Freiberg Disease (Freiberg Infraction)
Editors: Frassica, Frank J.; Sponseller, Paul D.; Wilckens, John H.
Title: 5-Minute Orthopaedic Consult, 2nd Edition
Copyright ©2007 Lippincott Williams & Wilkins
> Table of Contents > Freiberg Disease (Freiberg Infraction)
Freiberg Disease (Freiberg Infraction)
John T. Campbell MD
Description
-
“Freiberg infraction” is an eponym for osteonecrosis of the 2nd metatarsal head (1).
-
The most common presentation is in a
young or middle-aged adult with a history of well-localized pain to the
2nd MTP joint that is aggravated with activities and relieved with rest.-
It primarily affects the 2nd metatarsal head (2).
-
Rarely, the 3rd or other metatarsal heads may be involved.
-
It may be unilateral or bilateral.
-
-
Stages of involvement:
-
Early stages may show mottling of the metatarsal head or central collapse on radiographs.
-
Moderate disease shows flattening or collapse of the metatarsal head along with osteophytes or loose ossicles.
-
Late stages include loss of joint space and arthritis.
-
Epidemiology
Occurs more often in females than in males
Incidence
The true incidence is unknown because many cases are asymptomatic and discovered incidentally on radiographs (2).
Prevalence
Most common in 13–18-year-olds, with symptoms occasionally persisting into adulthood (1,2)
Risk Factors
-
Running
-
Dancing
-
Long 2nd metatarsal
Etiology
-
This disorder is characterized by AVN of the involved metatarsal head (Fig. 1).
-
Impaired microcirculation to bone (3,4)
-
Acute trauma
-
Repetitive microtrauma or overuse
-
The fact that the 2nd metatarsal is the longest metatarsal and is relatively immobile subjects it to increased stress (3).
Signs and Symptoms
-
Pain about the 2nd MTP joint is aggravated with activity and alleviated by rest.
-
Running or sports often is associated with increased pain.
-
Tenderness and soft-tissue thickening about the MTP joint may occur.
-
Stiffness of affected MTP joint may develop.
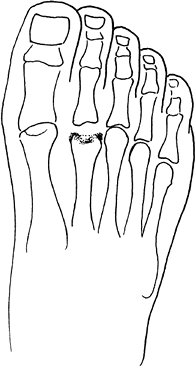 Fig. 1. Freiberg disease involves AVN of the 2nd metatarsal head.
Fig. 1. Freiberg disease involves AVN of the 2nd metatarsal head.
Physical Exam
-
Decreased joint ROM
-
Tenderness to palpation
-
Swelling after activity
-
Pain on toe-raising
Tests
Imaging
-
Radiography: Standing foot radiographs:
-
AP, oblique, and lateral views
-
Early findings include osteopenia and mild subchondral lucency.
-
Later stages show enlargement and flattening of the metatarsal head, sclerosis, cystic changes, and osteophytes.
-
End-stage disease shows arthritic narrowing and destruction of the joint.
-
-
Occasionally, in early or occult cases,
radiographs may be unremarkable and technetium bone scan or MRI may
help confirm the diagnosis.-
Bone scan shows focal intense uptake at the involved metatarsal head (3).
-
MRI shows bony edema with osteonecrosis of head.
-
Pathological Findings
-
Typical findings include:
-
Synovitis, loose bodies, osteophytes
-
Metatarsal head osteonecrosis, with fibrosis of the marrow space, spicules of dead bone, resorption, and collapse (2)
-
Arthritic changes with loss of cartilage
-
Differential Diagnosis
-
Idiopathic synovitis
-
Inflammatory arthritides
-
Acute fracture
-
Sprain of MTP joint
-
Metatarsal stress fracture
-
Morton neuroma
P.149
General Measures
-
Patients should avoid or limit activities that cause pain, especially running, jumping, and dancing.
-
Early disease may be treated with a hard-soled shoe, fracture boot brace, or a walking cast.
-
Symptoms may be relieved by using a metatarsal pad just proximal to the involved metatarsal head (1).
-
Taping or strapping the toe can help to immobilize the joint.
-
Judicious use of intra-articular corticosteroid injections may relieve synovitis.
-
Late stages of the disease may require surgery.
Medication
NSAIDs may alleviate swelling and pain.
Surgery
-
Surgery is indicated if nonoperative measures are unsuccessful.
-
Treatment options include (2):
-
Synovectomy
-
Joint debridement, including removal of fibrosis, loose bodies, and osteophytes (3)
-
Bone grafting of the metatarsal head if no flattening or joint surface collapse is present (3)
-
Dorsiflexion osteotomy of the involved metatarsal to rotate healthier plantar cartilage to articulate with the phalanx (4)
-
Metatarsal head resection arthroplasty (3)
-
Prosthetic joint replacement is not recommended because of transfer metatarsalgia, bony resorption, and implant failure.
-
Prognosis
In most patients, symptoms abate after the acute period and are replaced by an occasional ache.
Complications
-
Collapse of joint surface
-
Arthritis of the second MTP joint
-
Mechanical unloading of the joint with transfer metatarsalgia
References
1. Freiberg AH. The so-called infraction of the second metatarsal bone. J Bone Joint Surg 1926;8A: 257–261.
2. Katcherian DA. Treatment of Freiberg’s disease. Orthop Clin North Am 1994;25:69–81.
3. Helal B, Gibb P. Freiberg’s disease: a suggested pattern of management. Foot Ankle 1987;8: 94–102.
4. Kinnard P, Lirette R. Dorsiflexion osteotomy in Freiberg’s disease. Foot Ankle 1989;9:226–231.
Additional Reading
Daniels TR. Osteochondroses of the foot. In: Myerson MS, ed. Foot and Ankle Disorders. Philadelphia: WB Saunders, 2000:785–799.
Codes
ICD9-CM
732.5 Freiberg disease (osteochondrosis, metatarsal head)
Patient Teaching
Activity
-
Explain the concept of AVN, including the
slow process of revascularization, and warn that joint collapse may
occur if weight is borne prematurely. -
Describe activities likely to exacerbate the disorder, such as running and jumping.
-
Suggest substitute activities such as swimming.
FAQ
Q: What are the possible causes of Freiberg infraction (osteonecrosis of metatarsal head)?
A:
Overuse, trauma, vascular impairment, inflammatory disease, increased
2nd metatarsal length, and immobility of 2nd metatarsal leading to
increased stress.
Overuse, trauma, vascular impairment, inflammatory disease, increased
2nd metatarsal length, and immobility of 2nd metatarsal leading to
increased stress.
-
How is Freiberg infraction treated?
-
Rest, unloading or protection of the MTP
joint, NSAIDs, and corticosteroid injections are standard nonoperative
measures. Surgery is considered after failure of these methods.
