Talus Fractures: Open Reduction Internal Fixation
injuries. Because they are seen infrequently, most surgeons have
limited experience managing these fractures and their sequelae. Two
thirds of the talus is covered in articular cartilage, and all
fractures are articular injuries affecting one or more of the adjacent
joints. Operative treatment is usually necessary to restore hind foot
anatomy and mechanics, as well as joint congruity in the majority of
these fractures. Disruption of articular congruity and/or loss of talar
length, alignment, and rotation are general indications for operative
treatment. Even small residual-fracture displacement can result in a
significant compromise of subtalar, ankle, or talonavicular joint
function.
treated operatively if the fracture is displaced more than 1 to 2 mm.
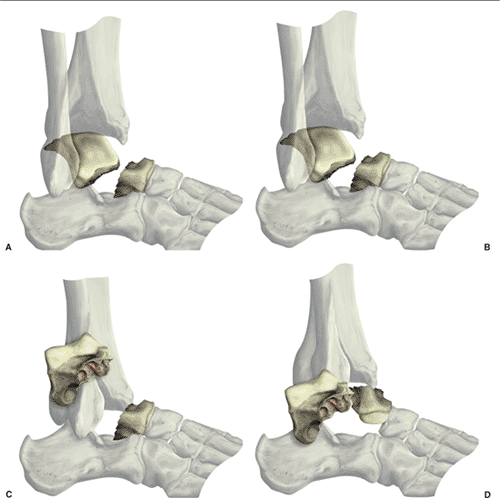
Talar neck fractures are classified into one of four types (Fig. 34.1).
Hawkins described types I, II, and III and Canale and Kelly described
type IV injuries that involve the talonavicular joint. Type I talar
neck fractures are nondisplaced injuries and can be managed
nonoperatively in cooperative patients who agree to frequent follow-up
x-rays. Any displacement should be considered significant and usually
warrants surgical intervention. Nondisplaced talar neck fractures that
are not visible on plain x-rays but diagnosed with other imaging
modalities, such as magnetic resonance imaging (MRI), computed
tomography (CT), or bone scans, may be treated nonoperatively. Types
II, III, and IV talar neck fractures are, by definition, displaced and
require reduction and fixation.
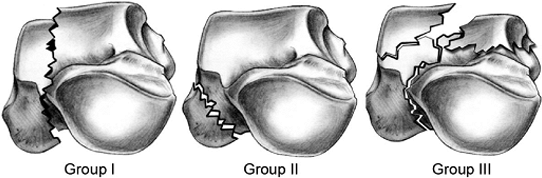
of both the tibiotalar and subtalar joints, and surgical restoration of
articular congruity, talar height, and ligamentous stability of the
ankle is usually the best option. Talar body fractures can be
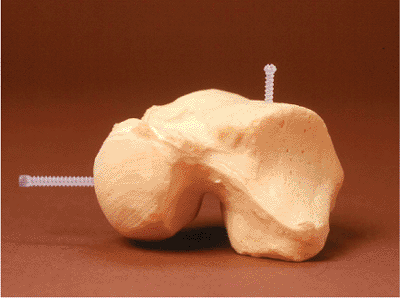
classified into cleavage, crush, and tubercle or process fractures (Fig. 34.2).
Because of the impaction mechanism of many of these injuries, anatomic
reduction of the joint surface is not always possible, but restoration
of height and stability of the hind foot is indicated to help diminish
long-term complications.
 |
|
Figure 34.1. Hawkins classification of talar neck fractures. A. Type I. B. Type II. C. Type III. D. Type IV.
|
 |
|
Figure 34.2. Talar body fractures. A. Group I cleavage fractures (horizontal, sagittal, coronal). B. Group II process or tubercle fractures. C. Group III crush with compression/impaction.
|
high-energy injuries. However, talar injuries are commonly overlooked
and may go unrecognized. This is particularly true in multiply injured
patients, and late treatment of the talar injury often results in
suboptimal outcomes. Occult foot or ankle injuries should be suspected
when foot and ankle swelling or ecchymosis is presented even when
obvious radiographic abnormalities are not found.
soft-tissue compromise, and limited ambulatory capacity are relative
contraindications to surgical management. Peripheral neuropathy is
highly variable in severity, and many elderly patients have some degree
of peripheral neuropathy that should not necessarily preclude operative
treatment. Loss of protective sensation, however, as judged by the
ability to differentiate a 5.07 monofilament, is a sensitive indicator
of significant neuropathy; therefore, failure to differentiate the
monofilament should be considered a relative contraindication to
surgery. The decision to operate also depends upon the fracture
pattern, ankle stability, and presence of dislocation or significant
joint subluxation and should be made on a case by case basis. A
minimally displaced talar body fracture in a patient with significant
neuropathy may be best treated nonoperatively, whereas a Hawkins III
talar neck fracture with posteromedial extrusion of the talar body
should be treated operatively, even in patients with significant
neuropathy, to relieve soft-tissue and/or neurovascular compromise.
Elderly patients with limited ambulatory capacity, similarly, may be
best treated nonoperatively if the joint is not significantly displaced
or dislocated.
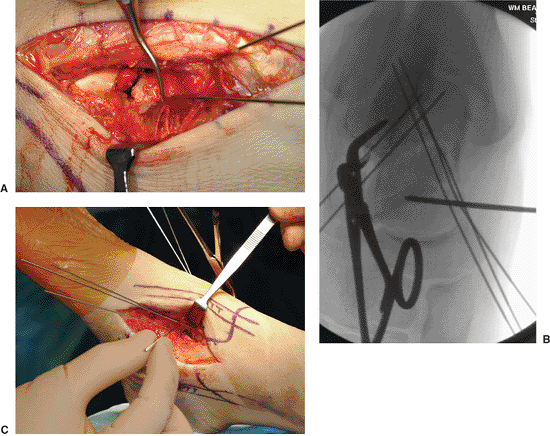
operative treatment of these fractures. For example, a dual incision
approach to a talar neck fracture may be contraindicated in situations
where the anterolateral skin is compromised (Fig. 34.3). Extensile exposures may also be contraindicated in patients with marginal perfusion of the extremity.
intervention for talar injuries remains controversial. Initial fracture
displacement, rather than the timing of reduction, is thought to be a
major factor controlling the development of osteonecrosis following
talar neck fractures. Fractures associated with joint subluxation or
dislocation, as well as those with soft-tissue compromise due to
fracture displacement, necessitate emergent reduction to avoid
neurovascular compromise and/or skin necrosis (see Fig. 34.3).
Because of the urgency of expedient reduction in these circumstances,
preoperative planning is invariably limited. If the peritalar joints
are reduced and fracture displacement is not significant, operative
fixation can be performed when soft-tissue swelling and bruising are
resolving and proper imaging studies have been obtained. In most
patients, a well-padded plaster or fiberglass splint provides adequate
temporary support and pain relief. Provisional, spanning, external
fixation to restore length and stability may occasionally be necessary
when the soft-tissue status precludes early open reduction.
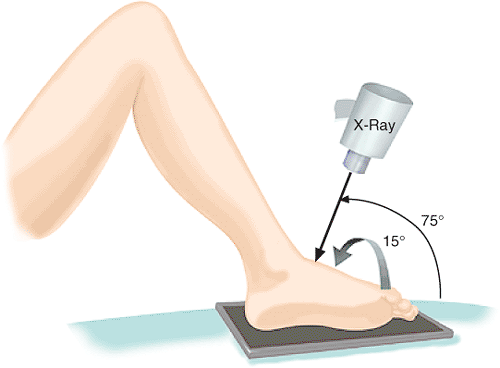
includes anteroposterior (AP), lateral, and oblique views of the foot
and ankle. The Canale oblique view (Fig. 34.4)
may be helpful to assess length and alignment of the talar neck.
Shortening of the medial column of the talus secondary to impaction is
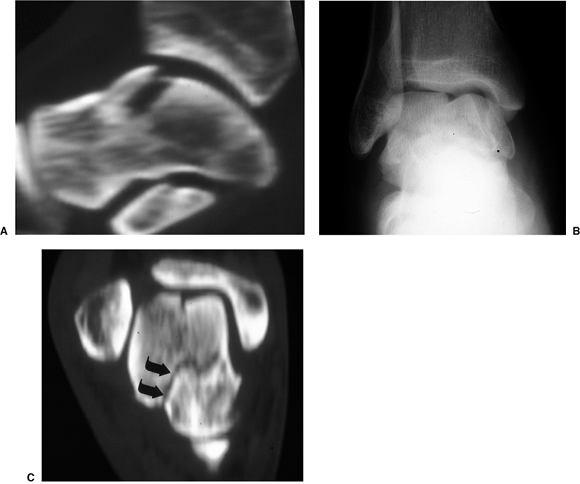
common in talar neck fractures and is well seen on the Canale view. CT
scans are also useful in defining the fracture pattern and detecting
occult fractures in the ankle and foot (Fig. 34.5). Concomitant osteochondral fractures are common with talar neck fractures and are not well visualized on plain x-rays.
very helpful when planning the surgical approach, methods of reduction,
and fixation techniques. For example, talar body fractures and type III
talar neck fractures with posteromedial extrusion of the talar body
often require transmalleolar exposure either through a concomitant
medial-malleolar fracture or osteotomy of the medial malleolus.
Reduction aids such as a femoral distractor may be necessary to reduce
an extruded talar body. Chondral and osteochondral fractures often
necessitate small-diameter subarticular screws or bioabsorbable
implants. By definition, talus fractures are articular injuries, and
having an assortment of small-diameter plates and screws will
facilitate anatomic restoration of the joint surface and rigid fracture
fixation to allow early motion.
 |
|
Figure 34.3. A,B. AP and lateral x-rays of a displaced talar neck fracture. C,D.
Clinical photos of the same patient with soft-tissue compromise and impending full-thickness necrosis because an early reduction was not performed. |
 |
|
Figure 34.4. Canale view to assess talar neck length and alignment.
|
 |
|
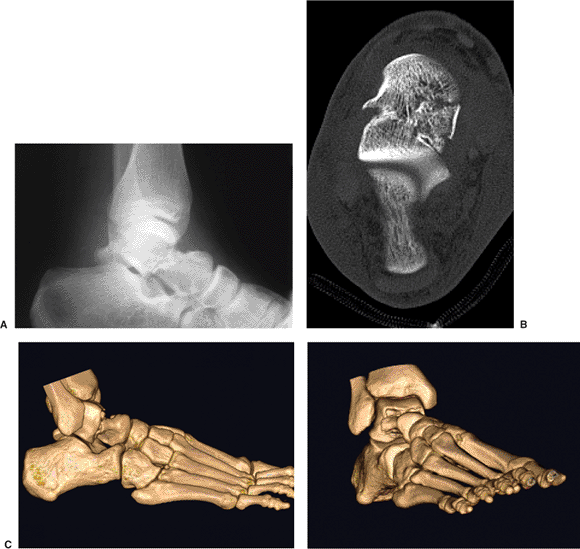
Figure 34.5. CT scanning can be helpful in identifying occult osteochondral fractures (A)
or fracture lines unrecognized on plain x-rays, such as this talar-neck fracture that occurred concomitant with a talar body fracture (B,C). |
extensile approaches are not recommended. Fracture pattern and
associated soft-tissue disruptions suggest potential avascular zones.
The goal of fracture surgery is to gain access to the bone for
reduction and fixation without further compromise of the remaining
blood supply. Unnecessary dissection should be avoided and ligamentous
attachments should be protected.
pattern, areas of comminution, medial neck shortening, and associated
osteochondral fractures (Fig. 34.6). The
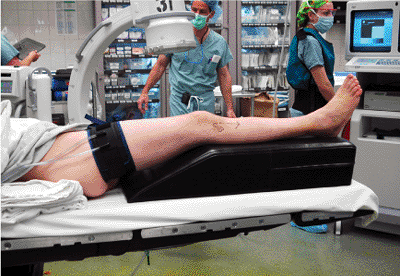
patient is positioned supine on a radiolucent operating table with a
bolster placed under the affected extremity. A well-padded pneumatic
tourniquet is placed on the proximal thigh. General anesthesia with
muscle paralysis is preferred to counteract potential
muscular-deforming forces in the hind foot. Intraoperative c-arm
fluoroscopy is utilized (Fig. 34.7).
dual incision technique in which anteromedial and anterolateral
incisions are utilized. Visualization of both the medial and lateral
talar neck regions allows for more accurate fracture reduction (Figs. 34.8 and 34.9). Oftentimes the dorsal and medial talar neck is comminuted and the lateral and plantar portion are not or visa versa.
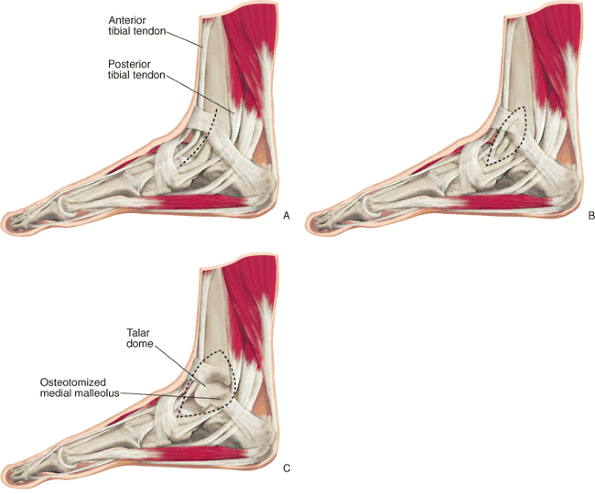
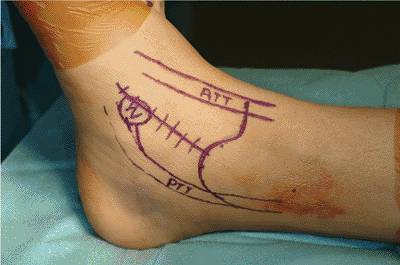
aspect of the medial malleolus to the medial cuneiform and is centered
midway between the tibialis anterior and tibialis posterior
tendons (Fig. 34.10).
This approach exposes the dorsomedial talar head and neck as well as
the anteromedial body. Proximally, the greater saphenous vein and nerve
are identified and protected. The tibiotalar and talonavicular joints
are exposed.
 |
|
Figure 34.6. A,B. Plain x-ray and CT image of Hawkins II talar neck fracture. C,D. Reconstruction images demonstrate medial neck comminution and varus angulation of the talar neck and supination of the foot.
|
 |
|
Figure 34.7. Patient positioning.
|
 |
|
Figure 34.8. A–C. Anterior medial approach to the talus.
|
preserved. The posterior, tibial, arterial branches should be protected
by avoiding plantar dissection along the medial neck. Similarly, the
integrity of the deltoid ligament must not be violated, and extensive
dissection of the tibiotalar joint capsule should be avoided.
Frequently the dorsal medial talar neck contains comminuted and or
impacted segments. The dorsal soft tissues are left intact and attached
to these fragments. Only 1 to 2 mm of periosteum around the fracture
site is elevated so a cortical reduction can be adequately visualized.
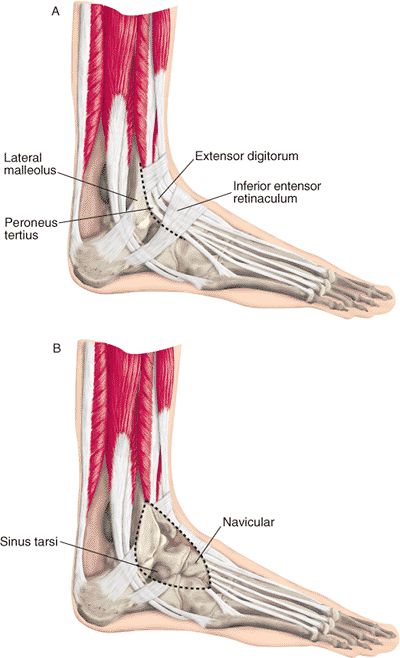
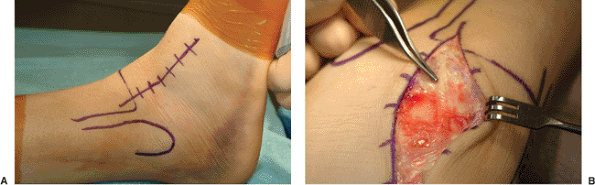
Proximally, it is midway between the tibia and fibula, and distally it
heads for the base of the fourth metatarsal. The intermediate branch of
the superficial peroneal nerve may be injured as it resides just
superficial to the fascia and extensor retinaculum (see Fig. 34.11B).
The nerve should be mobilized and protected. The extensor retinaculum
is sharply incised and the tendons retracted for improved visualization.
can be mobilized from lateral to medial by blunt dissection. The
extensor digitorum brevis is elevated and retracted distally and
inferiorly. This exposes the anterolateral body, lateral process, and
lateral talar neck, as well as the sinus tarsi.
and soft tissues between the two incisions should not be undermined.
The dorsalis pedis artery supplies this tissue flap, as well as
contributes blood supply to the talus through the dorsal soft-tissues
branches. If more exposure is desired, the anterior joint capsule can
be released from the anterior tibia. The fat pad about the sinus tarsi
can be debrided so the lateral neck and lateral process of the talus
can be better visualized. The subtalar joint is accessible through the
lateral incision. Longitudinal traction is then applied through the
calcaneus to distract the subtalar joint, and a pituitary rongeur is
used carefully to debride the joint (Figs. 34.12 and 34.13).
 |
|
Figure 34.9. A,B. Anterior lateral approach to the talus.
|
 |
|
Figure 34.10.
Medial approach: incision in the interval between the anterior and posterior tibial tendons from the medial malleolus to the navicular tuberosity. Proximal extension allows exposure for malleolar osteotomy. |
 |
|
Figure 34.11. Anterolateral approach. A. Incision from the anterolateral ankle joint in line with the fourth ray. B. Superficial peroneal nerve is vulnerable in the superficial dissection.
|
reduction and fixation. A Kirschner (K) wire can be placed across the
talar head fragment to act as a joystick and aid in reduction (Fig. 34.14C).
Typically, the lateral talar neck is not comminuted, and an anatomic
cortical reduction is possible. Length, alignment, and rotation are
corrected as the surgeon uses both incisions to judge reduction.
Smaller comminuted fragments are first reduced to the larger intact
segments and stabilized with K wires (see Fig. 34.14).
Once the gross reduction is achieved, it is checked with c-arm
fluoroscopy. Intraoperative axial alignment of the talar neck is best
evaluated using the Canale view. The tibiotalar reduction is best seen
on mortise and lateral views, and the subtalar joint is best assessed
on the lateral and 45-degree mortise view. The radiographic reduction
can be compared to like views of the contralateral side taken
preoperatively.
 |
|
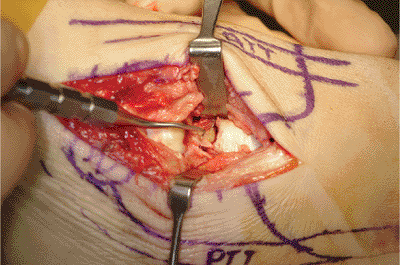
Figure 34.12.
Medial exposure showing medial neck comminution and shortening. (Copyright © 2001 American Academy of Orthopaedic Surgeons, Reprinted from the Journal of the American Academy of Orthopaedic Surgeons, Volume 9(2), pp. 114–127
, with permission.) |
 |
|
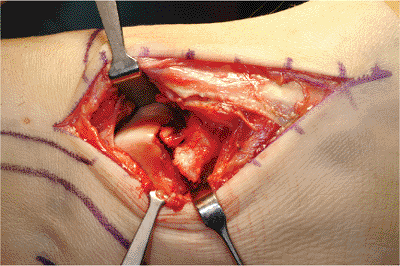
Figure 34.13. Anterolateral exposure showing displacement of the lateral talar neck.
|
comminution, and bone quality. Small-fragment and minifragment implants
of adequate strength and variety must be available. For noncomminuted
talar neck fractures, longitudinal, 3.5-mm, cortical, lag screws placed
from the talar head into the body provide adequate fixation (Fig. 34.15).
These screws are placed in both the medial and lateral columns of the
talus. The desired orientation of the screws approximates parallel, but
this is difficult to achieve because the navicular covers the talar
head and the forefoot hinders a longitudinal trajectory. The medial
navicular can be recessed using a burr or rongeur to allow a more
lateral and longitudinal starting point and trajectory for the medial
screw. When placing screws from an articular starting point, the
surgeon should countersink the screw head to minimize impingement.
 |
|
Figure 34.14. A. Provisional K-wire fixation. B,C. K wire in the talar head used as a joy stick to correct varus angulation and to restore medial neck length.
|
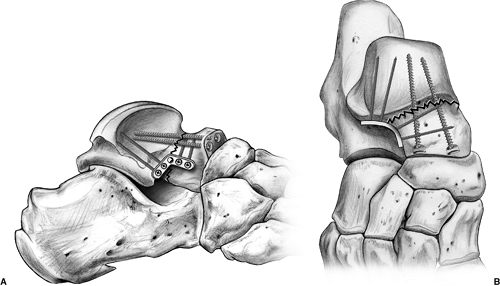
dorsomedial comminution. Longitu-dinal lag-screw fixation in these
cases results in fracture shortening, angulation, or displacement. For
these fractures, to improve fracture stability and prevent talar neck
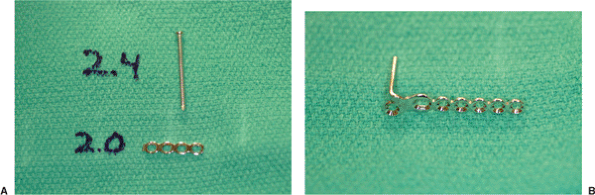
shortening, minifragment plates and screws are necessary; 1.5-, 2.0-,
2.4-mm implants are available (Fig. 34.16).
used for both comminuted and noncomminuted fractures. A five-hole
2.0-mm plate is contoured to fit the lateral talar neck and spans from
the anterior surface of the lateral process of the talus, along the
lateral talar neck, to the head and neck junction. This plate is
extra-articular, and the best fit is usually slightly plantar rather
than directly lateral. Lateral fixation can be supplemented with a
longitudinal, cortical, set screw from the talar head into the body (Fig. 34.17A).
plate fixation to preventvarus collapse. However, the medial talar neck
and tibiotalar joint anatomy limits options for plate placement. A
2.0-mm blade plate works well. The blade is placed transversely
across
the distal talar neck from medial to lateral, just posterior to the
medial talar-head articular surface. The plate is directed posteriorly
to sit just plantar to the medial talar-body articular cartilage (see Fig. 34.17B).
Care must be taken to insure that the plate and screw heads sit below
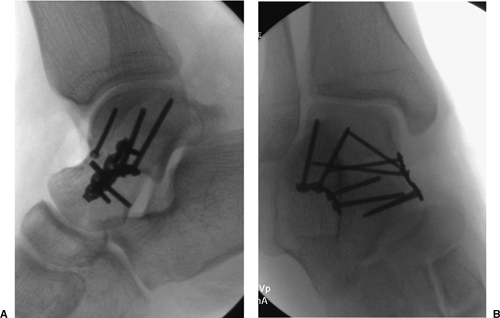
the level of the articular surface. Final x-rays are assessed to
confirm anatomic reduction and to assure that there has not been
intra-articular penetration of screws (Fig. 34.18).
 |
|
Figure 34.15. Typical construct for talar neck fracture without significant medial comminution showing lateral plating and medial set screw.
|
injuries and difficult to treat. The talar body frequently dislocates
posteromedially, hinging on the deltoid ligament. Reduction of the
dislocation should be done on an urgent basis. A closed reduction can
be attempted in the emergency department but is rarely effective. An
irreducible dislocation is best addressed by the dual incision
technique described.
 |
|
Figure 34.16. A. Implants for lateral plating: no. 2.0 plate and 2.4-mm screws. B. Miniblade plate for medial fixation.
|
muscle paralysis is imperative. The knee is flexed to relax and
longitudinal traction is placed through the calcaneus. The femoral
distractor can be a useful reduction aid. One Schantz pin is placed
into the anteromedial face of the tibia, and the other pin is placed
transversely across the calcaneus from medial to lateral. Small
osteochondral fragments are removed from the ankle joint. The tendons
and neurovascular bundle are carefully retracted, and the talar body is
manipulated back into the ankle joint. Usually the only remaining
soft-tissue attachment to the talar body is the deltoid ligament. Care
should be taken that the deltoid ligament not be cut because this
ligament transmits branches of the posterior tibial artery to the talar
body.
 |
|
Figure 34.17. A. Lateral plate fixation. B. Medial plate fixation.
|
should be bone grafted. Autologous cancellous bone is readily available
from the ipsilateral distal tibia or calcaneal tuberosity. Crushed
cancellous allograft is also effective.
 |
|
Figure 34.18. A,B. Final x-rays.
|
approach. A portion of the anterior talar body is accessible through
both the anteromedial and anterolateral incisions. Simple sagittal
fractures can be treated using a single exposure, and the incision
chosen is based on the fracture orientation seen on the CT scan. Joint
distraction using the femoral distractor as described can aid in
exposure of the talar dome.
and coronal plane patterns, as well as associated body and neck
fractures, are best addressed using the dual incision technique. The
anteromedial and anterolateral exposures can allow access to the
anterior one third to one half of the talar body. For fractures that
involve the posterior half of the dome, a medial malleolar osteotomy is
usually necessary. The anteromedial incision is extended proximally
along the mid anteromedial-tibial face. Subperiosteal dissection
exposes the medial malleolus. The deltoid ligament is then left intact.
Fixation for the malleolar osteotomy should then be planned. Transverse
lag screws with an antiglide plate or lag screws directed up the medial
malleolus parallel to the medial joint surface are adequate for
fixation. Prior to the osteotomy, the fixation implants are placed and
then removed so that the screw paths will line up perfectly when the
osteotomy is reduced.
metaphysis. It is inclined obliquely to enter the apex of the medial
ankle joint between the medial malleolus and the tibial plafond (see Fig. 34.8C).
Retractors are placed posterior to the medial malleolus to protect the
tendons and neurovascular bundle. The osteotomy path is outlined by
creation of multiple, small, drill holes. A microsagittal saw is used
to cut through the cancellous bone to the subchondral bone just above
the joint. A thin osteotome is used to complete the osteotomy and
fracture the cartilage. The osteotomy is displaced distally to expose
the medial talar body.
dome visualization. Indirect reduction techniques are utilized for
fracture reduction. Sagittal plane fractures can be fixed using medial
to lateral lag screws. Fragment size dictates the implant diameter.
When placed across articular cartilage, smaller implants are preferable
and include 1.5-, 2.0-, or 2.4-mm, countersunk, cortical, lag screws.
Medial to lateral lag screws can also be placed extra-articularly
through the deltoid fossa on the medial talar body. These screws should
also be countersunk to prevent impingement. As an alternative, headless
subarticular screws can be used (Fig. 34.19). Small osteochondral fragments are stabilized with countersunk, minifragment, cortical, lag screws or bioabsorbable implants (Fig. 34.20). Associated neck fractures are reduced and stabilized as described previously.
solitary fracture or as an associated pattern. The CT scan best details
these fractures. Fragment size, amount of comminution, and degree of
posterior facet involvement dictate treatment strategy. Large solitary
fragments can be approached via the anterolateral exposure. The
anterior talofibular ligament inserts on the lateral process and this
attachment should be preserved. Fixation depends on fragment size. A
2.0-mm plate and lag screw fixation can be used for large solitary
fragments.
splint. Prophylactic antibiotics are administered for 24 hours
following surgery. Once the wound is healed, patients are placed into a
removable boot and begin active range-of-motion exercises of the ankle,
subtalar, and midfoot joints. Patients refrain from weight bearing for
10 to 12 weeks or until the fracture is healed; the radiographic
presence of osteonecrosis is not a contraindication to weight bearing.
Supervised physical therapy is instituted on a case by case basis
depending upon the patient’s ability to comply and progress with a
self-directed home program.
intervals to assess healing and to monitor for signs of osteonecrosis.
A “Hawkins sign,” which is a subchondral radiolucency of the talar
dome, is usually visible between 6 and 8 weeks after the injury. The
presence of a Hawkins sign is a reliable indicator that the talus is
vascularized and osteonecrosis is
not
likely to occur. The absence of a Hawkins sign does not, however,
reliably predict the development of osteonecrosis. The utility of MRI
scanning for monitoring of osteonecrosis is controversial. It is not
practical or cost effective to perform serial MRI scans on a routine
basis. It can occasionally be helpful in determining the extent of
avascularity when subsequent reconstructive surgical procedures are
contemplated. Titanium implants have been suggested to cause less
interference with MRI visualization. CT scanning can be very helpful in
assessing healing when plain x-rays are equivocal.
 |
|
Figure 34.19. A,B. Horizontal-cleavage talar body fracture without comminution. C,D. Final fixation with lag and subarticular screws.
|
 |
|
Figure 34.20. Small bioabsorbable screws may be helpful alternatives to screws for small osteochondral fragments.
|
to excessive skin tension and soft-tissue compromise. Expedient
reduction is necessary to avoid the disastrous complication of
full-thickness tissue loss (see Fig. 34.3).
Delaying operative treatment can be preferable, however, when the
fracture is not significantly displaced and significant swelling could
compromise wound closure and healing. The dual surgical approach for
talar neck and body fractures necessitates careful soft-tissue handling
and proper timing to avoid wound edge necrosis. Superficial wound-edge
necrosis, although infrequent, can occur, and while it usually responds
to local wound care, it delays the initiation of range-of-motion
exercises. Open injuries require immediate and serial irrigation and
debridement followed by the appropriate coverage or closure to avoid
deep infection. Early onset of deep infection necessitates urgent
irrigation and culture-specific, intravenous, antibiotic therapy. Deep
infection can result in septic destruction of all of the peritalar
joints with significant bone loss that can be very difficult to salvage.
rather than a complication of treatment. The incidence of osteonecrosis
following talar neck fractures is related to the initial fracture
displacement and the extent of comminution rather than the timing of
reduction. Focal osteonecrosis without collapse is common following
talar neck and body fractures. It often is asymptomatic and does not
necessarily doom the patient to a poor result. Diffuse or global
osteonecrosis can result in collapse of the talar dome and progressive
posttraumatic arthritis in the ankle and subtalar joints. In the past,
the initial period in which weight bearing was suspended was prolonged
until revascularization, which was believed to protect the talar dome
from collapse, was completed. However, this approach is largely
unproven and impractical. Nonsurgical management of symptomatic
osteonecrosis includes bracing and shoe wear modification. Surgical
salvage typically consists of arthrodesis of the involved joints. As an
alternative in circumstances of complete fragmentation and collapse of
the talar body, a modified Blair fusion with removal of the nonviable
body and fusion of the talar neck and head to the anterior distal
tibia, can help control pain. With this procedure, patients retain more
motion than with a tibial talocalcaneal fusion.
frequent consequences of talar body and neck fractures. This often
occurs with some degree of focal osteonecrosis. It can be the result of
chondral damage at the time of injury or from abnormal joint kinematics
caused by malunion. Stable internal fixation that allows early motion
may minimize peritalar joint stiffness. When conservative measures are
ineffective, arthrodesis of the affected joint(s) is often necessary
for pain relief. Proper imaging studies prior to arthrodesis are often
necessary to detect areas of osteonecrosis, which may help the surgeon
determine the method of fusion or the need for bone grafting.
reported to occur in up to 36% of patients who underwent open reduction
and internal fixation. Shortening of the medial neck of the talus
caused by comminution or impaction can lead to varus malunion. The dual
incision approach facilitates adequate visualization and proper
restoration of talar length and alignment and therefore helps minimize
this complication.
talus is left plantarflexed relative to the neck and the head fragment
remains dorsal to the neck. This often leads to symptomatic impingement
of the dorsal talus on the distal tibia with maximal ankle
dorsiflexion. Even small amounts of residual displacement or
mal-alignment can lead to altered joint mechanics and arthrosis.
Treatment of symptomatic talar malunion can be extremely difficult and
is dependent upon the integrity of the peritalar joints. Long-standing
varus malunion with peritalar joint arthritis typically can only be
salvaged by arthrodesis with realignment to obtain a plantigrade foot.
Varus malunion typically leads to shortening of the medial column of
the foot and needs to be addressed at the time of salvage arthrodesis.
Malunion recognized before the onset of significant arthritis can be
treated by osteotomy with restoration of length, alignment, and
rotation. This may involve structural bone grafting to regain talar
neck length.
