Staying Out of Trouble with Cerebral Palsy
|
|
resulting from damage to the immature brain. The brain problem itself
is nonprogressive. If there does seem to
be progression of the neurologic problems with your cerebral palsy
patient, you should consult neurologists and others to determine the
proper diagnosis; the classic example of CP being mistaken for another
condition is Rett’s syndrome. Cerebral palsy is a disorder of movement,
posture, and intellect, the severity of which varies depending on the
region of the brain affected and the size of the brain injury. Many
children with CP are low birthweight, premature children. Classifying
the type of cerebral palsy—diplegic, quadriplegic, hemiplegic, spastic,
athetoid, etc.—can be difficult on some children, but is helpful
overall. By sorting out and categorizing these children, you can stay
out of trouble by expecting certain problems more frequently in
particular groups.
with CP should be working from a comprehensive history and physical
exam, the orthopaedic surgeon should specifically be attuned to a few
very important pieces of information. From the history and physical,
the orthopaedist should focus on causative factors for the cerebral
palsy, the highest level of the child’s function (e.g., head control,
sitter, ambulator, etc.), gait evaluation, joint range of motion, and
presence or absence of spinal deformity.
several pitfalls to avoid. Hip abduction should be tested with the hips
and knees extended. Patience is essential. If the exam is done hastily,
the child’s muscles will tense up and you will probably be testing
spasticity more than you are testing the actual joint range of motion.
When testing popliteal angles, the opposite hip must remain fully
extended. It is a rookie error to allow the opposite hip to flex, which
relaxes the hamstrings and leads to underestimation of the popliteal
angle. Test ankle dorsiflexion with the knee flexed and extended, and
be sure that the hindfoot is inverted, so that a flexible midfoot does
not fool you into underestimating the extent of the equinus
contracture. For quadriplegic children with severe CP, get them in the
sitting position to examine the spine.
be overwhelming to the less experienced. Start by watching the foot,
then the ankle, then the knee, then the hip, then the trunk. By taking
a stepwise observation strategy with each walk down the hall, you can
get a better sense of the problems. Watch the child walk with and
without braces, so you can assess the value of the brace for that
particular child. Look at the shoes of a walking child to assess
whether the toes are wearing out. This can be an excellent indicator of
rectus spasticity: the child will wear out the toes because of the
inability to clear the foot due to rectus spasticity.
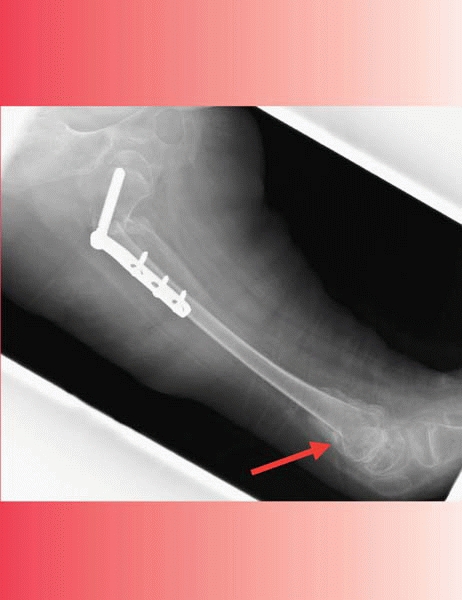
pelvis radiograph of the hips at about 2 to 3 years of age. If the
radiograph looks normal at this age, it is important not to be lulled
into a false sense of security, especially in the child with very high
tone and total involvement. Remember that a hip radiograph can look
relatively normal in a child less than 3 years of age, but the spastic
hip disease can progress relentlessly to complete dislocation a few
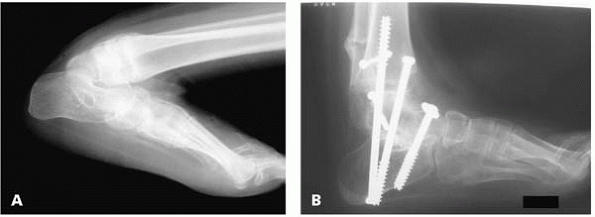
years later (Fig. 14-1).
establish the diagnosis of CP. Many neurologists are using an MRI of
the brain, looking for certain characteristic defects. Parents will
sometimes ask the orthopaedist to order the brain MRI or
to
review it with them. Depending on your comfort level, you may want to
work together with the neurologist. The pronouncement of CP can carry
such profound implications that, as the orthopaedic surgeon, you want
to be very careful about which child you label with that diagnosis.
Explain to the parents that although CP is not a progressive neurologic
problem, the musculoskeletal function can certainly worsen with time.
For example, with increased body weight but no increase in strength,
ambulation may deteriorate with a growth spurt and contractures may
worsen.
 |
|
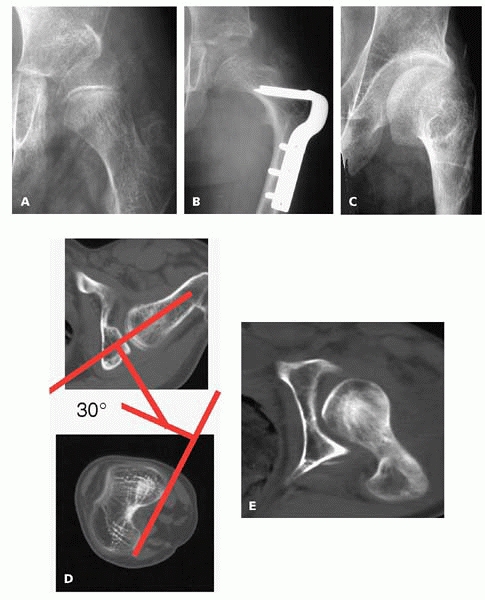
▪ FIGURE 14-1
Many children with developmental dysplasia of the hips are in the worst shape at birth, then stabilize with time and treatment. We can get used to discharging the DDH toddler from observation. Spastic hip disease is very different: don’t be lulled into a false sense of security by hips that look good at 21 months (A) or even at 5 years (B). By 8 years of age (C), the right hip was more that 60% subluxated, and a hip reconstruction was performed. |
-
Familial spasticity
-
Congenital ataxia
-
Brain or spinal cord tumors or infections
-
Metabolic or chromosomal abnormalities with spasticity
-
Rett’s syndrome
orthopaedists, one of the best ways to stay out of trouble is to work
with several other healthcare professionals interested in these
children. If your institution has such specialists (physiatrists,
pediatric neurologists, pediatric neurosurgeons, and occupational,
physical and speech therapists) it is best to combine your assessments
to prioritize a child’s needs. This allows the orthopaedic surgeon to
choose the operative interventions that will yield the most benefit
with the least downside for the child.
a few important things to consider to stay out of trouble. Avoid
multiple lower extremity procedures if the child is in a phase of motor
development in which rapid functional progress is being made. Be sure
to question parents and physical therapists carefully about this issue.
The classic case is a 3- or 4-year-old who is just starting to walk and
making great advances over the previous six months or year. You may
find that the child’s hamstrings or heel cords are tight and be
considering surgery. It is much better to wait until the child reaches
a plateau and is hampered by contractures and spasticity. Also, warn
families about the impact of multiple surgeries on a teenager with CP.
These older bigger children are slower to heal, and have a much less
favorable strength-to-weight ratio. Full recovery and rehabilitation
after a femoral osteotomy may take over a year, and is hastened by
involvement of a qualified therapist.1 You’ll do everyone a favor by being up front with this before the surgery.
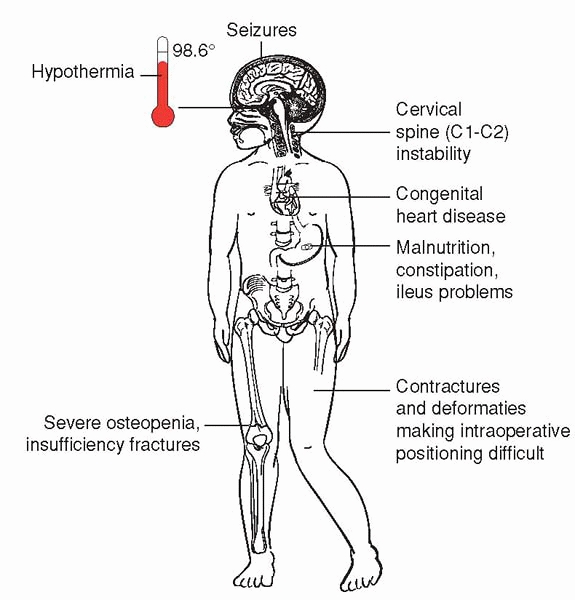
because the children with the most conditions tend to need the most
surgery. It is easy for the orthopaedic surgeon to overlook seizures,
congenital heart disease, malnutrition, shunts, hypothermia, and other
issues that could tremendously complicate the perioperative period and
recovery.
Insist on up-to-date medical summaries from the child’s pediatrician
and other specialists before heading into a big orthopaedic operation.
To stay out of trouble, don’t forget that children with CP can get
anaphylaxis from a latex allergy. We all think about this problem in
spina bifida, but it has been well described in the CP population as
well. An unusual but very severe problem after surgery can be a severe
dystonic reaction. This can occur after any surgery or casting in a
child with CP, and may manifest itself as uncontrollable total body
muscular contractions that can actually lead to myoglobinemia, and even
death. The treatment is anti-spasticity medicine, or even acute
sedation or anesthesia.
 |
|
▪ FIGURE 14-2 The many medical sources of trouble when operating on the child with CP.
|
when considering surgical intervention in children with CP. Multiple
muscle release surgeries should rarely be done in children who are less
than 3 years of age. In this population, the risk of rapid recurrence
of muscle contracture with growth is unacceptably high.2
Most experienced orthopaedists would plan such surgery for around age
5, although children need to be treated as individuals. Be especially
careful of doing procedures such as tendon transfers on children with
pure athetosis, in whom the results are very unpredictable. Mercer Rang
taught us that one of the keys to staying out of trouble caring for
children with CP is to avoid the “birthday syndrome,” in which a
different muscle group is released each year, leading to extensive
multiple surgeries. Today, most orthopaedic surgeons know to do
multiple muscle lengthenings at the same operative intervention.
Aggressive attack on the adductors that ablates the obturator nerve can
lead to hyperabduction of the hips. This may not manifest itself for
several months or even a few years, when an abductor contracture
creates seating difficulties. Overly aggressive hamstring lengthening,
especially in bigger older children with severe contractures, can lead
to sciatic nerve injury. A recent study showed a marked decrease in
sciatic nerve EMG—up to 86%—with progressive knee extension while the
hip is flexed. The EMG returned to normal as the hip was extended.3 The classic scenario is a 13- or
14-year-old that presents with popliteal angles of 90°. The surgeon
releases both medial and lateral hamstrings and gives everything a
really good stretch in the operating room, getting the knee nearly
straight. As an extra measure of insurance, the surgeon adds long leg
casts to keep the legs straight in the postoperative period. The child
then awakes with burning dysesthesia in both lower extremities, or
worse: loss of motor function or sensation. Should this occur, the best
treatment is to get casts off immediately and allow the knees to flex.
Some neurologists and physiatrists will prescribe Neurontin to help
with neurogenic lower extremity pain. The most common source of trouble
from overly aggressive muscle lengthenings occurs at the tendoachilles.
Many surgeons were trained to do percutaneous tenotomies in very young
children with CP. If such children grow up to be walkers, the heel cord
becomes incompetent and the teen is likely to develop hyperdorsiflexion
with minimal plantar flexion strength. They will go into a progressive
crouch as they get older and heavier. To stay out of trouble, it is
better to leave a competent gastrocnemius unit. Although the recurrence
rate is higher with a gastrocnemius fascial lengthening, it is much
easier for the child to walk with some recurrent equinus than it is to
watch helplessly as a large teen gives up walking because of severe
crouched gait exacerbated by an incompetent Achilles tendon
overlengthened in early childhood.
with CP, and can be avoided in many cases. Although short leg casts
work well after gastrocnemius fascial lengthenings, the surgeon should
exercise great care in cast application. The heel should be well
padded. The upper posterior edge of the short leg cast should be padded
enough so it doesn’t cut into the popliteal fossa. The footplate on the
cast should come out beyond the toes; if it does not, the children will
curl their toes over and may get blisters or skin irritation as they
walk. Casting above the knee risks distal femoral insufficiency
fractures. This usually occurs after the cast is removed and a well
meaning, but overly aggressive physical therapist attempts to regain
knee range of motion. (Even knee immobilizers can cause problems. Some
brands of knee immobilizer have metal struts that can cause skin
irritation and ulceration on the back of the calves. To keep children
with CP comfortable after surgery, diazepam should be used liberally to
help with the muscle spasms. Narcotics may be helpful at first, but are
not as valuable as the antispasticity medicines.
in caring for children with CP is the management of spastic hip
disease. The highest risk period for progressive spastic hip
subluxation seems to be between 3 to 8 years of age. Generally, there
is a low risk of hip subluxation in the CP child who is walking by 3
years of age. Be alert, however, for the atypical presentation of a
progressively unstable hip in an ambulatory spastic diplegic patient
that may indicate the presence of previously unrecognized raised
intraventricular pressure.4 The
diagnosis of spastic hip subluxation or dislocation can be very
difficult by physical examination alone. Asymmetric spasticity of the
lower extremity muscles can create apparent limb length inequalities.
The ability to feel instability in bigger older children is quite
limited. For this reason, even most experienced neuromuscular pediatric
orthopaedists rely on radiographic imaging to assess the status of the
hips in children with CP. It is not unusual for the parent of a
school-age child with cerebral palsy to present complaining that the
child has hip pain. To stay out of trouble, understand that there are
many different things that cause pain besides the hip joint itself.
Even with a radiograph that shows some hip subluxation, be
certain
that there is not an abdominal source for the pain. Reflux,
constipation, hernias and other conditions can mimic the pain of
spastic hip disease. Also, the spastic muscles alone may be the real
source of pain in a younger child. It is very unlikely to have actual
joint pain in a younger child, even with severe subluxation. Complaints
of pain or abnormal radiographs in children less than 4 years of age
may be better managed with initial soft-tissue releases rather than
bony reconstruction. A recent article5 showed a much higher rate of failure if hip reconstruction is done in children less than 4 years of age.
Low bone density, unfavorable biomechanics, persistently increased
tone, and associated medical problems can all combine to make the
postoperative period difficult. Be certain that the family knows the
goals and true risks of the surgery.
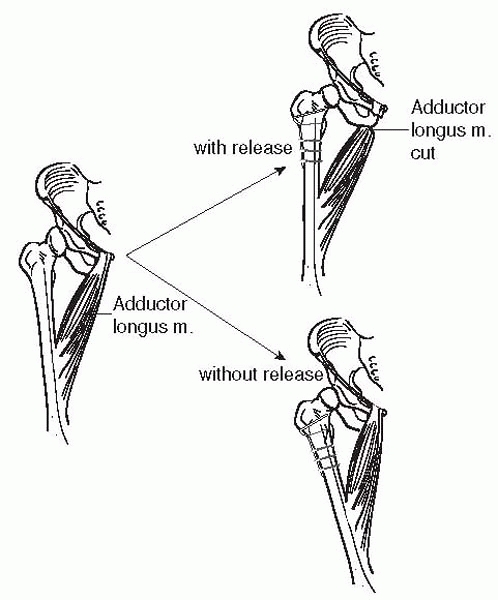
of trouble in CP hip surgery. It is essential to do a satisfactory
adductor lengthening prior to performing a varus derotational osteotomy
(VDRO). Otherwise, you will instead create adduction (Fig. 14-3).
Warn the families in advance about a leg length discrepancy. This is
especially visible in children who spend most of their time sitting. A
leg length discrepancy will obviously occur after a one-sided hip
reconstruction, but can even be present after both sides are
reconstructed. This is typically noted first by the physical therapist,
and can be a great source of concern to the parents if they are not
forewarned. Several liability claims have resulted from limb length
inequality after hip reconstruction. Indications for a capsulotomy are
controversial. A study from San Diego7
showed that a capsulotomy of the hip is valuable if the hip is more
than 70% subluxated. Otherwise, there is a high risk of failure of the
hip reconstruction.
disease is the iliopsoas. This strong spastic flexion muscle tends to
pull the hip proximally. Complete iliopsoas release in nonambulators is
an essential factor for success in the surgical
management
of spastic hip disease. This can be done either by a tenotomy, or by
resecting the entire lesser trochanter. To stay out of trouble,
recognize the reported problems of doing unilateral surgery in children
with windswept hips. Some investigators believe that fixing only the
adducted hip will lead to failure.9
They theorize that by fixing the abducted hip you will protect the
adducted hip from adducting further. Do not overdo the derotation! Most
hips in children with CP dislocate in the superior or posterior
direction.10 Most children with CP
have an excessive amount of femoral anteversion. If you overcorrect the
anteversion, you can put the hip in retroversion and it will dislocate
out the back (Fig. 14-4). The posterior
acetabulum is an impossible place to increase the femoral head coverage
with an acetabular osteotomy, so don’t put the femoral head back there
where it can’t be protected. In children with low bone density, it is
safer to delay weight bearing or aggressive range of motion after the
hip reconstruction. The fixation can cut out easily (Fig. 14-5).
As mentioned previously, casts in children with CP cause lots of
problems. They are frequently used by some surgeons after hip
reconstructions hoping to lessen the pain for the first few
postoperative days. However, children maintained for a few weeks in a
spica cast after hip surgery are
a set up for skin pressure ulcers and distal femoral insufficiency fractures (Fig. 14-6).
The classic time for these fractures is a couple of weeks after the
casts come off when the physical therapy is aggressively trying to
regain knee motion. Periodic radiographs are recommended for several
years after a proximal femoral osteotomy. Resubluxation is possible,
especially in younger children. Avascular necrosis (AVN) has been
reported, particularly if both a femoral and pelvic osteotomy are
performed (perhaps indicating a more severely displaced hip?).11
 |
|
▪ FIGURE 14-3 Persistent adduction made worse with VDRO.
|
 |
|
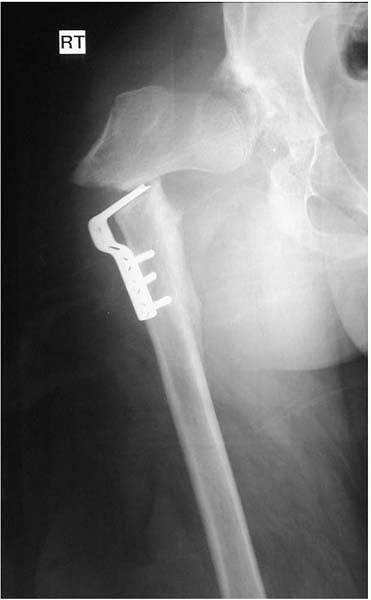
▪ FIGURE 14-4 Too much “DR” in a “VDRO?” Partial hip subluxation (A) was treated with a VDRO (B) and Dega pelvic osteotomy. (C)
Five years after healing and hardware removal, this AP radiograph shows a rotational abnormality that is difficult to interpret, and the hip has a severe fixed internal rotation contracture. (D) A CT scan shows 30 degrees of anteversion. Since this was felt to reflect primarily soft-tissue contracture, he had a lengthening for the adductor, gluteus minimus and medius, fascia lata, and anterior hip capsule. If there would have been any femoral retroversion, this would have had to be combined with a femoral derotation. (E) This followup CT scan obtained one year after the releases demonstrates a much improved relationship of the femoral head to the acetabulum. On examination, external rotation has been restored. (Courtesy of F. Miller, MD.) |
 |
|
▪ FIGURE 14-5
Intertrochanteric fracture following blade plate fixation as part of a hip reconstruction. Low bone density, spasticity and aggressive postoperative therapy combine to increase fracture risk. Technique was an additional factor in this case: the blade plate was quite low in the neck. |
with CP is salvage procedures of the hip. There are few that give the
children, parents, and surgeon much satisfaction. If confronted with a
skeletally immature child who is a
candidate for salvage procedure, think carefully before offering a
Castle procedure, Girdlestone, or proximal femoral resection. Several
surgeons have had experience with spectacular proximal migration of the
residual femoral shaft in the skeletally immature. In these salvage
procedures, warn the families that pain relief after proximal femoral
resection may take a long time—perhaps a year or more. Recent evidence
suggests that femoral head resection and valgus osteotomy may be a
better option than the Castle procedure.12
Heterotopic ossification is also very common. Radiation therapy can
help with this. Significant debilitating heterotopic ossification is
rare (Fig. 14-7) but some heterotopic ossification on the radiograph is almost inevitable.
 |
|
▪ FIGURE 14-6 A classic distal femoral insufficiency fracture with classic circumstances (arrow).
After hip reconstruction, the surgeon placed the child in a spica cast for a few weeks. Immobilization made the low bone density even worse. Of course, when cast came off, she was stiffer than ever, so she went to PT, where they enthusiastically went to work hard on her limited knee motion. Crack. Pain. Now what—more casting? |
up only about 5% of hip subluxations and dislocations in children with
CP, they can be more difficult to diagnose.13
To stay out of trouble, understand that the radiographs in children
with an anterior hip dislocation can look perfectly normal (Fig. 14-8).
These children do not usually have the classic hip flexion adduction
posture. Instead, they are usually in the figure-of-4 position with
their hip extended, abducted and
externally
rotated. If you feel a prominence in the groin and see this figure-of-4
position and are suspicious for an anterior dislocation, a CT scan of
the pelvis can be very helpful. Remember, in these children the hip is
out the front and the anterior acetabulum may be deficient. A Pemberton
or a Dega osteotomy that focuses on the front of the acetabulum is good
in this population.
 |
|
▪ FIGURE 14-7
Most heterotopic ossification after CP hip reconstruction is mild and causes no dysfunction; this case is the exception. The surgeon ignored standard recommendations of VDRO/periacetabular osteotomy, in favor of some sort of shelf procedure. Aggressive bone grafting and immobilization led to bone formation so exuberant that the child essentially has a single fused hip—in extension. Imagine how hard sitting is now. (Courtesy of F. Miller, MD.) |
 |
|
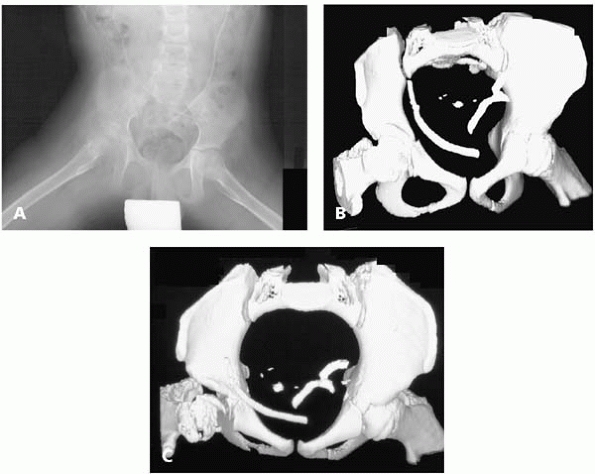
▪ FIGURE 14-8 This AP radiograph (A)
is difficult to interpret—the hips actually look fairly well reduced. The surgeon was suspicious, however, because the child preferred an abducted, extended hip position, and the parents could feel “clunking” with diapering, and sometimes noticed a lump in the groin. The surgeon obtained a CT (B,C), showing anterior hip subluxation. |
children with CP. These curves are not well managed with bracing, and
tend to progress even after skeletal maturity. The risk factors for
progression of scoliosis in spastic CP are: having a spinal curve of 40
degrees before age 15 years; having total body involvement; being
bedridden; and having a thoracolumbar curve.14
Perhaps the most important way to stay out of trouble in managing
severe neuromuscular scoliosis is to work closely with family members
to help them understand the effects of this condition on their child’s
function and health, and the risks and benefits of surgical management.15
Nationwide, the complication rate from managing neuromuscular scoliosis
in children with severe CP runs about 25%. There are few procedures
that we do in orthopaedics that carry such a high complication rate. Be
certain that the family accepts this high risk of complications, which
may even include death. They must understand that the primary goal of
spinal fusion for the typical thoracolumbar curve with pelvic obliquity
is to maintain the ability to sit comfortably. Surgery is primarily for
quality of life, not quantity
of life. Despite the surgical complexity and expected complications,
the overall good surgical results and high patient and caregiver
satisfaction confirm that corrective spinal surgery is beneficial for
most patients with total-body involvement CP and scoliosis.16
preoperative evaluation that focuses on underlying medical problems and
the overall health of the child.17
Don’t forget the shunt! Correction of a huge spinal deformity in a
child with a functioning shunt can lead to shunt disconnection,
postoperative hydrocephalus and possible death. There are several
reported cases of this postoperative complication. Prepare for a high
blood loss, especially if the child has been on Depakote. Use of
aprotinin has been helpful.18
Although there are conflicting studies, there is recent evidence that
staging the anterior and posterior procedures is safer and more
effective in some centers.19 To stay
out of trouble, fixation should go from the upper thoracic spine to the
pelvis. In almost every case of neuromuscular scoliosis, pelvic
obliquity is an important part of the deformity. Maximize the number of
spinal fixation points. In most cases, a sublaminar wire technique at
each level has been very effective. It is helpful to put a double wire
around the top level and around L5 as extra protection against pullout
or wire breakage. Some recommend leaving the interspinous ligament
intact at the top of the construct to prevent hyperkyphosis above. Some
surgeons believe that there is an advantage to using hooks or screws at
the top of the construct to help prevent hyperkyphosis. There has also
been the general caveat to avoid hip surgery and spine surgery during
the same operative intervention. There have been reports of heterotopic
ossification when these two procedures are done at the same time. It is
important to carefully assess the flexibility of the spine. Although
many of these curves are large and it is tempting to do an anterior
release, in many cases a very satisfactory, well-corrected,
well-balanced spine can be obtained by surgery from posterior fusion
alone. The goals of arresting progression and obtain good sitting
balance can usually be achieved with a posterior spine fusion, even
when the primary curve is 70° or more. Be alert to the fact that
children with severe hyperlordosis
(Fig. 14-9) of the lumbar spine create particular challenges. Dorsal rhizotomy may be a risk factor.20
Anterior kyphosing instrumentation may be helpful in the most severe
cases. In less severe cases, the Luque rod or the unit rod may need to
be inserted in segments due to the severe lordosis. For very thin
children, the first step may be a G-tube if the nutrition is poor.
 |
|
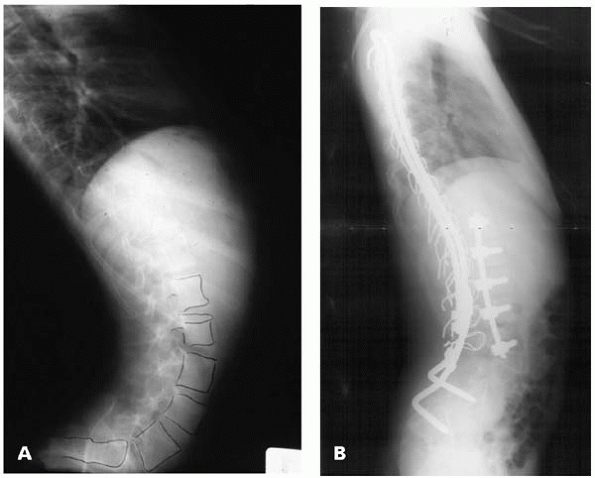
▪ FIGURE 14-9
Severe hyperlordosis of the lumbar spine is a very difficult deformity to treat. Sometimes, an anterior release with instrumentation can be used to purposely create kyphosis. Then a posterior spinal fusion with standard unit rod or Galveston instrumentation can be used (although the rods often need to be cut and inserted in sections when there is this much lordosis). |
management of neuromuscular scoliosis, although it is less common in
children with CP than in those with spina bifida.21 Be certain the parents and caregivers are aware of the high risk: most studies document a risk between 5-10%.22
CP is equinus. As previously discussed, the most common source of
trouble is overlengthening of the heel cord (Fig. 14-10).
A little bit of equinus is much better than any calcaneus, especially
in older children. An equinovarus foot is often managed quite
successfully with a split posterior tibial tendon transfer. The results
of split posterior tibial tendon transfer in children with hemiplegia
are outstanding—and make for happy children, happy families, and happy
surgeons. To stay out of trouble, study the deformity carefully. Look
for those children who have forefoot supination. Their problem is with
the anterior tibialis tendon; they would benefit from a split transfer
of the anterior tibialis tendon to the cuboid. There are a few other
caveats in this often successful operation. Beware of doing any tendon
transfers in very
young
children. Transferring a part of the posterior tibial tendon in a 3- or
4-year-old may be disappointing: the tiny bit of tissue you are
transferring may not lead to the desired correction. More concerning,
the child may develop the opposite deformity (hind foot valgus) in
later years. Therefore, most experts in CP recommend waiting until at
least the school years before doing a split posterior tendon transfer.
Finally, in older children, be certain that the hind foot has
sufficient flexibility. If the equinovarus deformity has been present
for many years, and the hind foot does not correct to at least neutral,
transferring part of the tendon will not give you very satisfying
correction. When the hind foot is rigidly in varus, a lateral closing
wedge osteotomy in the calcaneus is an important addition to the
soft-tissue surgery.
 |
|
▪ FIGURE 14-10 Overlengthening of the tendo Achilles when this child was young led to severe calcaneus deformity (A) when he was a teenager. This was treated with a fusion (B). (Courtesy of F. Miller, MD.)
|
in children with CP. Ambulatory teenagers with severe pes planovalgus
often develop a severe hallux valgus that crosses under the second toe.
Of their many orthopaedic problems, the bunion in these children is on
the list, but often low on the list. The standard textbook
recommendations have been to do a metatarsal phalangeal fusion in the
children with more severe neurologic involvement. Standard
reconstructions may be advisable in less involved children.
trouble with bunion surgery in children with CP is very careful patient
selection. The main goal should be pain management and shoe fitting,
not cosmetics. These children often need multiple procedures and the
last thing they need is an infection, hardware problem, or nonunion of
a bunion operation done primarily to make the feet look better.
-
Patience during
physical examination is crucial. If the exam is done hastily, the
child’s muscles will tense and you will probably be testing spasticity
more than you are testing the actual joint range of motion. -
As the orthopaedic surgeon, get input from your neurology and physiatry colleagues before you label with the child as having CP.
-
Avoid multiple lower
extremity procedures if the child is in a phase of motor development in
which rapid functional progress is being made. -
Warn families about
the impact of multiple surgeries on a teenager with cerebral palsy. The
full recovery and rehabilitation after a femoral osteotomy may take
over a year, and is hastened by involvement of a qualified therapist. -
Consider evaluation by the child’s pediatrician and other specialists before heading into a big orthopaedic operation.
-
Don’t forget that cerebral palsy children can get anaphylaxis from a latex allergy.
-
Multiple muscle
release surgeries should rarely be done in children who are less than 3
years of age. In this population, the risk of rapid recurrence of
muscle contracture with growth is unacceptably high. -
Be especially
careful of doing procedures such as tendon transfers on children with
pure athetosis. The results on this population are very unpredictable. -
Overaggressive adductor lengthening that includes the obturator nerve can lead to hyperabduction of the hips.
-
Over aggressive
hamstring lengthening, especially in bigger older children with severe
contractures, can lead to sciatic nerve injury. -
Casting above the knee risks distal femoral insufficiency fractures.
-
Generally, there is
a low risk of hip subluxation in the CP child who is walking by 3 years
of age. Be alert, however, for the atypical presentation of a
progressively unstable hip in an ambulatory spastic diplegic patient
that may indicate the presence of previously unrecognized raised
intraventricular pressure. -
Don’t rely on physical examination alone to follow hip subluxation.
-
Delay hip
reconstruction in the very young, if possible: there is a much higher
rate of failure if hip reconstruction is done in children less than 4
years of age. -
Do a satisfactory adductor lengthening prior to performing a VDRO. Otherwise, you will be really creating adduction.
-
Complete iliopsoas
release in nonambulators is an essential factor for success in the
surgical management of spastic hip disease. -
Do not overdo the derotation—the hip will come out the back.
-
Be alert: the radiographs in children with an anterior hip dislocation can look perfectly normal.
-
Work closely with
family members to help them understand the effects of this condition on
their child’s function and health, and the risks and benefits of
surgical management. Be certain that the family accepts this high risk
of complications, which may even include death. -
Perform a comprehensive preoperative evaluation that focuses on underlying medical problems and the overall health of the child.
-
Don’t forget the
shunt! Correction of a huge spinal deformity in a child with a
functioning shunt can lead to shunt disconnection, postoperative
hydrocephalus and possible death. -
For very thin children, the first step may be a G-tube if the nutrition is poor.
-
In the management of
equinus, the most common source of trouble is overlengthening of the
heel cord. A little bit of equinus is much better than any calcaneus,
especially in older children. -
Beware of doing any tendon transfers in very young children.
-
In the management of
equinovarus deformity in older children, be certain that the hind foot
has sufficient flexibility. If the equinovarus deformity has been
present for many years, and the hind foot does not correct to at least
neutral, transferring part of the tendon will not give you a very
satisfying correction.
R, Baumann JU. Long-term effects of intertrochanteric varus-derotation
osteotomy on femur and acetabulum in spastic cerebral palsy: an 11- to
18-year follow-up study. J Pediatr Orthop. 1997;17(5):585-591.
NP, Mubarak SJ, Wenger DR. One-stage correction of the dysplastic hip
in cerebral palsy with the San Diego acetabuloplasty: results and
complications in 104 hips. J Pediatr Orthop. 2000;20(1):93-103.
F, Giradi H, Lipton G, et al. Reconstruction of the dysplastic spastic
hip with peri-ilial pelvic and femoral osteotomy followed by immediate
mobilization. J Pediatr Orthop. 1997;17(5): 592-602.
HT, Wenger DR. Location of acetabular deficiency and associated hip
dislocation in neuromuscular hip dysplasia: three-dimensional computed
tomographic analysis. J Pediatr Orthop. 1997;17(2):143-151.
AI, Chhor K, Launay F, et al. Femoral head resection for painful hip
subluxation in cerebral palsy: Is valgus osteotomy in conjunction with
femoral head resection preferable to proximal femoral head resection
and traction? J Pediatr Orthop. 2005;25(1):70-73.
AI, Chang WN, Dabney KW, et al. Comparison of parents’ and caregivers’
satisfaction after spinal fusion in children with cerebral palsy. J Pediatr Orthop. 2004;24(1):54-58.
CP, Leach J, Wenger DR. Scoliosis in total-body-involvement cerebral
palsy. Analysis of surgical treatment and patient and caregiver
satisfaction. Spine. 1998;23(12):1412-1424; discussion 1424-1425.
AI, Chang WN, Dabney KW, et al. Comparison of one-stage versus
two-stage anteroposterior spinal fusion in pediatric patients with
cerebral palsy and neuromuscular scoliosis. Spine. 2003;28(12):1300-1305.
PD, LaPorte DM, Hungerford MW, et al. Deep wound infections after
neuromuscular scoliosis surgery: a multicenter study of risk factors
and treatment outcomes. Spine. 2000;25(19):2461-2466.