Anterior Glenohumeral Instability: Conservative Treatment, Traumatic and Multidirectional
III – Shoulder Reconstruction > Part B – Evaluation and Treatment of
Shoulder Disorders > 34 – Anterior Glenohumeral Instability:
Conservative Treatment, Traumatic and Multidirectional
injury. Anterior dislocation is usually associated with a shoulder that
is positioned in abduction and external rotation with an anteriorly
directed force on the humeral head.
taken to complete a comprehensive examination of the entire upper
extremity for any evidence of neurovascular injury, with special care
to examine the axillary and musculocutaneous nerve distributions.
Shoulder dislocation has been shown to result in clinically apparent
neurologic injury in about 10% of patients.1
Although most of these injuries are clinically insignificant and
recovery is complete, appropriate documentation is important. Accurate
examination of neurologic function is vital prior to any reduction
maneuver. Although neurologic studies are not routinely recommended,
patients who present with initial muscular paralysis may be examined
with electromyogram (EMG) and nerve conduction studies at least 3 weeks
after the injury if clinical recovery does not occur.
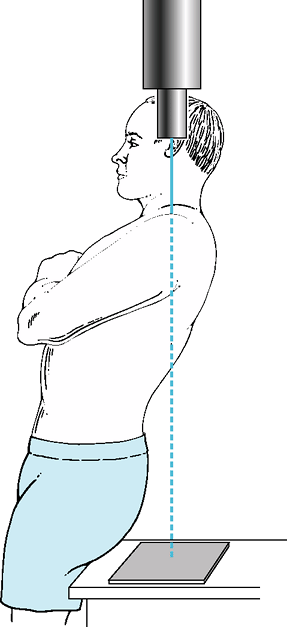
include a minimum of three views and must include an adequate axillary
view. Patients and staff may be reluctant to perform an axillary
radiograph owing to concerns about pain with arm positioning. However,
an adequate axillary radiograph can be safely obtained using a Velpeau
view (Fig. 34-1).
to the glenoid) and fractures of the humeral neck, glenoid, or
tuberosities are not uncommon and should be noted prior to reduction to
avoid confusion with an iatrogenic injury. Large humeral head
impactions (engaging Hill-Sachs lesions) and glenoid bone loss have
been identified as poor prognostic predictors of outcome in patients
who undergo arthroscopic instability repair.2
glenohumeral joint, an injury to the anterior soft tissues of the
shoulder occurs with detachment of the labrum and the inferior
glenohumeral ligament complex from the anteroinferior aspect of the
glenoid Bankart lesion.3 Although
multiple intra-articular injuries have been documented with arthroscopy
after shoulder dislocation, Bankart lesions have been described as the
“essential” lesion of shoulder instability and are seen in more than
90% of acute, traumatic shoulder dislocations.4
However, labral tearing alone is often not enough to lead to recurrent
shoulder instability and is usually associated with capsular
stretching. Initial management, both operative and nonoperative, is
directed at the management of these labral and capsular injuries.
attempting reduction of the glenohumeral joint. Although some
physicians are able to successfully reduce shoulders without sedation
on the playing field or immediately after a dislocation event, muscle
spasm and pain occur, with most patients requiring medication to assist
with the reduction maneuver. Injection of the glenohumeral joint with
intra-articular lidocaine has been found to be a safe and effective
method of analgesia to assist with reduction maneuvers.5
With this method, 10 to 15 mL of 1% lidocaine is injected into the glenohumeral joint.
 |
|
Figure 34-1 Positioning for the Velpeau axillary view is easy to perform.
|
literature for anterior-inferior dislocations. Postreduction
radiographs with at least three views including an axillary are
recommended to evaluate the glenohumeral joint for a complete
concentric reduction and the presence of any fracture.
In this method the patient lies in the supine position with a sheet
around the upper thorax. An assistant provides a steady countertraction
force to the thorax while the surgeon applies steady gentle traction to
the arm in the direction of the dislocation.
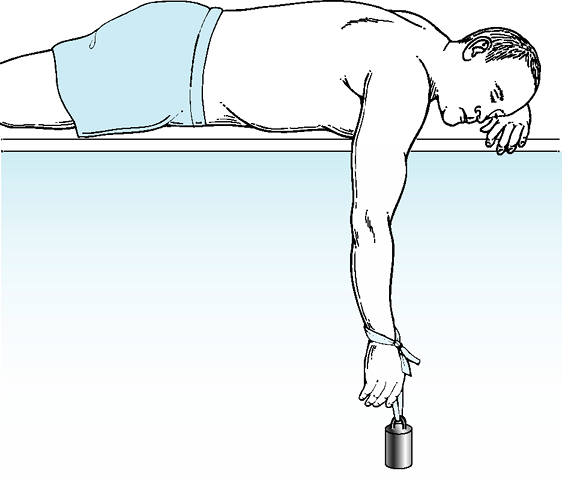
The patient is placed prone and the arm allowed to hang off the side of
the table perpendicular to the body. A light weight (approximately 5
pounds) is attached to the wrist, and the patient is allowed to relax.
Reduction is usually achieved within 10 to 20 minutes as the gentle
prolonged traction allows muscle relaxation and reduction of the
glenohumeral joint.
The reduction is performed with the patient in the supine position, and
the affected elbow flexed to 90 degrees with the arm adducted to the
level of the chest and the shoulder flexed forward 20 degrees. With the
elbow stabilized, the surgeon gently externally rotates the shoulder
with minimal force until the shoulder is reduced. Elderly patients or
those with subclavicular dislocations should not undergo this technique
because of the risk of iatrogenic fracture.
glenohumeral joint is concentric on radiographic examination, a period
of immobilization is warranted to maintain reduction, promote healing
of the injured soft tissues, and decrease the chance for recurrent
dislocations. Recommendations for length of immobilization of acute
dislocations are usually 4 to 6 weeks.
is debated, most authors recommend use of a simple sling with the
shoulder in the internally rotated position. Immobilization of the
shoulder in external rotation has recently been suggested. With this
method, a brace is used to immobilize the shoulder in the externally
rotated position. This position has been shown on MRI to reduce
anterior joint cavity volume and allow a more anatomic reduction of the
Bankart lesion to the glenoid neck and rim owing to increased tension
on the anterior soft tissues and subscapularis muscle. This position is
not tolerated well by most patients. Further studies examining the role
of external rotation bracing in the immediate postinjury period will be
required.8,9
regain shoulder motion and strength. Motion exercises including
active-assisted motion such as pulley and wand therapy are started
after the immobilization period. Rotator cuff, periscapular, and body
core strengthening and neurore-education are instituted after pain and
motion have improved.
special challenges. In uncomplicated initial cases, return to play or
activities is allowed only when range of motion and strength are equal
to the uninjured shoulder.10 Special
braces designed to limit overhead motion (abduction and external
rotation) have been used with varying degrees of success to prevent
instability so that athletes can return to play after in-season
dislocation. If the athlete has recurrent instability in season,
athletes and their parents should have a thorough understanding of the
risks of continued participation with a grossly unstable shoulder.
dislocation are mixed and seem to depend on the age of the patient and
desire to continue participation in the inciting event. Patients 18
years old or younger and contact athletes
have
higher rates of recurrent dislocation and have been reported to have
recurrent instability in >90% of patients with standard nonoperative
regimens (immobilization in internal rotation in a sling, therapy, and
return to activities). This high recurrence rate has led some authors
to pursue other forms of nonoperative therapy such as initial
immobilization in external rotation to minimize the rate of recurrence.
Early results from multicenter trials are not yet available.8,9
Other authors have explored early operative intervention when managing
younger patients with arthroscopic Bankart repair with short-term
results that have been favorable.11
Long-term sequelae of recurrent shoulder instability include
glenohumeral arthritis and have been identified in approximately 20% of
patients with long-term follow-up.12
 |
|
Figure 34-2 Stimson technique for glenohumeral reduction.
|
can be managed with conservative treatment and rehabilitation. Although
prolonged weakness of the shoulder may be owing to neurologic injury,
rotator cuff tearing is known to occur in patients older than 35 years
of age. Patients with continued weakness of the rotator cuff after a
few weeks of rehabilitation should be examined closely for cuff tearing
and may require appropriate imaging. Patients with tears of the
subscapularis are particularly prone to developing recurrent
instability and should be aggressively managed with operative treatment.13,14
Patients with subscapularis tearing may demonstrate increased passive
external rotation of the shoulder and inability to perform lift-off,
belly-press, or bear-hug tests.15
who fail nonoperative intervention and continue to dislocate despite
aggressive rehabilitation. Patients with irreducible dislocations or
open injuries warrant urgent surgical intervention. The treatment of
young patients (<18 years of age) or contact athletes with acute
dislocations is controversial, and recommendations continue to emerge.
Although characterization of what constitutes a chronic dislocation is
not well-defined in the literature, patients with a shoulder
dislocation present for ≥3 weeks are managed much differently than
those with acute dislocations and frequently require operative
intervention. These patients are generally cognitively impaired or
multitrauma patients and should undergo attempts at closed reduction
only in a well-controlled setting with adequate sedation and muscle
relaxation to avoid iatrogenic fracture or neurovascular injury.
define. Diagnosis of MDI is usually subjective, and agreement on
classification has not been achieved.16
However, it is generally accepted that patients with MDI have
instability in more than one direction (anterior, inferior, or
posterior). The treatment of MDI was first defined by Neer and Foster.17 Our understanding continues to evolve and is the subject of several ongoing studies.
patulous inferior capsule that increases glenohumeral joint volume,
thus diminishing the checkrein effect of the glenohumeral ligaments.
Rotator interval tissue is usually thinned and less robust than normal.
Although the tissue in patients is often less than ideal, neurologic
abnormalities also exist and seem to play a key role in the MDI
syndrome,18 A large joint capsule combined with loss of proprioceptive
control of the rotator cuff likely leads to loss of concavity
compression. Periscapular muscle control for scapular positioning may
lead to inappropriate glenoid position, thus leading to instability.
This is supported by recently reported data that atypical patterns of
muscle activity with resulting dysfunctional neuromuscular control of
the rotator cuff and periscapular musculature is a major contributing
factor to the pathologic cause of MDI.19,20
frequent complete dislocation of the shoulder, most patients with MDI
complain of vague sensations of pain or instability with routine
activities of daily living or at the end points of motion. MDI is seen
in two broad categories of patients: patients with general ligamentous
laxity at baseline, and patients who have long-standing microtrauma
with no discreet injury (swimmers, gymnasts, throwers, weight lifters,
and patients involved in racquet sports).
demonstrate hyperextendable joints (elbows, knees, wrists,
metacarpophalangeal). These patients generally have no tear of the
labrum (Bankart lesion), but may have an excessively “loose” shoulder
with an enlarged inferior capsular pouch. Patients with recurrent
microtrauma also frequently have loose shoulders from acquired
activities, such as swimming, that require extreme ranges of motion for
maximum performance and result in stretching of the shoulder capsule
through repetitive stress. However, in these patients, an acute event
occurs causing injury to the already capacious capsule. These patients
may have a labral or capsular tear and should be differentiated from
patients with generalized ligamentous laxity.
findings. Loose shoulders are common findings in young patients
(particularly girls), and reproduction of new or pathologic instability
leading to the patient’s symptoms should be the focus of the
examination. Examination of the asymptomatic shoulder is important and
can give insight to abnormalities in the affected shoulder.
Identification of a sulcus sign with prominent humeral head depression
below the acromion with gentle inferior traction applied to the wrist
indicates lax capsular rotator interval tissue. Asymmetric shoulder
laxity can be identified by examining for the amount of humeral head
translation off of the glenoid rim. Examination under anesthesia is
extremely useful and allows the surgeon to examine the shoulder with
variable amounts of rotation to identify areas of asymmetrical laxity.21,22
rehabilitation. An adequate understanding of the underlying problem
seems to facilitate patient compliance. Functional activities should
not only include strengthening of the rotator cuff and periscapular
muscles, but also should emphasize retraining of the scapula and
dynamic stabilizers of the shoulder for appropriate positioning of the
glenoid. Patients should be discouraged from any voluntary subluxation.
Rehabilitation may take several months, and patients (and physicians)
may become frustrated. However, a minimum of 6 months of therapy (some
authors recommend a year) is required for maximum benefit.
MDI is defined, long-term outcomes of patients with MDI are generally
favorable with nonoperative treatment. Satisfactory results were
reported in 29 of 33 (88%) patients with MDI by Burkhead and Rockwood.23
Children with voluntary dislocation/subluxation of the glenohumeral
joint usually do well long term with no increase in osteoarthritis in
adulthood and should be managed conservatively.24
an adequate trial of therapy and have continued instability. Surgery
for pain alone in patients with MDI has not been shown to be effective.
Operations should be avoided for patients who are unable to cooperate
with therapy or who have cognitive or mental health issues that would
preclude full participation in a postoperative rehabilitation program.
CP, Coene LN, Brand R, Tavy DL. The incidence of nerve injury in
anterior dislocation of the shoulder and its influence on functional
recovery. A prospective clinical and EMG study. J Bone Joint Surg Br. 1999;81:679–685.
SS, De Beer JF. Traumatic glenohumeral bone defects and their
relationship to failure of arthroscopic Bankart repairs: significance
of the inverted-pear glenoid and the humeral engaging Hill-Sachs
lesion. Arthroscopy. 2000;16:677–694.
DE, Roberts T. Intraarticular lidocaine versus intravenous analgesic
for reduction of acute anterior shoulder dislocations. A prospective
randomized study. Am J Sports Med. 1995;23:54–58.
KK, Dua A, Malhotra R, et al. The external rotation method for
reduction of acute anterior dislocations and fracture-dislocations of
the shoulder. J Bone Joint Surg Am. 2004;86:2431–2434.
E, Sashi R, Minagawa H, et al. Position of immobilization after
dislocation of the glenohumeral joint: a study with use of magnetic
resonance imaging J Bone Joint Surg Am. 2001;83:661–667.
E, Hatakeyama Y, Kido T, et al. A new method of immobilization after
traumatic anterior dislocation of the shoulder: a preliminary study. J Shoulder Elbow Surg. 2003;12:413–415.
CR, Wilckens JH, DeBerardino TM, et al. A prospective, randomized
evaluation of arthroscopic stabilization versus nonoperative treatment
in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30:576–580.
L., Augustini BG, Fredin H, et al. Primary anterior dislocation of the
shoulder in young patients. A ten-year prospective study. J Bone Joint Surg Am. 1996;78:1677–1684.
RJ, Neviaser TJ, Neviaser JS. Concurrent rupture of the rotator cuff
and anterior dislocation of the shoulder in the older patient. J Bone Joint Surg. 1988;70:1308–1311.
EG, Kim TK, Park HB, et al. The effect of variation in definition on
the diagnosis of multidirectional instability of the shoulder. J Bone Joint Surg Am. 2003;85:2138–2144.
CS II, Foster CR. Inferior capsular shift for involuntary inferior and
multidirectional instability of the shoulder. A preliminary report. J Bone Joint Surg Am. 1980;62:897–908.
SM, Warner JJP, Borsa PA, et al. Proprioception of the shoulder joint
in healthy, unstable, and surgically repaired shoulders. J Shoulder Elbow Surg. 1994;3:371–380.
RH, Irving JF. Evaluation and classification of shoulder instability.
With special reference to examination under anesthesia. Clin Orthop Relat Res. 1987;223:32–43. Review.
