Upper Extremity
problem despite improved obstetric techniques. Predicting a spontaneous
recovery requires identification of the level and severity of the
brachial plexus injury. Up to 92% of injured infants have a complete
recovery by 3 months of age. Infants who do not show recovery,
especially biceps function, by 3 months of age have an increased risk
of long-term disability and may benefit from neural microsurgery. Upper
extremity contracture and weakness may benefit surgical reconstructions
that include rotational osteotomies, tendon releases, and tendon
transfers.
-
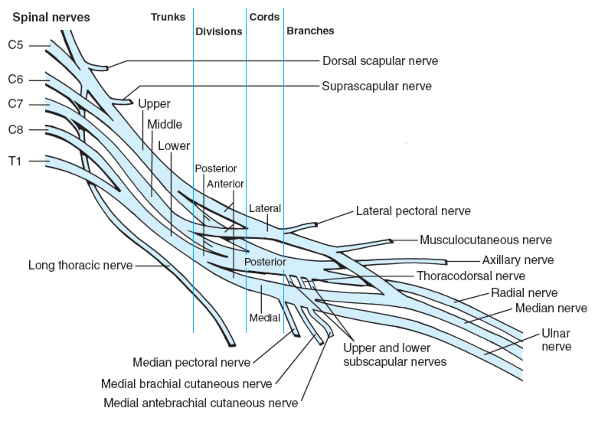
The brachial plexus is the amalgamation of ventral nerve roots arising from C5 to T1 (Fig. 28.1-1).
-
After the nerve roots exit their
respective neural foramina, they combine to form three well-defined
trunks— upper (C5, C6), middle (C7), and lower (C8, T1). -
The trunks divide into anterior and
posterior divisions, forming a posterior, medial, and lateral cord;
named with reference to subclavian artery proximity. -
The cords terminate in numerous branches, each supplying individual myotomes, and dermatomes.
-
The clavicle is an important landmark
separating the brachial plexus into proximal (roots, trunks, and
divisions) and distal (cords and branches) portions. -
The plexus lies in close proximity to the subclavian and axillary vessels.
-
The sympathetic chain lies adjacent to the nerve roots at the neural foramina of C8 and T1.
traction on the brachial plexus, most commonly the upper trunk (C5 and
C6) (Fig. 28.1-1). Traction usually occurs
during the late phase of delivery when the head is pulled laterally
away from the shoulder. Risk factors for an obstetric brachial plexus
injury include the following:
-
High birthweight
-
Prolonged labor
-
Breech presentation
-
Shoulder dystocia
-
Multiparous pregnancy
-
The incidence of brachial plexus injuries is reported to be 0.87 to 2.5 per 1,000 live births.
-
No association with race, gender, or maternal age has been described.
essential in understanding the effects of an injury. The prognosis of
an injury deteriorates when the nerve roots are avulsed from the spinal
cord (preganglionic lesions). Indications of a preganglionic lesion
include Horner syndrome, phrenic nerve palsy, and scapula winging
resulting from long thoracic nerve palsy.
 |
|
Figure 28.1-1
Structures of the brachial plexus. (Adapted from Waters PM. Obstetric brachial plexus injuries: evaluation and management. J Am Acad Surg 1997;5:206.) |
contribute to the suprascapular, axillary, and musculocutaneous nerves.
These nerves innervate the rotator cuff, deltoid, biceps, and
brachialis muscles. Therefore, weakness is present in shoulder
abduction and external rotation as well as elbow flexion. If C7 is also
involved, triceps elbow extension is weak. Hand function is more
affected by lower trunk lesions that involve C8 and T1, which are
usually preganglionic injuries (proximal).
-
Upper plexus palsy (Erb): C5, C6, and sometimes C7
-
Intermediate plexus palsy: C7 and sometimes C8, T1
-
Lower plexus palsy (Klumpke): C8 and T1
-
Total plexus palsy
usually a postganglionic injury, unless the delivery is breech, which
is associated with a preganglionic injury. An entire plexus injury is
less frequent and intermediate or lower plexus palsies are rarely seen.
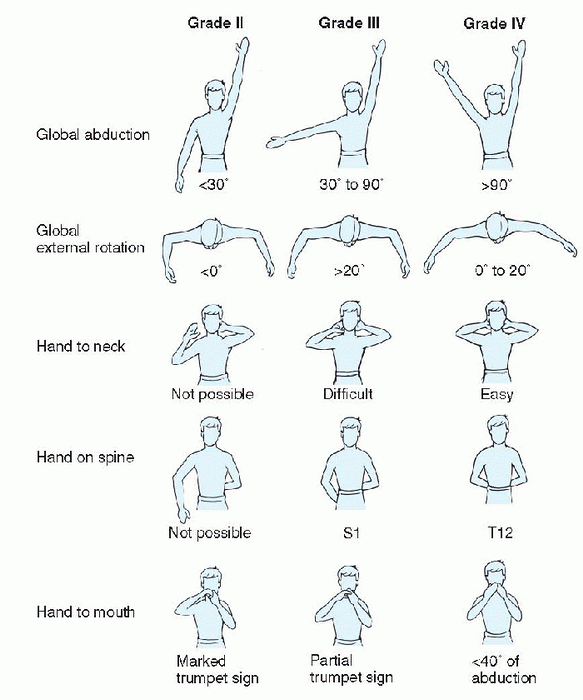
used in young children to assess upper trunk function and includes five
categories: global shoulder abduction, external rotation, hand to neck,
hand on spine, and hand to mouth. Each category is graded 0 to 5 with
grade 0 being no muscle contraction and grade 5 being normal voluntary
muscle contractions. Fig. 28.1-2 diagrams the intermediate grades II to IV. Muscle strength grading is similar to that used for adults.
period must be obtained from the parents. This information should
include complications during pregnancy, such as diabetes and toxemia.
The duration of the labor, method of delivery, and ease of delivery
should also be noted. An early postnatal history of respiratory
distress, clavicle or humerus fractures, Horner syndrome, and paralysis
is also helpful.
-
Spontaneous movements of the shoulder,
elbow, wrist, and finger are the best methods used to define the
severity of the neural injury.-
□ Performing neonatal reflexes, such as the Moro and asymmetric tonic neck reflexes, assists in providing this information.
-
-
Movements with and against gravity are
important for grading muscle strength and can be performed by placing
the infant in gravity-eliminated positions and stimulating specific arm
movements with toys. -
The “cookie test” is helpful in testing elbow flexion at 9 months.
-
□ During the test, the child is encouraged to place a cookie into the mouth with the affected shoulder adducted.
-
□ “The reverse cookie test” is similar
and requires the child to remove the cookie from the mouth with the
uninvolved extremity restrained.
-
-
Total plexopathy presents with a flail and insensate upper extremity.
-
Flexion of the fingers should not be
mistaken for active motion since this usually occurs as a result of the
tenodesis effect, whereby tension on the digital flexors is increased
with wrist extension leading to finger flexion. -
In Klumpke palsy, hand paralysis is present, but shoulder and elbow function are maintained.
-
Infants with a brachial plexus injury have a tendency to turn their head away from the involved arm.
-
Horner syndrome: characterized by
ipsilateral facial ptosis, enophthalmos, anhidrosis, and myosis (TEAM)—
usually indicates an avulsion injury of the lower trunk as the
sympathetic chain lies adjacent to the C8 and T1 nerve roots. -
Phrenic nerve paralysis should be
excluded preoperatively by observing abdominal motion and confirmed on
fluoroscopy (flattened hemidiaphragm and no motion with respiration) or
chest radiographs. -
Plication of the diaphragm may be necessary prior to surgery.
-
Other diagnoses should be ruled out by a careful physical examination.
-
□ Pseudoparalysis can be a result of compression on the brachial plexus by fractures of the clavicles, humeri, and ribs.
-
□ Shoulder dislocations have also been reported to cause brachial plexus palsies.
-
 |
|
Figure 28.1-2
Modification of the Mallet classification for assessing upper trunk function in young children. Grade I is no function and grade V is normal function. Grades II, III, and IV are depicted for each category. (Adapted from Waters PM. Obstetric brachial plexus injuries: evaluation and management. J Am Acad Surg 1997;5:207.) |
(CT-myelogram), and magnetic resonance imaging (MRI) are often used
preoperatively in adult plexopathies to identify pseudomeningoceles and
nerve root avulsions. True-positive rates of 84% for myelography and
94% for CT-myelography have been reported. MRI has the advantage of
being noninvasive and allowing for imaging of the entire plexus, while
having a true-positive rate similar to CT-myelography. While some
experts have found preoperative imaging helpful, many others question
the value. The treating physician must justify the potential
information gained from these tests as they are often invasive and
require general anesthesia in the pediatric population.
on radiographs in infants since the glenoid and humeral head have not
yet ossified. A CT, MRI, or arthrogram is sometimes necessary for
diagnosing a glenohumeral dislocation and can help identify deformities
of the glenoid or humeral head.
determine neural injury severity and location have provided unreliable
results. Denervation is uncommon in infants despite brachial plexus
ruptures and avulsions. In addition, sensation in a specific dermatome
is also hard to assess in infants. Therefore, many surgeons do not
routinely perform electrodiagnostic testing, although others claim
potential benefits in determining prognosis.
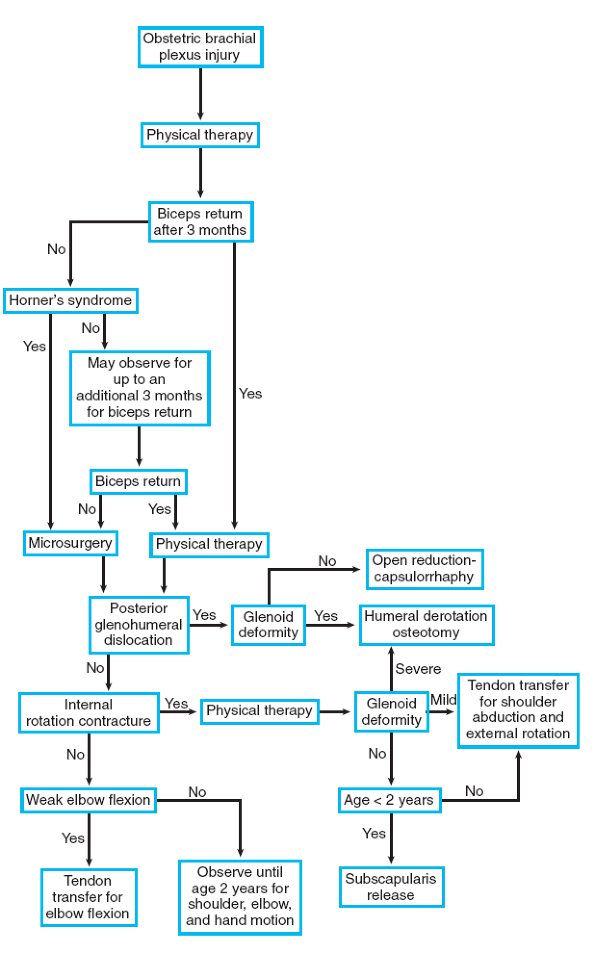
brachial plexus injury is to maximize upper-extremity function.
Treatment begins shortly after diagnosis with physical therapy. The
role of therapy is to limit further joint contracture and increase
passive motion, to ensure effective muscle function after
reinnervation. Physical therapy takes the form of passive joint
stretching, stretch casting, and nighttime splints. Recent interest has
focused on the use of botulin toxin to limit muscle imbalances.
 |
|
Algorithm 28.1-1 Algorithm for the management of obstetric brachial plexus injuries.
|
-
Hand: sensation in the hand and fingers
-
Elbow: flexion greater than grade III (ability to independently feed)
-
Shoulder: stability and abduction with external rotation greater than grade III.
however, are irreparable and require nerve transfers, neurotization, or
tendon transfers. Current surgical recommendations are as follows:
-
Extraforaminal ruptures
-
□ Neuroma resection, and sural nerve grafting
-
-
Upper trunk ruptures
-
□ Sural nerve grafts from C5 and C6 roots to the suprascapular nerve and musculocutaneous nerve or lateral cord
-
□ Nerve grafts from the upper-trunk
posterior division to the posterior cord to ensure elbow extension
(triceps) and deltoid function, respectively
-
-
Upper root avulsions
-
□ Nerve transfers from a branch of the spinal accessory nerve to the suprascapular nerve
-
□ Reestablish continuity of the
musculocutaneous nerve, lateral cord, and the posterior cord using
thoracic intercostal nerve transfers or grafts
-
-
Total plexopathy avulsions
-
□ Surgical options depend on the number of roots not avulsed and therefore amenable to nerve grafting
-
□ If possible, nerve grafts from the C5
and C6 roots to the median nerve and ulnar component of the medial cord
to restore hand sensation and function -
□ Spinal accessory and intercostal nerve transfers to the suprascapular nerve and the posterior and lateral cords.
-
-
Total plexus palsy with flail arm after 1 month and Horner syndrome
-
C5, C6 palsy after a breech delivery showing no signs of recovery by 3 months
prior to 3 months of age for anesthesia safety reasons. The literature
suggests microsurgical techniques prior to 6 months of age to ensure
optimal results.
external rotation is limited, and the humeral head is palpable
posteriorly. Dislocations can occur in infancy and may require an
arthrogram, ultrasound, CT, or MRI to confirm this diagnosis as the
humeral head is not yet ossified, and therefore poorly visualized with
radiographs.
-
Open reduction and capsulorrhaphy are necessary when a glenohumeral dislocation is present.
-
An anterior release and posterior capsulorrhaphy are performed through combined anterior and posterior approaches.
-
The shoulder is then immobilized in a spica cast for 4 weeks.
imbalance of the shoulder resulting in weak abduction and external
rotation while maintaining adduction and internal rotation. Subluxation
of the glenohumeral joint eventually occurs, which leads to internal
rotation contractures, and glenohumeral deformities.
-
A subscapularis release at 1 year of age
should be considered when the child has failed physical therapy
stretching and external rotation is less than 30 degrees when the
shoulder is adducted. -
The subscapularis is released from its origin as shoulder instability can result if detached from the humeral insertion.
function to patients with incomplete brachial plexus recovery in early
childhood, and are usually performed between 2 and 5 years of age.
Important principles that must be adhered to whenever performing tendon
transfers include the following:
-
Passive functional range of motion of the joint must be obtained preoperatively with physical therapy and dynamic splinting.
-
The joint must be reduced and congruent, which may require arthrogram, CT, or MRI confirmation.
-
Donor muscle strength must be at least a
grade 4 or 5 and not previously paralyzed, as the muscle grade will
diminish by one grade with tendon transfer. -
The donor muscle should have adequate excursion to perform the necessary function.
-
Each muscle should perform only one function.
including external rotation and abduction weakness, an anterior release
of the pectoralis major with transfer of the latissimus dorsi and teres
major muscles to the rotator cuff is helpful.
-
Anteriorly, the pectoralis major tendon is lengthened at its humeral insertion.
-
Posteriorly, the latissimus dorsi and teres major tendon insertion is transferred to the greater tuberosity.
-
This procedure is best performed between the ages of 2 to 7 years.
shoulder abduction, incurred as a result of deltoid weakness.
Techniques include transferring the pectoralis major to the deltoid,
transferring the trapezius to the deltoid insertion, and transferring
the short head of the biceps and long head of the triceps to the
acromion. These methods have been shown to be helpful, but results are
limited.
-
If severe glenohumeral deformity with
fixed internal rotation is present in an adolescent, a humeral
derotation osteotomy is preferred. -
A humeral osteotomy is made proximal to the deltoid insertion with the distal humerus placed in 30 degrees of external rotation.
pain, instability, articular deformity, and arthritis that cannot be
addressed with the above procedures. Functional
scapular
muscles and scapular stability are required for shoulder arthrodesis.
Prerequisites for a glenohumeral arthrodesis include a sensate and
functional arm and hand.
trunk brachial plexus palsy leads to weak elbow flexion. Many
procedures have been described to restore partial elbow flexion
function. One of the earliest transfers described included a transfer
of the origin of the flexor-pronator muscle group proximally. Although
simple to perform, this procedure may exacerbate a pronation deformity.
Results of this procedure allow elbow flexion of 3 to 5 lbs with a
range of motion between 30 and 100 degrees.
transpositions of the pectoralis major or the latissimus dorsi. The
procedure is technically demanding and requires transferring both the
origin and insertion of the muscle. Other procedures described in the
past, which are rarely performed today, include an anterior transfer of
the triceps insertion and a transfer of the sternocleidomastoid muscle
through a fascia lata graft.
have paralysis of the pronators with a supination contracture of the
forearm.
-
Transfer of the biceps tendon insertion to the radial aspect of the radial neck can be done to provide pronation.
-
If the forearm cannot be passively pronated, a release of the interosseous membrane is necessary.
-
An elbow capsuloplasty can be performed to reduce a subluxated or dislocated radial head.
-
The elbow is placed in a long arm cast with flexion at 90 degrees and pronation at 20 degrees for 4 to 6 weeks.
procedure maintain their correction, many surgeons now perform an
osteoclasis of the radius and ulna with intramedullary fixation. The
osteotomy can also be performed with a biceps tendon transfer to
decrease the recurrence rate.
-
Most newborns with a brachial plexus injury will do well without surgical intervention and have a complete spontaneous recovery.
-
For patients who do not show recovery by 3 to 6 months, microsurgery has been shown to be beneficial.
-
Patients who undergo microsurgery are
more likely to obtain a higher level of function than similar patients
treated nonoperatively. -
Children who undergo nerve grafting appear to have improved outcomes after secondary reconstructive procedures.
-
Secondary reconstructions (e.g., tendon
transfers and osteotomies) are clearly beneficial to patients with
contractures and deformities, allowing improved range of motion to
place the arm in a functional position and provide muscle strength of
grades III or IV.-
□ Patients are able to achieve improved function of their shoulder, elbow, and hand.
-
□ Function may not be completely normal even with microsurgery and secondary reconstruction procedures.
-
JB, Allan CH. Tendon transfers about the shoulder and elbow in
obstetrical brachial plexus palsy. J Bone Joint Surg (Am)
1999;81:1612-1626.
AG, Schute PC, Shively JL. Brachial plexus birth palsy: a 10-year
report on the incidence and prognosis. J Pediatr Orthop 1984;4:689-692.
error is great but malformations are fortunately rare. Amelia (complete
absence of a limb), phocomelia (almost complete absence), or ectromelia
(partial absence) can occur and defects may involve the whole width of
the limb (transverse defect), or the pre- or postaxial border
(longitudinal defect). There may be no parts distal to the defective
portion (terminal defect) or the middle portion of a series of limb
segments may be defective (intercalary defect).
-
Most congenital deformities of the upper
extremity occur in the embryonic period from the third to the seventh
weeks of gestation. -
Many limb abnormalities are isolated
lesions that occur sporadically; and rarely, multiple family members
have the same limb abnormalities. -
Limb defects also can be associated with non-limb malformation or be part of a genetically based multiple malformation syndrome.
-
When transverse terminal defects are present, the origin is most likely vascular.
-
Limb deficiency defects occur in 4.80 to 5.97 per 10,000 live births.
-
Upper extremity involvement is significantly more common than lower extremity involvement.
-
Unilateral defects occur in 75% to 80% and are more often right-sided, especially in the radius.
-
Associated anomalies are found in up to 53% (musculoskeletal defects most frequent).
-
Other abnormalities, including defects of
the head and neck, cardiovascular system, gastrointestinal tract, and
genitourinary tract are present in one-third of all cases. -
Associated abnormalities are seen most
frequently with radial defects but are not commonly found with ulnar
and transverse terminal lesions.
-
An abnormal limb may be the result of malformation, deformation, disruption, or dysplasia.
-
Malformations are the result of poor
formation of tissue that initiates a chain of additional abnormalities.
Affected structures seldom revert to normal and surgery is usually
required. -
Deformations occur as a result of
mechanical forces applied to a normal embryo or fetus and generally
occur in the third trimester.-
□ Deformities involving the upper extremity have a good prognosis since delivery ends the intrauterine molding.
-
□ Most 6 to 8 months after birth and surgery is uncommon (10%).
-
-
Disruptions are structural defects that
result from destruction of a part that has differentiated normally,
such as congenital constriction ring syndrome. -
Dysplasia describes conditions that arise from the abnormal arrangements of cells into tissues (e.g., hamartoma).
continues to be based on the gross morphologic presentation and it is
not possible to precisely classify all malformations.
|
TABLE 28.2-1 CLASSIFICATION OF UPPER EXTREMITY ANOMALIES
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
-
The initial evaluation should include a
careful history about the pregnancy, the child’s prenatal course, and
family history of similar disorders. -
The history may disclose fetal exposure
to drugs, medications, infectious agents, or maternal metabolic
imbalances that increase the risks of birth defects. -
Examination should include the general
appearance of the child with attention to stature, proportion, head and
facial symmetry and contralateral limb, leaving the affected limb to be
examined last.-
□ Look at the chest for affects in pectoralis major development (Poland syndrome) and the back for any obvious deformity.
-
□ Infants with positional deformations of
the upper limbs should be evaluated for neurologic conditions and
possible associated abnormalities in the cervical spine.
-
-
Radial dysplasia, triphalangeal thumb,
and hemihypertrophy are potentially associated with life-threatening
cardiac, hematopoietic, or tumorous conditions. -
Close communication with the child’s pediatrician is important, particularly if surgery is planned.
-
To date, most heritable upper extremity defects have not been linked to a specific gene locus and cannot be diagnosed in utero using molecular technology.
-
Most frequently affects one upper extremity with usual obvious digital anomalies
-
Short coalesced digits
-
Four types:
-
Fusion of adjacent digits
-
One of the most common congenital hand deformities
-
Males affected twice as frequently as females
-
10% to 40% familial
-
Forms:
-
□ Simple syndactyly—skin alone
-
□ Complex syndactyly—skin and bone
-
□ Complete syndactyly—whole web space
-
□ Incomplete syndactyly—partial web space
-
-
Associated with polydactyly, clefting, symbrachydactyly, or ring constrictions
-
Apert syndrome
-
□ Rare (1 in 45,000)
-
□ Craniosynostosis and severe complex syndactyly involving hands and feet
-
□ Usually arises by new mutation
-
□ Most patients have normal intelligence
-
□ Much can be done with the hands to enhance both function and appearance
-
-
Poland syndrome
-
□ Small or absent pectoralis major and syndactyly
-
-
Radial (thumb duplication), ulna, or central
-
Most common congenital hand anomaly in African Americans (10.7 per 1,000)
-
Twice as common in males
-
Ulnar polydactyly 10 times more common in African Americans than in Caucasians
-
Radial polydactyly occurs with equal racial frequency
-
Central polydactyly is extremely rare
-
Ulnar polydactyly varies from skin tag to duplicated finger
-
Occurs more frequently in males
-
Right more commonly than left
-
Duplication associated with a triphalangeal thumb may be associated with certain syndromes
-
Wassel’s classification of seven categories is based on the level of skeletal division (Table 28.2-2).
|
TABLE 28.2-2 CLASSIFICATION OF DUPLICATED THUMB
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||
-
One in 25,000 births
-
65% of children with bilateral deficiency have a positive family history
-
Most unilateral cases have a positive inheritance
-
Most frequent association is with thumb duplication
-
Less frequently seen with typical cleft
hands, radial dysplasias, congenital heart disease, ear anomalies,
blood dyscrasias, cardiovascular and gastrointestinal tract anomalies
-
Condition in which one or more digits are larger than normal.
-
May occur as an isolated anomaly (pseudomacrodactyly or true macrodactyly) or as part of a congenital syndrome.
-
□ True macrodactyly is noted at birth or soon after and its growth may be static or progressive.
-
□ Pseudomacrodactyly is usually due to soft tissue involvement (not bony).
-
-
Macrodactyly is present in several
congenital syndromes such as neurofibromatosis, Ollier disease,
Maffucci syndrome, and congenital lymphedema.
-
Absent proximal interphalangeal (PIP) joints with normal length of all phalanges
-
Often bilateral with radial digits more severely affected
-
Rare autosomal dominant inherited condition
-
No finger creases over PIP joints
-
A nontraumatic flexion deformity of the PIP joint of one or several fingers
-
Familial cases have an autosomal dominant pattern
-
Frequently associated with Marfan, Holt-Oram, and Poland syndromes
-
Small finger most commonly affected
-
Increasing contracture during growth spurts
-
Differential diagnosis: boutonniere
deformity, triggering (palpable nodule in the palm), congenital absence
of extensor mechanism -
Anomalous lumbricals, a consistent feature
-
Results of splintage variable
-
Surgery continues to evolve, and surgery before deformity is established probably offers best results.
-
Digital angulation in the radioulnar plane
-
A physical sign, not a disease
-
Arises from a disordered growth of bone for a variety of reasons
-
Four categories
-
Splinting alone does not correct.
-
Usually no functional loss
-
Beware of surgical correction complications.
-
Radial and volar curvature of the distal phalanx of the small finger
-
May not become apparent until puberty, progressive curvature
-
Radiographic diagnosis, majority need no treatment
-
Familial with autosomal dominant inheritance, frequent sporadic cases
-
Can be associated with a number of syndromes including Down and Turner
-
A triangular bone with a continuous physis or epiphysis along the shorter side that links the proximal and distal epiphysis.
-
The shape can be triangular, trapezoidal, or almost round.
-
Sporadic, inherited, or associated with many syndromes.
-
The last bone to develop a primary
ossification center shows the greatest disposition toward the anomaly
(middle phalanx of the small finger). -
Delta phalanx does not always produce clinodactyly and clinodactyly is not always the result of delta phalanx.
-
Mild deformity (10 degrees) can be ignored in the older child.
-
Treatment depends on the type of phalanx,
the contribution it makes to the length and deformity, the age at
presentation, and the family’s wishes and expectations. -
Treatment options:
-
□ Physiolysis (Langenskiöld procedure) to remove the tether on the short side and prevent its reformation with a fat graft
-
□ Corrective osteotomy
-
□ Closing is the simplest option, but leads to shortening
-
□ Opening osteotomy decreases the loss of length
-
-
Excision of abnormal phalanx if small
-
Attributed to the formation of amniotic bands in utero
-
Precise etiology is unknown but the
primary event appears to be rupture of the amniotic membrane so that
part of or all of the fetus lies outside the amnion. -
The accepted method of correcting the
circular constriction is to excise the deep part of the constriction
and break the line of the circular scar with Z-plasties.
-
Absence, hypoplasia, duplication, and abnormal attachment of tendons are all recognized.
-
The most commonly encountered functional tendon anomalies involve the thumb.
-
Trigger digits:
-
□ Clicking or snapping is experienced as
the digit moves from flexion to extension. The nodule on the flexor
tendon pops in and out through the annular pulley. -
□ Can be present at birth, occurs most commonly in the thumb.
-
□ May develop during childhood, most commonly in the first year
-
-
Triggering rarely seen, usually parents notice that the child does not extend the interphalangeal joint of the thumb
-
Possibility of spontaneous resolution during the first year of life and no fixed joint changes for 1 to 3 years
-
Consider release at the end of the first year.
-
Absence or hypoplasia of extensor pollicis brevis.
-
Characterized by flexion of the
metacarpal phalangeal (MP) joint and adduction of the first metacarpal
so the thumb lies across the palm.-
□ This is the normal posture for the
first 3 months, so the diagnosis can only be made after 3 months when
this is noted to be persistent.
-
-
Can be an isolated abnormality but more frequently part of a more complex disorder such as a windblown hand.
-
Main differential diagnosis is trigger thumb.
-
Splinting and passive stretching is usually effective by the end of the first year—if not, surgery is indicated.
-
Blauth’s classification is given in Table 28.2-3.
-
Treatment depends on the type and ranges from no treatment necessary to pollicization.
-
Incidence is 0.4 per 10,000 live births.
-
Cases occur sporadically but may be familial, autosomal dominant.
-
Clefting can occur without absence of a
digit, however most cases have absence of one or more digits and may
have varying degrees of polydactyly and syndactyly. -
Often the middle finger alone is missing
and the defect may extend to produce a deep V-shaped cleft with absence
of the metacarpal. -
Frequent synostosis between capitate and hamate.
-
Often bilateral and associated with comparable foot deformities.
-
If untreated, these patients or these “hands” develop remarkable hand function.
-
The deformity is unsightly and surgery can improve cosmesis while maintaining function.
|
TABLE 28.2-3 CLASSIFICATION OF HYPOPLASTIC THUMB
|
|||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||
-
Spectrum varies from a slightly
hypoplastic radius or minor degree of thumb hypoplasia to a total
absence of the radius, thumb, first metacarpal, scaphoid, and trapezium. -
The entire forearm may be shortened with the ulna thickened and bowed radially.
-
The wrist becomes unstable with decreased range of motion.
-
Range of motion of the fingers may be decreased.
-
Overall hand function can be severely limited.
-
Often associated with other congenital defects or syndromes:
-
□ Blood dyscrasias (e.g., Fanconi, TAR [thrombocytopenia-absent radius syndrome])
-
□ Congenital heart anomalies, (e.g., Holt-Oram),
-
□ Craniofacial defects (e.g., Nager)
-
□ Vertebral anomalies (e.g., VATER [vertebral anomalies, anal atresia, tracheoesophageal fistula, renal and radial anomalies])
-
-
The most common nonsyndromic associated anomalies are listed in Box 28.2-1.
-
Prevalence estimated at 1 per 55,000 to 1 per 100,000.
-
In unilateral cases, right is greater than left and opposite thumb is often hypoplastic or defective.
-
Complete absence of the radius is more frequent than partial or hypoplasia.
-
Bayne and Klug’s classification is described in Table 28.2-4.
-
Etiology still uncertain—probably multifactorial
-
Hereditary tendencies not common
-
Treatment options:
-
□ No treatment
-
□ Mild anomalies of the arm
-
□ Severe associated anomalies or syndromes
-
□ Older patients who have adjusted
-
□ Limited elbow flexion in which a straightened hand will not reach the mouth or perineum
-
□ Severe soft tissue contracture that involves the neurovascular structures
-
-
□ Splinting and stretching
-
□ Type I and II deficiencies with mild
radial deviation of the hand and a stable wrist may require only
stretching and maintenance until skeletal maturity.
-
-
□ Surgery
-
□ Severe type II, III, and IV with the hand severely displaced and deviated
-
□ Absent or hypoplastic thumbs and those with soft tissue contractures that cannot be reduced by manipulation and splints
-
□ Ideal time for surgery is age 6 months to 1 year
-
□ Enables soft tissue stretching in the first 6 months
-
-
-
Triphalangeal thumb
-
Radioulnar synostosis
-
Syndactyly
-
Scoliosis
-
Sprengel deformity
-
Club foot
-
Congenital dislocation of the hip
-
Vetriculoseptal defect
-
Lung abnormalities
-
Cleft lip and palate
-
Tracheoesophageal fistula
-
Anal atresia
-
Patent ductus arteriosus
-
Hydrocephalus
-
Deafness
-
Genitourinary tract anomalies
|
TABLE 28.2-4 CLASSIFICATION OF LONGITUDINAL RADIAL DEFICIENCY
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||
-
Incidence is 1 in 100,000 (1:10 ratio with radial deficiency).
-
Many variations and the upper arm elbow, forearm, wrist, and hand can be involved.
-
The elbow is frequently affected and because of the variable clinical picture, a standard treatment plan is difficult.
-
Associated anomalies mainly affect the
musculoskeletal system and the syndromes associated with radial club
hand are exceptional. -
Indication for surgery is not clear.
-
Debate continues about the need to excise the fibrocartilage anlage.
-
Despite the appearance, children adapt well to the functional challenges.
-
Operations on the forearm are difficult
and controversial but improving function of the hand is usually
straightforward and rewarding.
-
Hand: phalangeal and metacarpal synostosis.
-
Wrist: triquetrum to lunate and capitate to hamate most common.
-
Elbow: humeroradial and humeroulnar.
-
Forearm: radioulnar synostosis (most common).
-
Cleary and Omer’s classification is given in Table 28.2-5.
-
Bilateral in 60%
-
Normal pronation and supination within the carpus increases with congenital loss of forearm rotation.
-
Compensation for fixed supination deformity is easier to overcome than fixed pronation deformity.
-
Operative treatment (derotation
osteotomy) at the fusion site probably indicated for excessively
pronated forearm greater than 60 degrees -
Mobilization of the synostosis is difficult to maintain because of re-ankylosis.
-
Most common congenital anomaly of the elbow joint but still uncommon
-
Can occur as an isolated entity or as part of a more generalized skeletal malformation syndrome
-
Other skeletal disorders occur in 60% of cases.
-
Invariably bilateral
-
If unilateral, difficult to distinguish from traumatic origin
-
□ Bowing of the ulna suggests possibility of a traumatic dislocation.
-
□ Arthrography revealing the radial head outside the elbow capsule also suggests a traumatic dislocation.
-
-
Dislocation can be anterior, posterior, or lateral, with variable reports as to the most common.
-
The most characteristic feature radiologically is hypoplasia of the capitellum and a dome-shaped radial head.
-
In most cases, the dislocation causes virtually no noticeable disability in childhood.
-
Treatment is seldom indicated because of the lack of symptoms and normal function.
-
In adolescence and adult life, pain may occur as a consequence of degenerative changes.
-
Radial head excision is best avoided in
the growing child as it may lead to instability of the elbow, cubitus
valgus deformity, shortening of the forearm, and secondary subluxation
of the distal radioulnar joint.
|
TABLE 28.2-5 CLASSIFICATION OF SYNOSTOSIS
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||
|
TABLE 28.2-6 CLASSIFICATION OF SPRENGEL UNDESCENDED SCAPULA
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||
-
Failure of descent of the scapula from
the level of the embryonic limb bud opposite the fifth cervical
vertebrae to its thoracic position -
The failure of descent has been
attributed to tethering scapulovertebral articulations and defective
musculature unable to draw the scapula caudally. -
Most affected individuals have associated anomalies of the clavicle, ribs, vertebrae, and shoulder musculature.
-
□ Present for evaluation of a webbed neck or loss of shoulder motion or both
-
-
The Cavendish classification given in Table 28.2-6 aids in determining treatment.
-
□ Grades 1 and 2: can consider resection of the bony prominence and omovertebral bar
-
□ Grades 3 and 4: require the above for
improved cosmesis and derotation and relocation of the scapula if
shoulder abduction is less than 120 degrees
-
-
Represents the disruption of the normal
sequence of development of the pectoralis major associated with
abnormal development of the hand. -
Most patients with Poland syndrome have a
spectrum of disorders that includes hypoplasia or aplasia of the
pectoralis major, pectoralis minor, serratus anterior, and latissimus
dorsi; rib and costal cartilage defects; absence or hypoplasia of the
nipple or breast, axillary bands or webs in association with
brachydactyly, syndactyly or hypoplasia or aplasia of the carpus or
forearm, or all of these.
weeks of gestation by ultrasound. Early in gestation, fetal cutaneous
wounds heal without scar formation. There is exciting potential for
correcting some abnormalities in utero and
new endoscopic techniques are under development; however, many problems
still prevent nonlethal fetal conditions from being managed in this way.
function, prevent increasing deformity, improve appearance, and do no
further harm.
-
Immunity to infection develops over time
(the infant maintains passive immunity conferred by the mother for the
first 5 weeks of life). Active immunity matures by 5 months. Therefore,
avoid surgery between 5 weeks and 5 months. -
Early surgery prevents the emotional scarring associated with the child’s awareness of the deformity.
-
Hand length nearly doubles during the
first 2 years of life. A digit tethered to another that fails to grow
can produce a major deformity during the early growth spurt. -
Joint surfaces can remodel with growth if treated in the first year.
-
Grasp and pinch are established by 1 year
and accuracy of prehension and refinement of coordination continue
until 3 years. Therefore, abnormal grasp patterns as in cleft hand and
thumb aplasia or hypoplasia should be corrected before this time. -
Do not separate children under 5 years of age from parents.
-
Plans for surgical reconstruction should be designed to be completed by school age.
-
Children more than 2 years old should not have bilateral hands splinted at the same time.
-
Severe constriction band syndrome with distal edema
-
Many deformities can be arrested or even partially corrected by early splinting and therapy.
-
Decision to use a prosthesis in proximal
transverse deficiency. Early use enables the child to incorporate it
into normal function. If implemented later, the child will ignore it.
-
Early correction required because of rapid growth:
-
□ Syndactyly between digits of unequal
length (border digits). (Common long to ring finger syndactyly can wait
until 1 year of age.) -
□ Syndactyly with bone bridges between terminal phalanges
-
□ Acrosyndactyly with partial aplasia of the adjacent digit
-
□ Longitudinal radial deficiency (before fixed soft tissue contractures occur).
-
-
Early correction required because of functional concerns:
-
□ Early splinting for congenital clasped thumb may result in good outcome (if not improved by 6 months, do tendon transfer)
-
□ Cleft hand surgery
-
□ Thumb aplasia-pollicization
-
□ Duplicated thumb correction (particularly proximal)
-
-
Excision of extra digits
-
Surgery should be completed before school age.
-
Conditions such as trigger thumb and minor clinodactyly may never require surgery.
-
If rehabilitation after surgery requires cooperation, the procedure should be delayed until 5 to 6 years of age.
-
Anomalies associated with life-threatening problems may need to be delayed until the patient is stable.
-
Lack of elbow flexion in radial clubhand
-
Unilateral radioulnar synostoses
-
Other synostoses in the wrist and hand rarely need treatment
-
In older children a functional pattern may have already been established.
-
Apert syndrome
-
□ First surgery at 6 months; plan completion of releases by 3 years.
-
□ Surgeries 6 months apart to be sure of digit viability.
-
□ Do not release adjacent webs simultaneously.
-
-
Radial aplasia
-
□ Start with night splints and passive stretching.
-
□ Surgery at 6 months and pollicization 6 weeks later.
-
□ If bilateral, do first side at 6 months, other side at 9 months with pollicization completed by 15 months.
-
□ Splint full time until 6 years of age and then night splints until skeletally mature.
-
-
Brachydactyly
-
□ Minimal requirement is to achieve a mobile thumb to oppose against an ulnar post by age 2 to 3 years.
-
□ Transferred toe phalanges with intact periosteum must be done in first year.
-
-
Windblown hand
-
□ Splint and manipulate while awaiting surgery.
-
□ Treat before 2 years of age (over 5 years results are poor).
-
-
Physical abnormalities may be more difficult for families to cope with than hidden congenital problems.
-
Beware of unrealistic expectations.
-
Genetic counseling should play a major
role in the comprehensive medical management of a child with a hand
malformation and information about support groups is particularly
helpful.
D, Hotchkiss R, Pederson W, eds. Green’s operative hand surgery, 4th
ed. Vol 1. New York: Churchill Livingstone, 1999:325-551.
