describe movement—the translation of the body through space from one
point to another. It refers to both walking and running. There are
various methods used to describe gait ranging from the very
sophisticated three-dimensional computerized gait analyses systems to
the simple visual assessment done in either the clinical setting such
as the office or orthopaedic outpatient department or the nonclinical
setting such as normal observation of someone walking in the community.
Pathologic processes can have an effect on a patient’s gait. Some
conditions in which there can be a profound effect on a patient’s gait,
such as cerebral palsy, are best studied using the resources of a
sophisticated gait lab. However, one should be able to describe a
patient’s gait even without the availability of a gait lab through
direct observation.
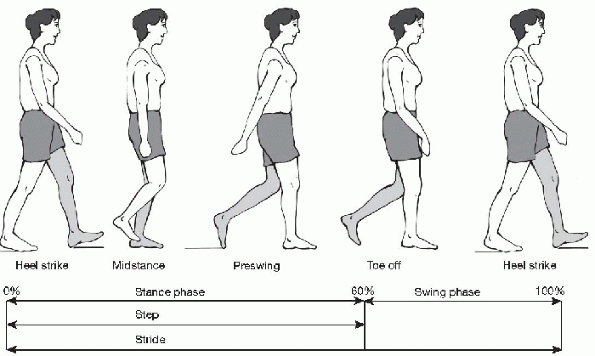
considering each leg individually: stance phase (when at least one leg
is in contact with the ground) and swing phase (when the leg is in the
air; Table 35-1). As well as providing forward
momentum to the leg, the swing phase also prepares and aligns the foot
for heel strike and ensures that the swinging leg clears the floor.
Usually, at normal walking velocity, the stance phase occupies
approximately 60% of the gait cycle and the swing phase 40% (Fig. 35-1).
The faster one walks the shorter the stance phase becomes and the
longer the swing phase becomes until the person is running, at which
point the stance phase can be as short as 20% and the swing phase as
long as 80%. Running is also typified by absence of a double-support
phase. In other words, at no time during running are both feet on the
ground simultaneously.
|
TABLE 35-1 TERMINOLOGY IN GAIT ANALYSIS
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
These determinants produce a dampening down of the excessive vertical
and side-to-side movement in gait by interacting to create a smooth
pathway for the forward displacement of the center of gravity.
heel-toe pattern until at least age 3.5 years, although there is
extreme variability in the walking patterns of many children.
 |
|
Figure 35-1 The gait cycle.
|
-
Stability in stance
-
Sufficient foot clearance during swing
-
Appropriate swing phase pre-positioning of the foot
-
Adequate step length
-
Energy conservation
-
Pelvic rotation
-
Pelvic tilt
-
Knee flexion after heel-strike in stance phase
-
Foot and ankle motion
-
Knee motion
-
Lateral displacement of the pelvis
major determinants in normal and pathological gait. J Bone Joint Surg
(Am) 1953;35:558.
-
With the child in shorts or other
suitable attire observe him or her both from the frontal plane or front
view and the sagittal plane or side view. -
Be aware that gait is occurring on a
three-dimensional basis, so be sure to assess rotation or line of
progression, which is in the coronal plane or transverse view. -
Watch the position of the child’s limbs (upper and lower) and the trunk in double limb stance, before the child begins to walk.
-
Ask the child to walk (usually at a “self-selected” pace) toward you and away from you.
-
Have the child run. Running can sometimes unmask certain pathologic conditions and exaggerate asymmetry.
-
Focus initially on the whole patient and the patient’s general movement.
-
Look for symmetry and asymmetry.
Appreciate trunk sway, arm swing, head and neck position first; then
concentrate on a single aspect of the walk, usually localized to one
segment of the child’s anatomy (Box 35-3).
gait. These scales have the observer assign a numeric value to the
patients’ walking characteristics. Generally, these reference scales
have not been validated but do serve a useful purpose to train the
observer to approach observational gait analysis in an orderly fashion.
The Physician’s Rating
Scale has been frequently referred to in articles dealing with gait assessment (Table 35-2).
-
Overall impression
-
□ Temporal/spatial characteristics
-
-
Trunk alignment
-
Leg positions
-
□ Stance phase
-
□ Swing phase
-
-
Foot position
-
□ Stance
-
□ Heel-toe
-
|
TABLE 35-2 PHYSICIAN’S RATING SCALE
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
-
Appreciate overall symmetry of the patient’s gait.
-
Assess the stride and step lengths.
-
Do the arms swing symmetrically?
-
Is walking speed abnormally fast or slow?
-
Exaggerated side-to-side trunk sway may
represent a compensated Trendelenburg sign. There is normally some
degree of trunk sway but it should be noted if excessive. -
The pelvis normally rises a few degrees
during single limb stance phase. Exaggerated ipsilateral pelvis
elevation during single limb stance is known as a positive
Trendelenburg sign and should be noted. -
Consistent asymmetry in pelvic heights
(anterior superior iliac spine [ASIS] or posterior superior iliac spine
[PSIS]) may indicate a leg length difference. -
Look for any scoliosis and any flank or waist crease asymmetry.
-
Watch for compensatory changes such as
circumduction when the hip is “thrown” out into external rotation
during swing phase. Some of these maneuvers are compensatory for a leg
length discrepancy or weakness. -
Appreciate any abduction contractures of
the leg (e.g., as seen in poliomyelitis), and look for adduction in
swing and in stance phase (“scissoring”) seen in patients with cerebral
palsy. Sometimes the thighs are so adducted in stance that it appears
the patient requires this for stability.
-
Watch on the frontal plane for excessive knee varus or valgus in stance.
-
Lateral or varus thrusting on mid- or
terminal stance at the knee may indicate medial or lateral instability
from trauma or, in the case of younger children, may be a reflection of
the health of the growth plate (e.g., Blount’s disease, rickets).
-
Static and dynamic knee and foot alignment can include varus and valgus of both the knee and foot.
-
Observe the position of the heel or foot at weight acceptance:
-
□ Is there excessive calcaneovalgus or calcaneovarus?
-
□ Is the foot flat or high arched?
-
□ Weight acceptance normally occurs with
the lateral border of the heel. The center of force normally then
passes distally toward the fifth metatarsal and then proceeds across
the metatarsals and exits near the great toe. This represents a
pronation then supination attitude to the foot during stance. -
□ The supinated foot prior to toe-off also may be slightly adducted for rigidity and strength (lever arm).
-
-
Appreciate the sagittal alignment of the whole thoracic and lumbar spine.
-
Comment on any increased or decreased spinal kyphosis or lordosis.
-
Watch for cervical spine and head position.
-
Is there an increased anterior pelvic tilt?
-
□ This can be partially age-related (common at ages 3 to 7 years).
-
□ Increased anterior pelvic tilt and lumbar lordosis can be seen following excessive hamstring lengthening in cerebral palsy.
-
□ Hip extensor weakness (spina bifida, muscular dystrophy) can also be associated with anterior tilt.
-
-
Posterior pelvic tilt can be seen with hamstring tightness or spasticity.
-
The hip normally flexes to its maximum
range at the end of the swing phase just before the foot strikes the
floor. This also assists in achieving toe clearance. -
The hip then goes into extension and
remains there throughout the rest of stance and reaches its maximum
degree of extension just before toe-off. This produces the proximal
portion of a rigid fulcrum or lever for maximum propulsion of the lower
leg.
-
The main function of the knee in swing is
to raise the foot off the ground to assist in appropriate toe
clearance. Only a few millimeters of toe clearance is required for
efficient walking. -
The knee therefore has its maximum degree of flexion in mid-swing.
-
Initial weight acceptance sees the knee
in almost full extension. This is followed by a few degrees of knee
flexion before fully extending in terminal stance in preparation of
toe-off and propulsion. This adds further strength to the lever arm for
lower leg propulsion in conjunction with the hip also in full extension. -
The purpose of knee flexion in initial stance is for a shock-absorbing effect.
-
Stiff-legged position at stance and swing
would be very tiring and probably lead to increased stresses seen at
other joints up the kinetic chain. -
Check for any knee hyperextension or
recurvatum that can sometimes occur in mid- to late stance in such
conditions as spasticity or equinus contractures. -
Look for persistent knee flexion throughout stance as can be seen in crouch gait.
-
The weight acceptance pattern during normal walking is that of heel to toe during stance.
-
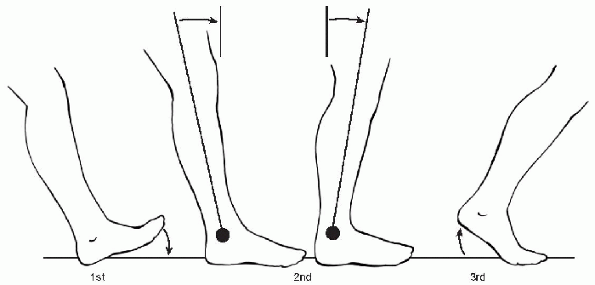
The ankle position has been described as having three rockers on the sagittal plane (Fig. 35-2):
-
□ The first rocker immediately follows heel strike when the ankle plantarflexes for full flat foot weight acceptance.
-
□ In mid-stance, the tibia then moves
over the talus at the ankle to form the second rocker. This means the
foot goes into relative dorsiflexion. -
□ The third rocker then follows as the foot plantarflexes for power generation to propel the patient forward at push-off.
-
-
The foot and ankle are held in
dorsiflexion during swing to achieve toe clearance and also to prepare
for weight acceptance at heel strike.
 |
|
Figure 35-2 The three ankle rockers. (Adapted from Gage JR. Gait analysis in cerebral palsy. Clin Dev Med 1991;121:82.)
|
-
There is normally some trunk rotation
seen with gait. The ipsilateral leg, when advancing, is associated with
internal trunk and pelvis rotation. -
When this normal rotation does not occur, terms such as pelvic retraction are used. This can commonly be seen in children with hemiplegia.
-
Circumduction and adduction (coronal
plane) can sometimes be confused with rotational changes seen in the
hip during swing phase of the gait cycle. -
Transverse plane describes internal and external rotation of the limb during swing and subsequently at weight acceptance.
-
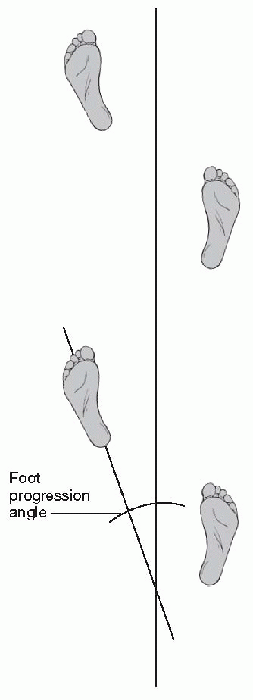
Exaggerated femoral anteversion will
produce an internally rotated line of progression, whereas femoral
retroversion will produce an out-toed gait. -
Sometimes these conditions are exaggerated with running or with fatigue.
-
The transverse plane rotational changes
that occur during gait at the knee are so small that they are difficult
to appreciate visually. -
There is normally a “screw-home” phenomenon that occurs in terminal stance, serving to lock the knee and provide stability.
-
The only way this rotation can be
appreciated is when it is increased as in knee instability syndromes.
The static rotational changes seen here are a reflection of the
developmental internal and external tibial torsion, which also can
produce an internally or externally rotated line of progression.
 |
|
Figure 35-3 The line of progression in gait. In-toeing is expressed as negative degrees and out-toeing as positive.
|
-
On the transverse plane, observe the line
of progression the foot makes in relation to the trunk and pelvic
alignment and comment on in-toeing or out-toeing gait pattern (Fig. 35-3). -
Abnormal foot positions such as metatarsus adductus can be appreciated.
-
The foot normally rotates into internal position just prior to toe-off.
accepted method to critically analyze gait in children and adults with
movement disorders. It is especially valuable to assist clinical
examination of those patients with complex movement patterns from such
conditions as cerebral palsy and spina bifida. Detailed understanding
of the intricacies of a gait laboratory is beyond the scope of this
chapter; however, the orthopaedic resident or surgeon should be able to
understand some of the basic methods of gait analyses and appreciate
the results and subsequent treatment recommendations.
the test combine visual analysis with video cameras capable of slow
motion for review. Kinematics, kinetics, electromyography, plantar
pressure profiles, and oxygen cost are also usually performed. The data
are collected using three-dimensional analysis: the x, y, and z
axes describing the coronal, sagittal, and transverse planes,
respectively. The information is gathered after appropriate
digitization and usually presented in graphic form. The graphs usually
show one stride length, standard deviations, and norms for age or
weight.
to describe the relationship of the body and its joints in space. It is
a description of motion independent of forces.
-
Temporal spatial characteristics: these include velocity, cadence, stride, and step lengths. Support times and step widths are also often included.
-
Trunk and pelvic orientations:
for both the right and left strides the rotation, anterior or posterior
lean, and elevation or depression are measured and compared with a set
of normal for age and weight. -
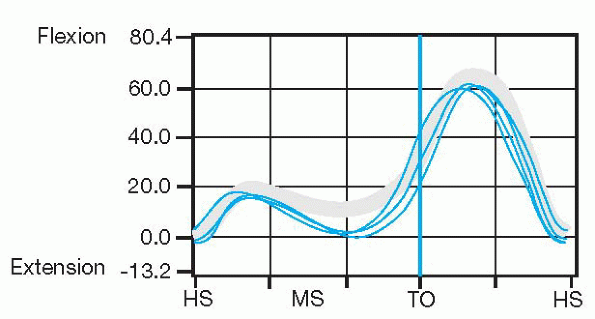
Hip, knee, and ankle joint angles:
on the sagittal plane, the degree of flexion and extension is measured
through the whole gait cycle (stance and swing phase). The hip has its
maximum flexed position at terminal swing whereas the knee has its
maximal degree of flexion at mid-swing in order to allow for ground
clearance of the swinging limb. Both hip and knee have their maximum
extended position in late and terminal stance (Fig. 35-4).
The ankle is described as three ankle rockers going from plantarflexion
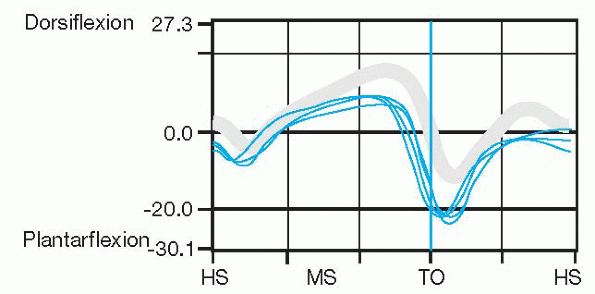
to dorsiflexion and then plantarflexion prior to toe-off (Fig. 35-5).
 |
|
Figure 35-4 Knee joint kinematics. This represents one complete gait cycle from heel-strike to heel-strike. HS, heel-strike; MS, mid-stance; TO, toe-off. (Adapted from Shriners Gait Lab, Sunny Hill Health Centre for Children, Vancouver, BC, Canada.)
|
 |
|
Figure 35-5 Ankle joint kinematics. This represents three separate trials walking in the sagittal plane. HS, heel-strike; MS, mid-stance; TO, toe-off. (Adapted from Shriners Gait Lab, Sunny Hill Health Centre for Children, Vancouver, BC, Canada.)
|
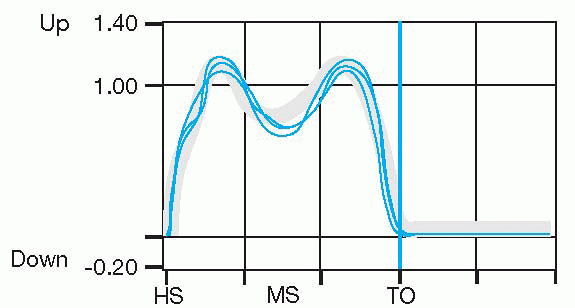
describes forces that produce movement. They are measured using a
specialized force plate concealed in the floor over which the patient
walks during the assessment. Data collected include ground reaction
forces, joint moments, sagittal joint powers, and forces (Fig. 35-6).
Plantar pressure profiles can show the dynamic weight acceptance
pattern of the foot and the development of medial and longitudinal foot
arches.
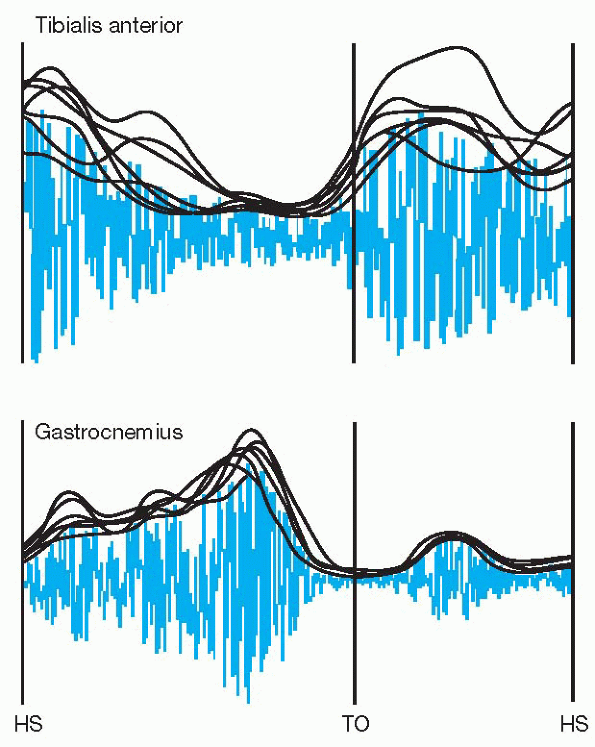
the muscle contraction can be measured using ambulatory or dynamic
electromyography. This allows the visualization of the muscle
contraction during various phases of the gait cycle. Appropriate or
inappropriate firing can be appreciated and recommendations made on
treatment of these abnormal muscle functions through either muscle or
tendon releases or transfers (Fig. 35-7).
 |
|
Figure 35-6
Kinetics showing ground reaction forces. This represents stance phase only, as there are no forces when the foot is off the force plate. HS, heel-strike; MS, mid-stance; TO, toe-off. (Adapted from Shriners Gait Lab, Sunny Hill Health Centre for Children, Vancouver, BC, Canada.) |
 |
|
Figure 35-7Electromyography
of tibialis anterior and gastrocnemius muscles. The gastrocnemius muscle fires in the pre-swing phase for toe-off (TO) and the tibialis anterior fires in swing to achieve ground clearance and fires again at heel-strike (HS) for eccentric deceleration of the foot. (Adapted from Shriners Gait Lab, Sunny Hill Health Centre for Children, Vancouver, BC, Canada.) |
JR. Gait analysis in cerebral palsy. Clin Dev Med 1991;121. Inman VT,
Ralston HJ, Todd F. Human walking. Baltimore: Williams & Wilkins,
1981.
LA, Mooney JF, Smith BP, et al. Management of spasticity in cerebral
palsy with botulinum-A toxin: report of a preliminary, randomized,
double-blind trial. J Pediatr Orthop 1994;14:299-303.
M. The diplegic child. Shriners Hospital for Crippled Children
Symposium. Rosemont, IL: American Academy of Orthopedic Surgeons, 1992.
