Distal Tibial and Fibular Fractures
reported that phalangeal physeal fractures were most common, followed
by physeal injuries of the radius and ankle. Approximately 4% of all
ankle fractures involve the physes.31
In skeletally immature individuals, physeal ankle fractures are
slightly more common than fractures of the tibial or fibular diaphysis.116
number of ankle injuries, including sprains and fractures. Up to 58% of
physeal ankle fractures occur during sports activities64,193 and account for 10% to 40% of all injuries to skeletally immature athletes.132,136,159,178 Physeal ankle fractures are more common in males than in females in some studies.175 Other studies have demonstrated that ankle injuries may be more likely in young female soccer players compared with males.103 Fractures of the ankle are associated with the following sport activities: trampolines,169 scooters,115 soccer,103 basketball,45 skating,131 and downhill skiing.13
associated with a significant number of distal tibia and fibular
fractures in children. These fracture occurs in approximately 10% to
20% of trauma patients presenting to the emergency room.13
Tibial physeal fractures are most common between the ages of 8 and 15
years, and fibular fractures are most common between 8 and 14 years of
age.175
as the most extensive early study of physeal fractures. He pointed out
that in children, ligaments are stronger than physeal cartilage so that
forces that result in ligament damage in adults cause fractures of the
physes in children. In 1922, Ashhurst and Bromer4
published a thorough review of the literature and the results of their
own extensive investigations and described a classification of ankle
injuries based on the mechanism of injury. This classification did not
differentiate between ankle injuries in adults and those in children.
Bishop,10 in 1932, classified 300
ankle fractures according to Ashhurst and Bromer’s system; 33 fractures
were physeal injuries, and the grouping of these injuries according to
mechanism of injury represents one of the first attempts to classify
physeal ankle injuries.
physeal ankle injuries in 1936 is one of the first to attempt to
determine the results of treatment of these injuries; he also outlined
an anatomic classification. Only one of his patients (5%) had a
deformity after fracture, in contrast to McFarland,120 who, in 1932, reported deformities in 40% of a larger series of patients. In 1955, Caruthers and Crenshaw31
reported 54 physeal ankle fractures, which were classified according to
their modification of Ashhurst and Bromer’s system. They confirmed that
growth-related deformities were frequent after adduction (Salter-Harris
type III and IV injuries) fractures and infrequent after fractures
caused by external rotation, abduction, and plantarflexion
(Salter-Harris type II injuries). Spiegel and colleagues,175
in a 1978 review of 237 physeal ankle fractures, reported a high
incidence of growth abnormalities after Salter-Harris type III and IV
injuries but also found complications in 11 (16.7%) of 66 patients with
Salter-Harris type II fractures. Most of these patients had only mild
shortening, but 6 had angular deformities that did not correct with
growth.
Anatomic classifications distinguish fractures based on the regions of
the metaphysis, physis, and epiphysis. Mechanism-of-injury
classifications incorporate the forces that produce the fracture and
the anatomic position of the foot and ankle that existed at the time of
the injury. Most mechanism-of-injury classifications include the
anatomic type of injury produced by a particular mechanism.
 |
|
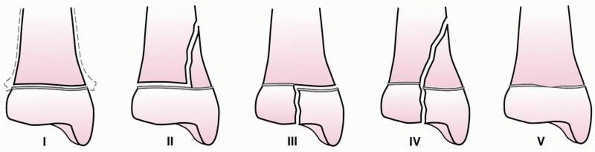
FIGURE 26-1 Salter-Harris anatomic classification as applied to injuries of the distal tibial epiphysis.
|
system has been widely used to describe the anatomic features of
fractures associated with open physes. This straight forward anatomic
classification (Fig. 26-1) is effective for rapid communication. It has five distinct categories, which can be applied to most periarticular regions.
injury may have some advantages. The description of the injury includes
the anatomic deformity and the forces that produced the injury.
Reduction of the displaced fracture may be enhanced by an understanding
of these forces and how they produced the distorted relationship
between the displaced fragments. Advanced imaging techniques that allow
for comprehensive three-dimensional visualization of the fracture
anatomy also facilitate surgical planning and reduction techniques.
can provide useful information for determining appropriate treatment.
The prognoses for growth and deformity have been predicted on the basis
of both types of classification (Table 26-1).88,89,175
A theoretical advantage of mechanism-of-injury classifications is that
identification of the force producing the injury might give even more
information about the possible development of growth arrest than
anatomic classifications. For example, a Salter-Harris type III or IV
fracture of the tibia produced by a shearing (Fig. 26-2)
or crushing force might be more likely to result in growth arrest than
a similar injury produced by an avulsion force. However, it is
difficult to establish that one type of classification is superior to
the other in this regard because of the relatively small numbers of
patients reported, the varying ages of patients in most series, and
questions about the reproducibility of various classifications.
studied the reproducibility of the Lauge-Hansen (mechanism-of-injury)
and Weber (anatomic) classifications in a series of adult ankle
fractures. After all investigators in the study had received a tutorial
on both systems and their application, they were asked to classify 94
fractures. On the first attempt, only the Weber classification produced
an acceptable level of interobserver agreement. On a second attempt,
the Weber classification and most of the Lauge-Hansen classification
achieved an acceptable level of interobserver agreement. These authors
concluded that all fracture classification systems should have
demonstrably acceptable interobserver agreement rates before they are
adopted, an argument made even more forcefully in an editorial by
Burstein.27 Vahvanen and Aalto185 compared their ability to
classify 310 ankle fractures in children with the Weber, Lauge-Hansen,
and Salter-Harris classifications. They found that they were “largely
unsuccessful” using the Weber and Lauge-Hansen classifications but
could easily classify the fractures using the Salter-Harris system.
|
TABLE 26-1 Representative Mechanism of Injury Classifications: Applied Force
|
|||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
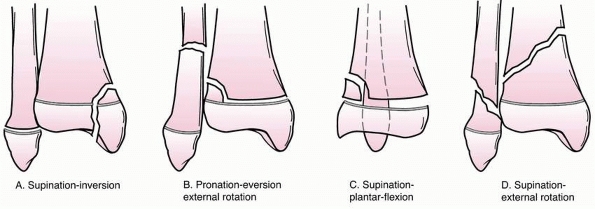
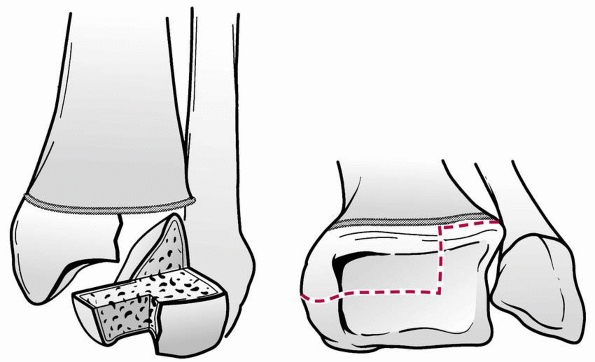
Their original classification (from 1978) consisted of four types in
which the first word refers to the position of the foot at the time of
injury and the second word refers to the force that produces the injury.
axial compression, juvenile Tillaux, triplane, and other physeal
injuries, by Tachjidan.179 Syndesmosis injuries have also been recently described.43
Although these are designated differently, the first three have
presumed mechanisms of injury. “Axial compression injury” describes the
mechanism of injury but not the position of the foot. Juvenile Tillaux
and triplane fractures are believed to be caused by external rotation.
The final category, “other physeal injuries,” includes diverse
injuries, many of which have no specific mechanism of injury.
 |
|
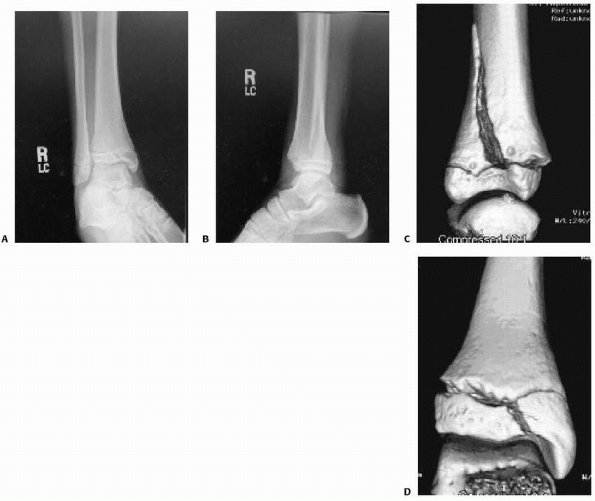
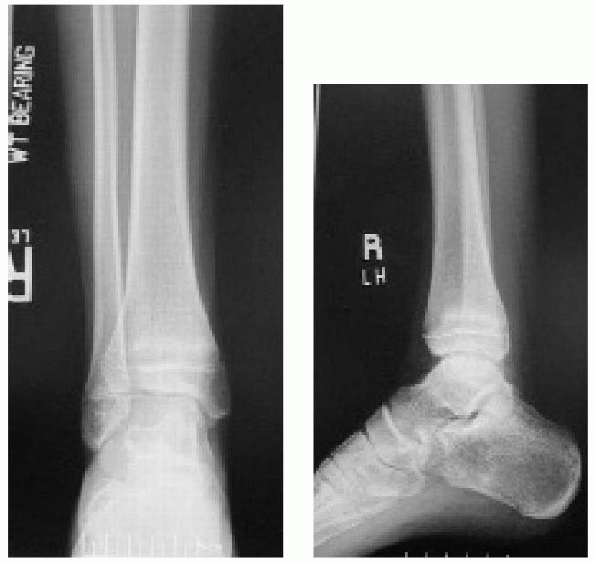
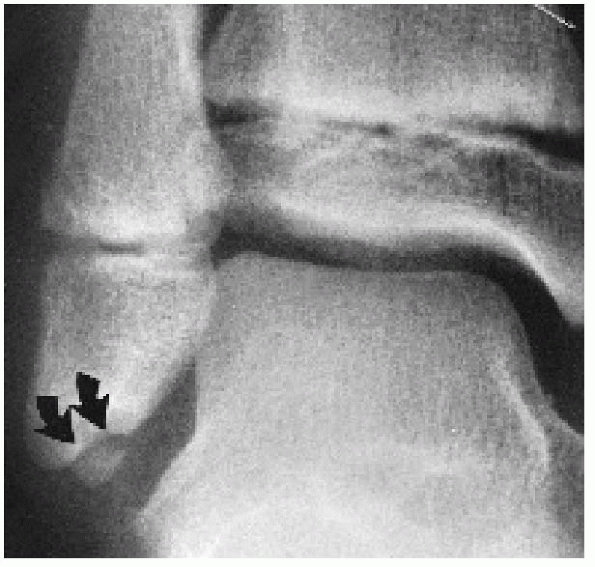
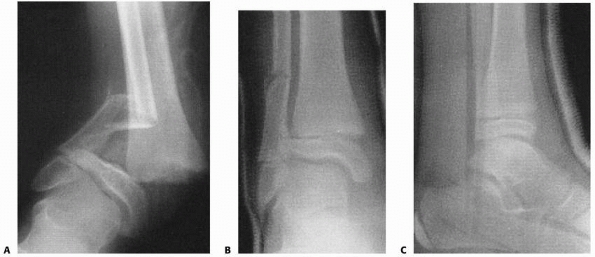
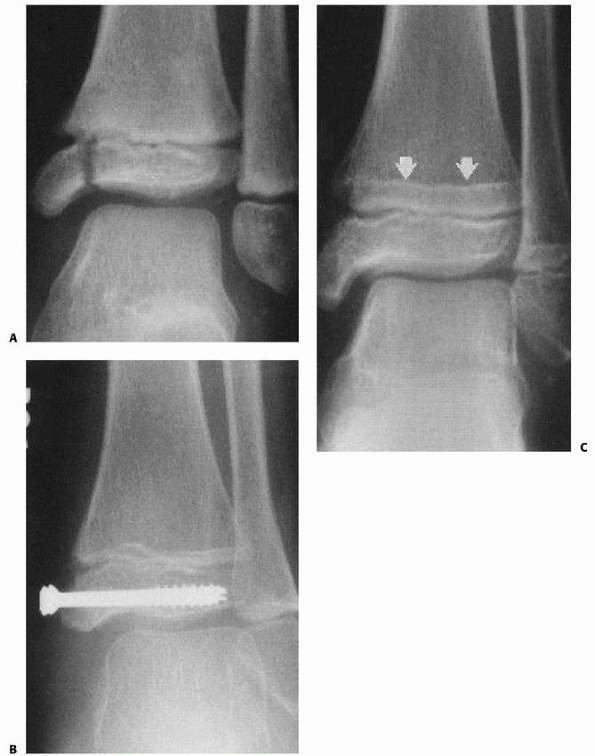
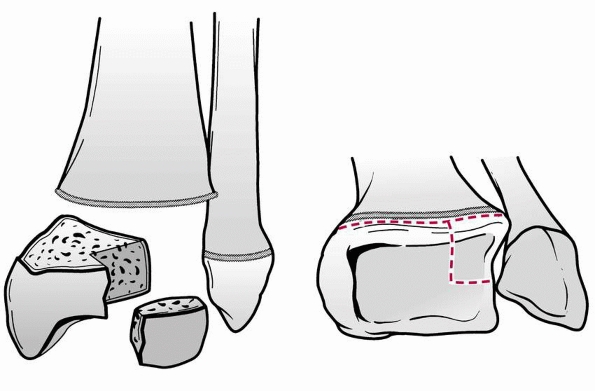
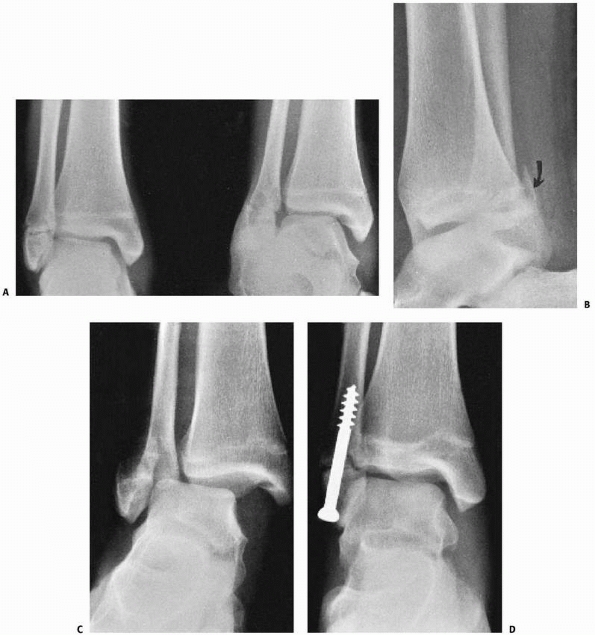
FIGURE 26-2
Comminuted Salter-Harris type IV fracture of the distal tibia and displaced Salter-Harris type I fracture of the distal fibula produced by an inversion (shearing) mechanism in a 10-year-old girl. |
-
Grade I: The adduction or inversion force
avulses the distal fibular epiphysis (Salter-Harris type I or II
fracture). Occasionally, the fracture is transepiphyseal; rarely, the
lateral ligaments fail. -
Grade II (Fig. 26-4):
Further inversion produces a tibial fracture, usually a Salter-Harris
type III or IV and rarely a Salter-Harris type I or II injury, or the
fracture passes through the medial malleolus below the physis (Fig. 26-5).
directly posteriorly, resulting in a Salter-Harris type I or II
fracture. Fibular fractures were not reported with this mechanism. The
tibial fracture may be is difficult to see on anteroposterior
radiographs (Fig 26-6).
-
Grade I: The external rotation force results in a Salter-Harris type II fracture of the distal tibia (Fig. 26-7).
The distal fragment is displaced posteriorly, as in a
supination-plantarflexion injury, but the Thurstan-Holland fragment is
visible on the anteroposterior radiographs, with the fracture line
extending
P.970proximally and medially. Occasionally, the distal tibial epiphysis is rotated but not displaced.
-
Grade II: With further external rotation,
a spiral fracture of the fibula is produced, running from
anteroinferior to posterosuperior (Fig. 26-8).
 |
|
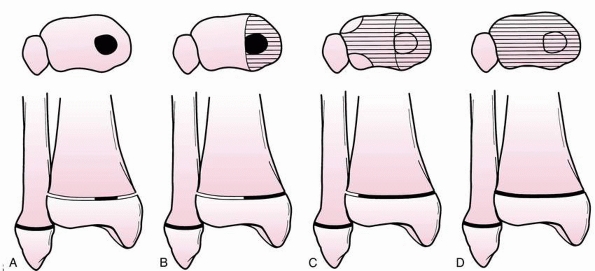
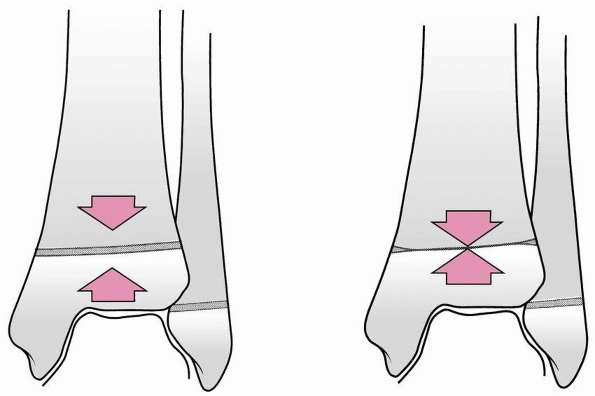
FIGURE 26-3 Dias-Tachdjian classification of physeal injuries of the distal tibia and fibula.
|
 |
|
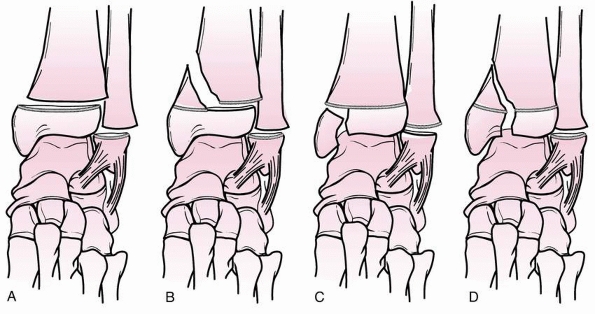
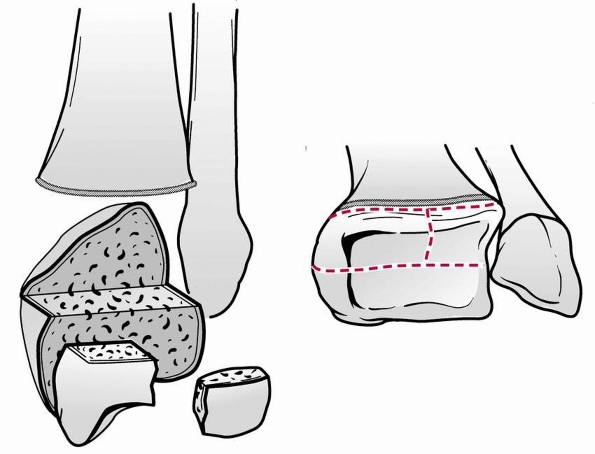
FIGURE 26-4 Variants of grade II supination-inversion injuries (Dias-Tachdjian classification). A. Salter-Harris type I fracture of the distal tibia and fibula. B. Salter-Harris type I fracture of the fibula, Salter-Harris type II tibial fracture. C. Salter-Harris type I fibular fracture, Salter-Harris type III tibial fracture. D. Salter-Harris type I fibular fracture, Salter-Harris type IV tibial fracture.
|
 |
|
FIGURE 26-5 Severe supination-inversion injury with displaced fracture of the medial malleolus distal to the physis of the tibia.
|
 |
|
FIGURE 26-6 Lateral view of a supination plantarflexion injury.
|
 |
|
FIGURE 26-7 Stage I supination-external rotation injury in a 10-year-old child; the Salter-Harris type II fracture begins laterally.
|
 |
|
FIGURE 26-8 Stage II supination-external rotation injury. A. Oblique fibular fracture also is visible on anteroposterior view. B. Lateral view shows the posterior metaphyseal fragment and posterior displacement.
|
tibia occurs simultaneously with a transverse fibular fracture. The
distal tibial fragment is displaced laterally and the Thurstan-Holland
fragment, when present, is lateral or posterolateral (Fig. 26-9).
Less frequently, a transepiphyseal fracture occurs through the medial
malleolus (Salter-Harris type II). Such injuries may be associated with
diastasis of the ankle joint, which is uncommon in children.
pattern over a period of about 18 months, injuries sustained during
this period can produce fracture patterns that are not seen in younger
children with completely open physes.113
This group of fractures has been labeled “transitional” fractures
because they occur during the transition from a skeletally immature
ankle to a skeletally mature ankle. Such fractures, which include
juvenile Tillaux and “triplane” fractures with two to four fracture
fragments, have been described by Kleiger and Mankin,97 Marmor,117 Cooperman and coworkers,39 Karrholm,87 and Denton and Fischer.46 The adolescent pilon fracture has been described by Letts et al.105 The incisural and syndesmosis fractures have been described by Cummings and Hahn44 and Cummings,43 respectively, and these injuries are described below.
that of other distal tibial fractures. Advocates of mechanism-of-injury
systems agree that most juvenile Tillaux and triplane fractures are
caused by external rotation, but they disagree as to the position of
the foot at the time of the injury.47,48,148 Some authors48
classify juvenile Tillaux fractures as stage I injuries, with further
external rotation causing triplane fractures, and still further
external rotation causing stage II injuries with fibular fracture.
Others emphasize the extent of physeal closure as the only determinant
of fracture pattern.38
 |
|
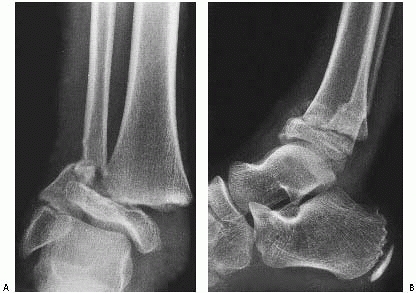
FIGURE 26-9 A.
According to the Dias-Tachdjian classification, this injury in a 12-year-old boy would be considered a pronation-eversion-external rotation injury resulting in a Salter-Harris type II fracture of the distal tibia and a transverse fibular fracture. B. The anterior displacement of the epiphysis, visible on the lateral view, however, makes external rotation an unlikely component of the mechanism of injury; the mechanism is more likely pronation-dorsiflexion. |
the different anatomic configurations triplane fractures may exhibit on
different radiographs projections, making tomography, computed
tomography (CT) scanning, or examination at open reduction necessary to
determine fracture anatomy and number of fragments. Because these
fractures occur near the end of growth, growth disturbance is rare.
Anatomic classification is, therefore, more useful for descriptive
purposes than for prognosis.
 |
|
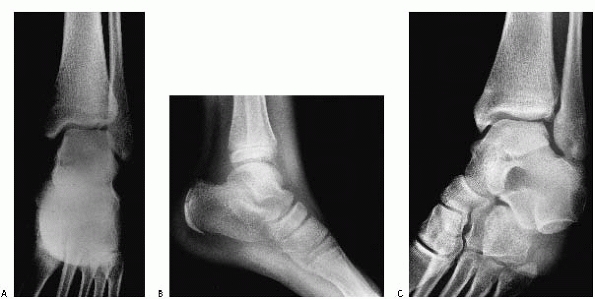
FIGURE 26-10 A. Anteroposterior radiograph of Salter Harris type III/juvenile Tillaux Fracture. B. Lateral radiograph of Salter Harris type III/juvenile Tillaux Fracture.
|
III fracture involving the anterolateral distal tibia. The portion of
the physis not involved in the fracture is closed (Fig. 26-10).
 |
|
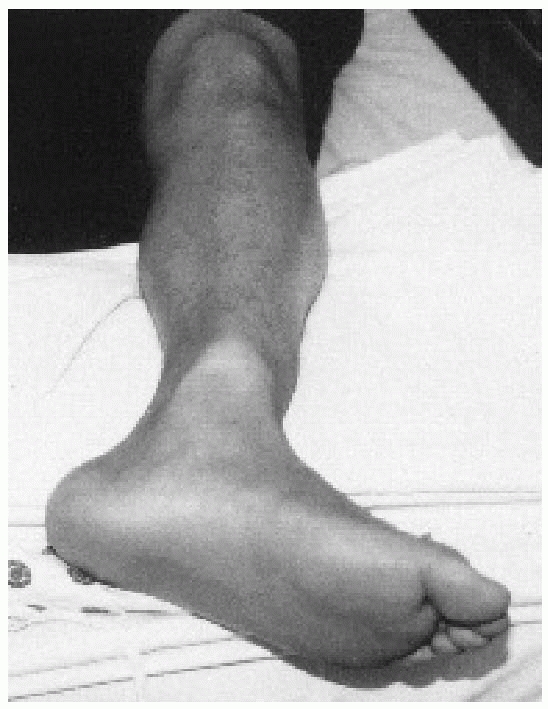
FIGURE 26-11 A. Anteroposterior view of triplane fracture. On this view, the fracture appears to be a Salter-Harris type III configuration. B. Lateral view of triplane fracture. On this view, the fracture appears to be a Salter-Harris type II configuration. C. Three-dimensional CT reconstruction can demonstrate significant metaphyseal displacement. D. Three-dimensional CT reconstruction can demonstrate intra-articular displacement.
|
common the appearance of a Salter-Harris type III fracture on the
anteroposterior radiographs and of a Salter-Harris type II fracture on
the lateral radiographs (Fig. 26-11). CT scans can be very helpful to understand the complex anatomy of these fractures (see Fig. 26-11). It has been proposed that the mechanism of injury for Tillaux and triplane fractures is external rotation.47,148
Some classify juvenile Tillaux fractures as stage I injuries, with
further external rotation leading to triplane fractures and stage three
leading to fibula fractures.47 Others suggest that the degree of physeal closure is the main determinant of fracture pattern.38
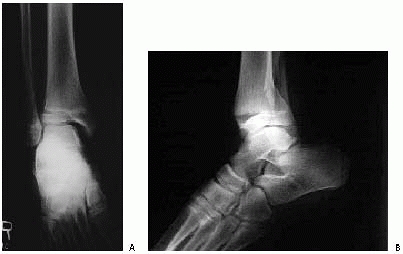
fracture of the “tibial plafond with articular and physeal involvement,
variable talar and fibular involvement, variable comminution, and
greater than 5 mm of displacement” (Fig. 26-12).105 Based upon a small number of cases, Letts et al.105
developed a three part classification system. Type 1 fractures have
minimal comminution and no physeal displacement. Type 2 fractures have
marked comminution and less than 5 mm of physeal displacement. Type 3
fractures have marked comminution and more than 5 mm of physeal
displacement.
on standard radiographs, but the size of the fragment is smaller than
that typically seen with the Tillaux fractures (Fig 26-13).44 On the CT scan, this fracture does not extend to the anterior cortex of the distal tibia (Fig 26-14).
The mechanism of injury may be an avulsion of the fragment by the
interosseous ligament. This may be a variant of an adult tibia-fibular
diastasis injury.
patients. These have been associated with fractures of the distal
fibula, Tillaux injuries, Salter-Harris type I fractures, and proximal
fibula fractures (Figs. 26-15, 26-16 and 26-17). These fractures are probably rare, and there is very limited literature on this injury.140
 |
|
FIGURE 26-12 Anterior posterior and lateral radiographs of an adolescent pilon fracture.
|
These patients may present with warmth, swelling, and pain around the
metaphyseal or physeal regions. In our experience, these injuries are
more common in running/endurance athletes. We have seen stress
fractures through the distal fibular physeal scar in running athletes.
reported, and one of the fractures can be missed if adequate images are
not obtained.81
 |
|
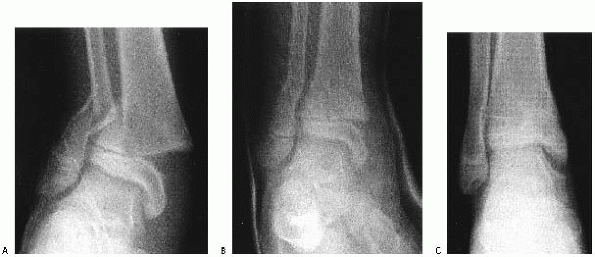
FIGURE 26-13 Anteroposterior (A), lateral (B), and oblique (C) views of the ankle demonstrating an apparent small juvenile Tillaux fracture in a 14-year-old girl.
|
severe pain and obvious deformity. The position of the foot relative to
the leg may provide important information about the mechanism of injury
(Fig. 26-20) and should be considered in planning
reduction. The status of the skin, pulses, and sensory and motor
function should be determined and recorded. Tenderness, swelling, and
deformity in the ipsilateral leg and foot should be noted. In patients
with tibial shaft fractures, the ankle should be carefully evaluated
clinically and radiographically.
 |
|
FIGURE 26-14
Incisural fracture: CT scan at the level of the tibiotalar joint demonstrates that the fracture fragment does not include the attachment of the anterior inferior tibiofibular ligament. |
If patients are admitted to the hospital, discussion with the nursing
staff about signs and symptoms of compartment syndrome are important.
If patients are treated as outpatients, communication with the patient
and family about the possibility of compartment syndrome is also
important. These families should return to the hospital for evaluation
if problems with pain control develop.
 |
|
FIGURE 26-15 A.
Syndesmosis injury with distal fibula fracture. Radiographs with comparison of right and left sides. Note the widening of the medial clear space and the syndesmosis. B. Use of two percutaneous placed cannulated screws to reduce the syndesmosis. |
fractures often have no deformity, minimal swelling, and moderate pain.
Because of their benign clinical appearance, such fractures may be
easily missed if radiographs are not obtained. Petit et al.145
reviewed 2470 radiographs from pediatric emergency rooms, demonstrating
abnormal radiographic findings in 9%. Guidelines known as The Ottawa
Ankle Rules have been established for adults to try to determine which
injuries require radiographs.177 The
indications for radiographs according to the guidelines are complaints
of pain near a malleolus with either inability to bear weight or
tenderness to palpation at the malleolus. Chande36
prospectively studied 71 children with acute ankle injuries to
determine if these guidelines could be applied to pediatric patients
with ankle injuries. It was determined that if radiographs were
obtained only in children with tenderness over the malleoli and
inability to bear weight, a 25% reduction in radiographic examinations
could be achieved without missing any fractures. The physical
examination should focus upon physeal areas of the tibia and fibula
when evaluating ankle injuries to determine if radiographs are
necessary. Interpretation of radiographs should focus upon signs of
physeal injury, including soft tissues swelling in these regions.
swelling only about the ankle, anteroposterior, mortise, and lateral
radiographs centered over the ankle may provide sufficient information
to plan treatment. Although obtaining views of the joint above and
below is recommended for most fractures, obtaining a film centered over
the midtibia to include the knee and ankle joints on the radiographs
significantly decreases the quality of ankle views and is not
recommended.
mortise view of the ankle is essential in addition to anteroposterior
and lateral views. On a standard anteroposterior view, the
lateral
portion of the distal tibial physis is usually partially obscured by
the distal fibula. The vertical component of a triplane or Tillaux
fracture can be hidden behind the overlying fibular cortical shadow.107 A study by Vangsness and coworkers186
found that diagnostic accuracy was essentially equal when using
anteroposterior, lateral, and mortise views compared with using only
mortise and lateral views. Therefore, if only two views are to be
obtained, the anteroposterior view may be omitted and lateral and
mortise views obtained.
 |
|
FIGURE 26-16 Triplane with deltoid injury and syndesmosis widening with stress views. A,B. Injury films. C-E. Postoperative films.
|
 |
|
FIGURE 26-17 A,B. Deltoid and possible syndesmosis injury associated with triplane fracture pattern.
|
 |
|
FIGURE 26-18
Distal tibia stress fracture. A 15-year-old male with 6 weeks of pain while running cross country. Anteroposterior radiograph shows callus formation in the distal tibia metaphysic. |
described two special views designed to detect avulsion fractures from
the lateral malleolus that are not visible on routine views and to
distinguish whether they represent avulsions of the anterior
tibiofibular ligament or the calcaneofibular ligament attachments. The
anterior tibiofibular ligament view is made by positioning the foot in
45 degrees of plantarflexion and elevating the medial border of the
foot 15 degrees. The calcaneofibular ligament view is obtained by
rotating the leg 45 degrees inward.
 |
|
FIGURE 26-19
Stress fracture of distal fibula. A 16-year-old male with 6 weeks of pain while running track. Anteroposterior radiograph shows widened physis. The clinical exam shows point tenderness over the fibular physis. |
 |
|
FIGURE 26-20
Severe clinical deformity in a 14-year-old boy with an ankle fracture. It is obvious without radiographs that internal rotation will be needed to reduce this fracture. |
ligamentous instability, although ligamentous injury at the ankle is
infrequent in skeletally immature patients. Stress views may be
considered to document a Salter-Harris type I fracture, but a patient
with clinical signs of this fracture should be treated appropriately,
regardless of stress-view findings.
studied the age at which the radiographic appearance of the incisura
fibularis, tibiofibular clear space, and tibiofibular overlap develop
in children. The purpose of their study was to facilitate the diagnosis
of distal tibiofibular syndesmotic injury in children. They found that
the incisura became detectable at a mean age of 8.2 for girls and 11.2
years for boys. The mean age at which tibiofibular overlap appeared on
the anteroposterior view was 5 years for both sexes; on the mortise
view, it was 10 years for girls and 16 years for boys. The range of
clear space measurements in normal children was 2 to 8 mm with 23% of
children having a clear space greater than 6 mm, a distance considered
abnormal in adults.
although many imaging departments no longer provide this modality. CT
evaluations involve less radiation to the patient. Cuts are generally
made in the transverse plane. With thin cuts localized to the joint, it
is possible to generate high-quality reconstructions that allow
evaluation in the coronal and sagittal planes without repositioning the
ankle. With plain tomography, the transverse anatomy can only be
deduced from the anteroposterior and lateral tomograms.
Three-dimensional CT reconstructions may add further useful
information, and readily available software packages allow easy
production of such images (Fig. 26-22). These images can assist with minimally
invasive approaches and the use of percutaneous reduction clamps and screws.
 |
|
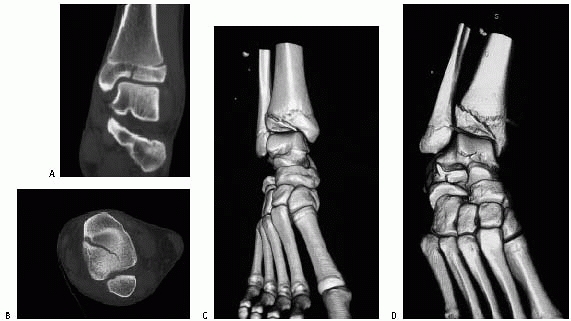
FIGURE 26-21 Coronal and sagittal CT images of Tillaux fracture A. CT scan sagittal image of juvenile Tillaux fracture. Note the degree of intra-articular displacement. B. CT scan coronal image of juvenile Tillaux fracture. C. CT scan can facilitate screw placement/orientation. D. Reduction with intraepiphyseal screws.
|
 |
|
FIGURE 26-22 Three-dimensional CT reconstruction of juvenile Tillaux fracture. A. Coronal CT image of minimally displaced juvenile Tillaux fracture. B. Sagittal CT Image of minimally displaced juvenile Tillaux fracture. C,D. Three-dimensional reconstruction of juvenile Tillaux fracture.
|
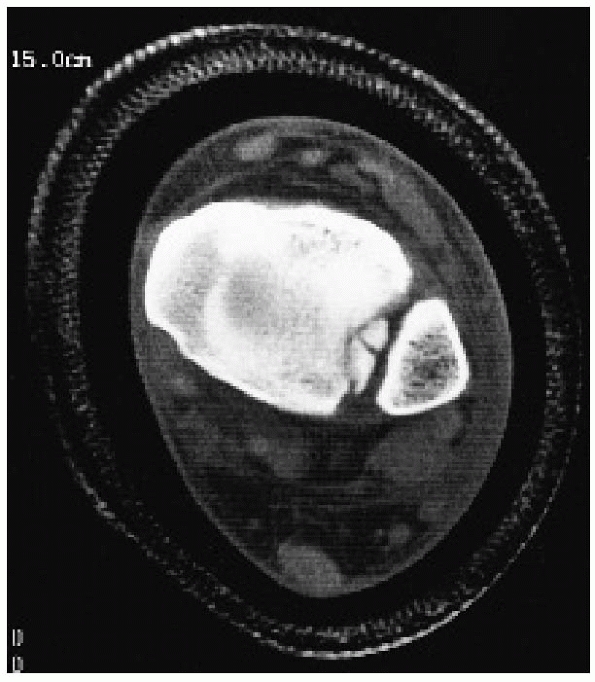
evaluation complex fractures of the distal tibia and ankle in patients
with open physes. Smith and associates174
found that of 4 patients with acute (3 to 10 days) physeal injuries,
MRI showed that 3 had more severe fractures than indicated on plain
films (Fig. 26-23). Early MRI studies (3 to 17
weeks after injury) not only added information about the pattern of
physeal disruption but also supplied early information about the
possibility of growth abnormality. MRI has been reported to be
occasionally helpful in the identification of osteochondral injuries to
the joint surfaces in children with ankle fractures.95
Although these injuries may be more common in adolescent and adult
fractures, we believe that these type of injuries are rare in younger
patients.
obtained MRI studies on 14 patients with known or suspected growth
plate injury. The MRI detected five radiographically occult fractures
in the 14 patients, changed the Salter-Harris classification in two
cases, and resulted in a change in treatment plan in 5 of the 14
patients studied. These studies would seem to contradict an earlier
study by Petit et al.144 that showed
only 1 patient in a series of 29 patients in whom MRI revealed a
diagnosis different from that made on plain films. Iwinski-Zelder et al.80 found that the MRI changed the management in 4 of 10 patient with ankle fractures seen on plain radiographs. Seifer et al.168
found the MRI identified physeal injuries that were not identified by
plain radiographs. At this time, the indications for MRI in the
evaluation of ankle fractures in skeletally immature patients are still
being defined, but this imaging modality may be a more sensitive tool
for identification of minimally displaced or more complex injuries. If
physeal arrest occurs, MRI scans have been reported useful for mapping
physeal bars.60,73
anatomic variations may cause confusion in the interpretation of plain
films of the ankle (Fig. 26-24). In a group of 100 children between the ages of 6 and 12 years, Powell149
found accessory ossification centers on the medial side (os subtibiale)
in 20% and on the lateral side (os subfibulare) in 1%. If they are
asymptomatic on clinical examination, these ossification centers are of
little concern, but tenderness localized to them may indicate an
injury. Stress views to determine motion of the fragments or bone
scanning may occasionally be considered if an injury to an accessory
ossification center is suspected.
 |
|
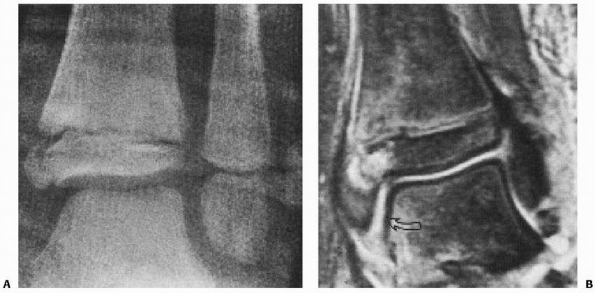
FIGURE 26-23 A.
Follow-up radiograph of a 7-year-old boy 1 week after an initially nondisplaced Salter-Harris type III fracture from a supination-inversion injury of the distal tibia. B. Because of the incomplete ossification of this area and concern that the fracture might have displaced, MRI was performed. Note that the distance between the medial malleolus and the talus is greater than the distance between the talus and the distal tibia or lateral malleolus, confirming displacement of the fracture. |
 |
|
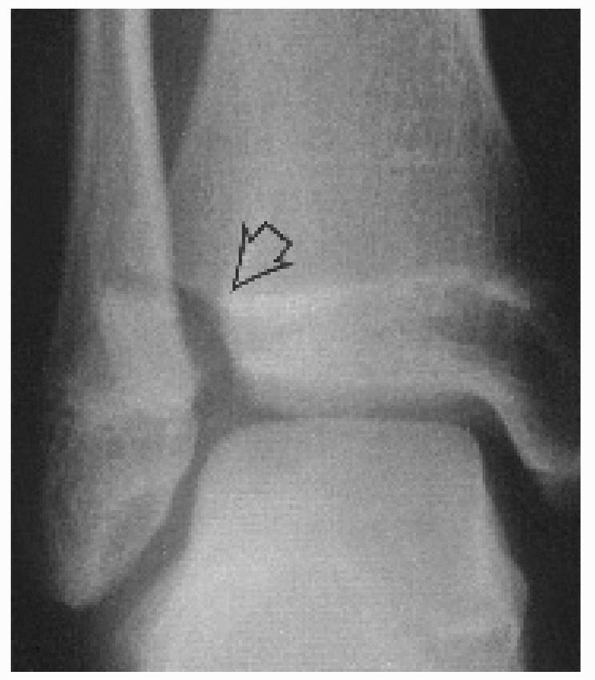
FIGURE 26-24 Secondary ossification center in the lateral malleolus (arrows)
of a 10-year-old girl. Note the smooth border of the fibula and the ossification center. She also has a secondary ossification center in the medial malleolus. |
simulate juvenile Tillaux fractures, and clefts in the medial side may
simulate Salter-Harris type III fractures.94 The presence of these
clefts on an radiographs of a child with an ankle injury may result in
overtreatment if they are misdiagnosed as a fracture. Conversely,
attributing a painful irregularity in these areas to anatomic variation
may lead to undertreatment (Fig. 26-25).
Other anatomic variations include a bump on the distal fibula that
simulates a torus fracture and an apparent offset of the distal fibular
epiphysis that simulates a fracture.
 |
|
FIGURE 26-25 A.
Mortise view of the ankle of a 10-year-old girl who had slight swelling and tenderness at the medial malleolus after an “ankle sprain.” The ossicle at the tip of the medial malleolus was correctly identified as an os subtibiale. A subtle line extending from the medial physis to just distal to the medial tibial plafond (arrow) was believed to also be an anatomic variant. B. Four weeks after injury, soreness persisted and radiographs clearly demonstrated a displaced Salter-Harris type III fracture. |
hinge joint. It is the articulation between the talus and the ankle
mortise, which is a syndesmosis consisting of the distal tibial
articular surface, the medial malleolus, and the distal fibula or
lateral malleolus.
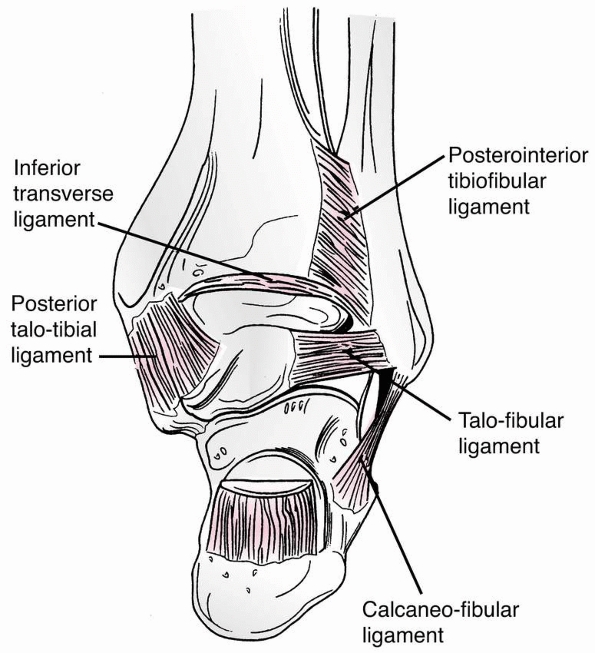
The anterior and posterior inferior tibiofibular ligaments course
inferiorly from the anterior and posterior surfaces of the distal
lateral tibia to the anterior and posterior surfaces of the lateral
malleolus. The anterior ligament is important in the pathomechanics of
“transitional” ankle fractures. Just anterior to the posteroinferior
tibiofibular ligament is the broad, thick inferior transverse ligament,
which extends down from the lateral malleolus along the posterior
border of the articular surface of the tibia, almost to the medial
malleolus. This ligament serves as a part of the articular surface for
the talus. Between the anterior and posterior inferior tibiofibular
ligaments, the tibia and fibula are bound by the interosseous ligament,
which is continuous with the interosseous membrane above. This ligament
may be important in the pathomechanics of what we have termed incisural
fractures.
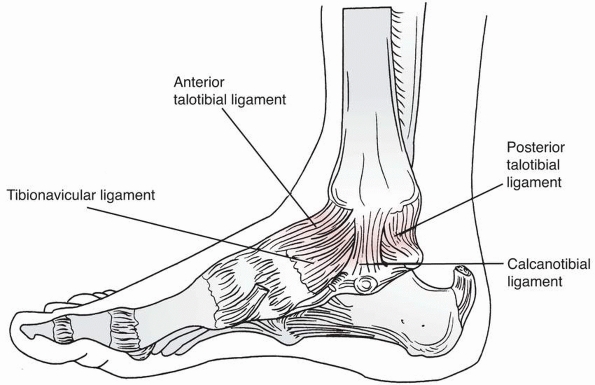
This ligament arises from the medial malleolus and divides into
superficial and deep layers. Three parts of the superficial layer are
identified by their attachments: tibionavicular, calcaneotibial, and
posterior talotibial ligaments. The deep layer is known as the anterior
talotibial ligament, again reflecting its insertion and origin. On the
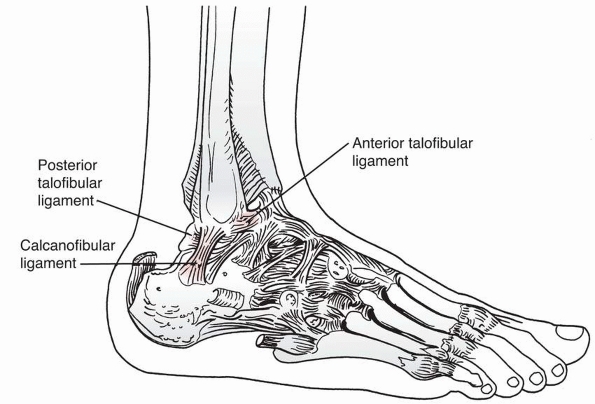
lateral side, the anterior and posterior talofibular ligament, with the
calcaneofibular ligaments, make up the lateral collateral ligament (see
Fig. 26-28).
the medial and lateral malleolae to the talus, and the distal tibial
epiphysis to the distal fibular epiphysis are attached to the malleolae
distal to the physes. Because the ligaments are stronger than the
physes,
physeal fractures are more common than ligamentous injuries in
children. When they accompany distal tibial physeal injuries, displaced
diaphyseal fibular fractures are usually associated with injuries to
and displacement of the entire distal tibial epiphysis rather than with
injuries to the ligaments, making diastasis of the ankle uncommon in
children (Fig. 26-29).
 |
|
FIGURE 26-26 Posterior view of the distal tibia and fibula and the ligaments making up the ankle mortise.
|
 |
|
FIGURE 26-27 Medial view of the ankle demonstrating the components of the deltoid ligament.
|
at 6 to 24 months of age. Its malleolar extension begins to form around
the age of 7 or 8 years and is mature or complete at the age of 10
years. The medial malleolus develops as an elongation of the distal
tibia ossific nucleus, although in 20% of cases, this may originate
from a separate ossification center, the os tibial. This can be
mistaken as a fracture.92 The physis
usually closes around the age of 15 years in girls and 17 years in
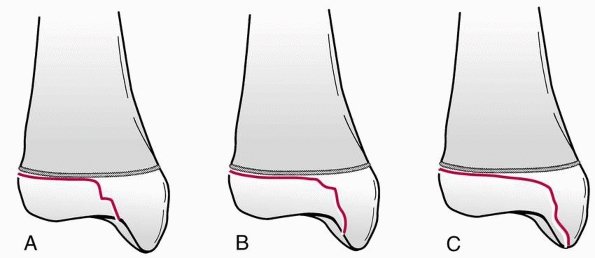
boys. This process takes approximately 18 months and occurs first in
the central part of the physis, extending next to the medial side, and
finally ending laterally. This asymmetric closure sequence is an
important anatomic feature of the growing ankle and is responsible for
the Tillaux fracture in adolescents (Fig. 26-30).
 |
|
FIGURE 26-28 Lateral view of the ankle demonstrating the anterior and posterior talofibular ligaments and the calcaneofibular ligament.
|
the age of 9 to 24 months. This physis is located at the level of the
ankle joint. Closure of this physis generally follows closure of the
distal tibial physis by 12 to 24 months.
anatomic landmarks, as surgical exposures should aim to protect these
structures. The superficial peroneal nerve branches may be most
vulnerable around the ankle, especially during arthroscopic and
arthrotomy approaches for triplane and Tillaux fractures.11
This is important when arthroscopic and percutaneous reduction
techniques are employed for fracture treatment (refer to section on
arthroscopic and percutaneous reduction techniques.)
depends on the location of the fracture, the degree of displacement,
and the age of the child (Table 26-2). Nondisplaced fractures may be
simply immobilized. Closed reduction and cast immobilization may be
appropriate for displaced fractures; if the closed reduction cannot be
maintained with casting, skeletal fixation may be necessary. If closed
reduction is not possible, open reduction may be indicated, followed by
internal fixation or cast immobilization.
 |
|
FIGURE 26-29 A.
Pronation-external rotation injury resulting in a Salter-Harris type I fracture of the distal tibial physis. Note that despite this severe displacement, the relationship between the distal epiphysis of the tibia and distal fibula is preserved, and a diastasis is not present. B,C. Anteroposterior and lateral radiographs demonstrate satisfactory closed reduction. |
the Salter-Harris classification), the mechanism of injury, and the
amount of displacement of the fragments are important considerations.
When the articular surface is disrupted, the amount of articular
step-off or separation must be measured. The neurovascular status of
the limb or the status of the skin may require emergency treatment of
the fracture and associated problems. The general health of the patient
and the time since injury must also be considered.
Salter-Harris type I fractures of the distal tibia can be caused by any
of four mechanisms: supination-inversion, supination-plantarflexion,
supination-external rotation, or pronation-eversion-external rotation.
Spiegel and associates175 reported
that these fractures accounted for 15.2% of 237 ankle injuries in their
series and occurred in children significantly younger (average age,
10.5 years) than those with other Salter-Harris types of fractures.
 |
|
FIGURE 26-30 Closure of the distal tibial physis begins centrally (A), extends medially (B) and then laterally (C) before final closure (D).
|
direction of displacement of the distal tibial epiphysis; for example,
straight posterior displacement indicates a supination-plantarflexion
mechanism. The type of associated fibular fracture is also indicative
of the mechanism of injury; for example, a high, oblique, or transverse
fibular fracture indicates a pronation-eversion-external injury, while
a lower spiral fibular fracture indicates a supination-external
rotation injury. Lovell,112 Broock and Greer,22 and Nevelos and Colton130
reported unusual Salter-Harris type I fractures in which the distal
tibial epiphysis was externally rotated 90 degrees without fracture of
the fibula or displacement of the tibial epiphysis in any direction in
the transverse plane.
Salter-Harris type I fractures of the distal tibia. A below-knee cast
worn for 3 to 4 weeks may suffice, with the first 2 to 3 weeks limited
to nonweight bearing. An above-knee cast may also be used, although
this may not be necessary as these fractures are usually very stable.
In very active patients that may not comply with
activity/weight-bearing restrictions, this type of cast may be an
advantage. After cast removal, use of a removable leg/ankle immobilizer
may be used, followed by a therapy program in older patients or those
trying to return to competitive sports at an earlier time. In our
experience, formal supervised therapy is not usually necessary in
younger patients. The normal activity of these children is usually
sufficient therapy. For older children and adolescents, a formal
supervised therapy program may be beneficial, especially in those
trying to return to high-level sports.
|
TABLE 26-2 Current Treatment Options
|
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
reduction and cast immobilization. An above-knee nonweight-bearing cast
is preferable initially, as this should reduce the risk of displacement
after reduction. These casts may be changed to a short-leg walking cast
or removable walking boot at 3 to 4 weeks. These fractures can displace
in the first 1 to 2 weeks postoperatively, and close follow-up for this
is necessary. One of the authors (Kevin G. Shea) frequently places one
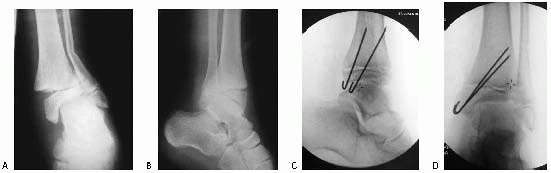
or two Kirschner wires at the time of closed reduction, to prevent
displacement after reduction, under anesthesia (Fig. 26-31).
These pins are usually removed in the clinic 2 to 3 weeks after
placement. As the pins are stabilizing the reduction, a below-knee cast
can be used.
 |
|
FIGURE 26-31 A,B. Displaced distal tibial Salter-Harris type II fracture, with distal diaphyseal fibula fracture. C,D. Fracture treated with closed reduction and internal fixation.
|
Salter-Harris type II fractures were the most common injuries (44.8%).
In addition to the direction of displacement of the distal tibial
epiphysis and the nature of any associated fibular fracture, the
location of the Thurstan-Holland fragment is helpful in determining the
mechanism of injury; for example, a lateral fragment indicates a
pronation-eversion-external rotation injury; a posteromedial
fragment, a supination-external rotation injury; and a posterior fragment, a supination-plantarflexion injury (Fig. 26-32).
 |
|
FIGURE 26-32 A. Severe plantarflexion injury with severe swelling of the ankle and foot; the reduction obtained was unstable. B. The reduction was stabilized by two transmetaphyseal screws placed percutaneously. C. Anteroposterior view confirms an anatomic reduction.
|
immobilization usually with an above-knee cast for approximately 3
weeks, followed by a below-knee walking cast or removable cast/walking
boot for another 2 to 3 weeks.
significantly displaced Salter-Harris type II ankle fracture should be
attempted, opinions differ as to what degree of residual displacement
or angulation is unacceptable and requires open reduction. Based on
follow-up of 33 Salter-Harris type II ankle fractures, Caruthers and
Crenshaw31 concluded that “accurate
reposition of the displaced epiphysis at the expense of forced or
repeated manipulation or operative intervention is not indicated since
spontaneous realignment of the ankle occurs even late in the growing
period.” They found no residual angulation at follow-up in patients who
had up to 12 degrees of tilt after reduction, even in patients as old
as 13 years of age at the time of injury. Spiegel and associates,175
however, reported complications at follow-up in 11 of 16 patients with
Salter-Harris type II ankle fractures. Because 6 of these 11 patients
had angular deformities that were attributed to lack of adequate
reduction of the fracture, Spiegel and associates recommend “precise
anatomic reduction.”
reviewed a series of Salter-Harris type I and II fractures. In patients
with more than 3 mm of physeal widening, the risk of physeal arrest was
60%, compared with 17% in patients with less than 3 mm of physeal
widening. Although they were unable demonstrate a significant decrease
in partial physeal arrest in those treated with surgery, they
recommended open reduction and removal of the entrapped periosteal flap.
reported 3 patients in whom the interposed soft tissue included the
neurovascular bundle, resulting in circulatory embarrassment when
closed reduction was attempted. In this situation, open reduction and
extraction of the soft tissue obviously is required. A less definitive
indication for open reduction is interposition of
the
periosteum, which causes physeal widening with no angulation or with
minimal angulation. Good results have been reported after open
reduction and extraction of the periosteal flap (Fig. 26-33).99
It is not clear that failure to extract the periosteum in such cases
results in problems sufficient to warrant operative treatment.
Wattenbarger,189 Pfieffer,146
and others have attempted to determine the relationship between physeal
bar formation and interposed periosteum, although at this time it is
unclear if the periosteal flap increases the risk of physeal arrest.
 |
|
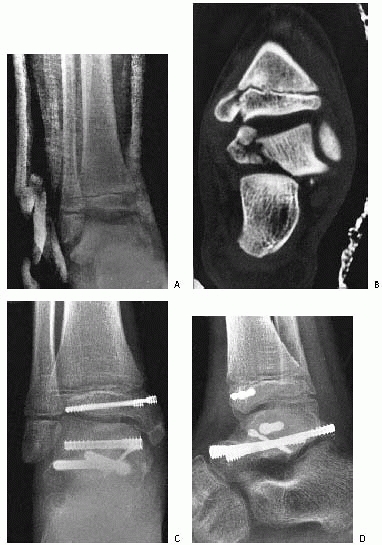
FIGURE 26-33 A. Severely displaced pronation-eversion-external rotation injury. B.
Closed reduction was unsuccessful, and a valgus tilt of the ankle mortise was noted. At surgery, soft tissue was interposed laterally (arrows). C. Reduction completed and stabilized with two cancellous screws placed above the physis. |
tibial physis during closed reduction, many authors recommend the use
of general anesthesia with adequate muscle relaxation for all patients
with Salter-Harris type II distal tibial fractures. However, no study
has compared the frequency of growth abnormalities in patients with
these fractures reduced under sedation and local analgesia to those
with fractures reduced with the use of general anesthesia. One of the
authors (R. Jay Cummings) compared 9 patients who underwent closed
reduction in the emergency department with the use of sedation and
hematoma block to 9 patients who had closed reduction in the operating
room with the use of general anesthesia. All fractures were reduced
with a single manipulation, except for one in the emergency department
group that required repeat manipulation. One patient in each group had
a growth alteration. One of the authors uses general anesthesia, and an
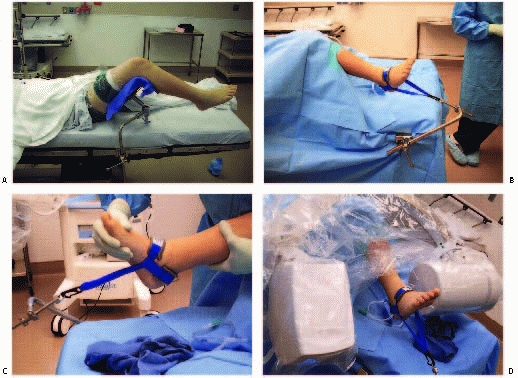
arthroscopic ankle
distractor
to distract the fracture before reduction, with the theoretical
advantage of reducing the risk of physeal damage during the reduction
maneuver (Fig. 26-34).
 |
|
FIGURE 26-34 Use of ankle distractor A. Thigh positioner to allow for ankle distractor. B. Sterile ankle distractor in place. C. Distractor can remain in place during reduction maneuvers. D. C-arm can be brought into the field to evaluate the reduction.
|
anesthesia, they are usually done under intravenous (IV) sedation.
Furia et al.41 demonstrated
significantly improved pain relief with hematoma block for ankle
fractures in a study comparing patients treated with IV sedation to
patients receiving hematoma block. IV regional anesthesia or Bier block
has also been reported to be effective for pain relief in lower
extremity injuries.102
general anesthesia is the ease with which percutaneous pins can be
placed to maintain reduction of the fractures. It is the experience of
one of the authors that Salter-Harris type I and II fractures will
occasionally displace after closed reduction and above-knee casting. If
there is any concern about redisplacement or stability, pins can be
placed at that time.
to 3 days after the fracture should lead one to consider the potential
for compartment syndrome. In fractures that have a higher risk of
compartment syndrome, regional anesthesia, especially peripheral nerve
blocks with longer acting agents, might delay the recognition of a
compartment syndrome.
together because their mechanism of injury is the same
(supination-inversion) and their treatment and prognosis are similar.
Juvenile Tillaux and triplane fractures are considered separately. In
the series of Spiegel and associates,175
24.1% of the fractures were Salter-Harris type III injuries and 1.4%
were type IV. These injuries are usually produced by the medial corner
of the talus being driven into the junction of the distal tibial
articular surface and the medial malleolus. As the talus shears off the
medial malleolus, the physis may also be damaged (Fig. 26-35).
can be treated with above-knee cast immobilization, but care must be
taken to be sure the significant intra-articular displacement is not
present. Radiographs frequently underestimate the degree of
intra-articular involvement and step-off of the articular surfaces. CT
scans may be necessary to fully appreciate the degree of displacement
(see Fig. 26-11). Follow-up radiographs and/or
CT scans in the first 2 weeks may also be necessary to confirm that no
displacement occurs after casting.
have a significant risk of physeal arrest. One study suggested that the
rate of physeal arrest could be reduced by the use of open reduction
and internal fixation.92,100
 |
|
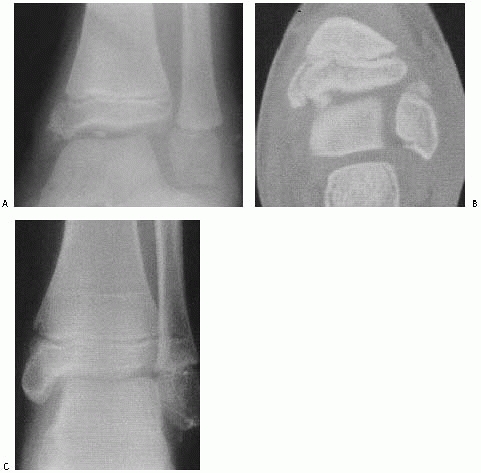
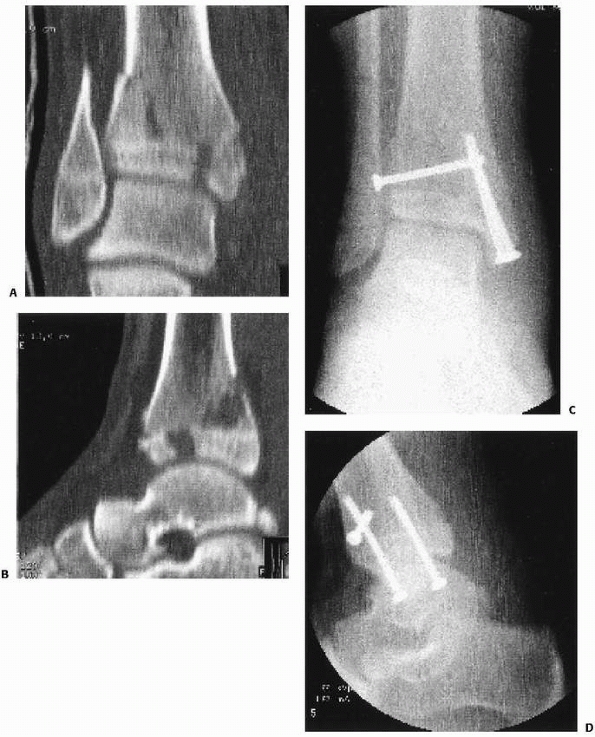
FIGURE 26-35 A.
Severe ankle injury sustained by an 8-year-old involved in a car accident. The anteroposterior view in the splint does not clearly show the Salter-Harris type IV fracture of the tibia. The dome of the talus appears abnormal. B. CT scan shows the displaced Salter-Harris type IV fracture of the medial malleolus and a severe displaced intra-articular fracture of the body of the talus. C,D. Open reduction of both fractures was performed, and Herbert screws were used for internal fixation. (Courtesy of Armen Kelikian, MD.) |
displaced intra-articular fractures require as anatomic a reduction as
possible. Studies in children confirming the importance of articular
reduction to within 2 mm are lacking,166
although most recommend articular reduction in displaced fractures
involving the articular surface. Failure to obtain anatomic reduction
may result in articular incongruity and posttraumatic arthritis, which
often becomes symptomatic 5 to 8 years after skeletal maturity.34
The risk of growth arrest has also been linked to the adequacy of
reduction, although the literature is still unclear if anatomic
reduction reduces the risk of physeal arrest (Fig. 26-36).100
Closed reduction may be attempted but is likely to succeed only in
minimally displaced fractures. If closed reduction is obtained, it can
be maintained with a cast or with percutaneous pins or screws
supplemented by a cast.
methods, open reduction and internal fixation or mini-open arthroscopic
reduction should be carried out. Lintecum and Blasier108
described a technique of open reduction achieved through a limited
exposure of the fracture with the incision centered over the fracture
site combined with percutaneous cannulated screw fixation. This
technique was performed on 13 patients: eight Salter-Harris IV
fractures, four Salter-Harris III fractures, and one triplane fracture.
The authors reported one growth arrest at follow-up averaging 12
months. Beaty and Linton8 reported a Salter-Harris type III fracture with an intra-articular fragment (Fig. 26-37);
these fractures require open reduction for inspection of the joint to
ensure that no osteochondral fragments are impeding reduction.
Arthroscopic evaluation of the joint may also be an option. Internal
fixation devices should be inserted
within the epiphysis, parallel to the physis, and should avoid the physis and ankle joint if possible (Fig. 26-38).
 |
|
FIGURE 26-36 A. Anteroposterior view of a patient with a pronation-eversion external rotation fracture. B. Postreduction view shows residual gapping of physis suggesting periosteal interposition. C. Anteroposterior view obtained for a new injury (medial malleolar fracture) shows premature closure of the physis.
|
 |
|
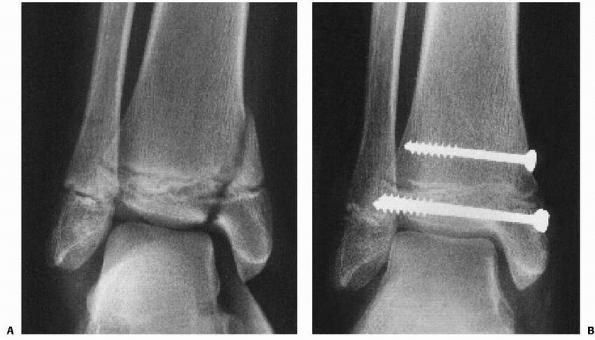
FIGURE 26-37 A.
Salter-Harris type III fracture of the medial malleolus and Salter-Harris type I fracture of the fibula in a 9-year-old girl. An intra-articular fragment was visible only on a mortise view radiograph. B. CT scan outlined the Salter-Harris type III fracture of the medial malleolus and the fragment of bone. C. Two years after excision of the osteochondral fragment, open reduction of the malleolar fracture, and internal fixation. (A,B, reprinted from Beaty JH, Linton RC. Medial malleolar fracture in a child: a case report. J Bone Joint Surg Am 1988;70:1254-1255, with permission.) |
 |
|
FIGURE 26-38 A.
Grade II supination-inversion injury in a 12-year-old girl, resulting in a displaced Salter-Harris type IV fracture of the distal tibia and a nondisplaced Salter-Harris type I fracture of the distal fibula. B. After anatomic open reduction and stable internal fixation. |
intra-articular involvement has been described by several centers.
Jennings et al.82 presented a series
of five triplane and one Tillaux fractures treated with arthroscopic
assistance. The outcome was excellent for fracture reduction and ankle
function.82 Kaya et al.93
reviewed 10 patients with juvenile Tillaux fractures treated with
arthroscopic assistance, demonstrating excellent reduction and clinical
outcomes.137 One of the primary
advantages of arthroscopic fixation is that it allows for visualization
of the articular surfaces, although the need for open reduction of the
metaphyseal and epiphyseal regions may still require open incisions.
Kirschner-wires, small fragment cortical and cancellous screws, and
4-mm cannulated screws (Fig. 26-39). Several reports9,18,26 have advocated the use of absorbable pins for internal fixation of ankle fractures. Benz and colleagues9
reported no complications or growth abnormalities after the use of
absorbable pins with metal screw supplementation for fixation of five
ankle fractures in patients between the ages of 5 and 13 years. In
reports of the use of absorbable pins without supplemental metal
fixation in adults,15,16,59,76
complications have included displacement (14.5%), sterile fluid
accumulation requiring incision and drainage (8.1%), pseudarthrosis
(8%), distal tibiofibular synostosis (3.8%), and infection (1.6%).
Bucholz and coworkers17 reported few
complications in a series of fractures in adults fixed with absorbable
screws made of polylactide and suggested that complications in earlier
series might be related to the fact that those pins were made of
polyglycolide. A report in 1993 by Bostman and associates,18
however, included few complications in a series of fractures in
children fixed with polyglycolide pins. A follow-up report by Rokkanen
et al.158 in 1996 reported 3.6% infection and 3.7% failure of fixation.
compared the cost effectiveness of absorbable implants in 994 patients
treated with absorbable implants to 1173 patients treated with metallic
implants. To be cost effective, the hardware removal rates required
were calculated to range from 19% for metacarpal fractures to 54% for
trimalleolar fractures.17 At this time, the use of absorbable pins remains investigational.
generation bioabsorbable screws have lower complication rates, and
their use may be increasing.150,173
Additional studies in adult patients using ultrasound and MRI have not
detected deleterious effects on healing with newer screw designs.68,118
Because children are typically smaller and lighter than adults, the
implants used for fixation may not need to be as strong or large as
those required by adult patients. This suggests that younger patients
may be better candidates for these bioabsorbable implants. The presence
of the physis and the low grade inflammation that may accompany the
dissolution of these implants may increase the risk of physeal arrest,
and additional studies in adult and pediatric patients will be
necessary to confirm the effectiveness and safety of these devices.91
As originally described, these injuries are not associated with
displacement of the epiphysis relative to the metaphysis, which make
diagnosis of acute injury impossible from plain radiographs; the
diagnosis can only be made on follow-up radiographs when premature
physeal closure is evident. Spiegel and associates175 have designated comminuted fractures that are otherwise unclassifiable as Salter-Harris type V injuries.
to establish because of the difficulty of diagnosing acute injuries. Spiegel and associates175 included two type V fractures in their series, but both were comminuted fractures rather than the classic crush injury.
 |
|
FIGURE 26-39 A. Supination-inversion injury with a Salter-Harris type III fracture of the medial malleolus. B. Six months after open reduction and internal fixation with two transepiphyseal cannulated screws. C. Eighteen months after injury, the fracture has healed with no evidence of growth arrest or angular deformity. (Arrows note normal, symmetric Park-Harris growth arrest line.)
|
 |
|
FIGURE 26-40 Compression-type injury of the tibial physis. Early physeal arrest can cause leg-length discrepancy.
|
specific treatment recommendations have been formulated. Treatment is
usually directed primarily toward the sequelae of growth arrest that
invariably follows Salter-Harris type V fractures. Perhaps more
sophisticated scanning techniques will eventually allow identification
and localization of areas of physeal injury so that irreparable damaged
cells can be removed and replaced with interposition materials to
prevent growth problems, but at present this diagnosis is made only
several months after injury.
subtibiale) and distal fibula (os fibulare) are common and may be
injured.
Treatment usually consists of cast immobilization for 3 to 4 weeks. Ogden and Lee135
reported good results after cast immobilization in 26 of 27 patients
with injuries involving the medial side of the tibia; only 1 patient
required surgery. In contrast, 5 to 11 patients with injuries involving
the lateral side had persistent symptoms that required excision. Bone
scan may be used to help identify these injuries and to help to
distinguish between normal accessory growth centers versus symptomatic
accessory growth centers after injury. Ogden and Lee135 recommend surgical excision in cases that do not respond to cast immobilization and remain chronically symptomatic.
and fibular physes, with physeal disruption, have been described. Most
of these injuries are caused by skiving of the bone by machinery such
as lawn mowers. They may result in growth arrest or retardation and in
angular deformities (see open fractures and lawn mower injuries.)
fracture described in adults by the French surgeon Tillaux. It occurs
when with external rotation of the foot, the anterior-inferior
tibiofibular ligament through its attachments to the anterolateral
tibia avulses a fragment of bone corresponding to the portion of the
distal tibial physis that is still open (Fig. 26-41). In the series of Spiegel and associates,175 these fractures occurred in 2.9% of patients.
The fibula usually prevents marked displacement of the fracture and
clinical deformity is generally absent. Swelling is usually slight, and
local tenderness is at the anterior lateral joint line, in contrast to
ankle sprains where the tenderness tends to be below the level of the
ankle joint.
reported a patient in whom the Tillaux fragment became entrapped
between the distal tibia and fibula producing apparent diastasis of the
ankle joint. To allow measurement of displacement from plain films, the
radiograph beam would have to be directly in line with the fracture
site, which makes CT confirmation of reduction mandatory after all
closed reductions of these fractures.
immobilization of nondisplaced juvenile Tillaux and triplane fractures.
Fractures with more than 2 mm of displacement, associated with
articular incongruity, may benefit from closed or open reduction.93
Closed reduction is attempted by internally rotating the foot and
applying direct pressure over the anterolateral tibia. A percutaneous
pin or screw can be used for stabilization of the reduction. If closed
reduction is not successful, open reduction or percutaneous reduction
with arthroscopic assistance may be required. Occasionally, a
percutaneously inserted pin can be used to manipulate the displaced
fragment into anatomic position and then advanced to fix the fragment
in place.165 Screw fixation within the epiphysis is usually adequate (see Fig. 26-21 and section on arthroscopic treatment of intra-articular fractures).
 |
|
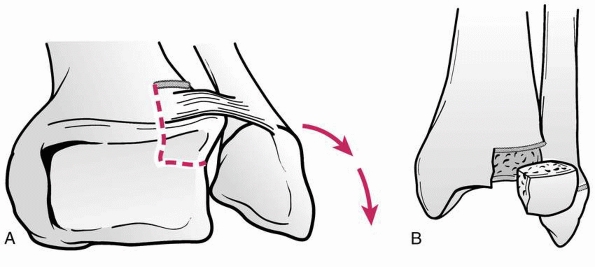
FIGURE 26-41
Juvenile Tillaux fracture. Mechanism of injury: the anteroinferior tibiofibular ligament avulses a fragment of the lateral epiphysis (A) corresponding to the portion of the physis that is still open (B). |
 |
|
FIGURE 26-42 Anteroposterior mortise view of a 14-year-old who sustained a juvenile Tillaux fracture.
|
described a triplane fracture in their report of 27 physeal ankle
injuries and reported that they had seen 10 such fractures. Despite
these earlier reports, the nature of triplane fractures was not
appreciated until Marmor’s117 report in 1970 of an irreducible ankle fracture that at surgery was found to consist of three parts (Fig. 26-43). Two years after Marmor’s report, Lynn113
reported two additional such fractures and coined the term triplane
fracture. He described the fracture as consisting of three major
fragments:
(i)
the anterolateral quadrant of the distal tibial epiphysis, (ii) the
medial and posterior portions of the epiphysis in addition to a
posterior metaphyseal spike, and (iii) the tibial metaphysis. Cooperman
and associates,39
however, in their 1978 report of 15 such fractures concluded that,
based on tomographic studies, most were two-part fractures produced by
external rotation (Fig. 26-44). Variations in
fracture patterns were attributed to the extent of physeal closure at
the time of injury. Karrholm and colleagues87
reported that CT evaluation of four adolescents with triplane fractures
confirmed the existence of two-part and three-part fractures and also
revealed four-part fractures (Fig.26-45). Denton and Fischer46
described a two-part “medial triplane fracture” that they believed was
caused by adduction and axial loading, and Peiro and associates139 reported a three-part medial triplane fracture.
 |
|
FIGURE 26-43
Anatomy of a three-part lateral triplane fracture (left ankle). Note the large epiphyseal fragment with its metaphyseal component and the smaller anterolateral epiphyseal fragment. |
studied 21 triplane fractures, identifying 19 as lateral triplane
variants, and 2 as medial variants. Twelve were 2 part fractures, 6
were three-part fractures, and 3 were four-part fractures.
a subgroup of two-part and three-part triplane fractures in which the
fracture line on the anteroposterior radiographs did not extend into
the ankle joint but into the medial malleolus instead (Fig. 26-46). Feldman and coworkers54 also reported a case of an extra-articular triplane fracture in a skeletally immature patient. Shin et al.170
reported 5 patients with intramalleolar triplane variants. They divided
these into three types: type I, an intramalleolar intra-articular
fracture, type II, an intramalleolar, intra-articular fracture outside
the weight-bearing surface, and type III, an intramalleolar,
extra-articular fracture (Fig. 26-47). These
authors found that CT scans with three-dimensional reconstruction were
helpful in determining displacement and deciding if surgery is
indicated.
 |
|
FIGURE 26-44
Anatomy of a two-part lateral triplane fracture (left ankle). Note the large posterolateral epiphyseal fragment with its posterior metaphyseal fragment. The anterior portion of the medial malleolus remains intact. |
 |
|
FIGURE 26-45
Anatomy of a four-part lateral triplane fracture (left ankle). The anterior epiphysis has split into two fragments, and the posterior epiphysis is the larger fragment with its metaphyseal component. |
reviewed 209 triplane fracture patients and found the mean age at the
time of injury was 14.8 for boys and 12.8 for girls. This type injury
did not occur in children younger than 10 or older than 16.7 years. The
incidence is higher in males than females.167
Patients with triplane fractures may have completely open physes.
Swelling is usually more severe than with Tillaux fractures, and
deformity may be more severe, especially if the fibula is also
fractured. Radiographic views should include anteroposterior, lateral,
and mortise views. Rapariz et al.152
found that 48% of triplane fractures were associated with fibular
fracture and 8.5% were associated with ipsilateral tibial shaft
fracture. Healy et al.74 reported a
triplane fracture associated with a proximal fibula fracture and
syndesmotic injury (Maisonneuve equivalent). Failure to detect such
injury may lead to chronic instability. Therefore, tenderness proximal
to the ankle should be sought and if found is certainly an indication
for radiographs of the proximal leg. CT scans have largely replaced
plain tomograms for evaluation of the articular surface and the
fracture anatomy (Fig. 26-48).
mm of displacement, as well as extra-articular fractures can be treated
with long-leg cast immobilization with the foot in internal rotation
for lateral fractures and in eversion for medial fractures. Fractures
with more than 2 mm of displacement, 65% of the injuries in the series
by Karrholm et al.,87 require
reduction; this may be attempted in the emergency department or in the
operating room with the use of general anesthesia. Closed reduction of
lateral triplane fractures is attempted by internally rotating the
foot. Based on the mechanism of injury, the most logical maneuver for
reduction of medial triplane fractures is abduction. If closed
reduction is shown to be adequate by image intensification as is the
case in about half the time, a long-leg cast is applied or percutaneous
screws are inserted for fixation if necessary. Well placed percutaneous
screws will prevent secondary
displacement
in a cast, and may make follow-up radiographs and clinical visits less
frequent. If closed reduction is unsuccessful, open reduction is
required. This can be accomplished through an anterolateral approach
for lateral triplane fractures or through an anteromedial approach for
medial triplane fractures. Additional incisions may be necessary for
adequate exposure.
 |
|
FIGURE 26-46 A,B. Anteroposterior and lateral radiographs of an “intramalleolar” variant triplane fracture in a 14-year-old boy. C,D. CT scans demonstrate extra-articular nature of the fracture.
|
 |
|
FIGURE 26-47 Schematic drawing of the immature distal tibial physis demonstrating types I, II, and III intramalleolar triplane fractures. A. Type I intramalleolar, intra-articular fracture at the junction of the tibial plafond and the medial malleolus. B. Type II intramalleolar, intra-articular fracture outside the weight-bearing zone of the tibial plafond. C.
Type III intramalleolar, extraarticular fracture. (Adapted from Shin A, Moran ME, Wenger DR. Intramalleolar triplane fractures. J Pediatr Orthop 1997;17:352-355, with permission.) |
described arthroscopic reduction of two-part triplane fractures in two
patients. With the arthroscope in an anterolateral portal and an
anteromedial portal used for inflow, two pins were inserted laterally
into the epiphyseal fragment and used to maneuver it into proper
position under direct arthroscopic vision. The pins were then advanced
for fixation of the fragment.
arthroscopic assistance may help with the reduction and minimize the
need for incisions. Careful review of the CT scans can help guide
percutaneous clamp and screw placement that improves the biomechanics
of clamp reduction and screw placement.85
Care should be taken to avoid injury to neurovascular structures during
clamp or percutaneous screw placement (see section on arthroscopy and
surgical reduction tips).
patient, these injuries can be associated with severe soft tissue
swelling and edema. Similar to the treatment in adults with these
injuries, management of the soft tissues is critical to prevent
complications of skin loss, infection, wound healing problems, etc.51,181
Initial approaches may consist of application of external fixation or
dressings to address swelling and edema, with delay of surgical
intervention for 5 to 15 days (Fig. 26-49).51
 |
|
FIGURE 26-48 Preoperative (A,B) and postoperative (C,D) anterior posterior and lateral views of an adolescent pilon fracture.
|
described a small series of pilon fractures in the skeletally immature.
The patients in this series did not have wound/skin complications, and
only two of eight patients developed postoperative osteoarthritis at
short-term follow-up. As these fractures may be higher risk for
complications, we believe that treatment principles used in adult
patients should be applied to this patient population as well.5,12,104,105,138,155
Despite 12 weeks of immobilization, these fractures had not healed.
Despite the appearance of nonunion on radiographs, these patients
remained symptom free at 2 years follow-up. One patient developed mild
symptoms of ankle pain several years later. If there is evidence of
syndesmotic injury, syndesmosis reduction and internal fixation should
probably be considered.
a triplane fracture in association with a syndesmosis injury, and both
authors have identified a small series of syndesmosis type injuries in
their practice.43 These have been
associated with the following fracture patterns: distal fibula,
Salter-Harris types I and II, triplane, and Tillaux. During surgical
treatment of pediatric/adolescent ankle fractures, evaluation
for
syndesmosis injuries should probably be performed in a manner similar
to the treatment of adult fractures. Syndesmosis reduction and fixation
may be necessary (see Fig. 26-15).
 |
|
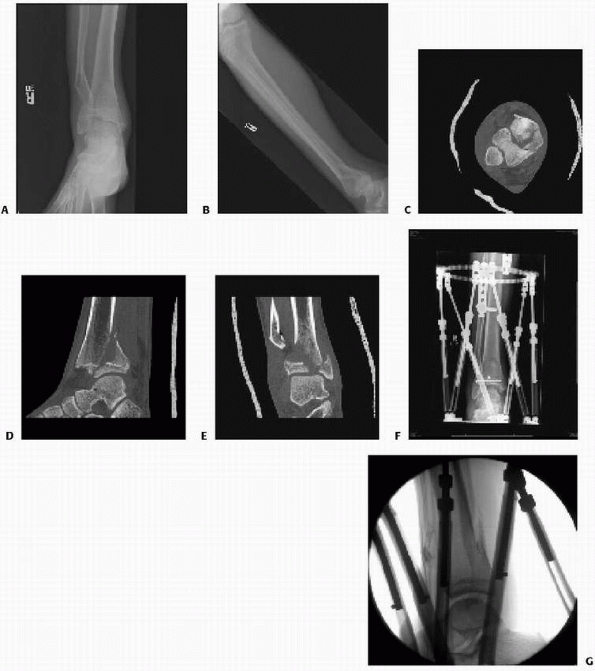
FIGURE 26-49 Pilon fracture treated with spatial frame. A,B. Preoperative anteroposterior and lateral view of adolescent pilon fracture with depressed articular region. C. Axial CT scan showing comminution of articular surface. D,E. Sagittal CT scan and coronal CT scan showing comminution of metaphysic and involvement of articular surface. F,G. Reduction of fracture with Taylor Spatial Frame and placement of percutaneous screws to reduce the articular surface.
|
Approximately 25,000 lawn mower injuries occur each year, 20% of which
are in children. Ride-on mowers produce the most severe injuries,
requiring more surgical procedures and resulting in more functional
limitations.1,3,50,57,161,188 Loder et al.109
reviewed 144 children injured by lawn mowers. The average age at the
time of injury was 7 years. The child was a bystander in 84 cases.
Sixty-seven children required amputation. Soft tissue infection
occurred in 8 of 118 and osteomyelitis in 6 of 117.
copious irrigation and débridement, tetanus toxoid, and intravenous
antibiotics. Gaglani et al.61
reported the bacteriologic findings in three children with infections
secondary to lawn mower injuries. They found that organisms infecting
the wounds were frequently different than those found on initial
débridement. Gram-negative organisms were common, and all three
patients were infected with fungi as well. In children with lawn mower
injuries, grass, dirt, and debris are blown into the wound under
pressure, and removal of these embedded foreign objects requires
meticulous mechanical débridement.
at the time of initial treatment. Exposed physeal surfaces should be
covered with local fat to help prevent union of the metaphysis to the
epiphysis. An external fixator may be used if neurovascular structures
are injured, but small pins should be used through the metaphysis and
epiphysis, avoiding the physis.77,84,111,153,160
Wound closure may be a problem in cases with significant soft tissue
injury and exposed bone. Skin coverage with local tissue is ideal; if
local coverage is not possible, split-thickness skin grafting is
generally the next choice. Free vascular flaps and rotational flaps may
be required for adequate coverage. Klein et al.98
reported two cases that had associated vascular injury precluding such
flaps that were covered successfully with local advancement flaps made
possible by multiple relaxing incisions. Mooney et al.125
reported cross extremity flaps for such cases. They found external
fixation for linkage of the lower extremities during the procedure to
be valuable. After fixation removal, range of motion returned readily.
 |
|
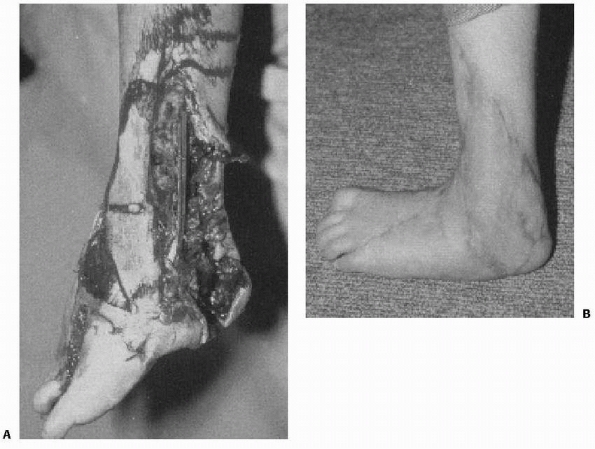
FIGURE 26-50 A. Severe lawn mower injury in a 5-year-old boy. B. One year after initial treatment with dé bridement, free flap, and skin graft coverage.
|
reported 33 patients with lawn mower injuries to the foot and ankle.
They found that the most severe injuries were to the posterior-plantar
aspect of the foot and ankle. Of their patients, five required
split-thickness skin grafts and one required vascularized flap for soft
tissue coverage. Two ultimately required Syme amputation. Four of the
patients had complete disruption of the Achilles tendon. Three had no
repair or reconstruction of the triceps surae tendon, and one had
delayed reconstruction 3 months after injury. Vosburgh and associates188
speculate that dense scarring in the posterior ankle results in a
“physiologic tendon” and that extensive reconstructive surgery is not
always necessary for satisfactory function. Boyer et al.20
reported a patient with deltoid ligament loss due to a severe grinding
injury that required free plantaris tendon graft to reconstruct the
ligament. Soft tissue coverage was achieved using a free muscle
transfer. Rinker et al.154 also described the use of soft tissue transfer to assist pediatric patients with severe soft tissue loss.
been a dramatic improvement in the treatment of these injuries and may
reduce the need for tissue transfers.75
Referral to centers with experience with these treatment protocols may
be necessary for these severe injuries. Our limited experience with the
use of vacuum-assisted closure devices in high-energy trauma with
severe soft tissue injury has shown very good results for limb salvage.
Salter-Harris type I or II fractures that are caused by a supination
-inversion injury. Isolated fibular fractures are usually minimally
displaced and can be treated with immobilization in a below-knee cast
for 3 to 4 weeks. Significantly displaced fibular fractures accompany
Salter-Harris type III and IV tibial fractures and usually reduce when
the tibial fracture is reduced. Internal fixation of the tibial
fracture generally results in stability of the fibular fracture such
that cast immobilization is sufficient. If the fibular fracture is
unstable after reduction and fixation of the tibial fracture, fixation
with a smooth intramedullary or obliquely inserted Kirschner wire is
recommended (Fig. 26-51F). In older adolescents
in whom growth is not a consideration, an intramedullary rod, screw, or
plate-and-screw device may be used as in adults (Fig. 26-52).
in children with inversion “sprain” type injuries to the ankle. These
may fail to unite with cast immobilization. Patients with such
nonunions may have pain without associated instability. In such
patients, simple excision of the ununited fragment usually relieves
their pain.46,71 When the nonunions are associated with
instability, reconstruction of one or more of the lateral ankle ligaments is required (see lateral ankle sprains).23,24
 |
|
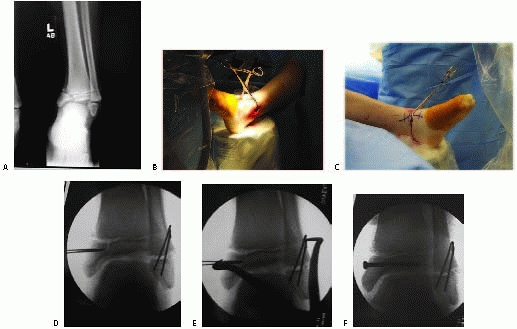
FIGURE 26-51 A.
Anteroposterior view of displaced Salter-Harris type I fibula fracture and Salter-Harris type IV intra-articular medial malleolus fracture. B. Use of percutaneous clamps to facilitate reduction of medial malleolus fracture. C. Use of percutaneous clamps to facilitate reduction. D. Use of two pins as “joysticks” to guide reduction of the displaced medial malleolus fracture. E. Use of percutaneous clamps to facilitate reduction and compression across the epiphyseal fracture. F. Use of percutaneous epiphyseal screws to gain compression across the fracture and to facilitate reduction. |
of the distal fibula (os subfibulare) are also common. In the series
report by Ogden and Lee,135 5 of 11 patients with injures treated with casting had persistent symptoms and required excision.
published a prospective study of 559 children who presented with severe
supination injuries or sprains of the ankle. Forty patients, 28 boys
and 12 girls, with an average age of 12 years (range 5 to 14) were
surgically explored. The indications for surgery included swelling,
pain over the anterior talofibular ligament, limp, clinical
instability, and, when visible, a displaced avulsion fracture. Such
fractures were visible radiographically in only 8 patients but were
found at surgery in 19. Thirty-six ankles were found to have injury of
the anterior talofibular ligament at surgery. Only 16 of these had
either a positive lateral or anterior drawer stress test. At follow-up,
all patients were pain free and none complained of instability. Based
upon the incidence of residual disability after such injuries in adults
reported in the literature (21% to 58%), these authors suggested
primary surgical repair.
reported 60 skeletally immature children with chronic ankle pain and
instability. Fifty of these children responded to rehabilitation, but
10 had persistent symptoms. While three of these patients’ initial
radiographs were within normal limits, all patients with persistent
symptoms eventually were found to have ununited osteochondral fractures
of the fibular epiphysis. All 10 patients with persistent symptoms were
treated with excision of the ununited osteochondral fracture and a
Broström reconstruction of the lateral collateral ligament. All were
able to return to activities and none reported further pain or
instability.
reported a 12-year-old girl who was seen with a posterior dislocation
of the ankle without associated fracture. This was a closed injury and
resulted from forced inversion of a maximally plantar flexed foot. The
dislocation was reduced under IV sedation and the ankle immobilized in
a short-leg cast for 5 weeks. The patient was asymptomatic at follow-up
4 years postinjury. The inversion stress views at that time revealed
only a 3-degree increase laxity compared to the uninjured side. The
anterior drawer sign was negative. There was no evidence of avascular
necrosis of the talus on follow-up radiographs. Mazur et al.119 also reported ankle dislocation without a fracture in a pediatric patient.
 |
|
FIGURE 26-52 A. Salter-Harris type II fracture of the distal fibula in a 15-year-old. B. Lateral view shows the fibular metaphyseal fragment (arrow). Considerable soft tissue swelling was noted in the medial aspect of the ankle. C. Stress films showed complete disruption of the deltoid ligament. D. The fibular fracture was fixed with a cannulated screw; the deltoid ligament was not repaired.
|
II fractures initially with above-knee cast immobilization. Nonweight
bearing is continued until 2 to 4 weeks postinjury, when the cast is
changed to a below-knee walking cast or walking boot which is worn for
an additional 2 to 3 weeks. Follow-up radiographs are obtained every 6
months for 2 years or until a Park-Harris growth arrest line parallel
to the physis is visible and there is no evidence of physeal deformity.
years of growth remaining, our objective is to obtain no more than
10-15 degrees of plantar tilt for posteriorly displaced fractures, 5-10
degrees of valgus for laterally displaced fractures, and 0 degrees of
varus for medially displaced fractures (Fig. 26-53).
Studies in the adult literature suggest that minor alteration in
alignment of the ankle joint may have significant effect on tibiotalar
contact pressures.92,182,184
If a question exists as to whether the child has enough growth
remaining to remodel the fracture, it is probably best to perform a
reduction. For children with 2 years or less of growth remaining, the
amount of acceptable angulation is
reduced
to less than 5 degrees. We prefer to attempt reduction of markedly
displaced fractures with the use of general anesthesia with good muscle
relaxation and image intensifier control. The use of an ankle
distractor can facilitate distraction across the fracture, and may
facilitate reduction (see Fig. 26-34).
In children with mildly displaced fractures, especially if anesthesia
is not going to be available for many hours, an attempt at gentle
closed reduction under a hematoma block supplemented as needed by
well-monitored IV sedation may be reasonable. Not all emergency rooms
are equipped with appropriate sedation equipment for young patients.
Once adequately reduced, the fractures are usually stable and a
long-leg cast can be used for immobilization. Rarely, for markedly
unstable fractures or severe soft tissue injuries that require multiple
débridements, percutaneous screws are used when the Thurstan-Holland
fragment is large enough to accept screw fixation. When the fragment is
too small, smooth wire fixation across the physis is the only
alternative. Repeated attempts at closed manipulation of these
fractures may increase the risk of growth abnormality and should be
avoided. In patients with fractures that are not seen until 7 to 10
days after injury, residual displacement is probably best accepted,
unless very significant deformity or angulation is present, to avoid
iatrogenic injury to the physis. If growth does not sufficiently
correct malunion, corrective osteotomy can be performed later.
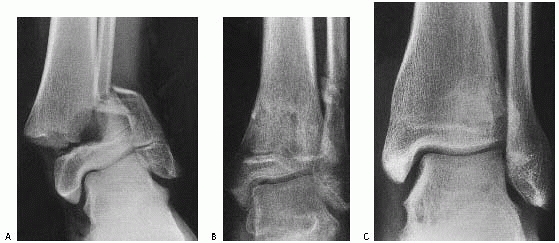 |
|
FIGURE 26-53 A.
Displaced pronation-eversion-external rotation fracture of the distal tibia in a 12-year-old boy was treated with closed reduction and cast immobilization. B. After cast removal, a 10-degree valgus tilt was present. C. At maturity, the deformity has completely resolved. |
indicated. The exception usually has been pronation-eversion-external
rotation fractures with interposed soft tissue, which may include
lateral and posterior displacement. For cases that have undergone an
attempt at closed reduction, close inspection of the medial physis
should be performed with image intensification. In some cases, the
medial physeal space will appear abnormally widened, which may suggest
incarceration of a large flap of periosteum in the physis. For these
fractures, a small anteromedial incision is made and any interposed
soft tissues, such as periosteum or tendons, are extracted. Even though
reduction is usually stable, we generally use internal fixation.
Fixation options include screw fixation through both the metaphyseal
and epiphyseal fragments, avoiding fixation across the physis if
possible (Fig. 26-54). Percutaneous smooth pins can also be placed from the medial malleolus, oriented proximally to engage the metaphysis (see Figs. 26-31 and 26-55).
fractures is the same as for nondisplaced type I and II fractures with
three modifications. Casting with a long-leg cast is confirmed with a
CT scan and/or radiographs. These patients are examined more frequently
(once a week) for the first 2-3 weeks after cast application to ensure
that the fragments do not become displaced. Third, these patients are
examined every 6 to 12 months after cast removal for 24 to 36 months to
detect any growth abnormality.
III and IV fractures, or those with 1 mm or less of displacement, can
be treated closed. Fractures with 2 mm or more of displacement require
open reduction and internal fixation with anatomical alignment of the
physis and intra-articular fracture fragments. Arthroscopic assistance
is also an option in these cases.
visualization of the ankle joint can also assist with the evaluation of
reduction. In some cases, the fractures may still have small gap
present with the articular surface, but the presence of step-off or
intra-articular incongruity can be clearly evaluated with arthroscopic
visualization of the articular surface. It has been our experience that
the C-arm views may show excellent reduction of the subchondral bone of
the articular-surface,
and
the arthroscopic views may show that the cartilage surfaces are not as
well reduced as one would expect based upon these radiographic images.
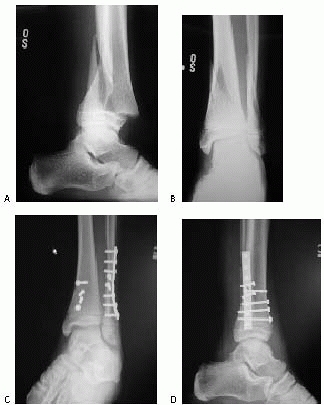 |
|
FIGURE 26-54 Salter Harris II with distal fibula. A. lateral view of Salter-Harris type II distal tibia fracture with fibular fracture. B. Anteroposterior view of Salter-Harris type II distal tibia fracture with fibular fracture. C. Anteroposterior view of percutaneous placement of tibial screws and plating of fibula fracture. D. Lateral view of percutaneous placement of tibial screws and plating of fibula fracture.
|
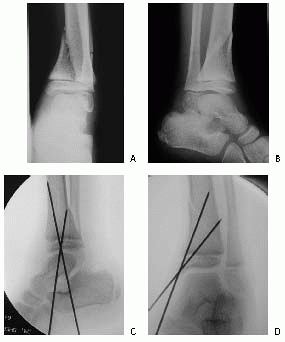 |
|
FIGURE 26-55 Salter-Harris type II distal tibia fracture. A. Anteroposterior view of Salter-Harris type II distal tibia fracture with fibular fracture. B. Later view of Salter-Harris type II distal tibia fracture with fibular fracture. C. Anteroposterior view of percutaneous placement of Kirschner-wires. D. Lateral view.
|
reduced, regardless of whether the fracture is acute or not. Closed
reduction can be attempted, but these fractures usually require open
reduction, arthroscopic assisted reduction, or mini-open reduction with
arthroscopic assistance. Occasionally, primary débridement of callus
and soft tissue back to normal-appearing physis and fat grafting have
been successful for fractures that are more than 7 days old.
below-knee casts may be used. If there is concern about fracture
stability, above-knee casts can be used.
is radiolucent at the lower extremity. After exsanguination of the
extremity and inflation of the tourniquet, longitudinal incisions are
made to expose the fracture. Relatively small incisions may be
acceptable, to allow for percutaneous or minimally invasive hardware
placement. The use of the C-arm may assist with the use of smaller
incision, allowing for visualization of the articular surface, with
minimal exposure of the metaphyseal areas. The fracture site is
identified, and an anteromedial capsulotomy of the ankle joint is
performed. The fracture surfaces are exposed and gently cleaned with
irrigation and forceps.
be elevated several millimeters from the metaphyseal fracture edges.
The epiphyseal edges and joint surfaces are examined through the
arthrotomy. The perichondral ring should not be elevated from the
physis. For Salter-Harris type III fractures, the reduction is
evaluated by checking the joint surface and epiphyseal fracture edges
through the arthrotomy. The epiphyseal fragment is grasped with a small
towel clip or reduction forceps, and the fracture is reduced. Internal
fixation is performed under direct vision and fluoroscopic control. It
is important to view both the lateral and anteroposterior projections
because of the curved shape of the distal tibial articular surface. If
the fragment is large enough, 4.0-mm cannulated lag screws are inserted
through the epiphyseal fragment; if the fragment is too small for
screws, smaller screws or smooth Kirschner wires are used. The
reduction and the position of the internal fixation are checked through
the arthrotomy. In fractures with a significant Thurstan-Holland
fragment, a metaphyseal screw may be used if a gap exists after the
epiphyseal screws are inserted. After reduction of the tibial fracture,
the associated Salter-Harris type I or II fibular fracture usually
reduces and is stable. If it is not, closed reduction and fixation with
percutaneous oblique smooth Kirschner-wires is performed.
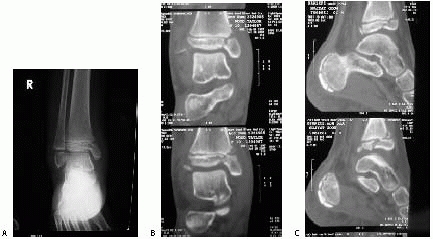 |
|
FIGURE 26-56 Salter-Harris type V distal fibula fracture. A. Anteroposterior ankle radiograph of crush injury to the medial malleolus. B. Coronal CT scan of medial malleolus crush injury. C. Sagittal CT scan of medial malleolus crush injury.
|
then the cast is changed to a below-knee walking cast, which is worn
for an additional 2 weeks. Frequent follow-up evaluations (every 3
months for the first year and yearly thereafter) are necessary to
detect growth abnormalities until skeletal maturity.
arrest is thought to be quite high for this injury pattern, due to
direct damage of the germinal layer of the physis.92
We have seen these fractures associated with a varus load to the ankle
joint, leading to a crush type injury to the medial malleolus (Figs. 26-56 and 26-57).
These fractures can be treated with reduction of the joint and physeal
surface, using minimally invasive techniques that avoid the physis and
perichondral ring (see Fig. 26-57).
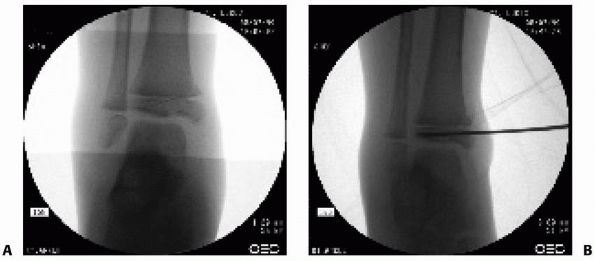 |
|
FIGURE 26-57 Salter-Harris type V patterns with crush injury to medial malleolus. A. Crush injury to medial malleolus and distal tibia metaphysis. B. The percutaneous pins can be used to manipulate the fracture.
|
prophylactic surgery to excise the physeal bar and implantation of a
fat graft might reduce the risk of physeal arrest. The prognosis for
this injury is poor, and treatment is usually focused upon treating the
complications of angular deformity and/or physeal arrest.92
than 2 mm, we prefer immobilization in an above-knee cast with the knee
flexed 30 degrees and the foot neutral or internally rotated. If the
position appears acceptable on plain films, CT scanning in the
transverse plane with coronal and sagittal reconstructions may be used
to confirm acceptable reduction. For fractures with more than 2 mm of
initial displacement, manipulation may be attempted by internal
rotation of the foot and application of direct pressure over the
anterolateral joint line. If reduction is not obtained with this
maneuver, reduction can be attempted by dorsiflexing the pronated foot
and then internally rotating the foot.114
If successful reduction is obtained, percutaneous fixation (screws or
pins) can be placed with C-arm guidance. In most cases, the medial
portion of the physis is already closed or closing, so this is one of
the rare times it is acceptable to cross the physis with screw
fixation. Percutaneous clamps can be used to hold reduction during
screw placement. If there are questions about the adequacy of
reduction, this can be confirmed by use of an arthrotomy or ankle
arthroscope.
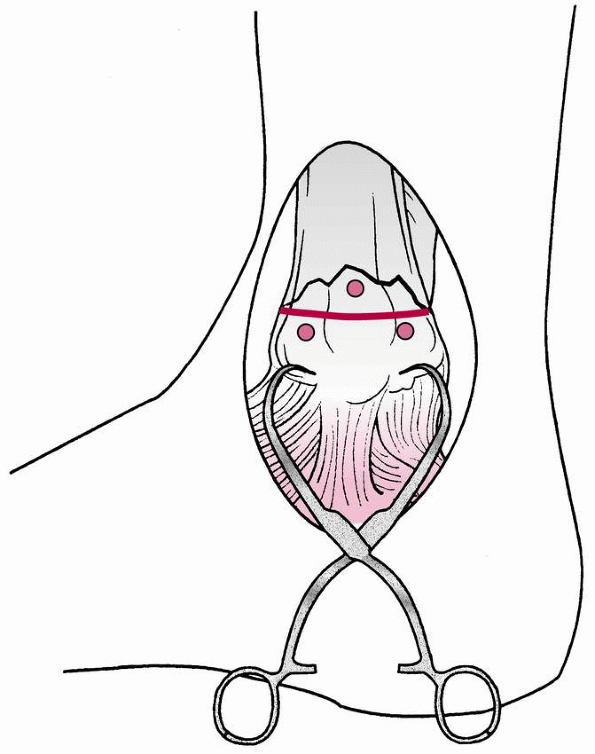 |
|
FIGURE 26-58 Technique for reduction of a Salter-Harris type IV fracture of the distal tibia.
|
Small Kirschner wires or the threaded tip wires from a cannulated screw
set can be inserted into the Tillaux fragment, to act as a “joystick”
to reduce the fracture (Fig. 26-58). This is
done under fluoroscopic control. Ideally, one or both of these pins can
then be passed across the fracture site after reduction has been
obtained, and the cannulated screw can then be placed over the pins (Figs. 26-59 and 26-60).
performed through an anterolateral approach or arthroscopic assistance
can be used to obtain anatomic reduction. For open techniques, the
following protocol is used. The patient is placed in a supine position,
and an incision is placed in the region of the fracture. A small
incision is made, perhaps 2 to 3 cm, to allow for visualization. The
fracture plane is identified, and direct pressure or clamps can be
applied to
maintain
the reduction. If necessary, a small arthrotomy or arthroscope can be
used to evaluate the articular reduction. A guidewire from the
cannulated screw system is used (a 4.0 mm cannulated system usually
works well in this age group) is placed, followed by placement of the
screw.
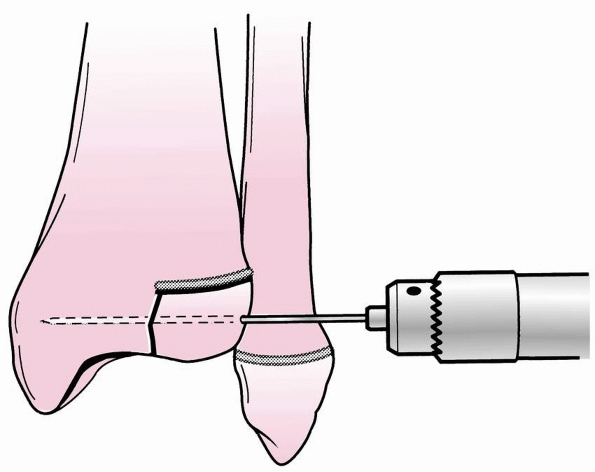 |
|
FIGURE 26-59 Advancement of pin after reduction of juvenile Tillaux fracture.
|
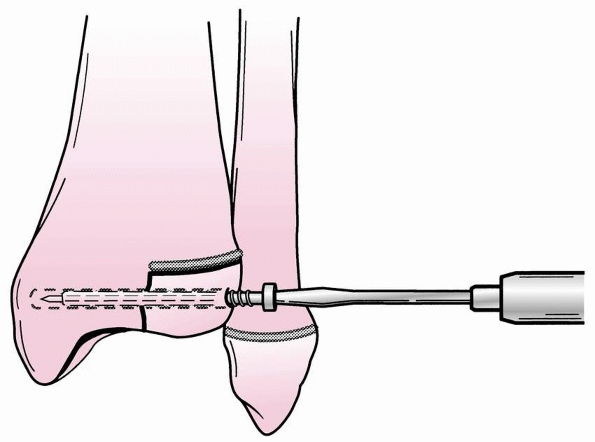 |
|
FIGURE 26-60
Percutaneous insertion of 4-mm cannulated screw over pin that has been advanced into the medial distal tibia after reduction of the juvenile Tillaux fracture fragment. |
followed by a weight-bearing cast or walking boot for another 2-3 weeks.
fractures, we prefer immobilization in a long-leg cast with the knee
flexed 30 to 40 degrees. The position of the foot may be influenced by
whether the fracture is lateral (internal rotation) or medial
(eversion), though this is certainly inexact. A CT scan is usually
obtained after casting to document adequate reduction. Plain films or
CT scans are obtained approximately 7 days after cast application to
verify that displacement has not recurred. At 3 to 4 weeks, the cast is
changed to a below-knee walking cast or walking boot, which is worn
another 2 to 3 weeks, though this may be delayed if there is concern
over displacement of the weight-bearing surface.
with appropriate conscious sedation varies between institutions. For
institutions that have such capabilities, fracture reduction can be
attempted in the emergency room. For fractures with more than 2 mm of
displacement, an attempt at closed reduction with sedation in the
emergency department may be performed. An above-knee cast is applied.
If fcplain radiographs show satisfactory reduction, a CT scan is
obtained. If reduction is acceptable, treatment is the same as for
nondisplaced fractures, though weight bearing could be delayed until
5-6 weeks.
attempted in the operating room with the use of general anesthesia. If
fluoroscopy shows an acceptable reduction, percutaneous screws are
inserted, avoiding the physis, and a short-leg cast is applied. If
closed reduction is unacceptable, open reduction or mini-open reduction
with the use of percutaneous clamps is performed. Preoperative CT
scanning may be helpful for evaluating the position of the fracture
fragments in the anteroposterior and lateral planes and for determining
the appropriate skin incisions, percutaneous clamp placements, and
screw location.
table with padded elevation behind the hip on the affected side. The
surgical approach depends on the fracture anatomy as determined by the
preoperative CT scan can be quite variable, and may even require more
than one incision. The goal is that the joint surface must be able to
be assessed.. A two-part medial triplane fracture can be approached
through a hockey-stick anteromedial incision. The fracture fragments
are irrigated to remove debris, and any interposed periosteum is
removed. The fracture is reduced, and reduction is confirmed by direct
observation through an anteromedial arthrotomy and by image
intensification. Two 4-mm cancellous screws are inserted from medial to
lateral or from anterior to posterior or both, depending on the
fracture pattern (Fig. 26-61). Anterior to
posterior screw placement may require an additional anterolateral
incision or the screws may be inserted percutaneously making sure
certain neurovascular structures are not damaged. Arthroscopic-assisted
techniques with the use of percutaneous clamps and screws may also be
used (Fig. 26-62).
approached with a hockey-stick anterolateral approach. The fracture is
reduced and stabilized with two screws placed from lateral to medial or
from anterior to posterior or both, and reduction is confirmed through
direct observation and by image intensification. In addition to open
techniques, arthroscopic-assisted techniques with the use of
percutaneous clamps and screws may also be used (see Fig. 26-62).
require more exposure for reduction and internal fixation.
Posteromedial approaches to the tibia can be used, with careful
attention to the surrounding neurovascular bundle and tendons. If the
fibula is fractured, posterior exposure of the tibial fracture can be
readily obtained by detaching the anterior and posterior inferior
tibiofibular ligaments and turning down the distal fibula on the
lateral collateral ligament (Fig. 26-63). If
the fibula is not fractured, a fibular osteotomy may be performed,
though this is uncommonly necessary. Careful dissection is necessary to
avoid iatrogenic fractures through the physis of the fibula. Medial
exposure is obtained through an anteromedial or posteromedial incision.
Reduction and internal fixation are carried out in a stepwise fashion.
For typical three-part fractures, the Salter-Harris type II fracture
may be reduced first by provisional fixation to the distal tibia
through the metaphyseal fragment. Usually, the Salter-Harris type III
fragment can then be reduced and provisionally fixed to the stabilized
type II fragment (Fig. 26-64). Occasionally,
the order of reduction and fixation should be reversed. Fractures with
four or more fragments require additional steps, but fixation of the
Salter-Harris type II or IV fragment through the metaphysis to the
distal tibia is usually best performed first. This step can be followed
by fixation of the Salter-Harris type III fragment or fragments (Fig. 26-65). After reduction, reliable patients may be treated with immobilization in a short-leg, nonweight-bearing cast
for 3 to 4 weeks. At 3-4 weeks, they may be converted to a
weight-bearing cast or walking boot for an additional 2 to 4 weeks if
there is stable fixation of the joint surface.
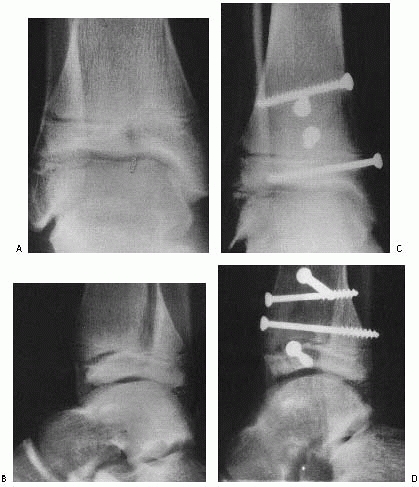 |
|
FIGURE 26-61 A,B. Irreducible three-part triplane fracture in a 13-year-old girl. C,D.
After open reduction with internal fixation. Note anterior-to-posterior and medial-to-lateral screw placement that avoids the physis. |
fixation of ankle fractures is best done before excessive swelling
occurs. Markedly swollen ankles often develop fracture blisters, which
may become infected. The integrity of skin closure and, even more
important, the vascularity of the wound edges also are threatened by
excessive soft tissue swelling. When marked soft tissue swelling
develops before surgery can be performed, elevation of the extremity in
a soft compression bandage until swelling begins to subside is
recommended, usually for no more than 5 days.
the time of open reduction and internal fixation reveals comminution at
the physeal line. In such cases, débridement of loose fragments back to
normal-appearing physis and the insertion of a fat graft into the
resulting void are recommended. This technique also can be useful for
fractures that present for treatment a week or more after injury. Early
callus that prevents the apposition of healthy physeal tissue at the
fracture site is dé brided and a fat graft is inserted (Fig. 26-66).
extra-articular fractures, such as Salter-Harris type I or II patterns.
When combined with the relaxation of general anesthesia, a few minutes
of distraction across the physis may facilitate reduction. Some believe
that distraction across the fracture may increase the likelihood that
the first attempt at reduction will be successful; this may reduce the
trauma to the physis during the reduction, perhaps reducing the risk of
physeal arrest. Juvenile Tillaux and triplane fracture reduction can
also be facilitated with ankle distraction, and this will also
facilitate arthroscopic ankle visualization. Instead of having the
surgeon pull manually for several minutes, the ankle distractor can
provide this distraction force. The surgeon can then focus on the
application of other forces, such as rotation or varus/valgus to
facilitate fracture reduction. Although skeletal traction using a
calcaneal pin is an option,33
we prefer to use an ankle strap and special distractor routinely used
for arthroscopy (Arthrex, Naples, FL). The ankle distractor can be
position to allow for anteroposterior and lateral C-Arm images (see Fig. 26-34).
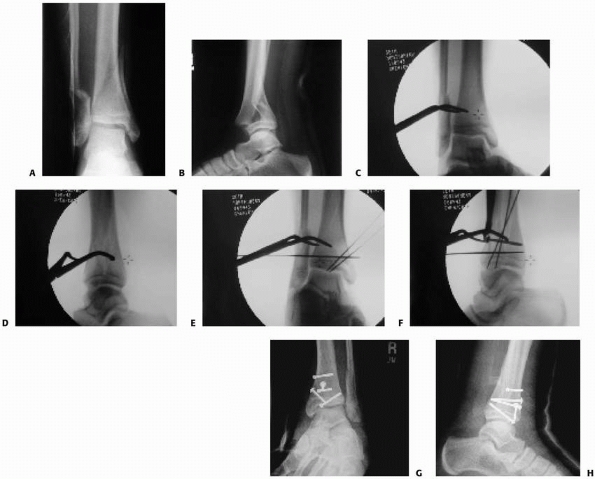 |
|
FIGURE 26-62 A,B. Anteroposterior and lateral radiograph of triplane fracture with involvement of medial malleolus. C,D. Use of percutaneous clamps for reduction, viewed in the anteroposterior plane (C) and in the lateral plane (D). E,F. Use of percutaneous clamps for reduction, followed by placement of guidewires to hold reduction. G,H. Percutaneous and mini-open placement of cannulated screws, anteroposterior view (G) and lateral view (H).
|
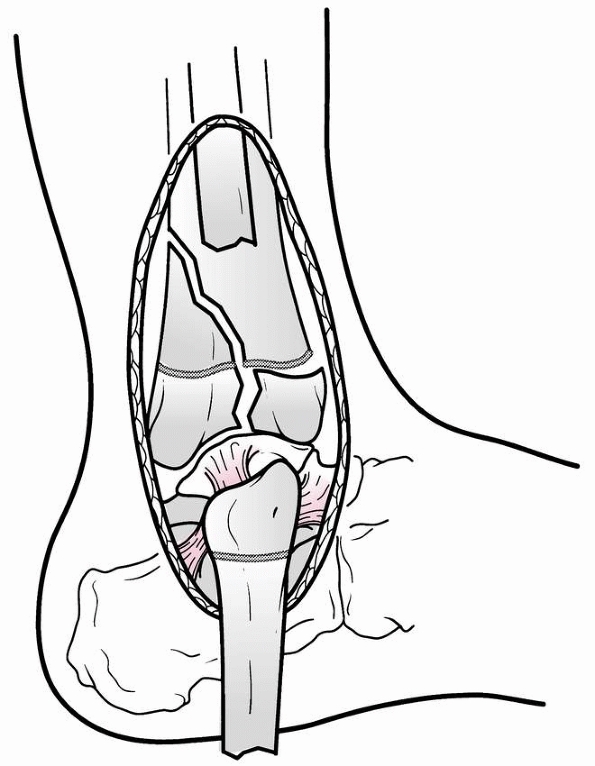 |
|
FIGURE 26-63 Transfibular approach to a complex triplane fracture.
|
intra-articular fractures or multiplanar fractures. High resolution
scans with three-dimensional reconstructions provide excellent anatomic
detail. For minimally invasive approaches using percutaneous screw
fixation, these images can be used for precise screw
placement
during surgery. The CT scan can also facilitate placement of clamp, to
allow for compression in the plane perpendicular to the fracture. A
clear preoperative evaluation should determine optimal screw position
and orientation, and these images should also be available during the
procedure to assist with screw placement.
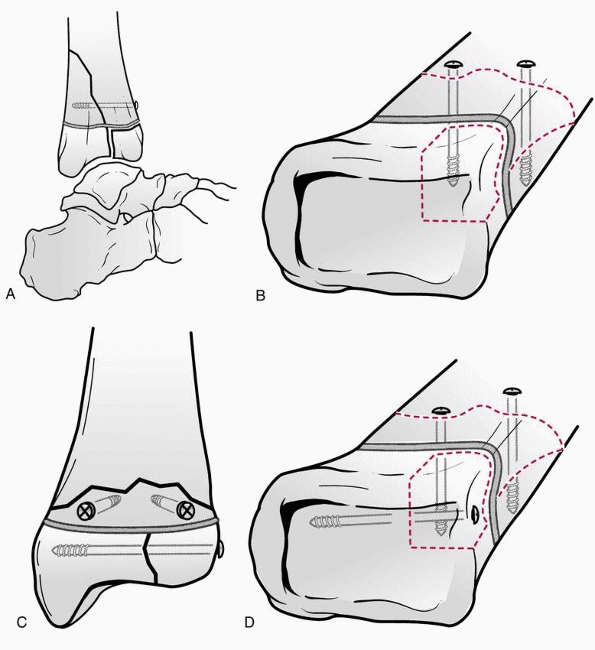 |
|
FIGURE 26-64 Open reduction with internal fixation of a three-part lateral triplane fracture. A,B. Reduction and fixation of the Salter-Harris type II fragment to the metaphysis. C,D. Reduction and internal fixation of the Salter-Harris type III fragment to the Salter-Harris type II fragment.
|
procedures. Several clinical series document the effectiveness of
arthroscopic assistance for Tillaux fractures122,137 and triplane fractures.79
The joint surfaces can be readily visualized through small incisions,
avoiding the need for a larger arthrotomy. Even in cases where an
arthrotomy is used, the scope can be utilized either with or without
fluid to visualize the reduction of the fragments in the joint (Fig. 26-67).
The fluid of the arthroscopy pump can also be used to wash out the
fracture site, increasing visualization during reduction. Avoidance of
high pump pressure will minimize the risks of soft tissue infiltration.
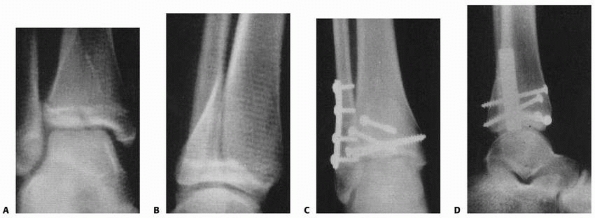 |
|
FIGURE 26-65 A,B. Irreducible three-part lateral triplane fracture in a 14-year-old boy. C,D.
After open reduction through a transfibular approach and internal fixation with anterior-to-posterior and lateral-to-medial screws. |
5.0 mm. Both scopes work well, although in smaller children, the 2.8 mm
scope may be a better choice. The smaller scope has a smaller field of
view, but this does not seem to be much of a disadvantage
for
viewing the displaced cartilage surfaces. The smaller scope also
delivers less fluid to the joint, which may require additional time to
clean the hematoma from the joint and fracture, but has a lower risk of
causing soft tissue infiltration around the joint.
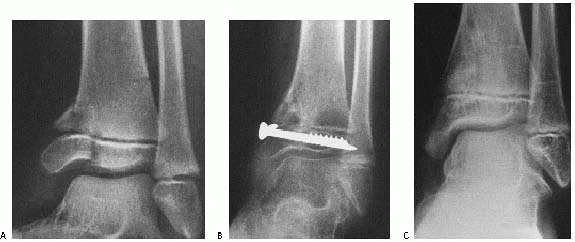 |
|
FIGURE 26-66 A. An 8-year-old girl who presented 10 days after a displaced Salter-Harris type IV fracture of the distal tibia. B.
At open reduction, comminution of the physis was noted. The physis was dé brided, and a fat graft was inserted before reduction and internal fixation of the fracture. C. Three years after injury, there is no evidence of physeal bar formation or growth abnormality. |
invasive approaches. This can be easily rotated to allow for
anteroposterior or lateral views. If the ankle distractor is used,
position the foot and distractor to allow easy access by the C-arm (see
Fig. 26-34).
of fractures. Careful study of imaging studies, especially CT scans,
can guide precise placement of clamps to provide maximal compression
across fracture planes. Forces normal or near normal to the fracture
planes are ideal. Care should be taken during placement to prevent
injury to neurovascular structures, including sensory nerves. The skin
can be divided, and then deeper dissection through the subcutaneous
tissues can be performed with a hemostat. The hemostat is used to
bluntly distract the tissues away from the skin portal and then
advanced to the bone surface. The tips of the clamp can now be placed
with minimal risk to neurovascular structures. The clamp can be
compressed to facilitate reduction of triplane and Tillaux fractures
(see Figs. 26-50, 26-51, and 26-62).
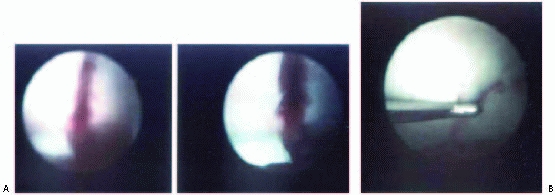 |
|
FIGURE 26-67 Ankle arthroscopy. A. Arthroscopic view of fracture gap in distal tibia articular surface. B. Arthroscopic view of fracture gap in distal tibial articular surface after reduction.
|
fractures. Smooth pins have the advantage that they do not place a
threaded tip across the physis, therefore reducing the risk of
iatrogenic physeal arrest. The main disadvantage of smooth pins is that
they do not allow for compression. These pins can also migrate through
bone and into soft tissues. Bending the ends at the surface of the bone
to prevent migration is important. These pins should be removed early,
as soon as the fracture stability is adequate.
 |
|
FIGURE 26-68 A,B. Displaced juvenile Tillaux fracture. Closed reduction was not successful. C. After open reduction with internal fixation with a small fragment screw.
|
devices across the physis should be avoided. In some cases, a screw
implant may be necessary to cross a physis to maintain an articular
reduction. The adequacy of reduction of the joint surface probably is
probably more important than the physis. In patients approach ing
skeletally maturity, the use of screw implants across a physis that is
approaching closure is probably a reasonable choice, especially in case
where compression and/or stability are important, such as juvenile
Tillaux fractures (Fig. 26-68).
with immobilization in a below-knee walking cast for 3 to 4 weeks.
Closed reduction of displaced Salter-Harris types I and II fibular
fractures is performed, but when reduction is unsuccessful, one of the
authors (R. Jay Cummings) accepts up to 50% displacement without
problems at long-term follow-up. Acceptance of this displacement may be
more reasonable in young patients with significant remodeling
potential, although in older patients, displaced fractures may have
more affect on ankle function, and more anatomic reduction may be
advantageous. Dias,48 however, reported a patient with a symptomatic spike that required excision after inadequate reduction.
younger patients, as these individuals are more likely to have
nondisplaced distal fibular physeal injuries. If the pain can be
localized to the ligaments and there is not pain over the distal
fibular physis, then a true ankle sprain may be present. Chronic pain
and instability can occur in young patients, especially adolescents.
Brostom type reconstruction24 may
be appropriate in these patients, although Letts et al.106
has described nonanatomic reconstruction in younger patients using
nonanatomic reconstructions (Evans, Watson-Jones, Chrisman, and Snook
techniques).
the distal fibula, and special radiographic views may facilitate
diagnosis.69 These avulsion type
injuries can lead to symptoms, and a high index of suspicion is
important in younger patients. Haraguchi et al.70
evaluated a series of severe ankle sprains, and found that 26% had
evidence of distal fibular avulsion injury. Children and adults over 40
years of age had the highest incidence of this injury. Patients were
treated with weight-bearing casts for 3 to 4 weeks. Nonoperative
treatment yielded satisfactory results in this series.
quadriceps, hamstring, and abductor exercises are begun as soon as pain
and swelling allow. Usually, a below-knee cast is worn during the last
2 to 3 weeks of immobilization, and weight bearing to tolerance is
allowed during this time. After immobilization is discontinued, ankle
range-of-motion exercises and strengthening exercises are begun.
Protective splinting or bracing is usually not required after cast
removal. Running is restricted until the patient demonstrates an
essentially full, painless range of ankle and foot motion and can walk
without a limp. Running progresses from jogging to more strenuous
running and jumping as soreness and endurance dictate. For athletes,
unrestricted running and jumping ability should be achieved before
return to sports. Protective measures such as taping or bracing are
recommended initially for return to most sports.
quickly and require little or no formal physical therapy. For this
reason, and because of compliance considerations, fractures treated
with internal fixation are usually protected with below-knee casting
instead of starting an early range-of-motion program in a removable
splint. In older patients that may have a higher risk of
arthrofibrosis, we may start early motion in a removable boot and start
a formal supervised physical therapy program.
reported one patient with a delayed union and one patient with a
previous physeal bar excision who had a nonunion that healed after open
reduction, internal fixation, and bone grafting. Siffert172
reported nonunion in a patient with avascular necrosis of the distal
tibial epiphysis. We have seen two younger patients with Salter-Harris
type III fractures that appeared to be progressing to nonunion. Because
neither patient had any complaints of pain nor any evidence of
progressive displacement of the fracture and stress views showed no
instability, no treatment was undertaken. Both fractures eventually
united. We have seen one patient with a nonunion after open reduction
and internal fixation in whom pin fixation and cast immobilization were
discontinued prematurely. The fracture healed after repeat open
reduction and internal fixation.
 |
|
FIGURE 26-69
Complex nonunion of a Salter-Harris type III fracture of the medial malleolus in an 8-year-old boy. Note that the distal tibial epiphysis is in valgus, whereas the talus is in varus. (Courtesy of Brent Broztman, MD.) |
fractures that are either incompletely reduced or are initially
immobilized in below-knee casts. It has also been reported after
Salter-Harris type I and II injuries. Derotational osteotomy may be
performed for extra-articular fractures if discomfort and stiffness
occur. Guille et al.67 reported a
rotational malunion of lateral malleolar fracture that led to a stress
fracture of the distal fibula that went on to delayed union. Their
patient required correction of the malrotated distal fibula and bone
grafting of the delayed union site.
occurs after supination-plantarflexion Salter-Harris type II fractures.
Theoretically, an equinus deformity might occur if the angulation
exceeds the range of ankle dorsiflexion before fracture, but this is
very rare, probably because the deformity is in the plane of joint
motion and tends to remodel with growth.
Salter-Harris type II fractures. The degree to which the deformity may
spontaneously resolve or remodel with growth is controversial.
Caruthers and Crenshaw31 reported resolution of a 12 degrees valgus deformity in a 13.5-year-old boy, but Spiegel and associates175 reported persistent residual deformity in a significant number of their patients (Fig. 26-70). Varus deformity most often results from growth abnormality and infrequently is the result of simple malunion.
of the ankle secondary to supination inversion injuries. These patients
went on to develop medial subluxation of their ankles with associated
internal rotational deformity. Takakura et al.180 described successful open wedge osteotomy for varus deformity in nine patients. Scheffer and Peterson164
recommend opening wedge osteotomy when the angular deformity is 25
degrees or less and the limb length discrepancy is or will be 25 mm or
less at maturity.164 Preoperative
planning should include templating the various types of osteotomies to
determine which technique will maintain the proper mechanical alignment
of the tibia and ankle joint and will not make the malleoli unduly
prominent (Fig. 26-71).
 |
|
FIGURE 26-70
Radiograph of a 14-year-old boy, 4 months after pronation-eversion-external rotation injury, reveals 16 degrees of valgus angulation. |
Its use for correction of complex deformities can allow for multiplanar
corrections, including rotation, length, and angular deformity. For
more complex deformities, this device may be useful for correction.55,171
Salter-Harris types III and IV fractures in which a physeal bar
develops at the fracture site, leading to varus deformity that
progresses with continued growth. Spiegel and associates175 reported growth problems in 9 of 66 patients with Salter-Harris type II fractures.
discount this explanation and claim that with anatomic reduction (open
reduction and internal fixation if needed), the incidence of physeal
bar formation can be decreased. The validity of this claim is difficult
to determine from published reports. One problem is the small numbers
of patients in all series and the even smaller numbers within each
group in each series. Another problem is the age of the patients in
operative and nonoperative groups in the various series; for example,
many children reported to do well with a particular treatment method
have so little growth remaining that treatment may have had little or
no effect on growth.
analyzed the outcome of 91 Salter-Harris type I and II fractures of the
distal tibia. They identified premature physeal closure in 40%. This
series identified a trend towards increased premature physeal closure
in fractures that had worse displacement after reduction. They
recommended operative reduction to restore anatomic alignment to reduce
the risk of premature physeal closure.
reported physeal bars in 2 of 5 patients treated nonoperatively and in
none of 3 patients treated operatively in children 10 years of age and
younger. In another series of 65 physeal ankle fractures, Kling and
coworkers99 concluded that the
frequency of growth-related deformities could be reduced by open
reduction and internal fixation of Salter-Harris type III and IV
fractures.
patients (R. Jay Cummings), 2 of 5 treated operatively developed
physeal bars, while none of the 3 patients treated nonoperatively had
physeal bars. This supports the conclusion of Cass and Peterson,32 Ogden,134
and others that growth problems after these injuries may not always be
prevented by open reduction and internal fixation. Open reduction of
displaced Salter-Harris type III and IV ankle fractures would seem
advisable to restore joint congruity, regardless of whether growth
potential can be preserved.
but one of the authors (R. Jay Cummings) has found that, although lines
parallel to the physis are reliable, lines that appear to diverge from
the physis may be misleading (Fig. 26-72). Harcke and colleagues72
reported early detection of growth arrest with bone scanning
techniques. The use of bone scan techniques may have very limited
indications with the availability of MRI and CT Scans.
but is rare. Most patients require excision of small bony bars and may
require correction of significant angular deformity with osteotomy (Fig. 26-73).
They found that continued fibular growth with complete arrest of tibial
growth was usually compensated by proximal migration of the fibula so
that varus deformity did not occur.
tibial physis is small (approximately 0.25 in per year) in most older
patients with these injuries, the amount of leg-length discrepancy
resulting from complete growth arrest tends to be relatively small.
Treatment may be required if the anticipated discrepancy is projected
to be clinically significant.
include plane radiographs, tomography, CT, and MRI. In most imaging
departments, standard tomography has been replaced by CT. CT scans can
be useful for clear delineation of the anatomy, especially in cases in
which surgical intervention is necessary. Recent studies have also used
MRI scans.60,110,163 Although the resolution capability is more limited, the avoidance of ionizing radiation is a major advantage of MRI scans over
CT scans, though the ankle is much less sensitive to radiation than many central organs.
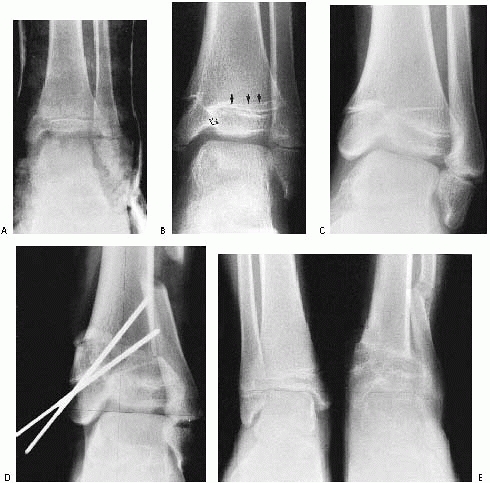 |
|
FIGURE 26-71 A.
This apparently nondisplaced medial malleolar fracture in an 11-year-old boy was treated with immobilization in a long-leg cast. B. Fourteen months after injury, there is a clear medial osseous bridge and asymmetric growth of the Park-Harris growth arrest lines (black arrows). Note the early inhibition of growth on the subchondral surface of the fracture (open arrow). C. Five years after injury, the varus deformity has increased significantly and fibular overgrowth is apparent. D. The deformity was treated with a medial opening-wedge osteotomy of the tibia, an osteotomy of the fibula, and epiphysiodesis of the most lateral portion of the tibial physis and fibula. E. Three months after surgery, the osteotomies are healed and the varus deformity is corrected; the joint surface remains irregular. (Courtesy of Earl A. Stanley, Jr., MD.) |
after fracture of the tibial diaphysis, in the absence of obvious
physeal injury.128
fractures of the distal tibia metaphysis and epiphysis. A recent series
of 83 patients with fractures in this region demonstrated 2 patients
with medial malleolus overgrowth. In both cases, there was no evidence
of functional impairment.129
joint have a low risk of posttraumatic arthritis, but injuries that
extend into the joint may produce this complication. Caterini and
coworkers34 found that 8 of 68 (12%)
patients had pain and stiffness that began from 5 to 8 years after
skeletal maturity. Ertl and associates53
found that 18 to 36 months after injury 20 patients with triplane
fractures were asymptomatic, but at 36 months to 13 years after injury
only 8 of 15 patients evaluated were asymptomatic.53
demonstrated in a cadaver study that 1 mm of lateral talar displacement
decreases tibiotalar contact area by 42%, which greatly increases the
stress on
this weight-bearing joint. More recently, Michelson and colleagues121
reported that a cadaver study using unconstrained specimens suggested
that some lateral talar displacement occurs with normal weight bearing.
Because of their findings, they questioned the current criterion of 2
mm of displacement for unstable ankle fractures. However, the results
of Ramsey and Hamilton’s151 study
correlate well with other studies that have shown increased symptoms in
patients in whom more than 2 mm of displacement was accepted.34,53
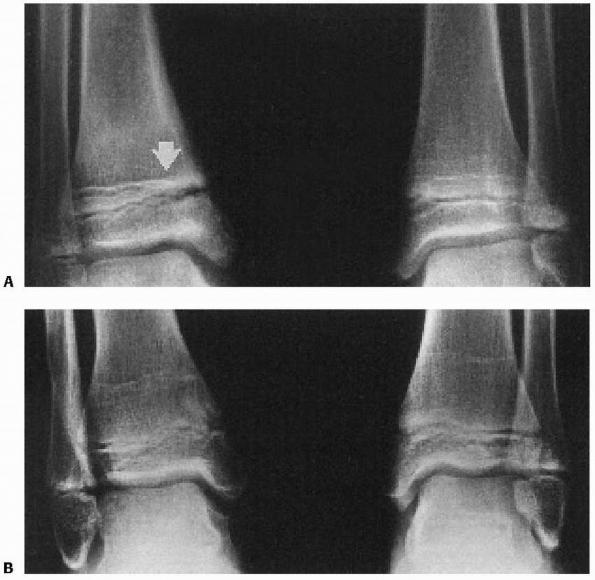 |
|
FIGURE 26-72 A.
Six months after cast immobilization of a nondisplaced supination-inversion Salter-Harris type III fracture of the right distal tibia in an 8-year-old boy. The Park-Harris growth arrest line (arrow) appears to end in the physis medially and diverge from the physis laterally. B. Two years later, no physeal bar is present and growth is normal. |
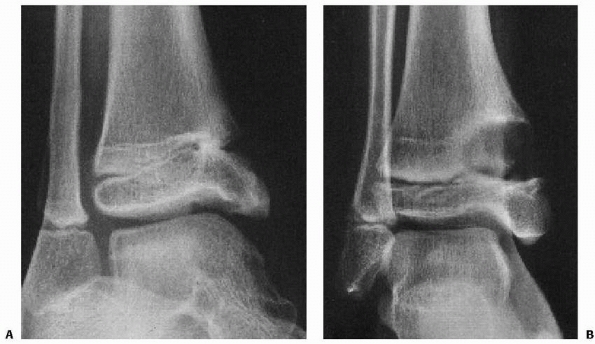 |
|
FIGURE 26-73 A.
One year after open reduction and internal fixation of a Salter-Harris type III fracture of the distal tibia in a 7-year-old boy, varus deformity has been caused by a physeal bar. B. Two years after excision of the physeal bar and insertion of cranioplast, satisfactory growth has resumed and the deformity has resolved. |
controversial, and the indications for removal are not well-defined in
the literature.28 Charlton et al.37
has demonstrated the periepiphyseal or subchondral screws may alter the
joint contact pressures about the ankle. After removal of the screws
from the subchondral
bone,
the contact pressure normalized. For hardware in the subchondral bone,
the study suggested that implant removal in transepiphyseal screws may
be appropriate.37
 |
|
FIGURE 26-74
Valgus deformity of the ankle, lateral displacement of the talus with widening of the joint medially, and severe shortening of the fibula after early physeal arrest in a child who sustained an ankle injury at 6 years of age. (Courtesy of James Roach, MD.) |
Treatment options include therapy and nonsteroidal anti-inflammatory
drugs, etc. Recent clinical studies have evaluated the affects of joint
distraction for posttraumatic chondrolysis, although experience with
this technique in young patients is very limited.162
in 1950, were the first to call attention to this complication of
distal tibial fractures. In their patient, the combination of nonunion
of a medial malleolar fracture and avascular necrosis caused pain that
required an arthrodesis 14 months after injury. Dias47
reported a patient with this complication who did not require
arthrodesis but who had a significant leg-length discrepancy that
required epiphysiodesis of the contralateral tibia. We have seen one
patient with this complication. The patient had significant joint
stiffness and developed a valgus deformity secondary to collapse. After
revascularization of the epiphysis, the ankle was realigned with a
supramalleolar osteotomy, and 5 years later the patient had
satisfactory function without pain.
has described a unique compartment syndrome associated with distal
tibial physeal fractures in 6 patients. These patients had clinical
symptoms of severe pain and swelling, with associated sensory and motor
deficits. The compartment pressure below the superior extensor
retinaculum was above 40 mm in all cases, and the pressure was less
than 20 mm in the anterior compartment. These patients were treated
with limited fascial release of the superior extensor retinaculum and
fracture stabilization.
complication of fractures in this region. This can lead to growth
disturbance, including angular deformity and lower extremity length
discrepancy.58,127
Synostosis in this area alters the normal pattern of movement between
the tibia and fibula and has been associated with pain in some
patients. In a small clinical series, Frick et al.58
demonstrated symptoms of pain, prominence of the fibula, and ankle
deformity in 5 of 8 patients with this synostosis. In this series, the
normal growth pattern of distal migration of the fibula was altered,
resulting in decrease distances between the proximal physes of the
tibia and fibula and proximal positioning of the distal fibula with
respect to the distal tibia. Munjal et al.127
demonstrated successful synostosis excision in a 7-year-old patient,
which lead to normalization of the ankle joint at 16 months postsurgery.
syndrome occasionally develops after these injuries and is treated
initially with an intensive formal physical therapy regimen that
encourages range of motion and weight bearing.92,191
For patients who do not respond quickly to such a program, physical
therapy in association with continuous epidural analgesia may be
considered.191
treatment of ankle fractures in skeletally immature patients. The
relationship between physeal displacement and the development of
subsequent physeal arrest is still unclear. Interposition of periosteum
in the fracture may place a role in physeal arrest, although this has
not been clarified in animal models or clinical trials.
that minimally angular deformities about the distal tibia can have
pronounced effects on the tibiotalar contact pressures.92,182,184
The limits of fracture remodeling and the magnitude of acceptable
deformity in growing children are still not well-defined in the
literature.
understanding of these fractures, and may play an increasing role in
the use of computer-aided reduction techniques and other forms of
minimally invasive surgery. CT scanning requires ionizing radiation,
but provides high-resolution model reconstruction. Future MRI
modalities may allow for higher quality images, including
three-dimensional reconstructions; this would avoid the need for
ionizing radiation.
eventually play a role in the treatment of these fractures, either to
prevent or treat a physeal arrest.96
APC, Bromer, RS. Classification and mechanism of fractures of the leg
bones involving the ankle. Arch Surg 1922;4:51-129.
M, Ray A, Stern R. The extensile approach for the operative treatment
of high-energy pilon fractures: surgical technique and soft-tissue
healing. J Orthop Trauma 2007;21(3):198-206.
A, Gaynor T, Mubarak SJ. Premature physeal closure following distal
tibia physeal fractures: a new radiographic predictor. J Pediatr Orthop
2003;23(6):733-739.
R. Die traumatische epiphysenlosung am distalen ende des schienbeines
und des wadenbeines. Hefte Unfallheilkd 1957;54:228-257.
G, Kallieris D, Seebock T, et al. Bioresorbable pins and screws in
paediatric traumatology. Eur J Pediatr Surg 1994;4(2):103-107.
JM, Botte MJ. Surgical anatomy of the superficial peroneal nerve in the
ankle and foot. Clin Orthop Relat Res 1994;305:229-238.
M, Bastian L, Krettek C, et al. Surgical options for the treatment of
severe tibial pilon fractures: a study of three techniques. J Orthop
Trauma 2001;15(3):153-160.
O, Hirvensalo E, Vainionpaa S, et al. Degradable polyglycolide rods for
the internal fixation of displaced bimalleolar fractures. Int Orthop
1990;14(1):1-8.
OM. Distal tibiofibular synostosis after malleolar fractures treated
using absorbable implants. Foot Ankle 1993;14(1):38-43.
OM. Metallic or absorbable fracture fixation devices. A cost
minimization analysis. Clin Orthop Relat Res 1996;329:233-239.
O, Mäkelä EA, Södergrd J, et ak. Absorbable polyglycolide pins in
internal fixation of fractures in children. J Pediatr Orthop
1993;13:242-245.
SH, Peach BG. Spontaneous resolution of an osseous bridge affecting the
distal tibial epiphysis. J Bone Joint Surg Br 1996;78(4):662-663.
MI, Bowen V, Weiler P. Reconstruction of a severe grinding injury to
the medial malleolus and the deltoid ligament of the ankle using a free
plantaris tendon graft and vascularized gracilis free muscle transfer:
case report. J Trauma 1994;36(3):454-457.
KJ, Jaramillo D, DiCanzio J, et al. Radiographic appearance of the
normal distal tibiofibular syndesmosis in children. J Pediatr Orthop
1999;19(1):14-21.
GJ, Greer RB. Traumatic rotational displacements of the distal tibial
growth plate. A case report. J Bone Joint Surg Am 1970;52(8):1666-1668.
SD, Kasser JR, Zurakowski D, et al. Analysis of 51 tibial triplane
fractures using CT with multiplanar reconstruction. AJR Am J Roentgenol
2004;183(5):1489-1495.
RW, Henry S, Henley MB. Fixation with bioabsorbable screws for the
treatment of fractures of the ankle. J Bone Joint Surg Am
1994;76(3):319-324.
BD, Pappas AM. Chronic, painful ankle instability in skeletally
immature athletes. Ununited osteochondral fractures of the distal
fibula. Am J Sports Med 1996; 24(5):647-651.
J, Spence L, Blickman H, et al. MRI of pediatric growth plate injury:
correlation with plain film radiographs and clinical outcome. Skeletal
Radiol 1998;27(5):250-255.
CO, Crenshaw AH. Clinical significance of a classification of
epiphyseal injuries at the ankle. Am J Surg 1955;89:879-889.
JR, Peterson HA. Salter-Harris Type-IV injuries of the distal tibial
epiphyseal growth plate, with emphasis on those involving the medial
malleolus. J Bone Joint Surg Am 1983;65(8):1059-1070.
CJ. Spontaneous resolution of varus deformity at the ankle following
adduction injury of the distal tibial epiphysis. A case report. J Bone
Joint Surg Am 1982; 64(5):774-776.
VT. Decision rules for roentgenography of children with acute ankle
injuries. Arch Pediatr Adolesc Med 1995;149(3):255-258.
M, Costello R, Mooney JF 3rd, et al. Ankle joint biomechanics following
transepiphyseal screw fixation of the distal tibia. J Pediatr Orthop
2005;25(5):635-640.
DA, Worlock PH. Triplane fracture of the distal tibia. A variant in
cases with an open growth plate. J Bone Joint Surg Br
1987;69(3):412-415.
DR, Spiegel PG, Laros GS. Tibial fractures involving the ankle in
children. The so-called triplane epiphyseal fracture. J Bone Joint Surg
Am 1978;60(8): 1040-1046.
G, Thambapillay S, Templeton PA. Compartment syndrome with an isolated
Salter Harris II fracture of the distal tibia. J Orthop Trauma
2008;22(2):148-150.
PJ, Clarke NM. Juvenile Tillaux fracture of the ankle associated with a
tibial shaft fracture: a unique combination. Injury 1996;27(3):221-222.
L. Fractures of the tibia and fibula. In: Rockwood CA, Wilkins KE, King
RE, eds. Fractures in Children. 3rd ed. Philadelphia: J.B. Lippincott,
1991.
JP, Azzoni M, Davidson RS, et al. Major lower extremity lawn mower
injuries in children. J Pediatr Orthop 1995;15 (1):78-82.
RP, Barei DP, Kubiak EN, et al. Early limited internal fixation of
diaphyseal extensions in select pilon fractures: upgrading AO/OTA type
C fractures to AO/OTA type B. J Orthop Trauma 2008;22(6):426-429.
JP, Barrack RL, Alexander AH, et al. Triplane fracture of the distal
tibial epiphysis. Long-term follow-up. J Bone Joint Surg Am
1988;70(7):967-976.
DS, Otsuka NY, Hedden DM. Extra-articular triplane fracture of the
distal tibial epiphysis. J Pediatr Orthop 1995;15(4):479-481.
DS, Shin SS, Madan S, et al. Correction of tibial malunion and nonunion
with six-axis analysis deformity correction using the Taylor Spatial
Frame. J Orthop Trauma 2003;17(8):549-554.
SL, Shoemaker S, Mubarak SJ. Altered fibular growth patterns after
tibiofibular synostosis in children. J Bone Joint Surg Am
2001;83-A(2):247-254.
J, Moller BN. Biodegradable fixation of ankle fractures. Complications
in a prospective study of 25 cases. Acta Orthop Scand
1992;63(4):434-436.
GT, Peterson HA, Berquist TH. Premature partial physeal arrest.
Diagnosis by magnetic resonance imaging in two cases. Clin Orthop Relat
Res 1991;272:242-247.
MJ, Friedman J, Hawkins EP, et al. Infections complicating lawnmower
injuries in children. Pediatr Infect Dis J 1996;15(5):452-455.
GG, Abbott LC. Varus deformity of ankle following injury to distal
epiphyseal cartilage of tibia in growing children. Surg Gynecol Obstet
1941;72:659-666.
JT, Lipton GE, Bowen JR, et al. Delayed union following stress fracture
of the distal fibula secondary to rotational malunion of lateral
malleolar fracture. Am J Orthop 1997;26(6):442-445.
L, Kiljunen V, Arnala I, et al. Effect of ultrasound therapy on bone
healing of lateral malleolar fractures of the ankle joint fixed with
bioabsorbable screws. J Orthop Sci 2005;10(4):391-395.
N, Kato F, Hayashi H. New radiographic projections for avulsion
fractures of the lateral malleolus. J Bone Joint Surg Br
1998;80(4):684-688.
N, Toga H, Shiba N, et al. Avulsion fracture of the lateral ankle
ligament complex in severe inversion injury: incidence and clinical
outcome. Am J Sports Med 2007;35(7):1144-1152.
N, Roye DP, Adler PA, et al. Nonunion of pediatric fibula fractures:
easy to overlook, painful to ignore. Pediatr Radiol 1994;24(4):248-250.
P, Lizler J. Magnetic resonance imaging in the evaluation of partial
growth arrest after physeal injuries in children. J Bone Joint Surg Am
1991;73(8):1234-1241.
WA 3rd, Starkweather KD, Meyer J, et al. Triplane fracture associated
with a proximal third fibula fracture. Am J Orthop 1996;25(6):449-451.
D Jr, Sanders RW, Scaduto JM, et al. Vacuum-assisted wound closure (VAC
therapy) for the management of patients with high-energy soft tissue
injuries. J Orthop Trauma 2003;17(10):683-688.
E. Fracture fixation with biodegradable rods. Forty-one cases of severe
ankle fractures. Acta Orthop Scand 1989;60(5):601-606.
JH, Nichter LS, Kenney JG, et al. Lawnmower injuries in children: lower
extremity reconstruction. J Trauma 1985;25(12):1138-1146.
D, O’Brien T. Growth disturbance lines after injury of the distal
tibial physis. Their significance in prognosis. J Bone Joint Surg Br
1988;70(2):231-233.
S, Takao M, Nishi H, et al. Arthroscopy-assisted reduction and
percutaneous fixation for triplane fracture of the distal tibia.
Arthroscopy 2004;20(10):e123-128.
J, Schmidt S, Ishaque N, et al. [Epiphyseal injuries of the distal
tibia. Does MRI provide useful additional information?]. Radiologe
1999;39(1):25-29.
JG, Miyanji F. The complex triplane fracture: ipsilateral tibial shaft
and distal triplane fracture. J Trauma 2001;51(4):714-716.
MM, Lagaay P, Schuberth JM. Arthroscopic assisted fixation of juvenile
intra-articular epiphyseal ankle fractures. J Foot Ankle Surg
2007;46(5):376-386.
EW Jr, Fahl JC. Fractures involving the distal epiphysis of the tibia
and fibula in children. Am J Surg 1957;93(5):778-781.
S, Phillips N, Ali F, et al. Triplane fractures of the distal tibia
requiring open reduction and internal fixation. Preoperative planning
using computed tomography. Injury 2003;34(4):293-298.
J. The triplane fracture: four years of follow-up of 21 cases and
review of the literature. J Pediatr Orthop B 1997;6(2):91-102.
J, Hansson LI, Laurin S. Computed tomography of intraarticular
supination-eversion fractures of the ankle in adolescents. J Pediatr
Orthop 1981;1(2):181-187.
J, Hansson LI, Laurin S. Pronation injuries of the ankle in children.
Retrospective study of radiographical classification and treatment.
Acta Orthop Scand. 1983; 54(1):1-17.
J, Hansson LI, Laurin S. Supination-eversion injuries of the ankle in
children: a retrospective study of radiographic classification and
treatment. J Pediatr Orthop 1982;2(2):147-159.
J, Hansson LI, Selvik G. Changes in tibiofibular relationships due to
growth disturbances after ankle fractures in children. J Bone Joint
Surg Am 1984;66(8): 1198-1210.
JP, Lamberg T, Korkala O, et al. Fixation of syndesmotic ruptures in 38
patients with a malleolar fracture: a randomized study comparing a
metallic and a bioabsorbable screw. J Orthop Trauma 2005;19(6):392-395.
A, Altay T, Ozturk H, et al. Open reduction and internal fixation in
displaced juvenile Tillaux fractures. Injury 2007;38(2):201-205.
DM, Caligiuri DA, Katzman BM. Local-advancement soft-tissue coverage in
a child with ipsilateral grade IIIB open tibial and ankle fractures. J
Orthop Trauma 1996; 10(8):577-580.
TF Jr, Bright RW, Hensinger RN. Distal tibial physeal fractures in
children that may require open reduction. J Bone Joint Surg Am
1984;66(5):647-657.
N. Fractures of the ankle. II. Combined experimental-surgical and
experimental-roentgenologic investigations. Arch Surg
1950;60(5):957-985.
WL, Jones WW. Intravenous lidocaine for anesthesia in the lower
extremity. A prospective study. J Bone Joint Surg Am
1984;66(7):1056-1060.
RE, Knox CL, Comstock RD. Epidemiology of 1.6 million pediatric
soccerrelated injuries presenting to US emergency departments from 1990
to 2003. Am J Sports Med 2007;35(2):288-293.
A, Stein H. Hybrid thin wire external fixation: an effective, minimally
invasive, modular surgical tool for the stabilization of periarticular
fractures. Orthopaedics 2004; 27(1):59-62.
M, Davidson D, Mukhtar I. Surgical management of chronic lateral ankle
instability in adolescents. J Pediatr Orthop 2003;23(3):392-397.
N, Blasier RD. Direct reduction with indirect fixation of distal tibial
physeal fractures: a report of a technique. J Pediatr Orthop
1996;16(1):107-112.
RT, Brown KL, Zaleske DJ, et al. Extremity lawnmower injuries in
children: report by the Research Committee of the Pediatric Orthopaedic
Society of North America. J Pediatr Orthop 1997;17(3):360-369.
EL, Ollivierre CO. Closed anatomic reduction of a juvenile tillaux
fracture by dorsiflexion of the ankle. A case report. Clin Orthop Relat
Res 1992;276:262-266.
AB, Mendoza-Sagaon M, Cardinaux C, et al. Evaluation of scooter-related
injuries in children. J Pediatr Surg 2002;37(5):755-759.
DC, Rajmaira S. Distribution of physeal and nonphyseal fractures in
2650 longbone fractures in children aged 0 to 16 years. J Pediatr
Orthop 1990;10(6):713-716.
K, Sato Y, Suzuki H, et al. MRI study of bioabsorbable poly-L-lactic
acid devices used for fixation of fracture and osteotomies. J Orthop
Sci 2006;11(2): 154-158.
JD, Clarke HJ, Jinnah RH. The effect of loading on tibiotalar alignment
in cadaver ankles. Foot Ankle 1990;10(5):280-284.
MD. Arthroscopically assisted reduction and fixation of an adult
Tillaux fracture of the ankle. Arthroscopy 1997;13(1):117-119.
R, Schuberth JM. Nonunion of an epiphyseal fibular fracture in a
pediatric patient. J Foot Ankle Surg 2006;45(6):410-412.
MS, Kim I, Rhee SK, et al. Varus and internal rotational deformity of
the ankle secondary to distal tibial physeal injury. Bull Hosp Jt Dis
1997;56(3):145-148.
JF 3rd, DeFranzo A, Marks MW. Use of cross-extremity flaps stabilized
with external fixation in severe pediatric foot and ankle trauma: an
alternative to free tissue transfer. J Pediatr Orthop 1998;18(1):26-30.
SJ. Extensor retinaculum syndrome of the ankle after injury to the
distal tibial physis. J Bone Joint Surg Br 2002;84(1):11-14.
K, Kishan S, Sabharwal S. Posttraumatic pediatric distal tibiofibular
synostosis: a case report. Foot Ankle Int 2004;25(6):429-433.
JA, Gonzalez-Lopez JL, Lopez-Valverde S, et al. Premature physeal
closure after tibial diaphyseal fractures in adolescents. J Pediatr
Orthop 2000;20(2):193-196.
SP, Papavasiliou VA, Papavasiliou AV. Outcome of physeal and epiphyseal
injuries of the distal tibia with intra-articular involvement. J
Pediatr Orthop 2005; 25(4):518-522.
AB, Colton CL. Rotational displacement of the lower tibial epiphysis
due to trauma. J Bone Joint Surg Br 1977;59(3):331-332.
I, Ezra E, Wientroub S. Closed posterior dislocation of the ankle
without associated fracture in a child. J Trauma 1999;46(2):350-351.
S, Saarela J. Exertion injuries to young athletes: a follow-up research
of orthopaedic problems of young track and field athletes. Am J Sports
Med 1978;6(2):68-74.
A, van Niekerk L. Arthroscopic assisted reduction and fixation of a
juvenile Tillaux fracture. Knee Surg Sports Traumatol Arthrosc
2007;15(4):415-417.
G, Kontakis G, Giannoudis P, et al. External fixation devices in the
treatment of fractures of the tibial plafond: a systematic review of
the literature. J Bone Joint Surg Br 2008;90(1):1-6.
HA, Madhok R, Benson JT, et al. Physeal fractures: part 1. Epidemiology
in Olmsted County, Minnesota, 1979-1988. J Pediatr Orthop
1994;14(4):423-430.
P, Panuel M, Faure F, et al. Acute fracture of the distal tibial
physis: role of gradient-echo MR imaging versus plain film examination.
AJR Am J Roentgenol 1996; 166(5):1203-1206.
P, Sapin C, Henry G, et al. Rate of abnormal osteoarticular
radiographic findings in pediatric patients. AJR Am J Roentgenol
2001;176(4):987-990.
LS, Meyer RA Jr, Gruber HE, et al. Effect of interposed periosteum in
an animal physeal fracture model. Clin Orthop Relat Res 2000;376:15-25.
H. Extra centre of ossification for the medial malleolus in children:
incidence and significance. J Bone Joint Surg 1961;43B:107-113.
PL, Hamilton W. Changes in tibiotalar area of contact caused by lateral
talar shift. J Bone Joint Surg Am 1976;58(3):356-357.
JM, Ocete G, Gonzalez-Herranz P, et al. Distal tibial triplane
fractures: long-term follow-up. J Pediatr Orthop 1996;16(1):113-118.
RB. The use of external fixation devices in the management of severe
lower-extremity trauma and pelvic injuries in children. Clin Orthop
Relat Res 1984;188:21-33.
B, Amspacher JC, Wilson PC, et al. Subatmospheric pressure dressing as
a bridge to free tissue transfer in the treatment of open tibia
fractures. Plast Reconstr Surg 2008;121(5):1664-1673.
MT, Gaynor TP, Pawelek J, et al. Salter-Harris I and II fractures of
the distal tibia: does mechanism of injury relate to premature physeal
closure? J Pediatr Orthop 2006;26(3):322-328.
S, Schwechter EM. Five-year follow-up of ankle joint distraction for
posttraumatic chondrolysis in an adolescent: a case report. Foot Ankle
Int 2007;28(8): 942-948.
F, Chotel F, Guibal AL, et al. Three-dimensional MR imaging in the
assessment of physeal growth arrest. Eur Radiol 2004;14(9):1600-1608.
MM, Peterson HA. Opening-wedge osteotomy for angular deformities of
long bones in children. J Bone Joint Surg Am 1994;76(3):325-334.
I, Wedge JH. Percutaneous reduction and fixation of displaced juvenile
Tillaux fractures: a new surgical technique. J Pediatr Orthop
1993;13(3):389-391.
J, Laun R, Paris S, et al. [Value of magnetic resonance tomography
(MRI) in diagnosis of triplane fractures of the distal tibia].
Unfallchirurg 2001;104(6):524-529.
AY, Moran ME, Wenger DR. Intramalleolar triplane fractures of the
distal tibial epiphysis. J Pediatr Orthop 1997;17(3):352-355.
A, Nordin L, Hill RA. Spatial frame correction of anterior growth
arrest of the proximal tibia: report of three cases. J Pediatr Orthop B
2008;17(2):61-64.
RS, Arkin AM. Posttraumatic aseptic necrosis of the distal tibial
epiphysis; report of a case. J Bone Joint Surg Am 1950;32-A(3):691-694.
IP, Luthje PM, Mikkonen RH. Ruptured tibiofibular syndesmosis:
comparison study of metallic to bioabsorbable fixation. Foot Ankle Int
2002;23(8):744-748.
BG, Rand F, Jaramillo D, et al. Early MR imaging of lower-extremity
physeal fracture-separations: a preliminary report. J Pediatr Orthop
1994;14(4):526-533.
PG, Cooperman DR, Laros GS. Epiphyseal fractures of the distal ends of
the tibia and fibula. A retrospective study of 237 cases in children. J
Bone Joint Surg Am 1978;60(8):1046-1050.
SD, Stricker SJ, Hulen CA. Juvenile Tillaux fracture simulating
syndesmosis separation: a case report. Foot Ankle Int
1998;19(5):332-335.
IG, Greenberg GH, McKnight RD, et al. A study to develop clinical
decision rules for the use of radiography in acute ankle injuries. Ann
Emerg Med 1992;21(4): 384-390.
Y, Takaoka T, Tanaka Y, et al. Results of opening-wedge osteotomy for
the treatment of a posttraumatic varus deformity of the ankle. J Bone
Joint Surg Am 1998; 80(2):213-218.
IS, Clare MP, Marcantonio A, et al. An update on the management of
high-energy pilon fractures. Injury 2008;39(2):142-154.
RR, Resnick CT, Wagner KS, et al. Changes in tibiotalar joint contact
areas following experimentally induced tibial angular deformities. Clin
Orthop Relat Res 1985; 199:72-80.
NO, Overgaard S, Olsen LH, et al. Observer variation in the
radiographic classification of ankle fractures. J Bone Joint Surg Br
1991;73(4):676-678.
AJ, Tarr RR, Sarmiento A, et al. The role of subtalar motion and ankle
contact pressure changes from angular deformities of the tibia. Foot
Ankle 1987;7(5):290-299.
CT J, Carter V, Hunt T, et al. Radiographic diagnosis of ankle
fractures: are three views necessary? Foot Ankle Int 1994;15(4):172-174.
Laer L. Classification, diagnosis, and treatment of transitional
fractures of the distal part of the tibia. J Bone Joint Surg Am
1985;67(5):687-698.
CL, Gruel CR, Herndon WA, et al. Lawnmower injuries of the pediatric
foot and ankle: observations on prevention and management. J Pediatr
Orthop 1995;15(4): 504-509.
JM, Gruber HE, Phieffer LS. Physeal fractures, part I: histologic
features of bone, cartilage, and bar formation in a small animal model.
J Pediatr Orthop 2002; 22(6):703-709.
TL, Martin DR, McIntyre LF, et al. Arthroscopic treatment of triplane
fractures of the ankle. Arthroscopy 1993;9(4):456-463.
RT, Berde CB, Wolohan M, et al. Reflex sympathetic dystrophy in
children. Clinical characteristics and follow-up of 70 patients. J Bone
Joint Surg Am 1992;74(6): 910-919.
