Distal Radius and Ulna Fractures
undergone an extraordinary evolution over the preceding twenty years.
Universal cast treatment gave way to neutralization with a bridging
external fixator, which in turn was replaced by dorsal buttress
plating. The technical advance of palmar locked plating has again
changed the management of this fracture in a real and seemingly
permanent way. The advance has also resulted in a growing understanding
that many techniques may result in satisfactory long term clinical
outcomes but have real short term advantages for patients. The
significance of these short term advantages for the patient must now be
weighed against the financial impact of routine operative intervention
has cost. In addition, with an aging society with greater longevity,
previously
held
dictums of cast treatment for geriatric patients are being challenged
both by surgeons and society. Although some patients still seem to
confirm Abraham Colles’ famous remarks that the casted wrist “will at
some remote period again enjoy perfect freedom in all of its motions
and be completely exempt from pain,”52 an increasing preponderance of published studies support the need for operative intervention in this aging population.204
Finally, and perhaps most importantly, it is becoming increasingly
apparent that operative intervention needs to be customized to the
patient and the fracture as well as the expertise of the surgeon.
Prospective randomized trials that group these factors may not result
in answers to the critical questions that surgeons wish to answer.
interventions, there are other equally disparate studies regarding
multiple facets of this fracture. Conflicting data exist regarding the
long term relationship between radiographic parameters and patient
reported outcomes. Fernandez, Trumble, and others have reported that as
little as 1 mm of articular incongruity is associated with a worse
functional outcome.75,256
Catalano et al. have indicated that although there is a correlation
between articular incongruity and radiographic arthrosis, there is not
a correlation with self reported function.42
Age is also a confounding variable in determining the need for
operative management. Young and Rayan indicated that in elderly
patients (mean age 72 years) the radiographic outcome did not correlate
with functional outcome despite significant collapse and incongruity.272
By contrast, Madhok indicated that 26% of elderly patients still
experience functional impairment following nonoperative management at 1
year following closed treatment.181
Current data confirm that patients over the age of 65 with
extra-articular fractures are more likely to be satisfied with closed
treatment than younger patients, but that there are still some
geriatric patients who will not accept shortening and angulation. Which
patients are likely to be pleased with nonoperative management in this
age group remains difficult to identify.96
Even when operative intervention is clearly indicated, controversy
still exists over the use of external fixation versus one of the
growing number of internal fixation devices. Although initial studies
indicated that there may be advantages of external fixation versus
internal fixation, more recent studies are concluding that the
restoration of normal anatomy is more important than the technique that
is used. The perception that internal fixation allows immediate range
of motion, and therefore an improved functional arc of motion at the
end of treatment, has been questioned. Immediate motion may not change
the outcome as much as the other factors associated with patient
demographics and fracture reduction.16
The perceived differences between the techniques are short term, and
patient perception of outcomes may equalize between 6 months and 1 year
regardless of the operative technique used.11,97,101,219,227,249
Perhaps more interesting is that the outcomes may be more related to
fracture severity, with superiority of internal fixation being seen in
the lower energy fractures.156 This
chapter will examine the presumably known variables including the
epidemiology, mechanism of injury, and classification systems as well
as the current trends in nonoperative and operative management, and the
complications and pitfalls of each.
Data extracted from the National Hospital Ambulatory Medical Care
Survey indicate that in 1998 there were approximately 644,985 fractures
of the distal radius treated in the United States. The incidence of
this injury appears to be both gender and age specific.100
There are three main peaks of fracture distribution: one in children
age 5-14, the second in males under age 50, and the third in females
over the age of 40 years.56 There
seems to be a growing incidence of these fractures in all three groups,
with the sharpest increase seen in both elderly females and younger
adult males.192,245,250
More importantly, these studies suggest that the difference in the two
peak incidences indicates that these fractures represent two very
different injuries: one, an insufficiency fracture in elderly patients
and the other a traumatic injury in younger males. The differences in
these injuries and corresponding groups may in some way account for
some of the discrepancies noted in the literature. Current data suggest
that distal radius fractures in the elderly may represent an
insufficiency fracture associated with all of the risk factors for
osteoporosis.192 The age-adjusted
incidence rates of distal radius fractures for women were 165 in 1986
and 211 in 1995, indicating a steady rise over ten years.100 In females the incidence rises sharply after the age of 40 from approximately 36.8/10,000 to 115/10,000 at age 70 years.182,202
In males aged 35 years and over the incidence is approximately 9/10,000
and remains constant until a slight rise at age 70 years.182,202 The data also indicate that this is the most common osteoporotic fracture,56 with a strong correlation with femoral neck bone mineral density.200
The sharpest increase in incidence occurs in elderly females, and has
been linked to estrogen withdrawal and reduced bone mineral density.187,192
Recent attention has focused on the incidence of osteoporosis in males
as well as females. In one study from Ireland the incidence of
osteoporosis in male patients with forearm fractures was found to be
27%, with a high association of vitamin D deficiency as well as
endocrine abnormalities.270 Further,
just as studies have indicated an increased mortality associated with
hip and vertebral fractures, there is evidence to suggest a higher
mortality rate following distal radius fractures, particularly in
elderly males.225
fractures in males under the age of 49 years, epidemiologic studies
suggest that the injury in younger adults is not as strongly related to
gender, but occurs more equally between the sexes.100,163
Further, the injury in this population is related to higher energy
injuries (21% of all fractures) rather than to simple falls. These data
suggest that one should regard distal radius fractures in this
population differently from those in elderly patients.57,163
The majority of fractures in the elderly are extra-articular, whereas
there is a much higher incidence of intra-articular fractures in
younger patients.235 There is also a
difference in the mechanism of injury between the groups. The majority
of osteoporotic fractures occur as the result of a fall, whereas the
majority of injuries in the younger patients are secondary to motor
vehicle accidents and sports.2,57,194
This may also explain the growing trend seen in hospital admissions for
this injury in younger patients, as these patients particularly are
being treated increasingly with operative intervention.
have been studied extensively. Decreased bone mineral density, female
gender, ethnicity, heredity, and early menopause have all been
demonstrated to be risk factors for this injury.154,183,184,192
Although the relationship between bone density and risk of distal
radius fracture is not as powerful as is seen with hip and spine
fractures, it is clearly evident in the epidemiologic literature.116,192 Furthermore, late onset of menopause and estrogen replacement may help protect against injury in this group.
displaced fractures of the distal radius may be related to the fact
that the fractured radius has shortened relative to the intact strut of
the ulna and has tilted in either a dorsal or a volar direction. This
relationship accounts for the radially deviated and dorsally prominent
distal forearm described by Goyrand94 and Colles.52
The degree of dorsal angulation and the presence of the prominent
palmar proximal fragment result in significant displacement of the
median nerve. This displacement of the nerve and the associated
hematoma in the carpal tunnel may result in symptoms of an acute carpal
tunnel syndrome. The acute shortening of the radius relative to the
ulna may manifest as an open wound palmarly and ulnarly where the
intact ulna buttonholes through the skin. Finally, the degree of radial
shortening accounts for the significant distal radioulnar joint
injuries seen with the fractured radius. A cadaveric study demonstrated
that shortening of the radius relative to the intact ulna of over 5 mm
must result in disruption of the distal radioulnar joint (DRUJ)
ligaments.2
thorough examination of the affected ipsilateral shoulder and elbow is
required to identify associated fractures, especially of the proximal
humerus in the elderly. Associated injuries have significant
implications regarding (1) the higher degree of energy imparted to the
fracture in younger patients and (2) rehabilitation challenges with
injuries to both the elbow and the wrist. Ipsilateral radial head and
distal radial fractures may indicate that sufficient energy has been
imparted to result in an Essex-Lopresti lesion.240
An effort should also be made to identify an ipsilateral scaphoid
fracture, which may direct the surgeon to consider operative versus
nonoperative management. Although there are no prospective studies in
the literature, there may be a benefit to rigid internal fixation of
the scaphoid to permit early motion of both injuries.111,255
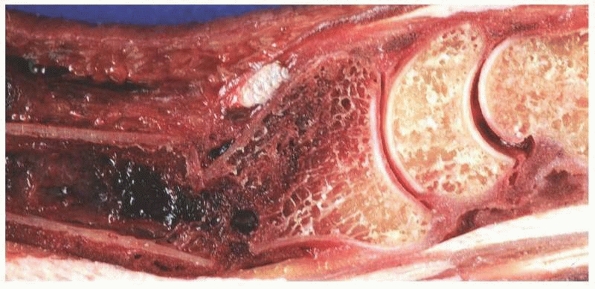
considerations. Open fractures typically result in soft tissue injury
palmarly and ulnarly where the distal ulna emerges as the radius
displaces dorsally. Direct blows and rotational injuries may result in
dorsal soft tissue injuries. A thorough evaluation of the extrinsic
flexor and extensors is indicated. Particular attention should be
directed to the extensor pollicis longus, which may be injured acutely
at Lister’s tubercle or may present with a late spontaneous rupture.
Finally, attention is directed to the neurologic complications. Median
nerve injury—either acute or chronic—is a common cause of functional
impairment and chronic pain secondary to complex regional pain
syndrome. Examination should include both a subjective evaluation of
the patient’s pain and an objective assessment of median nerve
function. Subjectively, the patient should be monitored for pain out of
proportion to the injury and also for “burning pain,” which is often
associated with nerve injury. Reduction of the fracture and elevation
of the limb typically will improve this type of pain. Objectively,
sensibility in the median innervated digits must be assessed and
monitored before and after reduction and immobilization. Abnormal
sensory examination despite reduction and immobilization may be
secondary to (1) direct contusion, (2) mechanical deformation of the
nerve, or (3) abnormal pressure within the carpal tunnel. Neurapraxia
is typically present at presentation and is associated with only
moderate pain with gradual improvement over time. Mechanical
deformation of the nerve typically improves with reduction and limb
elevation. Symptoms caused by increased pressure within the carpal
canal however may not improve and require more aggressive treatment.
This diagnosis is similar to a compartment syndrome involving the
median nerve and urgent treatment may be required to avoid long term
dystrophic symptoms. If fracture reduction and immobilization does not
improve symptoms, with patients continuing to report worsening pain and
if the degree of neurologic impairment does not improve objectively,
early decompression of the carpal canal is indicated.
is quantified numerically and the two point sensation is assessed in
both the median and the ulnar nerve distributions. After satisfactory
radiographic and clinical reduction of the deformity, the examination
is again performed to provide a baseline for subsequent serial
examinations. The upper extremity is elevated above the level of the
heart and oral narcotics are administered. Any worsening of the
patient’s symptoms from this point on requires repeat pain measurements
and assessment of sensory and motor function. The immobilization is
loosened down to the skin and ice packs may be applied. If no relief is
seen within 6 hours, then an immediate carpal tunnel release should be
performed. We prefer a longitudinal incision, which permits proximal
identification of the median nerve and subsequent release of the
antebrachial fascia and transverse carpal ligament. It should be noted
that the bony deformity, hematoma, and edema make visualization
difficult, and an extensile approach may be necessary to avoid
iatrogenic nerve injury. Any hematoma is evacuated, and a silastic
drain may be necessary to avoid reaccumulation. In general, it is not
necessary to release Guyon’s canal at this time. The exception to this
rule occurs when there is obvious extrusion of the palmar lunate facet
which may impinge on the ulnar nerve. Finally, if there is clinical
evidence of a compartment syndrome of the hand, then the compartment
pressures in the adductor and dorsal interosseous muscles must be
checked and the compartments decompressed when elevated pressures are
found.
views is useful to visualize a suspected fracture of the distal radius.
Additional
views may be obtained as needed to assess for displacement or additional injuries.
orientation of the distal radius are in common use, and it is important
to understand these in order to reduce interobserver error. Significant
discrepancy regarding intra- and interobserver reliability has been
demonstrated in the measurement of standard radiographic criteria in
the management of these fractures. For extra-articular fractures the
mean standard deviation between surgeons was 3.2 degrees for radial
angle, 3.6 degrees for palmar tilt in a true lateral view, and 2.1
degrees for palmar tilt in 15 degrees of rotation from the true lateral
view.127
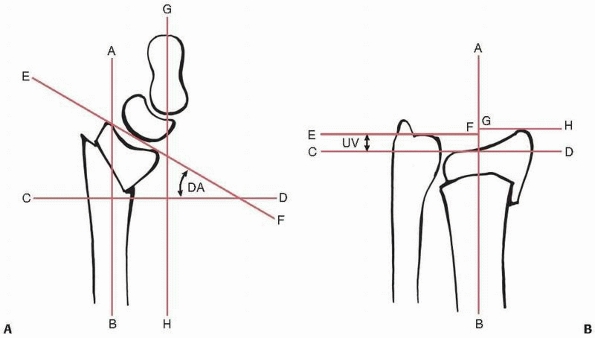
most distal points of the volar and dorsal lips of the radius. The
dorsal or palmar tilt is the angle created with a line drawn along the
longitudinal axis of the radius (Fig. 30-1A).
the distance in millimeters between a line drawn perpendicular to the
long axis of the radius and tangential to the most distal point of the
ulnar head and a line drawn perpendicular to the long axis of the
radius and at the level of the tip of the radial styloid (Fig. 30-1B).
confused with measurement of radial length. Ulnar variance is the
vertical distance between a line parallel to the medial corner of the
articular surface of the radius and a line parallel to the most distal
point of the articular surface of the ulnar head, both of which are
perpendicular to the long axis of the radius (Fig. 30-1B).
 |
|
FIGURE 30-1 A.
The dorsal angle (DA) is measured by finding the angle between a line (CD) perpendicular to the long axis of the radius (AB) and a line joining the dorsal and volar extremities of the radiocarpal joint (EF). Carpal alignment is assessed by the point of intersection of the line parallel to the long axis of the radius (AB) and a line parallel to the long axis of the capitate (GH). If these intersect outwith the carpus or do no intersect as in this illustration, then the carpus is malaligned. B. Ulnar variance (UV) is the distance between two lines perpendicular to the long axis of the radius (AB). The first is tangential to the ulnar corner of the radius (CD) and the second tangential to the ulnar head (EF). Radial length is the distance between line EF and a line tangential to the radial styloid (GH). (From Court-Brown C, McQueen M, Tornetta P. Orthopaedic Surgery Essentials: Trauma. Philadelphia: Lippincott Williams & Wilkins, 2006, with permission.) |
This is measured by the angle betwee a line drawn from the tip of the
radial styloid to the medial corner of the articular surface of the
radius and a line drawn perpendicular to the long axis of the radius (Fig. 30-1B).
fracture of the distal radius. The most common is malalignment that
compensates for the tilt of the distal radius which is extrinsic to the
carpus.253 On a lateral view one
line is drawn along the long axis of the capitate and one down the long
axis of the radius. If the carpus is aligned, the lines will intersect
within the carpus. If not, they will intersect outwith the carpus (Fig. 30-1A).
Carpal malalignment can also be caused by associated carpal ligament
disruption. The radiological diagnosis of this condition is detailed in
Chapter 28. Specific features should be assessed on each view of the distal radius as follows:
length/ulnar variance, (b) extent of metaphyseal comminution, and (c)
ulnar styloid fracture location (tip/waist/base). For intra-articular
fractures: assess (a) depression of the lunate facet, (b) gap between
scaphoid and lunate facet, (c) central impaction fragments, and (d)
interruption of the proximal carpal row.
tilt, (b) extent of metaphyseal comminution, (c) carpal alignment, (d)
displacement of the volar cortex, and (e) position of the DRUJ. For
intra-articular fractures: assess (a) depression of the palmar lunate
facet, (b) depression of the central fragment, and (c) gap between
palmar and dorsal fragments.
tilt are made on a true lateral view of the distal radius, because
malposition with rotation of the radial styloid in relation to the
shaft has a significant effect on the apparent alignment, with an
increase in palmar tilt with supination and a decrease with pronation.40
Johnson and Szabo found that rotation of the radius on the lateral view
resulted in a change in the apparent palmar tilt. A 5-degree rotational
change produces a 1.6-degree change in palmar tilt on the conventional
lateral view and a 1-degree change on the 15-degree lateral view.127
For intraarticular fractures, assess (a) the radial styloid for split
or depression and (b) depression of the dorsal lunate facet.
It eliminates the shadow of the radial styloid and provides a clear
tangential view of the lunate facet. It is useful to assess (a)
residual depression of the palmar lunate facet and (b) possible
hardware penetration into the articular surface.
traps applied after reduction. They indicate whether external fixation
may reduce the fracture sufficiently or whether direct reduction will
be required. A traction view also helps to identify fracture fragments
that may be obscured by the displacement of the fracture. Furthermore,
examination of the proximal carpal row may indicate the presence of
incongruity consistent with interosseous ligament injury.
assess the patient’s normal ulnar variance and scapholunate angle, both
of which vary between patients.
with residual intraarticular incongruity. They found a 91% incidence of
radiographically apparent arthrosis with any measurable intraarticular
step-off and a 100% incidence with over 2 mm of articular step-off.142
Subsequent authors also emphasized the relationship of as little a 1 mm
or more of articular incongruity with a worse clinical outcome.91,144
Although these studies indicate the importance of restoring articular
congruity, other authors question the ability of plain radiographs to
consistently demonstrate incongruity of less than 2 mm. Data on healed
fractures indicate that clinicians measuring step and gap deformity on
a random x-ray film will differ by more than 3 mm at least 10% of the
time. Repeat step or gap measurements by the same observer are also
expected to differ by more than 2 mm at least 10% of the time.145
articular congruity, some authors have proposed the use of computerized
tomography (CT) to assess intraarticular fractures. Clinical data
suggests that CT demonstrates intraarticular extension more accurately
than plain radiographs126 and it has
been shown to be superior in defining step-off and gaps in the
articular surface of the distal radius when compared with plain
radiographs. Cole et al. found that there was greater reproducibility
of measurements with CT and a poor correlation between radiographic
measurements and CT measurements.51
CT also allows more accurate measurement of gap formation between
palmar and dorsal fragments and has also been documented to be superior
for imaging the sigmoid notch. In one study comparing plain radiographs
to CT the authors found that in 20 consecutive fractures, plain
radiographs documented notch involvement in only 35% of the fractures
compared with 65% found on CT. Finally, CT may improve the reliability
of classification of these fractures by accurately determining the
presence of articular involvement.80
More recently three-dimensional computerized tomography has been used
to characterize these fractures. The use of this technique has
increased the perceived need for open exposure of displaced articular
segments when compared with conventional CT.104
Although it seems that plain radiographs do not reliably permit
measurements at the level of 1 mm, the clinical significance of these
studies remains unknown. The majority of clinical outcome studies have
relied on plain radiographs to assess both the injury and the treatment
outcomes.
has garnered so many eponyms over time than fractures of the distal
radius. Classifications of fractures as “Colle’s,” “Pouteau’s,”
“Barton’s,” “Smith’s,” “Chauffeur’s,” and “Reverse Barton’s” continue
to be presented despite the authors’ failure to read the original
descriptions. The resultant conflicting understanding of each eponym
creates difficulty in assessing outcomes following treatment.
proposed. To present a complete record of each would be exhaustive and
probably inadequate. Some proposed classifications seem to be more of
an attempt to stress the significance of some feature of the fracture
rather than to provide a more global approach. There are, however, some
classification patterns that have stood the test of time and continue
to be useful in understanding these fractures.
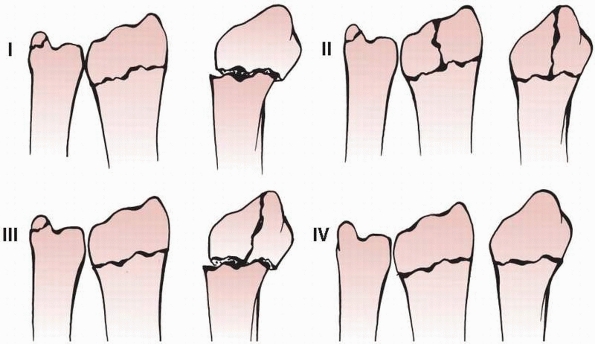
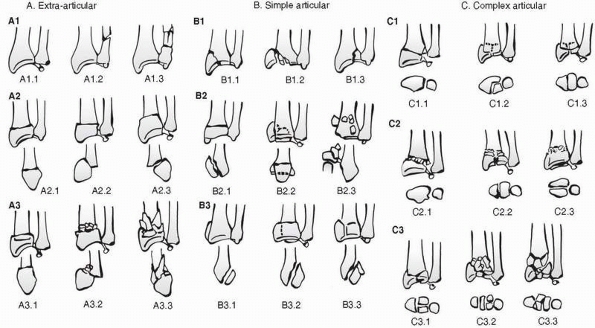
that assessed the three basic components of these injuries: (1)
metaphyseal comminution, (2) intra-articular extension, and (3)
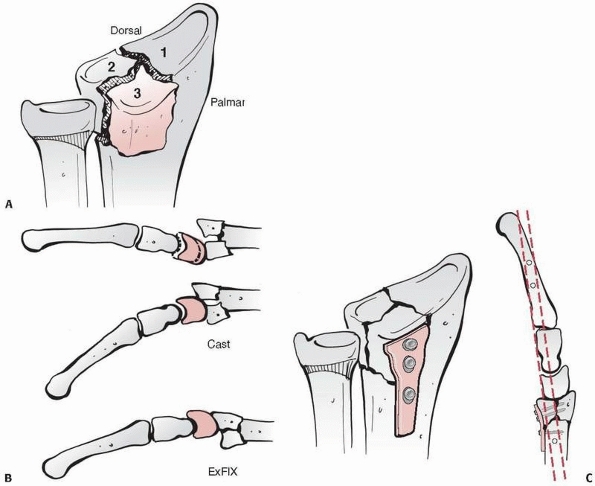
displacement of the fragments.87 Their classification system (which follows) has been accompanied by one of the first clinically useful outcomes scores (Fig. 30-2).
 |
|
FIGURE 30-2 Gartland and Werley Classification System.
|
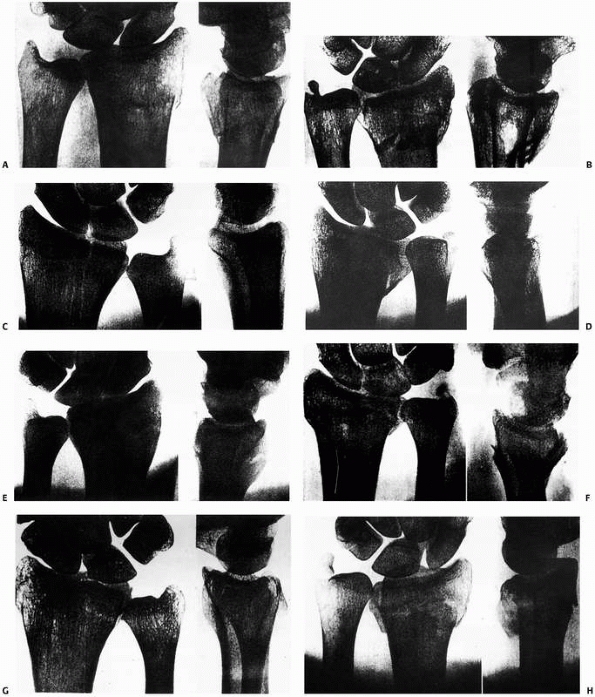
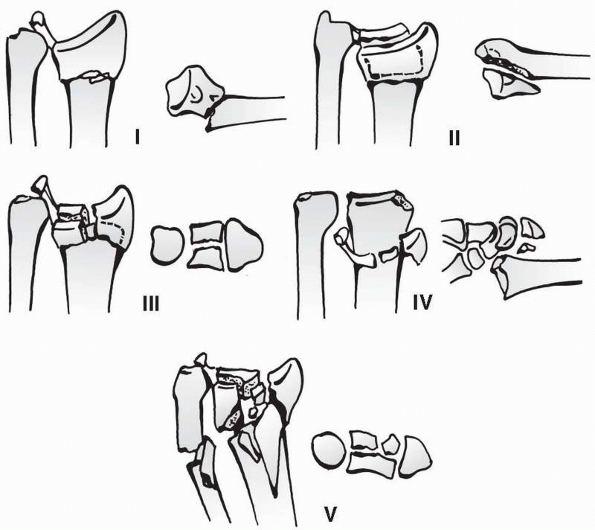
lunate on the radial articular surface to create four characteristic
fracture fragments (Fig. 30-4).191
-
Type I: Stable fracture without
displacement. This pattern has characteristic fragments of the radial
styloid and a palmar and dorsal lunate facet. -
Type II: Unstable “die punch” with
displacement of the characteristic fragments and comminution of the
anterior and posterior cortices-
Type IIA: Reducible
-
Type IIB: Irreducible (central impaction fracture)
-
-
Type III: “Spike” fracture. Unstable. Displacement of the articular surface and also of the proximal spike of the radius
-
Type IV: “Split” fracture. Unstable
medial complex that is severely comminuted with separation and or
rotation of the distal and palmar fragments -
Type V: Explosion injury
-
Type A: Extraarticular fracture. Subgroups are based on direction of displacement and comminution.
-
Type B: Partial articular fracture. Subgroups are based on lateral (radial styloid) palmar or dorsal fragments.
-
Type C: Complete articular. Subgroups are based on the degree of comminution of the articular surface and the metaphysis.
fracture line(s), the displacement of the distal fragment, the extent
of articular involvement, and the presence of an ulnar styloid
fracture. Critics point out that the simple classification systems
group fractures of differing severity and prognosis, whereas the more
complex systems have poor reproducibility. Anderson et al. compared
intra- and interobserver reliability for the AO, Frykman, Melone, and
Mayo classification systems, which emphasized fracture stability. They
found that interrater reliability was moderate for the Mayo system and
only fair for the AO, Frykman, and Melone classifications. This
apparent lack of interobserver reliability was not as evident with more
experienced surgeons, but was still present in evaluating the fractures
using the subgroups of the AO classification.8
Despite the plethora of classification systems, there continue to be
perceived deficits in our ability to classify these fractures
consistently and accurately in a manner that provides both prognosis
and treatment guidance. It has also become increasingly apparent that
outcome following these fractures may also be dependent on the degree
of soft tissue injury, including interosseous ligament injury and DRUJ
instability.128
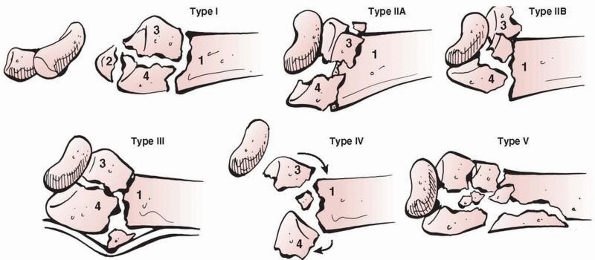
classification system that would address the potential for ligamentous
injury and thereby assist in treatment recommendations (Fig. 30-6)70:
-
Type I: Metaphyseal bending fractures
with the inherent problems of loss of palmar tilt and radial shortening
relative to the ulna (DRUJ injuries) -
Type II: Shearing fractures requiring reduction and often buttressing of the articular segment
-
Type III: Compression of the articular surface without the characteristic fragmentation; also the potential for significant interosseous ligament injury
-
Type IV: Avulsion fractures or radiocarpal fracture dislocations
-
Type V: Combined injuries with significant soft tissue involvement because of the high energy nature of these fractures
 |
|
FIGURE 30-3 A. Frykman Fracture Type I: Extra-articular fracture. B. Frykman Fracture Type II: Extra-articular fracture with ulnar styloid fracture. C. Frykman Fracture Type III: Radiocarpal articular involvement. D. Frykman Fracture Type IV: Radiocarpal involvement with ulnar styloid fracture. E. Frykman Fracture Type V: Radioulnar involvement. F. Frykman Fracture Type VI: Radioulnar involvement with ulnar styloid fracture. G. Frykman Fracture Type VII: Radioulnar and radiocarpal involvement. H. Frykman Fracture Type VIII: Radioulnar and radiocarpal involvement with ulnar styloid fracture.
|
 |
|
FIGURE 30-4 Melone classification.
|
provides sufficient pain-free motion and stability to permit vocational
and avocational activities in all age groups without the propensity for
future degenerative changes in the young. Although this goal may be
easily accepted, there is very little consistency regarding the
radiographic features that will afford this result.
11 degrees to 12 degrees of palmar tilt as having a significant effect
on functional outcome. Gartland and Werley concluded that residual
dorsal tilt has a more direct effect on outcome than residual radial
deviation, radial shortening, or loss of integrity of the radioulnar
joint.87 In a retrospective review
Kopylov found that loss of as little as 12 degrees from the normal tilt
resulted in an 80% increased risk of radiographically apparent
arthritis.144 McQueen examined 30
patients with extraarticular fractures and found that loss of 12
degrees or more of the normal palmar tilt resulted in functional
impairment when compared with those fractures which healed at neutral
or with a positive palmar tilt.173 Porter felt that loss of function did not occur until at least 20 degrees of palmar tilt was lost.208 Why the loss
of palmar tilt results in functional impairment is not entirely clear.
McQueen concluded that angulation of the distal radius resulted in
carpal malalignment, which correlated more closely with functional
outcome than measurement of the dorsal tilt, possibly because of the
inaccuracy of measurements.61
Taleisnik indicated that the dorsal shift of the proximal carpal row
results in a clinically apparent midcarpal instability with ulnar
deviation. The symptoms of instability resolved with corrective
osteotomy of the radius.253
 |
|
FIGURE 30-5 AO classification.
|
 |
|
FIGURE 30-6 Fernandez classification.
|
multifactorial; however, cadaveric data have provided some potential
explanations. The changes in palmar tilt affect not only radiocarpal
mechanics, but also radioulnar mechanics. Short et al. found that as
little as a 10-degree loss of palmar tilt causes the area of maximum
load on the radius to become more concentrated and to shift dorsally.
This change in load concentration may explain the clinical findings
relating dorsal tilt to radiographically apparent degenerative changes
at long-term follow-up.239 In
addition, the change in palmar tilt increases the tension on the palmar
and dorsal radioulnar ligaments, resulting in an increased load
required for forearm rotation.140
radiocarpal incongruity, collapse of the radial metaphysis results in
radioulnar incongruity. In a series of cadaver studies Adams found that
positive ulnar variance resulted in the most significant changes in the
kinematics of the radioulnar joint when compared with loss of radial
inclination and palmar tilt.2
Clinical studies have also indicated a strong correlation between
radial length and loss of strength. McQueen found that over 2 mm of
positive ulnar variance resulted in symptomatic loss of strength.173 Jenkins found that not only was shortening of over 4 mm associated with loss of strength, but it also correlated with pain.125
Solgaard retrospectively analyzed a series of 269 fractures and
concluded that reduction of the distal radius should primarily aim at
the correction of radial length.243
Their findings were corroborated by Batra and Gupta who noted that the
most important factor affecting functional outcome was radial length
followed by palmar tilt.23
response to loss of radial inclination, thereby resulting in increased
load on the triangular fibrocartilage complex (TFCC) and the ulna.
Although this effect is not as severe as other deformities, clinical
studies demonstrate a correlation between decreased radial inclination
and decreased grip strength.125 In addition, long term follow up indicates that this increases the risk of degenerative changes by 90%.144
The typical malunion is a three-dimensional deformity, which is
visualized using two-dimensional plain radiographs. Although the radius
is shortened with an apparent loss of palmar tilt, there is also a
rotational component, which is typically not visualized and may prove
to be significant. It is difficult, therefore, to separate out the
effect of one of these deformities from the others when assessing their
impact on outcome.
of the distal radius. The lunate tilts in the same direction as the
distal radius and the carpus adapts to this at the midcarpal joint with
flexion of the midcarpal joint in dorsal tilt and extension in volar
tilt in order to realign the hand on the forearm. This deformity is
therefore extrinsic to the carpus and occurs without any disruption of
the carpal ligaments. Taleisnik and Watson demonstrated relief of
symptoms when carpal malalignment was corrected by radial osteotomy.253 Since then carpal malalignment has been shown to correlate with poorer grip strength and rotation174 and with fewer good results.23
Bickerstaff and Bell found that the degree of carpal malalignment at 1
year after fracture was the most significant indicator of a poor result.28
malalignment in subsequent outcomes is only recently becoming apparent
as studies document significant associated ligament injuries during
arthroscopically assisted treatment.93,162,215,228
scapholunate angle caused by palmar flexion of the scaphoid may be
acceptable, it appears that a dorsiflexed lunate (a static DISI
deformity) is associated with a worse outcome.23,254
The critical shift is in the radiolunate angle, as it indicates a shift
of contact forces dorsally on the radius in the intermediate column.
There is as yet no defined threshold for this angle; however, more than
25 degrees has been correlated with a worse outcome.23
clinically significant radiographic parameter in younger patients with
regard to both functional outcome and future degenerative changes. The
threshold for acceptable amounts of radiographic congruity remains
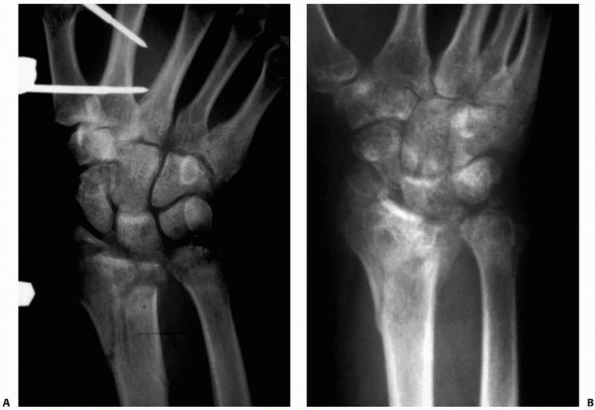
somewhat controversial. Knirk and Jupiter retrospectively evaluated 43
young adults at 6.7 years and found that any degree of articular
incongruity was associated with radiographically apparent arthritis. If
2 mm of incongruity was present, there was a 100% incidence of
degenerative changes on plain radiographs.142
Trumble et al. evaluated 52 intra-articular fractures in patients with
an average age of 37 years and found that the strongest indicator of
outcome was articular congruity.256
Note that both these studies documented the significance of residual
depression of the lunate facet following lunate impaction (die punch)
fractures as being the cause of residual articular incongruity. Cadaver
studies using pressure sensitive film document increases in contact
stresses with step-offs as small as 1 mm (Fig. 30-7).265
 |
|
FIGURE 30-7 There is incongruity of the radiocarpal joint despite attempted external fixation of the radius (A). The radiographic result (B) is significant arthrosis at 2 years, necessitating a fusion of the wrist.
|
radiographic changes seen following incomplete reduction of articular
congruity, their functional significance is debated.91,144
Catalano et al. examined 26 operatively treated intra-articular
fractures in young adults at a mean of 7.1 years. The authors found
that despite radiographically apparent arthrosis, there was no
correlation between residual articular congruity and the functional
outcome. They also found that step-off in the articular surface is more
significant than gapping between fragments of the same height.142
Similarly with extra-articular fractures, Tsukazaki et al. examined 83
consecutive patients and found poor correlation between final
angulation and functional outcome at 2 years.258
The discrepancy in these data combined with limitations in the ability
to visualize step-offs of less than 2 mm on plain radiographs makes
definitive recommendations difficult to mandate.145 As a result of these studies, the parameters presented in Table 30-1 are currently considered to be
acceptable radiographic parameters for a healed radius fracture in an active, healthy patient.
|
TABLE 30-1 Acceptable Radiographic Parameters for Healed Radius Fracture in an Active, Healthy Patient
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
remains relatively significant, pitfalls lie in interpretation of the
bony architecture using two-dimensional imaging, including fluoroscopy.
In addition, the complex ligamentous anatomy of both the extrinsic and
intrinsic aspects of the radiocarpal and distal radioulnar joints
compounds the challenge.
scaphoid facet, (3) lunate facet, and (4) sigmoid notch. The metaphysis
is flared distally in both the AP and the lateral planes with thinner
cortical bone lying dorsally and radially (Fig. 30-8).
The significance of the thinness of these cortices is that the
fractures typically collapse dorsoradially. In addition, the bone with
the greatest trabecular density lies in the palmar ulnar cortex.89
The fact that this bone is thicker even in osteoporotic cadaver
specimens may explain the success of internal fixation techniques,
which take advantage of this superior bone.203
Distally the radius has a somewhat trapezoidal shape. The radial
styloid rotates palmarly 15 degrees off the axis of the radius, which
makes capture difficult from a dorsal approach (Figs. 30-9 and 30-10).
under the lunate facet of the radius. The line of force passes down the
long finger axis through the capitolunate articulation and contacts the
radius at this location. The “palmar ulnar corner” is often referred to
as the keystone of the radius. It serves as the attachment for the
palmar distal radioulnar ligaments and also for the stout radiolunate
ligament. Displacement of this fragment is associated with palmar
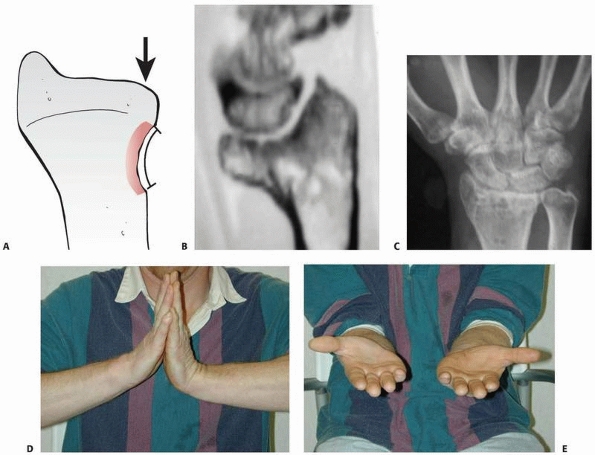
displacement of the carpus and also with loss of forearm rotation.10 Fig. 30-11
demonstrates residual depression of the lunate facet. The result is
loss of rotation as well as a step-off in the articular surface.
 |
|
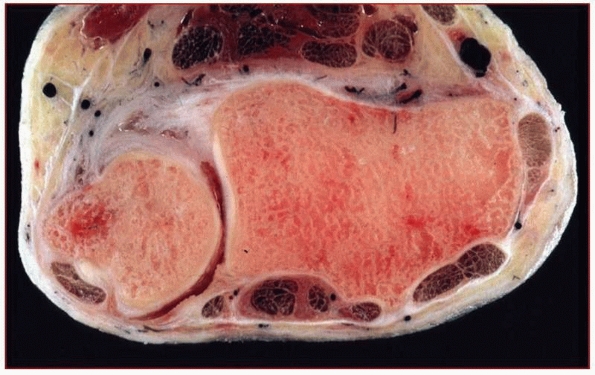
FIGURE 30-8
The cross-sectional anatomy of the radius with comminution dorsally and radially. Note the tendency to dorsal collapse is the result of dorsal comminution and the collapse at the midcarpal joint. |
 |
|
FIGURE 30-9
The cross-sectional anatomy of the radius immediately below the radiocarpal joint. Note that the radial styloid angles palmarly. Note that the extensor tendons are in immediate contact with the bone, whereas palmarly a layer of fat protects the flexors from the bone. |
 |
|
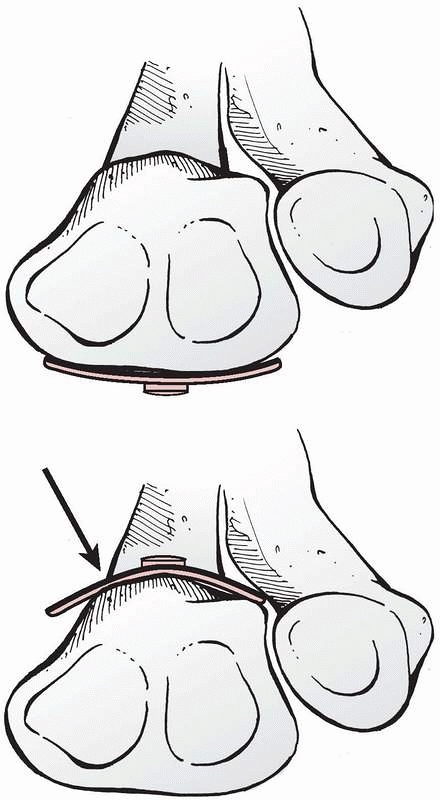
FIGURE 30-10
Cross-sectional anatomy of the radial metaphysis. Note that the dorsal surface is much more irregular than the palmar surface. The V-shape dorsally caused by Lister’s tubercle (arrow) makes it difficult to contour a plate to fit the dorsum of the radius. (From Papadonikolakis A, with permission.) |
 |
|
FIGURE 30-11 A. Disruption of the critical corner of the radius results in depression of the lunate facet. B-E. The radiographic and clinical effects are demonstrated.
|
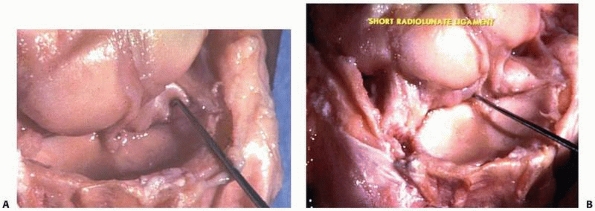
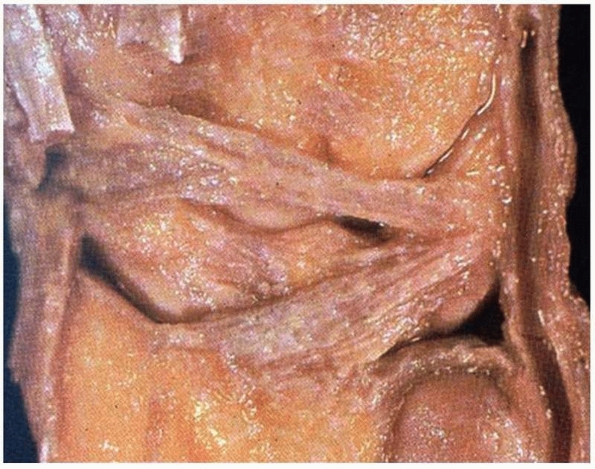
in the use of indirect reduction techniques. The palmar extrinsic
ligaments are attached to the distal radius, and it is these ligaments
that are relied on to reduce the components of a fracture using closed
methods. There are two factors about these ligaments that make them
significant for reduction: First the orientation of the extrinsic
ligaments from the radial styloid is oblique relative to the more
vertical orientation of the ligaments attached to the lunate facet. Figures 30-12 and 30-13 demonstrate the palmar and dorsal extrinsic ligamentous anatomy in the wrist.
because of the relative strengths of the thicker palmar ligaments when
compared to the thinner dorsal ligaments. In addition, the dorsal
ligaments are oriented in a relative “z” orientation, which allows them
to lengthen with less force than the more vertically oriented palmar
ligaments. The significance is that distraction will result in the
palmar ligaments becoming taut before the dorsal ligaments. Thus the
palmar cortex is brought out to length before the dorsal cortex. It is
for this reason that it is difficult to achieve reduction of the normal
12 degrees of palmar tilt using distraction alone (Fig. 30-13).
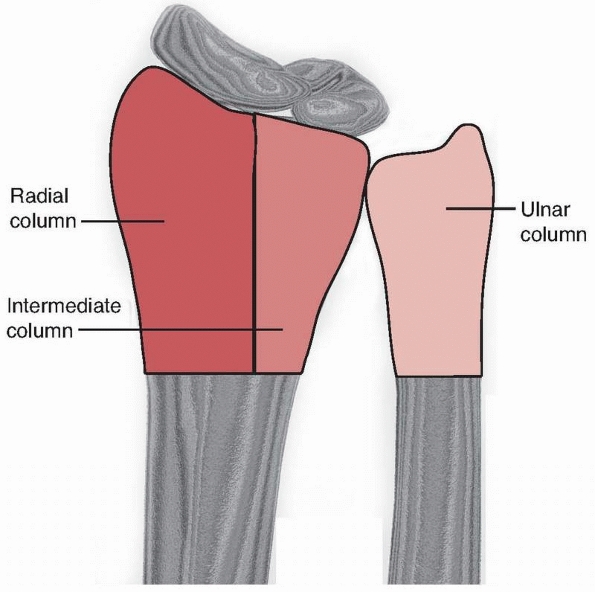
consisting of three distinct columns, each of which is subjected to
different forces and thus must be addressed as discrete elements.121 Figure 30-14 demonstrates the “columnar” approach to management of intra-articular fractures of the radius.
of the scaphoid fossa and the radial styloid. Because of the radial
inclination of 22 degreees, impaction of the scaphoid on the articular
surface results in a shear moment on the radial styloid causing failure
laterally at the radial cortex. The radial column, therefore, is best
stabilized by buttressing the lateral cortex.
consists of the lunate fossa and the sigmoid notch of the radius. The
intermediate column may be considered the cornerstone of the radius
because it is critical for both articular congruity and distal
radioulnar function. Failure of the intermediate column occurs as a
result of impaction of the lunate on the articular surface with dorsal
comminution. The column is stabilized by a direct buttress of the
dorsal ulnar aspect of the radius.
 |
|
FIGURE 30-12
These images show the thick palmar radial extrinsic ligaments when viewed from the back. Note that these ligaments are oriented obliquely off the radial styloid (A) and vertically off the lunate facet (B). Application of ulnar deviation to restore radial length with cast immobilization or external fixation results in a distraction of the radial styloid but does little to reduce the lunate facet. |
historically been the mainstay of treatment for these fractures. The
difficulty in treating patients with immobilization lies in the ability
to accurately predict the position of the fracture at final union. Cast
immobilization is indicated in (1) stable fractures in which the
expected radiographic outcome achieves the goals of treatment outlined
above, and (2) low demand elderly patients in whom future functional
impairment is less of a priority than immediate health concerns and/or
operative risks.27
is useful to consider the mechanical loads that caused the bone to fail
and present with the initial radiographic images (prereduction x-rays).
A fall on the outstretched hand may result in (1) a metaphyseal bending
fracture, (2) a lunate impaction fracture, or (3) an articular shear
fracture. The stability of the avulsion fractures is based on the
prognosis of the ligamentous injury, and combined injuries are
generally too unstable to be treated with cast immobilization.
 |
|
FIGURE 30-13
The dorsal ligaments of the wrist have a “z” configuration that allows for elongation. Compared with the palmar ligaments, the dorsal ligaments must stretch further to achieve reduction of the palmar tilt. |
must be able to resist (a) axial load and (b) dorsal displacement. A
cast with a dorsal mold may prevent dorsal displacement; however, a
cast does not resist collapse caused by an axial load. Resistance to
collapse is dependent on an intact palmar buttress. Several authors
have documented that when comminution extends into the palmar buttress,
collapse occurs even in the face of cast immobilization.81,274
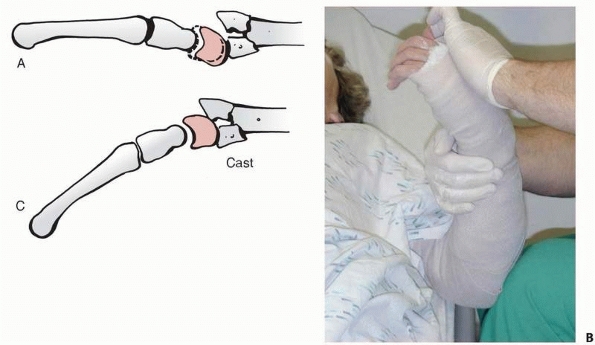
The critical degree to which the comminution extends from the dorsal
cortex to the palmar cortex as viewed on the lateral radiograph lies
somewhere between two thirds and three quarters of the radial
metaphysis (Fig. 30-15).274 Lunate impaction fractures typically result secondary to axial load. Although cast immobilization prevents dorsal displacement,
it does not resist axial loads, and as such cannot resist redisplacement of the lunate facet over time.
 |
|
FIGURE 30-14 The three columns of the wrist.
|
 |
|
FIGURE 30-15 The fate of the lunate facet with attempted closed treatment of an intra-articular fracture (A). Palmar flexion (B), which is used to restore palmar tilt, results in depression of the volar lunate facet (C).
|
-
The age of the patient. Patients over 80
years of age with a displaced fracture of the distal radius are three
times more likely to have instability than those less than 30 years of
age. This is even more striking in patients with minimally or
undisplaced fractures when the risk of instability increases tenfold in
older patients.180 Fractures in elderly patients with osteopenic bones may also displace at a later stage. -
The initial displacement of the fracture.122,243,251
The greater the degree of initial displacement (particularly radial
shortening), the more energy is imparted to the fracture resulting in a
higher likelihood that closed treatment will be unsuccessful. -
The extent of metaphyseal comminution
(the metaphyseal defect) as evidenced by either plain radiographs or
computerized tomography.122,180 -
Finally, displacement following closed
treatment is a predictor of instability, and repeat manipulation is
unlikely to result in a successful radiographic outcome.83,155,174,175
of over 3500 distal radius fractures and detailed the independently
significant predictors of early instability (redisplacement before 2
weeks), late instability (redisplacement between 2 weeks and fracture
union), and malunion for both undisplaced and displaced fractures.180
Mathematical formulae were constructed to give a percentage chance of
redisplacement or malunion for individual patients. The authors give an
example of an independent 85 year old lady with a dorsally displaced
fracture of the distal radius with metaphyseal comminution and a
positive ulnar variance of 2 mm. The calculated probability of malunion
is 82%. Clinical application of these formulae is likely to encourage
early treatment in appropriate cases and reduce the prevalence of
malunion.
management of a comminuted unstable fracture must also incorporate host
factors including physical demands, health status, independent
lifestyle, vocation, avocation, and comorbidities. With the use of
regional anesthesia and the results of several cohort series of elderly
patients having a favorable outcome with surgery, it has become more
difficult to identify those patients in whom nonoperative treatment is
indicated.
nonoperative management. Young et al. reported that at seven years
there was overall good function with nonoperative management and no
apparent advantage seen with external fixation.271
Young and Rayan indicated that in low demand patients over the age of
60, radiographic appearance at union had a poor correlation with
patient reported outcomes.5,209
Other authors noted persistent disability after nonoperative management
and have proposed more aggressive treatment in elderly patients to
avoid collapse.11,131
Although it is clear that restoration of normal anatomy is the goal, it
appears that the effect of “malalignment” of extra-articular fractures
may be mitigated in patients older than age 65, possibly because of
reducing demands.96 Future
prospective randomized studies will need to address whether patient
needs and expectations should affect the operative indications.
adequate pain relief to overcome muscle spasm. Hematoma block with
supplemental IV sedation or Bier block provides adequate anesthesia in
most settings although there is some evidence that haematoma block
provides poorer anesthesia and therefore a poorer reduction than
regional block.1,50
The use of finger traps may prove useful in the management of
completely displaced fractures and assist in the application of a cast
or splint.
direct pressure is applied on the displaced radial metaphyseal
fragment. Great care must be taken to avoid tearing of the skin,
particularly in elderly patients with parchment-like skin. Reduction
may be confirmed using sonography, fluoroscopy, or with plain radiographs after the maneuver.44
following reduction. The splint or cast should provide a dorsal
buttress to prevent collapse, but excessive palmar flexion of the
radius should be avoided. Palmar flexion of an uninjured wrist to 60
degrees has been demonstrated to cause a significant elevation of
pressure in the carpal tunnel. When palmar flexion is combined with the
swelling seen with a distal radius fracture, the elevation of pressure
may result in an acute carpal tunnel syndrome.266
The exact amount of palmar flexion of the wrist that places the median
nerve at risk is dependent on the degree of swelling, any pre-existing
carpal tunnel syndrome, and the presence of an associated hematoma. It
appears likely that a position of the wrist at greater than 30 degrees
of palmar flexion places the patient at an increased risk of an acute
carpal tunnel syndrome.34 Agee has
indicated that not only does the palmarly flexed position of the wrist
predispose the patient to median nerve symptoms, but it also places
tension on the extrinsic extensor tendons, thereby preventing complete
digital flexion.4 One study has shown no benefit to placing the wrist in flexion compared to the neural position or even dorsiflexion.98
joint is controversial, although immobilization in supination has been
proposed.244 This position restores
stability to the distal radioulnar joint and theoretically allows the
injured DRUJ complex to heal in the appropriate position. Nonetheless,
randomized studies showed no benefit in immobilisation of forearm
rotation, implying that the injury pattern determines the outcome.207,247,259
particular attention to (1) skin quality and integrity, (2) median and
ulnar nerve function as measured by 2-point discrimination, and (3)
continuity of the extrinsic digital flexor and extensor tendons, most
importantly those to the thumb.
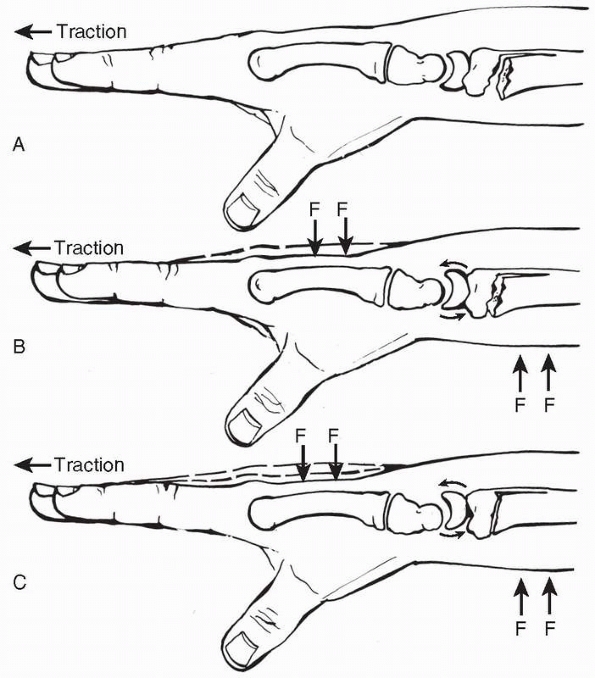
increasing the degree of the deformity and then applying longitudinal
traction. Only when sufficient traction has been applied can the distal
metaphyseal fragment be reduced on the shaft. The initial goal is to
reapproximate the palmar cortex. When the palmar cortex is
re-established then the cast has only to resist dorsal angulation
Finally, palmar tilt is restored using gentle pressure on the distal
fragment. In recalcitrant cases Agee’s technique of palmar translation
of the hand relative to the forearm may be successful in restoring
volar tilt (Fig. 30-16).3
Care is taken to avoid excessive palmar flexion of the radiocarpal
joint, which can result in an acute carpal tunnel syndrome. We find it
useful to have a portable fluoroscopy unit present to verify the
reduction. Although some surgeons prefer long arm casts, the literature
does not support their use and a forearm cast is sufficient.207,247
days. The postreduction radiographs must be compared with the initial
postreduction radiographs to exclude re-displacement.
controversial. Traditionally, distal radius fractures have been placed
in a cast for 5 to 6 weeks, but there is evidence that the less severe
fractures can be safely immobilised for 3 weeks.170,261 It may be unnecessary to use a cast at all in undisplaced fractures with outcomes shown to be better with a simple bandage.59
 |
|
FIGURE 30-16 To apply the Agee maneuver, traction is first applied either manually or with finger traps (A). Avolar translation force (F) is applied to the distal fragment of the radius (B). The lunate translates on the distal radius, causing the distal fragment to tilt in a volar direction (C).
(From Court-Brown C, McQueen M, Tornetta P. Orthopaedic Surgery Essentials: Trauma. Philadelphia: Lippincott Williams & Wilkins, 2006, with permission.) |
|
TABLE 30-2 Indications for Operative Intervention
|
|||||||
|---|---|---|---|---|---|---|---|
|
dependent on the associated soft tissue factors and the proposed
surgical procedure. As in all operative treatment of fractures,
optimally one should provide adequate soft tissue coverage of the
implants and all vital soft tissue structures. In the case of acute
fractures the fracture should be reduced by closed means as soon as
possible to minimize complications, and then operative stabilization
should be performed acutely in most cases. One exception is
arthroscopically assisted reduction and stabilization in which
operative treatment is delayed for at least 3 to 5 days to avoid
significant extravasation of irrigation fluid into the surrounding soft
tissue.228
stability is one of the earliest forms of internal fixation. This
technique can be used for both metaphyseal instability and
intra-articular displacement. It is minimally invasive and inexpensive.
It relies on the ability to reduce the distal segment and to maintain
the reduction while the pins are applied. For the larger fragments,
0.62-inch K-wires (Kirschner wires) may be used, whereas 0.45-inch
K-wires may be used to fix the intermediate column and for subchondral
fragment support. The radial styloid is pinned to the proximal shaft in
a reduced position. Once the lateral cortex is reconstituted, then the
intermediate column (lunate facet) is pinned from dorsal ulnar to
proximal radial (Fig. 30-17). Finally, any central impaction fragments can be supported using subchondral transverse wires.
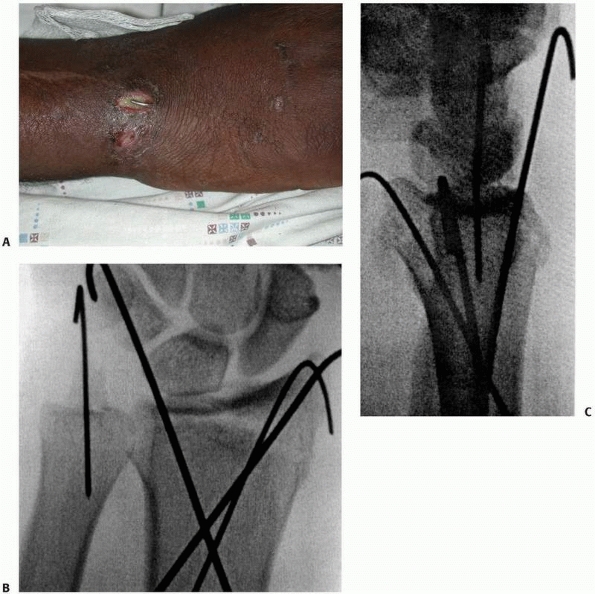 |
|
FIGURE 30-17 A-C. Comminuted radius fracture in a poly trauma patient treated with percutaneous pinning technique.
|
fragment by buttressing to prevent displacement. The wires are inserted
both radially and dorsally directly into the fracture site. The wires
are then levered up and directed into the proximal intact opposite
cortex. The fragments are thus buttressed from displacing dorsally or
proximally. In addition to being relatively simple and inexpensive,
this technique can be very effective (Fig. 30-18).221,231,257,264
A difficulty with this technique is the tendency to translate the
distal fragment in the opposite direction of the pin. This is
particularly problematic if the pins are placed dorsally resulting in
palmar displacement of the distal fragment, thereby preventing the
palmar cortex from reducing anatomically.
extra-articular and simple articular fractures in younger patients with
less comminuted fractures can be successful using percutaneous pinning.5,257,264
The major disadvantage of this technique is in older patients with
osteoporotic bone where randomized studies have shown no significant
advantage with the use of percutaneous
pins compared to cast management.18,248
Biomechanically, percutaneous pinning relies on fixation to the
proximal shaft. This results in an oblique orientation of the pins that
does little to prevent collapse of the fragments. A further
disadvantage lies in the need for associated cast immobilization to
neutralize the flexion-extension moments at the wrist, because the
fixation using this technique alone is often insufficient to prevent
displacement. Thus the technique does not eliminate the causes of so
called fracture disease that leads to digital swelling and stiffness.
In addition, the pins may become superficially infected as pin care is
difficult with the cast in place.268
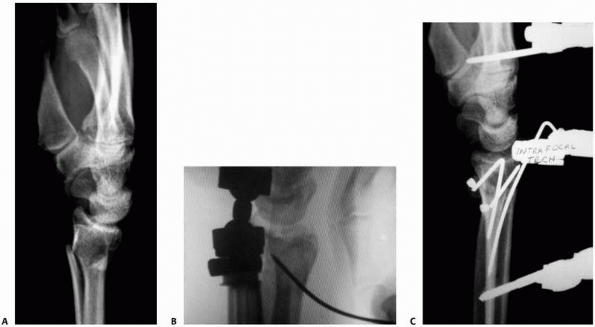 |
|
FIGURE 30-18 The Kapandji Technique: metaphyseal fracture with redisplacement after reduction (A). A pin is inserted into the fracture site, manipulated to elevate the fragment distally (B), and then driven into the opposite cortex (C). The fragments are thus trapped and prevented from dorsal displacement.
|
and Kapandji pinning remain effective techniques for extra-articular
fractures in younger patients, they are still unable to neutralize the
axial forces caused by the physiologic tension of the extrinsic flexors
and extensors. External fixation neutralizes the axial load imparted by
physiologic load of the forearm musculature. External fixation may be
performed in a “bridging” technique in which the fixation crosses the
radiocarpal joint or in a “nonbridging technique” in which the distal
fixation pins are placed in the subchondral bone and radiocarpal motion
is permitted.
allows distraction across the radiocarpal joint and directly
neutralizes axial load. Initially external fixation was felt to provide
“ligamentotaxis” to the fracture fragments. The philosophy was that the
intact wrist capsule and ligamentous structures would “indirectly”
reduce both the metaphyseal displacement and any impacted articular
fragments, and open reduction would not be necessary. Multiple cohort
series of patients have documented the efficacy of this technique.66,76,115
Several studies have compared external fixation to cast immobilization.
Although there is some conflicting data, it appears that external
fixation provides superior radiographic parameters when compared to
cast treatment.22,47,114,124,174
fixation alone may not be sufficiently rigid to prevent some degree of
collapse and some loss of palmar tilt during the course of healing,43,54,88,172,174
with some degree of collapse being seen in up to 50% of patients and
significant collapse in up to 10% of patients. Cadaver studies further
document the difficulty in utilizing external fixation alone to obtain
palmar tilt and that even augmented external fixation may not be as
stable as internal fixation.21,113
In an effort to allow the fixator to be removed earlier and to prevent
collapse of the fracture, many authors have advocated the use of
supplemental bone graft or a bone graft substitute within the fracture
site.39,107,159
Leung et al. retrospectively reviewed 72 cases in which the metaphyseal
defect was packed with cancellous autograft and the external fixator
was removed at 3 weeks, with the initiation of early range of motion.
Only five patients demonstrated radiographic evidence of collapse and
70 of 72 regained an average of 137 degrees of flexion-extension at
only 6 months.158 The additional
morbidity of obtaining cancellous autograft, however, prompted the use
of other substrates to fill the void; and cancellous allograft has
proved to be a useful adjunct to external fixation, particularly in the
elderly patient population (Fig. 30-19).
both bone inductive and conductive, which have been proposed to fill
the metaphysis and prevent fracture collapse. Of particular interest in
distal radius fractures is the potential for percutaneous application
of a liquid substrate that could harden and prevent articular collapse.
Cassidy and coauthors performed a prospective randomized study
comparing closed manipulation and percutaneous introduction of a
calciumphosphate bone cement to treatment with external fixation or
cast application. Although significant clinical differences were seen
at 6 and 8 weeks postoperatively, there were no substantial differences
at 3 months. The radiographic results demonstrated superior maintenance
of radial length in the cement group. The authors concluded that use of
this material may allow for a more accelerated rehabilitation, compared
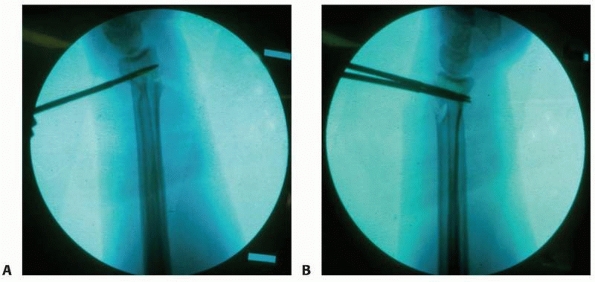
with external fixation or cast treatment.41 Their results corroborate a previous study comparing cement with cast treatment alone (Fig. 30-20).232
 |
|
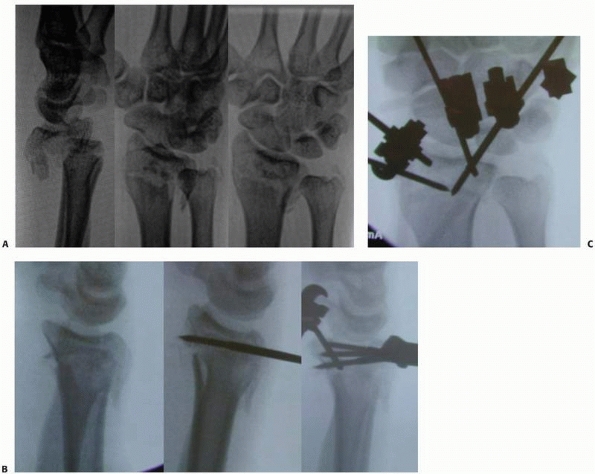
FIGURE 30-19 A,B.
A large metaphyseal defect is seen in a young adult with a comminuted fracture. The defect was filled with cancellous autograft and the fracture was stabilized with a dorsal plate. Note the appearance of the metaphysis after healing and plate removal (C). |
percutaneous pins has also been introduced to improve the stability of
external fixation and prevent loss of reduction. Cadaver studies have
demonstrated that supplemental wires increase the stability of the
construct to nearly that of dorsal plating.64
The use of crossed wires engaging the contralateral cortex
substantially further increases the rigidity of the construct. The
major complication seen with the use of pins is with iatrogenic injury
to the superficial radial nerve. The nerve emerges proximally through
the brachioradialis and arborizes distally. This risk of injury may be
lessened by making a small 5-mm incision and spreading with a hemostat
down to bone. Several authors have documented the clinical efficacy of
this technique in preventing loss of reduction and achieving excellent
clinical outcomes (Fig. 30-21).91,237
nonbridging external fixation in the wrist was reported by Ombrédanne
who used a nonbridging technique for fractures and osteotomies of the
forearm in children in 1929. Ombrédanne concluded that “temporary
osteosynthesis with external connection allows a mathematical
adjustment of the surgical correction … and guarantees further
retention with ample and sufficient precision.”74
ignored after the introduction of bridging external fixation by
Anderson and O’Neil.9 They
introduced bridging external fixation for severely comminuted
intra-articular fractures of the distal radius in young men in whom
nonbridging external fixation may not have been an option. Interest in
the nonbridging technique was stimulated in the 1990s by the
realization that bridging external fixation was not an ideal option for
the increasing numbers of fitter, elderly patients with low-energy
extra-articular or minimal articular fractures who, unlike previous
generations, were not prepared to accept malunion and possible
functional deficit.
extra-articular or minimal intra-articular dorsally displaced fractures
with metaphyseal instability and it is applicable to most of these
fractures.106 The technique is not
suitable for the treatment of volar displaced fractures. Fewer cases
with displaced articular extensions are suitable for nonbridging ex
fix, as after fixation of the
joint
surface they may lack the necessary space in the distal fragment for
the distal pins. Nevertheless, the use of multiplanar wires both to
reduce and hold the articular fragments and to hold the metaphyseal
alignment in a hybrid type construct of nonbridging external fixation
has been reported as a good treatment option for articular fractures.95
 |
|
FIGURE 30-20
Cement augmentation of a metaphyseal fracture of the distal radius. First the defect is compartmentalized using a balloon stent (A). Next the fracture is stabilized with a K-wire (B) and then the defect is filled with injectable calcium phosphate cement (C,D). |
nonbridging external fixation is lack of space for pins in the distal
fragment: approximately 1cm of intact volar cortex is required to give
purchase for the pins. Neither dorsal metaphyseal comminution nor
osteoporosis is a contraindication for the technique, because the pins
achieve their grip on the volar cortex and fixation failure is rare.25,79,106,172,174,176 As with any external fixation technique insertion of pins through areas of possible skin infection is contraindicated.
The first report of nonbridging external fixation with anatomic results
was a comparison of plaster and nonbridging external fixation in
patients under 60 with displaced distal radial fractures. The quality
of the reduction was good in both groups, but the reduced position was
maintained better (P < 0.01) by the external fixation group.123
 |
|
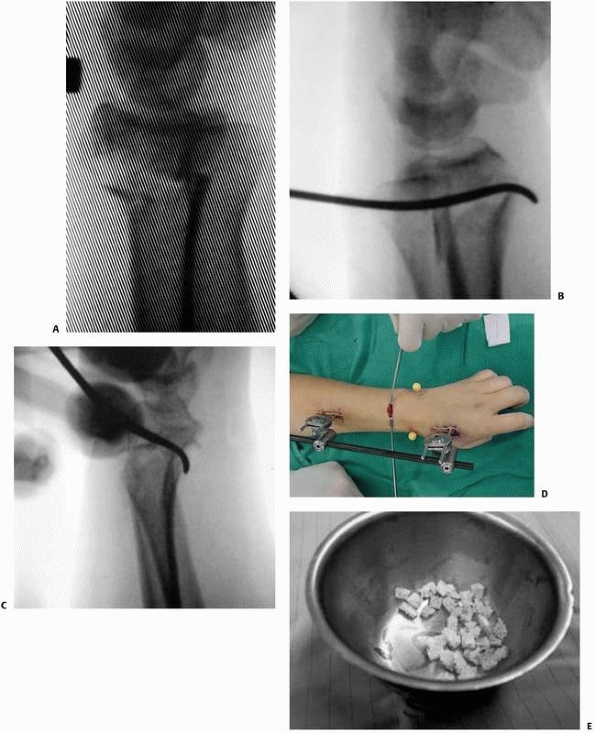
FIGURE 30-21 Technique of percutaneous pinning of a dorsally comminuted metaphyseal fracture (A).
First the palmar cortex is re-approximated percutaneously using a curved Hohman retractor through an incision dorsally in the interval between the third and fourth dorsal compartments (B,C). The palmar tilt is restored and held with the fixator (D) and the subsequent metaphyseal defect is grafted using cancellous allograft (E). (continues) |
fixation was a comparison with bridging external fixation. Sixty
patients with an average age of 61 years and redisplaced distal radial
fractures were studied. Nonbridging external fixation showed
statistically significant improvement in both dorsal angle and radial
shortening compared with bridging external fixation at all stages of
review, with no loss of volar tilt until final review at one year.172 There were no malunions in the nonbridging group in this study.
fixation is therefore restoration and maintenance of the normal volar
tilt of the distal radius. In bridging external fixation, reduction
of
the fracture depends on ligamentotaxis. Volar tilt may not be restored,
because the volar ligaments are shorter and stronger than the dorsal
ligaments and prevent full reduction.21
With nonbridging external fixation the reduction is performed using the
distal pins as a joystick, allowing the surgeon direct control of the
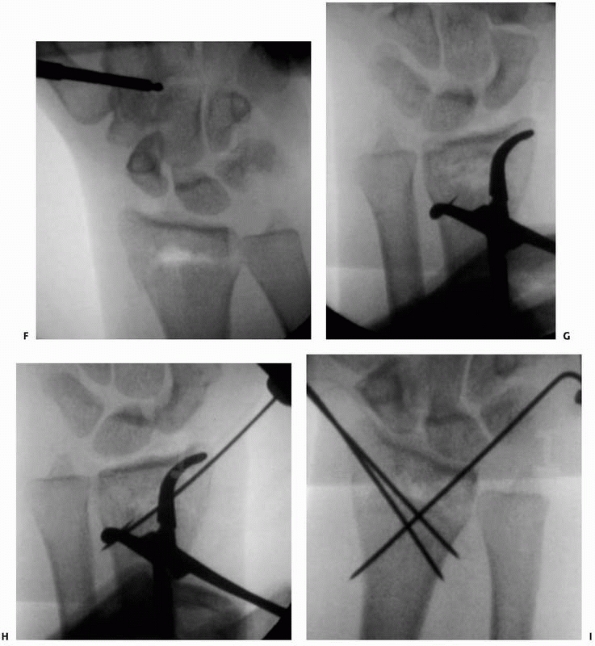
distal fragment and obviating the need for ligamentotaxis (Fig. 30-22).
 |
|
FIGURE 30-21 (continued) Finally, the lateral cortex is reduced with a percutaneously applied tenaculum clamp and crossed pins are inserted (F-H). The stability of the construct may be improved with the use of an additional pin applied radially (I).
|
nonbridging external fixation for acute fractures of the distal radius
compared with bridging techniques.172
In this study the average grip strength in the nonbridging group was
restored to 87% of the opposite normal side, allowing for dominance.
Other indices of function also showed superior results in the
nonbridging group. Nevertheless, when the technique is used for severe
articular fractures this difference disappears, probably because the
severity of the injury dictates the outcome,148,149
although with the use of smaller distal pins inserted orthogonally to
the intermediate and the radial column this technique has been
demonstrated to be useful in simple impaction fractures with articular
extension (Fig. 30-23).
for nonbridging external fixation is a good series of preoperative
films with true anteroposterior and lateral views of the wrist to
assess
the size of the distal fragment. On the lateral view the volar cortex
should be seen clearly: 1 cm of intact volar cortex is required. The PA
view also allows assessment of the size of the fragment particularly on
the ulnar side. Some distal fragments narrow towards the distal
radioulnar joint on the AP view. This configuration may not allow
sufficient purchase for an ulnar sided pin. More advanced imaging
usually is not necessary unless the nonbridging technique is to be used
for severe articular fractures, when CT scanning may be required to
visualise the articular fracture pattern and to plan placement of
hybrid type pins.
 |
|
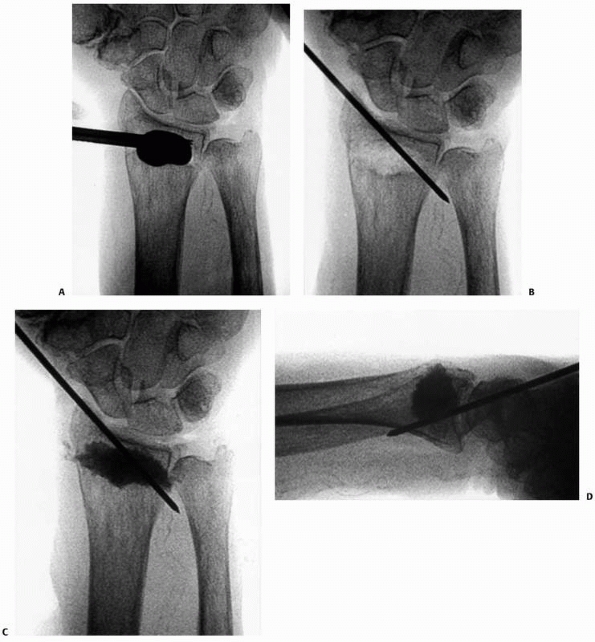
FIGURE 30-22 A.
A fluoroscopic view of the distal pins for a nonbridging external fixator. The fracture is unreduced and the pins have been inserted parallel to the radiocarpal joint, between the fracture and the joint and engaging the volar cortex. B. The fracture has been reduced into palmar tilt using the pins as a “joystick.” Note the defect in the dorsal cortex from dorsal comminution. |
 |
|
FIGURE 30-23 A. A three-part distal intra-articular fracture. B. Placement of shanz pins in the distal fragments through the palmar cortex allowing control of palmar tilt. C.
Note that these distal pins control both the radial and the intermediate column separately and that these fragments are locked into the construct |
recommended as some evidence shows that the use of this technique
reduces the incidence of complex regional pain syndrome type I.214 The patient is placed supine with the arm extended on the hand table and the wrist in neutral rotation. A tourniquet is applied
to the upper arm. The surgeon is seated on the cephalic side of the arm
table and the C-arm is positioned on the opposite side. Fracture
reduction prior to insertion of the pins is not necessary.
midway between the fracture site and the radiocarpal joint and on
either side of Lister’s tubercle (Fig. 30-22A).
If there is an undisplaced sagittal articular fracture, pins should be
placed on both the radial and ulnar sides of the articular extension. A
marker is placed on the skin and its position in relation to the entry
point on bone confirmed with the C-arm. A 1-cm longitudinal incision is
made at this point and the extensor retinaculum exposed. A longitudinal
incision is made in the extensor retinaculum under direct vision, with
care taken to protect the underlying tendons, and the bone is exposed.
A fixator pin is placed on the bone and its position confirmed on the
C-arm. The angle of the pin is then adjusted so that its projected
course is parallel to the radiocarpal joint on the lateral view. The
pin is then inserted by hand without predrilling until its tip
penetrates the volar cortex. Further pins may then be inserted using
the same technique with the spacing and relationship of the pins being
determined by the fixator used.
the fracture utilising open pin placement to avoid damage to the dorsal
branch of the radial nerve. A longitudinal skin incision is made over
the dorsum of the radius, followed by blunt dissection to expose the
tendons of extensor carpi radialis longus and extensor carpi radialis
brevis. The natural interval between these tendons is developed to
expose the radius. The proximal pins are then inserted by hand with or
without predrilling and should engage both cortices of the radius. The
fixator should then be assembled but not tightened. Reduction of the
fracture is then achieved using the distal pins as “joysticks,” which
requires little force in an acute fracture (Fig. 30-22B).
Where reduction has been delayed, forcible reduction should not be
attempted because this may cause pin loosening. In late cases reduction
using the pins should be gentle and gradual. A good reduction is
usually possible up to approximately 3 weeks after fracture. Should
reduction not be possible without undue force, a small incision should
be made over the dorsum of the fracture and a lever inserted to reduce
the fracture directly. The fixator is then tightened and the reduction
confirmed using the C-arm.
especially where there is overlap of the volar cortex. This should be
preventable as it is easily recognised radiologically. If the insertion
of distal pins proves unsuccessful because of insufficient intact volar
cortex, it is simple to convert the construct to a bridging construct
with or without augmentation.
stability and control over palmar tilt with the insertion of pins into
the distal metaphyseal fragment and attachment of them directly to a
bridging external fixator.35,63,186,269
As with nonbridging external fixation, direct control over the distal
fragment may eliminate some of the loss of reduction seen with external
fixators, including the loss of palmar tilt and radial collapse (Fig. 30-23).
Nonetheless, the use of this technique has limited application because
this can be achieved with nonbridging external fixation without any
disadvantages and without sacrificing early wrist motion.
 |
|
FIGURE 30-24
The fracture has been overreduced with excessive palmar tilt. This can be prevented by use of the fluoroscope and adjustment of the external fixator. |
when the articular fragments are felt to be too small and too numerous
for internal fixation with plate-screw constructs, and yet the fracture
does not reduce anatomically with standard techniques. It has been used
primarily for high-energy injuries with comminution both dorsally and
palmarly. The technique permits internal fixation of the comminuted
fragments palmarly, and the use of the external fixation device
prevents collapse on the side opposite the plate. Several cohort series
have documented success with this technique.22,212,217
The underlying principle is to create an intact palmar buttress using a
plate and then to prevent dorsal collapse by tensioning across it using
an external fixator. The technique was felt to obviate the need for
combined plate fixation and the extensive soft tissue stripping that
goes with it.230
when external fixation has been performed and persistent incongruity of
the palmar lunate facet is demonstrated. It is critical to reduce and
stabilize this facet to obtain both articular congruity and distal
radioulnar joint stability. A 5-cm skin incision is made ulnar to the
flexor tendons, which are gently retracted to expose the intermediate
column. The lunate facet is elevated and then held in position with a
palmar plate. Once the plate is fixed proximally it creates an intact
palmar buttress, across which tension can be applied (Fig. 30-25).
the radial limb of the plate or with percutaneously applied K-wires.
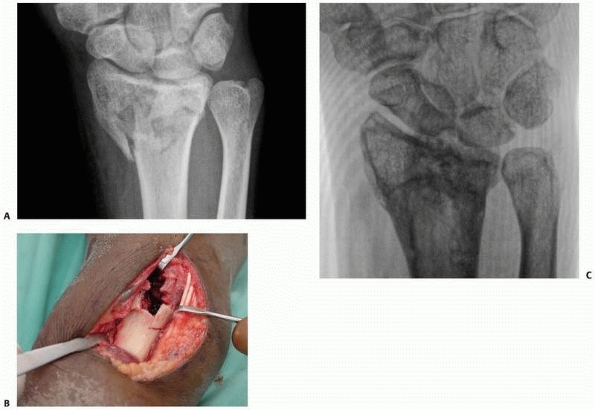
 |
|
FIGURE 30-25 A. Typical three-part intra-articular fracture of the distal radius. B. Depression of the lunate facet palmarly is difficult to reduce by closed methods. C. A plate applied palmarly to the lunate facet reduces and mortars both the DRUJ and the radiocarpal joint.
|
articular congruity in the outcome following distal radius fractures,
concern remains whether we can adequately visualize the articular
surface intraoperatively.70,73,90,142,256
Despite the reported significance of a residual step-off of 1 mm or
more, several authors have documented difficulty in the reliable
measurement of articular step-offs of 1 mm using conventional
radiographs or intra operative fluoroscopy.65,145
Arthroscopy has demonstrated residual displacement of articular
fragments in 33% to 71% of fractures following reduction under
fluoroscopy.17,65
The technique has also been extremely useful in documenting a wide
variety of chondral lesions, interosseous ligament injuries, and
avulsions of the triangular fibrocartilage.93,160,161,162,215
The incidence of interosseous ligament injuries associated with
intra-articular fractures appears to be approximately 50% for
scapholunate ligament injuries and 20% for lunotriquetral injuries.71
Triangular fibrocartilage injuries occur in approximately 40% of
fractures and direct chondral injury in up to 30% of fractures.161
existing knowledge of associated soft tissue lesions in distal radius
fractures, there is still some question whether the technique provides
outcomes superior to conventional techniques. Kazuteru et al. performed
a prospective randomized study comparing the results of 34 patients
treated using arthroscopically guided reduction, with 48 patients
treated with open reduction and internal fixation.138
The results indicated superior radiographic and functional outcomes
with the arthroscopically guided procedure. A second matched control
study comparing arthroscopically assisted external fixation with
fluoroscopically assisted external fixation, however, documented no
significant differences between groups with the exception of forearm
rotation and ulnar sided symptoms.228
The authors concluded that although arthroscopy provides superior
imaging of the articular surface, external fixation permits some
collapse during fracture union, which may detract from the subsequent
radiographic outcome measurements. One alternative is to make use of
arthroscopic assistance to assess reduction while using volar plate
fixation to stabilize the fracture. This approach has been shown to
accurately more assess the magnitude of step and gap in the articular
surface following fixation, using a palmar approach and fluoroscopic
assistance in reduction. A perceived difficulty with this approach is
that arthroscopy is used to assess the reduction only after the
hardware is in place, thereby precluding improving the reduction
without removing the fixation. Alternatively, direct control of the
articular surface using smaller pins that lock into the external
fixator may allow the surgeon to directly mimimize the step and gap
under arthroscopic control prior to fixation with a volar plate.
external fixation is controversial. Generally speaking, fractures with
extensive metaphyseal comminution might be best managed with formal
open reduction and internal fixation to prevent subsequent collapse. In
patients with a large ulnar styloid fracture fragment and distal
radioulnar instability, open reduction and internal fixation of the
ulnar styloid fragment may be required, and arthroscopy may not add
substantially to the care. Those fractures that may benefit most from
adjunctive arthroscopy are (1) complex articular fractures without
metaphyseal comminution, particularly those with central impaction
fragments, and (2) fractures with evidence of substantial interosseous
ligament or TFCC injury without a large ulnar styloid fragment (a
fracture at the base of the styloid).
and 15 days postinjury. When fragments are significantly displaced,
associated palmar and dorsal rents in the capsule may exist. This
situation permits extravasation of irrigation fluid into the
surrounding soft tissue, which is exacerbated with the use of a pump.
Waiting 5 to 7 days minimizes this complication.
reduction of the articular surface; however, there are advantages to
having the fixator in place prior to the arthroscopy. First the
extraarticular portion is reduced and out to length, thereby providing
a template for elevation of the depressed segments of the articular
surface. Second, the external fixator provides excellent distraction of
the joint for the arthroscopy.
metaphyseal defect must be addressed. Through a small 2-cm incision,
the dorsal metaphyseal comminution may be exposed and the defect may be
partially filled with graft. One should avoid interposing graft between
the major fragments of the articular surface. The window is left
exposed to allow for manipulation during the arthroscopy. A provisional
reduction is obtained and verified fluoroscopically. Additionally,
prepositioned K-wires in the major fragments are useful to facilitate
stabilization once the reduction has been effected.
and other debris from the joint and perform a diagnostic arthroscopy
through the 3-4 portal. This portal is best utilized for the purposes
of instrumentation, whereas the 6-R or 6-U portals permit superior
visualization of the fracture.228
Careful inspection of the scapholunate and lunotriquetral ligaments as
well as the TFCC is performed, both for prognostic and therapeutic
purposes. Any disruptions of the interosseous ligaments may require
further inspection through the midcarpal portals. Pathology is
addressed from the radial side, proceeding ulnarly. Incomplete ligament
injuries may be stable, and debridement can be performed if indicated.
Subluxations from complete ligament injuries are reduced and pinned
using Kirschner wires. Next the articular surface is reduced and
pinned. It is critical to have a landmark for length and tilt in order
to reduce the articular surface correctly. Kirschner wires are placed
in each of the major fragments and their depth of penetration is
verified at the end to avoid over penetration palmarly. Ulnarly the
lunotriquetral interosseous ligament (LTIO) is treated with pinning or
debridement. Finally, the TFCC may be repaired back to the extrinsic
carpi ulnaris (ECU) subsheath. If distal radioulnar joint instability
has been treated surgically, the forearm is placed in 30 degrees of
supination for a total of 3.5 weeks, after which range of motion is
initiated (Fig. 30-26).
complication rates for the use of external fixation to treat distal
radius fractures range from 6% to 60% depending on how “major” and
“minor” complications are reported.216,217,233
Although many complications of distal radius fractures are seen
regardless of the treatment, some are directly related to treatment
with an external fixator and or supplemental pins.119
Overdistraction during bridging external fixation has been implicated
in producing worse digital motion, worse functional outcomes, and worse
strength and pain scores following fracture treatment.132
Although there is no threshold limit for distraction, it appears that
there is a correlation between increasing carpal height index and worse
functional outcomes.133 The fact
that there is no threshold for overdistraction makes it difficult to
demonstrate a strict causal relationship, as evidenced by one study
that documented distraction of 5 to 8 mm across the radiocarpal and
midcarpal joints without a negative outcome.30
Overdistraction of the wrist, particularly if it is combined with
palmar flexion, results in relative lengthening of the extrinsic
extensor tendons and may prevent full active and passive digital
motion. Prolonged loss of full flexion combined with the swelling
following a wrist fracture can result in permanent loss of
metacarpophalangeal motion. Therefore it is critical to look for this
complication following completion of the procedure. The diagnosis is
suspected when there is a gap across the midcarpal joint on
fluoroscopic assessment during the procedure, and confirmed when full
passive digital motion is difficult to achieve.
recognize the limitations of external fixation alone in the management
of highly comminuted fractures. In extra-articular fractures, external
fixation in isolation does not typically restore the physiologic 12
degrees of palmar tilt. Cadaver studies indicate that the thicker and
vertically oriented palmar ligaments become taut before the thinner and
“Z” configured ligaments dorsally. Pure distraction results in the
palmar ligaments tightening before the dorsal ligaments and a failure
to achieve palmar tilt.21,55
Clinical studies also indicate that loss of palmar tilt is common
following external fixation alone without supplemental grafting or
pinning.35,54,55,58,172,174
In addition, external fixation in isolation may not elevate a displaced
intra-articular fracture. Central impaction fragments have no
capsuloligamentous attachments; therefore distraction alone will not
elevate these fragments. The palmar lunate facet may not reduce with
distraction alone, and ulnar deviation actually allows the lunate to
settle relative to the radial styloid because of the oblique
orientation of the extrinsic radial ligaments. This complication may be
avoided by recognizing the limitations of the technique and making use
of more direct reduction tools to achieve a congruent articular surface
and physiologic palmar tilt.
Injury to the superficial radial nerve may be seen following open pin
insertion, percutaneous half pin insertion, or with the use of
supplemental K-wires. The incidence varies; however, several series
report transient dysethesias in 16% to 21% of cases.38,113,150 In an effort to lessen this
complication several authors have recommended open rather than percutaneous half pin insertion.54,67,105
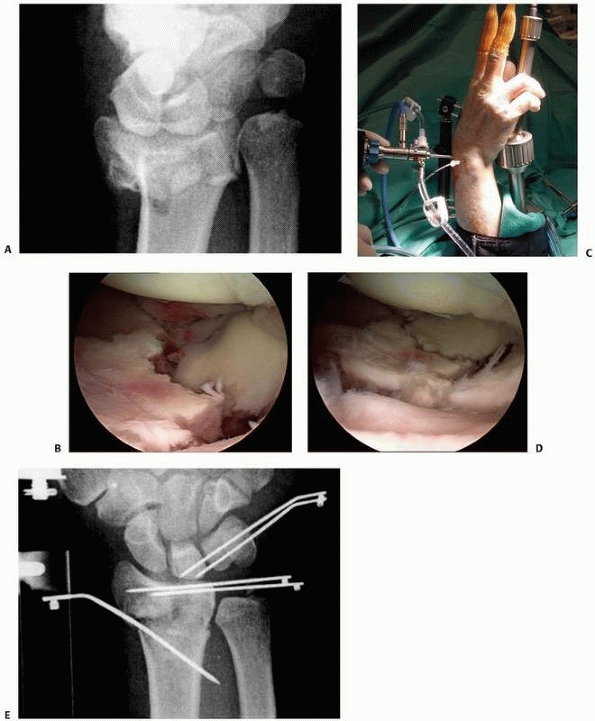 |
|
FIGURE 30-26 A lunate impaction fracture (A) is placed in an external fixator. The radial column is brought out to length and the arthroscope is placed (B). The impacted fragments are disimpacted and pinned with subchondral wires (C,D). Finally the lunotriquetral ligament disruption is reduced and pinned (E).
|
rigidity but may also result in the increased likelihood of injury
associated soft tissue structures, particularly branches of the
superficial radial nerve. These smaller branches have been shown to be
at risk with percutaneous introduction of pins in the distal radius or
the carpus.99 These injuries tend to
be transient, with resolution by 6 months, but they may also
precipitate a complex regional pain syndrome. Biomechanically, the pins
are best placed radially; however, the more dorsal the pin placement
the safer they are from iatrogenic cutaneous nerve injury (Fig. 30-27).
true incidence of pin tract infections is unknown, in part because of
failure to define whether such an entity is a transient cellulitis or a
deeper infection with or without bony involvement. For K-wires the
incidence ranges from 6% to as high as 33%.103 For external fixation
pins the incidence has been reported to range from 1% to 8%.54,67,118
Because the instance of pin tract infection is relatively low, studies
comparing predrilling with direct drilling of the pins are generally
underpowered, and the relationship of predrilling to the infection rate
has not been established.118 Egol et
al. performed a prospective randomized trial evaluating the use of
hydrogen peroxide wound care and chlorhexidine impregnated dressings
and found no statistical difference in pin site infections
in these groups when compared to sterile dry dressings.68
In general, pin tract infections will resolve with the use of oral
antibiotics and increased frequency of dressings. It is rare for pin
tract infections to affect the final outcome.
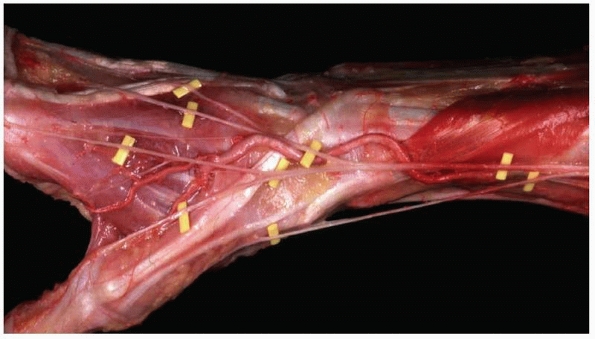 |
|
FIGURE 30-27
The anatomy of the superficial radial nerve at the distal radius. Note that the majority of the branches lie palmar to the second dorsal compartment. |
were published on distal radius fractures. Of these, 60 dealt with
internal fixation of the fracture. By contrast, the last 15 years have
produced over 2000 articles on distal radius fractures, 400 of which
focused on internal fixation.226
Internal fixation of periarticular fractures has many potential
advantages including direct fixation of articular fragments, early
range of motion of the joint, and avoidance of constrictive dressings
or casts. In a recent prospective randomized trial of 144
intra-articular fractures, internal fixation was found to have superior
results to bridging external fixation supplemented by percutaneous
pinning radiographically and using the Gartland and Werley outcome
score, especially for C2 fractures.156
On the other hand, an earlier study showed significant benefit with
external fixation and percutaneous pinning compared with open reduction
and internal fixation, provided the indirect reduction succeeded using
the Musculoskeletal Functional Assessment as the primary outcome.147
Open reduction and internal fixation of intraarticular fractures has
been considered technically difficult, and a number of soft tissue
complications have been noted with the use of plate fixation.236
has several theoretical advantages. Technically familiar to most
surgeons, the approach avoids the neurovascular structures on the
palmar side. Further, the fixation is on the compression side of most
distal radius fractures and provides a buttress against collapse.
Initial reports of the technique demonstrated successful outcomes with
the theoretical advantages of earlier return of function and better
restoration of radial anatomy than was seen with external fixation.102,108,121,143,218,223
were increasing reports of extensor tendon ruptures because of
prominent hardware, particularly at Lister tubercle.166,168,223,236,273
The more distally the plate is applied on the dorsum of the wrist, the
more proximally the distal screws need to be directed to avoid
articular penetration. This oblique orientation of the screws allows
the distal fragment to displace palmarly. The palmar displacement of
the fragment is particularly problematic because it results in (1)
incongruity at the distal radioulnar joint and (2) prominence of the
hardware dorsally with the tendency for extensor tenosynovitis or
tendon rupture (Fig. 32-28).
allow superior purchase in the distal fragment while permitting screw
placement from proximal to distal, thereby engaging the palmar fragment
and preventing it from collapsing palmarly. Although reports of
successful outcomes with dorsal plate fixation have been reported,
several retrospective studies indicate that there may be a higher
incidence of complications associated with the routine use of this
approach when compared with the palmar approach.213,227
In general most authors agree that the decision of palmar versus dorsal
plate application should be determined by the fracture fragment
displacement rather than routine use of one approach versus another.
longitudinal incision is centered over the fracture in line with the
ulnar aspect of Lister tubercle. The extensor retinaculum is incised in
a z-plasty manner that allows for one limb to be placed over the plate
and the second limb to be repaired over the extensor tendons to prevent
bow-stringing of the tendons with wrist extension. The extensor
pollicis longus tendon is dislocated from its position at the tubercle
and subperiosteal dissection is performed radially and ulnarly. Care
should be taken to preserve all of the dorsal fragments for
re-establishment of radial length. Traction is then applied by either
an assistant or by the use of finger traps with weights suspended off
the end of the table. Care should be taken to ensure that the hand is
not pronated relative to the forearm. The metaphyseal void can then be
filled with graft and the articular surface assessed. In the case of
residual incongruity of the articular surface, the joint may be
directly assessed by extending the periosteal dissection distally, but
care must be taken to avoid injury to the scapholunate interosseous
ligament. Skin hooks can be placed under the capsular flaps and the
articular surface can be visualized and reduced. Generally speaking, it
is preferable to achieve the reduction by supporting the articular
surface with supplemental graft and preventing subsequent displacement
with screws placed through the distal aspect of the plate. If an
arthrotomy is not performed, then the articular surface should be
visualized using a 20-degree inclined fluoroscopy view to assess for
palmar displacement of the lunate facet and screw penetration into the
articular surface. It is critical to ascertain whether the palmar
cortex is aligned and does not displace palmarly with plate
application. It is also advantageous to position the plate such that
the screws are oriented perpendicular to the radial shaft, rather than
directed from distal to proximal (Fig. 30-28C-F).
In cases when there is extensive palmar comminution, supplemental
fixation may be necessary. The addition of K-wires or a screw through
the radial styloid to engage the proximal cortex of the radius is
helpful to prevent palmar collapse.
rupture from prominent dorsal hardware, a number of authors have
proposed using palmar plating, originally reserved for palmar displaced
fractures (Figs. 30-29 and 30-30), for the stabilization of dorsally displaced fractures through a palmar approach (Fig. 30-33).53,61,134,153,157 This technique has gained widespread acceptance;
however, there is a paucity of well controlled prospective trials
documenting clear superiority of this technique. Although the position
of the plate on the side opposite the displacement does not permit a
direct buttress against dorsal displacement, the screw position in the
distal fragment directly buttresses collapse. The addition of locking
fixation of the screws in the distal fragment further prevents dorsal
displacement of the distal fragment. One concern over these locking
plates is the potential for articular penetration with distal plate
position on the palmar surface of the radius. The more distal the plate
placement on the radius, the more the screws need to angle back
proximally to avoid penetration into the lunate fossa (Fig. 30-31).
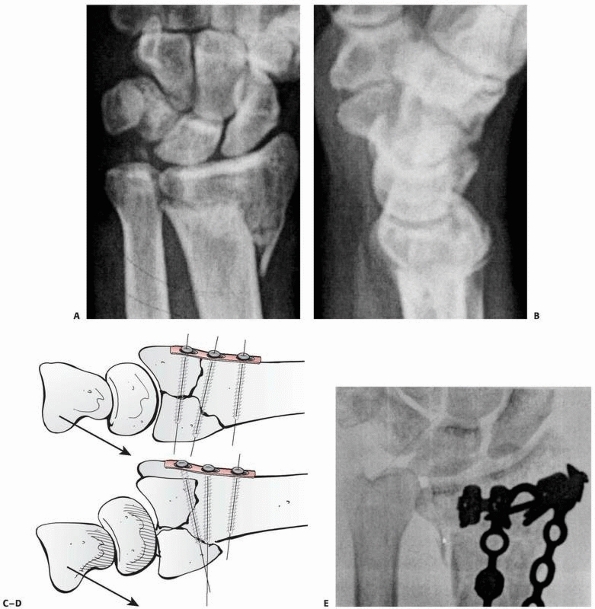 |
|
FIGURE 30-28 Fracture with both palmar and dorsal comminution (A,B). Dorsal plate application permits palmar collapse of the fragment in the absence of an intact palmar buttress (C,D).
The palmar displacement of the metaphyseal fragment relative to the distal ulna results in radioulnar incongruity and loss of rotation (E-G). (continues) |
penetration by the distal screws. This is reported to occur in up to
57% of cases and is a particular risk in osteopenic patients.12,13,61,224 A further complication that has been reported with locked plates is tendon irritation or rupture in up to 38% of cases,6,12,13,61,199,224 which is similar to rates of tendon problems with dorsal plating. Extensor tendon problems can be caused by penetration
of the screws through the dorsal cortex especially in the third dorsal
compartment, bony spurs, or excessive gapping at the fracture site.26
The former cause can be prevented by reducing the measured size of the
central distal screws. Too distal plate placement beyond the
“watershed” has been cited as a reason for flexor tendon damage.12
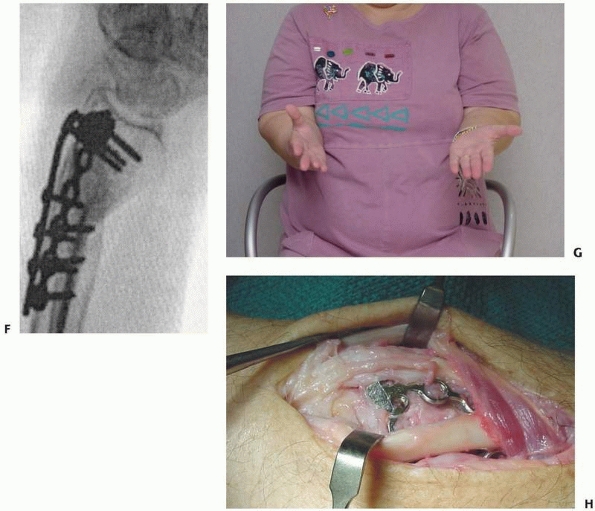 |
|
FIGURE 30-28 (continued)
Furthermore, hardware is now more prominent relative to the extensor tendons, resulting in extensor tenosynovitis and tendon rupture (H). |
plates may be applied through either a flexor carpi radialis
(FCR)/radial artery interval or through a midline flexor tendon/ulnar
neurovascular bundle interval. The FCR/radial artery approach is
preferable for (1) fixation of dorsally displaced fractures with dorsal
comminution and (2) fixation of partial articular fractures (articular
shear fractures). The skin incision is centered over the FCR, with care
being taken to avoid injury to the palmar cutaneous branch of the
median nerve that lies ulnar to the tendon. The radial artery is
mobilized, and dissection is carried radially by releasing the
brachioradialis tendon from the radial styloid. Using this approach,
the comminution on the dorsum of the radius can be visualized and graft
can be placed. Articular depression can also be seen by pronation of
the radius away from the rest of the articular surface. The depressed
articular surface may be visualized from within the fracture site. This
allows for subarticular graft placement. The pronator quadratus muscle
is released from its radial attachment and should be preserved to place
over the plate at the conclusion of the case. The main limitation of
this
approach is in the visualization of the palmar ulnar corner of the radius.
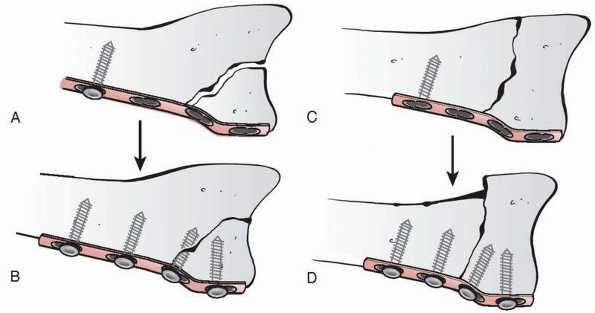 |
|
FIGURE 30-29
Palmar plating. The use of a palmar plate was originally reserved for articular shear fractures. Here use of a palmarly applied undercontoured plate allows compression of the volar lip back to the intact dorsal buttress (A,B). In the absence of an intact dorsal buttress, undercontouring of the plate will result in dorsal displacement of the entire articular surface as shown in C and D. |
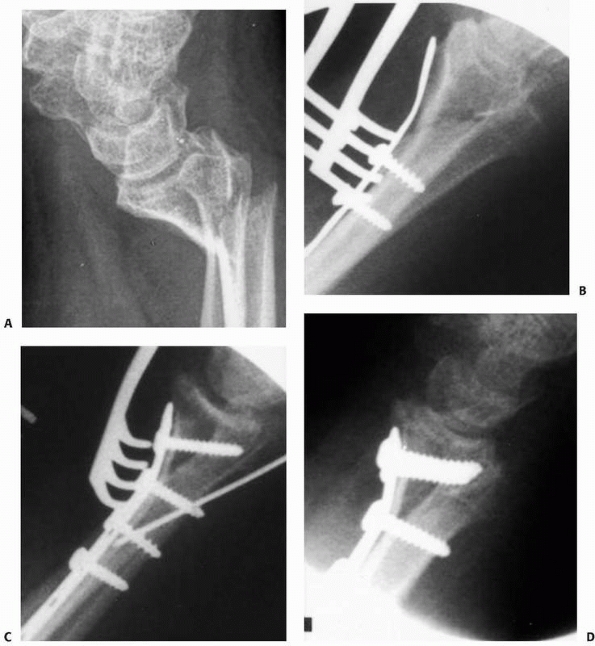 |
|
FIGURE 30-30 Sequential tightening of an undercontoured plate to the distal radius (A,B).
Note that the technique requires an intact dorsal cortex, otherwise the technique will push the distal radius dorsally. To prevent this, a temporary pin may be placed to provide a dorsal buttress while the plate is applied. The pin is then removed after the screws have been tightened (C,D). |
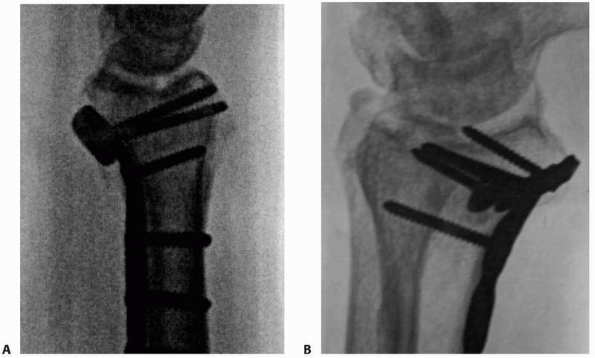 |
|
FIGURE 30-31 A,B.
Palmar plate fixation of a distal radius fracture. Note the anatomy of the volar lip of the radius distally. The more distal the placement of the plate, the more likely is the screw to penetrate the articular surface. |
flexor tendon/ulnar neurovascular bundle interval. The skin incision is
centered over the ulnar border of the palmaris longus, the flexor
tendons are mobilized radially, and the ulnar neurovascular bundle is
taken ulnarly. With this approach the pronator quadratus is released
from the ulna. The incision may be extended distally to release the
transverse carpal ligament, particularly if the patient had any median
nerve symptoms preoperatively. This incision is preferred when the
majority of the comminution is at the palmar lunate facet. Note that
the location of the skin incision does not preclude the surgeon from
developing the interval between the FCR and the radial artery through
the same incision. This incision permits the development of both
intervals if there is any question of the adequacy of the reduction.
to obtain an anatomic reduction. In extra-articular fractures with
dorsal displacement, this can be achieved using the plate. Screws are
placed distally in the plate parallel to the joint surface in the
lateral view, taking care not to penetrate the dorsal cortex. Pronated
and supinated oblique views are useful at this stage to ensure that the
distal screws have not penetrated the radiocarpal or distal radioulnar
joints. The plate is then lying off the shaft of the radius (Fig. 30-32A). The proximal limb of the plate is then gently pushed on to the shaft, the so-called lift technique242 and fixed in place (Fig. 30-32B). This usually reduces the distal fragment in a similar manner to the joystick effect of nonbridging external fixation (Fig. 30-22B).
intermediate columns must be reduced. The first column to reduce is the
one in which the cortex can be anatomically reduced and fixed using a
K-wire. Once the columns have been aligned, the fracture may be fixed
to the palmar plate. First the plate is temporarily fixed to the shaft,
preferably with either a unicortical screw or a screw in a sliding hole
in the plate. The lateral view is useful to determine if screws placed
through the plate are going to penetrate the articular surface. A
combination of traction and palmar flexion usually reduces the
metaphyseal fragment to the plate and then the remaining screws may be
placed (Figs. 30-33 and 30-34).
At this stage, pronated and supinated oblique views must be obtained to
verify that the screws have not penetrated the radiocarpal joint (Fig. 30-34).
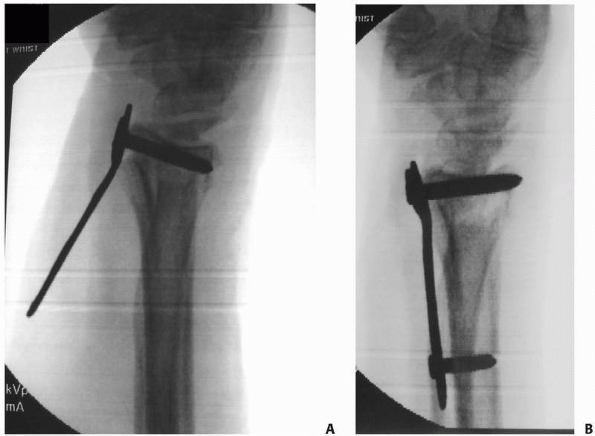 |
|
FIGURE 30-32 A. A volar plate has been applied to the distal fragment only, with the fracture unreduced. B. The “lift” technique. The plate has been pushed gently on to the shaft of the radius, reducing the fracture.
|
wide variety of techniques that may be applied successfully to nearly
every fracture. A dogmatic approach is not appropriate and cannot be
supported by the literature. Evidence that compares different options
indicates that the most important aspect of outcome is to achieve the
radiographic measures of a successful outcome in the least invasive
method possible.
result of a fall on the outstretched hand. The fracture is usually a
lower energy injury and may be considered as either a stable or an
unstable fracture. Stable fractures are characterized by (i) minimal
metaphyseal void with no palmar comminution, (ii) an intact palmar
cortex after reduction, and (iii) good quality bone stock without
osteoporosis or osteopenia secondary to advanced age or metabolic bone
disease.
shortening of the radius relative to the intact ulna and (ii) loss of
palmar tilt at the radiocarpal joint. Shortening of the radius relative
to the ulna during the injury disrupts the distal radioulnar joint
ligaments. Adams demonstrated that shortening of the radius relative to
the intact ulna of more than 5 mm must by definition disrupt the TFCC
or cause avulsion of the ulnar styloid.2
The resultant distal radioulnar joint instability may thus be
responsible for the ulnar sided pain noted in follow-up by several
authors.92,160 Further, the residual shortening results in long-term ulnar impaction syndrome with resultant pain with
ulnar deviation and strong grip. The ability to predict which fracture
will be unstable has been studied extensively. The most consistent
predictors of instability are (1) patient age, (2) degree of
metaphyseal comminution, and (3) the degree of radial shortening (ulnar
variance) at presentation. These factors may be used in an effort to
assess the risk of early and late instability and may prove useful in
counselling of patients regarding surgical versus nonoperative
management.179,180
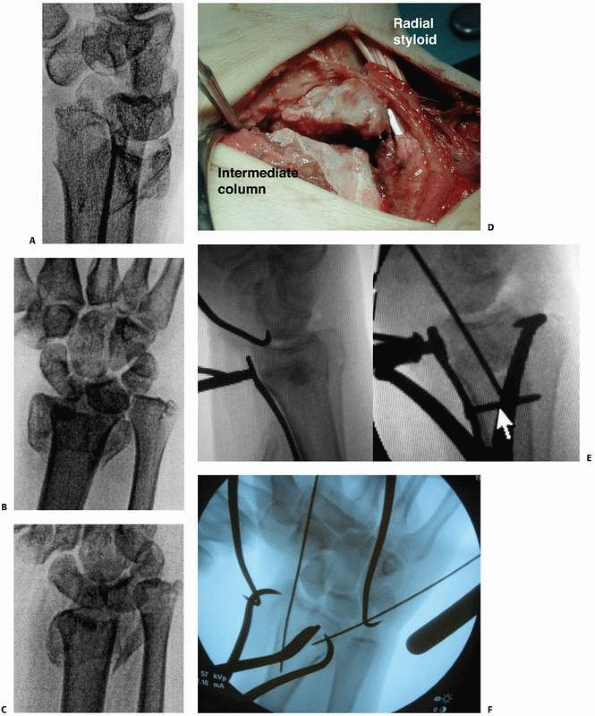 |
|
FIGURE 30-33 A comminuted dorsally angulated distal radius fracture with an associated nondisplaced scaphoid fracture (A-C). The flexor carpi radialis/radial artery interval is used, and the radial and the intermediate columns are reduced and pinned (D).
The plate is first applied to the shaft with one screw placed though the sliding hole. Then the correct proximal/distal location of the plate is determined on the lateral x-ray view. Once the palmar cortex has been reestablished with the plate, then tension and traction will restore palmar tilt. Alternatively, a tenaculum may assist in reestablishing palmar tilt. Gapping between the intermediate and radial columns may be reduced by use of a tenaculum clamp and provisional pinning (E,F). |
treated with either nonbridging external fixation or open reduction and
internal fixation with a palmar locked plate. Bridging external
fixation with augmentation with K-wires can be used where the distal
fragment is too small to accommodate either fixator pins or screws,
which is unusual in older patients.106
Nonbridging external fixation is less invasive than palmar locked
plating and its most common complication (minor pin tract infection)
rarely compromises the final outcome. However nonbridging external
fixation is less useful if the fracture is irreducible closed. This can
occur if there is marked radial shortening with overlap of the volar
cortex or if the surgery is delayed and early healing has occurred. In
this situation locked volar plating is preferred, with care taken to
avoid tendon impingement. In cases with severe osteoporosis and a large
metaphyseal defect, added support with a bone substitute or autograft
is required to prevent collapse around the plate.
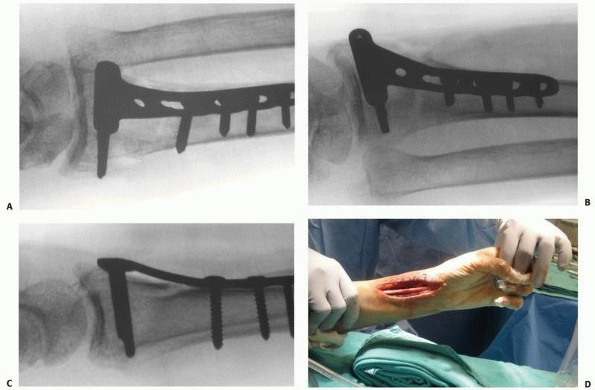 |
|
FIGURE 30-34
It is important to ensure that dorsal cortex and intra-articular screw penetration is avoided with application of a palmar plate. A. Pronation of 60 degrees demonstrates the intermediate column. B-D. The forearm is elevated 20 degrees off the table to obtain a true lateral of the radiocarpal joint. This shows a tangential tangential view of the intermediate column. |
one of the few accepted treatment modalities. Like most partial
articular fractures, the emphasis is on anatomic reduction of the
articular surface and compression across the fracture site to assist in
primary bone healing. Fixation should be sufficiently stable to allow
early range of motion. The ideal fixation is with a palmar buttress
plate that is slightly undercontoured relative to the degree of palmar
flexion of the radius (Fig. 30-34). This plate
not only prevents axial displacement of the palmar fragment, but also
compresses the fragment against the intact dorsal cortex (Fig. 30-29).
fractures with this technique are excellent; however, there are two
potential pitfalls. One is that these fractures represent an impaction
of both the scaphoid and the lunate on the volar lip of the radius. As
such, there may be a nondisplaced fracture line between the scaphoid
and the lunate facets. The implant must
extend
sufficiently ulnarly to stabilize the lunate facet and prevent it from
late collapse. The second pitfall lies in the potential for a
nondisplaced fracture across the dorsum of the radius. Undercontouring
of the plate in this fracture can result in displacement of the entire
articular surface dorsally (Fig. 30-30).130,139
one of the most controversial topics in wrist fracture surgery. The
most critical point in treating these injuries is to understand the
mechanism of the injury and recognize the fragments. Melone emphasized
the role of the lunate in the creation of intraarticular fractures.190
As the lunate impacts on the articular surface, it splits the lunate
fossa into two characteristic fragments with the potential for a third
“central impaction” fracture. The scaphoid impacts on the radial
styloid and results in a shearing force that typically does not split
the styloid into a palmar and a dorsal fragment. When faced with these
fractures, the surgeon is required to identify each fragment and assess
for displacement. Once the fragments have been identified, the decision
must be made whether to stabilize the displaced fragments based on the
fragment size and the degree of the displacement.
displaced articular fragments: external fixation and internal fixation.
The decision over which technique to use may be based in part on
whether direct reduction of the fragments is necessary and feasible
through a closed or percutaneous technique employed with external
fixation. In general, depressions on the palmar articular surface are
difficult to reduce in a closed fashion and often require open
reduction. In this case internal fixation may be preferred as the
surgeon already has the exposure necessary for internal fixation. Each
technique has its advantages and its complications. In an attempt to
directly compare each technique, one group of investigators
prospectively randomized patients between internal and external
fixation. The external fixation group demonstrated superior outcomes
provided that they were able to achieve satisfactory radiographic
parameters at the end of treatment. The authors concluded that the goal
should be to achieve satisfactory radiographic parameters using the
least invasive technique possible.147
In general terms it can be concluded that each individual surgeon will
have a level of comfort for which one technique or the other may be
preferable.
treating a variety of radius fractures; however, it is critical to
understand that certain fracture patterns will require more invasive
techniques. In the case of lunate impaction fractures, the lunate must
be assessed prior to obtaining patient consent. If the lunate facet is
split into a palmar and a dorsal fragment, traction alone may not
reduce the critical volar ulnar corner. The surgeon and the patient
must understand that if indirect reduction of this fragment does not
occur with traction, then direct reduction will be required.
Direct reduction may be performed either through a limited open or an
extensile approach. Smaller fragments may be fixed with wires, whereas
fragments that extend more proximally may require plate stabilization.
Because volar plating may actually address all the components of the
fracture, the surgeon may elect to use a locked volar plate only and
forego external fixation. Because of the multitude of variables,
extensive preoperative planning and templating is critical.
fixator. The preferred method of anesthesia is axillary block; a
tourniquet is used. A 3-cm dorsoradial skin incision is made at the
distal third of the radius. Careful dissection is performed to avoid
injury to the dorsal sensory portion of the radial nerve that emerges
from under the brachioradialis tendon 7.5 to 11.0 cm proximal to the
tip of the radial styloid (Fig. 30-35).
extensor carpi radialis brevis and longus. This position places the
extensor carpi radialis longus (ECRL) between the pin and the sensory
branch of the radial nerve. Predrilling and hand placement of the pins
may prevent overheating of the cortical bone and subsequent pin site
problems. To avoid interference with thumb retroflexion, the distal
pins should be placed 45 degrees off the sagittal plane at the adductor
tubercle of the index metacarpals. The fracture is then reduced
manually in the following sequence: (1) longitudinal traction is
applied to achieve radial length and the fracture is assessed for the
presence of a metaphyseal defect, (2) palmar translation (not palmar
flexion) of the carpus, and finally (3) ulnar deviation. If there is
evidence of significant radioulnar instability, the fracture is reduced
in supination to avoid displacing the radial metaphysis palmar to the
distal ulna as ulnar deviation is applied. The most critical element
to
this technique is to align the palmar cortex anatomically on the
lateral view. It is especially useful to incline the radius 15 degrees
to 20 degrees to the fluoroscopy beam to check the alignment. In order
to prevent collapse during healing and permit early removal of the
external fixator, the metaphyseal void may be filled with a bone graft
or a bone graft substitute at this time. It may be useful to
temporarily overdistract the fracture to enlarge the defect. The
majority of graft substitutes do not permit complete packing of the
defect and thus some temporary over distraction will allow better
filling of the void. As traction is decreased, the material will be
compacted. The metaphyseal comminution permits “opening” of the
fracture through a 2-cm wound dorsally immediately proximal to the
fracture. Small right angle retractors may facilitate exposure of the
thin metaphyseal dorsal cortical fragments. One or more of these
fragments may be removed after marking its distal aspect with a marking
pen to indicate its correct orientation for reinsertion. This opens the
fracture and exposes the metaphyseal defect to allow irrigation of the
clot from the fracture site. For extraarticular fractures the graft is
packed radially and distally, with care being taken to avoid
displacement of the palmar cortex.
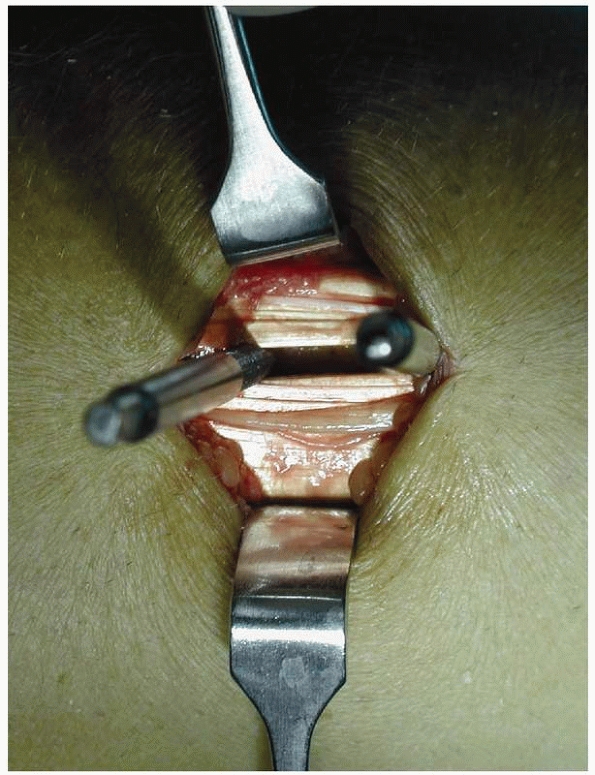 |
|
FIGURE 30-35
Pin position between the extensor carpi radialis longus and brevis. Note the proximity of the dorsal sensory branch of the radial nerve. Iatrogenic injury to this nerve is a frequent cause of neurogenic pain after external fixation and may be minimized by open rather than percutaneous pin insertion. |
is critical in external fixation of most compression fractures,
particularly those with a central impaction component. After irrigating
out the clot, a tamp can be used to gently elevate the compressed
segments. Start palmarly and work dorsally. It is theoretically useful
to elevate some of the native cancellous bone up with the fragments to
create a uniform subchondral surface for the intermediate column. The
supplemental graft can then be packed in the resultant defect. The
dorsal cortical “window” can then be replaced, with care being taken to
create a smooth surface for the extensor tendons.
critical to evaluate the lunate facet on the inclined lateral view with
traction in place. If traction fails to reduce the palmar facet, then
direct reduction will be required through an open rather than a
percutaneous approach.
radial column may be reduced with longitudinal traction and slight
ulnar deviation. The radial column is stabilized using two
percutaneously placed 0.45- or 0.62-inch Kirschner wires. Once the
radial column is out to length, the lunate fossa may be pinned in a
reduced position. If there is minimal comminution, a large tenaculum
clamp may be placed percutaneously between the dorsal ulnar corner and
the newly fixed radial column. In some cases where there is residual
depression of the lunate, percutaneous elevation may be required. After
verifying that the lunate fossa is out to length and that there is no
step-off between the scaphoid and the lunate facets, transverse wires
may be placed under the subchondral surface.
radial column again is reduced first. The lunate fossa should then be
assessed on a tilted lateral view. If the palmar lunate facet is
reduced following grafting and application of traction, transverse
subchondral wires may again be placed, with care being taken to direct
at least one of the wires to support the palmar lunate facet.
still depressed after application of traction and placement of graft
material, a direct reduction is performed. A skin incision is placed
longitudinally at the ulnar aspect of flexor tendons but radial to the
ulnar neurovascular bundle. The flexor tendons are retracted radially
and the ulnar neurovascular bundle is retracted ulnarly to expose the
critical palmar ulnar fragment. If the fracture lies distally and does
not involve the thick cortical support of the lunate facet, then the
fragment may be fixed with two Kirschner wires, leaving the wire
emerging dorsally for later removal. The more common fracture pattern
results in extension below the level of the sigmoid notch. The proximal
extension typically results in a triangular shaped fragment of cortical
bone that will require buttress fixation using a plate-screw construct.
If the surgeon plans to leave the external fixation in place and the
radial column is well stabilized, then a small 2.0- or 2.4-mm plate may
be applied to the intermediate column.
that the dorsal lunate facet is out to length when the distal screws
are placed. Failure to reduce the dorsal lunate facet will result in an
intra-articular step-off as the distal screws are placed. Once the
intermediate column is fixed, then the radial side is reassessed to
make sure that there is no step-off. The radial pins may need to be
readjusted to reflect the reduced position to the intermediate column (Fig. 30-33).
or greater, it becomes even more critical to support the articular
surface with bone graft or a bone graft substitute. Placing the graft
from the dorsum may result in the ability to restore a relatively
congruous articular surface from below.
evaluate for displacement of the palmar radial and ulnar facets. The
central impaction fragment may be reduced percutaneously from the
dorsal side using the subchondral graft and wires, although the palmar
articular facets remain a problem. If tilted radiographs reveal
displacement palmarly, then the surgeon should make a limited or an
extensile palmar approach. After stabilization of the intermediate
column with a small buttress plate, lateral radiographs may still
reveal some articular step-off palmarly, which reflects the split in
the radial styloid. The radial column is visible through the midline
incision, but it may not be stabilized by a smaller 2.0- or 2.4-mm
plate buttressing the lunate facet. At this time the surgeon can either
apply a more conventional “T” plate or maintain the reduction with
percutaneously applied K-wires exiting radially.
avoid the loss of palmar tilt and radial length following external
fixation, several authors have recommended supplemental fixation with
or without the use of adjunctive bone graft.64,237
On completion of the fixation it is critical to evaluate the tension in
the extrinsic extensor tendons by assessing passive metacarpophalangeal
motion. Overdistraction results in excessive tension on the digital
extensors. The metacarpal phalangeal joints may be passively
flexible,
but with excessive tension the digits “spring” back into extension when
the digit is released. If there is any doubt, the traction can be let
off and the passive motion reassessed. If the motion is improved after
releasing some distraction, fixation should be secured in this position.
fractures is determined by the location and degree of displacement of
the intra-articular component and the degree of comminution. In general
terms, for fractures that are primarily comminuted either palmarly or
dorsally, the most direct approach may be performed. When the
comminution involves both the palmar and the dorsal cortices, the use
of a palmar locked plate is preferred. Rarely comminution extends very
distally on the dorsal margin of the distal radius fracture. In this
case the purchase of the locking screws applied from the volar surface
may not provide adequate purchase, particularly in the dorsal lunate
facet. In this case the surgeon may need to stabilize this fragment
with an external fixator or one of the smaller plates, which may be
applied through a separate incision between the fifth and sixth dorsal
compartments.
postreduction films to determine the approach and the implant
selection. AP, lateral, and oblique radiographs following reduction
should be viewed to determine any displacement of the radial styloid
and the palmar and dorsal lunate facets. Any uncertainty about central
impaction is assessed with computerized tomography. Typically the
intermediate column is assessed for residual displacement first.
Residual displacement of the palmar lunate cortex should be addressed
with palmar plate. Comminution of the intermediate column should be
addressed first and then the displaced palmar lunate cortex should be
approached through the flexor tendon/ulnar neurovascular bundle
interval (Fig. 30-36A,B). Residual displacement of the radial styloid should be addressed with a separate plate or with percutaneous wires (Fig. 30-36C-F).
For residual dorsal displacement with the palmar cortex reduced, a
dorsal approach to the intermediate column should be used, with an
incision between third and fourth compartments (Fig. 30-37A,B). Separate fixation of the radial column may be needed to avoid dorsal impingement at the Lister tubercle (Fig. 30-37C-E).
fractures, and ulnar styloid fractures serve as markers of high energy
ligament injuries about the wrist.
high incidence of scapholunate ligament injuries in younger patients;
the scaphoid displaces relative to the lunate. A shear injury between
the two bones ruptures the scapholunate interosseous ligament.
Treatment should be geared toward the ligamentous injury and include
stabilization of the radial styloid. For acute injuries, a dorsal
ligament repair with reattachment of the dorsal extrinsic ligaments may
be performed. A cannulated screw or K-wires may be used to stabilize
the fracture.
size of the fragment relative to the remaining portion of the lunate
facet. Smaller ulnar sided fragments are indicative of a distal
radioulnar joint injury, and treatment may be geared toward reduction
and stabilization of the distal radioulnar joint. Larger fragments are
indicative of true palmar radiocarpal instability and should be
assessed for residual palmar displacement of the lunate relative to the
radiocarpal joint.46,198,241,252
Stabilization of these fragments may be difficult. Smaller fragments
may be neutralized by placing a wire through the fragment and through a
drill hole in the radius. The fragments are then sutured to the radius.
Larger fragments may be fixed with a plate screw construct. As these
fragments represent the insertions of the volar extrinsic ligaments,
there is a growing trend to repair, rather than excise, these
fragments. External fixation may be required to stabilize the
radiocarpal joint.
indicators of a variety of ligamentous injuries. In one review of 20
fractures of the dorsal articular margin the authors confirmed that
these injuries result in substantial injury to the volar extrinsic
ligaments and frequently include avulsion fractures of the volar lip of
the radius. In addition, there is frequently a component of impaction
with these injuries, and computerized tomography may prove of benefit
to assess for impaction of the articular surface before operative
management.167
of the radius, then both the radiocarpal joint and the scaphoid should
be assessed for stability. External fixation may be used to stabilize
the radiocarpal joint and percutaneous pinning may be used to fix the
intercarpal instability.
It is well accepted that the distal ulna is a common source of symptoms
after injury. The disability that arises directly from the fracture
versus the associated injury to the triangular fibrocartilage complex
remains controversial.92,136,222
Adams documented in cadaver studies that displacement of the radius
relative to the ulna of 5 mm or more must result in a fracture of the
ulna styloid or a disruption of the TFCC.2
The disruption may occur at the base of the ulnar styloid, the ulnar
insertion of the distal radioulnar ligaments, or the radial insertion
of the TFCC complex.
controversial. Although it is accepted that displacement of the radius
results in acute disruption of the joint, whether these injuries
require treatment is unknown. Lindau documented that persistent
radioulnar instability was a risk factor for a poor outcome independent
of radiographic appearance. Clinically apparent instability was present
in 26 of 76 patients at 1 year postinjury. Instability of the distal
radioulnar joint was associated with a worse wrist score and doubled
the score on the visual analog pain scale.164
Although fixation of the ulnar styloid and or repair of the TFCC has
been reported to have good outcomes, it is uncertain as to which
injuries require acute repair.229,238 The indications for treatment of ulnar styloid fractures is evolving.
Currently a fracture at the base of the ulnar styloid with both
significant displacement and gross palmar dorsal translation of the
radius relative to the ulna represents an indication for treatment.
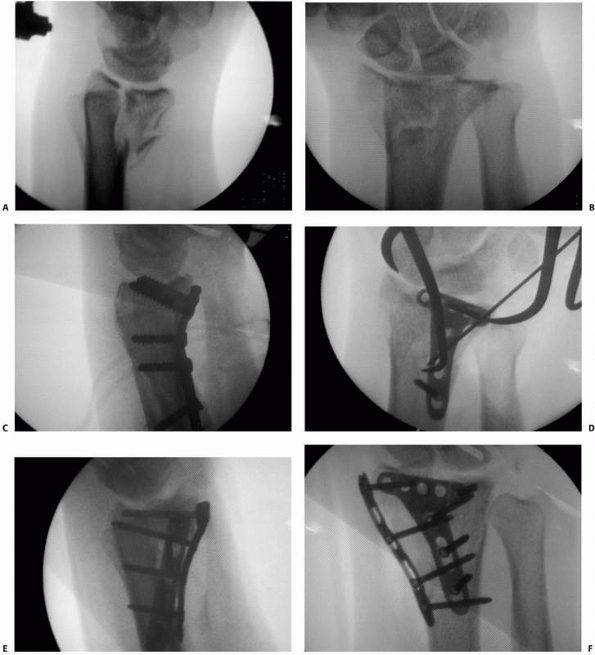 |
|
FIGURE 30-36 Lateral and PA fluoroscopy views (A,B)
after reduction in traction of a highly comminuted intra-articular fracture. Note that the dorsal cortex comes out to length whereas the palmar cortex remains displaced. Following application of a palmar plate, there still remains some residual comminution of the radial styloid (C,D). The radial styloid (particularly distally) may require adjunctive fixation with either a second plate or K-wires. For this case a separate radial column plate was used to create the final construct (E,F). |
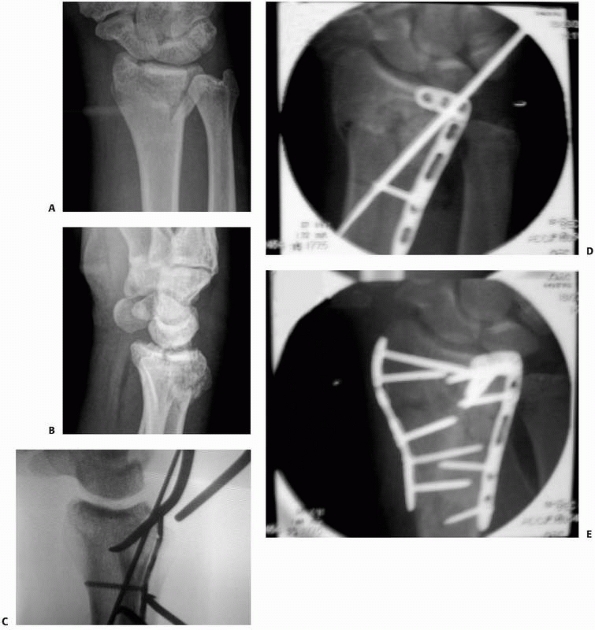 |
|
FIGURE 30-37 Residual displacement of the dorsal intermediate column (A,B)
can be addressed through a dorsal approach. The intermediate column is stabilized and then the radial column is assessed for palmar displacement and rotation (C,D). If necessary, a second radial plate is applied (E). |
styloid fragment that may appear to be lined up in the AP plane;
however, when the lateral view is examined, the styloid fragment is
actually displaced palmarly in relation to the distal ulna. Often this
problem is only recognized late when the patient has difficulty
achieving wrist supination either actively or passively. The treatment
for such a displaced fragment both acutely and subacutely is
reattachment of the styloid to the distal ulna.
incision over the extensor carpi ulnaris. Transverse branches of the
ulnar nerve are preserved. Often the extensor carpi ulnaris subsheath
is still attached to the fragment. The fragment typically will reduce
with supination of the wrist and will displace with pronation. It is
helpful to maintain the wrist in supination while repairing the styloid
to the distal ulna. For large fragments the simplest and most secure
fixation may be with a cannulated headless screw. For smaller
fragments, 0.28-inch K-wires and a 24-gauge tension band may be
applied. Care must be taken to bury the hardware, as it is often
prominent in this region and may require removal later.
Reattachment of the ulnar styloid alone may not result in restoration
of stability in this situation. Therefore it is critical to reassess
the stability of the DRUJ following repair of the styloid.
distal radioulnar joint by supinating the forearm. Immobilization of
the wrist in supination allows the soft tissue to heal in a reduced
position and may prevent late instability of the radioulnar joint (Fig. 30-38).
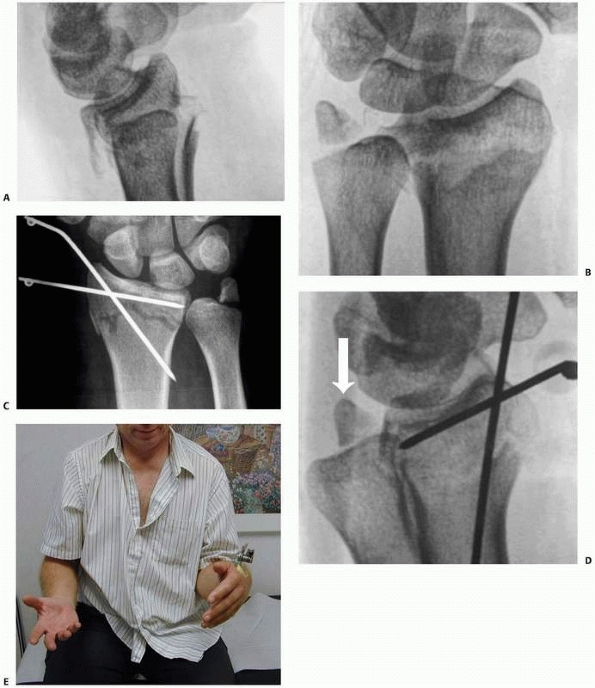 |
|
FIGURE 30-38 Characteristic fracture of the ulna styloid associated with late instability. A,B. Intra-articular fracture with shortening. There is a displaced fracture at the base of the ulnar styloid. C-E.
The radiographic and clinical appearance of the patient’s wrist 2 weeks after external fixation in the clinic. Note that the patient is unable to supinate because of the dorsal displacement of the ulna relative to the radius. Radiographically, there is the characteristic palmar position of the ulna styloid relative to the remainder of the ulna. (continues) |
In one report of 320 fractures the distal ulnar metaphysis was
fractured in 7% of cases, with the most common fracture pattern being
an extra-articular fracture of the ulna metaphysis. Although
nonoperative management may be successful, care should be taken to
immobilize the radioulnar joint in a reduced position and look for
radiographic evidence of impingement. Late heterotopic bone formation
is common and will result in significant loss of rotation with this
fracture pattern.
components of several of the other fracture types. These injuries
characteristically (1) are high energy, (2) have significant
comminution often with proximal extension, and (3) may have significant
soft tissue injuries. The management of these injuries is often complex
and may require several steps. It is useful to manage them in a
stepwise fashion by first achieving rigid skeletal stabilization and
then addressing the soft tissue injuries.
managed with a palmar plate. Using external fixation for the diaphyseal
component will result in significant collapse prior to fracture union.
Dorsal plates often will impinge where they intersect, thus a palmar
locking plate is preferred. When there is also extensive distal
comminution, then hybrid fixation may be necessary. In this case a
palmar plate is applied, and a dorsal external fixator may be used to
neutralize the displacement through the distal comminution. Extensive
grafting may be necessary in order to prevent late collapse.
 |
|
FIGURE 30-38 (continued) F,G. Appearance of the radius and the ulna after repositioning of the wrist in supination and maintaining it in this position. H,I. Final radiographic appearance at 2-year follow-up. The patient regained full pronation and supination.
|
has occurred, it is generally the result of extreme shortening of the
fractured radius relative to the intact ulna. In these cases
exploration reveals that the ulna has been stripped of the insertion of
the DRUJ ligaments and the ulnocarpal ligaments. In some cases with an
associated large ulnar styloid base fracture, those ligaments may still
be attached to the base of the ulnar styloid. Stability may be restored
by repairing the ulnar styloid base back to the shaft of the ulna,
fixing it with either a headless screw or a tension band wire
construct. In cases in which there is no associated ulnar styloid base
fracture, the ligaments may reapproximate to the ulna provided that the
DRUJ is reduced. For this reason, in patients with obvious DRUJ
instability and no large ulnar styloid fracture, the patient should be
immobilized in supination to reduce the DRUJ for 4 weeks before
permitting forearm rotation.
interosseous and distal radioulnar ligament injuries occur in
association with both metaphyseal bending and intra-articular fractures.
50% of all intra-articular distal radius fractures in younger patients
and
varies by fracture pattern.93,162
Geissler graded these injuries as follows: Grade I injuries have
attenuation or hemorrhage of the ligament. Grade II injuries have
incongruity of the ligament from the midcarpal portal, and the probe
may be inserted between the bones. Grade III injuries show an
incongruity from both the midcarpal and the radiocarpal portals, and
the probe may be passed all the way through the articulation. Grade IV
injuries have gross instability with manipulation, and the arthroscope
(2.7-mm) may be passed from the radiocarpal to the midcarpal joints.
They are seen most frequently in fractures that result in significant
displacement of the lunate facet from the radial styloid (Fig. 30-39).
injuries, the natural history of these soft tissue lesions remains
controversial. In one study of 51 patients with distal radius
fractures, there were a total of 10 grade III scapholunate ligament
injuries. The authors found at 1-year follow-up that 6 patients had
radiographic evidence of dissociation and an increased scapholunate
angle and that this may be associated with SL pain at follow-up.84
In a second study examining 76 patients following fracture,
radiographically apparent scapholunate instability was not associated
with either pain or functional impairment.164
In a purely radiographic study of 95 fractures, dissociative
ligamentous lesions were seen in 40 patients, of which 24 were noted to
progress at 1-year follow-up. The results of this study again found no
correlation between radiographic evidence of instability and symptoms
at 1 year.152
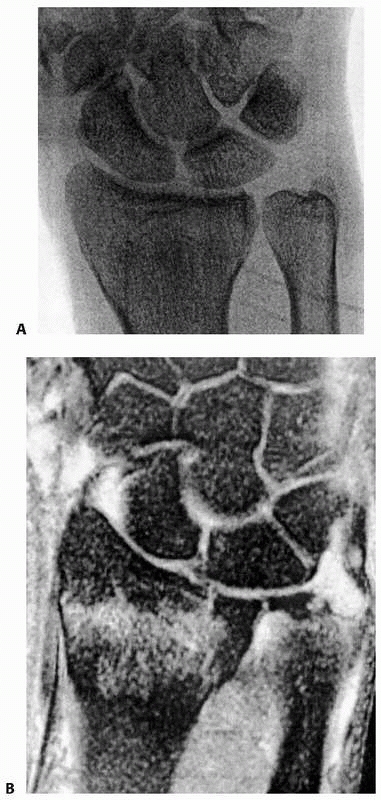 |
|
FIGURE 30-39 A,B.
Minimally displaced lunate impaction fracture with disruption of both the scapholunate interosseous ligament and the triangular fibrocartilage complex. |
The majority of these lesions are peripheral avulsions, generally from
the ulnar insertion compared with fewer central perforations. These
lesions may occur with or without fracture of the ulnar styloid. In
contrast to the interosseous ligament injuries, peripheral avulsions of
the TFCC appear to be more likely to be symptomatic at short term
follow-up. Lindau documented that 10 of 11 peripheral avulsions of the
TFCC had DRUJ instability and worse outcome scores than other
ligamentous injuries at 1-year follow-up.164
Repair of these injuries acutely has been documented to restore
stability and provide excellent results, yet the indications for acute
repair have yet to be elucidated.229
orthopedics where excellent prospective randomized studies have been
performed.* Although these important studies remain
excellent examples of outcome studies designed to answer a significant
clinical question, they have also raised several important questions
regarding the outcome of these fractures. Recent data suggests that
patient related outcomes may vary markedly from physician related
scores. Catalano et al reported on a significant discrepancy between
radiographic appearance of the radiocarpal joint and patients’ self
reported outcomes at 7 years following operative intervention.42
Several studies have indicated that perhaps one explanation may lie in
the soft tissue injuries to the intrinsic ligaments of the carpus, with
a resultant shift in carpal alignment or to associated trauma to the
TFCC.102,160,162,164
been appreciated over the past 5 years. Recent evidence indicates that
patient factors that are not associated with the injury or its
treatment play a significant role in patient related outcome scores. In
one comprehensive review of patients with successful volar plate
surgery, the only variables associated with patient related scores were
age and income.48 Perhaps most
significantly, the impact of patient’s underlying psychological
diagnoses may play a significant role in patient related outcome
scores. Symptoms such as depression, anxiety, and pain correlate
strongly with self reported outcome scores, thereby further confounding
outcome studies.
fractures of the distal radius often are difficult to assess as to
whether the complication was a sequela of the fracture or a
complication of the technique employed to treat the fracture. Certainly
there are complications that may be associated with a given technique,
such as pin tract infections associated with external fixation, but
other complications such as complex regional pain syndrome (CRPS) or
stiffness of the wrist or digits may be difficult to ascribe to one
technique versus another. With the recent enthusiasm for palmar plates
there is an effort being made to define the complications associated
with one technique versus another. In addition, one study indicated
that although palmar plating had a lower incidence of hardware related
complications than dorsal plates, there may be a higher incidence of
hardware collapse.224
continues to be a significant complication following nonoperative
management. In addition, as the number of operatively treated cases
increases, so too does the incidence of collapse and malunion seen in
previously treated fractures. The effect of radial malunion has to be
taken into consideration when considering treatment options. Malunion
of the radius results in alterations to (1) the radiocarpal joint, (2)
the midcarpal joint, and (3) the radioulnar joint. The effect of these
changes can be significant with regard to both immediate functional
impairment and the development of late degenerative changes.
radiocarpal mechanics. First, the loss of palmar tilt shifts the carpus
distally on the radius, thereby increasing contact stress on the dorsal
lip of the radius. In addition, the loss of radial inclination results
in increased stress at the radiolunate articulation.206,208,210 The increased contact stresses result in a higher likelihood of degenerative changes.144 Functionally, the shortening may account for the loss of grip strength that has been observed after malunion.210
There is also evidence that there is a functionally significant loss of
motion at the radiocarpal joint after malunited extra-articular
fractures.137 Finally, the extended
position of the lunate and the scaphoid may result in a compensatory
collapse at the midcarpal joint (see Fig. 30-8).195
significant change in contact stresses at the radiocarpal joint. Note
that depression of the lunate facet results in significant increases in
the contact forces at the radioscaphoid articulation. Clinical studies
indicate that 2 millimeters of lunate depression results in
degenerative changes and worse functional outcomes.142,144,196
has received significant attention. Dorsal angulation results in
increased strain on the radioulnar ligaments.19,37,62,109,197,234
Because of this increased strain, increased force is required to
achieve full rotation of the forearm. Loss of rotation in these cases
seems to occur at approximately 30 degrees loss of palmar tilt. By
contrast, in cases of severe angulation with significant shortening,
the same loss of rotation is not seen. One explanation offered for this
contradiction is that in cases of severe deformity, there are no longer
any attachments of the distal radioulnar ligaments to constrain the
joint. Unconstrained by soft tissue attachments, the joint enjoys its
full mobility.19,37,62,109,197,234
Cadaver studies have not examined the additive effects of radial
shortening and loss of tilt and associated ligamentous injuries. Most
surgeons perform corrective osteotomy for symptomatic malunion, with
the commonest symptoms being DRUJ pain with or without contracture,
midcarpal pain, carpal tunnel syndrome, or weakness of grip.177
In one review of 23 intrarticular malunions treated with corrective
osteotomy, the indications were (1) dorsal or palmar subluxation of the
radiocarpal joint or (2) articular incongruity of greater than 2 mm on
the AP radiograph,211 although in
general terms it is difficult to recommend surgical treatment of an
asymptomatic deformity. Likewise, correction of the deformity has to
offer a high likelihood of alleviating the patient symptoms.
early as the surgeon and the patient agree that there is a plateau in
the patient’s improvement. At one time there was a feeling that the
osteotomy should be delayed until the fracture callus had completely
incorporated. This practice is probably not necessary, because taking
down the callus and internal fixation may be technically easier and not
require bone graft when done before the fracture is healed.129
three-dimensional one, standard PA and lateral radiographs of both
wrists are considered adequate for planning the osteotomy. The
contralateral view is critical for assessing the radial length, radial
inclination, palmar tilt, and carpal alignment. Special attention must
be paid to the distal radioulnar joint to assess for congruency of the
distal radioulnar joint and for potential arthritis of the distal ulna,
which may require an associated resection.
preferred when the distal radioulnar joint can be salvaged, and a
closing wedge osteotomy is preferred with an associated hemiresection
of the ulna when the DRUJ cannot be reconstructed. For an
intra-articular osteotomy, computerized tomography with
three-dimensional reconstructions may be necessary to determine the
location of the intra articular step-off in both planes. Finally,
computerized tomography with superimposition of the proximal forearm
may also be useful for the correction of rotational deformity.
three components: (1) loss of radial inclination, (2) loss of palmar
tilt, and (3) pronation of the fracture fragment. The surgical
technique is dependent on the location of and the degree of the
deformity.
deformity. Typically an opening wedge osteotomy is performed and a
corticocancellous graft is placed. It is notable that with the use of
more rigid implants, it may be satisfactory to use cancellous graft
alone.72 Stabilization of the osteotomy has been described using K-wires, dorsal plates, palmar plates, and external fixators.* Regardless of the method of stabilization, the goal is to
correct the deformity and achieve early union. In general, a
trapezoidal defect is created after the osteotomy and correction of
both the palmar tilt and the radial inclination. The void is filled and
the bone is stabilized. Rotation is verified before fixation of the
osteotomy.
approached via a palmar approach. An associated carpal tunnel release
should be strongly considered if lengthening is to be achieved. The
osteotomy is again done at the previous fracture line. If radial
inclination has been lost then the FCR/radial artery approach allows
opening of the radial column and release of the contracted
brachioradialis tendon. A corticocancellous graft is inserted and a
palmar plate is applied. It is critical to recognize that an apex
palmar angulation is often associated with dorsal displacement of the
ulna relative to the radius, leading to loss of rotation. Restoration
of rotation must be assessed before finalizing the position of the
distal fragment relative to the proximal diaphysis. The results of
osteotomy to correct palmar angulation have been reported, with
restoration of rotation being better than the restoration of extension (Fig. 30-40).165
 |
|
FIGURE 30-40 Palmar malunion following dorsal plating and collapse (A,B).
Note the position of the ulna relative to the radius in the lateral plane. Although dorsiflexion was limited, the patient’s chief complaint was loss of supination (C,D). |
what the patient is seeking from the procedure from both a symptomatic
and a functional perspective. It is important to note the preoperative
range of motion, as some loss of the total arc of motion may be
expected. Because extension is typically more critical than flexion,
the surgeon may wish to template the wrist to a neutral palmar tilt
rather than to an anatomic 12 degrees of palmar tilt.
radioulnar joint. It is important to note the presence of significant
deformity or loss of articular cartilage on the distal ulna, which may
preclude salvage of a reasonably functioning radioulnar joint.
Computerized tomography may be indicated to assess the potential for
salvage of the distal radioulnar joint.
substitute to fill the defect after the deformity is corrected. Options
include autograft, allograft, or a variety of substiutes. In general,
the use of fixed angle devices through a palmar approach
is
perceived as sufficiently stable to permit the use of allograft or
substitutes, whereas prior studies espoused the use of autograft. If
the distal radioulnar joint is not salvageable in frail elderly
patients, consideration should be given to using the distal ulna as a
graft to avoid the need to harvest one from the iliac crest. If salvage
of the DRUJ is precluded, then complete restoration of radial length
may not be as important as correction of the tilt in the sagittal
plane. Restoration of palmar tilt requires a triangular graft, whereas
restoration of overall radial length may require a trapezoidal graft.
adjunctive procedures that may be required in order to achieve a
satisfactory outcome. Carpal tunnel symptoms preoperatively may be
exacerbated by an acute change in the length of the radius or by
swelling in the carpal canal.34
Although an opening wedge osteotomy may actually alleviate the
deformity that causes the carpal tunnel symptoms, it is critical to
consider whether the patient will tolerate the acute swelling and
lengthening of the nerve associated with an osteotomy.151 Decompression of the nerve associated with correction of the deformity may prevent an acute carpal tunnel syndrome.
with the patient preoperatively. In templating the deformity, we are
increasingly relying on tomography to assess the deformity in multiple
planes. These deformities are three-dimensional, and the surgeon should
have a low threshold for obtaining CT scans with reformatted images to
look for significant rotational deformity and the presence of
significant arthritis in the distal radioulnar joint. (Fig. 30-41)
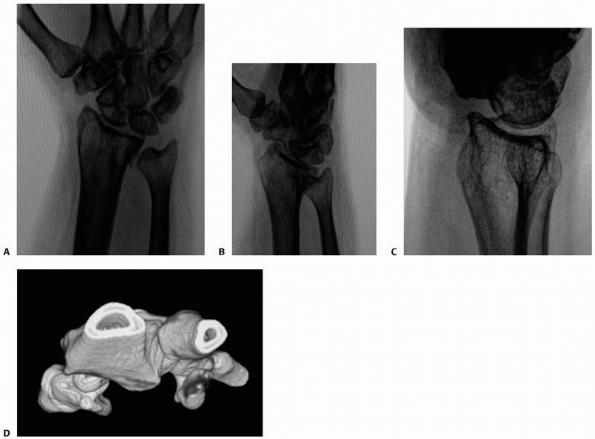 |
|
FIGURE 30-41 A-C. Typical malunion of the distal radius. The radius is collapsed dorsally. D. CT reconstruction demonstrates that the ulna is subluxated dorsally.
|
side, which is dorsal in most cases. A longitudinal approach is
performed and the extensor retinaculum is preserved to permit later
coverage of the plate. In cases of long-standing deformity or when
significant shortening has occurred, it is critical to release the
brachioradialis from its insertion on the distal radius. A z-plasty can
be performed if preoperative templating reveals the need for hardware
distally over the styloid; however, this is usually unnecessary and the
tendon may be left to heal back to the styloid. It is also helpful to
visualize the dorsal ulnar corner of the radius and assess the distal
radioulnar joint directly for articular changes that could preclude
salvage or require further DRUJ procedures.86
inserted proximal (preferably proximal to the proximal extent of the
plate) and perpendicular to the radial shaft. A second pin is placed
distally in the radial metaphysis parallel to the articular surface. In
the case of severe or long term deformity, it is helpful to use
terminally threaded pins from a small external fixator. Once the
osteotomy has been performed, the fixator can be
used
to maintain the radius in the reduced position while the bone graft
and/or the plate is applied. An oscillating saw is then used to cut the
bone. It is significant here again to assess whether correction should
be limited to palmar tilt or should include correction of radial length
and inclination as well. If the correction is for palmar tilt, then it
is easier to leave the palmar cortex intact and hinge the distal
fragment on the cortex. If correction of length is to be achieved, then
the osteotomy must be completed. In this situation the addition of the
external fixator is particularly helpful. The graft material is
harvested, preferably from the iliac crest graft, particularly when
radial length is required. In elderly patients or when the distal
radioulnar joint is not salvageable, the ulnar head may be harvested
and inserted in the defect; however, it is generally not sufficient for
complex deformities. Preoperative templating may now be confirmed
visually by directly measuring the defect when the pins are made
parallel on the lateral plane. The iliac crest graft is harvested with
an oscillating saw, matching as precisely as possible the measurements
of the defect.
applied. In the case of a trapezoidal graft to correct radial length,
it may be helpful to maintain its position with crossed wires to
prevent displacing the distal fragment proximally when the plate is
applied. Once the plate has been applied and the position confirmed
radiographically, the retinaculum may be closed over the plate and the
wounds closed. The length of immobilization is determined by the
stability of the construct and the distal radioulnar joint (Fig. 30-42).
volar locking plates to stabilize the osteotomy. The technique is
similar, with placement of pins to verify the correction of the
deformity. An extensile FCR radial artery approach may be used, which
allows the osteotomy to be performed from the radial column to the
intermediate column. Alternatively, a 2.5-cm incision may be made
dorsally at the osteotomy site and the saw may be used to cut the bone,
leaving an intact palmar hinge. The void may then be filled with
cancellous graft. Case cohort series indicate that this technique may
obviate the need for tricortical graft because of the perceived
strength of the palmar locked plates.185
This technique had the advantage of being minimally invasive with a
short transverse dorsal skin incision and of obviating the need for
hardware removal. Corticocancellous graft is used to allow removal of
the fixator after 6 weeks. This technique achieves excellent correction
of the deformity and improvement in all functional indices except
extension.177
interval that is followed is generally the FCR radial artery approach.
The incision is taken down to the volar carpal branch of the radial
artery. The pronator quadratus is detached and preserved to lie back
down over the plate. A pin may be placed perpendicular to the articular
surface and a second pin perpendicular to the proximal shaft. The
osteotomy may then be performed and the articular surface may be
manipulated back to the appropriate degree of tilt. In general, a small
corticocancellous graft enhances the stability, but is not always
necessary. A palmar plate is applied (Fig. 30-43).
incongruity at the distal radioulnar joint may not be amenable to an
osteotomy of the distal radius or demonstrate residual radial
shortening after corrective osteotomy. In these cases the treatment is
directed at the distal ulna in an effort to either restore congruity
(i.e., an ulnar shortening osteotomy) or to salvage function (i.e.,
arthroplasty).
significant loss of palmar tilt or radiocarpal incongruity, it is
preferable to perform an ulnar shortening osteotomy rather than a
radial lengthening.86 The procedure,
performed through a longitudinal approach to the ulna and fixed with a
dynamic compression plate, has been extensively reported for ulnar
abutment syndrome (Fig. 30-44).86,117,205,220
Contraindications to the procedure are: (1) ulnar translation of the
radial metaphysis in association with the deformity, as shortening of
the ulna results in excessive contact at the distal radioulnar joint;
and (2) excessive palmar tilt of the
radius, as shortening of the ulna will still leave the ulna dorsally
displaced relative to the radius. In cases where the radial length has
been restored but there remains DRUJ contracture or pain, an excisional
arthroplasty (Bower procedure) of the DRUJ can be successful.86
structures at the wrist may be classified as those injuries that
occurred at the time of the fracture and those that arise late as a
result of swelling, scarring, or deformity.
Risk factors are bleeding dyscrasias, open fractures, compressive
dressings, excessive wrist flexion maintained in a cast and a prolonged
period between injury and reduction. The pressure within the canal
following a closed fracture treated conservatively has been shown to be
at its highest during reduction and then to fall gradually during the
following 12 hours.60 Chronic
compressive neuropathy of the median nerve occurs in approximately 5%
of conservatively treated fractures of the distal radius.24,112 Acute carpal tunnel syndrome that does not resolve rapidly after reduction is an indication for decompression.
Acute injuries may be seen with displacement of the palmar lunate facet
or with a palmar distal radioulnar joint dislocation and are often
open. In a series of five cases the authors reported that these
represent neurapraxic injury to the ulnar nerve, and that decompression
should be limited to open wounds or associated acute carpal tunnel
syndrome.246 Late progressive ulnar nerve palsy has been reported caused by open distal radioulnar joint injuries.49
severe chronic cases with serious and sometimes devastating disability
are fortunately less common, occurring in less than 2% of cases. CRPS
type 2 occurs in association with damage to a peripheral nerve and CRPS
type 1 in the absence of nerve pathology.
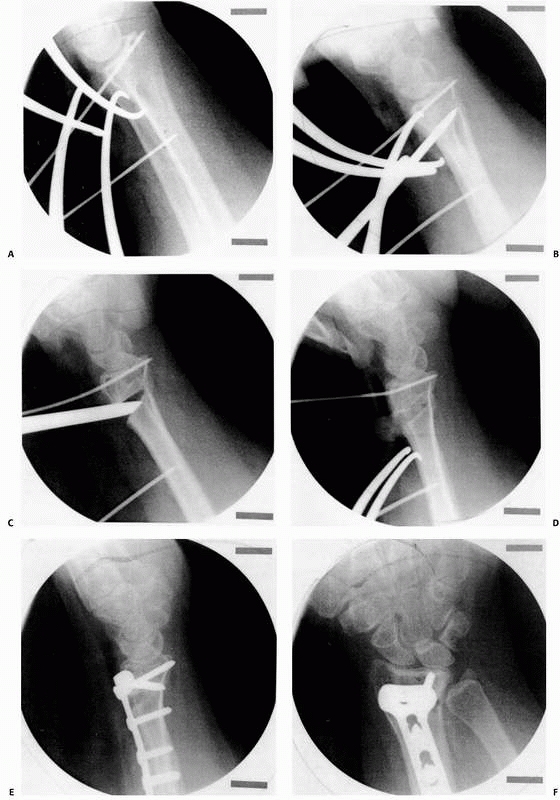 |
|
FIGURE 30-42 Technique of osteotomy for a dorsal malunion. Pins are placed parallel to the joint and perpendicular to the shaft (A). An oscillating saw is used to cut the dorsal cortex (B), whereas the palmar cortex is left intact. The fragment is levered into position (C), and the bone graft is placed (D) and a dorsal plate is applied (E,F).
|
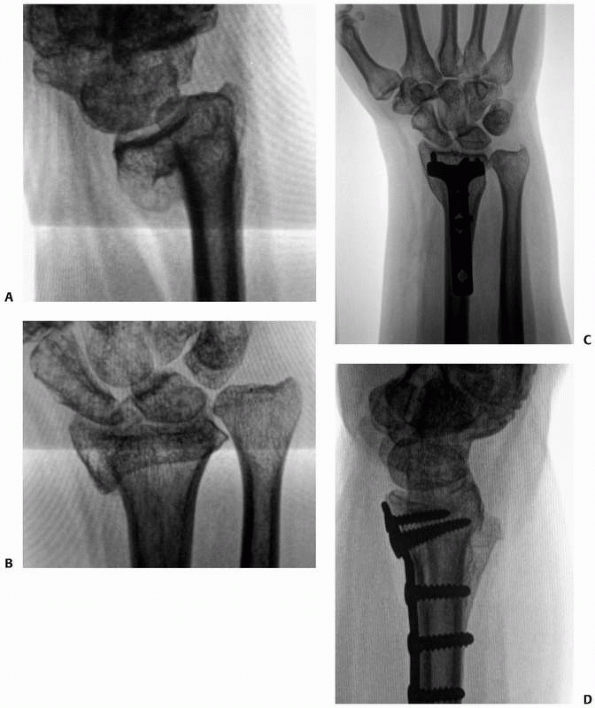 |
|
FIGURE 30-43 Palmar displacement of the distal fragment (A,B).
This deformity is common with collapse following dorsal plating. There is a profound effect on supination as the ulna becomes in essence “dislocated” dorsally because of the palmar displacement of the radius. The osteotomy is performed through a palmar approach and stabilized with a palmar plate (C,D). |
institute early treatment, and surgeons dealing with distal radius
fractures must maintain a high index of suspicion for CRPS. The
cardinal features are abnormal or neuropathic pain, temperature
changes, abnormal sweating, swelling, joint stiffness and atrophy, and
bone changes. Diagnosis in an orthopaedic setting is dealt with in
detail in Chapter 23.
effective analgesia often with the advice of a pain specialist and
intensive physical therapy. Surgery should be avoided unless there is
good evidence of peripheral nerve compression, mostly commonly a carpal
tunnel syndrome. Other treatment modalities include intravenous
guanethidine blockade, Vitamin C, and desensitisation. These are
discussed in detail in Chapter 23.
distal radius fractures occur as a result of penetrating trauma and
direct laceration. Closed ruptures, particularly of the extensor
pollicis longus, have been extensively reported; however, rupture
appears to be relatively uncommon in other tendons. These injuries may
occur either acutely as a result of the initial trauma or late and be
related to either increased pressure within the compartment or because
of attrition from either callus or hardware.
Interestingly, these ruptures occur most frequently in minimally
displaced fractures treated nonoperatively. The rupture is usually
painless and occurs late at 6 weeks to 3 months after injury. Treatment
is directed first at mobilizing the wrist and then performing an
appropriate transfer.
delayed fashion because of attrition.135
Late ruptures caused by hardware impingement have been described,
particularly secondary to attrition of the flexor pollicis on prominent
hardware.141,153
More recently with increased use of volar locking plates, extensor
tendon injury has been reported caused by dorsal penetration of locking
screws at the distal dorsal margin of the radius.6
Care must be taken intraoperatively to assess tangential views of the
radial and intermediate columns, to avoid dorsal screw penetration and
subsequent attritional tendon rupture (Fig. 30-45).
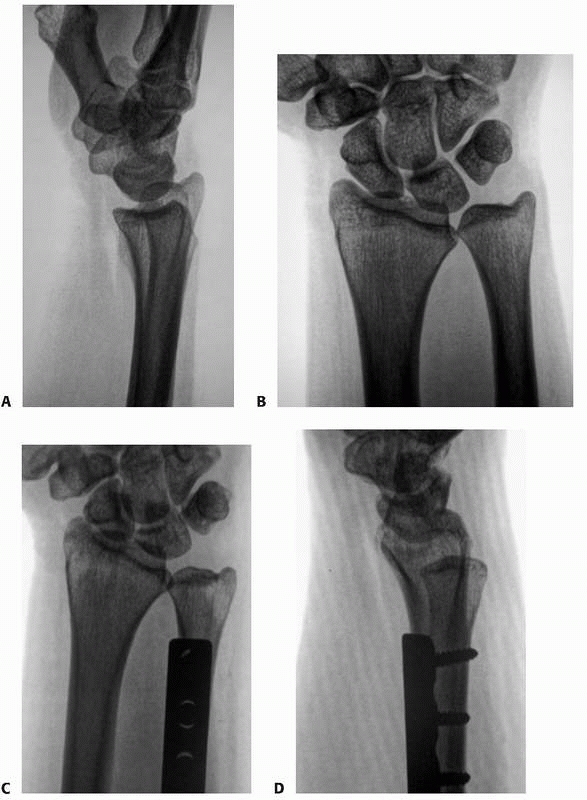 |
|
FIGURE 30-44 Malunion of the radius with loss of radial length and loss of forearm rotation (A,B). An ulnar shortening osteotomy eliminated the symptoms of impaction (C,D), and full rotation was restored.
|
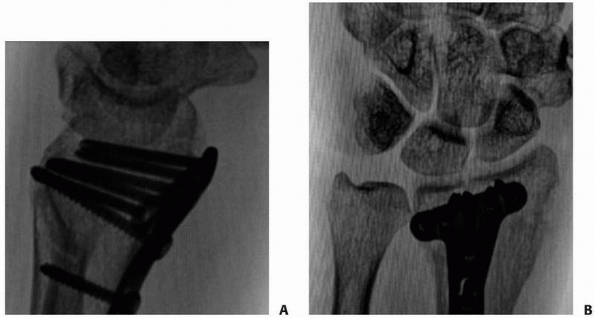 |
|
FIGURE 30-45 A,B.
A patient with an extensor pollicis longus tendon rupture following palmar plate application. Note that on the initial lateral view from the OR (continues) |
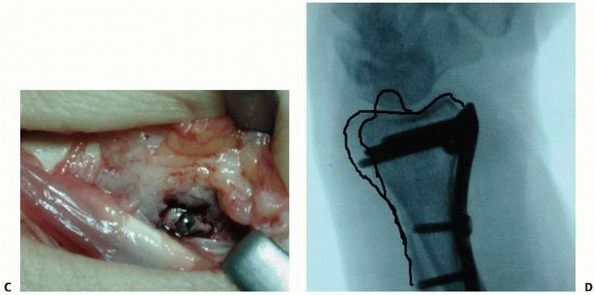 |
|
FIGURE 30-45 (continued) (A),
the screws appear to be well contained by the dorsal cortex. However, the Lister tubercle is the outline dorsally on the lateral view (C,D) and does not protect against dorsal cortical penetration either radially or ulnarly. |
H, Jonsson U. Regional anesthesia preferable for Colles’ fracture.
Controlled comparison with local anesthesia. Acta Orthop Scand
1990;61:348-349.
JM, Szabo RM, Chidgey LK, et al. Treatment of comminuted distal radius
fractures: an approach based on pathomechanics. Orthopedics
1994;17:1115-1122.
J, le Guilloux P, Le Mouel S, et al. Trans-styloid fixation of
fractures of the distal radius. A prospective randomized comparison
between 6- and 1-week postoperative immobilization in 60 fractures.
Acta Orthop Scand 1999;70:119-123.
M, Theivendran K, Craigen MA. Delayed ruptures of the extensor tendon
secondary to the use of volar locking compression plates for distal
radial fractures. J Bone Joint Surg Br 2006;88:1610-1612.
DJ, Blair WF, Steyers CM, Jr., et al. Classification of distal radius
fractures: an analysis of interobserver reliability and intraobserver
reproducibility. J Hand Surg Am 1996;21:574-582.
R, Lutz M, Fritz D, et al. Palmar locking plate for treatment of
unstable dorsal dislocated distal radius fractures. Arch Orthop Trauma
2005;125:399-404.
R, Lutz M, Hennerbichler A, et al. Complications following internal
fixation of unstable distal radius fracture with a palmar locking
plate. J Orthop Trauma 2007;21: 316-322.
H, Subasi M, Kesemenli C, et al. Distraction osteotomy for malunion of
the distal end of the radius with radial shortening. Acta Orthop Belg
2003;69:23-28.
I, Brogren E, Larsson GU, et al. Wrist-bridging versus non-bridging
external fixation for displaced distal radius fractures: a randomized
assessor-blind clinical trial of 38 patients followed for 1 year. Acta
Orthop 2006;77:445-531.
WK, Velazquez PA. The application of indirect reduction techniques in
the distal radius: the role of adjuvant arthroscopy. Arthroscopy
2000;16:830-835.
T, Ehrendorfer S, Coulton T, et al. Unstable extra-articular fractures
of the distal radius: a prospective, randomised study of immobilisation
in a cast versus supplementary percutaneous pinning. J Bone Joint Surg
Br 2005;87:837-840.
H, Lobeck F. Behaviour of the joint surface of the distal radio-ulnar
joint in malposition of the distal radius. Unfallchirurgie
1991;17:213-217.
R, Gris M, Tollet P, Schuind F, Burny F.[Corrective osteotomy using
Hoffmann II external fixators for extra-articular malunion of the
distal radius]. Acta Orthop Belg 2001;67:500-504.
RA, Saldana MJ. Intra-articular fractures of the distal radius: a
cadaveric study to determine if ligamentotaxis restores radiopalmar
tilt. J Hand Surg Am 1990;15: 18-21.
RL, Blair WF, Hubbard PP. Results of combined internal and external
fixation for the treatment of severe AO-C3 fractures of the distal
radius. J Hand Surg Am 1995; 20:373-381.
S, Gupta A. The effect of fracture-related factors on the functional
outcome at 1 year in distal radius fractures. Injury 2002;33:499-502.
EC, DeCarvalho A, Mikola EA, et al. Two potential causes of EPL rupture
after distal radius volar plate fixation. Clin Orthop 2006;451:218-222.
A, McQueen MM. Fractures of the distal radius in low demand elderly
patients: closed reduction is of no value in 53 of 60 wrists. Acta
Orthop Scand 2003; 74:98-100.
A. Over-distraction of the radio-carpal and mid-carpal joints following
external fixation of comminuted distal radial fractures. J Hand Surg Br
1993;18:506-510.
MR, Egol KA, Leibman M, et al. A comparison of immediate post-reduction
splinting constructs for controlling initial displacement of fractures
of the distal radius: a prospective randomized study of long-arm versus
short-arm splinting. J Hand Surg Am 2006;31:766-770.
FW, Jr., Osterman AL, Zielinski CJ. Osteotomy of the distal radius with
a biplanar iliac bone graft for malunion. Bull Hosp Jt Dis
1984;44:122-131.
RM, Gellman H. Dorsal pin placement and external fixation for
correction of dorsal tilt in fractures of the distal radius. J Hand
Surg Am 1994;19:653-655.
AJ, Trumble TE, Tencer AF. The effects of distal radius fracture
malalignment on forearm rotation: a cadaveric study. J Hand Surg Am
1997;22:258-262.
J, Niedzwiedz Z, Bednarski M, et al. [Acute carpal tunnel syndrome
after distal radius fractures—long term results of surgical treatment
with decompression and external fixator application]. Chir Narzadow
Ruchu Ortop Pol 2002;67:47-53.
DM, Juttmann JW. Cancellous grafting and external fixation for unstable
Colles’ fractures. J Bone Joint Surg Br 1997;79:428-432.
JT, Accousti K, Jacob G, et al. The effect of rotational malalignment
on X-rays of the wrist. J Hand Surg Eur 2009;34:166-172.
C, Jupiter JB, Cohen M, et al. Norian SRS cement compared with
conventional fixation in distal radial fractures. A randomized study. J
Bone Joint Surg Am 2003;85: 2127-2137.
LW, Cole RJ, Gelberman RH, et al. Displaced intra-articular fractures
of the distal aspect of the radius. Long-term results in young adults
after open reduction and internal fixation. J Bone and Joint
Am1997;79:1290-3102.
BK, Leong LC, Low CO, et al. The use of the external fixator in the
treatment of intra-articular fractures of the distal radius. Singapore
Med J 1999;40:420-424.
TC, Jou IM, Lai KA, et al. Sonography for monitoring closed reduction
of displaced extra-articular distal radial fractures. J Bone Joint Surg
Am 2002;84:194-203.
KR, Jupiter JB. Wire-loop fixation of volar displaced osteochondral
fractures of the distal radius. J Hand Surg Am 1999 ;24:525-533.
OM, Christiansen TC, Krasheninnikoff M, et al. Plaster cast compared
with bridging external fixation for distal radius fractures of the
Colles’ type. Int Orthop 2001;24:358-360.
KC, Kotsis SV, Kim HM. Predictors of functional outcomes after surgical
treatment of distal radius fractures. J Hand Surg Am 2007;32:76-83.
AC, Spencer RF. Ulnar nerve palsy following fractures of the distal
radius: clinical and anatomical studies. J Hand Surg Br 1991;16:438-440.
RJ, Bindra RR, Evanoff BA, et al. Radiographic evaluation of osseous
displacement following intra-articular fractures of the distal radius:
reliability of plain radiography versus computed tomography. J Hand
Surg Am 1997;22:792-800.
KJ, Clawson MC, Stern PJ. Volar neutralization plate fixation of
dorsally displaced distal radius fractures. Orthopedics 2002;25:125-128.
A. Over-distraction of the radiocarpal and midcarpal joints with
external fixation of comminuted distal radial fractures. J Hand Surg Br
1996;21:289.
J, Martinez AA, Herrera A, Domingo J. The incidence of distal forearm
fractures in Zaragoza (Spain). Chir Main 2003;22:211-215.
JJ, Wray CC, Jones JM, Gregg PJ. The value of early mobilisation in the
treatment of Colles’ fractures. J Bone Joint Surg Br 1987;69:463-467.
K, Peterson T, Schmit-Neuerburg KP. Compartment pressure in the carpal
tunnel in distal fractures of the radius. A prospective study. Arch
Orthop Trauma Surg 1994;113:285-289.
H, Kutscha-Lissberg E. Osteosynthesis of distal radial fractures with a
volar locking screw plate system. Int Orthop 2003;27:1-6.
CE, Thalmann R, Macy JC. The effect of rotational malunion of the
radius and the ulna on supination and pronation. J Bone Joint Surg Br
2002;84:1070-1074.
CE, Lindsay CS, Bicknell RT, et al. Ilizarov hybrid external fixation
for fractures of the distal radius: Part II. Internal fixation versus
Ilizarov hybrid external fixation: stability as assessed by cadaveric
simulated motion testing. J Hand Surg Am 2001; 26:218-227.
CE, Lindsay CS, Bicknell RT, et al. Supplemental pinning improves the
stability of external fixation in distal radius fractures during
simulated finger and forearm motion. J Hand Surg Am 1999;24:992-1000.
CC, Haraszti CJ, McGillivary GR, Gutow AP. Intra-articular distal
radius fractures: arthroscopic assessment of radiographically assisted
reduction. J Hand Surg Am 2001;26:1036-1041.
GS, Jr. Intra-articular fractures of the distal part of the radius
treated with the small AO external fixator. J Bone Joint Surg Am
1991;73:1241-1250.
KA, Paksima N, Puopolo S, et al. Treatment of external fixation pins
about the wrist: a prospective, randomized trial. J Bone Joint Surg Am.
2006;88(2):349-354.
E, Jupiter J. The management of acute fractures involving the distal
radioulnar joint and distal ulna. Hand Clin 1998;14:213-229.
DL, Fleming MC. History, evolution and biomechanics of external
fixation of the wrist joint. Injury 1994;25(Suppl 4):S-D-1-13.
DL, Jakob RP, Buchler U. External fixation of the wrist. Current
indications and technique. Ann Chir Gynaecol 1983;72:298-302.
J, Atkins RM. Algodystrophy is an early complication of Colles’
fracture. What are the implications? J Hand Surg Br 1997;22:178-82.
T, Koch P, Saager C, Kohut GN. The radio-radial external fixator in the
treatment of fractures of the distal radius. J Hand Surg Br
1999;24:604-609.
T, Nikkola-Sihto A, Kaaela O, et al. Poor interobserver reliability of
AO classification of fractures of the distal radius. J Bone Joint Surg
Br 1998;80:670-672.
T, Nikkola-Sihto A, Raatikainen T, et al. Role of metaphyseal
cancellous bone defect size in secondary displacement in Colles’
fracture. Arch Orthop Trauma Surg 1999;119:319-323.
T, Raatikainen T, Kaarela O, et al. Corrective osteotomy for malunion
of the distal radius. Arch Orthop Trauma Surg 2000;120:23-26.
T, Ristiniemi J, Hyvönen P, et al. Nonbridging external fixation in the
treatment of unstable fractures of the distal forearm. Arch Orthop
Trauma Surg 2003;123: 349-352.
DP, Lindau TR, Melsom DS. Intercarpal ligament injuries associated with
fractures of the distal part of the radius. J Bone Joint Surg Am
2007;89:2334-2340.
GK. Fractures of the distal radius including
sequelae-shoulder-hand-finger syndrome, disturbance in the distal
radio-ulnar joint and impairment of nerve function. Acta Orthop Scand
1967:Suppl 108:7-153.
T, Pennig D, Mader K. Principles of external fixation and supplementary
techniques in distal radius fractures. Injury 2000;31(Suppl 1):56-70.
T, Worner S, Pennig D, et al. Extraarticular external fixation in
distal radius fractures pinplacement in osteoporotic bone. Injury
2001;32(Suppl 4):SD79-SD85.
WB, Fernandes D. Percutaneous and limited open reduction of
intra-articular distal radial fractures. Hand Surg 2000;5:85-92.
WB, Fernandez DL. Percutaneous and limited open reduction of the
articular surface of the distal radius. J Orthop Trauma 1991;5:255-264.
WB, Fernandez DL, Lamey DM. Distal radioulnar joint injuries associated
with fractures of the distal radius. Clin Orthop1996;327:135-146.
WB, Freeland AE, Savoie FH, et al. Intracarpal soft-tissue lesions
associated with an intra-articular fracture of the distal end of the
radius. J Bone Joint Surg Am 1996;78:357-365.
G. Memoire sur les fractures de l’extremite inferieure du radius qui
simulent les luxations du poignet. Gaz Med 1832;3:664-667.
G, Jupiter JB, Gierer P, Mittlmeier T. Fractures of the distal radius
treated with a nonbridging external fixation technique using
multiplanar k-wires. J Hand Surg Am 2005;30:960-968.
R, MacDermid JC. The risk of adverse outcomes in extra-articular distal
radius fractures is increased with malalignment in patients of all ages
but mitigated in older patients. J Hand Surg Am 2007;32:962-970.
R, Perey B, Wilmink M, Stothers K. A randomized prospective study on
the treatment of intra-articular distal radius fractures: open
reduction and internal fixation with dorsal plating versus mini open
reduction, percutaneous fixation, and external fixation. J Hand Surg Am
2005;30:764-772.
H, Weinstabl R, Schmid L. [Anatomic studies of percutaneous bore wire
osteosynthesis of the distal radius]. Unfallchirurgie 1993;19:49-53.
H, Yamamoto K, Ohshiro H, et al. Changing incidence of hip, distal
radius, and proximal humerus fractures in Tottori Prefecture, Japan.
Bone 1999;24:265-270.
D, Platz A, Amgwerd M, Trentz O. Internal fixation of distal radius
fractures with dorsal dislocation: pi-plate or two 1/4 tube plates? A
prospective randomized study. J Trauma 1999;47:760-765.
DG, Drew SJ, Eckersley R. Kirschner wire pin tract infection rates: a
randomized controlled trial between percutaneous and buried wires. J
Hand Surg Br2004; 29:374-376.
NG, Ring D, Zurakowski D, et al. The influence of three-dimensional
computed tomography reconstructions on the characterization and
treatment of distal radial fractures. J Bone Joint Surg Am
2006;88:1315-1323.
DM, Johnston GH. Safety of the limited open technique of
bone-transfixing threaded-pin placement for external fixation of distal
radial fractures: a cadaver study. Can J Surg 1999;42:363-365.
AJ, Duffy PJ, McQueen MM. Bridging and non-bridging external fixation
in the treatment of unstable fractures of the distal radius: a
retrospective study of 588 cases. Acta Orthop 2008;79:540-547.
M, Chapman CB, Roh M, et al. Treatment of unstable distal radius
fractures with cancellous allograft and external fixation. J Hand Surg
Am 1999;24:1269-1278.
M, Faraj A, Craigen MA. Dorsal plating for displaced intra-articular
fractures of the distal radius. Injury 2003;34:497-502.
H, Neale PG, Lin YT, et al. Kinematic and torque-related effects of
dorsally angulated distal radius fractures. J Hand Surg Am
2003;28:614-621.
LM. Delayed rupture of the thumb extensor tendon. A 5-year study of 18
consecutive cases. Acta Orthop Scand 1994;65:199-203.
LM. Nerve entrapment and reflex sympathetic dystrophy after fractures
of the distal radius. Scand J Plast Reconstr Surg Hand Surg
1995;29:53-58.
LM, Furnes O, Nilsen PT, et al. Closed reduction and external fixation
of unstable fractures of the distal radius. Scand J Plast Reconstr Surg
Hand Surg 1997;31:159-164.
P, Stewart H, Hind R, Burke F. External fixation or plaster for
severely displaced comminuted Colles’ fractures? A prospective study of
anatomical and functional results. J Bone Joint Surg Br
1989;71(1):68-73.
K, Hunerbein M, Meeder PJ. External fixation of intra-articular
fracture of the distal radius in young and old adults. Arch Orthop
Trauma Surg 1996;115:38-42.
SL, Slemenda CW, Johnston CC, Jr. Age and bone mass as predictors of
fracture in a prospective study. J Clin Invest 1988;81:1804-1809.
TR, Hastings H, II, Graham T. A systematic approach to handling the
distal radioulnar joint in cases of malunited distal radius fractures.
Hand Clin 1998;14: 239-249.
DT, Bachus KN, Higgenbotham T. External fixation of the distal radius:
to predrill or not to predrill. J Hand Surg Am 2000;25:1064-1068.
DT, Strenz GO, Cautilli RA. Pins and plaster vs external fixation in
the treatment of unstable distal radial fractures. A randomized
prospective study. J Hand Surg Br 1995;20:365-372.
I, Pieterse HS, Sweet MB. External fixation for intra-articular
fractures of the distal radius. J Bone Joint Surg Br 1991;73:302-306.
M, Rikli DA, Regazzoni P. Fractures of the distal radius treated by
internal fixation and early function. A prospective study of 73
consecutive patients. J Bone Joint Surg Br 2000;82:340-344.
NH, Jones DG, Johnson SR, Mintowt-Czyz WJ. External fixation of Colles’
fractures. An anatomical study. J Bone Joint Surg Br. 1987;69:207-211.
N, Jones D, Mintowt-Czyz. External fixation and recovery of function
following fractures of the distal radius in young adults. Injury
1988;19:235-238.
GH, Friedman L, Kriegler JC. Computerized tomographic evaluation of
acute distal radial fractures. J Hand Surg Am 1992;17:738-744.
J, Fernandez DL. Comparative classification for fractures of the distal
end of the radius. J Hand Surg Am 1997;22:563-571.
JB, Fernandez DL, Toh CL, et al. Operative treatment of volar
intra-articular fractures of the distal end of the radius. J Bone Joint
Surg Am 1996;78:1817-1828.
JB, Ring D, Weitzel PP. Surgical treatment of redisplaced fractures of
the distal radius in patients older than 60 years. J Hand Surg Am
2002;27:714-723.
FA, Walker KM. External fixation for distal radius fractures: effect of
distraction on outcome. Clin Orthop 2000;380:220-225.
M, Honda Y, Kazuki K, Yasuda M. Palmar plating for dorsally displaced
fractures of the distal radius. Clin Orthop 2002;397:403-408.
N, Nemoto K, Arino H, et al. Ruptures of flexor tendons at the wrist as
a complication of fracture of the distal radius. Scand J Plast Reconstr
Surg Hand Surg 2002;36: 245-248.
JP, Karaharju EO, Porras M, et al. Functional recovery after fractures
of the distal forearm. Analysis of radiographic and other factors
affecting the outcome. Ann Chir Gynaecol 1988;77:27-31.
K, Kusunoki M, Yamada J, et al. Cineradiographic study of wrist motion
after fracture of the distal radius. J Hand Surg Am 1993;18:41-46.
D, Hattori Y, Otsuka K, et al. Intraarticular fractures of the distal
aspect of the radius: Arthroscopically assisted reduction compared with
open reduction and internal fixation. J Bone Joint Surg Am
1999;81:1093-1110.
JF, Court-Brown CM, McQueen MM. Internal fixation of volar-displaced
distal radial fractures. J Bone Joint Surg Br 1994;76:401-405.
H, Palmer AK, Werner F, et al. The effect of dorsally angulated distal
radius fractures on distal radiolunar joint congruency and forearm
rotation. J Hand Surg Am 1996;21:40-47.
RA, Press CM, Gonzalez MH. Rupture of the flexor pollicis longus tendon
after volar fixed-angle plating of a distal radius fracture: a case
report. J Hand Surg Am 2007;32:984-988.
JL, Jupiter JB. Intra-articular fractures of the distal end of the
radius in young adults. J Bone Joint Surg Am 1986;68:647-659.
GA, Bahler S. Open reduction and internal fixation of unstable distal
radius fractures: results using the trimed fixation system. J Orthop
Trauma 2002;16:578-585.
P, Johnell O, Redlund-Johnell I, et al. Fractures of the distal end of
the radius in young adults: a 30-year follow-up. J Hand Surg Br
1993;18:45-49.
HJ, Agel J, McKee MD, et al. A randomized, controlled trial of distal
radius fractures with metaphyseal displacement but without joint
incongruity: closed reduction and casting versus closed reduction,
spanning external fixation, and optional percutaneous K-wires. J Orthop
Trauma 2006;20:115-121.
HJ, Hanel DP, Agel J, et al. Indirect reduction and percutaneous
fixation versus open reduction and internal fixation for displaced
intra-articular fractures of the distal radius: a randomised,
controlled trial. J Bone Joint Surg Br 2005;87:829-836.
J, Chipchase LS, Slavotinek J. Intraarticular fractures of the distal
radius treated with metaphyseal external fixation. Early clinical
results. J Hand Surg Br 1998; 23:396-399.
J, Wigg AER, Walker RW, et al. Intra-articular fractures of the distal
radius: a prospective randomised controlled trial comparing static
bridging and dynamic nonbridging external fixation. J Hand Surg Br
2003; 28:417-421.
EH, Mellios K, Berwarth H. Treatment of complicated fracture of the
distal radius with external fixator. Follow-up—complications—outcomes.
Unfallchirurg 2002;105: 199-207.
O, Fuchs M, Schabus R. Opening wedge osteotomy for malunion of the
distal radius with neuropathy. 13 cases followed for 6 (1-11) years.
Acta Orthop Scand 1994;65:207-208.
J, Bismuth JP. Intracarpal ligamentous lesions associated with
fractures of the distal radius: outcome at one year. A prospective
study of 95 cases. Acta Orthop Belg 1999;65:418-423.
HC, Wong YS, Chan BK, et al. Fixation of distal radius fractures using
AO titanium volar distal radius plate. Hand Surg 2003;8:7-15.
GE, Anderson JJ, Tylavsky FA, et al. Update on the use of distal radial
bone density measurements in prediction of hip and Colles’ fracture
risk. J Orthop Res 1990; 8:220-226.
F, Ozkan M, Chow SP. Conservative treatment of intra-articular
fractures of the distal radius—factors affecting functional outcome.
Hand Surg 2000;5:145-153.
F, Tu YK, Chew WY, et al. Comparison of external and percutaneous pin
fixation with plate fixation for intra-articular distal radial
fractures. A randomized study. J Bone Joint Surg Am 2008;90:16-22.
F, Zhu L, Ho H. Palmar plate fixation of AO type C2 fracture of distal
radius using a locking compression plate—a biomechanical study in a
cadaveric model. J Hand Surg Br 2003;28:263-266.
KS, Shen W, Leung P, et al. Ligamentotaxis and bone grafting for
comminuted fractures of the distal radius. J Bone Joint Surg Br
1989;71:838-842.
KS, So W, Chiu V, et al. Ligamentotaxis for comminuted distal radial
fractures modified by primary cancellous grafting and functional
bracing: long-term results. J Orthop Trauma 1991;5:265-271.
T, Adlercreutz C, Aspenberg P. Peripheral tears of the triangular
fibrocartilage complex cause distal radioulnar joint instability after
distal radial fractures. J Hand Surg Am 2000;25:464-468.
T, Arner M, Hagberg L. Intraarticular lesions in distal fractures of
the radius in young adults. A descriptive arthroscopic study in 50
patients. J Hand Surg Br 1997; 22:638-643.
TR, Aspenberg P, Arner M, et al. Fractures of the distal forearm in
young adults. An epidemiologic description of 341 patients. Acta Orthop
Scand 1999;70:124-128.
T, Hagberg L, Adlercreutz C, et al. Distal radioulnar instability is an
independent worsening factor in distal radial fractures. Clin Orthop
2000;376:229-235.
L, Stattin J. Malunited fractures of the distal radius with volar
angulation: corrective osteotomy in 6 cases using the volar approach.
Acta Orthop Scand 1996;67: 179-181.
KJ, Gainor BJ, Hoskins JS. Extensor tendon rupture secondary to the
AO/ASIF titanium distal radius plate without associated plate failure:
a case report. Am J Orthop 2000;29:789-791.
SA, Doornberg J, Ring D. Fractures of the dorsal articular margin of
the distal part of the radius with dorsal radiocarpal subluxation. J
Bone Joint Surg Am 2006;88:1486-1493.
D, Quisling S, Lourie G, et al. Tilted lateral radiographs in the
evaluation of intra-articular distal radius fractures. J Hand Surg Am
1999;24:249-256.
TB, Hilliar KM, Coates CJ, et al. Early mobilisation of Colles’
fractures. A prospective trial. J Bone Joint Surg Br 1987;69:727-729.
MM. Redisplaced fractures of the distal radius. A randomised
prospective study of bridging versus non-bridging external fixation. J
Bone Joint Surg Br 1998;80; 665-669.
M, Caspers J. Colles’ Fracture: Does the anatomical result afftect the
final function? J Bone Joint Surg Br 1988;70:649-651.
MM, Hajducka C, Court-Brown C. Redisplaced unstable fractures of the
distal radius: A randomised, prospective study of bridging versus
non-bridging external fixation. J Bone Joint Surg Br 1996;78:404-409.
MM, Simpson D, Court-Brown CM. Metaphyseal external fixation of
redisplaced unstable distal radial fractures. Use of the Hoffman 2
compact external fixator. J Orthop Trauma 1999;13:501-505.
MM, Wakefield A. Distal radial osteotomy for malunion using
non-bridging external fixation: good results in 23 patients.Acta Orthop
2008;79:390-395.
JS, Taylor NF, McIlveen C. A randomised clinical trial of
activity-focussed physiotherapy on patients with distal radius
fractures. Arch Orthop Trauma Surg 2005; 125:515-520.
PJ. Re: An evaluation of two scoring systems to predict instability in
fractures of the distal radius. J Trauma 2005;59:1535.
R, Green S. Longer term functional outcome and societal implications of
upper limb fractures in the elderly. J R Soc Health 1993;113:179-180.
H, Ljunghall S. Incidence of Colles’ fracture in Uppsala. A prospective
study of a quarter-million population. Acta Orthop Scand
1992;63:213-215.
H, Ljunghall S, Naessen T. Colles’ fracture associated with reduced
bone mineral content. Photon densitometry in 74 patients with matched
controls. Acta Orthop Scand 1992;63:552-554.
H, Ljunghall S, Persson I, et al. Risk factors for fractures of the
distal forearm: a population-based case-control study. Osteoporos Int
1994;4:298-304.
KJ, Magnell TD, Freeman DC, et al. Surgical correction of dorsally
angulated distal radius malunions with fixed angle volar plating: a
case series. J Hand Surg Am 2006;31:366-372.
AD, Gellman H. Five-pin external fixation and early range of motion for
distal radius fractures. Orthop Clin North Am 2001;32:329-335.
T, Jordan D, Hosking DJ. Distal forearm fracture history in an older
communitydwelling population: the Nottingham Community Osteoporosis
(NOCOS) study. Age Ageing 2001;30:255-258.
MM, Lawton JN, Blazar PE. Ulnar styloid fractures associated with
distal radius fractures: incidence and implications for distal
radioulnar joint instability. J Hand Surg Am 2002;27:965-971.
EM. Opening-wedge osteotomy, bone graft, and external fixation for
correction of radius malunion. J Hand Surg Am 1997;22:785-791.
RP, Latimer BM. Hamann-Todd Collection aging studies: osteoporosis
fracture syndrome. Am J Phys Anthropol 1989;80:461-479.
BS, Taylor B, Widmann RF, et al. Cast immobilization versus
percutaneous pin fixation of displaced distal radius fractures in
children: a prospective, randomized study. J Pediatr Orthop
2005;25:490-494.
A, Ogino T. Midcarpal instability following malunion of a fracture of
the distal radius. A case report. Ital J Orthop Traumatol
1986;12:473-477.
M, Cooney W, Amadio P, et al. Open reduction and internal fixation for
distal radius fractures. J Hand Surg Am 1992;17:745-755.
DC, Hogan KA, Crisco JJ, III, et al. Three-dimensional in vivo
kinematics of the distal radioulnar joint in malunited distal radius
fractures. J Hand Surg Am 2002; 27:233-242.
DS, Idler RS. Volar fixation of dorsally displaced distal radius
fractures using the 2.4mm locking compression plates. J Hand Surg Am
2005;30:743-749.
TV, Center JR, Sambrook PN, et al. Risk factors for proximal humerus,
forearm, and wrist fractures in elderly men and women: the Dubbo
Osteoporosis Epidemiology Study. Am J Epidemiol 2001;153:587-595.
TW, Cooper C, Finn JD, et al.Incidence of distal forearm fracture in
British men and women.Osteoporos Int 2001;12:555-558.
JL, Fernandez DL. Volar fixation for dorsally displaced fractures of
the distal radius: a preliminary report. J Hand Surg Am 2002;27:205-215.
T, Sakai A, Zenke Y, et al. A comparative study of clinical and
radiological outcomes of dorsally angulated, unstable distal radius
fractures in elderly patients: intrafocal pinning versus volar locking
plating. J Hand Surg Am 2007;32:1385-1392.
J, Kingma J, Klasen HJ. Ulnar-shortening osteotomy after fracture of
the distal radius. Arch Orthop Trauma Surg 1993;112:198-200.
DJ, Viegas SF, Patterson RM, et al. Effects of distal radius fracture
malunion on wrist joint mechanics. J Hand Surg Am 1990;15:721-727.
M, Stockley I. Fractures of the distal radius. Intermediate and end
results in relation to radiologic parameters. Clin Orthop
1987;220:241-252.
A, Swol-Ben J, Rehm KE. Treatment methods for geriatric patients at the
Traumatology Clinic at the University of Cologne—retrospective studies.
Chir Narzadow Ruchu Ortop Pol 1996;61:315-318.
KJ, Lanz U. [Biomechanical aspects of malunited distal radius fracture.
A review of the literature.] Handchir Mikrochir Plast Chir
1999;31:221-226.
KJ, Ring D, del Pino JG, et al. Corrective osteotomy for
intra-articular malunion of the distal part of the radius. Surgical
technique. J Bone Joint Surg Am 2006;88(Suppl 1, Pt 2):202-211.
MD, Fischer MD. Treatment of unstable distal radius fractures: methods
and comparison of external distraction and ORIF versus external
distraction-ORIF neutralization. J Hand Surg Am 1997;22:238-251.
S, Schikore H, Schneiders W, et al. Results of dorsal or volar plate
fixation of AO type C3 distal radius fractures: a retrospective study.
J Hand Surg Am 2007;32: 954-961.
SS, Pristas R, Dixon D, et al. The incidence of CRPS after fasciectomy
for Dupuytren’s contracture: a prospective observational study of from
anaesthetic techniques. Anaesth Analg 2006;102:499-503.
RS, Bennett JD, Roth JH, et al. Arthroscopic diagnosis of
intra-articular soft tissue injuries associated with distal radial
fractures. J Hand Surg Am 1997;22: 772-776.
D, Jupiter JB, Brennwald J, et al. Prospective multicenter trial of a
plate for dorsal fixation of distal radius fractures. J Hand Surg Am
1997;22:777-784.
D, Kadzielski J, Fabian L, et al. Self-reported upper extremity health
status correlates with depression. J Bone Joint Surg Am
2006;88:1983-1988.
TD, Beredjiklian PK, Bozentka DJ. Functional outcome and complications
following two types of dorsal plating for unstable fractures of the
distal part of the radius. J Bone Joint Surg Am 2003;85:1956-1960.
TD, Blazar PE. Functional outcome and complications after volar plating
for dorsally displaced, unstable fractures of the distal radius. J Hand
Surg Am 2006;31: 359-365.
TD, Branas CC, Bozentka DJ, et al. Survival among elderly patients
after fractures of the distal radius. J Hand Surg Am 2002;27:948-952.
DS, Ginn TA. Open reduction and internal fixation of distal radius
fractures. Operative Techniques in Orthopaedics 2003;13:138-143.
DS, Papadonikolakis A. Volar versus dorsal plating in the management of
intraarticular distal radius fractures. J Hand Surg Am 2006;31:9-16.
DS, Vallee J, Poehling GG, et al. Arthroscopic reduction versus
fluoroscopic reduction in the management of intra-articular distal
radius fractures. Arthroscopy 2004;20:225-230.
DS, Yang CC, Smith BP. Results of acute arthroscopically repaired
triangular fibrocartilage complex injuries associated with
intra-articular distal radius fractures. Arthroscopy 2003;19:511-516.
DS, Yang C, Smith BP. Results of palmar plating of the lunate facet
combined with external fixation for the treatment of high-energy
compression fractures of the distal radius. J Orthop Trauma
2004;18:28-33.
Y, Hashizume H, Nagoshi M, et al. Mechanical strength of intramedullary
pinning and transfragmental Kirschner wire fixation for Colles’
fractures. J Hand Surg Br 2001; 26:550-555.
J, Munuera L, Madero R. Treatment of fractures of the distal radius
with a remodellable bone cement. J Bone Joint Surg Br 2000;82:856-863.
RA, Keppel FL, Waldrop JI. External fixation of distal radial
fractures: results and complications. J Hand Surg Am 1991;16:385-391.
S. Load transmission through the wrist joint: a biomechanical study
comparing the normal and pathological wrist. Nippon Seikeigeka Gakkai
Zasshi 1995;69:470-483.
DP, Chang B. Extensor tendon rupture after internal fixation of a
distal radius fracture using a dorsally placed AO/ASIF titanium pi
plate. Ann Plast Surg 2000;44: 564-566.
WH, Jr., Froimson AI, Leb R, Shapiro JD. Augmented external fixation of
unstable distal radius fractures. J Hand Surg Am 1991;16:1010-1016.
JA, Bruno A, Paul EM. Ulnar styloid fixation in the treatment of
posttraumatic instability of the radioulnar joint: a biomechanical
study with clinical correlation. J Hand Surg Am 1990;15:712-720.
AM, Castle JA, Ruch DS. Arthroscopic resection of the common extensor
origin: anatomic considerations. J Shoulder Elbow Surg 2003;12:375-379.
RS, Crick JC, Alonso J, et al. Open reduction and internal fixation of
volar lip fractures of the distal radius. J Orthop Trauma
1988;2:181-187.
S, Bunger C, Sllund K. Displaced distal radius fractures. A comparative
study of early results following external fixation, functional bracing
in supination, or dorsal plaster immobilization. Arch Orthop Trauma
Surg 1990;109:34-38.
HD, Innes AR, Burke FD. Functional cast-bracing for Colles’ fractures.
A comparison between cast-bracing and conventional plaster casts. J
Bone Joint Surg Br 1984; 66:749-753.
DV, Broos PL. Closed reduction versus Kapandji-pinning for
extra-articular distal radial fractures. J Hand Surg Br 1999;24:89-91.
EJ, Banerjee D, Kummer FJ, Tejwani NC. Evaluation of a novel,
nonspanning external fixator for treatment of unstable extra-articular
fractures of the distal radius: biomechanical comparison with a volar
locking plate. J Trauma 2008;64:975-981.
H, Takahashi S, Ando M. Comminuted intra-articular fracture of the
distal radius with rotation of the palmar medial articular fragment:
case reports. J Trauma 1992;32:404-407.
JB, Shi D, Gu YQ, et al. Can cast immobilization successfully treat
scapholunate dissociation associated with distal radius fractures? J
Hand Surg Am 1996;21:583-590.
TE, Schmitt S, Vedder NB. Factors affecting functional outcome of
displaced intra-articular distal radius fractures. J Hand Surg Am
1994;19:325-340.
TE, Wagner W, Hanel DP, et al. Intrafocal (Kapandji) pinning of distal
radius fractures with and without external fixation. J Hand Surg Am
1998;23:381-394.
T, Takagi K, Iwasaki K. Poor correlation between functional results and
radiographic findings in Colles’ fracture. J Hand Surg Br
1993;18:588-591.
der Linden W, Ericson R. Colles’ fracture. How should its displacement
be measured and how should it be immobilized? J Bone Joint Surg Am
1981;63:1285-1288.
Cauwelaert de Wyels J, De Smet L. Corrective osteotomy for malunion of
the distal radius in young and middle-aged patients: an outcome study.
Chir Main 2003;22: 84-89.
Hansen F, Staunstrup H, Mikkelsen S. A comparison of 3 and 5 weeks
immobilization for older type 1 and 2 Colles’ fractures. J Hand Surg Br
1998 23:400-401.
R, Wegener EE, Freeland AE. Use of a closing wedge osteotomy to correct
malunion of dorsally displaced extra-articular distal radius fractures.
Orthopedics 2000; 23:721-724.
A, McQueen MM. The role of physiotherapy and clinical predictors of
outcome after distal radial fracture. J Bone Joint Surg 2000;82:972-976.
NP, Brammar TJ, Hutchinson J, et al. Treatment of unstable distal
radial fractures by intrafocal, intramedullary K-wires. Injury
2001;32:383-389.
WF, Tencer AF, Kiser P. Effects of intra-articular distal radius
depression on wrist joint contact characteristics. J Hand Surg Am
1996;21:554-560.
PM, Kolettis GJ, Schwend R. Acute median neuropathy following physeal
fractures of the distal radius. J Pediatr Orthop 1994;14:173-177.
HK, Castle TH, Jr. Trapezoidal osteotomy of the distal radius for
unacceptable articular angulation after Colles’ fracture. J Hand Surg
Am 1988;13:837-843.
SC, Szabo RM. Severely comminuted distal radial fracture as an unsolved
problem: complications associated with external fixation and pins and
plaster techniques. J Hand Surg Am 1986;11:157-165.
KD, Raeder F, Brauer RB, et al. External fixation of distal radial
fractures: four compared with five pins: a randomized prospective
study. J Bone Joint Surg Am 2003; 85:660-666.
S, Beringer T, Taggart H, et al. A study of male patients with forearm
fracture in Northern Ireland. Clin Rheumatol 2007;26:191-195.
CF, Nanu AM, Checketts RG. Seven-year outcome following Colles’ type
distal radial fracture. A comparison of two treatment methods. J Hand
Surg Br 2003;28: 422-426.
BT, Rayan GM. Outcome following nonoperative treatment of displaced
distal radius fractures in low-demand patients older than 60 years. J
Hand Surg 2000;25: 19-28.
MG, Eglseder WA, Jr., Belkoff SM. Biomechanical evaluation of distal
radius fracture stability. J Orthop Trauma 1998 ;12:46-50.
