Humeral Shaft Fractures: Open Reduction Internal Fixation
shaft fractures can be treated nonoperatively with high rates of union
and excellent functional results. However, in specific clinical
settings, open reduction and internal fixation (ORIF) are favored over
closed functional methods. Good results can be expected (1,2,3) and outcomes are superior to comparable fractures treated with intramedullary nailing (4,5,6).
Although there are no absolute indications for plate fixation, we favor
its use in some patients and consider the fracture characteristics and
the presence of concomitant injuries in our decision (Table 5.1).
fractures in which a satisfactory reduction cannot be achieved or
maintained. The most common cause of a poor reduction in an otherwise
healthy individual is interposition of soft tissue. Failure to maintain
an acceptable closed reduction sometimes occurs in obese patients or
women with large breasts. Other indications include segmental and
peri-articular fractures. The latter can be difficult to control, and
the prolonged immobilization of the adjacent joint can lead to loss of
motion.
stabilization to allow optimal soft-tissue management. After thorough
debridement, ORIF of the humerus is a good method of fracture
stabilization for most grade I, II, and IIIA injuries with limited bony
defects. It produces a stable limb, improving postoperative wound
management. With extreme comminution or bone loss, acute shortening of
up to 5 cm is usually well tolerated.
pathologic humeral fractures frequently results in nonunion and
persistent pain. There is widespread agreement that patients with a
pathologic humeral fracture as a result of metastatic disease benefit
from
surgical
stabilization. Usually these fractures are best managed with a locked
intramedullary nail, but occasionally, a fracture is not amenable to
intramedullary nailing and is better managed with a long spanning plate
(7).
|
Table 5.1. Indications for Surgical Stabilization of Humeral Shaft Fractures
|
||||
|---|---|---|---|---|
|
arthroplasty frequently require internal fixation. Fractures that occur
around the stem of an implant occasionally require revision of the
prosthesis.
for ORIF of a humeral fracture. Delayed union is generally accepted to
mean that the fracture has failed to show progressive signs of healing
within 3 to 4 months, whereas nonunion is defined when the healing is
delayed or arrested beyond 6 months. Nonunions can occur because of
fracture instability, poor bone vascularity, or marked displacement.
Infection must be ruled out for nonunions of open fractures that have
been surgically repaired. Union is usually obtained following revision
ORIF and autogenous bone grafting (8), and in osteoporotic bone this may be done successfully with locking compression plates (9).
intervention because angular deformity is often well tolerated after
closed treatment. The amount of mal-alignment that can be accepted
varies between patients and is influenced by level of activity and
cosmesis. Most patients tolerate up to 20 degrees of varus, 15 degrees
of anterior angulation, and 5 cm of shortening.
indicated in a variety of circumstances due to concomitant injuries.
The patient with multiple injuries is the most common candidate for
operative treatment of humeral shaft fractures (10,11,12).
When patients sustain injuries to multiple body systems, early surgical
stabilization of long bone fractures may be life-saving. Fixation
should be undertaken early to reduce analgesic needs, allow early
mobilization, and facilitate nursing care.
elbow, or forearm often require operative treatment of their humeral
fracture. In bilateral humeral fractures or any contralateral
upper-extremity injury, fixation may be necessary to allow activities
of daily living and self-care. Humeral shaft fractures associated with
a fracture of both forearm bones require fixation of both the forearm
and the humerus to allow early range of motion. Finally, rehabilitation
of injuries to the lower extremities can be accelerated by fixation of
the humerus, which allows for the use of crutches through the
stabilized humerus.
with a closed fracture, then this should be stabilized at the time of
vascular repair. Internal fixation of the humerus through the vascular
approach is recommended to protect the vascular repair, to facilitate
ongoing assessment, and allow rehabilitation of the limb. Brachial
plexus or peripheral nerve injuries in the ipsilateral limb are often
an indication for internal fixation of a humeral fracture because
concomitant brachial plexus injuries may be associated with high rates
of delayed union, nonunion, and malunion of the humeral shaft when
treated closed (13). To prevent these
complications and to facilitate rehabilitation, operative treatment
should be considered with this combination of injuries.
The incidence of radial nerve injury in humeral fractures is
approximately 10%, with a range reported between 2% and 26%. Humeral
shaft fractures seen with a primary radial-nerve injury do not usually
require nerve exploration. If the fracture reduction can be maintained,
closed treatment will result in fracture healing and a good outcome
with a greater than 80% chance of spontaneous nerve recovery. The
majority of cases are neurapraxias, which should show signs of recovery
by 3 to 4 months, with improvements in muscle grade up to 2 years after
injury (11).
techniques and late exploration of radial nerve palsies, better than
90% recover (14,15).
Therefore, we recommend initial observation and late exploration for
nerve injuries that do not resolve. The injury should be documented
clinically and electrophysiologically with electromyogram/nerve
conduction studies (EMG/NCS) in the early stages. The hand should be
splinted, and an intensive physiotherapy program should be initiated to
maintain mobility at the elbow, wrist, and fingers. Patients are
evaluated monthly and have a follow-up EMG/NCS at 6 and 12 weeks. If
after 4 to 6 months there is no sign of radial nerve recovery, then we
explore the nerve.
radial-nerve palsy. Most commonly this occurs after closed reduction of
a humeral fracture. Traditionally, a nerve palsy occurring in such a
circumstance was considered an indication for nerve exploration and
internal fixation. Although some have shown that the nerve can be
trapped between the fracture fragments (17),
and while it seems reasonable to explore the nerve and free it from any
ongoing compression, there is no scientific evidence that the outcome
is improved by early surgery. Secondary radial-nerve palsy, however,
continues to be an accepted indication for early exploration.
shaft fractures include grade IIIB open fractures with massive
soft-tissue injury or extensive bone loss, soft-tissue or bone
infection, as well as severe osteoporosis, that would preclude fixation.
physical examination are mandatory. Associated injuries should be
identified and carefully assessed. Physical examination should include
the chest, neck, shoulder, arm, elbow, forearm, wrist, and hand. The
physical signs of fracture are usually obvious after humeral shaft
fractures with pain, swelling, crepitus, and motion at the fracture
site. The neurologic examination of the limb must be meticulous. Radial
nerve injury is the most commonly associated neurological injury, but
any peripheral nerve, including the brachial plexus, can be injured in
association with a humeral diaphyseal fracture. The vascular assessment
includes palpation of the axillary, brachial, and radial pulses and an
assessment of hand-tissue perfusion. The soft-tissue compartments of
the arm and forearm should be evaluated for compartment syndrome.
Anteroposterior (AP) and lateral views of the humerus should be
obtained that include the shoulder and elbow joints. The anatomic
location of the fracture, the fracture pattern, and the expected bone
quality are critical when developing a preoperative plan.
fracture, a surgical tactic should be developed that includes the
patient position, the surgical approach, the steps necessary for
fracture reduction, temporary fixation, and the implant to be used for
final fixation.
humerus: the anterolateral, straight lateral, posterior, and
anteromedial. However, the anteromedial approach is rarely used in
humeral-shaft fracture treatment and will not be discussed further. The
decision about which surgical approach to use is based on the fracture
level and configuration, the need for radial nerve exploration, and the
patient’s general condition. The most common approach is the
anterolateral. Fractures located anywhere in the proximal two thirds of
the humerus can be successfully managed through this approach, but it
does not allow adequate exposure of the distal one third of the
humerus; therefore, it cannot be used if the fixation
must
be extended into the distal third. In fractures involving the distal
two thirds of the humerus, with an associated radial-nerve injury that
requires surgery, we prefer the straight lateral approach. This
approach can be extended into the anterolateral approach and thereby
give access to the entire humerus if necessary. It may also be extended
proximally by utilizing the same muscular interval but passing
posteriorly to the deltoid, the proximal limit being the axillary nerve
(18). The posterior approach can be used for fractures that involve the distal half of the humeral shaft.
fixation before final fixation must be carefully considered. In most
cases, direct reduction techniques are appropriate. The fracture
hematoma is evacuated, and the fracture surfaces are anatomically
reduced. For spiral or oblique fracture patterns, temporary fixation
can usually be accomplished with Weber pointed reduction forceps.
Transverse fractures can usually be stabilized temporarily with
Kirschner (K) wires or by drilling a hole in each fragment and using
pointed reduction forceps away from the site of anticipated plate
application. Some comminuted fractures that still have cortical contact
between the main proximal and distal pieces cannot be temporarily
stabilized satisfactorily. In those cases, the appropriate plate is
secured to one fragment, the fracture is then reduced under the plate,
and fixation is completed.
indirect reduction techniques. The femoral distractor is used to secure
the reduction, which is confirmed under image intensification. The
appropriate plate is then secured to the main proximal and distal
fragments. The soft-tissue attachments to the comminuted intercalary
fragments are left intact. Bone grafting is not added when the indirect
reduction technique is used.
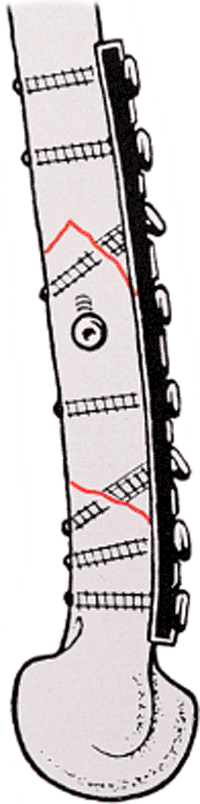
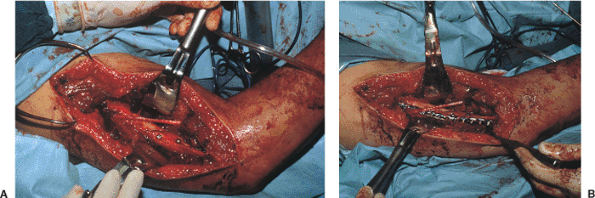
fractures, surgeons strive to achieve interfragmentary compression,
which can be done by using interfragmentary lag screws inserted either
outside (Fig. 5.1) or through the plate (Fig. 5.2).
Interfragmentary screws alone are insufficient fixation for humeral
shaft fractures and must be supplemented with a neutralization plate.
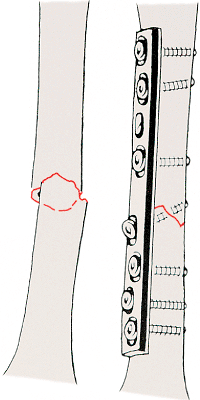
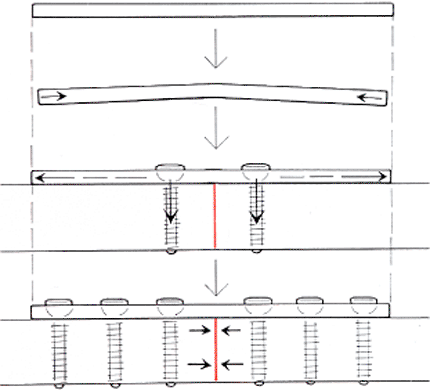
In transverse fracture patterns, interfragmentary compression is
achieved
by using a limited-contact dynamic-compression (LCDC) plate, and the
plate must be prestressed (prebent) to avoid a gap in the far cortex (Fig. 5.3).
In general, the plate of choice is a broad 4.5-mm LCDC. This is a
strong plate with a wide surface contact and offset screw holes to
prevent longitudinal splitting of the shaft from collinear screws. In
addressing acute fractures, we aim for at least six cortices of
fixation above and below the fracture. When dealing with osteoporotic
bone, we either use more cortices of fixation or locking compression
plates. Bone grafting should be planned with comminuted fractures. If
more than one third of the circumference of the humeral shaft is
comminuted, we generally use an autogenous iliac-crest bone graft.
 |
|
Figure 5.1. Initial fixation is accomplished with an interfragmentary screw. This is supplemented by a neutralization plate.
|
 |
|
Figure 5.2. Interfragmentary fixation through the plate.
|
 |
|
Figure 5.3. Transverse fracture pattern in which interfragmentary compression is achieved by using a prebent dynamic-compression plate.
|
plate cannot be used. In such a situation, a narrow 4.5-mm LCDC plate
can be used. Likewise, in the distal shaft, where extensive contouring
of the plate is necessary, a 3.5-mm pelvic reconstruction plate is
occasionally used for neutralization. However, this type of plate
should be used only when there is excellent interfragmentary
compression with multiple lag screws. It is important to avoid
encroachment of the hardware in the olecranon or coronoid fossae when
fixing the distal humerus.
nail brush: The area is washed off with saline and then chlorhexidine
is poured over the limb prior to formal prepping and draping. However,
for open fractures, iodine is preferred. A sterile tourniquet is used
if the fracture is in the middle or distal one third. If it is used,
the tourniquet is deflated prior to closure and hemostasis achieved;
therefore, a drain is rarely necessary.
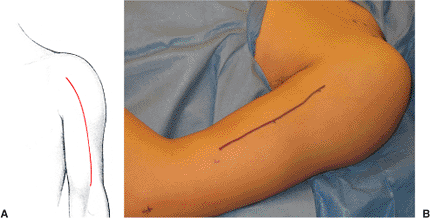
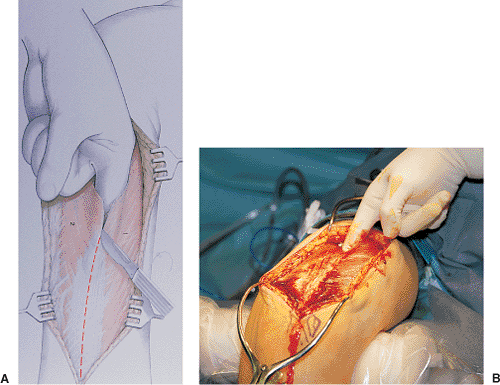
supine and a pad beneath the scapula. The arm is free draped allowing
access to the neck (subclavian vasculature) and placed on a radiolucent
arm board. Surface landmarks, coracoid process, deltopectoral groove,
lateral bicipital sulcus, and the lateral epicondyle, are marked with a
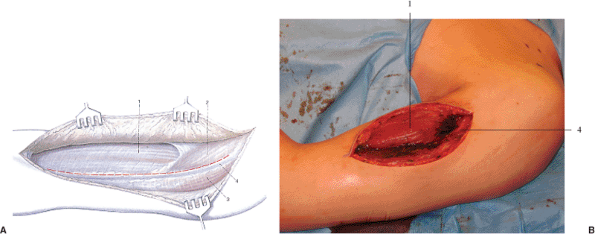
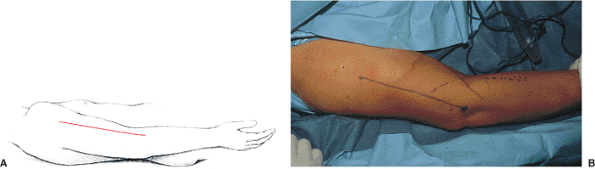
sterile pen (Fig. 5.4). Depending on the
fracture, the incision may extend from the coracoid process down to
approximately 6 cm from the lateral epicondyle (Fig. 5.5).
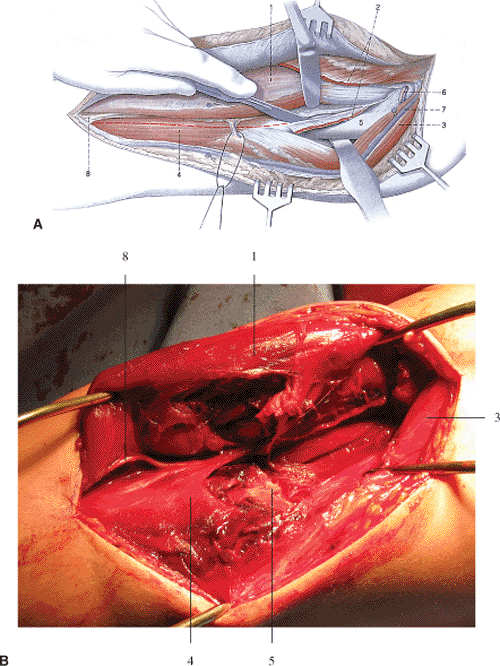
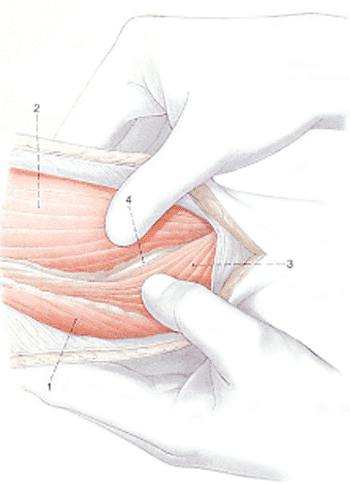
The deltopectoral groove is developed proximally. The belly of the
biceps is identified and its lateral border mobilized, exposing the
brachialis muscle (Fig. 5.6). Care is taken to
avoid injury to the proximal cephalic vein and the lateral cutaneous
nerve of the forearm in the medial aspect of the distal wound area. The
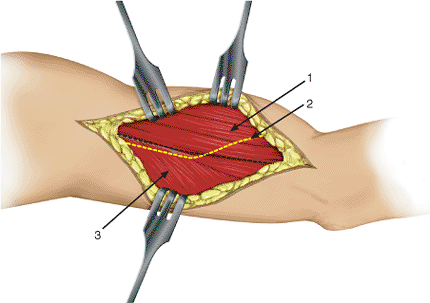
biceps is retracted medially, and the brachialis is divided
longitudinally, lateral to its midline and down to bone, aiming for the middle of the humeral shaft (Fig. 5.7).
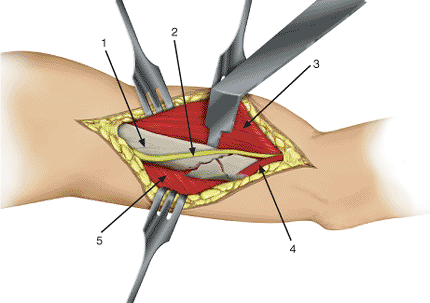
Through this approach, the radial nerve, which is lateral to the
brachialis, is protected and the innervation of the lateral portion of
the brachialis (radial nerve) is preserved. Flexion of the elbow, along
with partial (anterior) detachment of the deltoid insertion and of the
medial brachialis origin, is done to allow reduction and plating of the
anterolateral surface of the humerus (Fig. 5.8).
 |
|
Figure 5.4. A,B. Incision for the anterolateral approach.
|
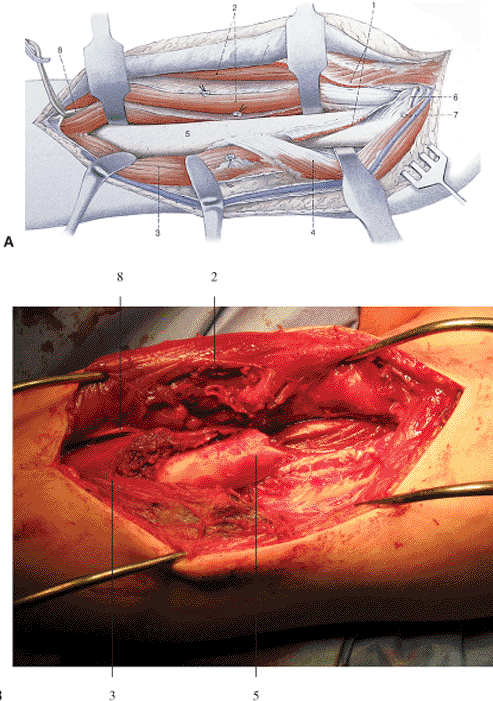
dissection but allows excellent visualization of the radial nerve and
adjacent structures. It is ideal for exploration of the radial nerve
and fixation of the distal humerus in a multiply injured patient. With
the patient supine, the arm is free draped and kept adducted along the
patient’s body. The surface landmarks are the lateral epicondyle,
deltoid tuberosity, and the coracoid process as necessary (Fig. 5.9).
epicondyle proximally to the deltoid tuberosity. After incision of the
investing fascia of the arm, the intervals between the triceps and
brachialis proximally and the brachioradialis and brachialis distally
are identified. The distal interval is first developed bluntly as
described by Henry (19): “…place well-gloved
thumbs, lengthwise and parallel, on each belly (brachialis and
brachioradialis), and open the plane like a book on your knee. The
nerve marks the place” (Fig. 5.10).
The radial nerve is isolated, looped with a rubber sling, and
protected. The nerve is retracted laterally while the proximal
dissection is completed. The periosteum anterior to the intermuscular
septum is split longitudinally, and subperiosteal elevation progresses
medially and proximally with direct visualization and protection of the
nerve at all times. This can be gently elevated if further access is
required. As the nerve courses posteriorly and proximally, one might
need to incise the intermuscular septum to mobilize the nerve and
visualize its relation to the fracture. The nerve is retracted
anteriorly, and the distal dissection is completed. The distal plane
between the brachioradialis and the triceps is identified (Fig. 5.11).
This plane is incised sharply, and the brachioradialis is reflected
anteriorly, protecting the distal portion of the nerve. The entire
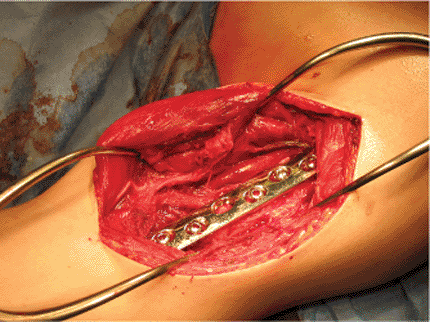
distal humerus is exposed laterally and anterolaterally (Fig. 5.12).
A narrow, 4.5-mm LCDC plate positioned laterally is often the best
implant with this exposure. The plate is often quite distal and screw
placement in the coronoid/olecranon fossae must be avoided (Fig. 5.13).
 |
|
Figure 5.5. A,B. Initial muscular exposure: (1) biceps; (2) pectoralis major; (3) deltoid; and (4) cephalic vein.
|
 |
|
Figure 5.6.
Splitting of the brachialis in the line of its fibers: (1) biceps; (2) pectoralis major; (3) deltoid; (4) brachialis; (5) humerus; (6) anterior, circumflex, humeral vessels; (7) cephalic vein; and (8) lateral cutaneous nerve of the forearm. |
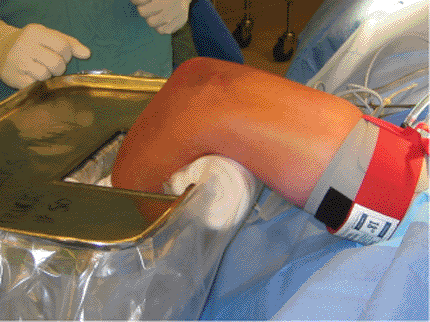
fractures in the distal half of the humerus. The patient is placed
prone and brought to the edge of the operating table. The arm is free
draped to allow access to the whole arm and the elbow. The shoulder is
abducted 90 degrees in neutral flexion and supported distally at the
elbow by a modified Mayo stand (Fig. 5.14). The
stand can be altered by cutting a hole at the edge of the tray and
padding the exposed rim of the stand. During the procedure, the forearm
and hand are dropped into the hole, which is lined by a sterile c-arm
pack protecting the forearm and hand from contamination that is
possible due to their low-lying position. An additional advantage of
using the Mayo stand is the ability to place instruments on it. An
alternative is to place the patient in a lateral position with a
bolster under the arm.
 |
|
Figure 5.7.
Completed exposure of the proximal two thirds of the humeral shaft: (1) pectoralis major; (2) biceps; (3) brachialis; (4) deltoid; (5) humerus; (6) anterior, circumflex, humeral vessels; (7) cephalic vein; and (8) lateral cutaneous nerve of the forearm. |
 |
|
Figure 5.8. Prebent, broad, 4.5-mm, dynamic-compression plate applied to a transverse fracture via an anterolateral approach.
|
 |
|
Figures 5.9. Positioning and skin incision for the straight lateral approach to the distal humerus.
|
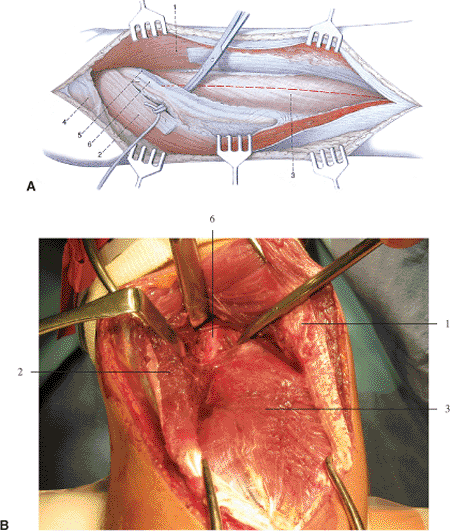
acromion and the olecranon. The straight incision extends from the
distal border of the posterior deltoid, along the lateral edge of the
long head of triceps, to the tip of the olecranon (Fig. 5.15). The long head can
be identified as a mobile mass on the posteromedial aspect of the arm.
Skin, subcutaneous tissue, and fascia are incised and the distal,
thick, white triceps tendon is identified. Proximally, the interval
between the long and the lateral heads of the triceps is identified and
dissected bluntly. Distally, these two superficial heads are sharply
dissected by division of the triceps tendon (Fig. 5.16). Careful blunt dissection is carried out to identify the radial nerve on the proximal aspect of the deep head of triceps (Fig. 5.17).
A rubber sling is placed around the radial nerve, which is protected
throughout the case. The deep triceps is split longitudinally in its
midline, and its medial and lateral portions are elevated, exposing the
humerus (Fig. 5.18). Reduction and fixation can
now proceed. The closure includes reapproximation of the triceps
aponeurosis with absorbable suture and superficial layer closure.
 |
|
Figure 5.10.
The radial nerve is identified in the interval between the brachialis and the brachioradialis: (1) triceps; (2) brachialis; (3) brachioradialis; and (4) radial nerve. |
 |
|
Figure 5.11.
The intervals between brachialis and triceps proximally and between brachioradialis and triceps distally are developed: (1) biceps brachii muscle; (2) radial nerve; and (3) triceps brachii muscle. |
 |
|
Figure 5.12.
The brachialis and brachioradialis are retracted anteriorly and the triceps posteriorly exposing the distal humeral shaft: (1) humerus; (2) radial nerve; (3) brachialis muscle; (4) brachioradialis muscle; and (5) triceps brachii muscle. |
 |
|
Figures 5.13. Reduction and internal fixation of a distal humeral fracture through the straight lateral approach.
|
 |
|
Figure 5.14. Positioning for the posterior approach with modified Mayo stand and sterile tourniquet.
|
 |
|
Figure 5.15. Skin incision for posterior approach.
|
patients are placed in a sling, which is removed to permit active
range-of-motion exercises of the shoulder and elbow within 1 or 2 days
of surgery. Full elbow and shoulder motion should be obtained within 6
weeks of surgery. Patients are seen on a monthly basis until the
fracture is united and they have returned to normal activity.
Radiographs are obtained at each visit. The patient is carefully
assessed for shoulder, elbow, wrist, and hand function. The radiographs
are studied for signs of fracture healing and any evidence of implant
failure. With stable fixation, fracture union is often difficult to
assess. If follow-up radiographs show maintenance of the reduction,
light weights are usually allowed at 6 weeks and regular weights at 12
weeks. At 12 weeks, patients can begin returning to normal activities.
Heavy work can be started at 16 weeks. Sporting activities, such as
tennis and golf, can also be started about 4 months after surgery.
 |
|
Figure 5.16.
The posterior approach. Identification of the long and lateral heads of triceps: (1) long head of triceps and (2) lateral head of triceps. |
 |
|
Figure 5.17.
Exposure of the deep head of the triceps and radial nerve: (1) long head of triceps; (2) lateral head of triceps; (3) deep (medial) head of triceps; (4) deltoid; (5) deep brachial artery; and (6) radial nerve. |
 |
|
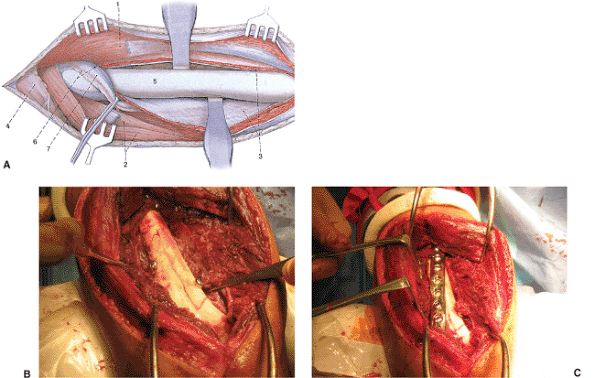
Figure 5.18. A.
Exposure of the distal half of the humeral shaft: (1) long head of triceps; (2) lateral head; (3) medial head; (4) deltoid; (5) humerus; (6) deep brachial artery; and (7) radial nerve. B. By using the posterior approach, reduction and lag screw fixation is achieved. C. This is followed by placement of a neutralization plate positioned laterally to avoid encroachment on the olecranon fossa. |
principles. Failure of fixation occurs in up to 4% of patients and can
be avoided by careful preoperative planning and implant selection as
well as limited soft-tissue dissection. When using a plate,
interfragmentary compression, either with lag screws and a
neutralization plate or with a compression plate alone, is essential.
At least 6 points of cortical fixation on each side of the fracture
must be obtained. If the fixation fails, revision ORIF is necessary,
usually with a longer locking plate and bone graft because nonoperative
management is rarely successful.
of cases. Factors thought to contribute to nonunion include open
fractures, middle-third transverse fractures, pathologic fractures,
patient alcohol abuse, or a technical error in the primary procedure.
Factors that can be controlled by the surgeon include accurate fracture
reduction, stability of fixation, and minimization of soft-tissue
stripping and bone grafting. Nonunion is treated by revision ORIF and
autogenous cancellous bone grafting. A longer plate must be used at the
revision procedure. Nonunion after intramedullary nailing is also best
treated by ORIF rather than exchange nailing (20).
motion of the shoulder or elbow is probably underreported. Several
studies report that 15% to 20% of patients have decreased shoulder and
elbow motion after ORIF. Etiologic factors include fractures with
extensive soft-tissue injuries or with ipsilateral bone or joint
injury. Stable fixation and early motion are recommended. If
significant stiffness is identified, a more vigorous physiotherapy
program is initiated. We have not needed to use any surgical modalities
to deal with joint stiffness after ORIF of humeral shaft fractures.
routine use of perioperative antibiotics, limited soft-tissue
dissection, careful hemostasis, and thorough debridement of open
fractures may reduce the rate of infection after ORIF. If infection
develops, then the
microorganism
must be isolated. This is followed by assessing and correcting problems
with stability, fragment approximation, vascularity, and soft-tissue
coverage. The infected site should be incised, drained, and thoroughly
debrided. The area is packed with antibiotic-loaded, acrylic, cement
beads and systemic parenteral antibiotics are given. The choice of
local and systemic antibiotic depends on the Gram stain findings and
the final culture and sensitivities. Parenteral antibiotics are
generally continued for 6 weeks. The local antibiotic depot is usually
removed at 7 to 10 days during repeated debridement and irrigation. If
the fixation is rigid, it is left in place, but if it is loose, it is
revised and rigid fixation is obtained.
injury. Iatrogenic radial-nerve palsy occurs in about 5% of surgical
cases. An intraoperative laceration should never occur, but if it does,
it should be repaired immediately by a trained microsurgeon. A
postoperative nerve palsy after identification and protection of the
nerve should be observed, and full functional recovery anticipated.
JR, Henley MB, Agel J, et al. Randomized prospective study of humeral
shaft fracture fixation: intramedullary nails versus plates. J Orthop Trauma 2000;14:162–166.
RG, Brien D, Buckley RE, et al. Fixation of fractures of the shaft of
the humerus by dynamic compression plate or intramedullary nail: a
prospective, randomised trial. J Bone Joint Surg Br 2000;82:336–339.
S, Stapert J, Boxma H, et al. Treatment of pathological fractures of
the humeral shaft due to bone metastases: a comparison of
intramedullary locking nail and plate osteosynthesis with adjunctive
bone cement. Eur J Surg Oncol 1996;22:621–626.
MJ, Beauchamp CG, Kellam JK, et al. The results of plating humeral
shaft fractures in patients with multiple injuries: the Sunnybrook
experience. J Bone Joint Surg Br 1985;67:293–296.
WA, Nisten MW, Duis H-J, et al. Treatment of humeral shaft fractures
related to associated injuries: a retrospective study of 237 patients. Acta Orthop Scand 1991;62:148–153.
WW, Gellman H, Becker V, et al. Management of fractures of the humerus
in patients who have an injury of the ipsilateral brachial plexus. J Bone Joint Surg Am 1990;72:1208–1210.
S, Barrios RH, Martinez-Peric R, et al. Surgical treatment of the
radial nerve lesions associated with fractures of the humerus. J Orthop Trauma 1993;7:211–215.
A, Horowitch A, Aboulafia A, et al. Functional bracing for comminuted
extra-articular fractures of the distal third of the humerus. J Bone Joint Surg Br 1990;72:283–287.
