The Pediatric Orthopaedic Examination
on the age of the child, the chief complaint, and the magnitude of the
problem. In all situations, the clinician should respect the dignity of
the child, family, and other health care professionals who accompany
the patient. The clinician begins by introducing himself or herself to
the patient and family. If a resident physician or medical student
accompanies the clinician into the exam room, it is important to
introduce him or her as well. The clinician does not remain standing,
but sits down and listens while taking an accurate history from the
patient and family.
fracture, a thorough history and physical examination are required for
evaluating a 2-year-old boy with developmental delay and inability to
walk. The history begins with the chief complaint in the words of the
patient or, if the patient is not yet old enough to talk, in the words
of the family. The history of present illness includes details
concerning when and how the problem started, how it has evolved,
whether it has been treated, and what situations, if any, aggravate or
relieve the symptoms. The developmental history includes the birth
history, with details concerning pregnancy, delivery, and perinatal
course. It also includes developmental milestones, such as the ages at
which the child first sat up, pulled to standing, cruised (walked
around while holding on to furniture), walked independently, and
developed handedness. The past medical history includes any allergies,
hospitalizations, surgical operations, major illnesses, and
medications. The family history seeks information about siblings,
parents, grandparents, and any other relatives with a medical problem
similar to that of the child. The review of systems, includes general
questions about each system, such as the gastrointestinal system, to
detect any other medical problems. The personal and social history
reviews the living situation of the patient and any habits that he or
she may have, such as smoking.
of the patient, a thorough examination of the skin, spine, and upper
and lower extremities, and a brief neurologic examination. The
pediatric orthopaedic examination does not typically include the vital
signs or a detailed examination of the head, eyes, ears, nose, throat,
chest, heart, or abdomen. The child’s pediatrician usually performs
these aspects of the physical examination, but if concerns about these
areas arise during the examination, they are examined in detail.
examination is conducted vary depending upon the age of the patient.
Infants and young children are unable to give a history, whereas an
older child will often give a more accurate history than the family
can. The teenage boy with a chief complaint of a postural round back
may have no concerns, but the family may be concerned that he will
develop a severe kyphotic deformity like his grandmother. Many
pediatric orthopaedic disorders develop only in certain age groups,
such as Legg-Calvé-Perthes disease, which typically develops in 4- to
10-year-old boys. As a result, the following discussion about the
pediatric orthopaedic examination is divided into three sections,
according to the age of the patient.
children from birth to 4 years of age. These patients are usually
unable to give an accurate history, so most of the history is obtained
from the family. The child may be apprehensive about going to the
doctor and is often afraid of being examined. A toy or sticker may be
helpful to relax the patient and allow the clinician to do a physical
examination. Most of the physical examination of an infant or young
child can be done in the mother’s lap. For pertinent parts of the
examination, the infant can be placed on the examining table. If the
infant is afraid and upset, bottle-feeding during this part of the
examination can be helpful. If the clinician can gain the respect and
trust of the child and family, the physical examination can be
performed more easily.
years of age. These patients are usually interested in participating in
the examination and will often correct their parents about certain
aspects of the history. They tend not to feel threatened and are
usually calm and cooperative during the physical examination. Many
children do not like removing their clothes. This situation can be
avoided if the child comes to the appointment wearing a T-shirt and a
pair of shorts. It is also important to have extra pairs of disposable
shorts and gowns in the office to address this issue. Some children
with special health needs will be particularly resistant to a physical
examination. In this situation, it is often helpful to tell the family
exactly what you would like to accomplish. For example, if you would
like to examine the child for scoliosis, this can easily be explained
to the family, who can then position the patient so that you can
perform the examination.
from 10 to 18 years of age. These patients are usually very motivated
to get better and will give an accurate history. Teenagers are also
concerned about removing their clothes, and will likely be reassured to
be told that they do not need to remove their T-shirts or shorts. If
the examination is conducted appropriately and in a manner that
respects their privacy, teenagers will allow the clinician to perform a
complete physical examination.
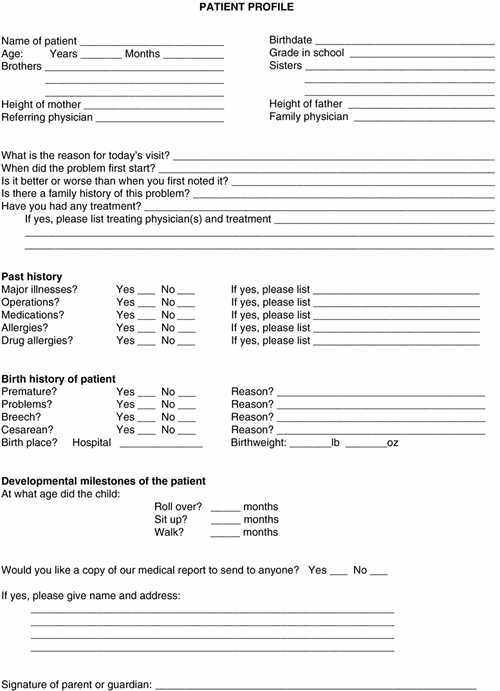
patient profile, which is filled out by the family (ages birth to 4
years old), the family with help from the patient (ages 4 to 10 years
old), or the patient with help from the family (ages 10 to 18 years
old), before proceeding with the history and physical examination (Fig. 5.1).
The patient profile includes the chief complaint and history of present
illness, with details concerning the birth and developmental history.
It also asks about family history, allergies, current medications,
previous hospitalizations, or surgical operations. To complete the
profile, the patient and/or family sign a release, so that a copy of
the office note may be mailed to the family or referring pediatrician.
Concerned that the baby might have a dislocated hip, the pediatrician
referred her for evaluation. The birth history reveals that this is the
mother’s first child and the pregnancy was normal, but the baby was in
the breech presentation and had to be delivered by cesarean section.
The birth weight was 3500 g (7 lb 11 oz) and the baby is otherwise
healthy. There is no family history of hip problems.
 |
|
Figure 5.1 Patient profile. This form can save valuable time while conducting the history and physical examination.
|
ligamentum teres gets trapped between the femoral head and the
acetabulum, or it may indicate a subluxatable or dislocatable hip as is
seen in developmental dysplasia of the hip (DDH). To distinguish
between these two different entities, the clinician focuses on certain
aspects of the history and physical examination that are associated
with DDH. The birth history is important because DDH is associated with
primigravida mothers, oligohydramnios, breech presentations, and
congenital muscular torticollis. The breech presentation is the most
important, because the incidence of DDH is 20% to 30% in infants in the
frank (single) breech presentation, even if the infant was delivered by
cesarean section. The developmental history may reveal that the infant
has a neuromuscular disorder, such as arthrogryposis multiplex
congenita. The family history is helpful because the incidence of DDH
is higher when other family members have the disorder.
in the mother’s lap. In this position, the infant is comfortable and
the clinician can examine the range of motion of the hands, wrists,
elbows, and shoulders. The range of motion of the neck is evaluated to
rule out a contracture of the sternocleidomastoid muscle that may be
secondary to a congenital muscular torticollis. The knees, ankles, and
feet can be examined to look for any anomalies that might be associated
with DDH. The baby can then be placed prone over the mother’s shoulder,
similar to the position for burping, while the clinician examines the
spine. A sacral dimple or hairy patch above the natal cleft may be a
sign of an underlying tethered spinal cord or lipomeningocele. These
disorders can cause partial paralysis of the lower extremities
resulting in a paralytic hip dislocation. Finally, after the rest of
the physical examination has been completed, the infant is placed on
the examining table to examine the hips.
examination. The examination should be performed on a firm surface with
the infant relaxed. If the infant is crying or upset, the DDH may not
be detected. In this situation, allow the family to feed or soothe the
infant and begin the examination when the infant is calm and relaxed.
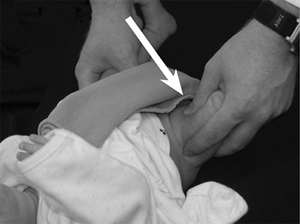
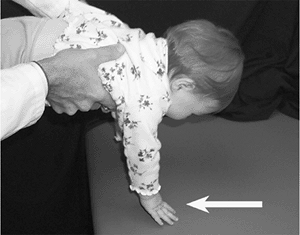
Barlow recommends that the examination be performed in two parts (1). Part one is the Ortolani maneuver.
The hips are flexed to a right angle with the knees fully flexed. Then,
the examiner places the long finger of each hand laterally, along the
axis of the femur over the greater trochanter, and the thumb of each
hand on the inner side of the thigh opposite the lesser trochanter. The
thighs are lifted into mid-abduction, and forward pressure is exerted
behind the greater trochanter using the middle finger of each hand,
while the other hand, in turn, holds the opposite femur and pelvis
steady. If the femoral head “clunks” forward into the acetabulum, the
hip has been dislocated. This maneuver, originally described by
Ortolani, represents a “sign of entry” as the femoral head reduces into
the acetabulum (Fig. 5.2). The Ortolani maneuver completes the first part of the Barlow provocative test.
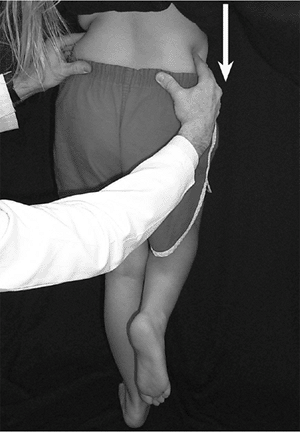
Part two consists of applying pressure backwards and outwards with the
thumb on the inner side of the thigh as the hip is adducted. If the
femoral head “clunks” or slips out over the posterior lip of the
acetabulum and back again after the pressure is released, the hip is
“unstable.” This maneuver represents a “sign of exit,” as the femoral
head subluxates or dislocates from the acetabulum (Fig. 5.3).
In subluxating hips the examiner may detect a sliding sensation as the
femoral head slides posteriorly in the acetabulum. Some investigators
believe it is best to examine the stability of each joint separately,
with the pelvis firmly held between a thumb on the pubis and the
fingers under the sacrum with one hand, while the other hand
manipulates the hip. The Barlow and Ortolani tests detect hip
instability with ligamentous laxity, and although these tests are
valuable during the neonatal period, they usually become negative by 3
months of age (2).
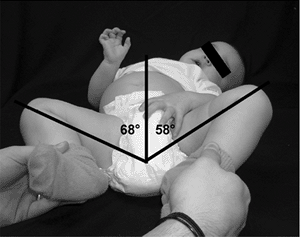
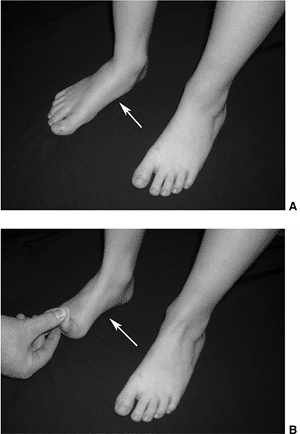
subluxated or dislocated, the adductor and flexor muscles gradually
develop contractures. The most common physical finding in older infants
with DDH is limited abduction of the hip (Fig. 5.4). This limited abduction may be
subtle, so it is important that the infant is positioned supine on a
firm table. An infant with bilateral DDH may have symmetric limited
abduction that can be detected only by a careful examination. The
superolateral subluxation or dislocation of the femoral head causes a
limb-length discrepancy. It shortens the thigh, causing more thigh
folds (telescoping) compared with the uninvolved side. Although
asymmetric thigh folds may be a normal finding, it alerts the clinician
to the possibility of DDH. If the hips are flexed to 90 degrees, the
subtle limb-length discrepancy can be detected because the knee on the
side of the involved hip will be lower than the knee on the opposite
side. This finding is termed a positive Galeazzi sign. In this patient, the Ortolani maneuver is positive, so treatment with a Pavlik harness is recommended.
 |
|
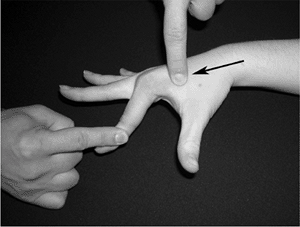
Figure 5.2
The first part of the Barlow provocative test is the Ortolani maneuver. This test is performed by gently abducting the hip and pushing forward with the long finger over the greater trochanter (arrow). A clunk is palpated as the femoral head slides over the posterior lip into the acetabulum. |
 |
|
Figure 5.3
The second part of the Barlow provocative test involves applying pressure backwards and outwards with the thumb on the inner side of the thigh (arrow) while adducting the hip. If the femoral head clunks or slips out over the posterior lip of the acetabulum and back again after the pressure is released, the hip is unstable. |
 |
|
Figure 5.4
After 3 months of age, the most common physical finding in a patient with developmental dysplasia of the hip (DDH) is limited abduction of the hip. The asymmetry may be subtle as in this 15-month-old girl with a dislocated left hip. She has decreased abduction of the left hip (58 degrees) compared with the right (68 degrees). |
when he was 3 months of age. When he began walking at 16 months of age,
the bowing was worse and his feet turned in. His feet now turn in so
much that he trips over them, falling frequently. The birth history
reveals that he was born after a 40-week gestation by normal vaginal
delivery, with a birth weight of 4000 g (8 lb 13 oz). He first sat at 7
months of age and began walking at 16 months of age. The family history
reveals that the father wore a brace until he was 2 years old because
his feet turned in.
clinician focuses on certain aspects of the history and physical
examination to determine whether the child has developmental delay. If
so, he may have problems with coordination or retention of primitive
reflexes. If the bowed legs represent physiologic bowing, one would
expect the deformity to be improving by 2 years of age. If the intoeing
is physiologic and represents a normal rotational variation, it will
usually be symmetric and is often not noticed until the child begins
walking. A unilateral problem involving the foot may indicate a mild
clubfoot or a neurologic problem such as a tethered spinal cord. The
clinician reviews the developmental history: most children will sit
independently by 6 to 9 months of age, cruise by 10 to 14 months of
age, and walk independently by 12 to 18 months of age (Table 5.1).
verify the details surrounding the birth to determine whether the child
was born premature, and whether there were any perinatal complications.
Premature infants, born at 25 to 30 weeks of gestation with birth
weights of 750 g (1 lb 10 oz) to 1500 g (3 lb 5 oz), have an increased
incidence of cerebral palsy with spastic diplegia. The first sign of
this disorder may occur when the family notes that their child is
delayed in walking or is tripping over his feet. When evaluating for
developmental delay, it is valuable to ask whether the infant is
ambidextrous. Most children will remain ambidextrous until 18 months to
3 years of age (Table 5.1). If a child who is
tripping over his left foot is also strongly right-handed, the birth
history may reveal an intrauterine cerebral vascular accident causing
cerebral palsy with spastic hemiplegia.
by asking the family if they would like to take their son for a walk
down the hall. Most 2-year olds will enjoy walking
away
from the clinician and the exam room, but they often need to be carried
back. While the family is walking down the hall, the clinician observes
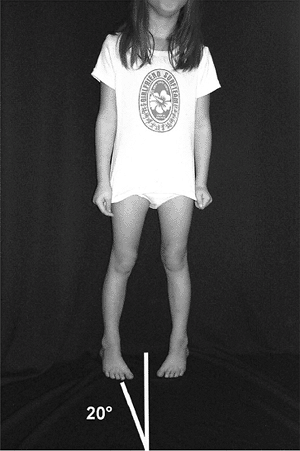
the child’s gait pattern including the foot-progression angle (3). The foot-progression angle is the angle between the axis of the foot and an imaginary straight line on the floor (Fig. 5.5).
The axis of the foot is derived from a line connecting a bisector of
the heel with the center of the second metatarsal head. The
foot-progression angle in children 1 to 4 years of age can vary from 20
degrees of inward to 20 degrees of outward rotation. The gait pattern
can also vary considerably in this age group, but will usually be
relatively symmetric, with a similar amount of time being spent in
stance phase (60% of the gait cycle) and swing phase (40% of the gait
cycle). Rotational values within two standard deviations of the mean
are termed rotational variations, and values outside two standard deviations are termed torsional deformities (4). The degree and location of any rotational variations can be documented by creating a rotational profile (Table 5.2).
The rotational profile includes the foot-progression angle, internal
rotation of the hips, external rotation of the hips, the thigh–foot
angle, and any foot deformities. The foot-progression angle measures
the degree of intoeing or outtoeing compared with an imaginary straight
line on the floor (normal range: 20 degrees inward to 20 degrees
outward rotation). The internal and external rotations of the hips give
a measure of the femoral rotational variation or torsion. The normal
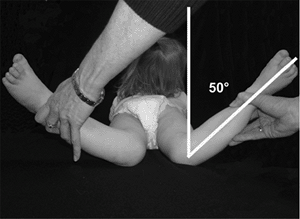
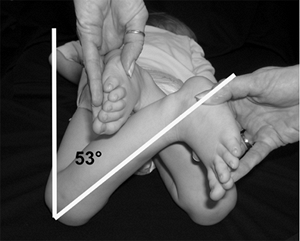
range of internal rotation is 20 degrees to 70 degrees (Fig. 5.6), and the normal range of external rotation is 25 degrees to 60 degrees (Fig. 5.7).
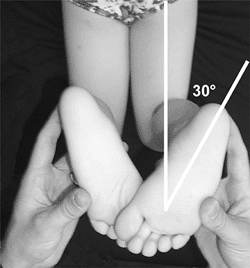
The thigh–foot angle is the angle between the axis of the thigh and the
axis of the foot, with the knee flexed 90 degrees. The thigh–foot angle
measures tibial rotational variation or torsion, and the normal range
is between 25 degrees of inward and 25 degrees of outward rotation (Fig. 5.8) (4).
The foot examination records any foot deformity that may be
contributing to the intoeing. Once the profile is filled out, it gives
an objective view of the location and magnitude of any rotational
variations or torsional deformities. This 2-year-old boy has internal
rotational variations of both femurs and tibias. The rotational profile
can be used as a baseline while following up
the child to document whether rotational variations are improving with growth.
|
TABLE 5.1 AVERAGE DEVELOPMENTAL ACHIEVEMENT BY AGE
|
||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
Figure 5.5
While the patient is walking, the foot-progression angle is the angle between the axis of the foot and an imaginary straight line on the floor representing the direction of movement. The axis of the foot is derived from a line connecting a bisector of the heel with the center of the second metatarsal head. This patient has a foot-progression angle of 20 degrees of internal rotation. |
refer to the orientation of the distal fragment compared with the
midline or proximal fragment. In a child with bowlegs, the distal
fragment (tibia) is angulated toward the midline compared with the
proximal fragment (femur), and is termed genu varum. In a child with knock-knees, the tibia is angulated away from the midline compared with the femur and is termed genu valgum.
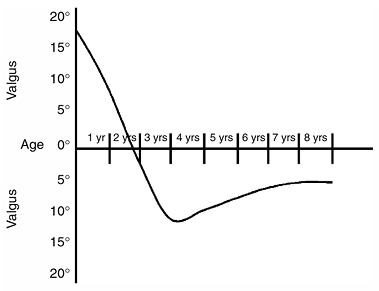
Most infants have bowed legs that spontaneously correct between 18 to
24 months of age. If the bowed legs correct between 2 and 4 years of
age, it is termed physiologic bowing. The lower extremities then
gradually develop genu valgum, which peaks between 3 and 4 years of
age, then decreases to reach the normal adult tibiofemoral alignment of
7 degrees of valgus by 7 to 8 years of age (Fig. 5.9) (5).
In this patient, the clinician determines whether the bowed legs
represent physiologic bowing or are associated with a growth problem
such as Blount disease or nutritional rickets. If
the
boy has short stature, more than two standard deviations from the mean,
it may be associated with nutritional rickets. In order to document
short stature, the clinician plots the patient’s height on a growth
chart.
 |
|
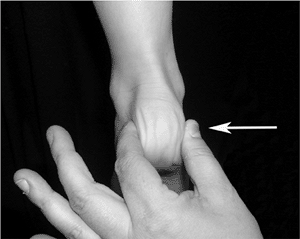
Figure 5.6
The internal rotation of the hips can be measured with the patient in the prone position with the clinician standing at the foot of the examining table. In this position, gravity allows the hips to fall into internal rotation. The angle between the leg and a line perpendicular to the tabletop measures the internal rotation (50 degrees in this patient). |
 |
|
Figure 5.7
The external rotation of the hips can be measured with the patient in the prone position and the clinician standing at the foot of the examining table. When the patient is prone, gravity allows the hips to fall into external rotation. The angle between the leg and a line perpendicular to the tabletop measures the external rotation (53 degrees in this patient). |
 |
|
Figure 5.8
The thigh-foot angle can be measured with the patient prone and the clinician standing at the foot of the examining table. The thigh–foot angle is the angle between the axis of the thigh and the axis of the foot, with the foot held in neutral position. The axis of the foot is derived from a line connecting a bisector of the heel with the center of the second metatarsal head. The thigh–foot angle measures the amount of tibial torsion (30 degrees in this patient). |
 |
|
Figure 5.9
Graph demonstrating the development of the tibiofemoral angle. Infants have genu varum that typically corrects by 18 to 24 months of age. The lower extremities then gradually develop genu valgum, which peaks between 3 and 4 years of age. The genu valgum then decreases to reach the normal adult tibiofemoral alignment of 7 degrees of valgus by 7 to 8 years of age. |
where the deformity is located. If the deformity is located in the
proximal tibia, it may indicate tibia vara or Blount disease. If the
deformity is symmetric involving both the distal femur and proximal
tibia, it may indicate physiologic bowing (6).
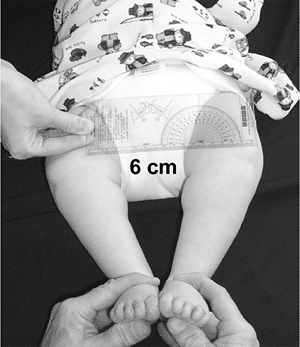
The amount of bowing is documented by measuring the “intercondylar
distance.” The intercondylar distance is measured in the supine
position with the hips and knees extended. The feet are brought
together until the medial malleoli are just touching; the intercondylar
distance is the distance between the femoral condyles (Fig. 5.10).
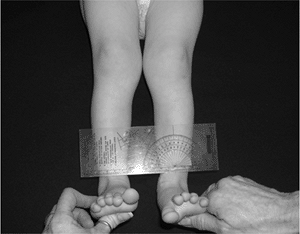
A genu valgum deformity is documented in the same fashion by measuring
the “intermalleolar distance.” With the child in the same position, the
feet are brought together until the femoral condyles are just touching;
the intermalleolar distance is the distance between the medial malleoli
(Fig. 5.11). If this patient has physiologic bowing, the intercondylar distance will decrease over the next 6 months.
months old and was still having difficulty with head control. They
became more concerned when he was not sitting at 10 months of age. He
finally sat at 14 months of age and has just recently begun pulling to
standing. He was born after a 28-week gestation, with a birth weight of
1100 g (2 lb 7 oz). He had perinatal respiratory difficulties and was
hospitalized in the neonatal intensive care unit for 2 months. He
developed a seizure disorder at 1 year of age, and his seizures are now
under control with medication.
 |
|
Figure 5.10
To measure the intercondylar distance, the child is supine with the lower extremities in extension. The feet are brought together until the medial malleoli just touch; the intercondylar distance is the distance between the femoral condyles (6 cm in this patient). |
 |
|
Figure 5.11
To measure the intermalleolar distance, the child is supine with the lower extremities in extension. The feet are brought together until the femoral condyles just touch; the intermalleolar distance is the distance between the medial malleoli (3 cm in this patient). |
physical examination will include a detailed neurologic examination and
developmental assessment. An 18-month-old boy with developmental delays
will usually not be apprehensive, and it is convenient to begin the
physical examination with the boy in the supine position. The clinician
grasps his hands, gradually pulling him into the sitting position,
while looking for head and trunk control. An infant will usually have
head control by 2 to 4 months of age and trunk control by 6 to 8 months
of age (Table 5.1). In infants there is a
series of primitive reflexes, including the Moro, grasp, neck-righting,
symmetric tonic neck, and asymmetric tonic neck; these are present at
birth and then gradually disappear in the process of normal development
by 3 to 10 months of age (Table 5.3). If these reflexes persist beyond 10 months of age, it may be a sign of a neuromuscular disorder.
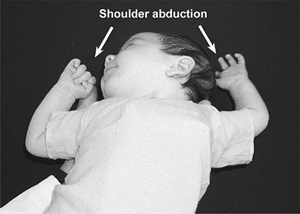
by introducing a sudden extension of the neck. The shoulders abduct and
the upper limbs extend, with spreading of the fingers, followed by an
embrace (Fig. 5.12). The Moro reflex usually disappears by 6 months of age (7). The grasp reflex
is elicited by placing a finger in the infant’s palm from the ulnar
side. The infant’s fingers will firmly grasp the examiner’s finger. If
traction is applied to the hand, the grasp reflex is so strong that the
examiner can lift the infant’s shoulder off the table. The grasp reflex
usually disappears by 3 months of age. The neck-righting reflex
is elicited by turning the head to one side; it is positive if the
trunk and limbs spontaneously turn toward the same side. This reflex
usually disappears by 10 months of age. The symmetric tonic neck reflex
is elicited by flexion of the neck, causing flexion of the upper limbs
and extension of the lower limbs. Similarly, extension of the neck
causes extension of the upper limbs and flexion of the lower limbs. The
asymmetric tonic neck reflex is elicited by
turning the head to the side, resulting in extension of the upper and
lower extremities on the side toward which the head is turned, and
flexion of the upper and lower extremities on the opposite side. This
position is termed the fencing position. The symmetric and asymmetric tonic neck reflexes usually disappear by 6 months of age.
|
TABLE 5.3 PRIMITIVE AND POSTURAL REFLEXES
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
Figure 5.12
The Moro reflex is elicited by gently lifting the infant with the right hand under the upper thoracic spine and the left hand under the head. The left hand is dropped to allow sudden neck extension. The infant abducts the upper limbs, with spreading of the fingers, followed by an embrace. |
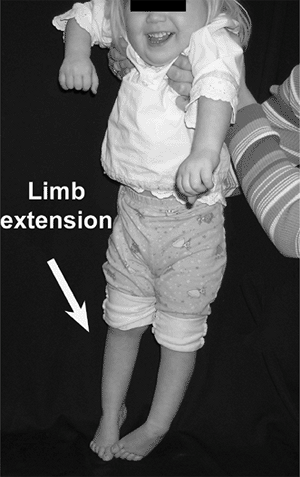
abnormal reflex, is elicited by holding the infant under the arms and
touching the feet to the floor, which causes a rapid extension of all
of the joints of the lower limb, progressing from the feet to the trunk
(Fig. 5.13). A normal infant will flex rather
than extend the lower extremities when placed in this position. These
primitive reflexes need to resolve with growth and development for the
child to be able to walk independently.
different stages of development, including the rooting, startle,
Gallant, and Landau reflexes. The rooting reflex
is elicited by touching the corner of the mouth, which causes the mouth
and tongue to turn toward the side that was stimulated. The startle reflex
is elicited by making a loud noise, which causes a mass myoclonic
response resembling a Moro reflex, except that the elbows remain
flexed. The startle reflex may persist until late childhood. The Gallant reflex
is elicited by stroking the side of the trunk, which causes the infant
to bend the spine toward the side that was stimulated. The Landau reflex
is elicited by supporting the infant by the trunk in the horizontal
prone position. The typical response is extension of the neck, spine,
and extremities; the collapse of the infant into an upside-down U may
indicate hypotonia.
gradually appears with the development of the nervous system, including
the parachute reflex and the foot-placement reaction (Table 5.3). The parachute reflex
is elicited by holding the infant in the air in the prone position,
then suddenly lowering the infant headfirst toward the table,
simulating a fall (Fig. 5.14). The reflex is
positive if the infant extends the upper extremities to break the fall.
This reflex usually appears by 12 months of age and remains until late
adulthood. The foot-placement reaction is elicited by holding the infant under the arms, then gently lifting the infant so that
the dorsum of the foot or the anterior surface of the tibia touches the
side of the table. The reaction is positive if the infant lifts up the
extremity and steps up onto the table. The foot-placement reaction
usually develops early in infancy and may persist until the age of 3 or
4 years.
 |
|
Figure 5.13
The extensor thrust is elicited by holding the infant under the arms and lowering the infant until the feet touch the floor. An extensor thrust is an abnormal reflex in which there is progressive extension of the lower limbs, progressing superiorly from the feet to the trunk. The response in an average infant is flexion of the lower extremities. |
who were 12 months of age or older and were not yet walking. He used
seven tests to predict whether an infant would subsequently walk. One
point was assigned for each primitive reflex that was still present,
and one point was assigned for each postural reflex that was still
absent (Table 5.4). A score of two points or
more indicated a poor prognosis for walking, a one-point score
indicated a guarded prognosis, and a zero-point score indicated a good
prognosis.
spine for any scoliosis or kyphosis. The upper and lower extremities
are examined to assess range of motion and to document any
contractures. If a contracture is identified, the clinician attempts to
passively correct it to determine whether it is flexible or rigid. An
18-month-old boy with cerebral palsy and spastic diplegia will
typically have contractures that can be passively corrected. A patient
with cerebral palsy and spastic quadriplegia may have rigid
contractures. When attempting to passively correct a rigid contracture,
if the contracture shows continuous resistance to passive correction,
the condition is termed lead-pipe rigidity. If the contracture has discontinuous resistance to passive correction, it is termed cogwheel rigidity (7). A patient with cerebral palsy and athetosis may have purposeless type movement patterns, particularly involving the hands and upper extremities. If the athetosis is of the tension type,
it can often be “shaken out” of the limb by the clinician. The reflexes
are also tested to determine whether the patient has hyperreflexia,
clonus, and a positive Babinski reflex.
This patient has cerebral palsy with spastic diplegia. He may have an
associated neuromuscular hip disorder, so an anteroposterior pelvis
radiograph is recommended.
 |
|
Figure 5.14
The parachute reflex is elicited by holding the infant in the air in the prone position, then suddenly lowering the infant headfirst toward the table, simulating a fall. The reflex is positive if the infant extends the upper extremities as if to break the fall (arrow). |
|
TABLE 5.4 PROGNOSIS FOR WALKING
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||
baby boy, the mother was told that the baby was not moving his right
arm. The pregnancy was normal, but the delivery was difficult because
of right shoulder dystocia. The delivery team had to apply considerable
traction on the head to deliver the baby. They noted some swelling and
tenderness on the right side of the baby’s neck shortly after birth,
but this resolved in the first week. At the 2-month appointment with
the pediatrician, the baby was moving his hand but always kept the
upper extremity at his side.
upper extremities, comparing the paralyzed right side with the
uninvolved side, looking for asymmetry. It is important to distinguish
a traumatic brachial plexus neuropathy, which causes a paralysis of the
upper extremity, from osteomyelitis, septic arthritis, or a birth
fracture, which can cause a pseudoparalysis. The treatment for each of
these conditions is different, and a delay in treatment of
osteomyelitis or septic arthritis can lead to devastating outcomes. An
infant with osteomyelitis, septic arthritis, or a birth fracture will
usually have swelling at the site, whereas an infant with traumatic
brachial plexus palsy will usually have no swelling in the extremity,
but may have swelling in the neck. An infant with traumatic brachial
plexus palsy or birth fracture of the humerus will usually have
paralysis at birth, whereas an infant with osteomyelitis or septic
arthritis may use the arm normally, and then suddenly develop the
pseudoparalysis. Traumatic brachial plexus palsy is a common birth
injury, typically seen in primigravida mothers with large babies after
difficult deliveries. It occurs because of traction and lateral tilting
of the head to deliver the shoulder. If the baby is in the breech
presentation, it occurs because of traction and lateral tilting of the
trunk and shoulders to deliver the head. Traumatic brachial plexus
palsy may have an associated fracture of the clavicle or humerus. There
are three types of brachial plexus palsies, depending upon which part
of the brachial plexus is affected.
is rare in newborns. The prognosis for recovery depends on the level
and magnitude of the injury and the time at which certain key muscles
recover function. If the biceps recover function before 3 months of
age, the prognosis is excellent for a full recovery. The presence of a Horner syndrome usually indicates a poor prognosis (8).
Upper brachial plexus palsy in an infant is easily recognized by the
absence of active motion of the involved extremity in the Moro reflex (Fig. 5.12),
or the asymmetric tonic neck reflex. Paralysis of C5 and C6 causes the
shoulder to be held in adduction and internal rotation, with the elbow
in extension, the forearm in pronation, and the wrist and fingers in
flexion. This posture is termed the waiter’s tip as if the infant is cleverly asking for a tip (Fig. 5.15). This posture is not seen in an infant with osteomyelitis, septic arthritis, or birth fracture.
 |
|
Figure 5.15
Paralysis of C5 and C6 causes the shoulder to be held in adduction and internal rotation, with the elbow in extension, the forearm in pronation, and the wrist and fingers in flexion. This posture is termed the waiter’s tip, as if the infant is cleverly asking for a tip (arrow). |
palsy is easily recognized by an absence of the grasp reflex in the
involved extremity. The hand is flaccid, with little or no voluntary
control. When there is total plexus involvement, the entire extremity
is flaccid, and the Moro (Fig. 5.12) and grasp
reflexes are both absent. A Horner syndrome refers to the constellation
of signs resulting from the interruption of sympathetic innervations to
the eye and ocular adnexae. The clinical findings include a triad of
signs: ipsilateral blepharoptosis, pupillary miosis, and facial
anhidrosis. This patient shows no sign of biceps motor function after 3
months of age, so the prognosis for recovery is guarded.
hip when she twisted her foot and fell going down the stairs. She was
fine but her son immediately began crying and refused to walk. When she
tried to stand him up, he would not put any weight on his right lower
extremity. She believes that when she fell, she may have landed on his
right leg. She has not noticed any swelling, and he stopped crying
after she gave him some anti-inflammatory medication. He is in good
health and has not had any chills or fever. She is a single mother with
four other children. She called the
pediatrician,
who recommended an x-ray; the x-ray showed a fractured tibia, and the
pediatrician referred the child for evaluation and treatment.
Although children have been harmed by their caregivers for centuries,
the medical profession did not officially acknowledge the
battered-child syndrome until 1962 (9). The age
of the boy is important because most child abuse involves children
younger than 3 years of age. It has been estimated that 10% of trauma
cases seen in emergency departments in children under 3 years of age
are nonaccidental (10). Although a number of
risk factors have been identified, it is important to remember that
children of all socioeconomic statuses, backgrounds, and ages can be
victims of abuse.
quiet environment talking with the mother about the details surrounding
the accident to determine whether they are consistent with the physical
findings. If the history is not consistent with the physical findings,
it may cause the clinician to suspect child abuse. While going over the
details of the injury, the clinician closely observes the mother’s
demeanor to determine whether she is being forthright with her answers.
If the mother seems nervous or uneasy while describing the
circumstances surrounding the accident, this should raise a red flag,
alerting the clinician that someone may have deliberately harmed the
child. After reviewing the details of the mechanism of injury, the
clinician reviews the past medical history to determine whether this is
the boy’s first fracture. A history of multiple previous fractures may
be consistent with battered-child syndrome or osteogenesis imperfecta.
The birth and developmental history are reviewed to determine whether
there is any underlying disorder that may make this child more
susceptible to fracture. The clinician spends time learning about the
home environment, and interviews other family members about the injury.
It is important to rule out battered-child syndrome because if it is
missed, there is a possibility that the child will be injured again,
and the next injury could be life-threatening. Each year, more than 1
million children in the United States sustain injuries that are
inflicted by their caregivers.
whole child because the clinician looks for other injuries that may
indicate battered-child syndrome. The height and weight are measured to
determine whether there is any evidence of growth retardation or
failure to thrive (11). The skin is closely
inspected for any contusions, ecchymoses, abrasions, welts, or burn
scars. Skin lesions are the most common presentation of physical abuse,
and in some cases may be the only physical finding. Bruises are common
over the shins and knees in 18-month-old boys, but bruises over the
buttocks or genitalia should raise a red flag. The head, eyes, ears,
nose, and throat are also closely examined for bruises or contusions.
Head trauma is the most frequent cause of morbidity and mortality in
abused children.
of the upper and lower extremities are palpated to evaluate for
contusions or fractures. An 18-month-old boy should not have any
discomfort when the clinician gently squeezes his arms, forearms,
thighs, and legs, but will have considerable discomfort if there is a
fracture. After skin lesions, fractures are the second most common
presentation of physical abuse. If there is any question about the
possibility of battered-child syndrome, it may be beneficial to contact
the pediatrician to determine whether neglect has ever been considered.
If the story is straightforward and the mother is forthcoming,
treatment can proceed without any further studies.
yesterday afternoon, when his mother noticed that he seemed to be
limping. Later that evening his limp became more obvious and he
complained of pain in his right knee. This morning he awoke complaining
of right knee pain and refused to walk. His parents called their
pediatrician, who referred him for evaluation to rule out a possible
infection. The past history reveals that 2 weeks ago he had a fever and
cough that lasted for 5 days.
typical for a patient with transient synovitis of the hip, it may also
be consistent with septic arthritis, pelvic osteomyelitis, or
Legg-Calvé-Perthes disease. A 4-year-old boy will often describe
exactly where it hurts and may point to the groin, thigh, or knee. It
is important to remember that pain can be referred, and a hip problem
presenting as knee pain is a classic example of referred pain. The
clinician asks whether the pain is constant or intermittent. The fever
and cough 2 weeks ago is an important part of the history because an
upper respiratory infection is often a precursor of transient synovitis
of the hip. Kocher et al. compared a group of patients having transient
synovitis with a group of patients having septic arthritis (12).
They reported that the patients with septic arthritis appeared to be
sicker, with fever, chills, inability to bear weight, elevated
erythrocyte sedimentation rate, leukocytosis, lower hematocrit values,
and an altered peripheral blood differential. A patient with acute
septic arthritis involving the hip would typically have a history of 1
to 2 days of severe pain, whereas a patient with juvenile arthritis may
have had intermittent low-grade pain for several weeks to months. The
pain associated with juvenile arthritis is typically worse in the
mornings, and this is not usually seen in other disorders. If the
history reveals he had chicken pox 2 weeks ago, the clinician may be
concerned that he is immunocompromised and may have an infection.
to determine whether it is symmetric. If the child has an antalgic
(painful) gait on the right side, the stance phase would be shortened
on that side. If the child will stand, he is asked to stand on one leg
and then on the opposite leg. When standing on one leg, the hip
abductor muscles contract to hold the pelvis up on the opposite side,
increasing the joint reactive forces in the hip. If the patient has an
irritable hip, the increased joint reactive forces are so painful that
he will not contract the hip abductor muscles. This causes the pelvis
to drop on the opposite side and is termed a positive Trendelenburg test (Fig. 5.16).
to the symptomatic side. The lower extremities are observed for any
swelling or asymmetry. The clinician palpates the spine, pelvis, and
lower extremities for tenderness. The hips are examined with the child
in the supine position, and the clinician looks for any asymmetry as
the hips are taken through a full range of motion. The range of motion
of both hips, especially internal rotation, should be symmetric. If the
patient has an irritable hip, he will guard and contract his muscles,
not allowing the clinician to take the hip through a full range of
motion. This is particularly noted in attempting to internally and
externally rotate the hip, with the hip and knee in 90 degrees of
flexion. If the patient is in a lot of pain, the clinician can gently
“log roll” the extremity, with the hip and knee in full extension. This
is more comfortable for the patient, and if he has severe pain even
with log rolling, the pain would be unbearable with the hip and knee in
flexion. If there is any question about the diagnosis, hip aspiration
under fluoroscopic guidance is recommended.
 |
|
Figure 5.16
The clinician palpates the iliac crests while the patient stands only on the left lower extremity. In single-limb support involving the left lower extremity, the right iliac crest should rise as the left hip abductor muscles contract to support the pelvis. If the right iliac crest drops (arrow), it is termed a positive Trendelenburg test, indicating weakness of the left hip abductor muscles. The Trendelenburg test can also be positive if the patient has an irritable left hip. In this case, the increased joint reactive forces are painful, so the patient will not contract the left hip abductor muscles. |
In this position, if the knee is pushed toward the examining table, it
transmits a tensile force to the sacroiliac joint. If the patient has
pyogenic arthritis involving the sacroiliac joint, he will experience
discomfort with this test. This patient has transient synovitis of the
right hip, so close follow-up is recommended to be certain that the
symptoms are resolving.
she walks. The problem was first noted by the maternal grandmother when
the child began walking at 13 months of age.
The
family is concerned that the problem is getting worse and they want to
know whether the girl should have arch supports or special shoes. The
birth and developmental history are within normal limits. The family
history reveals that her father has flat feet and wore special shoes
until he was 2 years old.
 |
|
Figure 5.17 With the patient supine, the right lower extremity is placed in the Figure 4
position with the hip in flexion, abduction, and external rotation (FABER test). The knee is gently pushed toward the examination table (arrow) transmitting a tensile force to the sacroiliac joint that may cause pain if the sacroiliac joint is inflamed. |
determine when the flat feet were first noticed. This information is
helpful because a rigid pes planus deformity, such as that seen in a
patient with a congenital vertical talus, is typically noticed at
birth. A rigid pes planus deformity that is seen in a patient with a
tarsal coalition is often not noticed until the child is 10 years of
age, when the cartilaginous bar begins to ossify and causes pain and
decreased motion of the foot. A flexible pes planus deformity collapses
with weight bearing, so it is not unusual that it was noticed only when
the child first began walking. A 3-year-old girl with a flexible
flatfoot will not usually have any pain.
take the child for a walk in the hall. The clinician notes that she
walks with a symmetric heel-toe gait pattern, with a foot-progression
angle of 15 degrees of external rotation (Fig. 5.5).
A patient with a planovalgus deformity will often toe-out, whereas a
patient with a cavovarus deformity will often toe-in. Before focusing
on the feet, a general physical examination of the back, upper, and
lower extremities is performed. A patient with flexible pes planovalgus
will often have generalized ligamentous laxity. Ligamentous laxity can
be detected by asking the patient to hyperextend the little finger
metacarpophalangeal joint (greater than 90 degrees indicates
ligamentous laxity), hyperextend the elbows, hyperextend the knees, and
touch the thumb to the volar surface of the forearm (Fig. 5.18).
Flexible pes planus is common and is most likely caused by excessive
laxity of the ligaments and joint capsules, allowing the tarsal arch to
collapse with weight bearing. It is important to differentiate this
benign condition from the more serious types of flatfeet, such as
congenital vertical talus or tarsal coalition.
 |
|
Figure 5.18 Ligamentous laxity can be detected by asking the patient to try to touch the thumb to the volar surface of the forearm.
|
subtalar, and tarsal joints to determine whether there is any loss of
motion. A contracture of the Achilles tendon often accompanies
symptomatic flatfeet (13). In standing, a
patient with flexible pes planus has a collapsed medial longitudinal
arch, a valgus hindfoot, and a supinated externally rotated forefoot (Fig. 5.19A).
The arch returns when the patient is sitting, because the
weight-bearing force that caused the collapse of the arch is relieved.
The arch also returns when the child stands on tiptoe, or with passive
extension of the metatarsophalangeal joint of the great toe, the toe-raise test, because of the windlass effect of the plantar fascia (Fig. 5.19B).
The clinician uses these tests to document that this patient has
ligamentous laxity with flexible pes planus, a benign condition that
does not require treatment.
 |
|
Figure 5.19 A: In the standing posture, a patient with a flexible pes planus has a collapsed medial longitudinal arch (arrow), a valgus hindfoot, a supinated forefoot, and an externally rotated forefoot. B: A patient with flexible pes planus will have a positive toe-raise test. When the great toe is dorsiflexed at the metatarsophalangeal, the arch is restored (arrow) because of the windlass effect of the plantar fascia.
|
a soccer game 2 months ago. The limp went away, but 3 days later he
complained of right groin pain and they noticed that he was limping
again. They went to their pediatrician, who asked whether the boy could
have pulled a muscle while playing soccer. The pediatrician noted that
he was in the fifth percentile for height and the ninety-fifth
percentile for weight. The pain and limp were worse with activity and
relieved by rest. He was otherwise in excellent health.
age, and symptoms of a groin muscle injury will typically improve in 2
to 4 weeks. If the patient had been African American, the clinician may
have considered the possibility of sickle cell disease with a bone
infarct involving the proximal femur. A bone infarct in a patient with
sickle cell disease will typically present with the sudden onset of
pain in the groin, rather than pain and limping for 2 months. A patient
with Legg-Calvé-Perthes disease will often complain of pain in the
groin, and may have short stature and a delayed bone age. It is
important to remember that a patient with Legg-Calvé-Perthes disease
may develop symptoms well after the actual onset of the disease.
Patients with Legg-Calvé-Perthes disease go through several stages,
including destructive and reparative phases (14).
Most of the symptoms develop early during the destructive phases, and
when the patient begins the reparative phases the symptoms gradually
resolve. A patient with multiple epiphyseal dysplasia may have short
stature and may have pain and a limp. Multiple epiphyseal dysplasia is
inherited as an autosomal dominant trait, so there may be a family
history of the disorder. The insidious onset of pain and a limp may
develop in a patient with a bone cyst or tumor involving the proximal
femur. A patient with an osteoid osteoma involving the proximal femur
(typically an older child) will often complain of night pain that is
relieved by aspirin.
walk in the hall. A patient with pain and a limp may have an antalgic
(painful) gait. This is characterized by a decreased time in the stance
phase on the side involved. The clinician also notes swaying or bending
of the trunk over the painful hip, to decrease the reactive forces on
the joint. This is termed a Trendelenburg gait pattern
and is an important clinical observation, because it leads the
clinician to suspect a hip problem. After observing the patient’s gait
pattern, the clinician examines the back and the upper and lower
extremities, looking for any asymmetry between the symptomatic side and
the uninvolved side. A patient with Legg-Calvé-Perthes disease and
synovitis involving the hip will typically have a loss of internal
rotation, abduction, and extension. The loss of internal rotation is
usually the most pronounced, and is best demonstrated by examining the
patient in the prone position with the hips in extension (Fig. 5.6).
degrees, and gently rotated internally and externally through a range
of motion. The clinician notes the amount of internal and external
rotation of each hip, and feels for any involuntary muscle guarding.
Guarding usually indicates that the patient has synovitis in the hip
with an associated effusion. In a patient with Legg-Calvé-Perthes
disease, the finding of persistent synovitis is associated with a less
favorable prognosis (15). If there is decreased
internal rotation without guarding, it may indicate a retroversion
deformity of the femoral neck, which is a condition that is often seen
in patients with developmental coxa vara. This patient likely has
Legg-Calvé-Perthes disease, so anteroposterior and frog pelvis
radiographs are recommended.
and Swelling of the Left Elbow After Falling from the Monkey Bars at
School
earlier today, when he fell from the monkey bars at school and
complained of severe pain in his left elbow.
about the accident and apprehensive about having to go to the emergency
room. The patient is usually found on a gurney, with the elbow in a
temporary splint. The mechanism of injury is important because it
reflects the magnitude of the injury and the likelihood of associated
neurovascular injuries. The patient recalls falling approximately 6
feet and landing on his outstretched arms. A fall on an outstretched
arm is the same mechanism of injury that can cause a distal humerus
fracture, an elbow dislocation, a forearm fracture, a distal radius
fracture, or a combination of these injuries. The frequency of
associated neurovascular injuries correlates with the magnitude of
injury. The past history may be helpful in detecting an underlying
disorder such as osteogenesis imperfecta. If the patient had
osteogenesis imperfecta, he may have a pathologic fracture, which is
usually minimally displaced and is not accompanied by neurovascular
injuries. A pathologic fracture is a fracture through weakened bone.
him during the examination. After a general examination of the spine
and lower extremities to evaluate for other injuries, the splint is
removed. The uninjured arm is examined first, so that the patient is
more at ease with the examination. The injured arm is then observed and
compared with the uninjured arm. It is observed that there is marked
swelling and ecchymosis over the distal humerus and elbow; these
findings are consistent with a supracondylar fracture of the distal
humerus. The clinician gently palpates the distal humerus to locate the
point of maximum tenderness. This
point
will be on the tension side of the fracture, because there is more
soft-tissue injury on the tension side than on the compression side.
immediate concern is whether there are associated neurovascular
injuries. Prior to treatment, a complete neurocirculatory examination
of the forearms and hands is performed in order to document pulses,
capillary fill, pain, light touch, strength, and range of motion of the
fingers. A supracondylar fracture can interfere with the circulation to
the hand by directly injuring the brachial artery, kinking the artery,
or causing too much swelling in the volar compartment of the forearm (16,17).
develop before or after treatment. A compartment syndrome develops when
there is too much swelling within a closed space. After a supracondylar
fracture, the compartment that most often develops excessive swelling
is the volar compartment of the forearm. When the pressure in the
compartment surpasses the systolic blood pressure, it will obliterate
the radial and ulnar pulses at the wrist. A compartment syndrome may be
first detected when it is noticed that the patient is experiencing pain
that seems out of proportion to the physical findings. Another early
sign is pain on passive stretching of the ischemic muscles. In a volar
compartment syndrome, the flexor muscles are ischemic, so the patient
may complain of pain on passive extension of the fingers. Early
detection is crucial because, by the time the pulses are obliterated,
the muscles in the forearm may already be necrotic. When the necrotic
muscles develop fibrosis and scarring, a Volkmann ischemic contracture
develops, causing a flexion deformity of the wrist and fingers that can
markedly interfere with hand function. If there is any question about a
possible compartment syndrome, urgent measuring of compartmental
pressures is crucial, and early fasciotomy of the compartments is
recommended.
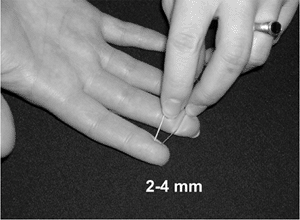
component of a nerve in a 6-year-old boy is to test two-point
discrimination using a paper clip, comparing the injured side with the
uninjured side (Fig. 5.20). The radial nerve is
tested by checking the sensation in the dorsal web space between the
thumb and the index finger (sensory), and by asking the patient to
extend his fingers (motor). The median nerve is tested by checking the
sensation on the volar aspect of the index finger (sensory), and asking
the patient to flex the long and ring fingers (motor). The ulnar nerve
is tested by checking the sensation on the volar aspect of the little
finger (sensory), and asking the patient to spread his fingers apart
(motor). The last muscle innervated by the ulnar nerve is the first
dorsal interosseous muscle. This muscle can be tested by placing a
finger on the radial side of the distal phalanx and another finger on
the muscle belly of the first dorsal interosseous muscle. The patient
is asked to push against the finger on the distal phalanx, and the
clinician palpates a contracture of the first dorsal interosseous
muscle if motor function is intact (Fig. 5.21).
The anterior interosseous nerve does not have a sensory component, so
an injury may not be detected unless the clinician tests the motor
component. The anterior interosseous nerve is tested by holding the
index finger in extension at the metacarpophalangeal and proximal
interphalangeal joints, and asking the patient to flex the tip of the
finger (motor). If the patient is extremely anxious and in severe pain,
it is possible that the physical examination may be compromised. If
that occurs, it is important to document the problem in the medical
record. In this case, a supracondylar fracture of the distal humerus is
suspected, so anteroposterior and lateral radiographs of the elbow are
recommended.
 |
|
Figure 5.20
To evaluate the sensory component of a nerve in a child, one can accurately and painlessly test two-point discrimination using a paper clip, comparing the injured side with the uninjured side. Most individuals have two-point discrimination of 2 to 4 mm in the index finger. |
 |
|
Figure 5.21
The last muscle innervated by the ulnar nerve is the first dorsal interosseous muscle. This muscle is tested by flexing the index finger metacarpophalangeal to 60 degrees, placing a finger on the radial side of the distal phalanx, and another finger on the muscle belly of the first dorsal interosseous muscle. The patient is asked to push against the distal finger, and a contraction of the first dorsal interosseous muscle is palpable (arrow) if motor function is intact. |
left heel pain 1 month ago after playing soccer. The pain is worse in
the evenings, particularly if he had played soccer earlier in the day.
He does not have any pain in the right foot or ankle. The pain seems to
be aggravated by running and relieved by rest. The family has noticed
mild swelling over the boy’s left heel. He is otherwise in excellent
health.
but the differential diagnosis includes tumor, infection, bone cyst,
tarsal coalition, leukemia, Reiter syndrome, and juvenile arthritis.
Calcaneal apophysitis is the most common cause of heel pain in the
immature athlete and is more common in boys (18).
Symptoms develop bilaterally in approximately 60% of cases. In 1912,
Sever described the condition as an inflammatory injury to the
apophysis associated with muscle strain, but recent investigators
attribute the symptoms to overuse and repetitive micro trauma.
stiffness, as one might see in patients with juvenile arthritis. He
denies having any pain at night, as might be seen in a patient with a
tumor or bone cyst. Heel pain that is persistent may be a sign of
childhood leukemia, so it is important to ask about any associated
symptoms.
hips, and knees are unremarkable. The feet appear symmetric with no
swelling, erythema, or skin changes. The pain is located right over the
calcaneal apophysis and is aggravated by medial-to-lateral compression
of the apophysis, or by squeezing the heel (Fig. 5.22).
There is no pain at the insertion of the Achilles tendon, as would be
seen in a patient with Achilles tendonitis, and there is no pain at the
origin of the plantar fascia, as would be seen in a patient with
plantar fasciitis. Achilles tendonitis and plantar fasciitis, although
common in adults, are not frequently seen in children. Ankle
dorsiflexion on the right is to 30 degrees and on the left is only to
20 degrees. It is common to have associated heel cord tightness in a
patient with calcaneal apophysitis. In the standing position he has
mild pes planovalgus and forefoot pronation, which are also conditions
seen in association with calcaneal apophysitis. Because calcaneal
apophysitis is an overuse syndrome, the symptoms should subside with
activity modification. Close follow-up is recommended to document
resolution of the symptoms.
 |
|
Figure 5.22
A patient with calcaneal apophysitis (Sever disease) has pain over the calcaneal apophysis. The pain is reproduced by medial-to-lateral compression of the apophysis, or squeezing the heel (arrow). |
when he began walking at 2 years of age. Although able to walk with his
feet flat on the floor, he walks on his toes 95% of the time. The birth
history reveals that he was born after a 28-week gestation, when his
mother spontaneously went into labor. The birth was by normal vaginal
delivery and the birth weight was 1400 g (2 lb 14 oz). The perinatal
course was complicated, and the patient was hospitalized in the
neonatal intensive care unit for 6 weeks because of respiratory
problems. The developmental history reveals that he sat up at 11 months
and walked at 2 years of age. The family first noticed that he was
right-handed at 12 months of age when he preferred to use his right
hand while playing with toys. He has been receiving physical,
occupational, and speech therapy through an early intervention program.
visit so that he will not have to change his clothes. The exam begins
by asking him to walk in the hall with his mother. He walks on his
toes, but will occasionally bring his heel to the floor. Sutherland et
al. reported that a mature gait pattern is well established at the age
of 3 years (19). Normal gait has a heel-toe
pattern in stance phase, beginning with heel strike, followed by foot
flat, and ending with toe-off. This patient has a toe-toe gait pattern
and, occasionally, a toe-heel gait pattern. In normal gait, during
early stance the foot plantarflexes between heel strike and foot flat.
This early ankle plantarflexion is termed the first rocker.
In midstance, there is forward rotation of the leg over the foot, and
the ankle dorsiflexes to accommodate this forward motion. This ankle
dorsiflexion is termed the second rocker. In terminal stance, the ankle plantarflexes at pushoff, and this plantarflexion is termed the third rocker.
When this patient ambulates with a toe-toe gait pattern, there is a
loss of the first rocker and a decrease of the second and third
rockers. When he ambulates with a toe-heel gait pattern, the first
rocker is reversed as the ankle dorsiflexes to get to
foot
flat, and there is a decrease of the second and third rockers. The gait
pattern is asymmetric, as he spends more time in the stance phase on
his right side, compared with the left. This is an important
observation, because a patient with muscular dystrophy or idiopathic
toe walking will typically have a symmetric gait pattern. In this
patient, the knees do not extend completely at the end of the swing
phase, and the hips do not extend completely at the end of the stance
phase. When walking at a faster pace, he lacks the symmetric fluid
reciprocating swinging motion of the upper extremities. Instead, he
postures both upper extremities, left more than right, with the elbows
in flexion, the forearms in pronation, and the wrists in flexion. This
is an important observation because posturing of the upper extremities
during gait is commonly seen in patients with spastic cerebral palsy.
During gait, he is noted to have a foot-progression angle of 10 degrees
of inward rotation on the left and 5 degrees of inward rotation on the
right (Fig. 5.5).
examination includes the spine and upper and lower extremities. The
spine is examined from the back with the patient standing to look for
any asymmetry. The clinician’s hands are placed on the patient’s iliac
crests; the right iliac crest is 5 mm higher than the left, indicating
a slight limb-length discrepancy, with the right longer than the left.
Patients with cerebral palsy and spastic diplegia will often have some
asymmetry, and the lower extremity will often be slightly shorter on
the side with greater involvement. The patient is then asked to bend
forward at the waist, as if he is touching his toes, and the examiner
looks for a rib or lumbar prominence, which may be associated with a
spinal deformity.
examination. He is asked to pick up an object so that the clinician can
determine whether there is a hand preference, and whether he can lift
the object with either hand. Grip strength is tested by having the
patient squeeze the clinician’s index and long fingers of both hands at
the same time. Pinch strength is tested by having the patient pick up a
pen between the index finger and the thumb. Stereognosis is tested by
placing a known object, such as a coin, into the hand, and asking the
patient to identify the object without looking at it. The shoulders,
elbows, forearms, and wrists are taken through a full range of motion,
to determine whether there are any contractures. A patient with spastic
cerebral palsy may have an adduction contracture of the shoulder, a
flexion contracture of the elbow, a pronation contracture of the
forearm, a flexion contracture of the wrist, and a thumb-in-palm
deformity in the hand.
lower extremities. The hips are passively taken through a full range of
motion. Patients with spastic cerebral palsy will often have flexion
and adduction contractures of the hips. The Thomas test or the prone
hip extension test (Staheli test) can be used to examine for a hip
flexion contracture. The Thomas test is
performed by flexing one hip completely, to flatten the lumbar spine,
and observing the amount of residual flexion of the other hip. The
residual flexion represents the hip flexion contracture (Fig. 5.23A). The prone hip extension test
is performed by placing the patient prone with the lower extremities
flexed over the end of the table. This position flattens the lumbar
spine, leveling the pelvis. One hip remains flexed at 90 degrees; the
clinician gradually extends the other hip while palpating the pelvis (20). As soon as pelvic motion is detected, the amount of residual hip flexion represents the flexion contracture (Fig. 5.23B). A flexion contracture in a patient with spastic cerebral palsy is often
secondary to an iliopsoas contracture but may also be secondary to a rectus femoris contracture. The Ely test
is used to test the rectus femoris muscle. The Ely test is performed in
the prone position with the hip extended. The knee is gradually flexed
to 130 degrees. If the hip spontaneously flexes, causing the buttocks
to rise off the table, it indicates a contracture of the rectus femoris
component of the quadriceps muscle. A positive Ely test is an accurate
predictor of rectus femoris dysfunction during gait (21).
 |
|
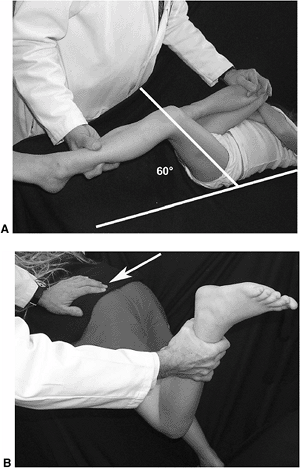
Figure 5.23 A:
The Thomas test is performed by flexing one hip to the knee-chest position, and observing the amount of residual flexion of the other hip. Maximum flexion of the one hip flattens the lumbar spine leveling the pelvis, allowing gravity to extend the hip that is being examined. Any residual flexion represents the hip flexion contracture (60 degrees in this patient). B: The prone hip extension test (Staheli test) is performed in the prone position with the lower extremities flexed over the end of the table. This position flattens the lumbar spine, leveling the pelvis. One hip remains flexed at 90 degrees; the clinician gradually extends the other hip while palpating the pelvis (arrow). As soon as pelvic motion is detected, the amount of residual hip flexion represents the flexion contracture. |
with the patient lying in either the supine or the prone position, but
the author prefers the prone position (Figs. 5-6 and 5-7).
Patients with spastic cerebral palsy often have increased anteversion
of the proximal femur, which causes an increase in internal rotation
and a decrease in external rotation of the hips. In contrast, patients
with developmental coxa vara often have a retroversion deformity of the
proximal femur, which causes an increase in external rotation and a
decrease in internal rotation of the hips.
degrees, the hips should abduct symmetrically to at least 75 degrees.
Limited abduction, particularly if associated with flexion contracture,
may indicate hip subluxation or dislocation. The Phelps-Baker test
is used for determining the hamstring’s contribution to the hip
adduction contracture. This test is performed with the patient in the
prone position. The amount of hip abduction with the knees flexed is
compared to that with the knees extended. The extent to which abduction
is decreased with the knees extended represents the contribution of the
medial hamstrings to the adduction contracture. The Ober test is used to examine for a hip abduction contracture. The Ober test
for the right hip is performed in the lateral decubitus position with
the left lower extremity in the knee–chest position. The right hip is
adducted with the knee extended and with the knee flexed (22).
The right lower extremity should easily adduct to the table, and any
loss of adduction represents a hip abduction contracture. The
difference between the abduction contracture with the knee flexed,
compared with the knee extended, represents the tensor fascia lata
contribution to the hip abduction contracture. A patient with spastic
cerebral palsy will usually develop an adduction contracture of the
hip, whereas a patient with poliomyelitis will usually develop an
abduction contracture.
patient supine on the examination table. The range should be from 0
degrees to 130 degrees. A flexion contracture may be caused by a
hamstring contracture. A hamstring contracture is detected by
performing a straight-leg-raising test (Fig. 5.24A).
Straight-leg-raising should normally be possible up to anywhere from 60
degrees to 90 degrees. Limited straight-leg-raising often indicates a
contracture of the hamstring muscles, but it may be associated with a
neurologic problem such as a tethered spinal cord. A hamstring
contracture can also be detected by measuring the popliteal angle. To
measure the popliteal angle, the hip is flexed to 90 degrees and the
knee is gradually extended to the first sign of resistance. The angle
between the thigh and the calf is the popliteal angle (Fig. 5.24B). This popliteal angle should be distinguished from its complement, which is also called the popliteal angle by some investigators (7).
Elmer et al. chose to call the angle between the calf and the thigh the
popliteal angle, as originally described by Amiel-Tison, because they
believed it was a more appropriate description of the angle subtended
by the popliteal fossa (23).
 |
|
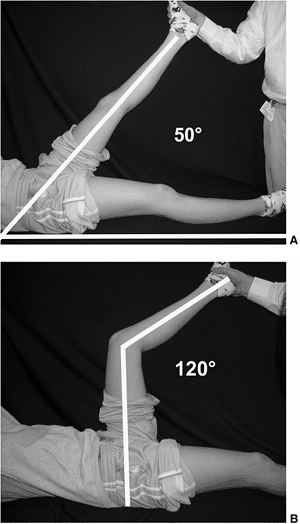
Figure 5.24 A:
With the patient supine, the clinician gradually raises one lower extremity by flexing the hip with the knee in extension. The straight-leg-raising test measures the angle between the raised limb and the tabletop (50 degrees in this patient). B: With the patient supine, the clinician gradually flexes the hip and knee to 90 degrees. The knee is gradually extended to the first sign of resistance. The angle between the thigh and the calf is the popliteal angle (120 degrees in this patient). This popliteal angle should be distinguished from its complement, which is also called the popliteal angle by some investigators. |
dorsiflex to 30 degrees and plantarflex to 40 degrees, and the hindfoot
should be supple. When testing dorsiflexion of the ankle it is
important to supinate the hindfoot, locking the subtalar joint, because
hypermobility in the subtalar and tarsal joints can mask an equinus
contracture. The decrease in the extent of ankle dorsiflexion with the
knee extended, compared to that with the knee flexed, represents the
contribution of the gastrocnemius muscles to the equinus contracture;
this is termed the Silverskiold test (24).
This patient has cerebral palsy with asymmetric spastic diplegia and
may have a neuromuscular hip subluxation or dislocation, so an
anteroposterior pelvis radiograph is recommended.
that the boy seemed to walk oddly, but he definitely began limping on
the right side shortly after his fifth birthday. He has been limping
for 3 months and the limp is worse at the end of the day when he is
tired. He never complains of pain and she has not noticed any swelling.
pattern. He walks with an obvious limp on the right, but he spends an
equal amount of time in stance phase on both limbs, indicating a
painless limp. The differential diagnosis of a painless limp is
different from that of a painful (antalgic) limp. A painless limp could
be caused by DDH or a limb-length discrepancy, whereas a painful limp
could be caused by Legg-Calvé-Perthes disease or transient synovitis.
If the patient had bilateral DDH, the limp may be subtle with a
waddling gait pattern associated with increased lumbar lordosis.
on the iliac crests and notes that the left iliac crest is 2 cm higher
than the right, indicating a limb-length discrepancy, with the left
lower extremity longer than the right. When the child is asked to stand
on the left leg, the right iliac crest elevates 5 mm. When he is asked
to stand on the right leg, the left iliac crest drops 15 mm. The
inability of the hip abductor muscles to hold the pelvis with
single-limb support is termed a positive Trendelenburg test (Fig. 5.16).
Because the patient has no pain, the positive Trendelenburg test
indicates weakness of the hip abductor muscles. In a patient with
developmental coxa vara, the decrease in the neck-shaft angle decreases
the articulotrochanteric distance between the femoral head and the
greater trochanter. This disrupts the normal length–tension relation of
the abductor muscles, causing weakness.
on the left, and 120 degrees on the right. The Thomas test reveals
extension to 0 degrees on the left and a flexion contracture of 25
degrees on the right (Fig. 5.23A). Abduction is
to 80 degrees on the left and to 50 degrees on the right, and adduction
is to 30 degrees bilaterally. Internal rotation is to 60 degrees on the
left and 0 degrees on the right, and external rotation is to 60 degrees
on the left and to 70 degrees on the right (Figs. 5-6 and 5-7).
These changes in range of motion may be secondary to a retroversion
deformity of the proximal femur, often seen in a patient with
developmental coxa vara or slipped capital femoral epiphysis (SCFE).
Because the latter condition typically occurs during puberty, it would
be unlikely in a 5-year-old boy unless he had an underlying endocrine
disorder.
a patient with a limb-length discrepancy is to place him in the prone
position with the hips in full extension and the knees flexed to 90
degrees. In this patient the right knee is 2 cm shorter than the left,
indicating that the entire limb-length discrepancy is secondary to a
short right femur (Fig. 5.25A). The tibial lengths are measured by comparing the levels of the heels (Fig. 5.25B).
These findings are consistent with the diagnosis of developmental coxa
vara, so an anteroposterior pelvis radiograph is recommended.
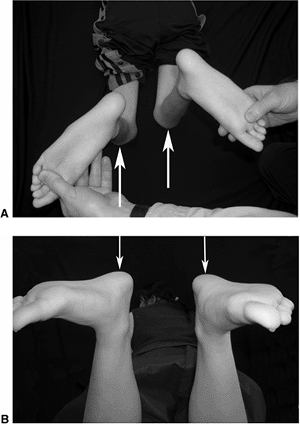 |
|
Figure 5.25 A:
To measure femoral lengths in the prone position, the hips are extended and the knees are flexed to 90 degrees. The difference in the length of the thighs (arrows) represents the discrepancy in the lengths of the femurs. B: To measure tibial lengths in the prone position, the hips are extended and the knees are flexed to 90 degrees. The difference in the heights of the heels (arrows) represents the discrepancy in the lengths of the tibias. |
she had scoliosis. She was given a note to take home, recommending an
evaluation for scoliosis. The pediatrician detected shoulder asymmetry
and a rib prominence and referred her for evaluation. The patient had
never noticed any spinal deformity and is active in sports. She
occasionally gets pain in the lower back, but this does not interfere
with her activities. She denies having any problems with bowel or
bladder function, and she first began menses 1 month ago. The family
history reveals that she has two maternal cousins with scoliosis, one
of whom required surgical correction of the spinal deformity. The
mother states that the girl has grown 5 cm (2 in.) in the last 6
months. She is 178 cm (5 ft 10 in.) tall; her mother is 175 cm (5 ft 9
in.) tall, and her father is 188 cm (6 ft 2 in.) tall.
activities is common in patients with scoliosis. Ramirez et al.
evaluated 2442 patients with idiopathic scoliosis and reported that 560
(23%) had back pain at the time of presentation, and an additional 210
(9%) had back pain during the period of observation (25).
In contrast, a history of severe back pain associated with rapid
progression of the scoliosis, weakness or sensory changes, bowel or
bladder complaints, or balance problems is not typical in a patient
with idiopathic scoliosis, and suggests a possible intraspinal problem.
standing. The trunk’s shape and balance are observed from behind. The
clinician looks for any asymmetry in the neck, levels of the shoulders,
levels of the scapular spines, prominence of the scapulae, surface
shape of the rib cage, or the contour of the waist. A patient with
lumbar scoliosis that is convex to the left will have asymmetry of the
waist, with the left side being straight and the right side contouring
inward, giving the appearance of a limb-length discrepancy. The iliac
crest is more accentuated on the concave side and the patient often
interprets this as the right hip sticking out. The skin is observed for
any café-au-lait marks or freckling in the axilla that may indicate
neurofibromatosis. If the patient is tall and has long prominent
fingers (arachnodactyly), it may indicate Marfan syndrome.
If the patient is standing erect and the spine is compensated, the head
should be centered directly over the pelvis, and a plumb bob suspended
from the spinous process of the seventh cervical vertebra should fall
directly over the gluteal cleft (Fig. 5.26). If
the spine is decompensated, the distance from the plumb bob to the
gluteal cleft is recorded in centimeters. The posterior iliac dimples
in stance are observed to determine whether they are symmetric and
level, indicating equal limb lengths. The clinician’s hands are placed
on the iliac crests to determine whether the pelvis is level, or
whether there is a limb-length discrepancy (Fig. 5.27).
If there is a limb-length discrepancy, the difference in the levels of
the iliac crests is recorded in centimeters. A limb-length discrepancy
causes a compensatory postural scoliosis deformity, convex toward the
shorter limb, to balance the head over the pelvis. This postural
scoliosis will correct when the limb-length discrepancy is corrected by
placing an appropriate sized wooden block under the foot of the short
leg to equalize the limb lengths. The spinous processes are palpated to
determine whether there is any focal tenderness, and the patient is
asked to arch her back, to see whether it causes discomfort. Patients
who have a spondylolysis will often have discomfort when the spinous
process of the involved vertebra is palpated, or when they attempt to
arch their backs.
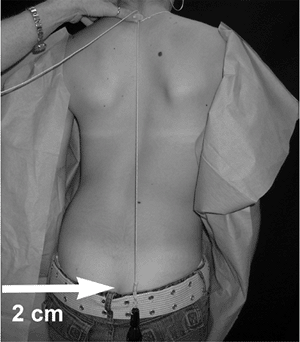 |
|
Figure 5.26
If the spine is compensated, the head should be centered over the pelvis and a plumb bob suspended from the spinous process of the seventh cervical vertebra should fall directly over the gluteal cleft. If the spine is decompensated, the distance from the plumb bob to the gluteal cleft is recorded in centimeters (2 cm to the right in this patient). |
the clinician observes the spine to determine whether it is supple and
flexes symmetrically. If the patient bends to one side instead of
straight ahead, it may indicate a hamstring contracture associated with
a spondylolisthesis, disk herniation, or neoplasm. As the patient bends
forward, if the spine flexes excessively in the thoracic area, it may
indicate Scheuermann disease.
When the patient is in the forward-bending position, the clinician
looks for any asymmetry of the trunk, and measures the angle of trunk
rotation, or rib prominence, using a scoliometer (Fig. 5.28) (26).
The rib prominence reflects the rotational component of the scoliosis
deformity that occurs in the axial plane. The most common type of
scoliosis is a convex right thoracic curve, in which the vertebrae
rotate into the convexity of the curve, causing the ribs to appear more
prominent posteriorly on the patient’s right side. The ribs are also
more prominent anteriorly on the patient’s left side, which may cause
breast asymmetry. While the patient is in the forward-bending position,
she is asked to bend to the right and left to assess the flexibility of
the scoliosis.
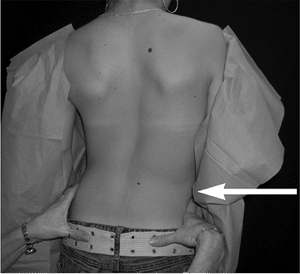 |
|
Figure 5.27
The patient is observed from behind, looking for any asymmetry in the neck, levels of the shoulders, levels of the scapular spines, prominence of the scapulae, surface shape of the rib cage, contour of the waist, and levels of the iliac crests (arrow). |
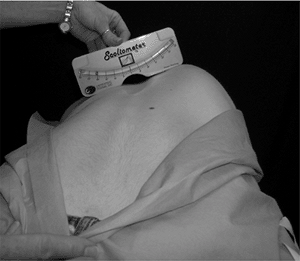 |
|
Figure 5.28
The Adams forward-bending test is performed by asking the patient to place her hands together in front of her and bend forward at the waist, as if she were touching her toes. As the patient bends forward, the clinician observes the spine to determine whether it is supple and flexes symmetrically. Once the patient has bent forward so that the spine is parallel to the floor, the clinician looks for asymmetry of the trunk and measures the angle of trunk rotation using a scoliometer. |
disorders (muscular dystrophy) and with spinal cord anomalies
(syringomyelia). A thorough neurologic examination is essential to rule
out a neuromuscular disorder. With the patient in a standing posture,
the Romberg sign is elicited by asking her
to place her feet close together. She is then asked to close her eyes,
while the clinician looks for any sway or instability. A patient with
cerebellar ataxia will sway or move her feet to maintain balance. This
test may be important because scoliosis is frequently seen in patients
with Friedreich ataxia. An evaluation of
the strength, sensation, and reflexes of the upper and lower
extremities is essential in order to rule out an occult neuromuscular
disorder. A straight-leg-raising test is performed to look for
hamstring tightness or radiculopathy (Fig. 5.24A).
Straight-leg raising to less than 40 degrees may indicate tight
hamstrings associated with a spondylolisthesis, disc herniation, or
neoplasm. The abdominal reflexes are tested by gently stroking the side
of the abdomen; the umbilicus should deviate toward the stimulus. Any
asymmetry of the abdominal reflexes is important because it may
indicate an intraspinal problem.
assess the maturity of the patient, because the risk of curve
progression is higher in young patients and in patients with larger
spinal curves (27). The risk of progression is
highest when the patient is at her peak growth velocity. The peak
growth velocity typically occurs 12 months before the onset of menses.
Most investigators recommend radiographs if the angle of trunk rotation
is greater than 7 degrees; scoliosis posteroanterior and lateral
radiographs are recommended, to be taken with a tube-to-film distance
of 183 cm (72 in.) on a 91 cm (36 in.) cassette.
ago when she developed low back pain after a soccer game. Over the last
3 months the pain has increased to such an extent that she is unable to
play for more than 5 minutes. The pain is relieved by rest and
aggravated by playing soccer. She describes the pain as being in the
lower back and worse on the right side. The pain does not radiate into
the buttocks or lower extremities.
and noting she has a normal heel-toe gait pattern. A patient with lower
back pain may have subtle changes in her gait, which can be detected by
an astute observer. A patient with spondylolisthesis may have a
hamstring contracture that prevents full extension of the knee in
terminal swing, causing a decrease in step length and stride length.
Step length is the distance from the foot strike of one foot to the
foot strike of the other foot. Stride length is the distance from one
foot strike to the next foot strike by the same foot. Therefore, each
stride length comprises one right and one left step length (28).
In a patient with severe spondylolisthesis, the hamstring contractures
may be so severe that the patient ambulates with a toe-toe gait pattern.
shape and balance are observed from behind. The clinician looks for any
asymmetry in the neck, scapulae, shoulders, rib cage, waist, or hips (Fig. 5.27).
Low back pain can cause muscle spasms on the side that has the pain,
causing a scoliosis convex to the opposite side. The paraspinal muscles
are palpated to determine whether they are in spasm. An osteoid osteoma
involving the posterior elements of the spine may be associated with a
painful scoliosis. The patient describes increased pain when she arches
her back. Hyperextension of the lumbar spine increases the pressure on
the posterior elements, causing a patient with spondylolysis to
experience increased pain with this maneuver. This test is important
because most patients with back pain will not experience any increase
in pain with this maneuver. The spinous processes of the lumbar
vertebrae are palpated to determine whether palpation causes
discomfort. A patient with a spondylolysis at L5 will often experience
pain with palpation of the spinous process of L5. Palpation increases
the pressure on the pars interarticularis, reproducing the pain in a
patient with a spondylolysis.
examinations of the upper and lower extremities are performed. A disc
protrusion affecting the L5 nerve root may compromise the function of
the extensor hallucis longus and posterior tibial muscles, and can be
detected from weakness in dorsiflexion of the great toe, weakness in
inversion, and a decreased posterior tibial tendon reflex. An L5 disc
protrusion may also cause sensory changes over the dorsal and medial
aspects of the foot, particularly in the web space between the first
and second toes. A disc protrusion affecting the S1 nerve root could
compromise the functioning of the gastrocsoleus muscle, and can be
detected from weakness in the gastrocsoleus muscle and a decreased
Achilles tendon reflex. Occasionally it is difficult to elicit the
Achilles tendon reflex. This problem can be resolved by having the
patient kneel on a chair with the feet dangling over the edge. In this
position, the reflex hammer typically elicits a good ankle jerk. A
patient with an S1 disc protrusion may have sensory changes over the
plantar and lateral aspects of the foot.
Limited straight-leg raising may indicate hamstring tightness
associated with spondylolisthesis or nerve root irritation from disc
herniation or neoplasm. Young athletes with spondylolysis will often
experience increased pain while playing soccer. Debnath et al.
evaluated 22 young athletes who had surgery for low back pain
associated with a spondylolysis; 13 (59%) of them were soccer players (29). This patient’s pain may be secondary to a spondylolysis, so radiographs of the lumbar spine are recommended.
ago when he developed pain in his left knee. Several weeks later, his
mother noticed he was limping on his left leg. The pain and limping
have increased and are aggravated by activity. There is no history of
injury, and he has not had any swelling in the knee. The personal and
social history reveals that he has always been overweight.
left knee pain and a limp should prompt the clinician to consider the
diagnosis of SCFE. Most children with SCFE are obese. Obesity is also
associated with femoral retroversion, with anteversion averaging only
0.4 degrees in obese adolescents, as compared to 10.6 degrees in
adolescents of average weight (30). Obesity and
femoral retroversion increase the mechanical shear stresses across the
physis, increasing the risk of slip progression in a patient with SCFE.
lb, greater than the ninety-fifth percentile for weight for his age).
His gait pattern shows that he ambulates with an antalgic (painful)
limp on the left lower extremity. He leans his head and trunk to his
left during the stance phase. The shifting of weight over the left
lower extremity in stance phase decreases the reactive forces in the
hip joint, and is termed a Trendelenburg gait pattern.
He has a shortened stance phase on the left, and his foot-progression
angle is 10 degrees of external rotation on the right and 35 degrees of
external rotation on the left (Fig. 5.4). With
the patient in the standing position, the shoulders, scapular spines,
and spine are observed from behind, and no asymmetry is noted. The
clinician’s hands are placed on the iliac crests, and the left iliac
crest is noted to be 1 cm lower than the right, indicating a
limb-length discrepancy (Fig. 5.27). In single-leg stance, he is noted to test positive with the Trendelenburg test (Fig. 5.16).
of the left knee. A patient with SCFE may complain of knee pain, rather
than hip, thigh, or groin pain. This phenomenon occurs because the
obturator, sciatic, and femoral nerves that supply the hip also supply
the knee. When a patient with hip pathology complains of knee pain, it
is a classic example of referred pain. The range of motion of his
hips
reveals flexion to 130 degrees on the right and to 120 degrees on the
left. When the right hip is flexed to the knee–chest position, it
remains in neutral rotation, but when the left hip is flexed it
spontaneously goes into abduction and external rotation. This abduction
and external rotation occurs because a patient with SCFE has a
retroversion deformity of the proximal femur. The femoral neck
displaces anteriorly through the physis, creating apex–anterior
angulation of the proximal femur (31).
Abduction is to 70 degrees on the right and to 50 degrees on the left.
Internal rotation is to 20 degrees on the right and to minus 20 degrees
on the left (Fig. 5.6). External rotation is to 70 degrees on the right and to 85 degrees on the left (Fig. 5.7).
These physical findings indicate a retroversion deformity of the left
femoral neck, with an increase in external and a decrease in internal
rotation of the left hip. An obese adolescent boy who displays these
physical findings has a high probability of having SCFE, so
anteroposterior and frog-lateral pelvis radiographs are recommended.
when she collided with another player in a soccer game and landed
directly on her left knee. She had moderate swelling of the knee that
resolved in 7 days. Her knee felt better after soccer season, but the
pain recurred when she began playing basketball. The pain is aggravated
by sitting in the back seat of the car with the knee flexed. The pain
is also worse when going up and down stairs.
syndrome will often experience pain when sitting with the knee flexed
for a prolonged period of time. This finding has been termed a positive
movie sign, from sitting for several hours
in the movie theater. Patients with anterior knee pain will often have
increased pain going up and down stairs. The patient may note catching
and giving way of the knee, but true locking is unusual.
injured knee with the uninjured knee looking for loss of the dimples on
either side of the patella that would indicate a large effusion (Fig. 5.29).
If the patient does not have a large effusion, the suprapatellar pouch
is milked from medial to lateral, moving any fluid into the lateral
compartment of the knee. The lateral side is then milked while
observing for a fluid wave on the medial side. Visualizing the fluid
wave is the most sensitive test to detect a trace effusion. In
describing the pain, the patient points to the medial and lateral sides
of the patella. She has tenderness to palpation on the undersurface of
the patella. This is elicited with the knee in extension, by gently
pushing the patella laterally to palpate the lateral facet, and
medially to palpate the medial facet. A patient with anterior knee pain
may have a contracture of the lateral retinaculum. This is detected by
the inability to elevate the lateral margin of the patella when tilting
the patella medially and laterally during the tilt test. If the pain is
caused by pressure in the patellofemoral joint, it can be reproduced by
the patellar inhibition test. This test is
performed in the supine position with the knee extended. The patient is
asked to do a straight-leg raise while the clinician holds the patella,
preventing it from ascending along the femoral sulcus (Fig. 5.30).
This maneuver increases the pressure between the patella and the
femoral sulcus, reproducing the pain in a patient with patellofemoral
pain syndrome. If the pain is caused by patellofemoral instability it
can be reproduced by the patellar apprehension test. This test is performed with the
knee flexed to 30 degrees and the clinician gently pushing the patella laterally (Fig. 5.31).
If the patient immediately contracts her quadriceps to prevent the
patella from subluxating, it indicates a positive test, which often
occurs in patients who have previously had a subluxation or dislocation
of the patella.
 |
|
Figure 5.29 The uninjured right knee has “dimples” (white arrows) on either side of the patella. The injured left knee has a large effusion that stretches out the dimples (black arrows).
|
 |
|
Figure 5.30 The patellar inhibition test is performed with the patient supine and the knee in extension. The clinician holds the patella (arrow),
inhibiting it from ascending along the femoral sulcus, while the patient performs a straight-leg raise. This maneuver increases the forces in the patellofemoral joint, causing discomfort in a patient with a patellofemoral disorder. |
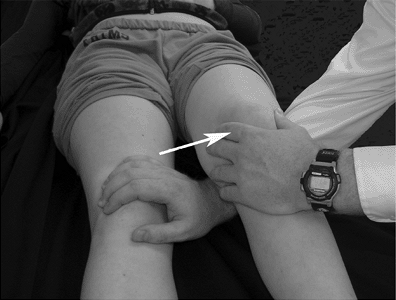 |
|
Figure 5.31
The patellar apprehension test is performed with the patient supine and the knee flexed to 30 degrees. The clinician gently pushes the patella laterally (arrow). If the patient experiences apprehension, it indicates patellofemoral instability. |
may be more susceptible to lateral subluxation of the patella. This
syndrome includes a combination of internal femoral torsion and
external tibial torsion, and causes the patellae to face in (squinting patellae)
when the feet are pointing straight ahead. Patients with miserable
malalignment syndrome may have knee pain with an increased Q-angle. The
Q-angle is the angle formed between a line connecting the anterior
superior iliac spine with the center of the patella and a line
connecting the tibial tubercle with the center of the patella (Fig. 5.32).
The Q-angle should be measured with the knee in 30 degrees of flexion
so that the patella is in contact with the femoral sulcus. Patients
with an increased Q-angle may have knee pain because of lateral
tracking of the patella in the femoral sulcus. The maltracking can be
detected by observing the patella as the patient actively extends the
knee. Sitting with the knees flexed to 90 degrees over the side of the
table, the patient is asked to gradually extend the knee. The patella
is observed to remain in the femoral sulcus as it ascends along the
axis of the femur, but as the knee reaches full extension, the patella
deviates laterally like an upside-down J. This is termed a positive J sign, and if the patient has patellofemoral instability, the patella may subluxate with this maneuver.
full range of motion from 0 degrees to 135 degrees. The pain is often
described as being circumferential around the patella and there is
usually no evidence of an effusion. A patient with Osgood-Schlatter disease will have pain over the tibial tubercle, and a patient with Sinding-Larsen-Johansson disease (jumper’s knee) will have pain at the inferior pole of the patella (32).
A patient with osteochondritis dissecans will have pain elicited by
direct palpation over the articular surface of the medial femoral
condyle. The pain can also be reproduced by flexing the knee to 90
degrees, internally rotating the tibia, then gradually extending the
knee. As the knee approaches 30 degrees of flexion, a patient with
osteochondritis dissecans involving the medial femoral condyle will
experience pain that is relieved by externally rotating the tibia. This
phenomenon is termed a positive Wilson test (33).
A patient with a torn meniscus will typically have pain at the joint
line. A torn meniscus can be evaluated by flexing the knee to 135
degrees, applying a valgus stress, and gradually extending the knee
while externally rotating the tibia. Pain and a palpable “clunk,”
elicited with this maneuver, are secondary to a torn meniscus, and are
termed a positive McMurray test. With the
patient prone, pressure is applied to the heel, loading the knee in
compression, while the tibia is internally and externally rotated. A
patient with a torn meniscus will experience pain with this maneuver
when the meniscus is trapped between the tibia and the femur. This test
is termed a positive Apley test. With the
patient supine and the knee extended, the clinician elevates the foot,
then drops it several inches, causing the knee to hyperextend, flex,
then hyperextend again. Most patients will not have discomfort with
this maneuver, but if there is a torn meniscus, the maneuver causes
pain and a reflex contraction of
the hamstrings preventing the knee from hyperextending. This inability to hyperextend the knee is termed a positive bounce test.
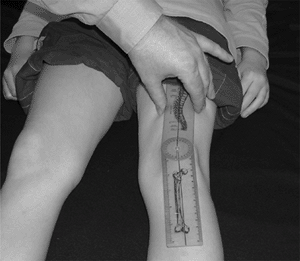 |
|
Figure 5.32
The Q-angle is the angle formed between a line connecting the anterior superior iliac spine with the center of the patella and a line connecting the tibial tubercle with the center of the patella. The Q-angle is measured with the knee in 30 degrees of flexion, so that the patella is in contact with the femoral sulcus. |
typically have any ligamentous instability, these important knee
stabilizers are examined. With the patient in the supine position and
the knees flexed to 90 degrees, the clinician looks for a posterior sag
of the tibia, which is often seen in a patient with a
posterior-cruciate-ligament-deficient knee. A torn posterior cruciate
ligament can be elicited by the quadriceps active test (34).
This test is performed with the patient in the supine position and the
knee flexed to 90 degrees. The patient is asked to slide her foot down
the table, while the clinician prevents the foot from moving. The force
of the quadriceps muscle will pull the tibia anteriorly, reducing the
posterior subluxation in a patient with a
posterior-cruciate-ligament-deficient knee (Fig. 5.33). An anterior-cruciate-ligament-deficient knee is evaluated by performing the anterior drawer test.
This test is performed with the patient supine and the knee flexed to
90 degrees. The foot is stabilized by the clinician’s thigh, while the
tibia is pulled forward at the knee. The clinician should feel a solid
stop after 3 to 5 mm of translation of the tibia on the femur,
indicating an intact anterior cruciate ligament (Fig. 5.34).
It is important to palpate the hamstring tendons while performing this
test because a torn anterior cruciate ligament may not be detected if
the patient contracts the hamstring muscles during the test. A more
sensitive test to detect an anterior-cruciate-ligament-deficient knee
is the Lachman test. This test is
performed with the patient supine and the knee flexed to 30 degrees.
The femoral condyles are held in one hand, while the tibia is pulled
anteriorly and pushed posteriorly with the other hand (Fig. 5.35).
Subluxation greater than 5 mm, without a solid end point, indicates
anterior cruciate ligament insufficiency. An
anterior-cruciate-ligament-deficient knee can also be detected by the pivot-shift test.
This test is performed with the patient supine and the knee in
extension. A valgus and internal rotation force is applied to the leg,
and in an anterior-cruciate-ligament-deficient knee, this force will
cause
the tibia to subluxate anteriorly. As the knee is flexed, when the
iliotibial band crosses the axis of the knee joint, the tibia rapidly
shifts to its normal position, and the clinician can feel a pivot shift.
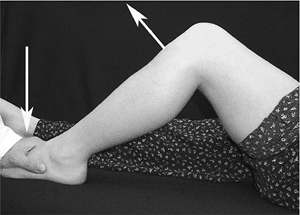 |
|
Figure 5.33
The quadriceps active test is performed with the patient supine and the knee flexed to 90 degrees. In this position, the tibia is subluxated posteriorly in a patient with a posterior-cruciate-ligament-deficient knee. The patient is asked to slide her foot down the table while the clinician prevents the foot from moving (down arrow). The force of the quadriceps muscle pulls the tibia anteriorly (up arrow), reducing the posterior subluxation. |
 |
|
Figure 5.34
The anterior drawer test is performed with the patient supine and the knee flexed to 90 degrees. The foot is stabilized by the clinician’s thigh, while the tibia is pulled forward at the knee (arrow). The clinician should feel a solid stop after 3 to 4 mm of translation, indicating an intact anterior cruciate ligament. It is important to palpate the hamstring tendons to be sure the hamstring muscles are relaxed, because contracting hamstrings can mask an anterior-cruciate-ligament-deficient knee. |
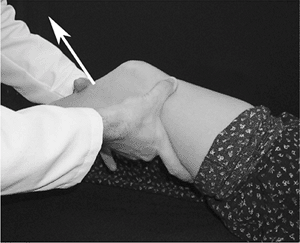 |
|
Figure 5.35
The Lachman test is performed with the patient supine and the knee flexed to 30 degrees. To test the left knee, the femoral condyles are held with the right hand, while the tibia is pulled anteriorly with the left hand (arrow). Anterior subluxation greater than 5 mm, without a solid end point, indicates an anterior-cruciate-ligament-deficient knee. |
just under the skin, so an injury to these ligaments is associated with
pain on palpation over the ligament. By gently palpating the uninjured
side and comparing it with the injured side, the clinician can often
pinpoint the location of the injury. The medial and lateral collateral
ligaments are tested with the knee in 30 degrees of flexion because
varus or valgus instability can be masked by intact cruciate ligaments
with the knee in extension. The medial joint line is palpated with a
finger while the examiner applies a valgus stress to the knee, and the
lateral joint line is similarly palpated while the examiner applies a
varus stress to the knee. The amount of joint line opening is recorded
in millimeters, and 0 to 5 mm of opening with a solid end point is
considered to be a normal amount of ligamentous laxity. Medial and
lateral collateral ligament sprains are classified according to the
amount of opening of the joint space on physical examination. A grade I
sprain shows pain over the ligament and opens 0 to 5 mm, a grade II
sprain opens 6 to 10 mm, and a grade III sprain opens more than 10 mm.
This patient has anterior knee pain secondary to a direct blow to the
patella when she fell on her knee.
foot 2 years ago. Six months later he developed similar symptoms in the
right foot. He describes several instances of the left ankle giving out
while he was walking. The last episode occurred 1 month ago, when he
was walking down the stairs and the left ankle gave out, causing
swelling over the lateral aspect of the ankle. The swelling resolved
over the next few days. The pain under both arches has worsened over
the last year and is aggravated by exercise. His mother states that he
has always had high arches. There is a family history of this
condition, with his father and paternal grandfather having high arches.
with a neuromuscular disorder until proven otherwise. The most common
neurologic disorder associated with pes cavus is Charcot-Marie-Tooth disease.
The inheritance pattern for Charcot-Marie-Tooth disease is autosomal
dominant, so the clinician asks about the high-arched feet in the
family. Both the father and grandfather had high arches, but neither
had any medical problems.
heel-toe pattern, but walks on the lateral side of the foot with
hindfoot varus. In the standing posture, he has high-arched feet, and
he points to the medial arches of both feet when describing the pain.
He has painful callosities under the metatarsal heads, particularly the
first metatarsal. He also has painful callosities under both heels, at
the bases of the fifth metatarsals, and over the dorsal surfaces of the
proximal interphalangeal joints of the lateral toes. The lateral toes
have mild claw-toe deformities. Detailed motor, sensory, and reflex
examinations of the upper and lower extremities reveal no problems. The
longitudinal arch of each foot is elevated, shortening the medial
border of the foot, creating a concave appearance. The lateral side of
each foot is convex, lengthening the lateral border of the foot,
creating a bean-shaped deformity. There are callosities over the bases
of the fifth metatarsals, and the first metatarsal is plantarflexed
bilaterally. The average foot has a “tripod” structure with
weight-bearing balanced between the heel, first metatarsal head, and
fifth metatarsal head. If the forefoot develops a pronation deformity,
with plantarflexion of the first metatarsal, weight-bearing will force
the hindfoot into varus. The flexible hindfoot varus deformity will
eventually become a structural deformity as the soft tissues of the
subtalar joint contract. The flexibility of the hindfoot deformity is
important when contemplating surgical reconstruction of a cavus foot.
The forefoot contribution to the hindfoot varus deformity is determined
by the Coleman block test (35).
This test is performed with the patient standing with his back facing
the clinician, and the amount of hindfoot varus is noted (Fig. 5.36A).
A 2 to 3 cm block is placed under the lateral aspect of the foot and
heel, allowing the first metatarsal to hang freely, negating any effect
it may have upon the hindfoot by eliminating the tripod mechanism (Fig. 5.36B).
The amount of correction of the hindfoot deformity, when standing on
the block with the first metatarsal on the floor, represents the
forefoot contribution to the hindfoot varus deformity. A similar test
can be performed with the patient prone and the knee flexed to 90
degrees. The foot is dorsiflexed by applying pressure to the lateral
border of the foot, allowing the first metatarsal to remain
plantarflexed, and the amount of correction of the hindfoot varus is
observed. These tests are crucial in preoperative planning, because a
flexible hindfoot will correct when the forefoot deformity is
corrected. This patient has idiopathic pes cavus, so standing
anteroposterior, lateral, and axial radiographs are recommended.
after swimming practice 3 months ago. The pain is aggravated by
swimming freestyle (crawl) and relieved by rest. He describes the pain
as an ache in the front of the left shoulder. He has never noticed any
swelling and he cannot recall any injury. He has been a competitive
swimmer since he was 6 years old, and currently practices 6 days a
week. He has taken anti-inflammatory medication with some relief of his
symptoms.
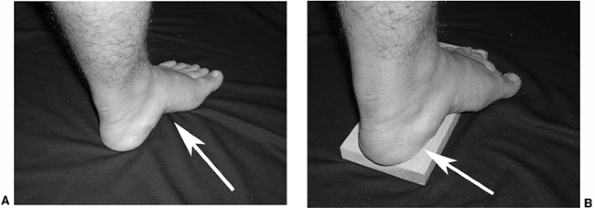 |
|
Figure 5.36 A: This foot has a rigid pes cavus deformity with a high longitudinal arch (arrow), hindfoot varus, and a plantarflexed first metatarsal. B:
The Coleman block test evaluates the forefoot contribution to the hindfoot varus deformity. The patient stands with the lateral aspect of the foot and heel on a 2 to 3 cm block, allowing the first metatarsal to hang freely, negating any effect it may have upon the hindfoot by eliminating the tripod mechanism. The amount of correction of the hindfoot varus deformity (arrow) represents the forefoot contribution to the hindfoot varus deformity. |
is having difficulty with shoulder pain will often have an overuse
injury caused by excessive or improper training. Activity modification,
such as cross training or correction of a simple training error, may
resolve his symptoms. It is important to monitor a patient with an
overuse injury, because if the symptoms are not resolving with activity
modification, there may be a serious underlying problem.
reveals no muscle wasting, swelling, or deformity. Palpation reveals
tenderness over the supraspinatus tendon and the anterior aspect of the
acromion. A patient with imbalance of the rotator cuff muscles may have
impingement with tendonitis involving the supraspinatus tendon. The
range of motion of the shoulders reveals elevation to 180 degrees
bilaterally, external rotation with the arm at the side to 70 degrees
bilaterally, and internal rotation to the point where the thumbs touch
the spinous process of T4 on the right, and T9 on the left. The limited
internal rotation on the left side indicates tight posterior
structures, a common finding in patients who do overhead athletics.
Muscle strength testing of shoulder flexion, abduction, internal, and
external rotation are graded from 0 to 5, according to the scale of the
Medical Research Council (Table 5.5) (36).
A rotator cuff imbalance is often seen in patients with weakness of the
periscapular muscles, including the rhomboids, serratus anterior,
subscapularis, and trapezius muscles.
|
TABLE 5.5 GRADING OF MUSCLE STRENGTH USING THE MEDICAL RESEARCH COUNCIL RATING SYSTEM
|
||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
with multidirectional instability, or rotator cuff tendonitis with
impingement. There are several tests to detect instability and
impingement. Ligamentous laxity with instability can be evaluated by
palpating glenohumeral translation. With the patient seated, the
clinician evaluates the amount of glenohumeral translation by
stabilizing the scapula and clavicle with one hand while pushing and
pulling the proximal humerus in the anterior and posterior directions
with the other hand. The amount of glenohumeral translation is measured
in millimeters, and compared with the uninjured shoulder (Fig. 5.37). Another test for ligamentous laxity is the sulcus sign.
With the patient standing, the clinician applies a longitudinal
inferior traction force on the upper extremity while palpating the
distance
between the humeral head and the acromion (Fig. 5.38). Excessive laxity of the superior glenohumeral ligament will allow the humeral head to subluxate inferiorly.
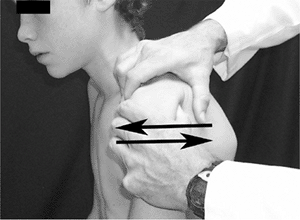 |
|
Figure 5.37
Ligamentous laxity of the left shoulder is evaluated with the patient seated, by holding the scapula and clavicle with the right hand while pushing the humeral head anteriorly and pulling it posteriorly with the left hand (arrows). The amount of glenohumeral translation is measured in millimeters, and compared with the uninjured shoulder. This test is a shoulder drawer sign. |
used to evaluate for anterior shoulder instability. This test can be
performed with the patient sitting or in the supine position. If the
left shoulder is being examined, the clinician abducts the shoulder to
90 degrees, then gradually increases the amount of external rotation
using the left hand. The right hand is placed over the humeral head,
and the clinician gently pushes the humeral head forward with the right
thumb, with the fingers strategically placed anteriorly to control any
instability. A patient with anterior instability will experience
discomfort or apprehension with this test, as the humeral head
subluxates anteriorly (Fig. 5.39). The relocation test
can be performed with the patient sitting or supine. In the supine
position, the apprehension test is performed first, and the clinician
notes the amount of shoulder external rotation when the patient first
experiences apprehension (Fig. 5.40A). The
apprehension is relieved when the clinician pushes posteriorly on the
humeral head, reducing it in the glenoid, and allowing increased
external rotation of the shoulder (Fig. 5.40B). If the apprehension is relieved with this maneuver, it is termed a positive relocation test.
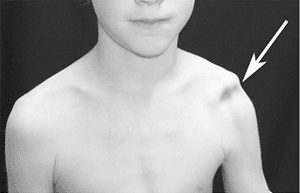 |
|
Figure 5.38
Ligamentous laxity of the shoulder can also be evaluated by applying a longitudinal inferior traction force to the upper extremity while observing the distance between the humeral head and the acromion (arrow). Excessive laxity of the superior glenohumeral ligament will allow the humeral head to subluxate inferiorly; this is a sulcus sign. |
involving the rotator cuff muscles, particularly the supraspinatus
tendon. To determine whether the patient has tendonitis, the clinician
performs impingement tests. If the patient has tendonitis involving the
supraspinatus tendon, elevation of the arm to 180 degrees, with the
shoulder internally rotated, will cause discomfort as the inflamed
tendon impinges against the anterior inferior acromion and
coracoacromial ligament. This discomfort is termed a positive Neer impingement sign (Fig. 5.41).
Another method of detecting impingement is to flex the shoulder forward
to 90 degrees in neutral rotation, with the elbow flexed to 90 degrees.
In this position, internal rotation of the shoulder will cause
discomfort as the supraspinatus tendon impinges
against the coracoacromial ligament. This maneuver is termed a positive Hawkins sign (Fig. 5.42) (37).
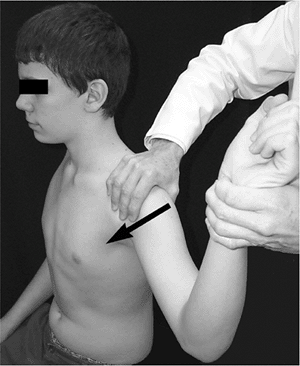 |
|
Figure 5.39
The apprehension test of the left shoulder is performed with the shoulder abducted to 90 degrees and externally rotated by the clinician’s left hand. The clinician gently pushes the humeral head forward with the right thumb (arrow), while the fingers are strategically placed anteriorly in front of the humeral head, to prevent any sudden instability. Apprehension with this maneuver indicates anterior instability of the shoulder. |
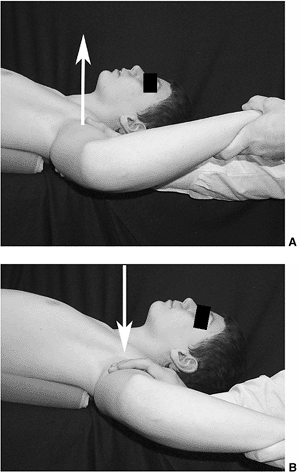 |
|
Figure 5.40 A:
The relocation test is performed with the shoulder abducted to 90 degrees. The shoulder is externally rotated up to the point where the patient experiences apprehension (arrow). B: The clinician stabilizes the humeral head by pushing it posteriorly (arrow). The increased external rotation and loss of apprehension reflects a positive relocation test. |
swimming may have multidirectional instability, with an associated tear
of the glenoid labrum. The labrum surrounds the glenoid cavity,
deepening the glenohumeral joint, and the humeral head rests against
the labrum. If there is a tear of the superior labrum, it is termed a superior labrum anterior and posterior (SLAP) lesion. If the labral tear involves the anteroinferior labrum, it is termed a Bankart lesion.
If the attachment of the labrum to the glenoid is torn, it causes
increased shoulder instability because the capsular attachment to the
glenoid has been disrupted.
cuff muscles. Activity modification, in consultation with the swim
coach to alter the training program, is recommended. Close follow-up is
important to document that the symptoms are resolving.
 |
|
Figure 5.41
If the patient has tendonitis involving the supraspinatus tendon, elevation of the arm to 180 degrees with internal rotation of the shoulder will cause discomfort when the inflamed tendon impinges against the anterior inferior acromion and coracoacromial ligament (arrow). This is termed a positive Neer impingement sign. |
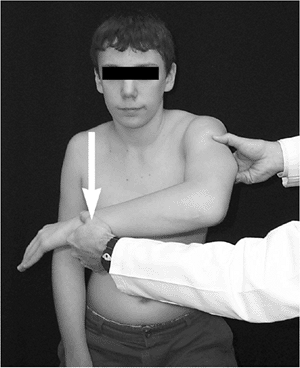 |
|
Figure 5.42
The Hawkins test is performed with the shoulder flexed forward to 90 degrees. If internal rotation in this position causes discomfort, it indicates impingement between the inflamed supraspinatus tendon and the anterior inferior acromion and the coracoacromial ligament (arrow). |
PM. Comparison of the natural history, the outcome of microsurgical
repair, and the outcome of operative reconstruction in brachial plexus
birth palsy. J Bone Joint Surg Am 1999;81:649.
MS, Zurakowski D, Kasser JR. Differentiating between septic arthritis
and transient synovitis of the hip in children: an evidence-based
clinical prediction algorithm. J Bone Joint Surg Am 1999;81:1662.
VS. Calcaneal lengthening for valgus deformity of the hindfoot: results
in children who had severe, symptomatic flatfoot and skewfoot. J Bone Joint Surg Am 1995;77:500.
B, Varghese G, Mulpuri K, et al. Natural evolution of Perthes disease:
a study of 610 children under 12 years of age at disease onset. J Pediatr Orthop 2003;23:590.
MC, Alexander J, Sutherland DH, et al. Clinical utility of the
Duncan-Ely test for rectus femoris dysfunction during the swing phase
of gait. Dev Med Child Neurol 2003;45:763.
UK, Freeman BJC, Gregory P, et al. Clinical outcome and return to sport
after the surgical treatment of spondylolysis in young athletes. J Bone Joint Surg Br 2002;85:244.
