Examination of the Pupils
Authors: Lewis, Steven L.
Title: Field Guide to the Neurologic Examination, 1st Edition
Copyright ©2004 Lippincott Williams & Wilkins
> Table of Contents > Section 2
– Neurologic Examination > Cranial Nerve Examination > Chapter 10
– Examination of the Pupils
– Neurologic Examination > Cranial Nerve Examination > Chapter 10
– Examination of the Pupils
Chapter 10
Examination of the Pupils
PURPOSE
Examination of Resting Pupillary Size and Symmetry and the Pupillary Response to Light
The purpose of the assessment of pupillary size and
symmetry and the pupillary light reaction is to provide information
regarding the efferent pathways that constrict and dilate the pupils,
as well as the afferent pathways through which light is transmitted in
the optic nerves.
symmetry and the pupillary light reaction is to provide information
regarding the efferent pathways that constrict and dilate the pupils,
as well as the afferent pathways through which light is transmitted in
the optic nerves.
Examination of the Pupillary Response to Near
The purpose of examining the pupillary response to near
is to assess for the presence of rare disorders that impair the ability
of the pupil to constrict to light but spare the ability of the pupil
to constrict when focusing on a close object.
is to assess for the presence of rare disorders that impair the ability
of the pupil to constrict to light but spare the ability of the pupil
to constrict when focusing on a close object.
Examination for an Afferent Pupillary Defect (the Swinging Flashlight Test)
The purpose of testing for an afferent pupillary defect
is to look for any significant asymmetry of optic nerve function of one
side compared to the other.
is to look for any significant asymmetry of optic nerve function of one
side compared to the other.
WHEN TO PERFORM THE DIFFERENT COMPONENTS OF THE PUPILLARY EXAMINATION
Examination of Resting Pupillary Size and Symmetry
Observation of resting pupillary size and side-to-side
symmetry should be performed on all patients as part of a standard
neurologic examination.
symmetry should be performed on all patients as part of a standard
neurologic examination.
Examination of the Pupillary Response to Light
Testing for the pupillary light reaction should be performed on all patients as part of a standard neurologic examination.
Examination of the Pupillary Response to Near
Testing for pupillary constriction to near needs to be
performed only when there is an obviously absent or extremely slow
pupillary light reaction, either unilaterally or bilaterally. There is
no need to check for pupillary constriction to near if normal
constriction to light is already demonstrated, because there is no
clinically important condition that affects pupillary constriction to a
near stimulus alone.
performed only when there is an obviously absent or extremely slow
pupillary light reaction, either unilaterally or bilaterally. There is
no need to check for pupillary constriction to near if normal
constriction to light is already demonstrated, because there is no
clinically important condition that affects pupillary constriction to a
near stimulus alone.
Examination for an Afferent Pupillary Defect (the Swinging Flashlight Test)
Testing for an afferent pupillary defect needs to be
performed only when there is a clinical complaint (or evidence) of
unilateral visual dysfunction or a history suggestive of a previous
episode of significant visual dysfunction affecting one eye more than
the other. Without a history of significant asymmetric vision loss,
there is no need to test for an afferent pupillary defect.
performed only when there is a clinical complaint (or evidence) of
unilateral visual dysfunction or a history suggestive of a previous
episode of significant visual dysfunction affecting one eye more than
the other. Without a history of significant asymmetric vision loss,
there is no need to test for an afferent pupillary defect.
P.34
NEUROANATOMY OF PUPILLARY FUNCTION
Resting Pupillary Size and Symmetry
Resting pupillary size is determined by the balance
between the parasympathetic efferent pathways that constrict the pupils
and the sympathetic efferent pathways that dilate the pupils. Symmetry
of pupillary size occurs because of the reflex pathways that mediate
the bilateral consensual pupillary constriction to light described in
the following section, Pupillary Response to Light.
between the parasympathetic efferent pathways that constrict the pupils
and the sympathetic efferent pathways that dilate the pupils. Symmetry
of pupillary size occurs because of the reflex pathways that mediate
the bilateral consensual pupillary constriction to light described in
the following section, Pupillary Response to Light.
Pupillary Response to Light
Pupillary constriction to light is a reflex mediated
afferently by visual pathways that begin in each retina and travel in
each optic nerve. After crossing in the optic chiasm, reflex fibers
from each eye project to the midbrain and bilaterally innervate the
Edinger-Westphal nuclei, components of the third nerve nuclei. Efferent
fibers from each Edinger-Westphal nucleus travel with the third cranial
nerve, synapse in the parasympathetic ciliary ganglion, and cause
contraction of the muscles that constrict the pupil. Because of the
bilateral reflex innervation to the Edinger-Westphal nuclei, light
shined on one eye should cause constriction of that eye (the direct
response) and also cause constriction of the opposite eye (the
consensual response).
afferently by visual pathways that begin in each retina and travel in
each optic nerve. After crossing in the optic chiasm, reflex fibers
from each eye project to the midbrain and bilaterally innervate the
Edinger-Westphal nuclei, components of the third nerve nuclei. Efferent
fibers from each Edinger-Westphal nucleus travel with the third cranial
nerve, synapse in the parasympathetic ciliary ganglion, and cause
contraction of the muscles that constrict the pupil. Because of the
bilateral reflex innervation to the Edinger-Westphal nuclei, light
shined on one eye should cause constriction of that eye (the direct
response) and also cause constriction of the opposite eye (the
consensual response).
Pupillary Response to Near
When attempting to focus on a close object, a reflex
occurs that results in bilateral pupillary constriction mediated
efferently by parasympathetic fibers from the ciliary ganglion. This
pupillary constriction to near (which can be seen clinically)
accompanies the reflex thickening of the lens, called accommodation
(which cannot be assessed clinically), that occurs due to contraction
of the ciliary muscles that are also innervated by the ciliary ganglion.
occurs that results in bilateral pupillary constriction mediated
efferently by parasympathetic fibers from the ciliary ganglion. This
pupillary constriction to near (which can be seen clinically)
accompanies the reflex thickening of the lens, called accommodation
(which cannot be assessed clinically), that occurs due to contraction
of the ciliary muscles that are also innervated by the ciliary ganglion.
Afferent Pupillary Defect
The neuroanatomy of an afferent pupillary defect is described in the section Abnormal Findings.
EQUIPMENT NEEDED TO EXAMINE THE PUPILS
-
A bright flashlight
-
The cheap, disposable flashlights common
in hospital settings are good when brand new, but they quickly become
dim and of little value for the pupillary examination. More expensive
flashlights with replaceable batteries are reasonable alternatives, as
long as they can be focused into a beam that can reliably constrict
normal pupils. The light of a rechargeable otoscope is a good source of
light for the pupillary examination.
HOW TO EXAMINE THE PUPILS
Examination of Resting Pupillary Size and Symmetry
-
Ask the patient to look straight ahead at
a distant spot in a dim room. It is helpful to show the patient a
specific spot on the wall (or the ceiling, if the patient is lying
down) to fixate on. -
Look at the resting position of both
pupils. Note whether both pupils are approximately the same size or
whether there is any obvious difference in pupillary size. If necessary
(especially if there is a difference in size between sides), pupillary
diameter can be measured with a ruler or the pupillary size chart found
on most pocket visual acuity cards.
P.35
Examination of the Pupillary Response to Light
-
Ask the patient to look straight ahead at a distant spot in a dim room.
-
Shine a bright light in one eye. Shine
the light from the lateral side of the eye or from beneath to help
ensure that the patient doesn’t accommodate to a near stimulus during
the assessment of pupillary light reaction. Assess whether the pupil
constricts to the light stimulus. -
After removing the light stimulus and
waiting a few seconds, move the light to the other eye and assess
whether that pupil constricts to light.
Examination of the Pupillary Response to Near
-
In a well-lit room (so that you can see
the pupils without shining a light into them), ask the patient to
fixate on a distant spot directly ahead, such as a spot on the wall.
Note the pupillary size while the patient fixates on that spot. -
Next, ask the patient to look down at his
or her nose. If the patient has difficulty with this maneuver, an
alternative near stimulus is to have the patient look at an object,
such as your finger or a pen, held within inches in front of the eyes. -
Observe for pupillary constriction while the patient focuses on this near stimulus for at least several seconds.
Examination for an Afferent Pupillary Defect (the Swinging Flashlight Test)
-
Assess the pupillary light reaction of
one pupil as described above. After that pupil constricts, immediately
move the flashlight over to the other eye and assess the reaction of
the other pupil (constriction or dilatation) to direct light. The light
should be kept on each pupil for approximately 1 to 2 seconds before
moving the flashlight over to the other eye. -
Next, move the flashlight back to the original eye and assess its response to direct light.
-
Repeat the process of moving the
flashlight from eye to eye a few times while you confirm the response
of each pupil after the light has been moved to that eye.
NORMAL FINDINGS
Examination of Resting Pupillary Size and Symmetry
Normally, the pupils should be approximately equal in size.
Examination of the Pupillary Response to Light
Normally, each pupil should constrict when a light is
shined directly into it (the direct pupillary response), and each pupil
should constrict when a light is shined into the contralateral pupil
(the consensual pupillary response).
shined directly into it (the direct pupillary response), and each pupil
should constrict when a light is shined into the contralateral pupil
(the consensual pupillary response).
Examination of the Pupillary Response to Near
Normally, the pupils should both constrict when focusing on a near object.
Examination for an Afferent Pupillary Defect (the Swinging Flashlight Test)
Normally, each pupil should constrict or stay the same size when the light is moved to it from the other eye.
P.36
 |
|
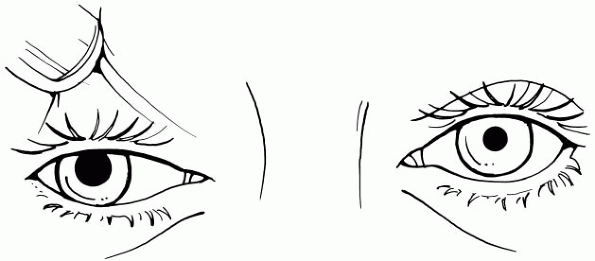
Figure 10-1
Unilateral pupillary dilatation due to a third cranial nerve palsy. The pupil does not react to light, and in this case, the ptosis is so severe that the examiner needs to lift the patient’s eyelid to examine the eye. There is also lateral and downward deviation of the eye because of the weakness of third nerve-innervated extraocular muscles. |
ABNORMAL FINDINGS
Examination of Resting Pupillary Size and Symmetry
-
Asymmetry of the size of the pupils
(anisocoria) may be seen when there is any lesion of the efferent
pathways that constrict or dilate the pupil. When anisocoria is
present, it is not always immediately obvious as to which pupil is the
abnormally large or small one, but certain clues (see below) usually
help determine this. -
As long as the pupils are approximately
equal in size bilaterally, the absolute size of the pupils—whether
bilaterally small or large—is usually of no clinical significance in
awake patients. In comatose patients, however, pupillary size, even
when symmetric, may have significant diagnostic value, as discussed in Chapter 42, Examination of the Comatose Patient.
Examination of the Pupillary Response to Light
-
A unilaterally enlarged (dilated) pupil
that reacts poorly or not at all to light suggests a lesion of the
pupillary constricting fibers of the ipsilateral third cranial nerve.
Although pupillary dilatation may be the only sign of a third nerve
palsy, other clues include ptosis on the side of the dilated pupil and
weakness of adduction, upward, and downward movement of the eye. Figure 10-1 illustrates a patient with unilateral pupillary dilatation due to a third cranial nerve palsy. -
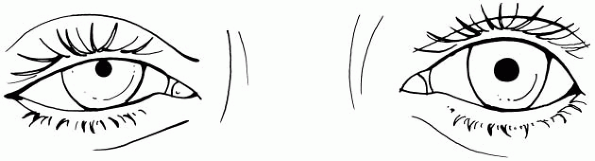
A unilaterally small (constricted or
miotic) but reactive pupil suggests a lesion anywhere along the
ipsilateral sympathetic pathway that normally dilates the eye (Horner’s
syndrome). In addition to miosis, other findings of Horner’s syndrome
may also be present, including slight ptosis and diminished sweating on
the same side of the face as the small pupil. Figure 10-2 illustrates a patient with a unilateral miotic pupil due to Horner’s syndrome. -
Complete absence of a direct pupillary
response to light on one side with retention of the consensual response
of that pupil when light is shined in the other eye is most consistent
with severe optic nerve dysfunction on the side of the absent direct
response. This is the ultimate afferent pupillary defect (see below).
P.37
 |
|
Figure 10-2
Unilateral pupillary constriction (miosis) due to Horner’s syndrome. The pupil is small, reacts to light, and there is slight ptosis on the side of the miotic pupil. |
Examination of the Pupillary Response to Near
-
A pupil with an absent reaction to light but normal constriction to near is called a light-near dissociated pupil.
-
Light-near dissociated pupils are found
in relatively rare conditions, such as Adie’s pupil syndrome, Argyll
Robertson pupil of neurosyphilis, or lesions of the pineal region (the
dorsal midbrain/thalamic region).
Examination for an Afferent Pupillary Defect (the Swinging Flashlight Test)
-
The finding of immediate pupillary
dilation—rather than constriction or no change in size—when the light
is moved to it is consistent with an afferent pupillary defect (also
known as a Marcus Gunn pupil) on that side. -
The finding of an afferent pupillary
defect implies significant relative dysfunction of the afferent visual
pathway anterior to the optic chiasm (most likely the optic nerve) of
that eye compared to the other eye. -
The clinical finding of an afferent
pupillary defect occurs because the pupil on the side of the abnormal
optic nerve retains its ability to constrict to a light shined in the
contralateral eye due to the intact efferent pathways of the consensual
pupillary reflex. When a light is moved from the good eye and then
shined in the affected eye, however, dilatation occurs because the
direct response through the abnormal side is a weaker stimulus than the
constriction that occurred from the consensual response.
ADDITIONAL POINTS
Examination of Resting Pupillary Size and Symmetry
-
Small, side-to-side differences in pupillary size (e.g., approximately 1 mm) may be physiologic (called physiologic anisocoria).
-
Lesions involving the visual afferent
pathways anterior to the optic chiasm (the retina or the optic nerves)
do not cause anisocoria, because of the bilateral innervation of the
reflex mechanism for consensual pupillary constriction. -
Lesions of the visual pathways posterior to the optic chiasm also do not affect resting pupillary size or symmetry.
Examination of the Pupillary Response to Light
Lesions of the afferent visual pathways posterior to the
optic chiasm do not affect the pupillary response to light, because the
pathways for the pupillary light reaction occur anterior to the chiasm.
optic chiasm do not affect the pupillary response to light, because the
pathways for the pupillary light reaction occur anterior to the chiasm.
P.38
Examination of the Pupillary Response to Near
Although it is not necessary to test for pupillary
constriction to near except in cases in which there is an abnormal
pupillary light reaction, it is useful to practice this test in
patients with normal pupillary light responses so that you will be
adept at performing this examination when it is clinically appropriate.
constriction to near except in cases in which there is an abnormal
pupillary light reaction, it is useful to practice this test in
patients with normal pupillary light responses so that you will be
adept at performing this examination when it is clinically appropriate.
Examination for an Afferent Pupillary Defect (the Swinging Flashlight Test)
-
Afferent pupillary defects are most
obvious when the patient has severe unilateral vision loss due to an
optic nerve lesion, such as from optic neuritis. -
By definition, it is impossible to have bilateral afferent pupillary defects!
-
Do not confuse hippus (common mild waxing and waning variations in pupillary size) with an afferent pupillary defect.
-
Patients with afferent pupillary defects
do not have anisocoria because of the presence of normal bilateral
reflex mechanisms for efferent pupillary constriction (see above).
