Hammer Toe Correction
They can be painful when the toe box of a shoe presses on the prominent
area of the deformity, usually the flexed portion of the proximal
interphalangeal joint. The deformity can be flexible or rigid and
usually results from an imbalance between the extrinsic and intrinsic
muscles of the foot. Often, the discomfort can be treated by shoe
modifications; however, with a persistently painful hammer toe, surgery
is indicated.
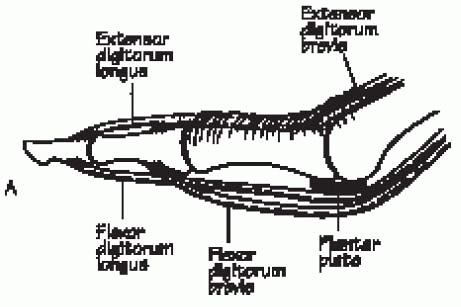
stabilizers of the toe. The passive stabilizers consist of the
collateral ligaments, the plantar aponeurosis, the volar plate, and the
capsule. The active stabilizers include the extrinsic and intrinsic
muscles of the foot. Extrinsically, the flexor digitorum longus (FDL)
inserts plantarly on the distal phalanx. The extensor digitorum longus
(EDL) inserts dorsally on the extensor hood at the level of the
proximal phalanx and then continues further to insert into the distal
phalanx. The intrinsic muscles act to support and balance the extrinsic
muscles. The extensor digitorum brevis (EDB) inserts onto the middle
phalanx, and the lumbricals and interossei tendons course plantar to
the center of rotation of the metatarsophalangeal (MTP) joint and
insert into the extensor hood. The lumbricals work to plantarflex the
MTP joint and extend the interphalangeal joints. There are no tendinous
insertions onto the proximal phalanx (Fig. 35-1).
 |
|
FIGURE 35-1. Normal position of the bones, joints, and extrinsic tendons of a functional lesser toe. (From Hansen ST. Functional reconstruction of the foot and ankle. Philadelphia: Lippincott Williams & Wilkins, 2000, with permission.)
|
the intrinsic and extrinsic muscles of the foot. The pull of the EDL
and the antagonistic pull of the weaker intrinsic muscles determine the
position of the proximal phalanx at the MTP joint. The pull of the long
and short flexors determines the position of the middle and distal
phalanges. The toe deformity is the result of an imbalance between the
strong extrinsic muscles and the weaker intrinsic muscles.
inflammatory arthritis or with neuromuscular diseases. However, they
are most commonly a result of poorly fitting shoes and are more common
in women. Shoes with a narrow, pointed toe box force the proximal
phalanx into extension and the proximal interphalangeal (PIP) joint
into flexion. This is exacerbated by a high heel, which allows the toes
to slide forward into the narrow toe box (Fig. 35-2).
The second toe is most commonly affected because it is often the
longest ray and therefore most affected by pressure from the toe box of
the shoe.
 |
|
FIGURE 35-2.
Poor fitting shoe with (1) a narrow toe box, which forces proximal phalanx into extension and proximal interphalangeal joint into flexion, and (2) an excessively high heel, which allows the toes to slide forward into the narrow toe box. |
 |
|
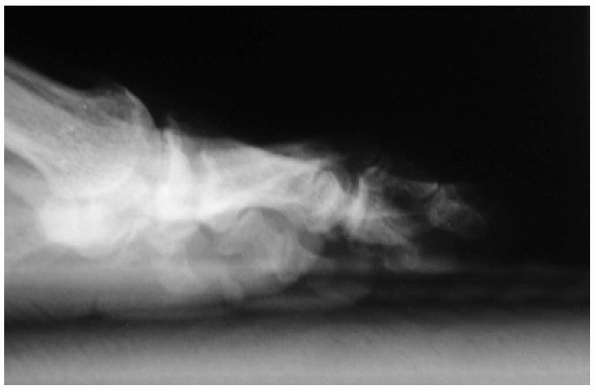
FIGURE 35-3. Weight-bearing lateral radiograph of a moderate hammer toe.
|
plantar plate and the collateral ligaments of the MTP joint. Over time,
these stabilizers become stretched, and a deformity gradually develops.
As the hammer toe becomes more rigid, the toe strikes the top of the
shoe at the PIP joint, and the proximal phalanx forces the metatarsal
head plantarly. Eventually, the volar plate at the MTP joint stiffens,
the proximal phalanx subluxates dorsally, and the plantar fat pad
migrates distally. This deformity exposes the metatarsal heads
plantarly, and metatarsalgia occurs. Usually, these deformities are
painful at the dorsal aspect of the PIP joint, where a callous is often
present. A painful callus sometimes forms at the metatarsal head
plantarly.
moderate, and severe forms. A mild deformity is flexible without a
fixed contracture at the MTP or PIP joints. It is often caused by a
contracture of the FDL. The deformity occurs with ankle dorsiflexion or
with weight bearing but is absent when the patient is not bearing
weight and the foot is in equinus. A moderate deformity has a fixed
flexion contracture at the PIP joint but without an extension
contracture at the MTP joint. (Fig. 35-3). A severe deformity has a fixed flexion contracture at the PIP joint, with a fixed extension contracture at the MTP joint (Fig. 35-4).
In addition to dorsal pain at the PIP joint, patients may also complain
of pain plantarly, near the corresponding metatarsal head.
wear and pain not responsive to standard conservative care.
Conservative care includes properly fitting shoes, splinting devices,
and doughnut cushions.
the severity of deformity (i.e., flexible or fixed). Preoperative
radiographs (anteroposterior and lateral weight-bearing views of the
foot) are valuable to determine the amount of contracture at the PIP
and MTP joints and to rule out other pathology (Fig. 35-4).
-
Esmarch tourniquet, cast padding
-
Bone cutter
-
Kirschner wires (K-wires), 0.045 and 0.062 inches
-
K-wire driver
-
Telfa bolsters
-
Postoperative shoe
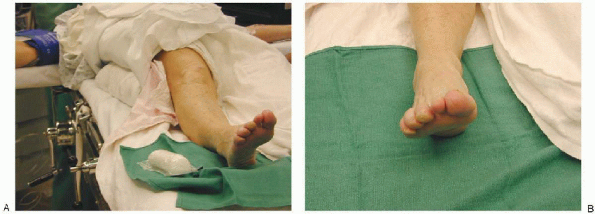
Surgery can be performed with use of an ankle block. A full roll of
cast padding is wrapped above the malleolus. A bloodless field is
obtained by exsanguinating the foot with an Esmarch and then tightly
wrapping the Esmarch three times above the malleolus on the cast
padding. This allows the Esmarch bandage to act as a tourniquet.
extensor tendon transfer (i.e., Girdlestone-Taylor procedure). The FDL
is transferred to the extensor hood, where it assumes the role of an
intrinsic (i.e., plantar flexion at the MTP joint and extension of the
PIP and DIP joints), thereby eliminating the deformity. Expectations for the surgery must be discussed with the patient preoperatively. A
flexor-to-extensor transfer eliminates a hammer toe deformity, but active flexion of the toe is lost.
 |
|
FIGURE 35-4.
Weight-bearing lateral radiograph of a severe hammer toe demonstrates flexion of the proximal interphalangeal and metatarsophalangeal joints of the second toe. |
 |
|
FIGURE 35-5. The patient is supine with a bump under the ipsilateral hip (A) to place the foot in a neutral position (B).
|
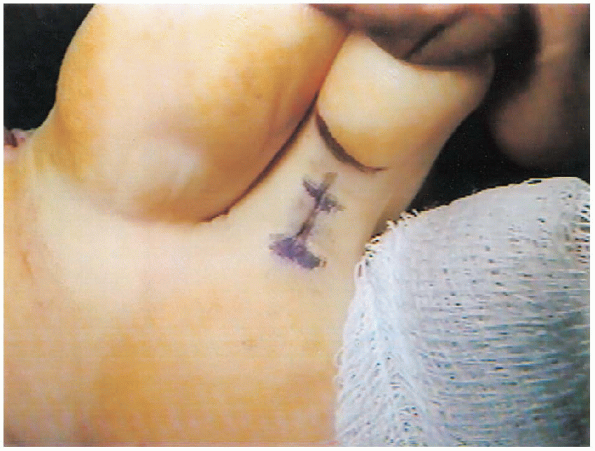
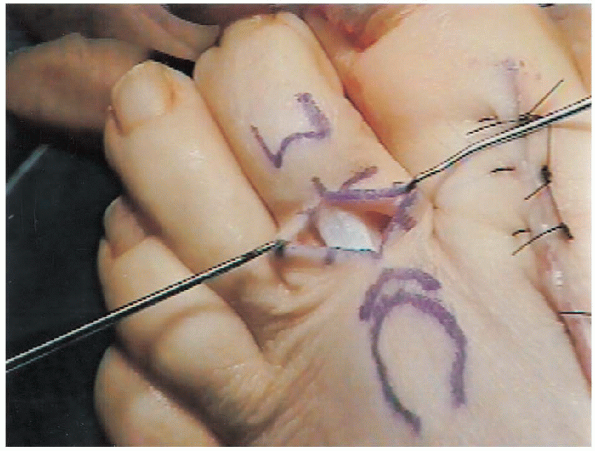
flexor-to-extensor tendon transfer. A 1.5-cm longitudinal incision is
made on the plantar surface of the toe at the level of the proximal
flexion crease to harvest the FDL (Fig. 35-6).
A plantar transverse stab incision is made at the distal phalanx crease
to release the insertion of the FDL from the distal phalanx. A third
longitudinal incision is made on the dorsal aspect of the toe over the
middle phalanx to affix the FDL to the extensor hood (Fig. 35-7).
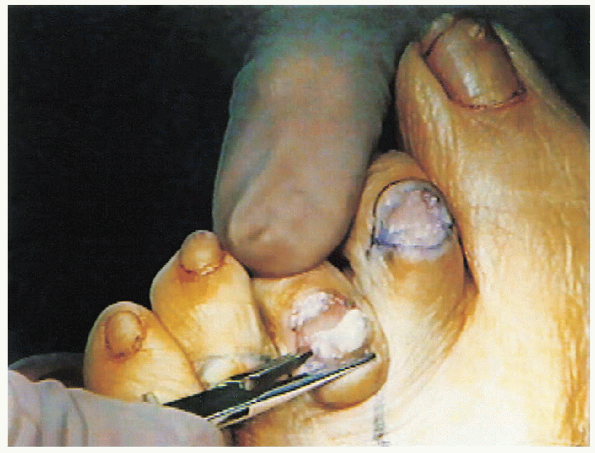
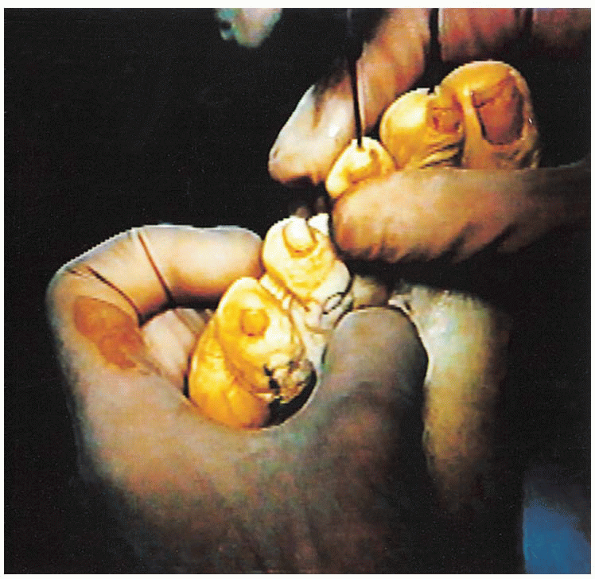
the FDL is harvested through the longitudinal plantar incision.
Dissection is carried to the level of the flexor sheath, which is split
in line with the incision. The FDL is identified as the middle of the
three flexor tendons (Fig. 35-8) and held outside the skin using a hemostat.
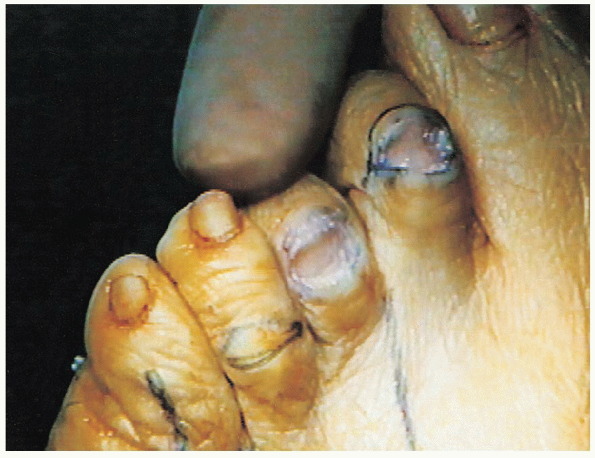
 It is released from its insertion on the plantar aspect of the distal phalanx using the small plantar stab incision (Fig. 35-9).
It is released from its insertion on the plantar aspect of the distal phalanx using the small plantar stab incision (Fig. 35-9). 
The FDL is then delivered into the proximal wound. The raphe in the
midline of the FDL is split a distance of 1.5 to 2.5 cm to create two
tails (Fig. 35-10).

 |
|
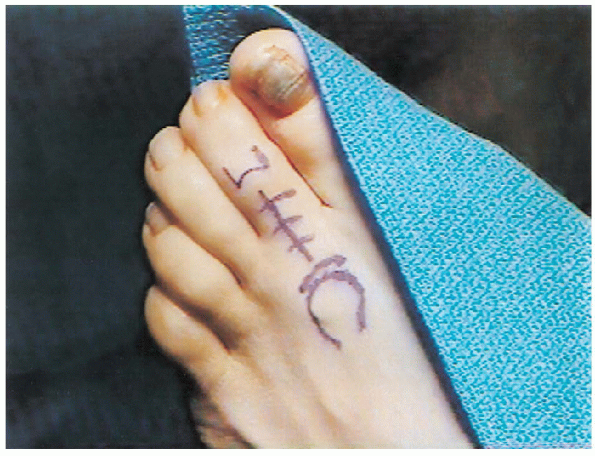
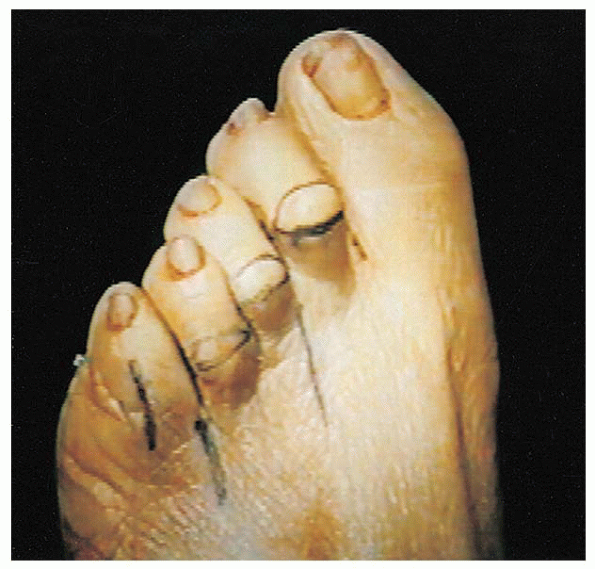
FIGURE 35-6. Plantar incision markings.
|
Medial and lateral tunnels are created adjacent to the extensor hood
for passage of the FDL tendon slips. To create these tunnels, a
hemostat is passed from dorsal to plantar aspects, deep to the
neurovascular bundle, to retrieve the FDL tails
 and bring them to the dorsal wound (Fig. 35-12).
and bring them to the dorsal wound (Fig. 35-12).The tails are then sutured to the extensor mechanism in the middle of
the proximal phalanx using 3-0 or 4-0 absorbable suture (Fig. 35-13).
 The optimal position
The optimal positionfor suturing the tendon is determined with the ankle in neutral and the
toe plantar flexed 20 degrees at the MTP joint. After the transfer
(with the ankle in neutral), the MTP joint should rest in neutral, and
the PIP joint should rest in neutral or in less than 10 degrees of
flexion (Fig. 35-14). The dorsal wound is closed with nylon suture, and the plantar wound is closed with chromic suture.
 |
|
FIGURE 35-7. Dorsal incisions.
|
 |
|
FIGURE 35-8. Flexor digitorum longus and flexor digitorum brevis tendons.
|
 |
|
FIGURE 35-9. Release of the flexor digitorum longus tendon.
|
 |
|
FIGURE 35-10. Two tails of the flexor digitorum longus tendon.
|
 |
|
FIGURE 35-11. Extensor hood.
|
 |
|
FIGURE 35-12. Retrieved flexor digitorum longus tails.
|
 |
|
FIGURE 35-13. Suturing of the flexor tails to the extensor hood.
|
 |
|
FIGURE 35-14. After the flexor tendon is sutured to the extensor tendon, the metatarsophalangeal joint should rest in neutral.
|
 |
|
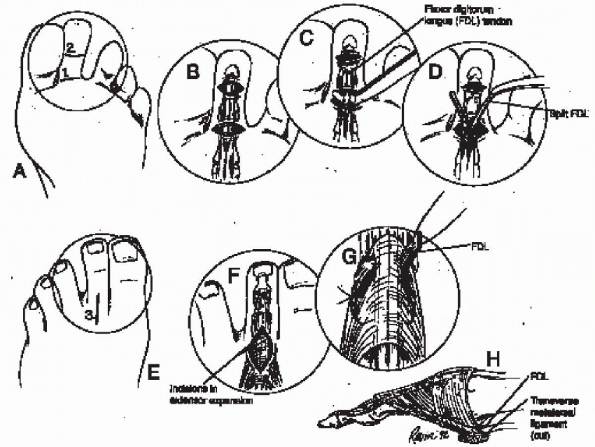
FIGURE 35-15. Flexor digitorum longus (FDL) transfer for mild deformity. A: Transverse incisions at the distal interphalangeal (DIP) and proximal interphalangeal joint creases. B: The flexor tendon is released at the DIP joint. C: The FDL is brought into the proximal wound with a hemostat. D: The FDL is split about 2 cm along natural cleavage line in its center. E and F:
A 2-cm longitudinal incision is made over the dorsum of the proximal half of the proximal phalanx. Separate, smaller incisions are placed through the extensor expansion in the distal part of the wound for windows through which FDL slips will pass. G: FDL slips pass plantar to the transverse metatarsal ligament, which is essential for any flexion moment at the metatarsophalangeal joint. H: Tendon slips may be crossed and sutured together, but this may leave a small knot beneath skin. (From Richardson EG. Lesser toe abnormalities. In: Crenshaw AH, ed. Campbell’s operative orthopaedics, 8th ed. St. Louis: Mosby-Year Book, 1992, with permission.) |
Sutures are removed at 3 weeks. For 6 weeks, the toe is taped to
maintain PIP extension and prevent dorsiflexion at the
MTP. Alternatively, a Budin splint can be used to maintain the toe position (Fig. 35-16).
 |
|
FIGURE 35-16. Budin splint (A)
and a splint applied to the second toe to maintain proximal interphalangeal joint extension and prevent dorsiflexion at the metatarsophalangeal hammer toe (B). |
PIP joint (i.e., DuVries arthroplasty). The distal aspect of the middle
phalanx is excised to form a fibrotic or bony union at the PIP joint
with the joint in a straightened position. Expectations
for the surgery must be discussed with the patient. With a DuVries
arthroplasty, the deformity is eliminated, but in most cases, a stiff,
shorter toe results. Rarely, a floppy toe occurs.
incision over the dorsal aspect of the PIP joint that includes most or
all of the dorsal callus (Fig. 35-17). The
extent of the transverse incision is defined by the medial and lateral
aspects of the toe crease when the toe is flexed at the PIP joint. The
typical width of the ellipse is 4 to 5 mm. When operating on the fifth
toe, a dorsal longitudinal incision is made over the PIP joint (Fig 35-17).
 |
|
FIGURE 35-17. Incision over the dorsal aspect of the proximal interphalangeal joint.
|
incision for a DuVries arthroplasty is a full-thickness incision that
includes skin with the callus, the extensor tendon, and the joint
capsule.

After the full-thickness flap is removed, the PIP joint is flexed, and
the collateral ligaments are detached from their proximal origin on the
PIP joint with a no. 15 scalpel blade. To cut the medial collateral
ligaments, the toe is flexed at the PIP joint, and the scalpel is
passed from the plantar aspect of the proximal phalanx (parallel to the
proximal phalanx) to the medial aspect of the proximal phalanx.
 The same is done to cut the lateral collateral ligament.
The same is done to cut the lateral collateral ligament.  Care is taken to stay close to the bone when releasing the collateral ligaments to avoid damage to the neurovascular bundles.
Care is taken to stay close to the bone when releasing the collateral ligaments to avoid damage to the neurovascular bundles.With the release of the collateral ligaments, the head of the proximal
phalanx is delivered into the wound. Next, the soft tissue is cleared
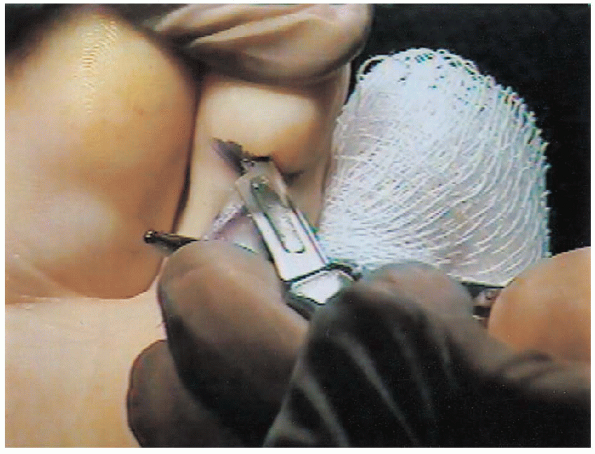
from the distal aspect of the phalanx,  and a straight snap is used to define the meta-physeal-diaphyseal junction and protect the skin (Fig. 35-18). A bone cutter is used to remove the head of the proximal phalanx just proximal to the condyles of the proximal phalanx (Figs. 35-19 and 35-20).
and a straight snap is used to define the meta-physeal-diaphyseal junction and protect the skin (Fig. 35-18). A bone cutter is used to remove the head of the proximal phalanx just proximal to the condyles of the proximal phalanx (Figs. 35-19 and 35-20).
If there is continued flexion deformity at the PIP, an additional 2 to
3 mm of bone can be resected, or the FDL can be released. To release
the FDL, an incision is made in the volar plate, and the FDL is cut. If
an arthrodesis is desired, the articular surface of the base of the
middle phalanx is roughened using a curette. More
bone should be resected in longer-standing deformities and in older
individuals to allow adequate correction and to avoid neurovascular
compromise. Removal of excessive bone from the proximal phalanx can lead to a floppy toe.
 |
|
FIGURE 35-18. A straight snap is placed at the distal proximal phalanx to protect the soft tissue.
|
 |
|
FIGURE 35-19. Cutting the distal portion of the proximal phalanx with a bone cutter.
|
 |
|
FIGURE 35-20. Appearance after removal of the condyles of the proximal phalanx.
|
 |
|
FIGURE 35-21. Kirschner wire through the middle and distal phalanx.
|
is directed distally from the middle phalanx through the distal phalanx
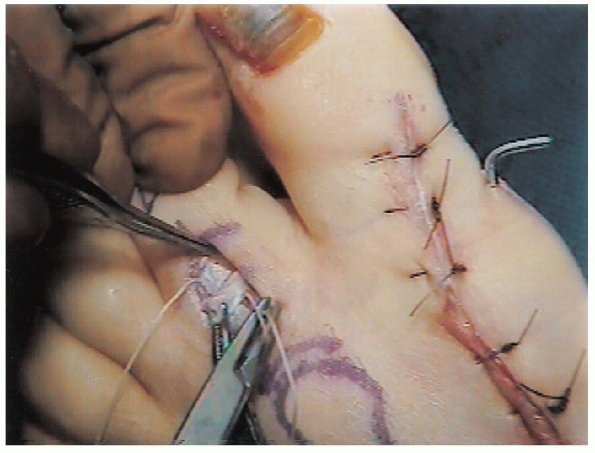
and out the tip of the toe (Fig. 35-21). The K-wire is then drilled retrograde across the resected PIP joint into the proximal phalanx (Fig. 35-22). When a K-wire is used, the wound is closed with at least two horizontal mattress sutures, incorporating the extensor tendon.
bolsters to keep the PIP joint extended. Two Telfa bolsters are placed
transversely, proximally and distally to the PIP joint. These bolsters
are incorporated into the 3-0 nylon suture vertical mattress closure.
When the sutures are tied over the bolsters, leverage is created that
extends the PIP joint into satisfactory alignment (Fig. 35-23). After
a DuVries arthroplasty, the toe should be examined with the ankle in
slight dorsiflexion to determine if there is an extension deformity at
the MTP joint. With a mild extension deformity,
a percutaneous EDL tenotomy (performed at the level of the MTP) may be necessary. With a more extensive deformity, the MTP joint should be released, as discussed in the Severe Deformity procedure.
 |
|
FIGURE 35-22. Kirschner wire through the proximal phalanx and metatarsophalangeal joint.
|
 |
|
FIGURE 35-23. A and B: Telfa bolsters are used to close the proximal interphalangeal joint wound.
|
shoe. The K-wire and sutures are removed 3 weeks postoperatively.
Taping (as previously described) or a Budin splint is used for 6 weeks
postoperatively to keep the PIP joint extended and prevent MTP
dorsiflexion.
PIP joint (i.e., DuVries arthroplasty) with release of the extension
deformity at the MTP joint (i.e., contracture, subluxation, or
dislocation).
the PIP joint as described for a moderate hammer toe deformity. A
second longitudinal incision (2 to 3 cm) is made over the dorsal aspect
of the MTP joint.
moderate hammer toe deformity. Before placement of the K-wire,
attention is turned to the deformity at the MTP joint.
longitudinal incision overlying the MTP joint is performed and
dissection is carried down to the level of the extensor tendon (Fig. 35-17). The EDL tendon is Z-lengthened (Fig. 35-24),
and a tenotomy of the EDB tendon is performed. A transverse dorsal
capsulotomy of the MTP joint is executed with resection of a
rectangular piece of the dorsal capsule. The joint is then manipulated
out of extension. If an extension deformity persists, the collateral
ligaments are released from their proximal origin on the metatarsal.
The ligaments are released by making a dorsal longitudinal incision on
the metatarsal neck and subperiosteally releasing the soft tissues
medially and laterally. If necessary, an MTP arthroplasty (i.e.,
resection of the distal 2 mm of the metatarsal head) can be performed
for continued extension deformity or severe arthritis.
and PIP joints as previously described for a moderate hammer toe
deformity (Fig. 35-21). The wire is placed across the MTP joint while holding the ankle in neutral dorsiflexion and the toe in neutral alignment (Figs. 35-22 and 35-25). The
foot must be held in a plantigrade position while crossing the MTP
joint with the K-wire to ensure proper alignment of the joint.
The EDL tendon is repaired with resorbable suture. The PIP joint wound
is closed with nylon mattress sutures incorporating the extensor
tendon, and the MTP joint incision is closed with interrupted nylon
sutures.
 |
|
FIGURE 35-24. Z-lengthening of the extensor digitorum longus.
|
 |
|
FIGURE 35-25. Kirschner wires across interphalangeal and metatarsophalangeal joints.
|
shoe. The sutures and K-wire are removed 3 weeks after surgery. A Budin
splint or taping is then used for 6 weeks.
correction at the MTP and PIP joints, reduction of the MTP and PIP
joints may place tension on the neurovascular bundle. Neurovascular
compromise which does not resolve several minutes after the tourniquet
is removed may require removal of the K-wire to allow the toe to assume
a more shortened position. After removal of a K-wire, extra care must
be used with the postoperative dressing to maintain the position of the
toe. The reoperated toe is particularly vulnerable to neurovascular
compromise.
flexor-to-extensor transfer varies, with many studies reporting
satisfactory results for more than 90% of cases. Swelling of the toe
may persist for 4 to 6 months. Complications are uncommon and include
transient numbness, postoperative vascular impairment, toe stiffness,
hyperextension of the DIP joint, or recurrence of deformity.
for 4 to 6 months after surgery. Complications of a DuVries
arthroplasty include postoperative vascular impairment, infection, toe
angulation, recurrence of deformity, flail toe, and mallet toe
deformity.
