Immature and Adolescent Athletes
Editors: Schepsis, Anthony A.; Busconi, Brian D.
Title: OSE Sports Medicine, 1st Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > Section I – Special Issues > 5 – Immature and Adolescent Athletes
5
Immature and Adolescent Athletes
Peter G. Gerbino
The number of immature and adolescent athletes increases
yearly. Despite the oft-lamented rise in childhood obesity, sports
participation by young boys and girls has continued to become an
essential part of childhood for more children. Strength, speed, and
sophistication have increased, raising performance levels and injury
levels. As in adult sports medicine, most injuries are overuse problems
that respond to rest and attention to technique. Macrotrauma injuries
have also increased, as has awareness of the natural history of
undertreated macrotrauma injuries. Pediatric sports medicine is the
understanding and management of overuse and macrotrauma injuries by
operative and nonoperative means.
yearly. Despite the oft-lamented rise in childhood obesity, sports
participation by young boys and girls has continued to become an
essential part of childhood for more children. Strength, speed, and
sophistication have increased, raising performance levels and injury
levels. As in adult sports medicine, most injuries are overuse problems
that respond to rest and attention to technique. Macrotrauma injuries
have also increased, as has awareness of the natural history of
undertreated macrotrauma injuries. Pediatric sports medicine is the
understanding and management of overuse and macrotrauma injuries by
operative and nonoperative means.
All sports injuries are caused by the interplay of two
or more risk factors. What would be an acceptable level of activity in
one child could be excessive in another with, for example, weaker bone.
Risk factors are divided into two groups: those related to the host or
athlete and those arising from the athlete’s environment. Surgery on
athletes is for repairing damaged tissues and for modifying host risk
factors. The most common host and environmental risk factors for injury
in the young athlete are listed in Box 5-1.
or more risk factors. What would be an acceptable level of activity in
one child could be excessive in another with, for example, weaker bone.
Risk factors are divided into two groups: those related to the host or
athlete and those arising from the athlete’s environment. Surgery on
athletes is for repairing damaged tissues and for modifying host risk
factors. The most common host and environmental risk factors for injury
in the young athlete are listed in Box 5-1.
SHOULDER
Little League Shoulder
Pathogenesis
-
Little League shoulder was originally
called “Little Leaguer’s shoulder” and refers to a stress reaction of
the proximal humeral physis. -
Risk factors include number of skilled throws per outing and open physes.
-
The disorder occurs in the throwing arm of pitchers or the racquet arm of tennis players with open physes.
-
-
The mechanism of injury is felt to be
repetitive torsion at the physis leading to physeal microfracture and
widening from lateral to medial.
Diagnosis
-
Diagnosis is made in an overhead throwing
or racquet sport athlete with lateral shoulder pain that can sometimes
radiate to the elbow. -
There is point tenderness at the lateral physis and pain with throwing or forced shoulder rotation.
-
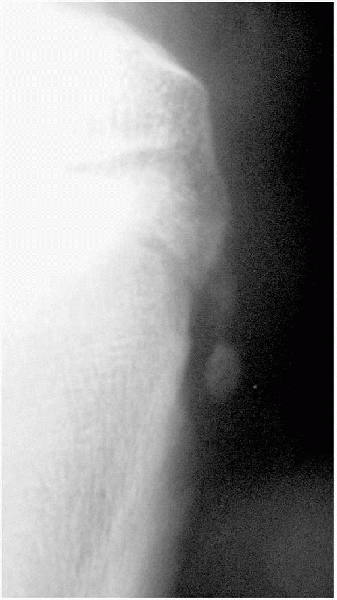
Radiographs typically show a widened lateral physis, compared with the contralateral side (Fig. 5-1).
P.62
BOX 5-1 RISK FACTORS ASSOCIATED WITH PEDIATRIC SPORTS INJURIES
Host
-
Growth tissues
-
Growth spurts
-
Gender
-
Anatomical malalignment
-
Conditioning, strength, flexibility
-
Preexisting medical condition
-
Psychological conditions
Environmental
-
Training error
-
Technique error
-
Coaching
-
Equipment
-
Playing surface
-
Drugs, supplements
-
Nutrition
-
Weather, temperature, humidity
Treatment
-
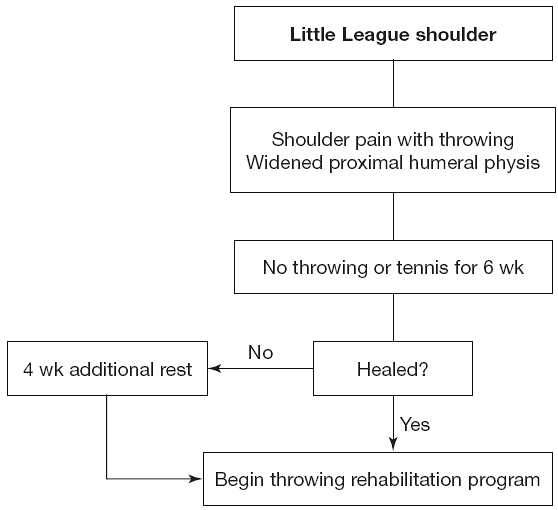
Treatment is rest from throwing or tennis until pain resolves in 6 to 8 weeks (Algorithm 5-1).
-
A gradual return to throwing is begun.
-
Limitations on number and types of pitches can prevent recurrence.
-
Complications from untreated Little League shoulder have not been described.
 |
|
Figure 5-1 Little League shoulder is a widened lateral physis of the proximal humerus. Cause is thought to be from torsional stress.
|
 |
|
Algorithm 5-1 Management of Little League shoulder.
|
Dislocation
Pathogenesis
-
Shoulder dislocations are extremely rare in children younger than 12 years of age.
-
In the adolescent athlete, it is similar to the adult injury, but care must be taken to rule out physeal fracture.
-
Most shoulder dislocations are anterior
and are caused by forced external rotation and abduction. This occurs
in falls and improper tackling in football. -
The nerves of the brachial plexus can be damaged during a shoulder dislocation.
Diagnosis
-
Diagnosis is made on the basis of the mechanism of injury, clinical appearance of the shoulder, and radiographs.
-
An anterior dislocation will be held in abduction and external rotation.
-
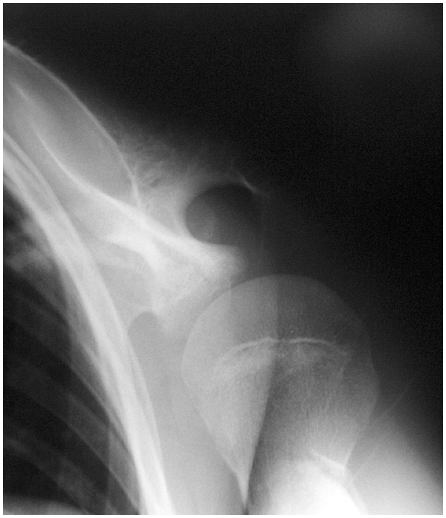
A standard axillary view is not usually
possible, so the shoulder trauma series of anteroposterior glenoid,
axillary, and scapula-Y views is modified to use a Velpeau axillary or
other “protected” axillary view (Fig. 5-2).
Treatment
-
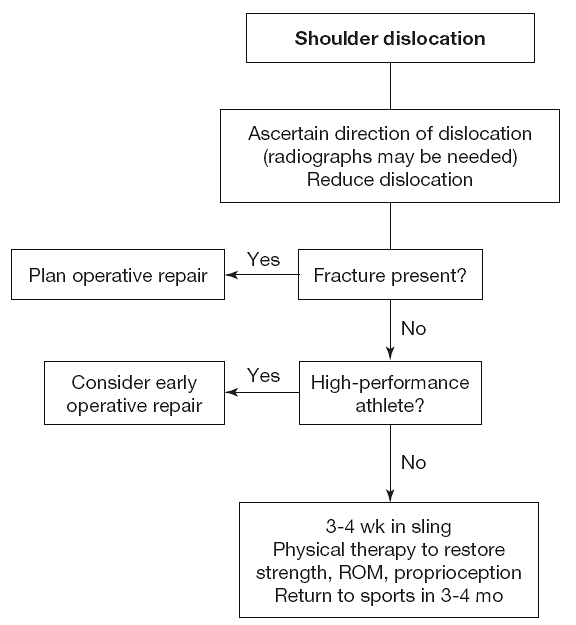
Qualified personnel can reduce the
dislocated shoulder immediately, but more commonly, the athlete is sent
to the emergency department some time later (Algorithm 5-2). -
Several reduction techniques have been
described, all of which use pain relief, muscle relaxation, and
traction of the upper extremity. -
Postreduction management is periscapular stabilization exercises following 3 to 6 weeks of rest in a sling.
-
In the competitive athlete, the case has been made for early operative repair, but this remains controversial.
-
As more sports medicine orthopedists
become comfortable with arthroscopic shoulder stabilization techniques,
more early repairs are being recommended. -
Despite this, the standard of care remains nonoperative treatment for first-time dislocations.
-
-
All recurrent dislocations are stabilized by arthroscopic or open means, usually with direct repair of the Bankhart lesion.
-
Even athletes with multidirectional
dislocations, traditionally not good operative candidates, are operated
on if symptoms persist despite adequate nonoperative therapy.
-
-
Untreated recurrent shoulder dislocation
may lead to degenerative arthritis. Overconstraint at repair leads to
rapid arthrosis and dysfunction. -
Operative repair always involves repair
of a Bankhart lesion with transglenoid suture holes or suture anchors
placed at or just on the articular portion of the glenoid rim.-
If lax, the rotator interval is closed,
but care is taken not to restrict external rotation so much that the
athlete generates pathologic joint reaction forces in an effort to
externally rotate and abduct. -
Normally, 20 to 30 degrees of external rotation beyond neutral is considered ideal.
-
 |
|
Figure 5-2
The Velpeau axillary view permits evaluation of the glenohumeral joint in the transverse plane without abduction of the shoulder. |
 |
|
Algorithm 5-2 Management of shoulder dislocation.
|
Microinstability
Pathogenesis
-
Microinstability is a newer concept that
explains the anterior shoulder pain felt by throwers, swimmers, and
others with repetitive overhead shoulder use. -
The capsule and rotator cuff become attenuated and the labrum frays, tears, and/or “peels back” from the glenoid rim.
-
Labral tears and peel-back can result in
painful snapping, and anterior humeral head subluxation is painful at
the rotator interval and coracoacromial arch. -
Damaged, painful areas result in reflex
inhibition and frequently lead to muscle imbalances between the rotator
cuff and major shoulder muscles causing a secondary subacromial
impingement. -
Primary impingement is not believed to exist in the young athlete.
-
In swimmers, posterior capsule tightness, combined with anterior capsulolabral pathology and impingement, is seen.
Diagnosis
-
Microinstability with or without labral tear should be suspected in any overhead athlete with impingement symptoms.
-
Positive impingement tests as described by Neer and Hawkins confirm the secondary muscle imbalance.
-
Subtle anterior laxity may be detected by the shift and load test or apprehension test.
-
Radiographs are normal, and magnetic resonance imaging (MRI) may miss a labral tear.
-
Even a direct arthrogram MRI using intra-articular gadolinium may not identify all labral tears.
 |
|
Figure 5-3
The clunk test is one of several tests useful for stressing the anterior labrum. It is performed by forcing the humeral head onto the area of suspected labral instability and then reducing the head (abduction when testing the anterior labrum) to produce a “clunk” when positive for laxity. |
Treatment
-
Initial treatment steps include rest from the causative activity and periscapular stabilization in physical therapy.
-
If this fails, labral repair, closure of the rotator interval, and limited capsulorrhaphy are indicated.
-
Thermal capsulorrhaphy has been used for
this condition but must be used judiciously with a rehabilitation
program, and prevent excessive stretching for at least 4 to 6 weeks to
prevent recurrence. -
Most surgeons now use arthroscopic plication to replace or enhance thermal capsulorrhaphy.
-
Overconstraint in a pitcher can result in the persistent loss of pitching ability.
ELBOW
Little League Elbow
Pathogenesis
-
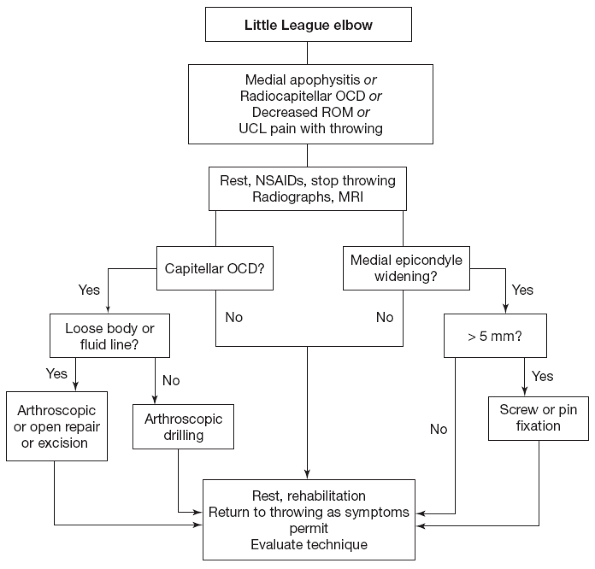
Originally called “Little Leaguer’s
elbow,” this group of injuries occurs in throwers and includes medial
epicondyle apophysitis from excessive traction, lateral
compression-induced radiocapitellar osteochondritis dissecans,
posterior ulnohumeral chondromalacia, and anterior soft-tissue tension
injuries. -
Within the six phases of throwing, early
and late cocking are most responsible for the valgus stress leading to
medial and lateral injuries. -
Acceleration, deceleration, and follow-through are most responsible for the anterior and posterior lesions.
-
The intrinsic risk factors for injury include age-dependent tissue strength, conditioning, and muscle strength.
-
Extrinsic factors include pitches thrown per outing, types of pitches, and throwing technique.
Diagnosis and Treatment
-
Diagnosis and treatment are considered in Algorithm 5-3.
Medial Epicondyle Avulsion
Pathogenesis
-
This can occur without warning after a single pitch or after weeks or months of medial epicondyle apophysitis.
-
The medial epicondyle is avulsed by the violent valgus forces of early-to-late cocking.
-
The elbow does not usually dislocate, but the ulnar collateral ligament (UCL) can be damaged by the valgus stress.
-
The number of pitches (or other hard throws) is the only risk factor associated with this injury.
Diagnosis
-
The athlete will have a painful swollen medial elbow.
-
Ulnar neuritis can occur but is uncommon.
-
There is usually a history of medial epicondyle pain and apophysitis.
-
Valgus stress will be painful, and there may or may not be valgus laxity as measured by palpable gapping.
-
Radiographs demonstrate a variable amount of medial epicondyle displacement (Fig. 5-4).
-
A gravity stress radiograph has been advocated to assess medial integrity if there is a question.
-
The MRI can be used to assess UCL integrity.
Treatment
-
Nondisplaced medial epicondyle avulsions are treated closed in a cast for 4 to 6 weeks.
-
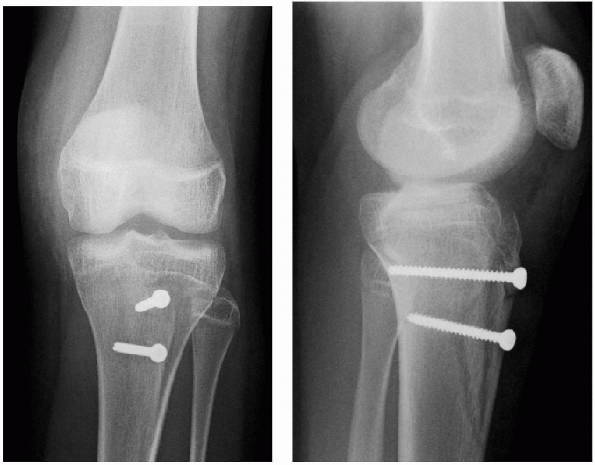
Avulsions larger than 1 cm are repaired with pins or 3.5-or 4.0-mm cannulated screws and direct repair of the UCL if torn (Fig. 5-5).
-
Fragments displaced between 3 and 10 mm are treated closed by some, repaired by others.
-
In a throwing athlete, the trend is to treat displacement greater than 3 to 5 mm with repair, but this continues to evolve.
-
Immediate repair allows early range of
motion and may prevent some of the flexion contracture complications
seen with closed treatment.
WRIST
Gymnast’s Wrist
Pathogenesis
-
Gymnasts and weightlifters place
supraphysiological loads on their wrists, using them as weight-bearing
joints. Over time, this can lead to physeal damage and dorsal impaction. -
Dorsal impaction refers to bone bruising and synovitis at the radiocarpal joint from repetitive wrist dorsiflexion under load.
-
Both can be chronically painful, and
physeal damage can lead to premature closure and a shorter or malformed
distal radius (Madelung’s deformity).
P.65
 |
|
Algorithm 5-3 Management of Little League elbow.
|
 |
|
Figure 5-4
Radiograph demonstrating medial epicondyle avulsion. Comparison films may be necessary. Early repair permits immediate motion and may decrease stiffness and permit faster recovery. |
 |
|
Figure 5-5 Repair of medial epicondyle avulsion with 4.0-mm cannulated screw.
|
P.66
Diagnosis
-
Gymnasts and weightlifters with wrist
pain require a thorough evaluation, but most commonly there will be
dorsal tenderness at the radiocarpal joint, radial physis, or both. -
Radiographs demonstrating positive ulnar variance, radial physeal bridging, or distal radius deformity are late findings.
-
MRI can detect paraphyseal edema, early physeal bridging or radiocarpal bone bruising.
Treatment
-
Rest will decrease pain and lead to healing of minor physeal damage or bone bruises.
-
Conservative measures include rest, technique changes, and use of wrist braces that limit dorsiflexion such as “lions-paws.”
-
Physeal bridging can be resected if
small, but large, physeal closures and deformity are treated with ulnar
epiphysiodesis and shortening with radius osteotomy as needed.
SPINE
Spondylolysis
Pathogenesis
-
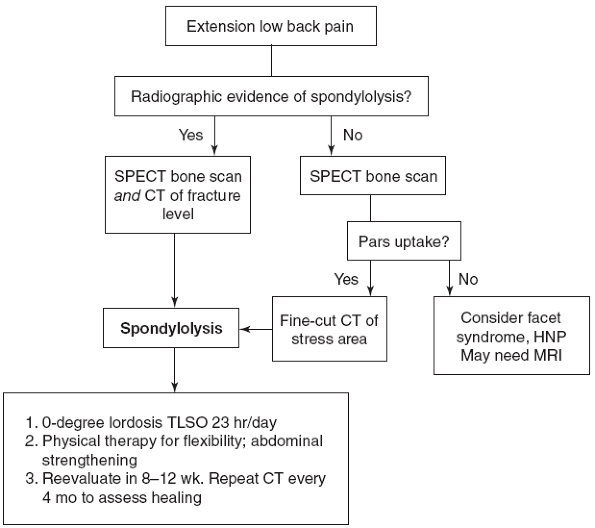
In the young athlete, 47% of all low back pain is caused by spondylolysis.
-
Repetitive spine hyperextension causes unilateral or bilateral stress fractures at the pars interarticularis, usually at L5.
-
Other levels or multiple levels may be involved.
-
Athletes in sports with spine extension
(such as diving, volleyball, soccer, dance, and figure skating) are at
higher risk, as are athletes with other spinal irregularities.
Diagnosis
-
The history will identify spine extension as a source of pain.
-
Physical examination confirms pain in extension, but not in flexion.
-
Radiculitis is uncommon.
-
Radiographs will show spondylolysis only when there is pars gapping or ongoing sclerosis.
-
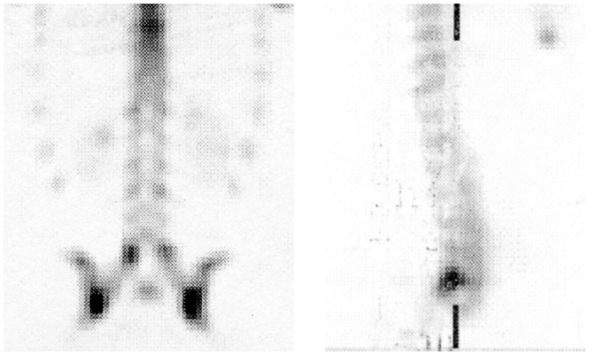
The single-photon emission computerized
tomography bone scan has been shown to be the best study for detecting
early pars stress injury (Fig. 5-6). -
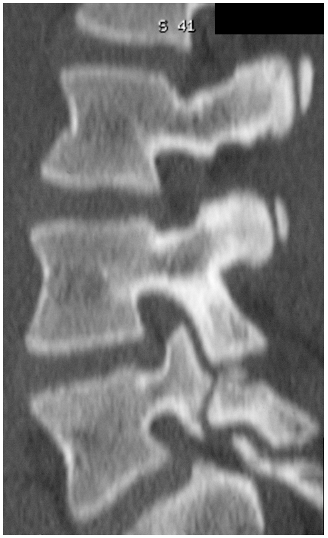
Focal computed tomography (CT), is
necessary to examine the metabolically active areas to ascertain
whether fracture or stress reaction is present and to document healing
after treatment (Fig. 5-7).
 |
|
Figure 5-6
Single-photon emission computerized tomography bone scan demonstrating increased uptake at pars interarticularis. A hot bone scan indicates increased metabolic activity with or without a visible fracture. A cold bone scan does not preclude a long-standing quiescent pars fracture. |
Treatment
-
It may take 6 to 9 months for complete healing.
-
Bilateral fractures and those that are metabolically quiet may heal with a painless fibrous union or may remain painful.
-
Persistent pain is an indication for repair or fusion.
 |
|
Figure 5-7
Focal CT is used to assess whether there is a visible fracture or simply prefracture stress reaction. It is also used to assess progressive healing. |
 |
|
Algorithm 5-4 Management of spondylolysis.
|
Juvenile Disc Herniation
Pathogenesis
-
A herniated nucleus pulposus (HNP) in a
young athlete is caused by the same extension and twisting forces under
load that cause HNP in an adult. -
There is much less collateral spine and
disc degeneration in an adolescent, and the disc is as likely to
herniate into an adjacent vertebral end plate (atypical Scheuermann’s
disease) or centrally as it is to herniate into the classic
posterolateral foramen. -
HNP fragmentation is less common in this age group.
Diagnosis
-
The history provided by the adolescent with HNP will typically indicate back and buttock or proximal thigh pain.
-
True sciatica occurs but less commonly than in the adult.
-
A negative straight-leg raising test does not rule out HNP.
-
Radiographs will not show disc space narrowing or degenerative changes.
-
The MRI will show the herniation, be it central, posterior lateral, or into an end plate.
Treatment
-
Herniated discs in the young athlete rarely require surgery.
-
They are treated with rest, supportive
bracing, and physical therapy to stretch tight hamstrings and
strengthen paraspinal muscles and abdominals. -
Persistent pain or sciatica sometimes
responds to lumbar epidural steroid injections, and, if all else fails,
surgical discectomy is warranted.
HIP
Snapping Psoas
Pathogenesis
-
The iliopsoas tendon attaches to the lesser trochanter after crossing the anteromedial hip joint.
-
A tight tendon, bursitis, or prominent femoral head can cause snapping with inflammatory changes and pain.
-
Poor technique, such as forward pelvic
rotation and lumbar lordosis, allows greater hip external rotation but
shortens the psoas tendon and presents a more prominent humeral head to
the tendon on external rotation. -
Painful snapping during hip external rotation is the result. The tendon snaps over the femoral head or iliopectineal eminence.
-
It is believed that the rectus femoris tendon can contribute to the snapping phenomenon.
Diagnosis
Treatment
-
Correction of technique, psoas stretching, rectus stretching, and core stabilization techniques address the cause.
-
A chronic or resistant case may require fluoroscopicguided injection of corticosteroid to the psoas and rectus femoris sheaths.
-
Rarely is partial surgical release or psoas lengthening necessary.
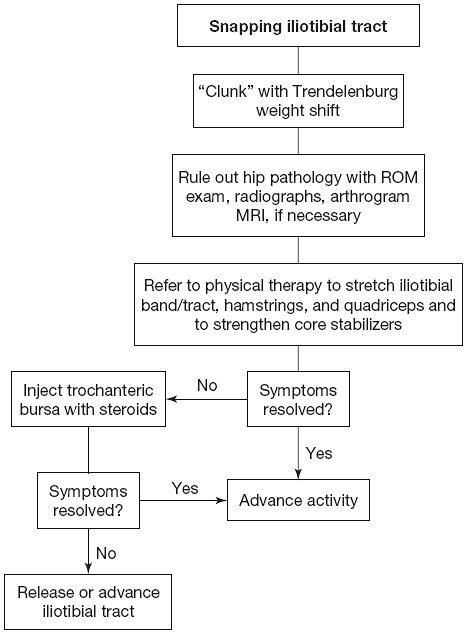
Snapping Iliotibial Tract
Pathogenesis
-
The iliotibial tract connects the gluteus maximus to Gerdy’s tubercle on the anterior lateral tibia.
-
Excessive use or tightness in the tract results in painful snapping at the greater trochanter.
-
Bursitis ensues, eventually leading to fasciitis and fibrosis.
-
Risk factors for development are
controversial but are thought to include overuse of the gluteus maximus
because of relative weakness in the other peripelvic muscles. -
Femoral anatomy has been theorized to be a risk factor, but no conclusive evidence has been found.
Diagnosis
-
The standing patient can usually shift
his or her body weight to the opposite leg by thrusting the pelvis
laterally, thus causing a large “clunk” to be felt and heard. -
Many times, the clunk is painless, but chronic snapping can lead to refractory pain.
-
The Ober test usually demonstrates a tight iliotibial band but often is normal.
-
Hamstrings are frequently tight and quadriceps, abdominals, abductors, and paraspinals are frequently weak.
Treatment
-
The mainstays of iliotibial tract treatment include avoiding the habit of making the hip snap and core muscle strengthening.
-
Hamstring and quadriceps strengthening is also important, and iliotibial band stretching is needed when tight.
-
Injecting the trochanteric bursa with corticosteroid can decrease pain (Algorithm 5-5).
-
Resistant cases are treated with excision of the snapping section of the iliotibial tract.
-
This may be a thickened window resection over the greater trochanter or a release of the posterior half of the tract.
KNEE
Meniscus Tears and Discoid Meniscus
Pathogenesis
-
Meniscus tears are frequently caused by twisting injuries to the knee.
-
Compression and shear forces lead to various tear patterns.
-
Peripheral meniscus avulsions can occur in tension.
-
A discoid meniscus is usually lateral and congenital.
-
The tear of a discoid occurs when the
anterior-posterior excursion of the lateral meniscus is lost when the
horns are connected because of the discoid shape. -
The meniscus can form with no posterior
attachment or tear anteriorly or posteriorly to allow meniscus motion,
which must occur during knee flexion-extension. -
A painless or painful clunk is usually palpable with knee flexion-extension.
-
A bucket handle tear can get trapped in the notch preventing full extension.
 |
|
Algorithm 5-5 Management of snapping iliotibial tract.
|
Diagnosis
-
An isolated meniscus tear is painful along the joint line in the region of the tear.
-
The accompanying knee hemarthrosis occurs over several hours.
-
A classic McMurray test of a painful clunk with extension after hyperflexion occurs in a small number of tears.
-
Knee hyperflexion and external or internal tibial rotation stresses the posterior horns and is a very sensitive test for a tear.
-
Radiographs are usually negative.
-
MRI is sensitive and can rule out bone bruises that can mimic meniscus tears.
P.69
Treatment
-
A locked knee needs to have the meniscus tear reduced and repaired within the first 1 to 2 weeks of injury for best results.
-
Children’s meniscus tears heal better than adults, but more peripheral tears still heal better than those in the avascular zone.
-
Irreparable tears are excised.
-
Repairs can be done using outside-in, inside-out or all-inside techniques.
-
Frequently, all-inside devices are used
for the most posterior region; inside-out for the majority of the
meniscus and outside-in for the anterior horn.
-
-
Discoid meniscus tears are especially difficult and must be saucerized, as well as repaired.
-
The repair is protected from full weight-bearing or range of motion (ROM) for 4 to 6 weeks.
-
Sports are permitted after 3 to 4 months of physical therapy to restore ROM, strength, and proprioception.
Anterior Cruciate Ligament Tears
Pathogenesis
-
Anterior cruciate ligaments (ACLs) are torn with a valgus deceleration mechanism or by hyperextension.
-
The ligament fails in tension.
-
Females—especially soccer, basketball,
and volleyball athletes—have a 4- to 10-fold increased risk of ACL tear
compared with males.-
The reason for the discrepancy remains
unknown, but hypotheses concerning landing style, muscle balance, and
ligament size are most consistent with the research findings.
-
-
The ligament can fail at the tibia, femur, or midsubstance.
-
Most injuries occur close to the femoral attachment.
Diagnosis
-
The athlete with an ACL tear usually describes a “pop,” followed by the inability to continue with the game.
-
A rapid (within 1 hour) effusion is typical.
-
Early examination shows increased anterior tibial translation with the Lachman and anterior drawer test.
-
Once the effusion is substantial, the athlete may not be comfortable enough to cooperate with the examination for 1 or 2 weeks.
-
Other than demonstrating the soft-tissue distension from effusion, the plain radiographs are usually normal.
-
The Segond or lateral capsular avulsion fracture has been described as diagnostic of ACL tear.
-
MRI is diagnostic.
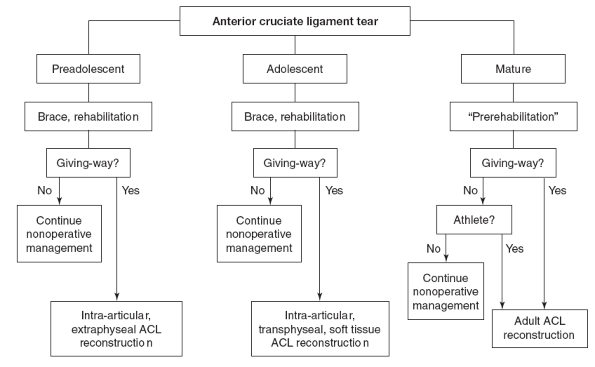
Treatment
-
Acutely, ice is used to decrease effusion.
-
Crutches allow protected weight-bearing.
-
No bracing is needed acutely.
-
Physical therapy can restore ROM and decrease swelling.
-
Aspiration can relieve distension pain and allow earlier examination.
-
Recent evidence has led to more and earlier ACL reconstruction in athletes.
-
Reconstruction techniques employ patellar tendon, hamstring, quadriceps tendon, or iliotibial band autograft and allograft.
-
In the immature athlete, the open physis must not be damaged.
-
The adolescent with less than 2 cm of
growth remaining or at Tanner stage 3 or greater is considered mature.
The full spectrum of adult procedures can be used (Algorithm 5-6). -
In the postpubescent athlete with more
than 2 cm growth remaining, transphyseal soft tissues (usually
hamstring) grafting is used. -
In the prepubescent, every effort is first made to brace and rehabilitate the athlete nonoperatively.
-
If giving way persists, an intra-articular, extraphyseal technique is used, utilizing the hamstring or iliotibial band.
-
This repair is not isometric but studies have not shown that these athletes need a second procedure after maturity.
-
-
Rehabilitation is typically the same 6-month closed-chain adult protocol.
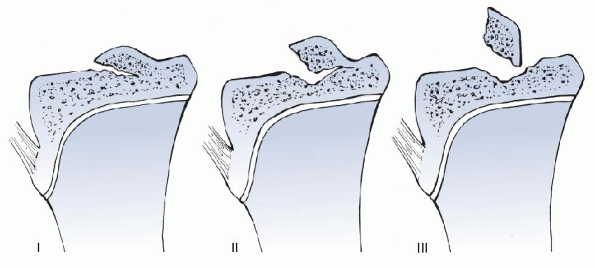
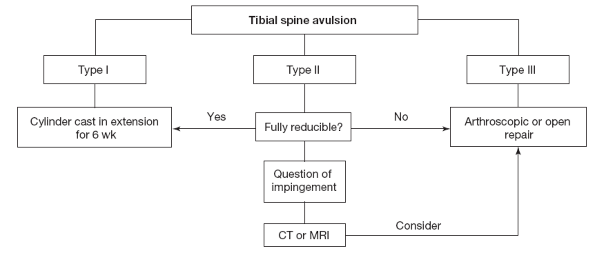
Tibial Spine Avulsion
Pathogenesis
-
Valgus deceleration or hyperextension does not always lead to ACL tear.
-
The tibial plateau bone sometimes fails before the ligament.
-
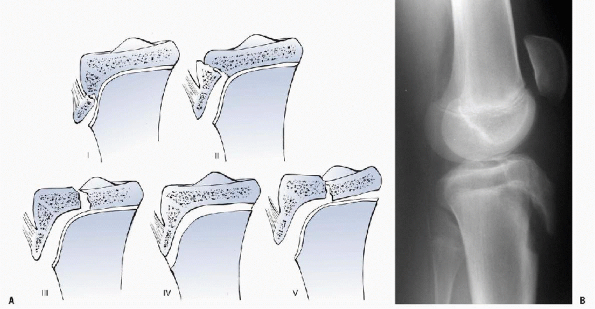
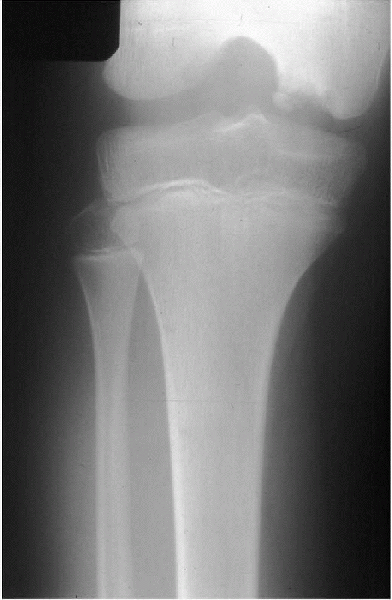
This type of tibial spine avulsion has been described, depending on the degree of fragment displacement (Fig. 5-8).
Diagnosis
-
Tibial spine avulsion fracture is very similar to ACL tear.
-
A distinct “pop” at the time of injury is less common.
-
Physical examination will show only a positive Lachman in type III, completely displaced fragments.
-
Radiographs show the fracture but it can
be difficult to assess a loose but anatomically positioned type III
from a hinged type II. -
CT or MRI can be used to assess fragment position more accurately.
Treatment
-
Type I and reducible type II fractures can be treated by 6 weeks of cast immobilization in extension (Algorithm 5-7).
-
Some type II fractures have the
intrameniscal ligament or anterior horn of the medial meniscus
entrapped under the fragment anteriorly.-
These may be impossible to reduce, leading to a “cyclops” lesion and loss of terminal extension.
-
-
Some other type II fractures are completely separated from the tibia and have reduced healing potential.
-
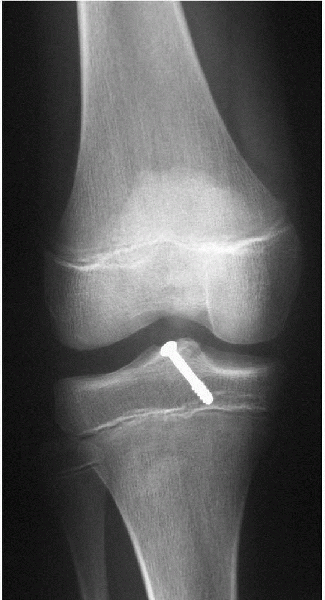
Irreducible type II and all type III fractures are treated with operative repair.
-
This can be done open or arthroscopically with predictable healing in 6 weeks (Fig. 5-9).
-
-
Long-term problems have not been reported for these fractures when treated properly.
P.70
 |
|
Algorithm 5-6 Management of ACL tear.
|
Tibial Tubercle Avulsion
Pathogenesis
-
A sudden supramaximal force on the tibial tubercle by the patellar tendon can avulse the apophysis.
-
The highest peak forces occur with eccentric loading such as landing a jump.
-
A preexisting apophyseal stress fracture (Osgood-Schlatter’s syndrome) is common.
-
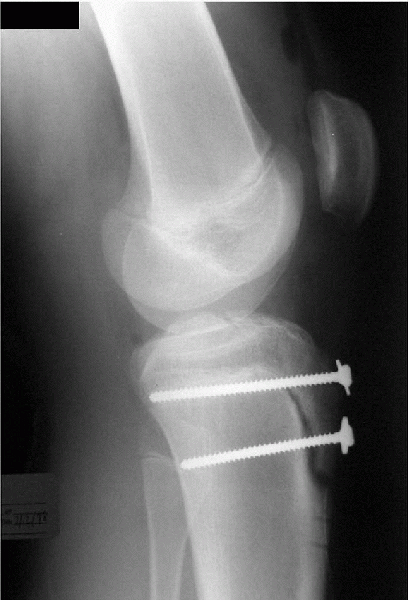
The fracture is graded by degree of separation from minimal displacement to intra-articular extension and gross displacement (Fig. 5-10).
 |
|
Figure 5-8
Meyers and McKeever classification of tibial spine fractures. Type I has minor displacement and is treated closed in extension. Type II is hinged posteriorly, but with plain radiographs the attachment may be difficult to assess. If reducible, type II fractures can be treated nonoperatively. Many type II fractures cannot be reduced because the medial meniscus or intrameniscal ligament is entrapped. Type III fractures always require operative repair. |
Diagnosis
-
The athlete has pain after intensive extensor mechanism activation.
-
There is swelling and a variable amount of tibial tubercle prominence.
-
Straight-leg raising is painful with an extensor lag.
-
The tibial tubercle is tender to palpation.
-
Radiographs show minimal to complete avulsion.
Treatment
-
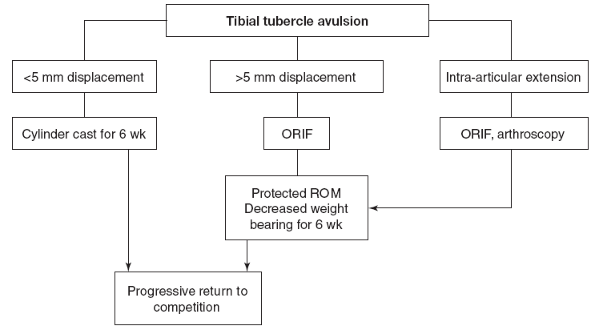
Ice and immobilization are the first line of treatment, with casting in extension for minimally displaced fracture.
-
Displacement of more than 5 mm is treated with open reduction internal fixation with two screws (Fig. 5-11, Algorithm 5-8).
-
If the fracture extends into the joint, arthroscopic visualization can ensure anatomic reduction.
-
With stable fixation, motion can begin immediately.
-
Healing and full weight-bearing can be expected by 6 weeks.
P.71
 |
|
Algorithm 5-7 Management of tibial spine avulsion.
|
 |
|
Figure 5-9
Repair of a type III tibial spine avulsion. Most surgeons are using arthroscopic means and avoiding the physis. Comminuted fractures can be repaired with suture through holes made with the ACL tibial tunnel guide. |
Patellofemoral Stress Syndrome
Pathogenesis
-
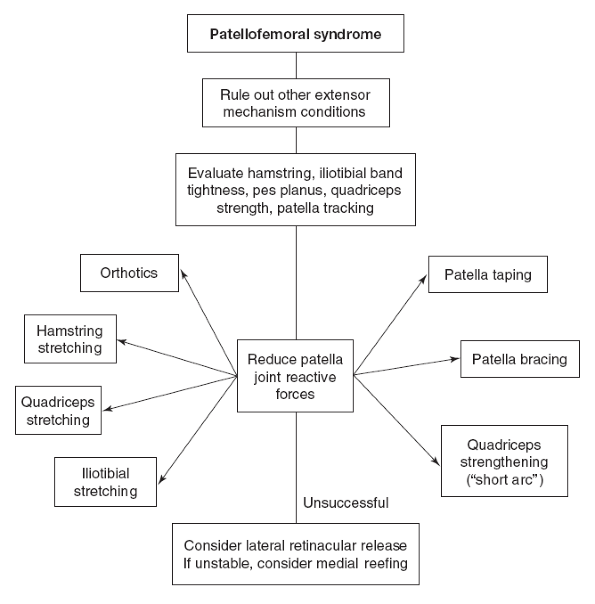
Patellofemoral stress syndrome represents several poorly understood injuries to the extensor mechanism.
-
A major component of patellofemoral stress syndrome is joint-reactive force overload to the patella.
-
Abnormal patella tracking, hamstring
tightness, quadriceps weakness, patella alta, excessive foot pronation,
and/or a sudden increase in activity are the usual causative factors. -
The exact pathophysiology is not known
but one hypothesis for the patellar component is that patella
deformation under load leads directly to patella pain. -
Synovitis, neuroma formation, and pain in the other surrounding tissues have been implicated in the genesis of this syndrome.
Diagnosis
-
Anterior knee pain is very common, and it is first necessary to eliminate other sources of pain.
-
If there is pain with anterior-posterior compression of the patella, the diagnosis is patellofemoral stress syndrome.
-
Associated risk factors—such as quadriceps strength, hamstring tightness, patella tracking, and pes planus—are assessed.
-
Radiographs demonstrating patella tilt are not necessary to make the diagnosis.
-
Other imaging studies have not been found to provide additional information.
 |
|
Figure 5-10 A:
Classification of tibial tubercle fractures. Type I has minimal separation. Type II requires fixation, and type III displays intra-articular extension. Type IV is a SH-I fracture of the entire tibial physis. Type V is a combination of types III and IV. B: A type III fracture is shown. |
 |
|
Figure 5-11
Repair of the displaced tibial tubercle fracture. The screws can cause pain with kneeling and are frequently removed. Problems with growth arrest leading to knee recurvatum have rarely been reported. |
Treatment
-
There is little evidence-based medicine to guide the treatment of patellofemoral stress.
-
Empirical studies show that quadriceps
strengthening with minimal patella joint reaction forces (straight-leg
raising) is effective. -
Patella taping can improve symptoms, as can bracing to displace the patella medially.
-
Other interventions—such as orthotics for
pes planus, hamstring stretching if tight, and limiting sprinting and
jumping—can be helpful (Algorithm 5-9).
Patellar Instability
Pathogenesis
-
A patella can recurrently subluxate or
dislocate when there is lateral patella tracking, generalized
ligamentous laxity, patella alta, severe genu valgum, or medial
attenuation after traumatic dislocation. -
Virtually all patella instability leads to lateral subluxation.
-
Medial instability can occur after surgical overcorrection.
-
The medial patellofemoral ligament is the primary restraint to lateral motion.
-
Genu valgum and other anatomic alignments
resulting in a Q-angle greater than 20 degrees result in lateral
patella displacement caused by a lateral tibial attachment.
P.73
 |
|
Algorithm 5-8 Management of tibial tubercle avulsion.
|
 |
|
Algorithm 5-9 Management of patellofemoral syndrome.
|
P.74
Diagnosis
-
Frequently, the athlete will be aware of the subluxation episodes. Other times, there is only a history of painful giving way.
-
Physical examination will demonstrate patellofemoral pain, a positive lateral apprehension test (Fig. 5-12) and one or more risk factors, such as patella alta, lateral tracking or genu valgum.
-
The J-sign (patellar tracking in a J-pattern) has been described in association with both lateral tracking and instability.
-
No studies have shown that this sign can predict pathology or effects of various treatments.
-
-
Radiographs can demonstrate patella tilt but cannot predict instability.
-
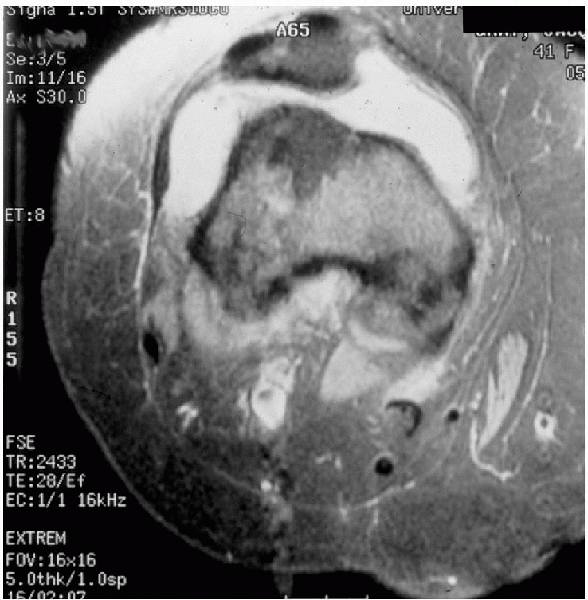
MRI can show lateral condyle bruising and medial retinacular tearing after dislocation (Fig. 5-13).
Treatment
-
Acutely extending the knee and moving the patella medially will reduce a dislocated patella.
-
Radiographs are obtained to ensure that no fracture or loose bodies are present.
-
Most often, a 4-week course of nonoperative therapy is tried with restricted ROM and a brace to displace the patella medially.
-
Straight-leg raising exercises to
strengthen the quadriceps and especially the vastus medialis obliquus
are begun. This is the same regimen used for chronic lateral
subluxation. -
If instability persists, a medial retinacular repair, reefing, or reconstruction with or without lateral release can be done.
-
Where there is gross instability, an anatomic mediofemoral patellar ligament reconstruction can be performed.
-
If instability persists or recurs
following proximal realignment or if there is tubercle malalignment, a
medial tubercle transfer or Fulkerson procedure can be done after
physeal closure (Fig. 5-14).
 |
|
Figure 5-12
The apprehension test is performed by displacing the patella laterally. Pain or apprehension that the patella will dislocate indicates previous negative experience with lateral subluxation. |
 |
|
Figure 5-13 MRI of a knee after patella dislocation, lateral condyle bruising, and medial retinacular disruption are diagnostic.
|
Osgood-Schlatter’s Syndrome
Pathogenesis
-
Osgood-Schlatter’s syndrome is a poorly understood overuse problem at the patellar tendon’s attachment to the tibia.
-
Variously referred to as a tendonitis,
apophysitis, or enthesitis, there is no evidence that this is an
inflammatory condition. Rather, it is most likely a stress fracture of
apophyseal cartilage from traction forces. -
It occurs predominantly in 12- to 13-year-old boys who are running and jumping excessively.
-
There seems to be relatively weak quadriceps and tight hamstrings in this population, but this has not been formally studied.
P.75
 |
|
Figure 5-14
Anteriomedialization of the tibial tubercle realigns the patellofemoral mechanism distally to prevent subluxation. It elevates the tubercle to decrease joint-reactive forces. |
Diagnosis
-
The athlete complains of pain while running and jumping.
-
Symptoms may have occurred on and off in the past.
-
The tibial tubercles may or may not be enlarged but will always be tender to palpation.
-
The hamstrings are usually tight and the quadriceps weak for the athletic demands required.
-
Radiographs and MRIs are normal early in the process.
-
As the condition progresses, the more
vertical portion of the tibial physis width increases, and the
apophysis becomes irregular or fragmented (Fig. 5-15).
Treatment
-
Osgood-Schlatter’s syndrome has been treated in many ways.
-
Benign neglect is advocated by some who
note that, if the tubercle does not become avulsed, pain will cease
when the physes close. -
Others prescribe rest from running and jumping with or without physical therapy to stretch and strengthen the thigh muscles.
-
Historically, casting has been used with success.
-
In hyperactive boys who have failed to
heal with relative rest, casting or use of an immobilizer may be the
only effective treatment. -
If left untreated, complications can
include chronic pain, tubercle avulsion, and painful accessory tibial
tubercle ossicle as an adult.
P.76
 |
|
Figure 5-15 Osgood-Schlatter’s syndrome with widening of the physis and fragmentation of the apophysis.
|
Osteochondritis Dissecans
Pathogenesis
-
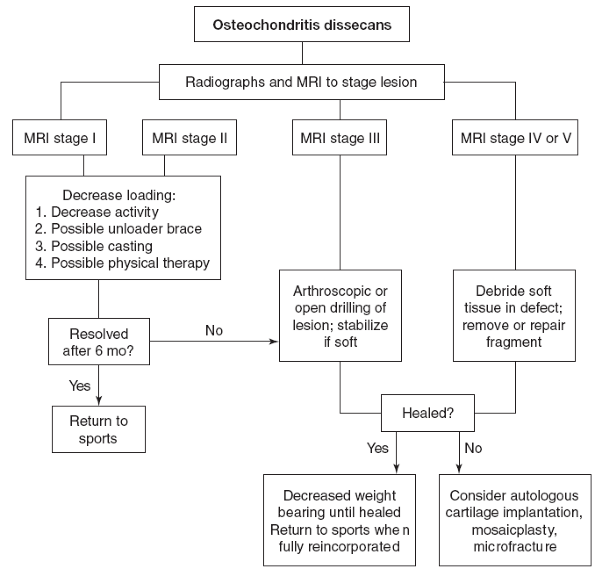
Osteochondritis dissecans (OCD) is a
condition occurring in the young athlete characterized by progressive
injury to the subchondral weight-bearing bone. -
It has been described in most joints but is most often seen at the posterolateral aspect of the medial femoral condyle.
-
One theory is that it is caused by
repetitive impact with the tibial spine, but this can only explain some
OCD cases. A second theory holds that these injuries result from
circulation abnormalities. A third theory maintains that the
subchondral bone is transiently weak during growth and susceptible to
crush injury. -
Asymptomatic subchondral bone bruising and edema are the earliest signs.
-
Progressive subchondral damage occurs if
the stresses continue, leading to avascular necrosis, fragment
separation from the underlying bone, fracture of the articular
cartilage, and finally dislocation of the fragment (Fig. 5-16).
 |
|
Figure 5-16 Advanced OCD of the knee with AVN and fragmentation.
|
Diagnosis
-
When OCD becomes symptomatic, the first complaints are that of activity-related knee pain.
-
The location of the pain is frequently difficult for the athlete to localize.
-
Effusion will occur at more advanced stages and locking or catching only when there is a loose body.
-
Palpation will frequently localize tenderness to the medial femoral condyle and the remainder of the knee examination is normal.
-
Wilson’s sign or an external rotation gait has not been shown to predict OCD.
-
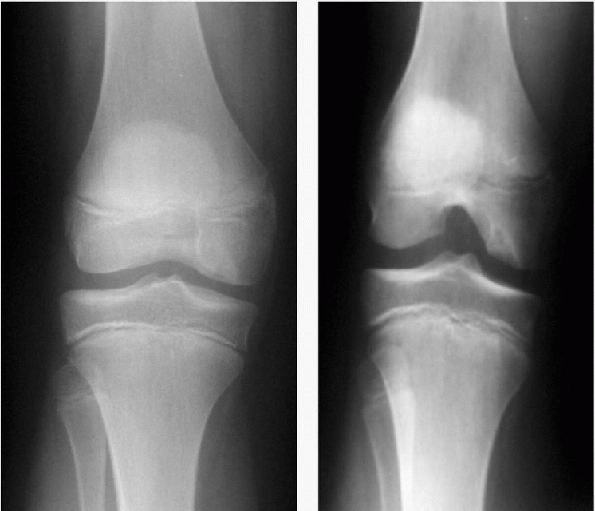
Radiographs must include a tunnel or notch view to avoid missing the typically posterior lesion (Fig. 5-17).
-
Plain radiographs, bone scans, or MRIs can reveal lesion staging (Fig. 5-18).
Treatment
-
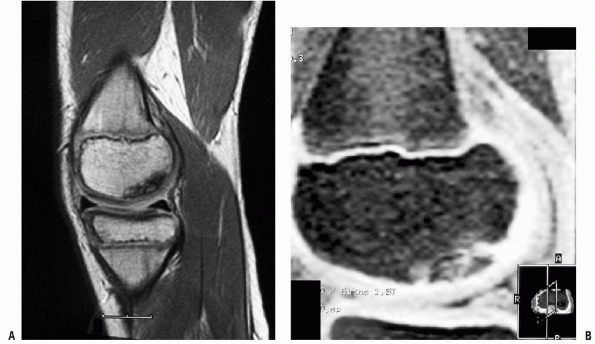
MRI stage I or II lesions are treated nonoperatively by decreasing loading forces to the lesion (Algorithm 5-10).
-
Activity reduction is a part of all treatment plans.
-
Some advocate a period of cast immobilization.
-
Others will achieve the pain-free state with a combination of activity reduction, unloader bracing, and crutch gait as needed.
-
Physical therapy to optimize lower-extremity muscle balance and flexibility has been advocated.
-
-
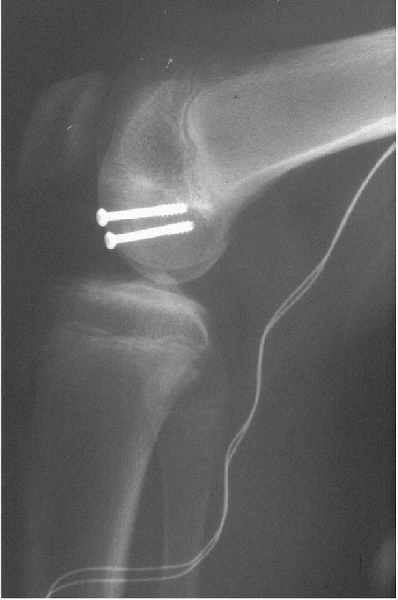
Surgical intervention is indicated for stage III (fragment-condyle fluid interface) or greater lesions.
-
Surgery is also indicated for stage I or stage II lesions that fail to heal after 6 months of nonoperative treatment.
-
For stable lesions, retrograde or transchondral drilling of the lesion stimulates the healing process.
-
Intact, unstable lesions are drilled, then fixed in situ with absorbable pins or screws.
-
Headed screws must be removed prior to weight-bearing or full motion.
-
-
Arthroscopic or open techniques can be used (Fig. 5-19).
-
Partially or fully detached lesions
require removal of any soft tissue in the fragment-condyle interface
prior to drilling and stabilization. -
Fragmented lesions are debrided and the defect treated with microfracture.
-
Defects larger than 2 cm2 or
that are associated with persistent pain or locking are treated with
allograft or autograft mosaicplasty or autologous chondrocyte
implantation.
-
ANKLE
Posterior Heel Pain
Pathogenesis
-
One of the most common complaints in the young athlete is posterior heel pain.
-
Achilles tendonitis, Sever’s apophysitis, and plantar fasciitis occur individually and in combination in this age group.
-
Lack of adequate ankle dorsiflexion in a running or jumping athlete is always causative.
-
There is a high incidence of
overpronation in this population, but pronation-eversion is more likely
to be compensation for lack of true dorsiflexion than to be causative. -
Athletes who wear soccer-type shoes are at greater risk because the shoes have four cleats at the heel and nine at the sole.
-
This results in deeper soil penetration
posteriorly, effectively, creating a “negative-heel” shoe that
increases the need for ankle dorsiflexion.
P.77
 |
|
Figure 5-17
Comparison of the anteroposterior view with the tunnel view in the same knee showing the ease with which the OCD lesion can be missed. |
 |
|
Figure 5-18 MRI staging of OCD lesions. A: Stage I. Homogeneous signal without fluid line or chondral breach. B: Stage II. Fluid line at base of lesion usually without definable chondral breach. Stages III and IV are not shown.
|
P.78
 |
|
Algorithm 5-10 Management of osteochondritis dissecans.
|
 |
|
Figure 5-19
Repair of stage III OCD with screws. Good compression is achieved, but the screws must be removed before moving the knee or weight-bearing. |
Diagnosis
-
The athlete complains of heel pain with activity, worsened when in soccer-style shoes.
-
Physical examination shows tenderness
along the Achilles tendon, at the calcaneal physis and/or at the medial
plantar fascia attachment. -
Frequently, there is hypertrophy of the
adductor brevis muscle. When asked to dorsiflex the ankle, the athlete
will evert and pronate.-
With the hind foot held in inversion, dorsiflexion will rarely be present beyond neutral.
-
-
Radiographs can occasionally show advanced Sever’s calcaneal apophysitis or a calcaneal spur but are not routinely obtained.
-
Likewise, MRI is only obtained for chronic cases of Achilles tendonitis to look for degeneration.
P.79
Treatment
-
Extensive Achilles stretching with the
heel locked in mild inversion is the mainstay of treatment. Stretching
several times per day is necessary to be effective. -
The knee is kept in extension as the soleus is not usually tight.
-
Heel cups or lifts to allow healing can be helpful.
-
Orthotics can take away compensatory pronation and exacerbate symptoms if used before adequate dorsiflexion is achieved.
-
Physical therapy is prescribed to ensure
proper stretching technique is followed and administer ultrasound for
tendonitis or fasciitis. -
Running and jumping are permitted as symptoms resolve.
Gymnast’s Ankle
Pathogenesis
-
Anterior ankle pain occurring in gymnasts and cheerleaders has become increasingly common.
-
Pain occurs with dorsiflexion only.
-
The underlying mechanism seems to be dorsal impaction from hyperdorsiflexion, leading to bone bruising or anterior synovitis.
Diagnosis
-
Anterior ankle pain on landings, dismounts, and floor exercises is the typical complaint.
-
The ankle soft tissues are tender to palpation and ankle dorsiflexion increases pain.
-
Forced dorsiflexion is frequently painful even without soft-tissue palpation.
-
Radiographs are normal.
-
MRI may show increased anterior
soft-tissue volume or bone bruising at the talar neck or anterior
tibial plafond but is usually normal.
Treatment
-
Rest and oral anti-inflammatory
medication can cure mild cases, but chronic cases can require
arthroscopic soft-tissue debridement. -
Simply instructing the gymnast to avoid deep landings with forced-ankle dorsiflexion is frequently effective.
-
Sometimes, the gymnast will need to strengthen the quadriceps before the technique can be corrected.
-
The condition will promptly recur if the gymnast’s technique is not corrected.
FOOT
Accessory Navicular
Pathogenesis
-
Painful accessory navicular occurs in
young athletes who have excessive tension in the posterior tibial
tendon or from direct mechanical rubbing in the shoe. -
Because the function of the posterior
tibial muscle and tendon is to support the arch, the typical athlete
with painful accessory navicular also has pes planus. -
Whether the accessory navicular is present at birth or occurs as a result of repetitive tension on the tendon is unknown.
-
Both tendonitis at the insertion and pain from the fibrocartilaginous nonunion are felt to contribute to pain.
Diagnosis
-
The athlete will indicate an enlarged erythematous area on the medial midfoot as the source of pain.
-
Examination will show an enlarged bony area at the insertion of the posterior tibial tendon on the navicular.
-
The site may rub on the inside of the athletic shoe.
-
The tendon is also tender for a variable distance from the insertion.
-
Frequently, the athlete will have generalized ligamentous laxity.
-
Radiographs show an enlarged navicular with an accessory ossicle medially.
-
Avulsion is rare.
Treatment
-
Nonoperative treatment includes rest and orthotics.
-
If this fails to relieve symptoms or if
the problem recurs, excision of the ossicle with navicular osteoplasty
and posterior tibial tendon repair are warranted. -
The Kidner procedure is no longer advocated.
Avascular Necrosis
Pathogenesis
-
There are two common sites of avascular
necrosis (AVN) of the foot in young athletes: the navicular (Kohler’s
disease) and the second metatarsal head (Frieberg’s infarction). -
The mechanism of injury is unknown, but
it is thought that excessive forces lead to compression or vascular
injury, thus initiating the process. -
Most cases resolve over time with rest.
-
Others can progress to fragmentation and loss of joint surface congruence.
Diagnosis
-
Foot pain localized to the second metatarsal head or navicular warrants radiographs.
-
Radiographs show AVN at the site.
-
MRI can show the extent of the lesion and whether fragmentation or instability is present.
Treatment
-
Initial treatment is rest, decreasing weight-bearing until symptoms are resolved.
-
This may require casting and crutch use for several weeks.
-
-
As pain resolves, weight-bearing is permitted.
-
Healing progress is evaluated with plain radiographs and, if necessary, MRI.
-
Failure of conservative therapy, loose fragments, and multiple fragments are indications for surgery.
-
Stable lesions are drilled, unstable lesions are fixed, and fragmented lesions excised much the same as for OCD.
P.80
SUGGESTED READING
Borges JL, Guille JT, Bowen JR. Kohler’s bone disease of the tarsal navicular. J Pediatr Orthop 1995;15:596-598.
Burkhart
SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of
pathology. Part I: pathoanatomy and biomechanics. Arthroscopy
2003;19:404-420.
SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of
pathology. Part I: pathoanatomy and biomechanics. Arthroscopy
2003;19:404-420.
d’Hemecourt PA, Gerbino PG II, Micheli LJ. Back injuries in the young athlete. Clin Sports Med 2000;19:663-679.
DiFiori
JP, Puffer JC, Aish B, et al. Wrist pain in young gymnasts: frequency
and effects upon training over 1 year. Clin J Sport Med 2002;12:348-353.
JP, Puffer JC, Aish B, et al. Wrist pain in young gymnasts: frequency
and effects upon training over 1 year. Clin J Sport Med 2002;12:348-353.
Dobbs
MB, Gordon JE, Luhmann SJ, et al. Surgical correction of the snapping
iliopsoas tendon in adolescents. J Bone Joint Surg Am 2002;84-A:420-424.
MB, Gordon JE, Luhmann SJ, et al. Surgical correction of the snapping
iliopsoas tendon in adolescents. J Bone Joint Surg Am 2002;84-A:420-424.
Dorizas JA, Stanitski CL. Anterior cruciate ligament injury in the skeletally immature. Orthop Clin North Am 2003;34:355-363.
Gerbino PG. Elbow disorders in throwing athletes. Orthop Clin North Am 2003;34:417-426.
Heintjes
E, Berger M, Bierma-Zeinstra S, et al. Exercise therapy for
patellofemoral pain syndrome. Cochrane Database Syst Rev 2003;
4:CD003472
E, Berger M, Bierma-Zeinstra S, et al. Exercise therapy for
patellofemoral pain syndrome. Cochrane Database Syst Rev 2003;
4:CD003472
Kartus
J, Perko M. The disabled throwing shoulder: spectrum of pathology. Part
II: evaluation and treatment of SLAP lesions in throwers. Arthroscopy
2004;20:336.
J, Perko M. The disabled throwing shoulder: spectrum of pathology. Part
II: evaluation and treatment of SLAP lesions in throwers. Arthroscopy
2004;20:336.
Katcherian DA. Treatment of Freiberg’s disease. Orthop Clin North Am 1994;25:69-81.
Kocher MS, Klingele K, Rassman SO. Meniscal disorders: normal, discoid, and cysts. Orthop Clin North Am 2003;34:329-340.
Micheli
LJ, Ireland ML. Prevention and management of calcaneal apophysitis in
children: an overuse syndrome. J Pediatr Orthop 1987; 7:34-38.
LJ, Ireland ML. Prevention and management of calcaneal apophysitis in
children: an overuse syndrome. J Pediatr Orthop 1987; 7:34-38.
Rowe CR. Historical development of shoulder care. Clin Sports Med 1983;2:231-240.
Shea
KG, Apel PJ, Pfeiffer RP. Anterior cruciate ligament injury in
paediatric and adolescent patients: a review of basic science and
clinical research. Sports Med 2003;33:455-471.
KG, Apel PJ, Pfeiffer RP. Anterior cruciate ligament injury in
paediatric and adolescent patients: a review of basic science and
clinical research. Sports Med 2003;33:455-471.
Tullos HS, Fain RH. Little league shoulder: rotational stress fracture of proximal epiphysis. J Sports Med 1974;2:152-153.
Wall E, Von Stein D. Juvenile osteochondritis dissecans. Orthop Clin North Am 2003;34:3413-3453.
Warme
WJ, Arciero RA, Taylor DC. Anterior shoulder instability in sport:
current management recommendations. Sports Med 1999; 28:209-220
WJ, Arciero RA, Taylor DC. Anterior shoulder instability in sport:
current management recommendations. Sports Med 1999; 28:209-220
