Femoral Head
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > IV – Lower Extremity Fractures and Dislocations > 28 – Femoral Head
28
Femoral Head
EPIDEMIOLOGY
-
Almost all are associated with hip dislocations.
-
These fractures complicate 10% of posterior hip dislocations.
-
Most are shear or cleavage type, although
recently, more indentation-type or crush-type fractures have been
recognized with the increased use of computed tomography (CT). -
Indentation fractures are more commonly associated with anterior hip dislocations (25% to 75%).
ANATOMY
-
The femoral head receives its blood supply from three sources (Fig. 28.1):
-
The medial femoral circumflex artery supplies the majority of the superior weight-bearing portion.
-
The lateral femoral circumflex artery and the artery of the ligamentum teres supply the remainder.
-
-
Seventy percent of the femoral head
articular surface is involved in load transfer, and thus damage to this
surface may lead to the development of posttraumatic arthritis.
MECHANISM OF INJURY
-
Most femoral head fractures are secondary to motor vehicle accidents, with axial load transmission proximally through the femur.
-
If the thigh is neutral or adducted, a
posterior hip dislocation with or without a femoral head fracture may
result. These fractures may be the result of avulsion by the ligamentum
teres or cleavage by the posterior acetabular edge. -
In anterior dislocations, impacted femoral head fractures may occur because of a direct blow from the acetabular margin.
CLINICAL EVALUATION
-
Formal trauma evaluation is necessary because most femoral head fractures are a result of high-energy trauma.
-
Ninety-five percent of patients have injuries that require inpatient management independent of femoral head fracture.
-
In
addition to hip dislocation, femoral head fractures are also associated
with acetabular fractures, knee ligament injuries, patella fractures,
and femoral shaft fractures. -
A careful neurovascular examination is essential, because posterior hip dislocations may result in neurovascular compromise.
RADIOGRAPHIC EVALUATION
-
Anteroposterior (AP) and Judet (45-degree oblique) views of the pelvis should be obtained.
-
Hip dislocation is almost always present.
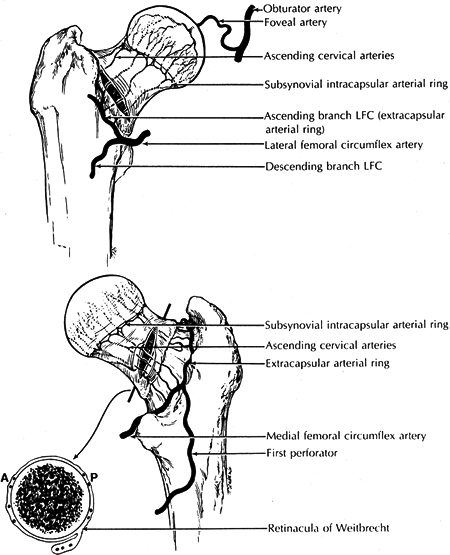 Figure
Figure
28.1. Vascular anatomy of the femoral head and neck. Top: Anterior
aspect. Bottom: Posterior aspect. LFC, lateral femoral circumflex
artery.(From Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 4th ed, vol. 2. Philadelphia: Lippincott-Raven, 1996:1662.) -
The AP radiograph of the pelvis may demonstrate femoral head fragments in the acetabular fossa.
-
If closed reduction is successful, CT is
necessary to evaluate the reduction of the femoral head fracture and to
rule out the presence of intraarticular fragments that may prevent hip
joint congruity. -
Some authors recommend CT evaluation even if the closed reduction is unsuccessful to evaluate associated acetabular fractures.
-
Sagittal CT reconstruction may also be helpful in delineating the femoral head fracture.
P.314
P.315
CLASSIFICATION
 |
|
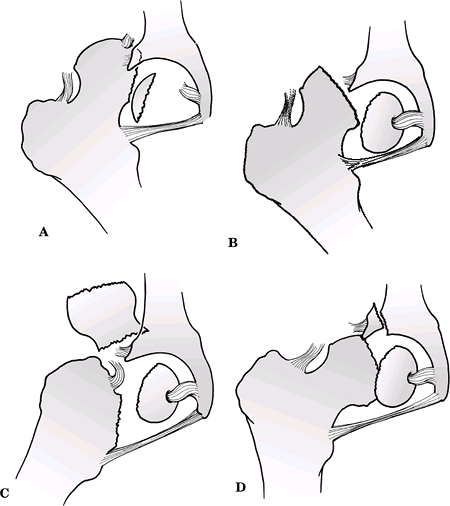
Figure
28.2. The Pipkin classification of dislocations with femoral head fractures. (A) Type I. (B) Type II. (C) Type III. (D) Type IV. (From Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006.)
|
Pipkin (Fig. 28.2)
| Type I: | Hip dislocation with fracture of the femoral head inferior to the fovea capitis femoris |
| Type II: | Hip dislocation with fracture of the femoral head superior to the fovea capitis femoris |
| Type III: | Type I or II injury associated with fracture of the femoral neck |
| Type IV: | Type I or II injury associated with fracture of the acetabular rim |
Brumback et al.
| Type 1A: | Posterior hip dislocation with femoral head fracture involving the inferomedial (non-weight-bearing) portion of the head and minimal or no fracture of the acetabular rim with stable hip joint after reduction |
| 1B: | Type 1A with significant acetabular fracture and hip instability |
| Type 2A: | Posterior hip dislocation with femoral head fracture involving the superomedial (weight-bearing) portion of the head and minimal or no fracture of the acetabular rim with stable hip joint after reduction |
| 2B: | Type 2A with significant acetabular fracture and hip instability |
| Type 3A: | Any hip dislocation with femoral neck fracture |
| 3B: | Any hip dislocation with femoral neck and head fracture |
| Type 4A: | Anterior dislocation of the hip with indentation of the superolateral weight-bearing surface of the femoral head |
| 4B: | Anterior dislocation of the hip with transchondral shear fracture of the weight-bearing surface of the femoral head |
| Type 5: | Central fracture-dislocations of the hip with fracture of the femoral head |
P.316
OTA Classification of Femoral Head Fractures
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
TREATMENT
Pipkin Type I
The femoral head fracture is inferior to the fovea. These fractures occur in the non-weight-bearing surface.
-
If reduction is adequate (<1 mm step-off) and the hip is stable, closed treatment is recommended.
-
If the reduction is not adequate, open
reduction and internal fixation with small subarticular screws using an
anterior approach are recommended. -
Small fragments may be excised if they do not sacrifice stability.
Pipkin Type II
The femoral head fracture is superior to the fovea. These fractures involve the weight-bearing surface.
-
The same recommendations apply for the
nonoperative treatment of Type II fractures as for Type I fractures,
except that only an anatomic reduction as seen on CT and repeat
radiographs can be accepted for nonoperative care. -
Open reduction and internal fixation generally comprise the treatment of choice through an anterior approach.
Pipkin Type III
A femoral head fracture occurs with an associated fracture of the femoral neck.
-
The prognosis for this fracture is poor and depends on the degree of displacement of the femoral neck fracture.
-
In younger individuals, emergency open
reduction and internal fixation of the femoral neck are performed,
followed by internal fixation of the femoral head. This can be done
using an anterolateral (Watson-Jones) approach. -
In older individuals with a displaced femoral neck fracture, prosthetic replacement is indicated.
P.317
Pipkin Type IV
A femoral head fracture occurs with an associated fracture of the acetabulum.
-
This fracture must be treated in tandem with the associated acetabular fracture.
-
The acetabular fracture should dictate
the surgical approach, and the femoral head fracture, even if
nondisplaced, should be internally fixed to allow early motion of the
hip joint.
Femoral Head Fractures Associated with Anterior Dislocations
-
These fractures are difficult to manage.
-
Indentation fractures, typically located
on the superior aspect of the femoral head, require no specific
treatment, but the fracture size and location have prognostic
implications. -
Displaced transchondral fractures that
result in a nonconcentric reduction require open reduction and either
excision or internal fixation, depending on fragment size and location.
COMPLICATIONS
-
Osteonecrosis:
-
Patients with posterior hip dislocations
with an associated femoral head fracture are at high risk for
developing osteonecrosis and posttraumatic degenerative arthritis. The
prognosis for these injuries varies. Pipkin Types I and II are reported
to have the same prognosis as a simple dislocation (1% to 10% if
dislocated <6 hours). Pipkin Type IV injuries seem to have roughly
the same prognosis as acetabular fractures without a femoral head
fracture. Pipkin Type III injuries have a poor prognosis, with a 50%
rate of posttraumatic osteonecrosis. -
Ten percent of patients with anterior
dislocations develop osteonecrosis. Risk factors include a time delay
in reduction and repeated reduction attempts.
-
-
Posttraumatic osteoarthritis: Risk
factors include transchondral fracture, indentation fracture greater
than 4 mm in depth, and osteonecrosis.
