Hand
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > III – Upper Extremity Fractures and Dislocations > 24 – Hand
24
Hand
EPIDEMIOLOGY
-
Metacarpal and phalangeal fractures are common, comprising 10% of all fractures; >50% of these are work related.
-
The 1998 United States National Hospital
Ambulatory Medical Care Survey found phalangeal (23%) and metacarpal
(18%) fractures to be the second and third most common hand and forearm
fractures following radius fractures. They constitute anywhere from
1.5% to 28% of all emergency department visits, depending on survey
methods. -
Location: Border digits are most commonly involved with approximate incidence as follows:
-
Distal phalanx (45%)
-
Metacarpal (30%)
-
Proximal phalanx (15%)
-
Middle phalanx (10%)
-
-
Male-to-female ratios run from 1.8:1 to
5.4:1, with higher ratios seen in the age groups associated with the
greatest incidence (sports injuries in the early third decade and
workplace injuries in the fifth decade).
ANATOMY
Metacarpals
-
They are bowed, concave on palmar surface.
-
They form the longitudinal and transverse arches of the hand.
-
The index and long finger carpometacarpal articulation is rigid.
-
The ring and small finger carpometacarpal articulation is flexible.
-
Three palmar and four dorsal interosseous muscles arise from metacarpal shafts and flex the metacarpophalangeal (MCP) joints.
-
These muscles create deforming forces in
the case of metacarpal fractures, typically flexing the fracture (apex
dorsal angulation).
Phalanges
-
Proximal phalanx fractures usually angulate into extension (apex volar).
-
The proximal fragment is flexed by the interossei.
-
The distal fragment is extended by the central slip.
-
-
Middle phalanx fractures are unpredictable.
-
Distal phalanx fractures usually result from crush injuries and are comminuted tuft fractures.
MECHANISM OF INJURY
-
A high degree of variation in mechanism
of injury accounts for the broad spectrum of patterns seen in skeletal
trauma sustained by the hand. -
Axial load or “jamming” injuries are
frequently sustained during ball sports or sudden reaches made during
everyday activities such as to catch a falling object. Patterns
frequently resulting from this mechanism are shearing articular
fractures or metaphyseal compression fractures. -
Axial loading along the upper extremity
must also make one suspicious of associated injuries to the carpus,
forearm, elbow, and shoulder girdle. -
Diaphyseal fractures and joint
dislocations usually require a bending component in the mechanism of
injury, which can occur during ball handling sports or when the hand is
trapped by an object and is unable to move with the rest of the arm. -
Individual digits can easily be caught in
clothing, furniture, or workplace equipment to sustain torsional
mechanisms of injury, resulting in spiral fractures or more complex
dislocation patterns. -
Industrial settings or other environments
with heavy objects and high forces lead to crushing mechanisms that
combine bending, shearing, and torsion to produce unique patterns of
skeletal injury and associated soft tissue damage.
P.258
CLINICAL EVALUATION
-
History: a careful history is essential as it may influence treatment. This should include the patient’s:
-
Age
-
Hand dominance
-
Occupation
-
Systemic illnesses
-
Mechanism of injury: crush, direct trauma, twist, tear, laceration, etc.
-
Time of injury (for open fractures)
-
Exposure to contamination: barnyard, brackish water, animal/human bite
-
Treatment provided: cleansing, antiseptic, bandage, tourniquet
-
Financial issues: workers’ compensation
-
-
Physical examination includes:
-
Digital viability (capillary refill should be <2 seconds).
-
Neurologic status (documented by two-point discrimination [normal is 6 mm] and individual muscle testing).
-
Rotational and angulatory deformity.
-
Range of motion (documented by goniometer).
-
Malrotation at one bone segment is best
represented by the alignment of the next more distal segment. This
alignment is best demonstrated when the intervening joint is flexed to
90 degrees. Comparing nail plate alignment is an inadequate method of
evaluating rotation.
-
RADIOGRAPHIC EVALUATION
-
Posteroanterior, lateral, and oblique
radiographs of the affected digit or hand should be obtained. Injured
digits should be viewed individually, when possible, to minimize
overlap of other digits over the area of interest.
P.259
CLASSIFICATION
Descriptive
-
Open versus closed injury (see later)
-
Bone involved
-
Location within bone
-
Fracture pattern: comminuted, transverse, spiral, vertical split
-
Presence or absence of displacement
-
Presence or absence of deformity (rotation and/or angulation)
-
Extraarticular versus intraarticular fracture
-
Stable versus unstable
Open Fractures
Swanson, Szabo, and Anderson
| Type I: | Clean wound without significant contamination or delay in treatment and no systemic illness |
| Type II: | One or more of the following: |
-
Contamination with gross dirt/debris, human or animal bite, warm lake/river injury, barnyard injury
-
Delay in treatment >24 hours
-
-
Significant systemic illness, such as diabetes, hypertension, rheumatoid arthritis, hepatitis, or asthma
| Rate of infection: | Type I injuries (1.4%) Type II injuries (14%) |
-
Neither primary internal fixation nor
immediate wound closure is associated with increased risk of infection
in type I injuries. Primary internal fixation is not associated with
increased risk of infection in type II injuries. -
Primary wound closure is appropriate for type I injuries, with delayed closure appropriate for type II injuries.
OTA Classification of Metacarpal Fractures
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
OTA Classification of Phalangeal Fractures
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
TREATMENT: GENERAL PRINCIPLES
-
“Fight-bite” injuries: Any short, curved
laceration overlying a joint in the hand, particularly the
metacarpal-phalangeal joint, must be suspected of having been caused by
a tooth. These injuries must be assumed to be contaminated with oral
flora and should be addressed with broad-spectrum antibiotics (need
anaerobic coverage). -
Animal bites: Antibiotic coverage is needed for Pasterella and Eikenella.
-
There are essentially five major treatment alternatives:
-
The general advantages of entirely
nonoperative treatment are lower cost and avoidance of the risks and
complications associated with surgery and anesthesia. The disadvantage
is that stability is less assured than with some form of operative
fixation. -
CRIF is expected to prevent overt
deformity but not to achieve an anatomically perfect reduction. Pin
tract infection is the prime complication that should be mentioned to
patients in association with CRIF. -
Open treatments are considered to add the
morbidity of surgical tissue trauma, titrated against the presumed
advantages of the most anatomic and stable reduction. -
Critical elements in selecting between
nonoperative and operative treatment are the assessments of rotational
malalignment and stability.-
If carefully sought, rotational discrepancy is relatively easy to determine.
-
Defining stability is somewhat more
difficult. Some authors have used what seems to be the very reasonable
criterion of maintenance of fracture reduction when the adjacent joints
are taken through at least 30% of their normal motion.
-
-
Contraction of soft tissues begins
approximately 72 hours following injury. Motion should be instituted by
this time for all joints stable enough to tolerate rehabilitation. -
General indications for surgery include:
-
Open fractures.
-
Unstable fractures.
-
Irreducible fractures.
-
Multiple fractures.
-
Fractures with bone loss.
-
Fractures with tendon lacerations.
-
-
Treatment of stable fractures:
-
Buddy taping or splinting is performed, with repeat radiographs in 1 week.
-
Initially unstable fractures that are
reduced and then converted to a stable position: External
immobilization (cast, cast with outrigger splint, gutter splint, or
anterior-posterior splints) or percutaneous pinning prevents
displacement and permits earlier mobilization.
-
-
Treatment of unstable fractures:
-
Unstable fractures that are irreducible
by closed means or exhibit continued instability despite closed
treatment require closed reduction or ORIF, including Kirschner wire
fixation, interosseous wiring, tension band technique, interfragmentary
screws alone, or plates and screws.
-
-
Fractures with segmental bone loss
-
These continue to be problematic. The
primary treatment should be directed to the soft tissues, maintaining
length with Kirschner wires or external fixation.
-
P.261
MANAGEMENT OF SPECIFIC FRACTURE PATTERNS
Metacarpals
Metacarpal Head
-
Fractures include:
-
Epiphyseal fractures.
-
Collateral ligament avulsion fractures.
-
Oblique, vertical, and horizontal head fractures.
-
Comminuted fractures.
-
Boxer’s fractures with joint extension.
-
Fractures associated with bone loss.
-
-
Most require anatomic reduction (if possible) to reestablish joint congruity and to minimize posttraumatic arthrosis.
-
Stable reductions of fractures may be
splinted in the “protected position,” consisting of
metacarpal-phalangeal flexion >70 degrees to minimize joint
stiffness (Fig. 24.1). -
Percutaneous pinning may be necessary to
maintain reduction; severe comminution may necessitate the use of
minicondylar plate fixation or external fixation with distraction.
-
-
Early range of motion is essential.
Metacarpal Neck
-
Fractures result from direct trauma with
volar comminution and dorsal apex angulation. Most of these fractures
can often be reduced closed, but maintenance of reduction may be
difficult (Fig. 24.2).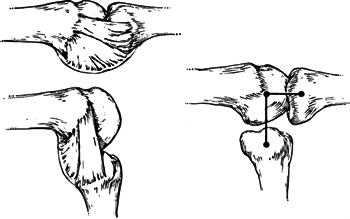 Figure
Figure
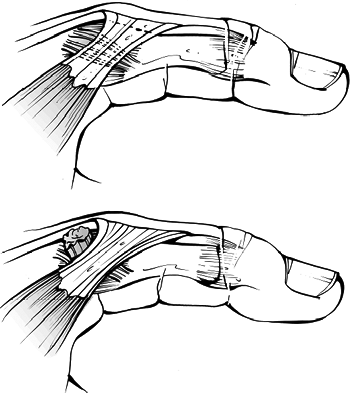
24.1. Left: The collateral ligaments of the metacarpophalangeal joints
are relaxed in extension, permitting lateral motion, but they become
taut when the joint is fully flexed. This occurs because of the unique
shape of the metacarpal head, which acts as a cam. Right: The distance
from the pivot point of the metacarpal to the phalanx in extension is
less than the distance in flexion, so the collateral ligament is tight
when the joint is flexed.(From Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 4th ed, vol. 1. Philadelphia: Lippincott-Raven, 1996:659.)![]() Figure
Figure
24.2. Reduction of metacarpal fractures can be accomplished by using
the digit to control the distal fragment, but the proximal
interphalangeal joint should be extended rather than flexed.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
The degree of acceptable deformity varies according to the metacarpal injured:
-
Less than 10-degree angulation for the second and third metacarpals.
-
Less than 30- to 40-degree angulation for the fourth and fifth metacarpals.
-
-
Unstable fractures require operative
intervention with either percutaneous pins (may be intramedullary or
transverse into the adjacent metacarpal) or plate fixation.
P.262
Metacarpal Shaft
-
Nondisplaced or minimally displaced fractures can be reduced and splinted in the protected position.
-
Operative indications include rotational
deformity, dorsal angulation >10 degrees for second and third
metacarpals, and >40 degrees for fourth and fifth metacarpals. -
Ten degrees of malrotation (which risks
as much as 2 cm of overlap at the digital tip) should represent the
upper tolerable limit. -
Operative fixation may be achieved with
either closed reduction and percutaneous pinning (intramedullary or
transverse into the adjacent metacarpal) or open reduction and plate
fixation.
P.263
Metacarpal Base
FINGERS
-
Fractures of the base of the second,
third, and fourth fingers are generally minimally displaced and are
associated with ligament avulsion. Treatment is by splinting and early
motion in most cases. -
The reverse Bennett fracture is a fracture-dislocation of the base of the fifth metacarpal/hamate.
-
The metacarpal is displaced proximally by the pull of the extensor carpi ulnaris.
-
The degree of displacement is best
ascertained via radiograph with the hand pronated 30 degrees from a
fully supinated (anteroposterior) position. -
This fracture often requires surgical intervention with ORIF.
-
THUMB
-
Extraarticular fractures: These are
usually transverse or oblique. Most can be held by closed reduction and
casting, but some unstable fractures require closed reduction and
percutaneous pinning. The basal joint of the thumb is quite forgiving,
and an anatomic reduction of an angulated shaft fracture is not
essential. -
Intraarticular fractures (Figs. 24.3 and 24.4):
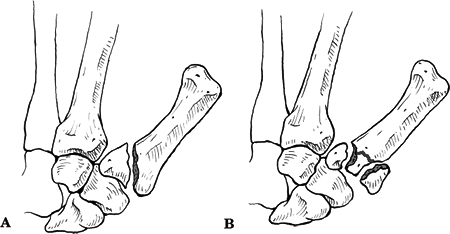 Figure
Figure
24.3. The most recognized patterns of thumb metacarpal base
intraarticular fractures are (A) the partial articular Bennett fracture
and (B) the complete articular Rolando fracture.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)![]() Figure
Figure
24.4. Displacement of Bennett fractures is driven primarily by the
abductor pollicis longus and the adductor pollicis resulting in
flexion, supination, and proximal migration.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
P.264
| Type I: | Bennett fracture: fracture line separates major part of metacarpal from volar lip fragment, producing a disruption of the first carpometacarpal (CMC) joint; first metacarpal is pulled proximally by the abductor pollicis longus. |
| Type II: | Rolando fracture: requires greater force than a Bennett fracture; presently used to describe a comminuted Bennett fracture, a “Y” or “T” fracture, or a fracture with dorsal and palmar fragments. |
-
Treatment: Both type I and II fractures
of the base of the first metacarpal may be treated with closed
reduction and percutaneous pins, or ORIF.
Proximal and Middle Phalanges
Intraarticular Fractures
-
Condylar fractures: single, bicondylar, osteochondral
-
They require anatomic reduction; ORIF should be performed for >l mm displacement.
-
Comminuted intraarticular phalangeal
fractures should be treated with reconstruction of the articular
surface, if possible. Severely comminuted fractures that are deemed
nonreconstructible may be treated closed with early protected
mobilization.
-
P.265
Fracture-Dislocations
-
Volar lip fracture of middle phalangeal base (dorsal fracture-dislocation)
-
Treatment is controversial and depends on percentage of articular surface fractured:
-
Hyperextension injuries without a history
of dislocation with <30% to 35% articular involvement: Buddy tape to
the adjacent digit. -
More than 30% to 35% articular
involvement: Some recommend ORIF with reconstruction of the articular
surface or a volar plate arthroplasty if the fracture is comminuted;
others recommend nonoperative treatment with a dorsal extension block
splint if the joint is not subluxed.
-
-
Dorsal lip fracture of middle phalangeal base (volar fracture-dislocation)
-
Usually this is the result of a central slip avulsion.
-
Fractures with <1 mm of displacement: may be treated closed with splinting, as in a boutonniere injury.
-
Fractures with >l mm of displacement
or volar subluxation of the proximal interphalangeal (PIP) joint:
Operative stabilization of the fracture is indicated.
-
Extraarticular Fractures
-
Fractures at the base of the middle
phalanx tend to angulate apex dorsal, whereas fractures at the neck
angulate the apex volarly owing to the pull of the sublimis tendon (Fig. 24.5).
P.266
Closed reduction should be attempted initially with finger-trap traction followed by splinting.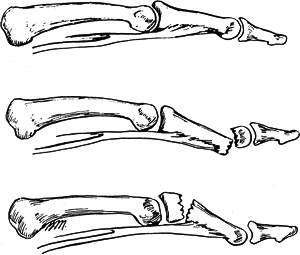 Figure
Figure
24.5. Top: A lateral view, showing the prolonged insertion of the
superficialis tendon into the middle phalanx. Center: A fracture
through the neck of the middle phalanx is likely to have a volar
angulation because the proximal fragment is flexed by the strong pull
of the superficialis. Bottom: A fracture through the base of the middle
phalanx is more likely to have a dorsal angulation because of the
extension force of the central slip on the proximal fragment and a
flexion force on the distal fragment by the superficialis.(From Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 4th ed, vol. 1. Philadelphia: Lippincott-Raven, 1996:627.)![]() Figure
Figure
24.6. Fracture patterns seen in the distal phalanx include (A)
longitudinal shaft, (B) transverse shaft, (C) tuft, (D) dorsal base
avulsion, (E) dorsal base shear, (F) volar base, and (G) complete
articular.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Fractures in which a stable closed
reduction cannot be achieved or maintained should be addressed with
closed reduction and percutaneous pinning or ORIF with minifragment
implants.
Distal Phalanx (Fig. 24.6)
Intraarticular Fractures
-
Dorsal lip
-
Treatment remains somewhat controversial.
-
Some recommend nonoperative treatment for
all mallet fingers with full-time extension splinting for 6 to 8 weeks,
including those with a significant articular fracture and joint
subluxation. -
Others recommend CRIF for displaced
dorsal base fractures comprising >25% of the articular surface.
Various closed pinning techniques are possible, but the mainstay is
extension block pinning.
-
-
Volar Lip
-
This is associated with flexor digitorum
profundus rupture (“jersey finger:” seen in football and rugby players,
most commonly involving the ring finger). -
Treatment is primary repair, especially with large, displaced bony fragments.
Extraarticular Fractures
-
These are transverse, longitudinal, and comminuted (nail matrix injury is very common).
-
Treatment consists of closed reduction and splinting.
-
The splint should leave the PIP joint
free but usually needs to cross the distal interphalangeal (DIP) joint
to provide adequate stability. Aluminum and foam splints or plaster of
Paris are common materials chosen. -
CRIF is indicated for shaft fractures with wide displacement because of the risk for nonunion.
Nailbed Injuries (Fig. 24.7)
-
These are frequently overlooked or
neglected in the presence of an obvious fracture, but failure to
address such injuries may result in growth disturbances of the nail.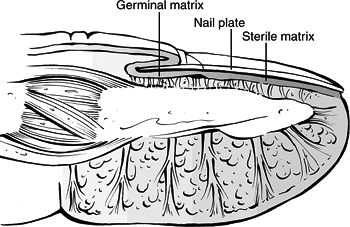 Figure
Figure
24.7. An intimate relationship exists between the three layers of the
dorsal cortex of the distal phalanx, the nail matrix (both germinal and
sterile), and the nail plate.(From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.) -
Subungual hematomas should be evacuated with cautery or a hot paper clip.
-
If the nailplate has been avulsed at its
base, it should be removed, cleansed with povidone-iodine, and retained
for use as a biologic dressing. -
Nailbed disruptions should be carefully sutured with 7-0 chromic catgut under magnification.
-
Polypropylene artificial nail dressings may be used if the original nailplate is not usable as a biologic dressing.
P.268
Carpometacarpal (CMC) Joint Dislocations and Fracture-Dislocations
-
Dislocations at the finger CMC joints are
usually high-energy injuries with involvement of associated structures,
including neurovascular injury. -
Particular care must be given to the
examination of ulnar nerve function, especially motor, owing to its
close proximity to the fifth CMC joint. -
Overlap on the lateral x-ray obscures
accurate depiction of the injury pattern, and most authors recommend at
least one variant of an oblique view. -
When fracture-dislocations include the
dorsal cortex of the hamate, computed tomography may be necessary to
evaluate the pathoanatomy fully. -
Most thumb CMC joint injuries are
fracture-dislocations rather than pure dislocations. Terms associated
with these fracture-dislocations are Bennett (partial articular), and
Rolando (complete articular) fractures. -
Dorsal finger CMC fracture-dislocations
cannot usually be held effectively with external means alone. For those
injuries that can be accurately reduced, CRIF is the treatment of
choice.
Metacarpophalangeal (MCP) Joint Dislocations (Fig. 24.8)
-
Dorsal dislocations are the most common.
-
Simple dislocations are reducible and present with a hyperextension posture.
-
They are really subluxations, because some contact usually remains between the base of proximal phalanx and the metacarpal head.
-
Reduction can be achieved with simple
flexion of the joint; excessive longitudinal traction on the finger
should be avoided. Wrist flexion to relax the flexor tendons may assist
reduction. -
The other variety of MCP joint
dislocation is a complex dislocation, which is by definition
irreducible, most often the result of volar plate interposition.-
Complex dislocations occur most frequently in the index finger.
-
A pathognomonic x-ray sign of complex dislocation is the appearance of a sesamoid in the joint space.
-
-
Most dorsal dislocations are stable following reduction and do not need surgical repair of the ligaments or volar plate.
-
Volar dislocations are rare but are particularly unstable.
-
Volar dislocations are at risk for late instability and should have repair of the ligaments.
-
Open dislocations may be either reducible or irreducible.
P.269
Thumb Metacarpophalangeal (MCP) Joint Dislocations
 |
|
Figure
24.8. Simple metacarpophalangeal joint dislocations are spontaneously reducible and usually present in an extended posture with the articular surface of P1 sitting on the dorsum of the metacarpal head. Complex dislocations have bayonet apposition with volar plate interposition that prevents reduction. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
The thumb MCP joint, in addition to its
primary plane of flexion and extension, allows abduction-adduction and
a slight amount of rotation (pronation with flexion). -
With a one-sided collateral ligament
injury, the phalanx tends to subluxate volarly in a rotatory fashion,
pivoting around the opposite intact collateral ligament. -
The ulnar collateral ligament may have a
two-level injury consisting of a fracture of the ulnar base of proximal
phalanx with the ligament also ruptured off the fracture fragment. -
Of particular importance is the proximal
edge of the adductor aponeurosis that forms the anatomic basis of the
Stener lesion. The torn ulna collateral ligament stump comes to lie
dorsal to the aponeurosis and is thus prevented from healing to its
anatomic insertion on the volar, ulnar base of the proximal phalanx (Fig. 24.9). -
The true incidence of the Stener lesion remains unknown, because of widely disparate reports.
-
Nonoperative management is the mainstay of treatment for thumb MCP joint injuries.
-
Surgical management of thumb MCP joint
injuries is largely limited to ulna collateral ligament disruptions
with a Stener lesion and volar or irreducible MCP dislocations.
P.270
Proximal Interphalangeal (PIP) Joint Dislocations
 |
|
Figure
24.9. The Stener lesion: The adductor aponeurosis proximal edge functions as a shelf that blocks the distal phalangeal insertion of the ruptured ulnar collateral ligament of the thumb metacarpophalangeal joint from returning to its natural location for healing after it comes to lie on top of the aponeurosis. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
-
Dislocations of the PIP joint have a high rate of missed diagnoses that are passed off as “sprains.”
-
Although large numbers of incomplete
injuries occur (especially in ball-handling sports), complete
disruptions of the collateral ligaments and the volar plate are also
frequent (50% occur in the long finger followed in frequency by the
ring finger). -
Congruence on the lateral radiograph is the key to detecting residual subluxation.
-
Residual instability is quite rare in
pure dislocations, as opposed to fracture-dislocations, in which it is
the primary concern. -
Recognized patterns of dislocation other
than complete collateral ligament injury are dorsal dislocation, pure
volar dislocation, and rotatory volar dislocation. -
Dorsal dislocations involve volar plate injury (usually distally, with or without a small flake of bone).
-
For pure volar dislocations, the
pathologic findings are consistently damage to the volar plate, one
collateral ligament, and the central slip. -
Volar dislocation occurs as the head of
proximal phalanx passes between the central slip and the lateral bands,
which can form a noose effect and prevent reduction. -
In pure dislocations, stiffness is the
primary concern. Stiffness can occur following any injury pattern and
responds best at the late stage to complete collateral ligament
excision. -
Chronic missed dislocations require open reduction with a predictable amount of subsequent stiffness.
-
Treatment
-
Once reduced, rotatory volar
dislocations, isolated collateral ligament ruptures, and dorsal
dislocations congruent in full extension on the lateral radiograph can
all begin immediate active range of motion with adjacent digit
strapping. -
Dorsal dislocations that are subluxated on the extension lateral radiograph require a few weeks of extension block splinting.
-
Volar dislocations with central slip
disruptions require 4 to 6 weeks of PIP extension splinting, followed
by nighttime static extension splinting for 2 additional weeks. The DIP
joint should be unsplinted and actively flexed throughout the entire
recovery period. -
Open dorsal dislocations usually have a
transverse rent in the skin at the flexion crease. Debridement of this
wound should precede reduction of the dislocation.
-
P.271
Distal Interphalangeal (DIP) and Thumb Interphalangeal (IP) Joint Dislocations
-
Dislocations at the DIP/IP joint are often not diagnosed initially and present late.
-
Injuries are considered chronic after 3 weeks.
-
Pure dislocations without tendon rupture
are rare, usually result from ball-catching sports, are primarily
dorsal in direction, and may occur in association with PIP joint
dislocations. -
Transverse open wounds in the volar skin crease are frequent.
-
Injury to a single collateral ligament or to the volar plate alone at the DIP joint is rare.
Nonoperative Treatment
-
Reduced dislocations that are stable may begin immediate active range of motion.
-
The rare unstable dorsal dislocation
should be immobilized in 20 degrees of flexion for up to 3 weeks before
instituting active range of motion.-
The duration of the immobilization should
be in direct proportion to the surgeon’s assessment of joint stability
following reduction. -
Complete collateral ligament injuries should be protected from lateral stress for at least 4 weeks.
-
-
Should pin stabilization prove necessary
because of recurrent instability, a single longitudinal Kirschner wire
is usually sufficient.
Operative Treatment
-
Delayed presentation (>3 weeks) of a
subluxed joint may require open reduction to resect scar tissue and to
allow tension-free reduction. -
Open dislocations require thorough debridement to prevent infection.
-
The need for fixation with a Kirschner
wire should be based on the assessment of stability, and it is not
necessarily required for all open dislocations. -
The duration of pinning should not be >4 weeks, and the wire may be left through the skin for easy removal.
P.272
COMPLICATIONS
-
Malunion: Angulation can disturb
intrinsic balance and also can result in prominence of metacarpal heads
in the palm with pain on gripping. Rotational or angulatory
deformities, especially of the second and third metacarpals, may result
in functional and cosmetic disturbances, emphasizing the need to
maintain as near anatomic relationships as possible. -
Nonunion: This is uncommon, but it may
occur with extensive soft tissue injury and bone loss, as well as with
open fractures with gross contamination and infection. It may
necessitate debridement, bone grafting, or flap coverage. -
Infection: Grossly contaminated wounds
require meticulous debridement and appropriate antibiotics depending on
the injury setting (e.g., barnyard contamination, brackish water, bite
wounds), local wound care with debridement as necessary, and possible
delayed closure. -
Metacarpal-phalangeal joint extension
contracture: This may result if splinting is not in the protected
position (i.e., MCP joints at >70 degree) owing to soft tissue
contracture. -
Loss of motion: This is secondary to tendon adherence, especially at the level of the PIP joint.
-
Posttraumatic osteoarthritis: This may result from a failure to restore articular congruity.



