Patellofemoral Syndrome
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Patellofemoral Syndrome
Patellofemoral Syndrome
Henry Boateng MD
John H. Wilckens MD
Description
-
Patellofemoral syndrome:
-
Disorder of the patellofemoral joint presenting with anterior knee pain.
-
Insidious in onset
-
Exacerbated by activity involving strenuous or continuous flexion
-
General Prevention
-
Quadriceps muscle strengthening
-
Avoidance of overuse in activities requiring repetitive knee flexion
-
Improvement in training protocols
-
Avoidance of open-chain quadriceps exercise
Epidemiology
-
More common in females than in males (1)
-
Seen especially in the adolescent athlete (1)
-
Most common cause of knee pain in runners (1)
Incidence
Common, but true incidence is unknown.
Prevalence
Prevalence is unknown.
Risk Factors
-
Training errors (e.g., rapidly increased mileage)
-
Female gender
-
Poor quadriceps strength
-
Dysplastic vastus medialis obliquus
-
Generalized ligamentous laxity
-
Heel cord and hamstring tightness
-
Patella alta
-
Extensor mechanism malalignment (increased femoral anteversion, increased Q angle (Fig. 1-1), genu varum/valgus, external tibial torsion, pronated feet)
Genetics
No known inheritance pattern
Pathophysiology
Biomechanical malalignment of the patella, causing
uneven pressure and wear on the patellofemoral joint, leading to
anterior knee pain
uneven pressure and wear on the patellofemoral joint, leading to
anterior knee pain
Etiology
-
Extensor mechanism malalignment
-
Contracted lateral retinaculum (also may be result)
Associated Conditions
-
Quadriceps dysplasia/weakness
-
Extensor mechanism malalignment
-
Patellar instability
Signs and Symptoms
History
-
Pain in the anterior knee, worse after strenuous and bent-knee activities
-
Pain with stair climbing, worse with going down
-
Pain after prolonged knee flexion, such as at theatres (“movie-goer’s knee”) or during long car rides
-
Pain with squatting and rising from squatted position
-
Pseudo giving-way of the knee
Physical Exam
-
Extensor mechanism alignment:
-
Q angle
-
Femoral anteversion
-
Tibial torsion
-
Pronated feet
-
-
Tender medial and lateral patella retinaculum
-
Patellar laxity/instability (lateral displacement with apprehension) (Fig. 2)
-
Tight quadriceps, hamstrings, Achilles tendon
-
± Effusion
-
Pain with patellar loading
Tests
Imaging
-
Plain radiographs:
-
AP
-
Lateral: Look for patella alta
-
Axial:
-
Merchant standardized tangential view of the patella with 30° of flexion
-
“Sunrise” views require more knee flexion and do not show subtle malalignment and instability.
-
-
-
CT and MRI are useful for recalcitrant cases (>6 months of symptoms).
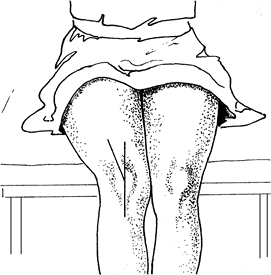 Fig.
Fig.
1. The Q angle is the angle formed between the tibial tubercle, the
patella, and the femur. The greater the angle, the more likely the
development of patellofemoral syndrome.
Diagnostic Procedures/Surgery
Arthroscopy may show patella maltracking and patella chondromalacia.
Pathological Findings
-
Extensor mechanism malalignment
-
Patella chondromalacia
-
Instability
Differential Diagnosis
-
Quadriceps tendinitis
-
Patellar tendinitis
-
Patellofemoral arthritis
-
Osteochondritis desiccans
-
Symptomatic plica
-
Patellofemoral instability
-
Fat pad impingement
Initial Stabilization
-
Initial stage of treatment is reduction of symptoms.
-
NSAIDs
-
Ice
-
Activity modification
-
Isometric quadriceps and core strengthening
-
Quadriceps, hamstring, and Achilles stretching
General Measures
-
The overall goal in treatment is to reduce pain.
-
Nonoperative measures include physical therapy, activity modification, and NSAIDs.
-
NSAIDs and ice may help with pain reduction in acute exacerbations.
Activity
-
Activity modification, such as avoidance of open-chain leg extensions and uphill running
-
Graduated training protocols to avoid acute increase in activities
-
Quadriceps and hamstring stretching before and after running
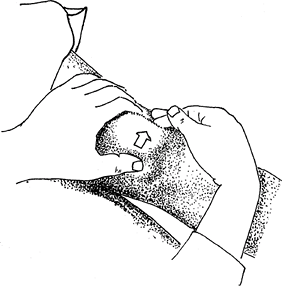 Fig.
Fig.
2. Patients who previously experienced patellofemoral subluxation or
dislocation exhibit a positive apprehension sign when the patella is
pushed laterally.
P.315
Special Therapy
Bracing during activity, such as using a patellar
sleeve, may help with patella tracking and improve muscle
proprioception (muscle responsiveness).
sleeve, may help with patella tracking and improve muscle
proprioception (muscle responsiveness).
Physical Therapy
-
Physical therapy for quadriceps strengthening and stretching is the initial line of treatment.
-
Alternative exercises (swimming)
-
Reconditioning:
-
Eccentric quadriceps strengthening
-
Modalities such as iontophoresis
-
Hamstring and Achilles stretching
-
Core strengthening
-
Medication
NSAIDs
Surgery
-
Only when symptomatic and after an exhaustive and documented course of physical therapy (6 months)
-
Lateral release for contracted, tight lateral retinaculum:
-
Too vigorous a release can lead to medial instability.
-
-
Realignment (proximal and/or distal), depending on type of malalignment
-
Chondroplasty for extensive chondromalacia
-
Early quadriceps activation
-
Early ROM
Disposition
Issues for Referral
Anterior knee pain associated with patellar instability or malalignment should be referred.
Prognosis
-
Most patients improve with physical therapy and nonoperative measures.
-
Surgery is successful for patients with identified mechanical causes of pain such as instability or malalignment of the patella.
Complications
Hemarthrosis is the most common complication after lateral release (2).
References
1. DeHaven KE, Dolan WA, Mayer PJ. Chondromalacia patellae in athletes. Clinical presentation and conservative management. Am J Sports Med 1979;7:5–11.
2. Small NC. An analysis of complications in lateral retinacular release procedures. Arthroscopy 1989;5:282–286.
Additional Reading
Carson
WG, Jr, James SL, Larson RL, et al. Patellofemoral disorders: physical
and radiographic evaluation. Part I: physical examination. Clin Orthop Relat Res 1984;185:165–177.
WG, Jr, James SL, Larson RL, et al. Patellofemoral disorders: physical
and radiographic evaluation. Part I: physical examination. Clin Orthop Relat Res 1984;185:165–177.
Carson
WG, Jr, James SL, Larson RL, et al. Patellofemoral disorders: physical
and radiographic evaluation. Part II: Radiographic examination. Clin Orthop Relat Res 1984;185:178–186.
WG, Jr, James SL, Larson RL, et al. Patellofemoral disorders: physical
and radiographic evaluation. Part II: Radiographic examination. Clin Orthop Relat Res 1984;185:178–186.
Fox JM, Del Pizzo W, eds. The Patellofemoral Joint. New York: McGraw-Hill, 1993.
Fulkerson JP, Shea KP. Disorders of patellofemoral alignment. J Bone Joint Surg 1990;72A:1424–1429.
Hungerford DS, Lennox DW. Rehabilitation of the knee in disorders of the patellofemoral joint: relevant biomechanics. Orthop Clin North Am 1983;14:397–402.
Kujala
UM, Kvist M, Osterman K, et al. Factors predisposing army conscripts to
knee exertion injuries incurred in a physical training program. Clin Orthop Relat Res 1986;210:203–212.
UM, Kvist M, Osterman K, et al. Factors predisposing army conscripts to
knee exertion injuries incurred in a physical training program. Clin Orthop Relat Res 1986;210:203–212.
Theur
PC, Fulkerson JP. Knee. Section E: Patellofemoral joint. Part 6:
Anterior knee pain and patellar subluxation in the adult. In: DeLee JC,
Drez D, Jr, Miller MD, eds. DeLee & Drez’s Orthopaedic Sports Medicine: Principles and Practice, 2nd ed. Philadelphia: WB Saunders Co, 2003:1772–1815.
PC, Fulkerson JP. Knee. Section E: Patellofemoral joint. Part 6:
Anterior knee pain and patellar subluxation in the adult. In: DeLee JC,
Drez D, Jr, Miller MD, eds. DeLee & Drez’s Orthopaedic Sports Medicine: Principles and Practice, 2nd ed. Philadelphia: WB Saunders Co, 2003:1772–1815.
Codes
ICD9-CM
-
717.7 Chondromalacia patella
-
719.46 Patellofemoral pain syndrome
Patient Teaching
-
It is important to stress that surgery
may improve patellar tracking and prevent dislocation or subluxation,
but it is not guaranteed to relieve pain. -
Proper conditioning
-
Avoid training errors such as too rapid increase in mileage/intensity.
FAQ
Q: What radiographs are helpful for evaluating the knee with patellofemoral pain syndrome?
A:
In addition to AP and lateral radiographs of the knee, a standardized
axial or tangential view of the patella (Merchant view) is helpful to
evaluate alignment, tilt, and stability.
In addition to AP and lateral radiographs of the knee, a standardized
axial or tangential view of the patella (Merchant view) is helpful to
evaluate alignment, tilt, and stability.
Q: What should be emphasized in the rehabilitation of patellofemoral pain syndrome?
A:
In addition to identifying and correcting training errors, therapy
should emphasize quadriceps, hamstring, and hip flexor stretching and
strengthening and core strengthening. Patellar taping may help reduce
pain during therapy.
In addition to identifying and correcting training errors, therapy
should emphasize quadriceps, hamstring, and hip flexor stretching and
strengthening and core strengthening. Patellar taping may help reduce
pain during therapy.
Q: When would surgery be considered for anterior knee pain?
A:
Patients with demonstrated patellar malalignment and/or instability for
whom a rigorous rehabilitation program has failed may be candidates for
surgery.
Patients with demonstrated patellar malalignment and/or instability for
whom a rigorous rehabilitation program has failed may be candidates for
surgery.
