a
temperature regulating shunt.
-
The patient with this tumor presents a
classic history of pain that is often severe, cold sensitivity, and
tenderness over the distal phalanx. -
Physical findings may include
discoloration (reddish-blue) beneath the fingernail, if the lesion is
subungual; ridging or deformity of the nail plate; and point tenderness. -
Radiographs may reveal a bony defect in the osseous phalanx because of pressure from the glomus tumor.
-
Although often subungual, any painful and
tender subcutaneous area in the digit with the above noted history
should be considered to be a glomus tumor. -
Figure 3-21
demonstrates a patient with a longstanding glomus that was being
treated as an infection (note the changes in the finger nail), and the
intraoperative appearance of the lesion. Figure 3-21C shows the intraoperative appearance of another glomus tumor, which is smaller.
-
Excision of the lesion is the treatment
of choice. It is performed through a window in the nail, or by
elevating the nail proximally to expose the lesion. -
Many of the lesions are in the soft
tissues proximal to the nail plate, and may be removed through an
incision in this region without disturbing the nail plate (see Figure 3-21C).
 |
|
Figure 3-17
A clinical example of digital fibroma of infancy. This lesion enlarged rapidly in this infant of 1 year of age. Note the enlarged little finger and the alarming appearance of the lesion. |
-
Histologic findings include endothelial pericyte and nonmyelinated nerve fibers.
-
The majority of these tumors are seen within the first 4 weeks of life.
-
Females are affected three times as frequently as males.
-
Rapid growth may be noted in the first year of life, followed by slower growth thereafter.
-
The final stage is represented by involution; by age 7, 70% of the lesions have involuted.
-
Noninvoluting lesions are capillary or cavernous.
![]() Figure 3-18 Another example of digital fibroma of infancy (proximal phalanx of the middle finger) in another slightly-older child (A) who was treated with an excision and skin graft (B).
Figure 3-18 Another example of digital fibroma of infancy (proximal phalanx of the middle finger) in another slightly-older child (A) who was treated with an excision and skin graft (B).-
The capillary hemangiomas are represented by the port-wine stain.
-
The cavernous hemangiomas are represented by arteriovenous connections that may be either low or high flow in nature.
-
-
The capillary hemangioma is represented by a minimally raised port-wine stain lesion of variable size.
-
It presents as a bluish, raised subcutaneous mass that is nontender, soft, and often multiloculated.
-
An MRI offers the diagnostic advantage of
being noninvasive, and may delineate the proximity of neural
structures. It is especially useful in visualizing skeletal muscle
hemangiomas. -
Radiographs of cavernous hemangiomas may show phleboliths (calcific deposits in a vein wall or thrombus).
-
The preoperative and intraoperative appearance of a cavernous hemangioma is seen in Figure 3-22.
-
Management of hemangiomas is usually conservative, since most will involute by 7 years of age.
-
Surgical management may be indicated in
noninvoluting lesions if the diagnosis is in question, or if
ulceration, bleeding, or recurrent infection is a problem. -
Surgery involves ligation of feeder vessels and complete excision of the lesion.
-
Cryosurgery and YAG laser treatment has been used.
-
This is a fast-growing skin tumor that mimics the appearance of squamous cell carcinoma.
-
It most often occurs on the hair-bearing dorsal skin of the forearm, wrist, and hand.
-
In 1 to 2 months, it may grow from a small papule to a raised lesion that is 2 to 3 cm in diameter.
 |
|
Figure 3-19 (A) Intraoperative appearance of this example of nodular fasciitis in the forearm. (B)
Histologic appearance of this benign lesion. Note the cellular “nodule” in the lower right. (Hematoxylin and eosin, original magnification × 160.) |
-
The history of rapid growth, and its size
and alarming appearance, may make it difficult to distinguish it from
squamous cell carcinoma. -
However, the central keratin plug in this
lesion is in contrast to the small area of central necrosis seen in
squamous cell carcinoma. -
Their rapid growth is in marked contrast to the slower growth of squamous cell carcinoma.
-
Figure 3-23A demonstrates the clinical appearance of the lesion.
-
Although the natural history of this
lesion is spontaneous regression after a latent phase of variable
duration, the lesion should be excised for an accurate diagnosis. -
The resultant defect may be closed by
skin grafts as needed, and the resultant scar will, more often than
not, be less noticeable than the original lesion.![]() Figure 3-20 Two examples of pyogenic granuloma, both of which were excised without recurrence.
Figure 3-20 Two examples of pyogenic granuloma, both of which were excised without recurrence. -
Figure 3-23B demonstrates the postoperative appearance of this lesion following excision and split-thickness skin grafting.
-
The entire tumor must be evaluated. A
pathologist experienced in skin tumors is useful in distinguishing this
lesion from squamous cell carcinoma. -
Figure 3-23C shows the histologic appearance of the lesion at × 35 magnification.
-
Although not a neoplasm, an aneurysm may be appropriately included in a discussion of tumors of the hand
P.52P.53and wrist since it must be differentiated from a true neoplasm.
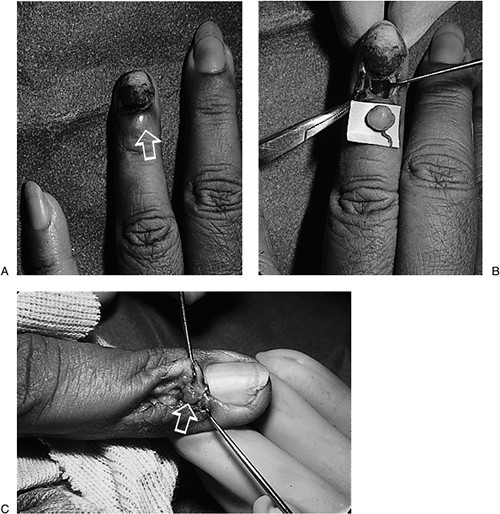 Figure 3-21 (A) A soft tissue mass (arrow) proximal to the fingernail, with deformity of the fingernail. (B) Surgery revealed a classic glomus tumor. (C) Another example (arrow) of a glomus tumor.
Figure 3-21 (A) A soft tissue mass (arrow) proximal to the fingernail, with deformity of the fingernail. (B) Surgery revealed a classic glomus tumor. (C) Another example (arrow) of a glomus tumor.![]() Figure 3-22 (A) This patient presented with a long-standing history of a soft and pain-free mass over the index finger. (B) At surgery, the grape-like clusters of a cavernous hemangioma were noted and excised.
Figure 3-22 (A) This patient presented with a long-standing history of a soft and pain-free mass over the index finger. (B) At surgery, the grape-like clusters of a cavernous hemangioma were noted and excised.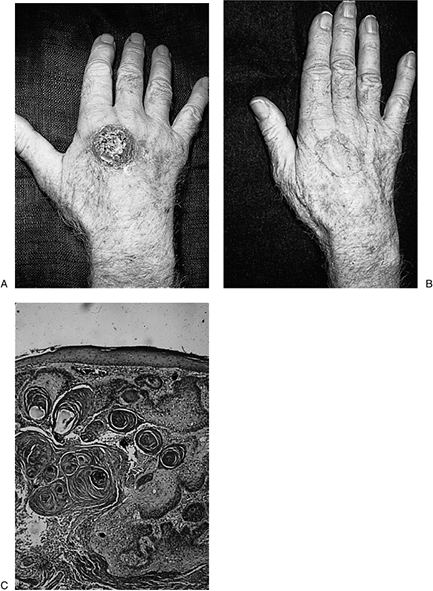 Figure 3-23 (A) This elderly man presented with this ominous-looking lesion that he said began as a small bump only 6 weeks before. (B)
Figure 3-23 (A) This elderly man presented with this ominous-looking lesion that he said began as a small bump only 6 weeks before. (B)
The rapid growth of this lesion indicated the probability that the
lesion was a keratoacanthoma, and excision followed by skin graft was
performed. (C) Note the histologic appearance of the keratoacanthoma. (Hematoxylin and eosin, original magnification × 35.) -
Aneurysms may be false or true.
-
False
aneurysms result from a penetration of the blood vessel wall, with
subsequent hemorrhage and hematoma formation that organizes to form a
lumen in continuity with the injured vessel. This often global-shaped
lesion does not have a true vascular endothelial lining. -
A true
aneurysm results from an injury to the vessel wall that permits gradual
expansion or dilatation of the vessel wall, and has a true vascular
epithelial lining.
-
-
True
aneurysms occur most frequently in areas subjected to repetitive
trauma, such as the ulnar artery and the superficial arch in the palm.
Mechanics, bakers, or others that use their hypothenar eminence as a
tool for forceful pounding or pushing may experience such injuries. -
False
aneurysms are most often seen after penetrating injuries, and are most
common at the palmar side of the wrist. They may occur in the radial
artery in the anatomical snuffbox, the palmar arch, and the digits.
Aneurysms of the ulnar and digital vessels are evenly distributed
between the false and true types.
-
Large aneurysms may present as visible and palpable masses at the wrist, or in the palm of the hand.P.54
![]() Figure 3-24 (A)
Figure 3-24 (A)
This baker noted a slowly growing mass on the ulnar aspect of his right
hand for several months. It was believed that repetitive impact over
the hypothenar eminence may have been associated with the lesion. (B) Occlusion of the radial and ulnar arteries at the wrist diminished the size of the mass. (C)
At surgery, an aneurysm of the ulnar artery was identified and excised,
and the resultant arterial defect was bridged by a vein graft. -
True aneurysms are usually fusiform-shaped, whereas false aneurysms are global- or spherical-shaped.
-
Neurologic deficits may occur due to pressure on adjacent nerves.
-
Large aneurysms may have a bruit that is audible with a stethoscope.
-
Doppler ultrasonography and arteriography are useful diagnostic aids.
-
Arteriography aids in preoperative
planning and defines the nature of collateral blood flow and thus may
aid in the method of treatment. -
Figure 3-24 demonstrates a true aneurysm of the ulnar artery in a 34-year-old baker.
-
Gouty tophi, although not true neoplasms,
may occur throughout the hand and wrist, and may be associated with
joint and tendon dysfunction.
-
Gouty deposits may be small or large, and may often erode through the skin over the extensor surfaces of the hand.
-
They are chalky white collections of a toothpaste-like material that is unmistakable in appearance.
-
Figure 3-25 shows the clinical, x-ray, and intraoperative appearance of gout in the left hand.
-
Treatment is directed at the medical control of the gout.
-
Surgical intervention is directed at removal of large deposits that may compromise joint and/or tendon function.
-
These lesions are located on the dorsum of the hand and wrist in the areas of sun exposure.
-
They ultimately present as raised erosions, with an occasional “pearly” border.P.55
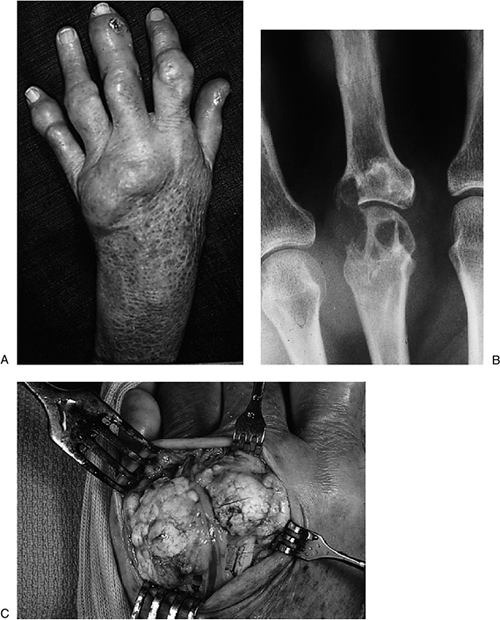 Figure 3-25 (A)
Figure 3-25 (A)
This patient with a longstanding history of gout presented with gouty
tophi and skin erosion over the middle finger distal interphalangeal
joint. (B) Radiographs revealed bone erosions at the metacarpophalangeal joint. (C) Clinical appearance of the tophi at the time of excision. -
They are slow growing but may invade deeper tissues over time.
-
There are many variations in the
appearance of this tumor, and they may present as areas of skin
atrophy, pink discoloration, or telangiectatic changes. They also may
have a scar-like quality to their advancing edges.
-
Surgery is by excision of the lesion with
a sufficient margin, followed by immediate histologic confirmation of
the adequacy of excision. -
Closure may be by direct means in small lesions, or by skin grafts or flaps in larger cases.
-
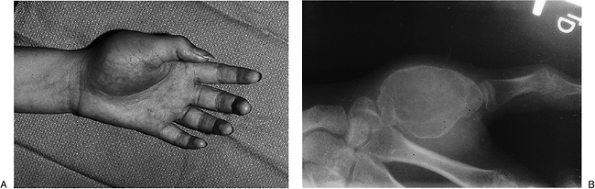
These lesions are the most common malignant tumor in the hand.
-
They have the capacity to expand locally and to metastasize via the lymphatic or blood vessels.
-
They may vary from wart-like,
slow-growing lesions under or near the fingernail, to large, ulcerated,
or exophytic growths most commonly over the dorsum of the finger and
hand.
 |
|
Figure 3-26 (A) This patient was being treated for a chronic infection about his left index finger. (B)
X-rays demonstrated an erosion of the osseous phalanx, and surgery confirmed the presence of squamous cell carcinoma of the nail bed. |
-
Treatment will vary depending on the location, size, and extent of the lesion, and presence or absence of metastatic lesions.
-
In those lesions confined to the terminal phalanx, amputation at, or proximal to, the DIP joint may be an effective treatment.
-
The incidence of these dangerous and
insidious tumors continues to increase, and a significant percentage of
these lesions involve the upper extremity. -
They represent 5% of skin cancers, but are responsible for 75% of deaths from skin cancer.
-
Sun exposure is considered to be the major cause for this increase.
-
Four major types have been described.
-
Melanomas are cancers of the melanocytes.
-
Half arise from atypical moles; the other half arise de novo.
-
This is the most common type in Caucasians, and represents 70% of all melanomas.
-
It is most likely to arise from, or adjacent to, a pre-existing nevus.
-
It begins as a pigmented plaque, and has a radial growth phase of months to years before vertical growth begins.
-
Metastatic spread is associated with the vertical growth phase.
-
This type represents 15% of all melanomas, and has little or no radial growth phase. It may metastasize early.
-
It grows rapidly, and usually arises de novo.
-
It is usually dark blue-black in color, but may be gray or pink. If it is, it is called an amelanotic melanoma.
-
This type represents 2% to 8% of all melanomas, and is found on palmar surfaces and the fingernail.
-
It does not appear to be associated with sun exposure, and is seen in all ethnic groups.
-
In those groups where melanoma is uncommon (African American and Hispanics), it is the most common variant found.
-
A slow-growing radial growth phase occurs
before vertical growth. Because of its location, it is an area not
routinely examined—so the diagnosis may be delayed. -
The subungual melanoma is in this category, and usually affects the matrix of the thumbnail or great toenail.
-
Acral lentiginous melanomas must be
differentiated from subungual hematomas. A subungual hematoma is
usually associated with a history of injury, and may progress distally
as nail growth occurs.
-
This type represents 4% to 10% of all melanomas, and is a type of de novo growth that is associated with long-term sun exposure.
-
It is sometimes associated with actinic keratoses, and is most common on the dorsal surface of the forearm.P.57Table 3-3 Breslow System for Staging Malignant Melanoma
Depth of Lesion (mm) 5-Year Survival Rate (%) <0.76 89 0.76–1.49 75 1.5–2.49 58 2.5–3.99 46 >3.99 25 -
It begins as a tan, flat lesion that may have a radial growth phase of 1 to 2 decades.
-
The depth of invasion of the malignant melanoma determines the recommended treatment.
-
Melanoma in situ that has not gone beyond the basement membrane is excised with a 0.5 to 1.0 cm margin.
-
Tumors less than 1.0 mm deep should be
excised with a 1 cm margin. In the subungual location, this means
amputation at, or just proximal to, the DIP joint. -
Melanomas 1 to 4 mm in depth should be
excised with a 2 cm margin, and the proximal lymph nodes should be
evaluated with scintigraphy and biopsy as indicated. If a lymph node is
positive, consideration may be given to a chemotherapy protocol. That
is beyond the scope of this chapter. -
Melanomas greater than 4 mm in depth have a very high incidence of lymph node involvement.
-
Excision with a 3 cm margin is advised, and clinically involved nodes should be resected.
-
Chemotherapy may be considered based upon the patient’s general medical condition.
-
-
Soft tissue sarcomas are relatively uncommon in the hand.
-
Most soft tissue sarcomas present as a painless mass that has been present for a long time but has recently grown.
-
An epithelioid sarcoma is a notable exception, and may present as an ulcerated nodule that has been treated as an infection.
-
In general, soft tissue sarcomas may be misdiagnosed as infection, ganglion, or lipoma.
-
In addition to assessment of size, location, depth, and mobility, the lymph nodes should be evaluated.
-
Plain radiographs may demonstrate regional calcification and bone involvement.
-
An MRI is useful for determining abnormal
anatomy and the extent of disease. It also may lead to a suitable
preoperative diagnosis and aid in pre-operative planning. -
Although very small lesions may be
excised with a surrounding cuff of tissue, larger lesions may be
evaluated with an incisional biopsy. -
The biopsy incision must be planned to
meet the needs of more extensive treatment later on, and transverse,
oblique, or similar incisions should be avoided. -
It should be considered that biopsies will contaminate all adjacent tissue planes.
-
After the diagnosis of a sarcoma has been
established, systemic staging should be performed with CT of the chest
and axilla, as upper extremity sarcomas commonly spear to the lungs and
regional lymph nodes. -
Staging is based on grade, size, and the presence or absence of metastatic lesions, as well as the histologic grade.
-
A useful guide is the system developed by Enneking and adopted by the Musculoskeletal Tumor Society (see Table 3-1).
study, and changes to current recommendations and new modalities may
emerge as new or modified treatment protocols are developed and
evaluated. Surgery is the primary form of local treatment for soft
tissue sarcoma. It is planned as two distinct parts, and consists of
resection and reconstruction.
-
Excision is the initial form of
treatment. Primary consideration is for an appropriate resection, while
secondary consideration is for reconstruction. -
The goal of surgery is to achieve complete resection of the tumor, with a surrounding cuff (2 to 3 cm) of normal tissue.
-
If these margins cannot be achieved, then amputation should be considered.
-
Following wide excision of a large,
high-grade lesion, external radiation or radiation implants
(brachytherapy) therapy may be performed. -
The role of chemotherapy in the preoperative or postoperative period is still under investigation.
-
Patients with metastases may be treated by chemotherapy and/or resection of lung lesions.
-
This tumor is said to be the most common soft tissue sarcoma of the hand.
-
This tumor presents as a slow-growing,
benign-looking, firm nodule that may occur in the digits, palm, or
volar forearm in a young adult. -
The nodule may ulcerate. It tends to
spread proximally along the course of tendons, lymphatics, and fascial
planes, and does not respect fascial boundaries. -
It is often misdiagnosed, and has a propensity for recurrence and regional lymph node involvement.
-
This lesion must be treated aggressively, with a wide excision, radical resection, or amputation.
-
Lymph node biopsy is indicated even without clinical evidence of involvement.
-
Marginal excision is not advised.
-
Radiation may be considered after wide
excision of large lesions; chemotherapy may be considered in those
patients with lymph node involvement, recurrence, or metastatic lesions.
-
Histologic features include formation of discrete nodules of epithelial cells with areas of central necrosis.
-
Synovial cell sarcoma is one of the more common sarcomas in the hand and wrist.
-
They typically occur over the wrist, are seldom seen in the finger, and occur in the 15 to 40 age group.
-
They typically arise around joints, tendons, and bursae.
-
These tumors often present as slow growing, painless, and firm masses that may have been present for several years.
-
Soft tissue calcification may be seen on plain radiographs.
-
Surgery is the initial form of treatment.
Primary consideration is for an appropriate resection. Reconstruction
is a secondary consideration. -
The goal of surgery is to achieve complete resection of the tumor, with a surrounding cuff (2 to 3 cm) of normal tissue.
-
If these margins cannot be achieved, amputation should be considered.
-
Small size may not be associated with a more favorable prognosis.
-
Histologic sections reveal two cell types: epithelial cells and spindle cells.
-
These bone lesions are the most common primary bone tumors of the hand, and 35% of all enchondromas arise in the hand.
-
The proximal phalanx is the most common site of occurrence, followed by the metacarpal and middle phalanx.
-
Most lesions occur in patients 10 to 40 years of age.
-
The usual presentation is with a painless swelling over a phalanx or metacarpal.
-
Pain and deformity may be the presenting complaint due to a pathologic fracture through the enchondroma.
-
Pathological fractures in the hand are most often associated with enchondroma.
-
X-rays reveal a well-defined lytic lesion, with calcification of the matrix in some cases.
-
The vast majority of cases may be diagnosed without CTs or MRIs.
-
X-ray appearance, intraoperative findings, and histologic appearance are depicted in Figure 3-27.
-
Small lesions that are incidental findings on a radiograph may be treated by observation.
-
Larger lesions, or those associated with fractures, may be treated by curettage and bone grafting.
-
In patients with a pathologic fracture,
it is best to reduce the fracture as needed and allow the fracture to
heal before curettage and bone grafting. -
The osseous phalanx is often thin at the
site of the lesion, and attempts at open reduction, fixation, and bone
grafting may be difficult because of the lack of sufficient bone for
anatomic reduction and fixation. -
Shortening or deformity may be the end result.
-
After healing of the fracture, however, good bone stock is present, and definitive curettage and bone grafting may be achieved.
-
Histologic sections reveal a characteristic cartilage matrix with scattered lacunae that contain cartilage cells.
-
Multiple enchondromatosis is an uncommon
and nonhereditary disorder manifested by multiple enchondromas in the
metaphysis and diaphysis of the long bones and of the short, tubular
bones of the hands and feet.-
These benign lesions may become malignant
chondrosarcoma or osteosarcoma in 30% of the patients, so careful
monitoring is indicated.
-
-
Maffucci’s syndrome is a rare condition,
and its x-ray findings are similar to Ollier’s disease. However,
patients may also have multiple hemangiomas.-
These patients may also develop sarcomas of the bone and of the soft tissue.
-
-
This lesion accounts for about 5% of all benign bone tumors, but only 3% to 5% of these lesions occur in the hand.P.59
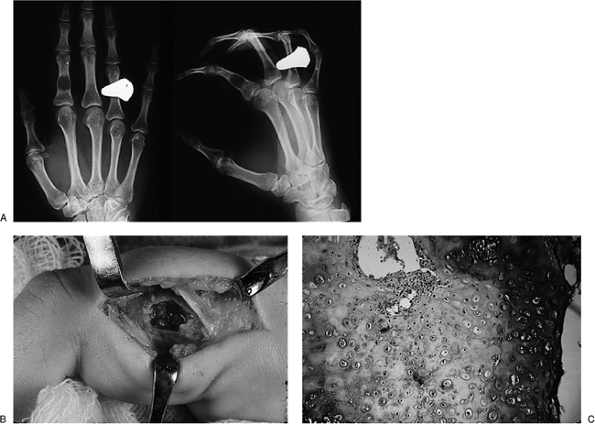 Figure 3-27 (A) This patient’s hand radiograph revealed an incidental finding of a lytic lesion of the proximal phalanx of the index finger. (B) Biopsy, followed by curettage, revealed an enchondroma. (C) The histologic appearance of an enchondroma. (Cartilage stain, original magnification × 160.)
Figure 3-27 (A) This patient’s hand radiograph revealed an incidental finding of a lytic lesion of the proximal phalanx of the index finger. (B) Biopsy, followed by curettage, revealed an enchondroma. (C) The histologic appearance of an enchondroma. (Cartilage stain, original magnification × 160.) -
Hand lesions are most common in the second decade, and metacarpal involvement is more common than involvement of the phalanx.
-
These lesions often present as a rapidly enlarging, alarming-appearing mass.
-
Radiographs demonstrate an expanding lesion on the bone metaphysis/diaphysis, with thinning of the cortex.
-
An MRI may suggest a fluid-filled lesion.
-
Soft tissue extension is uncommon, and metastasis has not been reported.
-
This lesion is demonstrated in Figure 3-28.
-
A biopsy and limited curettage was
performed shortly after this depiction, and the lesion gradually
diminished in size over the next several months.
-
An incisional biopsy is performed followed by curettage, cryosurgery, and bone grafting, if sufficient bone stock is available.
-
If bone stock is not available, wide
excision and reconstruction may be indicated. Cryosurgery may be
associated with damage to the physis and subsequent growth arrest.
-
This lesion accounts for about 5% of all benign bone tumors, but only 2% of these lesions occur in the hand.
-
This tumor occurs most commonly in the
4th decade and may involve the distal radius, the metacarpals and
phalanges, and, rarely, the carpal bones.
-
The usual clinical presentation is with pain and swelling in the affected region.
-
Radiographs demonstrate a lytic lesion with no matrix and indistinct borders.
-
Cortical expansion, destruction, and soft tissue extension are common.
 |
|
Figure 3-28 (A) This otherwise healthy teenager presented with a rapidly enlarging mass in her left thumb. (B)
X-ray examination revealed an expanding osteolytic lesion of the thumb metacarpal. Biopsy revealed an aneurysmal bone cyst, and curettage resulted in involution of the lesion. |
-
Giant cell tumors of bone, although
considered to be benign bone lesions based on their histology, behave
aggressively, may metastasize, and may ultimately result in death. -
Lesions in the hand have a higher risk of
local recurrence. These lesions should be approached as malignant
lesions, and should be staged following an incisional biopsy with chest
radiographs and a bone scan.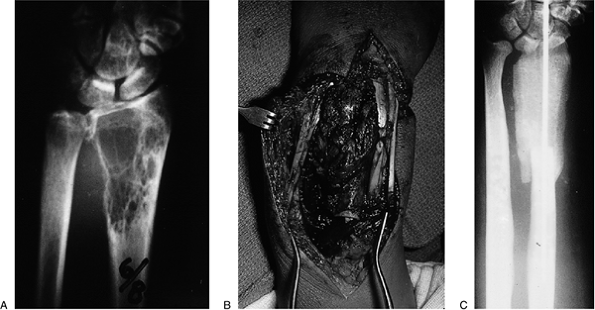 Figure 3-29 (A) This giant cell tumor of bone had been initially treated by curettage, followed by recurrence as noted here. (B) Wide excision of soft tissue and bone was performed. (C) The resultant defect was treated with a large iliac crest bone graft and wrist fusion.
Figure 3-29 (A) This giant cell tumor of bone had been initially treated by curettage, followed by recurrence as noted here. (B) Wide excision of soft tissue and bone was performed. (C) The resultant defect was treated with a large iliac crest bone graft and wrist fusion. -
Lesions in the metacarpals or phalanges
that have penetrated the cortex may be treated with wide excision and
reconstruction, or amputation. -
Distal radius lesions confined within the
cortex may be treated with curettage, burring, cryosurgery, and
cementation if sufficient bone stock is available. -
Those lesions that have pathologic
fracture or cortical perforation are treated by wide excision of the
distal radius, and reconstruction. Figure 3-29 depicts such a lesion that was treated by wide soft-tissue and bone
P.61resection, followed by an immediate bone graft from the iliac crest, and wrist fusion.
-
About 5% to 15% of these benign bone lesions appear in the hand and wrist.
-
This lesion is most often seen in the carpal bones or proximal phalanx. It mostly presents in the 2nd or 3rd decade.
-
Patients with this lesion often present
with a history of a dull ache in the affected region, which is often
relieved by nonsteroidal anti-inflammatory medication. -
Swelling and tenderness is usually
present. Radiographs may demonstrate reactive and sclerotic bone, with
or without a small nidus surrounded by a radiolucent area. -
A CT scan may further delineate the lesion.
-
Lesions in the distal phalanx may result in swelling in the pulp and nail deformity.
-
The clinical and preoperative x-ray appearance, as well as the intraoperative radiograph, are depicted in Figure 3-30A-C.
-
Surgery in the form of excision of the nidus often results in a cure.
-
Some have argued that treatment may be
nonsurgical, since nonsteroidal anti-inflammatory medication may
relieve the pain. Also, the natural history of this reactive and benign
bone lesion is one of gradual involution over a several-year period.
-
The histologic appearance of the dense bone is illustrated in Figure 3-30D.
-
Although not a true neoplasm, this bony
prominence is often misdiagnosed as a ganglion cyst or other tumor over
the dorsal aspect of the wrist. -
It is an osteophytic lesion that develops
at the base of the index and middle finger metacarpals and the adjacent
carpal capitate. -
Carpal boss is most common in women, and usually presents in the 3rd and 4th decades.
-
The lesion is bony, hard, nonmobile, and sometimes-tender mass that is most noticeable when the wrist is flexed.
-
Radiographs profiling the mass (30 to 40
degrees of supination and 20 to 30 degrees of ulnar deviation) reveal a
prominent, raised triangular bony mass that arises from the opposing
dorsal aspect of the metacarpal and capitate. -
An irregular and narrow
pseudo-articulation is noted between the two opposing halves of the
mass. The abutment of the two opposing surfaces may be likened to an
osteoarthritic joint, and may explain some of the symptoms of
tenderness and discomfort. -
A small, thin-walled, bursa-like sac may develop over the boss, and may be confused with a ganglion cyst.
-
This lesion is depicted in Figure 3-8.
-
In patients with significant symptoms, the two sides of the boss are removed down to normal articular cartilage.
-
Care is taken to avoid detachment of the
extensor carpi radialis brevis (ECRB) tendon insertion on the base of
the middle finger metacarpal.
-
This is the most common malignant bone tumor in children and adolescents, but is rarely seen in the hand.
-
When it does appear in the hand, it is usually in patients in the 4th to 6th decades.
-
It is most often found in the proximal phalanges and metacarpals, and rarely in the carpus.
-
The usual presentation is that of a rapidly enlarging mass that is firm and painful.
-
Radiographs may reveal an expanding
sclerotic tumor with new bone formation or a lytic lesion and an
associated soft tissue mass.
-
Incisional biopsy should be performed with the anticipated need for limb salvage and amputation.
-
In the finger, wide excision or ray amputation may be entertained along with neoadjuvant chemotherapy.
-
This lesion is the most common primary malignant bone tumor that occurs in the hand.
-
The lesion occurs mainly in the proximal phalanges and metacarpals in patients over the age of 60 years.
-
The lesion often presents as a firm, slow-growing, and sometimes painful mass.
-
Radiographs show a lesion with poorly defined borders and with areas of lysis and stippled calcification.
-
Cortical breakthrough and extension into the soft tissues helps to distinguish it from enchondroma.
-
Chondrosarcomas are slow growing.
-
Metastasis of about 10% may be seen after local recurrence following intralesional treatment.
 |
|
Figure 3-30 (A)
This patient noted pain and progressive swelling in the proximal phalanx of the right ring finger, which was relieved by aspirin. (B) X-rays revealed an osteoblastic lesion that appeared to have a segment (nidus) that was denser in its distal aspect. (C) This dense area was removed using a high-speed burr, and the symptoms resolved. (D) Review of the specimen by the pathologist confirmed the preoperative diagnosis of osteoid osteoma. (Hematoxylin and eosin, original magnification × 160.) |
-
Incisional biopsy is performed and reviewed by a pathologist very familiar with cartilage lesions.
-
Preoperative treatment includes a chest CT, because these lesions most often metastasize to the lungs.
-
Treatment is by wide excision, including digit or ray amputation.
-
Metastatic lesions in the hand (acrometastases) are uncommon and the incidence is less than 0.3%.
-
When it does occur, the phalanges and metacarpals are equally involved, and involvement of the carpal bones is said to be rare.P.63
 Figure 3-31 Metastatic carcinoma of the wrist. (A) This man, age 62, with bronchogenic carcinoma of the lung complained of pain and swelling in the right wrist. (B) Radiographs demonstrated an osteolytic metastatic lesion (arrows) in the radial aspect of the wrist.
Figure 3-31 Metastatic carcinoma of the wrist. (A) This man, age 62, with bronchogenic carcinoma of the lung complained of pain and swelling in the right wrist. (B) Radiographs demonstrated an osteolytic metastatic lesion (arrows) in the radial aspect of the wrist. -
Bronchogenic carcinoma of the lung is said to be the primary malignancy in about 50% of the cases.
-
Other primary sources are renal, esophageal, breast, colon, prostate, thyroid gland, and bone cancer.
-
Clinical findings sometimes mimic an infection with pain, swelling, and erythema being present.
-
Radiographs usually reveal a lytic lesion, although metastatic prostate cancer can appear as a sclerotic lesion.
-
If the metastatic lesion appears without
a history of prior tumor, then a suitable workup is performed to
identify the primary site. -
Biopsy and cultures of the lesion will usually confirm the diagnosis.
-
Figure 3-31 shows clinical and x-ray views of a 62-year-old man with bronchogenic carcinoma of the lung that has metastasized to the wrist.
-
Treatment is usually palliative and is based on the needs of the patient.
K, Leung D, Zelefsky M, et al. Adjuvant brachytherapy for primary
high-grade soft-tissue sarcoma of the upper extremity. Ann Surg Oncol
2002;9:41–56.
E. Tumors. In: Trumble, TE, ed. Hand surgery update 3, hand, elbow,
shoulder. Rosemont, IL: American Society for Surgery of the Hand,
2003:555–588.
P, Arner M. Soft-tissue sarcoma of the upper extremity: descriptive
data and outcome in a population-based series of 108 adult patients. J
Hand Surg 1999;24A:668–674.
AB, Lyons AR, Davis TR. A prospective study of two conservative
treatments for ganglia of the wrist. J Hand Surg 1999;24B:104–105.