the Physis
structure that is responsible for bone growth in all long bones. The
growth plate consists of columns of chondrocytes that are separated by
fibrous septae. The integrity of this architecture is essential for
continued growth. The cells in each column undergo a precise
proliferation and maturation pattern. Calcification does not occur
until the last layer at the border of the metaphysis. Calcification
earlier in the process would result in premature closure of the growth
plate. The process of bone growth and calcification is strictly
regulated. Control is mainly hormonal, but there are mechanical
influences on the physis that can both inhibit or promote growth.
Closure of the physis occurs around age 13 in girls and age 16 in boys.
Infection, injury, or disease can result in growth disturbances, which
can be angular, if only part of the physis closes, or result in
shortening of the entire bone if the majority of the physis is involved.
-
Resting or reserve zone
-
Zone of proliferation
-
Zone of maturation
-
Zone of hypertrophy
-
Zone of provisional calcification
-
The reserve or resting zone remains a
region of mystery in terms of its exact function, although matrix
production is very active in this zone. -
The reserve zone is characterized
histologically by the irregular distribution of cells within the matrix
in contrast to the stacked orderly cell layers in the zones above.-
□ Cell proliferation is sporadic although
most of the cells in the resting layer are actively making proteins as
evidenced by an abundance of intracellular endoplasmic reticulum. -
□ Blood vessels pass through the reserve
zone en route to the proliferative zone without oxygenating the reserve
zone where the oxygen tension is low. -
□ The matrix surrounding the cells contains irregular fibrils of collagen rich in type 2 collagen.
-
□ The reserve zone contains more matrix collagen than any other zone of the physis.
-
□ The proteoglycans in the matrix are in an aggregate form that prohibits the mineralization of the matrix.
-
-
-
The zone of proliferation contains the first columnar cells as well as a single germinal cell layer.
-
□ If this single layer of cells is damaged during trauma, arrest of the entire physis can occur.
-
□ These stem cells undergo clonal expansion when stimulated.
-
-
The cells are regularly arranged but much flatterappearing than the cells in the hypertrophic zone.
-
Cells are undergoing differentiation and maturation.
-
Oxygen tension is high, as are glycogen stores.
-
Aerobic glycolysis supports rapid proteoglycan synthesis.
-
The growth from a particular physis is determined by the number of cell divisions in the proliferative zone.
-
The matrix remains disorganized.
-
The cells in the zone of hypertrophy gain height compared to the cells in the proliferative zone.
-
□ The amount of cell hypertrophy correlates to the growth rate.
-
-
The cells in the zone of hypertrophy align parallel to the diaphyseal shaft of the bone.
-
Cells in the zone of hypertrophy actively synthesize matrix proteins, alkaline phosphatase, and type X collagen.
-
The cells have a low intracellular
conversion of adenosine triphosphate (ATP) to adenosine diphosphate
(ADP) compared with the cells in other zones. -
Oxygen tension is low and anaerobic glycolysis is used for energy production.
-
The growth-plate chondrocytes control
matrix mineralization through intracellular calcium transport using
specialized mitochondria that transport calcium. -
Factors that control matrix mineralization include:
-
□ Hormones [parathyroid hormone (PTH,) calcitonin, insulin-like growth factor 1 (IGF-1)]
-
□ Intracellular calcium stores
-
□ Extracellular matrix
-
□ Local environment
-
which hormones travel from other areas of the body to exert an effect
on the growth plate. Examples of such hormones include growth hormone,
thyroid hormone, or vitamin D. Other signaling occurs locally from
within the growth center (paracrine) or from the cell itself
(autocrine). Examples of locally acting molecules include IGF-1,
fibroblast growth factors (FGFs), bone morphogenic proteins,
transforming growth factor-β (TGF-β), and parathyroid-related protein
(PTHrP).
-
Peptide hormone produced by the pituitary
-
Acts on all zones of the growth plate, but the mechanism by which growth hormone (GH) exerts an effect is not completely known
-
□ GH may cause chondrocytes to produce IGF-1.
-
□ GH also regulates the IGF receptors on the target cells.
-
-
Effects chondrocytes in the zone of proliferation
-
The thyroid secretes thyroxine (T4), which is then deionized in the liver or kidney to form the more potent form, triiodothyronine (T3).
-
Thyroid hormones act to increase DNA synthesis in the cells in the zone of proliferation.
-
These hormones also function to stimulate cell maturation.
-
Thyroid hormone interacts with other hormones such as IGF-1.
-
This protein is produced in the parathyroid glands.
-
Acts at the zone of hypertrophy
-
□ Stimulates chondrocyte proliferation and causes an increase in synthesis of proteoglycans
-
□ Shares a common receptor with PTHrP
-
□ Through the receptors PTH and PTHrP, PTH causes maturation of cells and transformation to the hypertropic phenotype
-
-
Two active forms of vitamin D with different mechanisms of action on growth-plate chondrocytes.
-
□ 25(OH)1D3 is deiodinized in the liver.
-
□ 1,25(OH)2D3 and 24,25(OH)2D3 are deiodinized for a second time in the kidney.
-
-
The absence of vitamin D causes the elongation of cells in the hypertrophic zone and a decrease in mineralization.
-
□ Vitamin D metabolites cause a decrease
in systemic calcium and phosphorus leading to a decrease in
mineralization of growth-plate matrix.
-
-
24,25(OH)2D3 has a direct effect of increasing DNA synthesis, while 1,25(OH)2D3 inhibits proteoglycan production.
-
Previously called somatomedins
-
Stimulate cellular production of RNA and DNA as well sulfated proteoglycans
-
A family of more than 10 heparin-binding polypeptides
-
□ Which specific FGF exerts an effect depends on the age of the host.
-
□ FGF-2 causes development of neonatal chondrocytes, while FGF-1 acts on older growth plates.
-
-
The effects may be potentiated by interaction with IGF1 as well as autocrine or paracrine modulation in response to GH.
-
The FGFs stimulate chondrocytes in mitogenesis, receptor regulation, and protease production.
-
Superfamily includes the bone morphogenic proteins.
-
These growth factors tend to up-regulate production of matrix elements.
-
TGF-β may both suppress and stimulate chondrocytes depending on the local effect of other hormones.
-
The physis responds to loads placed across it.
-
The Heuter-Volkman law explains this
phenomenon and, in general, describes the observation that compressive
forces across the physis decrease growth while growth of the bone is
enhanced by distraction-type forces. -
There are exceptions to the Heuter-Volkman law as excessive distraction seems to impede growth as much as compressive force.
-
Compressive forces:
-
□ Example: stapling of the physis is
thought to stop growth across the physis by compression (applied either
to one side of the physis to correct angular deformities occurring in
Blount disease or placed on both sides of the physis to stop the growth
of the limb (staple epiphysiodesis). -
□ Deformity in the staples can be
measured and demonstrates the large mechanical load the physis can
produce estimated at 1 to 5 MPa.
-
-
Distraction forces:
-
□ Distraction across a limb.
-
□ Clinical observations have shown decrease in predicted growth after lengthening.
-
□ In an animal model of distraction,
osteogenesis lengthening of greater than 30% of the limb resulted in
decreased growth of the limb that seemed to affect the overall amount
of lengthening more than the rate of lengthening.
-
-
□ Direct distraction across the physis.
-
Has become a less popular technique, as
continued growth of the physis is unpredictable after attempts to
lengthen across the physis.
-
-
-
The physis has different mechanical
properties depending on location within the physis and based on the
structure of the growth plate.-
□ The periphery of the growth plate is more compliant and less permeable than the center of the growth plate.
-
□ In animal models of the physis
subjected to strain, the thicker the physis, the weaker the physis at
resisting the forces placed across it.
-
-
The physis withstands stress or tensile forces better than compression or crushing type forces.
-
□ Shear loading causes separation of the physis at the zone of hypertrophy, often leaving the resting zone intact.
-
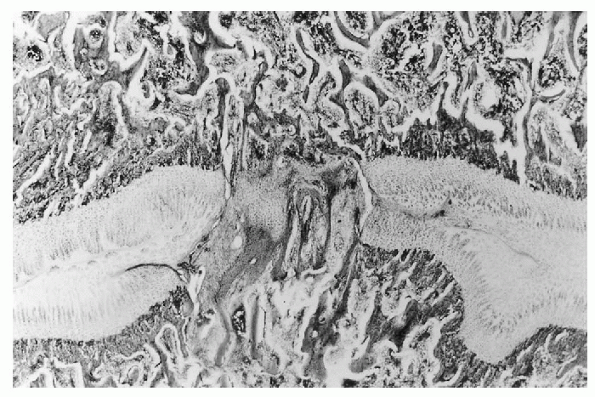
□ The fate of the physis ultimately rests in the fate of the single cell stromal layer in the proliferating zone (Fig. 29-1).
-
-
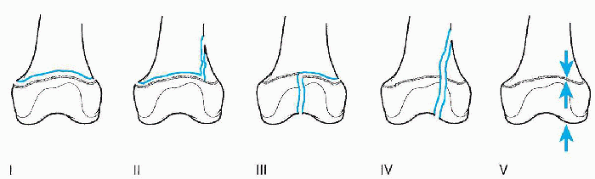
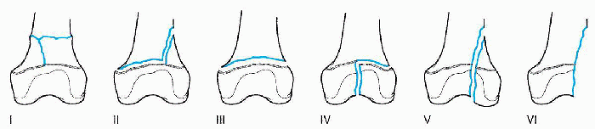
Classification system (Table 29-1 and Figs. 29-2 and 29-3):
-
□ In general, the larger the number, regardless of which schema, the more likely the chance of a physeal closure.
-
□ Prognosis of a physeal closure is also based on:
-
□ Patient age
-
□ Severity of the fracture
-
Skin integrity
-
Amount of comminution
-
Amount of fracture displacement
-
-
□ Location of the physis
-
The physes about the knee (distal femur and proximal tibia) contribute most to longitudinal growth (greater than 1 cm/year).
-
-
-
-
If the entire physis closes, there is
loss of overall length of the bone; if only part of the physis closes,
there can be significant angular deformity.-
□ The physis closes in trauma as new healing bone forms across the growth plate forming a bone bridge or bar.
-
□ Impending physeal closure is not possible to make an initial diagnosis either clinically or radiographically.
-
□ Often, 6 months or more must elapse
before there is an obvious change in the alignment of the bone or there
is evidence of bone bridging on radiographic images. -
□ Extensive bars can be seen on plain
films, other more subtle growth-plate disturbances require computed
tomography, magnetic resonance imaging, or tomograms.
-
-
-
Treatment of a premature physeal closure:
-
□ For bars of less than 50% of the entire
physis, excision of the bar with placement of an interpositional
material (cranioplast or fat). -
□ Bars not suitable for excision may require complete physeal closure to stop angular deformities from developing.
-
□ If the physis has closed, choices for
treatment include closure of the identical physis on the opposite limb,
or treatment of the limb length discrepancy with either a shoe lift or
a lengthening procedure (depending on the amount of predicted limb
length discrepancy at skeletal maturity).
-
|
TABLE 29-1 CLASSIFICATION OF PHYSEAL INJURIESa
|
|||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||
 |
|
Figure 29-1
Experimental physeal bar created in a pig model of hip dysplasia after pelvic osteotomy. (From Leet AI, Mackenzie WG, Szoke G, et al. Injury to the growth plate after Pemberton osteotomy. J Bone Joint Surg [Am] 1999;81:169-176.) |
 |
|
Figure 29-2
Salter and Harris classification of physeal fractures (1963). (Adapted from Peterson HA. Physeal fractures. Part 3: classification. J Pediatr Orthop 1994;14:439-448.) |
 |
|
Figure 29-3
Peterson classification of physeal fractures (1994). (Adapted from Peterson HA. Physeal fractures. Part 3: classification. J Pediatr Orthop 1994;14:439-448.) |
-
Infection in children occurs first in the metaphyseal region of the bone where the capillaries form sinusoidal loops.
-
□ The growth plate tends to block
infection from spreading into the epiphysis, but significant infection
can cause destruction of the physis leading to angular deformity or
growth arrest. -
Since infections can occur very early in life the amount of limb length discrepancy can be substantial.
-
□ Treatment is often with distraction osteogenesis.
-
-
-
Infection tends to spread from the
metaphysis (osteomyelitis) to the periosteum (subperiosteal abscess)
and finally into the joint space (septic joint).-
Bones in which the metaphysis is
intracapsular are at higher risk for a septic arthritis and include the
proximal humerus and femur, the radial head, and the distal fibula.
-
-
Common organisms responsible for infection in childhood are listed in Box 29-1.
-
Staphylococcus aureus
-
Group B Streptococcus
-
Enterobacteriacae
-
Neisseria gonorrhoeae
-
S. aureus
-
Streptococcus pyrogenes
-
Streptococcus pneumoniae
-
Haemophilus influenzae (all but irradicated in children who have been vaccinated)
-
S. aureus
-
Streptococci
-
N. gonorrhoeae
-
S. aureus
-
Sickle cell disease Salmonella
-
Immunosuppressed S. aureus Staphylococcus epidermidis Pseudomonas aeruginosa
-
Achondroplasia is the most common genetic skeletal dysplasia.
-
Rhizomelia, seen in achondroplasia, results from decreased growth involving the proximal long bones.
-
Achondroplasia results from a point mutation of the fibroblast growth factor receptor 3 (FGFr-3).
-
□ FGFs are a family of heparin-binding
polypeptides that are potent mitogens of growth-plate chondrocytes
whose actions are controlled by receptors (FGFr-1 through 4) on the
cell surface. -
□ FGFs interact with receptors on the cell surface to cause transphosphorylation and cellular signal transduction.
-
□ Other genetic mutations of the FGF receptors can result in skeletal dysplasias.
-
□ Periosteal bone formation continues
normally, causing the radiographic feature of widened metaphyses
occurring from the uncoupling of longitudinal and latitudinal growth.
-
-
Presentation
-
□ Shortening of the limbs.
-
□ Bowing deformities.
-
□ Developmental delay.
-
□ Spinal deformity.
-
□ Kyphosis prior to walking.
-
□ Spinal stenosis in adulthood.
-
-
-
Treatment
-
□ Multidisciplinary approach to address specific problems
-
-
Tibia vara, congenital or late onset
-
Risk factors
-
□ Early walking
-
□ Obesity
-
-
Pathology
-
□ Biopsy specimens show loss of columnar arrangement of the cells throughout the physis.
-
□ More pathology is seen on the medial side than on the lateral side.
-
□ Bone bars (see “Trauma” section earlier in the chapter) have also been identified.
-
-
Presentation
-
□ Painless
-
□ Bowing deformity of the involved lower extremity
-
-
Treatment
-
□ Bracing in young children with three-point fixation and a locked knee hinge
-
□ Surgical correction in older children or after failure of bracing
-
□ For recurrence of deformity,
identification and resection of a physeal bar using interpositional
material or revision osteotomy to restore mechanical alignment
-
-
Defined as a decrease in the neck shaft angle (can be congenital or acquired)
-
Biopsy specimens taken from the growth plate show:
-
□ Derangement of the cells in the resting zone
-
□ Loss of columnar organization in the proliferative and hypertrophic zones
-
□ Absence or poor formation of the zone of provisional calcification
-
□ Pathology similar to that seen in Blount disease.
-
-
Presentation
-
□ Acquired, idiopathic form develops around age 6
-
□ Usually painless with a limp noted by the family
-
□ If unilateral, a limb length discrepancy may occur
-
□ Waddling gait (weakness of hip abductor muscles)
-
□ Limited range of motion in abduction and internal rotation of the hip
-
-
Treatment
-
□ Corrective osteotomy to restore normal hip joint mechanics
-
-
The perichondral ring protects the physis
against shear forces, with subsequent physeal separation through the
hypertrophic zone. -
In slipped capital femoral epiphysis
(SCFE), the physis is composed of multiple layers of both dense
fibrotic tissue and loosely packed cells. -
In SCFE, there is loss of integrity to the perichondral ring.
-
□ If the disruption is slow and consists
of plastic deformation the patient presents with limp and hip pain of
long-standing duration; if the ring fails acutely the presentation can
be similar to a fracture with loss of ability to bear weight.
-
-
Risk factors
-
□ Increased body weight which applies more load to the physis
-
□ Change in orientation of the physis in
adolescents from a more horizontal to vertical direction, leading to
more shear stress across the growth center -
□ Endocrine disorders, such as hyperparathyroidism and renal failure
-
-
Presentation
-
□ Pain in the lateral thigh, groin, or knee area
-
□ Inability to bear weight (by definition an unstable slip)
-
□ Limp
-
□ Obligate external rotation of the hip
-
-
Treatment
-
□ In situ pinning of the head
-
□ Corrective osteotomy for residual deformity
-
-
Causes can be nutritional (rickets), or
resulting from matrix defects in chondrocytes (mucopolysaccharidosis)
or osteoblast dysfunction (osteogenesis imperfecta).
-
Vitamin D derangement occurring from nutritional deficiencies or from cellular resistance to vitamin D
-
Lack of vitamin D results in impaired calcification at the zone of provisional calcification.
-
Clinical features
-
□ Bowing of limbs
-
□ Lower than predicted height for age
-
□ Radiographs show pathognomonic cupping of the growth plates with growth plate widening.
-
-
Treatment consists of maximizing medical
management which often corrects limb deformity. Surgical correction is
the choice of last resort.
-
Genetic defects in enzymes that mediate proteoglycan metabolisms resulting in accumulation of fat in the cells
-
Clinical presentation varies depending on
particular condition but can include mental retardation, stunted
growth, facial dysmorphism, and orthopaedic problems such as hip
dysplasia, coxa vara, Madelung deformity -
Treatment
-
□ Bone marrow transplantation
-
-
Caused by a mutation of either the COL1A1 or COL1A2 gene, both of which have a direct effect on the triple helical pattern of collagen.
-
Presents with frequent fractures, blue sclera, and poor dentition.
-
Treatment
-
□ Recently, medical treatment with bisphosphonates has shown some promise in decreasing the rate of fracture.
-
□ Rodding procedures are also often required.
-
JA, Einhorn TA, Simon SR, eds. Orthopedic basic science, 2nd ed.
Rosemont, IL: American Academy of Orthopedic Surgeons, 2000.
JA, Erlich MG, Sandell LJ, et al, eds. Skeletal growth and development:
clinical issues and basic science advances. Rosemont, IL: American
Academy of Orthopedic Surgeons, 1998.
DI, Wall EJ, Rupert MP, et al. Growth plate forces in the adolescent
human knee: a radiographic and mechanical study of epiphyseal staples.
J Pediatr Orthop 2001;21:817-823.
B, Chorney GS, Phillips DP, et al. The microstructural tensile
properties and biochemical composition of the bovine distal femoral
growth plate. J Orthop Res 1992;10:263-275.
B, Chorney GS, Phillips DP, et al. Compressive stress-relaxation
behavior of bovine growth plate may be described by the non-linear
biphasic theory. J Orthop Res 1994;12:804-813.
WE III, Zaleske DJ, Schiller AL, et al. Vascular events associated with
the appearance of the secondary center of ossification in the murine
distal femoral epiphysis. J Bone Joint Surg 1987;185-189.
HA. Physeal injuries and growth arrest. In: Beaty JH, Kasser JR, eds.
Rockwood and Wilkins’ fractures in children, 5th ed. Philadelphia:
Lippincott Williams & Wilkins, 2001:92-138.
JL, Do PD, Eick JD, et al. Tensile properties of the physis vary with
anatomic location, thickness, strain rate and ag e. J Orthop Res
2001;19:1043-1048.
