Continuous Interpleural Block
Lateral decubitus with the arm dangling anteriorly and cephalad so as
to rotate the scapula forward and expose the posterolateral chest wall.
Postoperative analgesia following mastectomy, nephrectomy, and
cholecystectomy. Analgesia for rib fractures, pancreatitis, neuralgia,
and invasive tumor of the chest wall, flank, and retroperitoneum.
The site of needle insertion is at the seventh or eighth intercostal
space at the level of the tip of the scapula and the cephalad border of
the rib in a vertical direction perpendicular to the chest wall. Once
inserted to a depth of 1 cm into the intercostal muscles, a syringe
(with its plunger removed) is attached to the needle. The open syringe
barrel is filled with saline. The needle is then slowly advanced while
observing for both a “clicking” sensation and a downward movement (the
“falling column”) of the saline as it is drawn into the chest by the
negative pleural pressure. The syringe is removed (Fig. 30-1B)
and the epidural catheter threaded 6 to 10 cm into the interpleural
space. The Tuohy needle is removed, and the catheter is secured with 12
mm × 100 mm Steri-Strip (3M, St. Paul, MN) and covered with a
transparent dressing (Fig. 30-1C).
-
An alternative site is 8 to 10 cm lateral from the posterior midline.
-
Interpleural blockade routinely causes
pneumothorax due to the entrance of air through the needle. This is
typically of small degree (<10%) and asymptomatic. The risk of lung
injury is reduced by the use of proper technique and by avoiding
percutaneous
P.257
placement
in patients with pulmonary bullae or those likely to have pleural
adhesions. Proper technique includes (a) the use of a visual end point
such as the “falling column” technique as opposed to a
“loss-of-resistance” technique, and (b) placement during spontaneous
ventilation as opposed to controlled ventilation or apnea.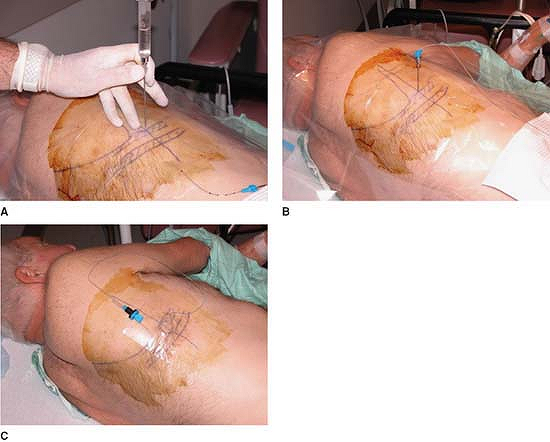 Figure 30-1. A: Anatomic landmarks. B: The syringe is removed and the epidural catheter threaded 6 to 10 cm into the interpleural space. C: The Tuohy needle is removed, and the catheter is secured and covered with a transparent dressing.
Figure 30-1. A: Anatomic landmarks. B: The syringe is removed and the epidural catheter threaded 6 to 10 cm into the interpleural space. C: The Tuohy needle is removed, and the catheter is secured and covered with a transparent dressing. -
As a result of drug sequestration, uneven
distribution, and drug loss through chest tubes, interpleural block has
not proven particularly useful after thoracotomy. However, satisfactory
blockade can, at times, be achieved in the presence of a chest tube
(e.g., rib fractures) by clamping the chest tube for 30 minutes
following intermittent bolus of local anesthetic. -
Placement at too low an intercostal space can lead to intraperitoneal placement of the needle and catheter.
-
The catheter should thread freely without
resistance, which may indicate improper placement, lung penetration, or
the presence of pleural adhesions. -
Epinephrine should be added to any bolus to reduce peak systemic levels of local anesthetic.
-
Patient positioning will determine where
the local anesthetic pools are, where it traverses the parietal pleura,
and which nerves are affected. Lateral position (blocked side up) will
promote blockade of the sympathetic chain while a supine or lateral
position (blocked side down) will promote blockade of the intercostal
nerves. A
P.258
Trendelenburg
position will promote upper thoracic and cervical sympathetic blockade
(producing Horner syndrome) and even, at times, blockade of inferior
roots of the ipsilateral brachial plexus. -
Interpleural block is most useful when
combined with multimodal analgesic therapies which may include
nonsteroidal antiinflammatory drugs (NSAIDs) or a COX-2 inhibitor
(celecoxib), NMDA blockade, alpha-2 agonists, A-2 delta calcium channel
blockade (pregabalin), and opiates. -
To minimize risk of systemic toxicity
from the rapid reabsorption of local anesthetic solution in the
interpleural space, lidocaine may be the preferred local anesthetic for
infusion. While this author has typically used a 1% solution, a lower
concentration may prove adequate. -
Interpleural block will not usually
provide the degree of neural blockade seen with thoracic paravertebral
block (TPVB), but its simplicity is especially useful in certain
patients, for example, the ventilated ICU patient with multiple rib
fractures who is receiving low molecular weight heparin anticoagulation.
CE, Kirz LI, VadeBoncouer TR, et al. Continuous infusion of
interpleural bupivacaine maintains effective analgesia after
cholecystectomy. Anesth Analg 1991;72:516–521.
DP, Lema MJ, de Leon-Casasola OA, et al. Interpleural analgesia for the
treatment of severe cancer pain in terminally ill patients. J Pain Symptom Management 1993;8:505–510.
Kleef JW, Logeman EA, Burm AG, et al. Continuous interpleural infusion
of bupivacaine for postoperative analgesia after surgery with flank
incisions: a double-blind comparison of 0.25% and 0.5% solutions. Anesth Analg 1992;75:268–274.
