Radial Nerve
nerve palsy originating in the arm will be encountered on an upper
extremity service and it is appropriate to discuss it in the context of
this book.
with fractures of the humerus in the middle third or at the junction of
the middle and distal thirds. Radial nerve palsy at this location is
distinguished from the more proximal “Saturday night palsy” and “crutch
palsy” seen in the upper arm and axilla, respectively. These more
proximal lesions usually recover spontaneously in 60 to 90 days and are
not the topic of discussion here.
-
The proximity of the radial nerve to bone in the spiral groove.
-
The relative fixation of the radial nerve
in the spiral groove and at the site of penetration of the nerve
through the lateral intermuscular septum on its way from the posterior
to the anterior aspect of the arm.
postulate the etiology of the neurapraxia based on traction, contusion,
or hematoma.
issue of early versus late exploration of radial nerve palsy associated
with humeral fracture, most palsies recover spontaneously, and early
surgical exploration is recommended in only three circumstances: (1)
open fractures, (2) fractures that require open reduction and or
fixation, and (3) fractures with associated vascular injuries. The
onset of radial nerve palsy after fracture manipulation is not an
indication for early nerve exploration
fracture of the distal humerus in seven patients, five with radial
nerve paralysis and two with paresis. They noted radial angulation and
overriding at the fracture site. As the radial nerve courses anteriorly
through the lateral intermuscular septum, it is less mobile and subject
to being injured by the movement of the distal fracture fragment.
Because of the high incidence of radial nerve dysfunction, early
operative intervention was advised.
trauma-related palsy. A fibrous arch and accessory part of the lateral
head of the triceps has been associated with nerve compression
secondary to swelling of the muscle after muscular effort. Some cases
of radial nerve entrapment in this region of the lateral head of the
triceps have been reported as spontaneous in onset and some following
strenuous muscular activity. What appears to be a familial radial nerve
entrapment syndrome has been reported in a 15-year-old girl with a
total and spontaneous radial nerve palsy. Her sister had recently
sustained an identical lesion that improved spontaneously, and her
father also suffered from intermittent radial nerve palsy. These cases
appear to represent a genetically determined defect in Schwann cell
myelin metabolism.
-
Although a patient with entrapment
neuropathy with an acute onset after overactivity sometimes recovers
spontaneously, entrapment in the advanced stage should be surgically
decompressed because prolonged compression might result in intraneural
fibrotic changes secondary to long-term compression. -
The surgical approach of choice is posterior between the long and lateral heads of the triceps.
superficial radial nerve at the wrist that he called cheiralgia
paresthetica. The condition is characterized by pain, burning, or
numbness on the dorsal and radial aspect of the distal forearm and
wrist that radiates into the thumb, index, and middle fingers. The
symptoms are often associated with a history of a variety of traumatic
and iatrogenic causes, including a direct blow to the nerve, a tight
wristwatch band or bracelet, handcuffs, or an injury due to laceration
or compression from retraction during surgery. Although Wartenberg
classified it as “neuritis,” it is a form of nerve entrapment
positioned beneath the BR muscle as it travels towards the wrist, where
it exits from beneath the BR tendon and between the ECRL tendon to
pierce the antebrachial fascia. In 10% of specimens, the nerve may
pierce the tendon of the BR. It becomes subcutaneous at a mean of 9 cm
(with a range of 7 to 10.8 cm) proximal to the radial styloid. In
supination the SBRN lies beneath the fascia, but without compression.
In pronation, the ECRL crosses over the BR and may create a scissoring
or pinching effect on the SBRN.
-
A useful provocative test is to ask the
patient to fully pronate the forearm. A positive test is manifested by
paresthesia or dysesthesia on the dorsoradial aspect of the hand. -
In addition to this provocative test, a
positive Tinel’s sign may be noted over the nerve distal to the BR
muscle belly as well as altered moving touch and vibratory sense.
-
Treatment is based on the particular
cause, and is usually conservative in the form of splinting, altered
physical activities, and physical therapy including stretching and
tissue gliding exercises. -
In patients who require surgery, release
of the deep fascia and the fascia joining the BR and ECRL, as well as
neurolysis of the SBRN, may be utilized in selected cases.
through the spiral groove to enter the anterolateral aspect of the
distal third of the arm on its way to the forearm, where it lies
between the brachioradialis laterally and the brachialis medially. The
ECRL covers it anterolaterally, and the capitellum of the humerus is
posterior. The radial tunnel begins at the level of the radiohumeral
joint and extends through the arcade of Frohse to end at the distal end
of the supinator. Division of the radial nerve into motor (posterior
interosseous) and sensory (superficial radial) components may occur at
any level within a 5.5-cm segment, from 2.5 cm above to 3 cm below
Hueter’s or the interepicondylar line (a line drawn through the tips of
the epicondyles of the humerus). The superficial radial nerve remains
on the underside of the brachioradialis until it reaches the
mid-portion of the forearm and is not subject to compression in the
radial tunnel
(the distal border). The fibrous bands are anterior to the radial head
at the beginning of the radial tunnel, and are the least likely cause
of compression. The radial recurrent vessels cross the PIN to supply
the adjacent brachioradialis and ECR muscles, and it is postulated that
engorgement of these vessels with exercise may compress the nerve. The
tendinous proximal margin of the ECRB also may compress the PIN, and
may be mistakenly identified as the arcade of Frohse, which lies deep
to the proximal margin of the ECRB muscle. The arcade of Frohse is the
fibrous proximal border of the superficial portion of the supinator. It
is the most common site of compression of the PIN, and is located from
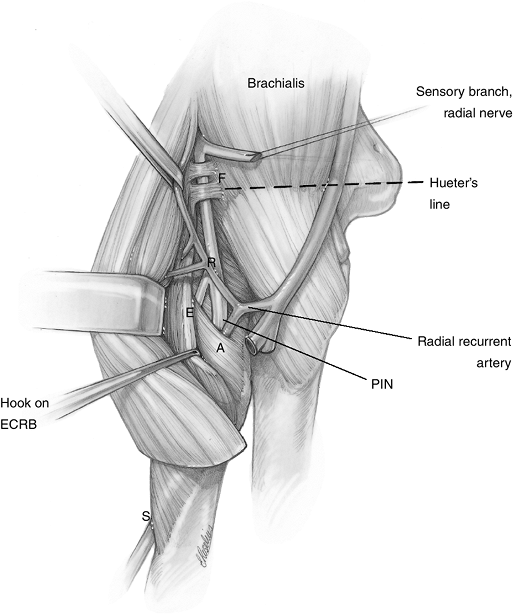
3 to 5 cm below Hueter’s line (Figure 7.3-2).
Sometimes the tendinous margin of the ECRB and the arcade of Frohse may
overlap and form a scissors-like pincer effect on the radial
nerve
in this area. It is appropriate to continue the exploration to the
distal border of the supinator, although it is a rare site of
compression. More often, a mass, such as a ganglion, may be found
beneath the superficial portion of the supinator.
 |
|
Figure 7.3-1
Potential sites of compression of the radial nerve in radial tunnel syndrome (RTS). F, fibrous tissue bands; R, radial recurrent vessels; E, fibrous edge of ECRB; A, arcade of Frohse; S, supinator (see text). |
 |
|
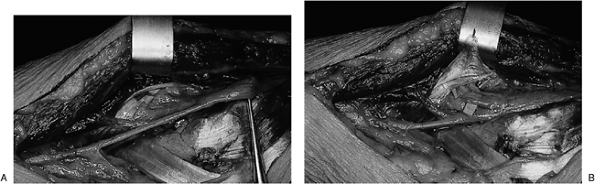
Figure 7.3-2 Fresh cadaver dissection of the ECRB and supinator. (A) The fibrous tissue edges of the ECRB and the supinator are in close proximity to the PIN as it enters the supinator. (B)
The ECRB has been reflected superiorly. Fat has been removed from around the supinator to reveal its two heads and to reveal the fibrous tissue edge of the superficial head that forms the arcade of Frohse. |
-
The radial tunnel syndrome (RTS) must be distinguished from PIN syndrome (PINS).
-
RTS is a subjective symptom complex
without motor deficit, which involves a motor nerve. This is in
contrast to PINS, which is an objective complex with motor deficit
affecting a motor nerve. -
The symptoms in RTS are similar to
lateral epicondylitis, with complaints of pain over the lateral aspect
of the elbow that sometimes radiates to the wrist. Because compression
of a motor nerve is believed to cause the pain, the description of the
pain as a deep ache is not surprising. -
A dynamic state may exist in which
pronation, elbow extension, and wrist flexion are combined with
contraction of the wrist and finger extensors to produce compression of
the PIN.
-
-
Physical findings may include point tenderness 5 cm distal to the lateral epicondyle.
-
The absence of sensory or motor disturbances in RTS is characteristic.
-
To a limited extent, provocative tests
may give some indication of the anatomic location of the compression,
but are not always reliable. -
The so-called middle finger test involves
extension of the middle finger with the elbow in extension and the
wrist in neutral. The test is considered to be positive if pain is
produced in the region of the proximal portion of the ECRB. Sanders has
modified this test as follows:-
With the elbow in full extension, the
forearm in full pronation, and the wrist held in flexion by the
examiner, the patient is asked to actively extend the long and ring
fingers against resistance. -
According to Sanders, these positional
modifications produce maximum compression on the PIN, and represent a
more reliable form of the test. -
If symptoms are reproduced with the elbow
in full flexion, the forearm in supination, and the wrist in neutral,
then fibrous bands are suspected. -
Reproduction of symptoms by passive
pronation of the forearm—with the elbow in 45 to 90 degrees of flexion
and the wrist in full flexion—indicates entrapment by the ECRB. -
Compression at the arcade of Frohse is
suspected if the symptoms are reproduced by isometric supination of the
forearm in the fully pronated position.
-
-
The most reliable test is the injection
of 2 to 3 mL of 1% lidocaine without epinephrine into the radial
tunnel. Relief of pain and a PIN palsy confirms the diagnosis. -
A prior injection into the lateral epicondylar region that did not relieve pain also supports the diagnosis.
-
Electrodiagnostic studies to date have
not been useful in the diagnosis because there are no motor deficits,
and studies of conduction velocity through the radial tunnel are
unreliable.
-
Treatment may be nonoperative, in the
form of rest to the extremity and avoidance of the activities that
aggravate the condition. -
The judicious injection of steroids about the site or sites of possible compression may result in some relief.
-
Surgical intervention is in the form of release of all possible points of compression of the nerve.
motor signs of entrapment of the PIN manifested by weakness or complete
palsy of the finger and thumb extensors. There usually is no history of
antecedent trauma.
-
In complete PINS, active extension of the
wrist occurs with radial deviation owing to loss of the ECRB, whereas
the more proximally innervated ECRL remains intact. -
There is associated loss of finger and thumb extension.
-
Partial loss of function is more common, with lack of extension of one or more fingers or isolated loss of thumb extension.
-
Sensation always is intact.
-
In contrast to RTS, EMG is positive in the muscles innervated by the PIN.
-
Computed tomography scans or magnetic resonance imaging may show a mass in the radial tunnel.
-
The nerve should be explored from the arm
to the distal aspect of the supinator, based upon the clinical findings
and the findings at surgery.
digital nerve of the thumb. It results from external pressure from the
margin of the thumb hole in a bowling ball. It usually involves the
ulnar nerve, and is characterized by pain, paresthesias, and a tender
mass on the ulnar aspect of the proximal phalanx of the thumb. A
variation known as cherry pitter’s thumb has been described by Viegas.
-
Both conditions may be treated by
activity modification, and, in the case of bowler’s thumb, by enlarging
the thumb hole in the bowling ball.
R, Meunier M. Chapter 21. Carpal tunnel syndrome. In: Trumble, TE, ed.
Hand surgery update 3, hand, elbow & shoulder. Rosemont, IL:
American Society for Surgery of the Hand, 2003:299–312.
AL, Chiu DTW. Chapter 22. Cubital and radial tunnel syndromes. In:
Trumble, TE, ed. Hand surgery update 3, hand, elbow & shoulder.
Rosemont, IL: American Society for Surgery of the Hand, 2003:313–323.
AL. Diagnosis and treatment of ulnar nerve compression of the elbow.
Techniques in Hand and Upper Extremity Surgery 2000;4:127–136.
JH, O’Brien ET, Linscheid RL, et al. Bowler’s thumb: diagnosis and
treatment. A review of seventeen cases. J Bone Joint Surg 1972;54:751.
JR, Botte MJ. Elbow. In: Surgical anatomy of the hand and upper
extremity. Philadelphia: Lippincott Williams & Williams,
2002:365–406.
JR, Botte MJ. Forearm. In: Surgical anatomy of the hand and upper
extremity. Philadelphia: Lippincott Williams & Williams,
2002:407–485.
JR, Botte MJ. Palmar hand. In: Surgical anatomy of the hand and upper
extremity. Philadelphia: Lippincott Williams & Williams,
2002:532–641.
W, Dellon AL, Mackinnon SE. Cheiralgia paresthetica (entrapment of the
radial sensory nerve). J Hand Surg 1986;11:196–199.
