Triceps Tendon Repair and Reconstruction
acute and chronic settings. The treatment is different in each setting;
thus the method of managing both of these conditions is presented.
the patient has functional extension weakness, fatigue, or pain and the
patient who requires extension strength. (This includes almost
everybody.)
or ongoing or generalized enthesopathy and morbidity are present that
will not be addressed by triceps reconstitution, other methods may be
necessary.
weakness has become a major limitation of one’s daily activities, if
there has been no improvement over last 3 months, or if pain is rarely
a major factor.
unclear or unreasonable expectations of the reconstruction, or if he or
she is unable or unwilling to participate in the postoperative program
or to accept the period of postoperative recovery.
 |
|
Figure 11-1. A radiograph with bone fleck signifying triceps avulsion is a helpful but uncommon finding.
|
weakness is present in all, but complete loss of extension is observed
in less than 20% if untreated. Acute avulsion with fleck of bone is
seen in only about 15% (3,4). Pain subsides after 10 to 14 days, leaving residual weakness and fatigue pain as the major findings.
An MR examination is not usually required to make the diagnosis. There
may be some merit in localizing the disruption, which is usually at the
site of attachment of the central slip (11). The defect is palpable in about two-thirds of cases.
as the patient extends against resistance. Usually, the anconeus
expansion is intact, so some extension is possible. This is an
important determination, as the muscle may be used for rotational
reconstruction in chronic cases.
arm is prepped and draped but the tourniquet is not inflated. A
straight posterior skin incision is made and centered just medial to
the tip of the olecranon (Fig. 11-2). The
dissection carries through the triceps fascia and the defect is
identified. In most instances, the avulsion is from the central
attachment to the olecranon. Cruciate drill holes are placed in the
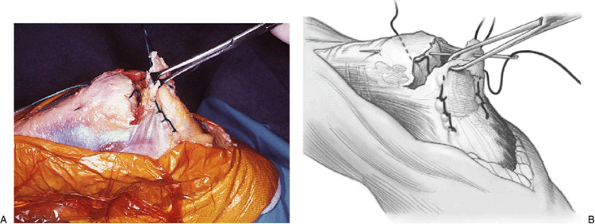
proximal ulna (Fig. 11-3). A No. 5 Mersilene
suture is introduced from distal to proximal. The triceps disruption is
mobilized and penetrated laterally by the suture. A Krachow type of
stitch is then placed with three to four passes on each side of the
triceps midtendinous locking region. The suture is then brought back
through the opposite cruciate hole (Fig. 11-4). This results in a very firm and
adequate repair, but a second transverse suture may be placed if there
is any question about the security of the attachment. The precise site
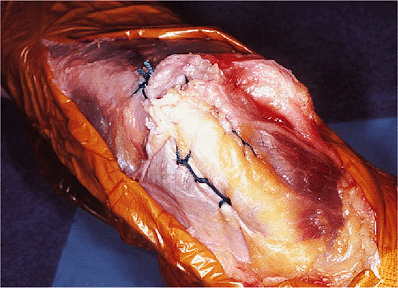
of disruption is roughened with a rongeur to enhance healing. Sutures
are tied at the margin of the subcutaneous border of the ulna with the
elbow in approximately 45 degrees of extension (Fig. 11-5).
 |
|
Figure 11-2. Midline incision showing tip of olecranon and medial epicondyle.
|
 |
|
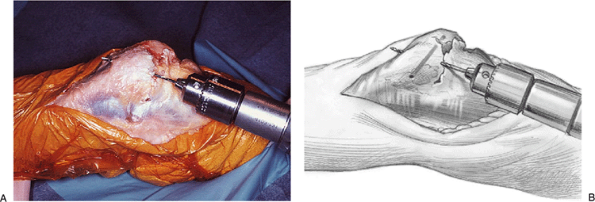
Figure 11-3. A,B: Cruciate drill holes are placed in the olecranon.
|
 |
|
Figure 11-4. A,B: A Krachow stitch secures the tendon as the suture is being brought back across the olecranon. Note: The tissue is handled with an Allis clamp to avoid crush injury.
|
 |
|
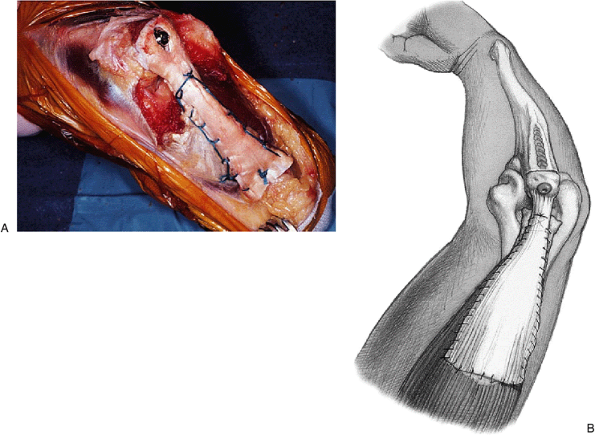
Figure 11-5. The completed repair is quite secure. Care is taken to tie the knot off the subcutaneous border to avoid irritation.
|
first or second day. This is maintained for approximately 4 or 5 days,
after which gentle passive assisted motion is allowed. Flexion is
limited to 90 degrees for the first 3 weeks. At the end of 3 weeks
flexion past 90 degrees is encouraged and allowed by active assist.
Passively assisted extension occurs with gravity and with the opposite
extremity. At 4 to 6 weeks active flexion and extension are allowed but
no forced extension is permitted for an additional 4 weeks. At 10 weeks
routine daily activities are permitted but no extension force greater
than 10 to 15 pounds is allowed. After 3 months if there is no pain,
the patient can gradually resume full daily activities. Over the next 3
months, full extension strength is allowed.
anconeus rotational reconstruction are as described earlier. If the
residual tendon is contracted and cannot be advanced to bone (Fig. 11-6) but the anconeus is present, Kocher’s interval is entered and the anconeus is mobilized (Fig. 11-7).
Ideally, the translocated muscle is left intact distally and the
proximal fascial attachment to the triceps is preserved. The muscle is
elevated from the ulna and rotated medially (Fig. 11-8).
The proximal ulna is prepared with cruciate drill holes. With the elbow
in about 30 degrees of flexion, a No. 5 nonabsorbable suture is used to
secure the rotated anconeus/triceps mechanism. Additional sutures are
placed as necessary and the original defect is closed if possible (Fig. 11-9).
 |
|
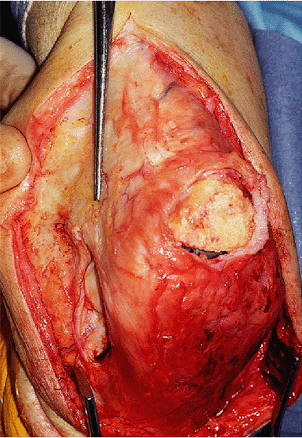
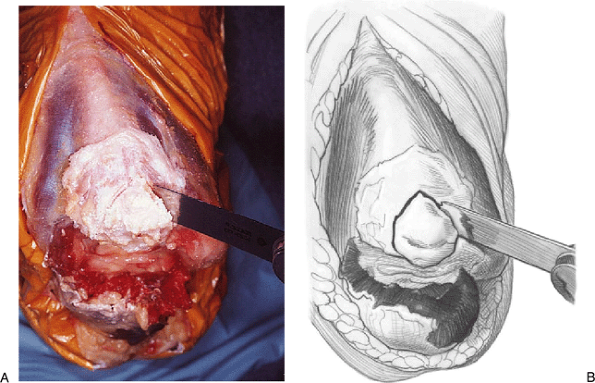
Figure 11-6. Large defect at the central attachment of the triceps in patient with total elbow arthroplasty.
|
 |
|
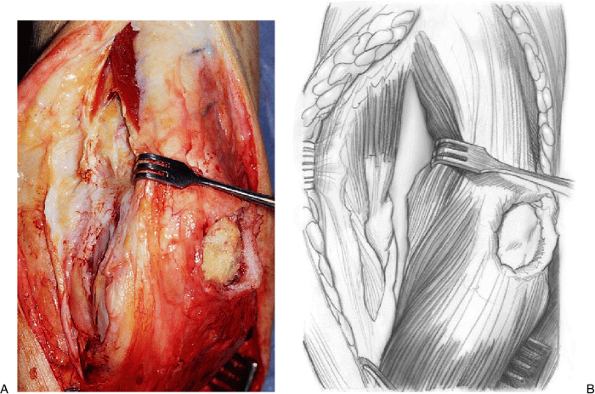
Figure 11-7. A,B: The anconeus is identified and separated from the extensor carpi ulnaris in Kocher’s interval.
|
 |
|
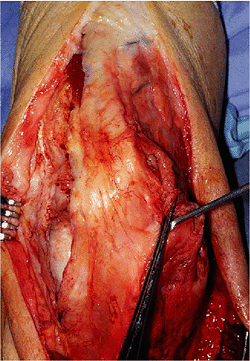
Figure 11-8. The anconeus is mobilized to cover the proximal ulna, leaving its distal attachment intact.
|
 |
|
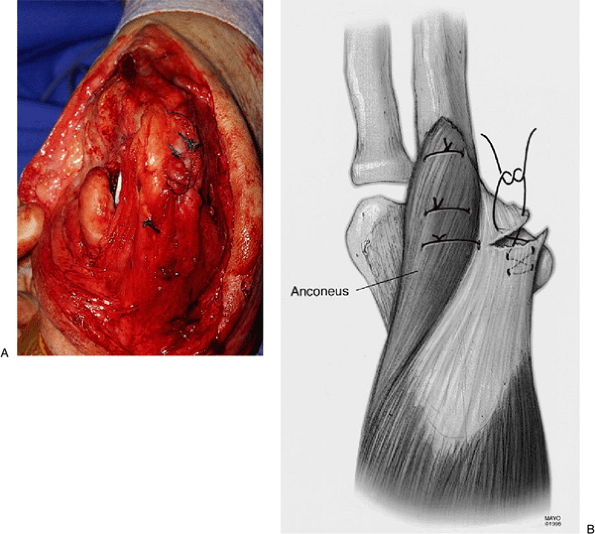
Figure 11-9. A,B: The anconeus is sutured with a crisscross stitch into bone. The defect is sewn to itself.
|
the attachment to the triceps has been violated, an Achilles tendon
allograft reconstruction is employed (Fig. 11-10). In this setting a chevron cut is made in the tip of the olecranon (Fig. 11-11). The calcaneal attachment of the Achilles tendon is then fashioned with the same angle (Fig. 11-12).
Care is taken to dissect the tendon sufficiently to identify its
precise insertion site on the calcaneus so the chevron cut in the
calcaneus is precisely positioned. The calcaneus from the Achilles
allograft is then fit within the V-shaped bed of the olecranon. Once
the proper position has been obtained, it is secured with a single AO
cancellous screw (Fig. 11-13). An additional
suture is placed with a transverse drill placed through the proximal
ulna, and a Krachow stitch is employed to further stabilize the tendon
allograft to the host olecranon. After the distal attachment
has
been secured, the triceps is mobilized as far distally as possible
according to the dictates of the pathology. The central portion of the
triceps, which contains the triceps tendon, is secured with a Krachow
stitch, and the triceps is then attached to the tendon graft as far
distally as possible with the elbow in about 30 degrees of extension (Fig. 11-14). Once this has been secured, the remainder of the Achilles graft is used to envelope the triceps musculature (Fig. 11-15). An absorbable No. O suture is used as a running stitch to secure the allograft over the triceps musculature.
 |
|
Figure 11-10.
Large defect in the triceps does not allow direct repair to bone. Violation of the anconeus attachment precludes anconeus rotation as a solution. |
 |
|
Figure 11-11. A,B: A chevron cut is made in the olecranon to receive the Achilles graft.
|
 |
|
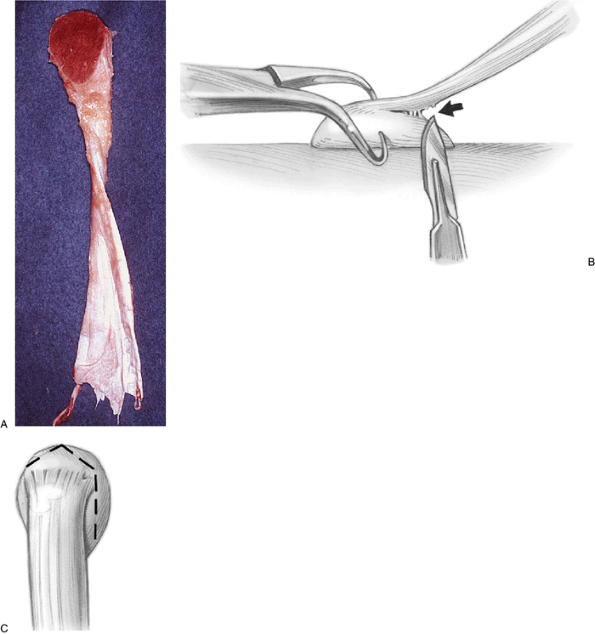
Figure 11-12. Achilles tendon allograft with calcaneus attached (A).
Preparation for attachment to olecranon requires dissection so attachment is approximately the length of the resected olecranon (B). The chevron cut in the calcaneus matches that of the olecranon (C). |
 |
|
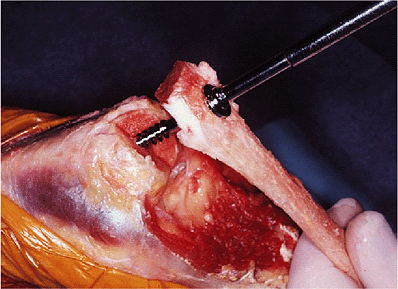
Figure 11-13. Calcaneus from the graft being secured with AO screw to the olecranon.
|
 |
|
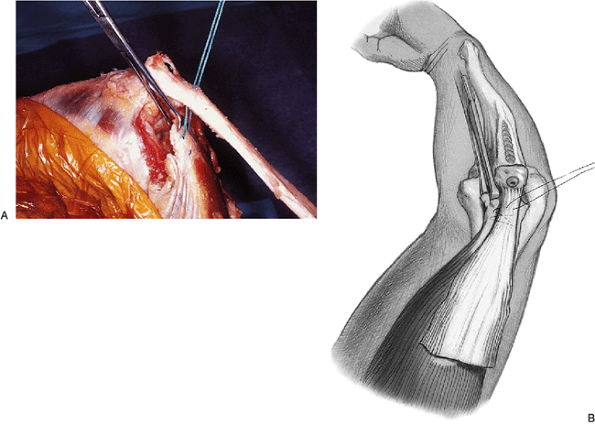
Figure 11-14. A,B:
The triceps is mobilized and securely attached to the allograft with a No. 5 nonabsorbable suture and tied at about 30 degrees of flexion. |
 |
|
Figure 11-15. A,B: The triceps is enveloped with the remainder of the Achilles graft.
|
intervention for triceps deficiency. Most communiqués are case reports.
If the avulsion includes a portion of bone, the AO tension band method
of fixation generally allows virtually normal function (1,2,5,8,10).
procedures. An acute repair was carried out in eight and a
reconstructive procedure was done in the other eight (4).
Of those repaired, strength returned to within an average of 90% of
“normal” of the opposite extremity. In those with a reconstruction the
mean strength recovery was about 85% of normal. Subjectively, all eight
repairs and seven of eight reconstructions were satisfied with their
outcome, and one had mild pain. Four of eight were noted as excellent
results in the acute and two of eight were noted as excellent results
in the reconstruction. The time to recovery was somewhat prolonged,
however, averaging more than 6 months, with some reconstructions still
demonstrating improvement a year after surgery.
had a transient ulnar nerve palsy, one patient developed a rerupture,
and one patient had persistent weakness and discomfort.
longer period for return of function than those with biceps tendon
repair. In our experience, rarely is significant strength improvement
noted before 6 months, and improvement continues for up to 1 year.
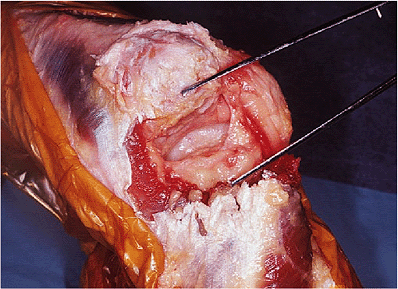
attachment of the triceps to the olecranon after open reduction with
internal fixation for a type II olecranon fracture treated by tension
band wiring. The triceps tissue was scarred and contracted, not
allowing direct suture repair (Fig. 11-16). Because the anconeus was intact, the extensor mechanism was reconstructed
with an anconeus rotational flap. The reconstruction allowed excellent
restoration of the triceps mechanism. The quality of the tissue and
repair is well demonstrated in the illustration.
 |
|
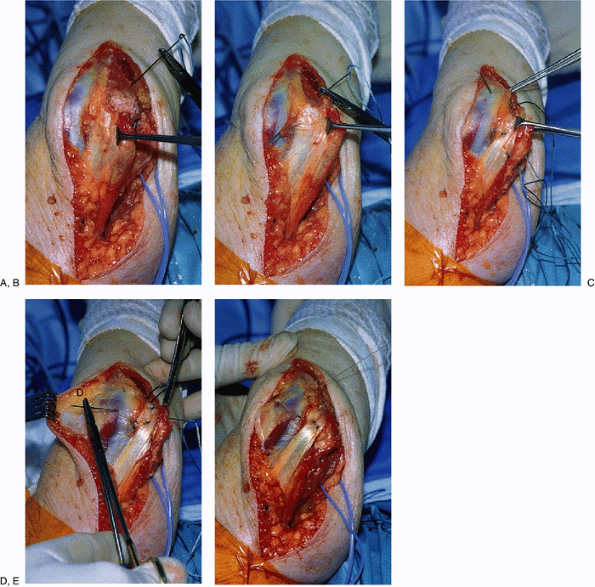
Figure 11-16.
Clinical example. The olecranon of 38-year-old female is devoid of tendon and has been drilled to allow reattachment in reconstruction (A). The anconeus muscle is mobilized and the needle punctures the anconeus/triceps attachment (B). The No. 5 nonabsorbable suture has been placed in the tendon with a Krachow stitch and is passed through the midolecranon drill hole (C). A second transverse suture is placed (D). The repair was secure with restored continuity of the triceps mechanism (E). |
