Pediatric Ultrasound
especially useful because the blocks are often performed under general
anesthesia. In small children (less than 30 kg) a high frequency
transducer (7 MHz to 15 MHz) may be used for deep blocks such as
sciatic and infraclavicular blocks as well as superficial blocks. The
following probes are recommended.
-
25 mm linear array (6 MHz to 13 MHz):
This probe is used for all blocks in children less than 15 Kg with the
exception of infraclavicular blocks where a probe with a smaller
footprint is useful. This probe is also useful for interscalene and
supraclavicular blocks in larger children who weigh more than 30 kg. -
11 mm curved array (4 MHz to 8 MHz):
This probe is useful for infraclavicular blocks in children of all
sizes because of its small footprint. The small footprint allows the
user to place the probe near to the clavicle and still have room to
manipulate the needle which is directed toward the plexus in a saggital
plane superior to the probe. This probe may also be useful for sciatic
blocks in the popliteal fossa and for femoral nerve blocks. -
38 mm linear array (6 MHz to 13 MHz): This probe is useful for sciatic blocks in larger children.
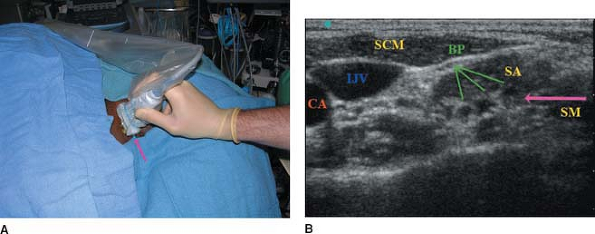
The brachial plexus is visualized in cross section and a series of
anechoic circles is seen between the anterior and middle scalene muscle
and beneath the sternocleidomastoid muscle (Fig. 43-1). The block needle is inserted posterior to the probe using an in plane technique (Fig. 43-1).
This technique is especially useful when the practitioner wishes to
target the lower roots of the brachial plexus. This approach allows for
direct visualization of
the
needle in real time. When inserting a catheter for postoperative
analgesia after shoulder surgery, the upper roots of the brachial
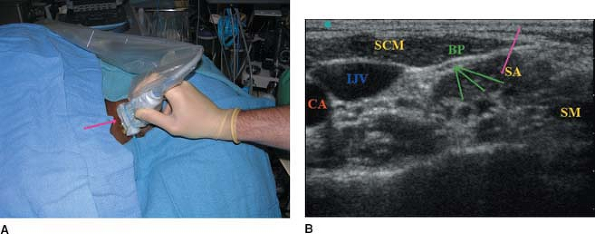
plexus need to be blocked. In this setting, it may be preferable to
insert the needle inferior to the probe using an out of plane technique
(Fig. 43-2).
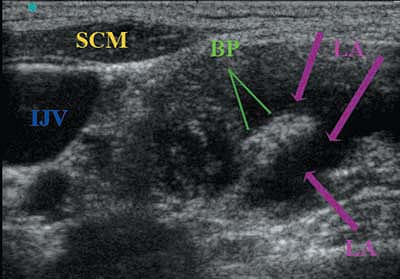
The needle is directed cephalad to the plexus and the catheter is
placed adjacent to roots C5 and C6. Diffusion of the local anesthetic
around the roots is seen after injection (Fig. 43-3).
 |
|
Figure 43-1. The arrow
shows the direction of the block needle, which enters the neck parallel to the longitudinal axis of the probe. The placement of a catheter using this approach to the brachial plexus will most likely result in positioning the catheter next to the lower roots of the brachial plexu (C8-T1). CA, carotid artery; IJV, internal jugular vein; SCM, sternocleidomastoid muscle; BP, brachial plexus; SA, anterior scalene; SM, middle scalene. |
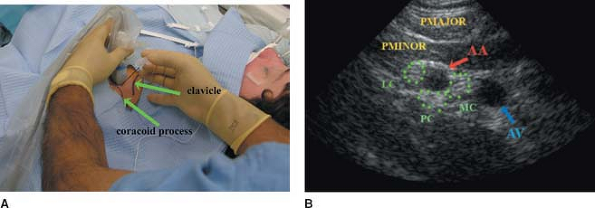
is the coracoid process. With the arm abducted, to better expose the
axillary vessels, the probe is placed 1 to 1.5 cm below
the
coracoid process in the saggital plane. The needle is introduced
superior to the probe and introduced nearly perpendicular to the skin (Fig. 43-4).
The needle is advanced through the pectoralis major and minor muscles
toward the lateral cord. Local anesthetic is injected around the
lateral cord (Fig. 43-5). The needle is then redirected underneath the axillary artery to reach the posterior cord (Fig. 43-6).
The same technique can be used to selectively block the medial cord. In
older children it is useful to block each cord. In younger children it
is sufficient to inject the local anesthetic around one cord and allow
it to diffuse to the other cords.
 |
|
Figure 43-2. The arrow
shows the direction of the block needle, which enters the neck perpendicular to the longitudinal axis of the probe. The placement of a catheter using this approach to the brachial plexus will most likely result in positioning the catheter next to the higher roots of the brachial plexus (C5-C6). CA, carotid artery; IJV, internal jugular vein; SCM, sternocleidomastoid muscle; BP, brachial plexus; SA, anterior scalene; SM, middle scalene. |
 |
|
Figure 43-3.
The local anesthetic has been injected and the brachial plexus structures are now isolated from the anterior and middle scalene muscle and are easily identifiable. IJV, internal jugular vein; SCM, sternocleidomastoid muscle; BP, brachial plexus; LA, local anesthetic. |
 |
|
Figure 43-4.
The probe is held 1 cm below the coracoid process and the needle is advanced at a 5° to 10° angle, in relationship to the probe. The brachial plexus cords surround the axillary artery. AA, axillary artery; AV, axillary vein; PMAJOR, pectoralis major muscle; PMINOR, pectoralis minor muscle; LC-PC-MC, lateral, posterior, medial cord of the brachial plexus. |
 |
|
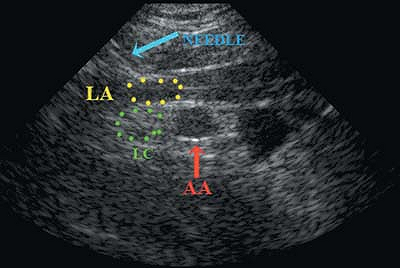
Figure 43-5.
The tip of the needle is in the pectoralis minor muscle and the local anesthetic is collecting above the lateral cord. LA, local anesthetic; AA, axillary artery; LC, lateral cord of the brachial plexus. |
 |
|
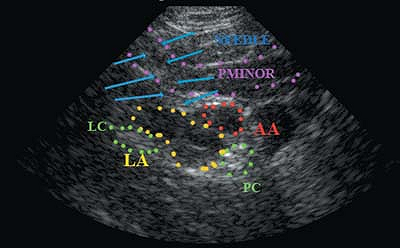
Figure 43-6.
The tip of the needle is below the pectoralis minor and the local anesthetic is collecting around the axillary artery, pushing the lateral cord more laterally. LA, local anesthetic; AA, axillary artery; LC, lateral cord; PC, posterior cord; PMINOR, pectoralis minor. |
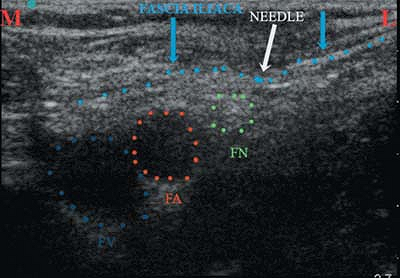
at or below the level of the inguinal crease. The femoral nerve can be
visualized in short axis, lateral to the femoral artery, beneath the
fascia iliaca and superficial to the iliopsoas muscle. The typical
triad, femoral
nerve-femoral artery-femoral vein can be seen in Fig. 43-9.
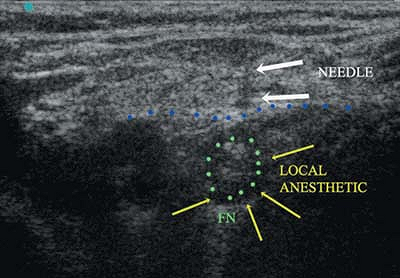
The needle is introduced inferior to the probe using an out of plane
technique. Direct visualization of the needle is difficult with this
approach, however the position of the needle relative to the nerve can
be inferred by the movement of adjacent tissues such as the fascia
iliaca as the needle is advanced. Alternatively, injection of a small
amount of local anesthetic may demonstrate the position of the needle
relative to the nerve (Fig. 43-10).
A femoral block conducted solely on neurostimulation may fail because
stimulation across the thin fascia iliaca is possible in small children
even at low stimulation thresholds. Figure 43-11
shows the femoral nerve and artery pushed apart by the local
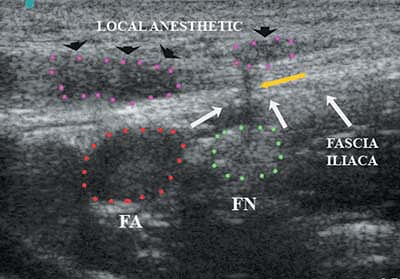
anesthetic, indicating the correct placement of the block needle.
Ultrasound can also confirm the proper distribution of the local
anesthetic around the femoral nerve. Larger needles (18–19 gauge) can
make significant holes
in the fascia allowing the local anesthetic to extravasate above the plane of the fascia iliaca (Fig. 43-12).
 |
|
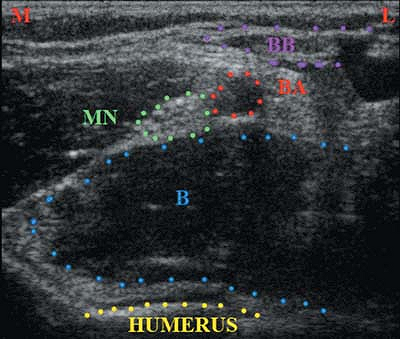
Figure 43-7.
Ultrasound image of the radial nerve, approximately 2 cm above the medial epicondyle of the humerus. B, brachialis muscle; BA, brachial artery; BB, biceps brachii muscle; MN, median nerve; M, medial side of the arm; L, lateral side of the arm. |
 |
|
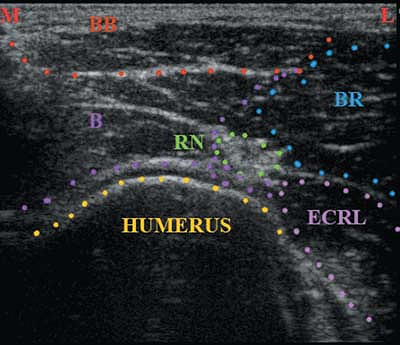
Figure 43-8.
Ultrasound image of the radial nerve, approximately 2 cm above the lateral epicondyle of the humerus. B, brachialis muscle; BB, biceps brachii muscle; BR, brachioradialis muscle; ECRL, extensor carpi radialis longus; RN, radial nerve; M, medial side of the arm; L, lateral side of the arm. |
 |
|
Figure 43-9.
The femoral vein and femoral artery lie medial to the femoral nerve, underneath the fascia iliaca. The distance between the femoral nerve and the femoral artery varies, depending on the child’s age. FN, femoral nerve; FA, femoral artery; FV, femoral vein. |
 |
|
Figure 43-10.
Indentation of the fascia iliaca by the block needle as it is advanced toward the femoral nerve. Because of the thinness of the fascia iliaca in children, it is often possible to obtain elevation of the patella, resulting from femoral nerve stimulation, despite the stimulating needle being above the fascia iliaca. The use of ultrasound helps to avoid this mistake. FV, femoral vein; FA, femoral artery; FN, femoral nerve; M, medial side of the patient; L, lateral side of the patient. |
 |
|
Figure 43-11.
The needle is below the fascia iliaca and the ultrasound visualizes the local anesthetic surrounding the femoral nerve. FN, femoral nerve; arrows, block needle. |
 |
|
Figure 43-12.
The local anesthetic has leaked around the block needle from the area surrounding the femoral nerve into the space above the fascia iliaca. This may explain the high failure rate of so-called 3-in-1 blocks. FA, femoral artery; FN, femoral nerve; arrowheads, collection of local anesthetic above the fascia iliaca; yellow arrow, block needle. |
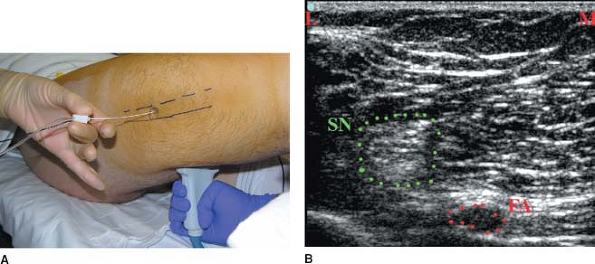
sciatic nerve is relatively simple compared with the posterior
approach: the probe is far from the field and thus does not require a
sterile cover. Visualization of the needle is relatively simple because
the needle trajectory is within the plane of the transducer (Fig. 43-13). The identification of the sciatic nerve in
the middle of the thigh can be difficult because it is surrounded by
the biceps, semitendinosus and the semimembranosis muscles. Neural
structures at this level can be easily confused with artifacts. An easy
approach consists in initially localizing the popliteal vessels in the
popliteal fossa. The patient is placed supine and the knee is bent to
facilitate the placement of the probe in a transverse orientation
posterior to the popliteal fossa. The vessels are identified and the
tibial nerve and common peroneal nerves are identified (Fig. 43-14). These nerves are traced cephalad until they join to form the sciatic nerve which lies deep and lateral to the femoral artery (Fig. 43-13).
The needle is introduced perpendicular to skin in line with the
transducer until the needle tip is adjacent to the sciatic nerve. Local
anesthetic is then injected around the sciatic nerve. Some
practitioners prefer to inject the local anesthetic more distally in
the popliteal fossa. In this case, an injection around the tibial nerve
and common peroneal nerve are required (Fig. 43-15).
 |
|
Figure 43-13.
Visualization of the sciatic nerve at the mid-thigh level. SN, sciatic nerve; FA, femoral artery; M, medial side of the patient; L, lateral side of the patient. |
 |
|
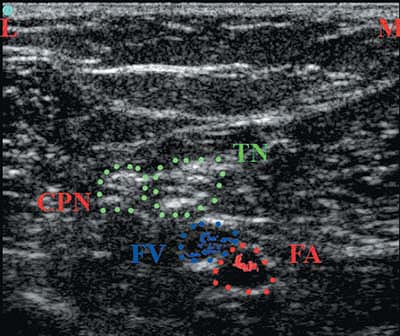
Figure 43-14.
Visualization of the sciatic nerve terminal branches (common peroneal and tibial nerve) at the popliteal fossa level. TN, tibial nerve; CPN, common peroneal nerve; FV, femoral vein; FA, femoral artery; M, medial side of the patient; L, lateral side of the patient. |
 |
|
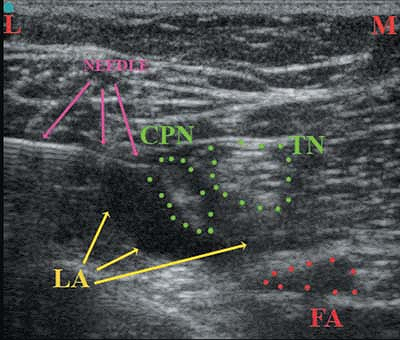
Figure 43-15.
The block needle tip is in proximity of the tibial nerve and the local anesthetic is collecting around the components of the sciatic nerve. LA, local anesthetic; CPN, common peroneal nerve; TN, tibial nerve; FA, femoral artery; M, medial side of the patient; L, lateral side of the patient. |
