Fractures of the Coronoid and Complex Instability of the Elbow
that destabilizes the elbow because of interarticular fracture and
disruption to the ligamentous structures (2).
Others add soft-tissue involvement, including neural and vascular
injuries, as essential for the diagnosis of complex injury, but these
associated problems are uncommon (8).
approximately 50% of the varus/valgus stability of the joint, and the
articular surfaces provide an additional 50% (4).
The anterior band of the medial collateral ligament and the ulnar part
of the lateral collateral ligament are the primary constraints to
valgus and posterolateral rotatory instability, respectively. Both the
ulnar and radial parts of the lateral collateral ligament resist varus.
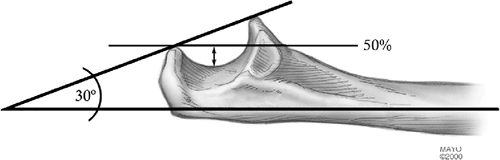
somewhat clearer. Treatment of a fractured coronoid is an essential
element of managing complex elbow instability. The amount of the
coronoid required for stability depends on the ligamentous integrity
and that of the radial head but is always at least 50% (Fig. 7-1).
This becomes important in preoperative planning and surgical approach,
which are necessary for effective restoration and fixation of coronoid
fractures.
When the medial and lateral ligaments are intact, it is not required
for stability. If the medial collateral ligament or coronoid are
damaged, it emerges as an important secondary stabilizer. Hence the
value of either fixing the fracture, if possible, or replacing the head
with a prosthesis is clear in the face of these specific associated
injuries. Procedures to address fractures of the radial head and
olecranon are discussed in detail in Chapters 5 and 6.
proximal ulna is restoration of the ulnohumeral joint. This principle
cannot be overstated (3,6).
 |
|
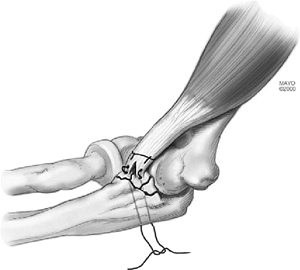
Figure 7-1. Coronoid 50% rule. A line from the tip of the olecranon and parallel to the shaft passes through 50% of the coronoid.
|
various loading configurations is proportional to the amount of
olecranon articulation present. The critical amount necessary for
maintenance of stability is at least 50%. In some instances the elbow
is unstable, with less than 50% of the olecranon fractured because of a
concomitant fracture of the coronoid. For this reason each elbow is
individually assessed for instability.
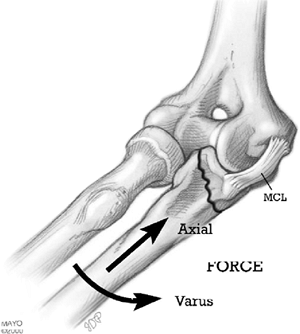
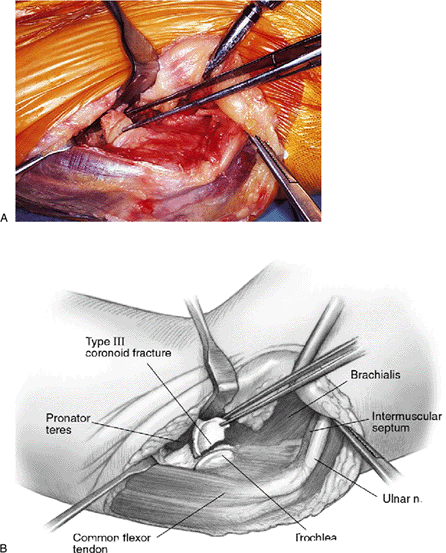
that a varus moment applied to the elbow in an extended position may
create a sagittal coronoid fracture. This fracture usually includes the
attachment of the ulnar collateral ligament on the sublime tubercle (Fig. 7-3) and might be termed a type IV or anterior medial fracture.
 |
|
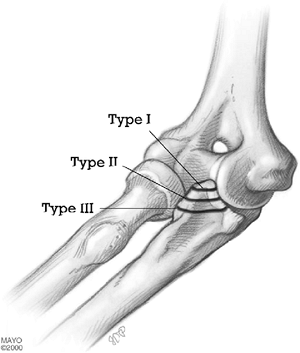
Figure 7-2. Regan-Morrey classification of coronoid fractures. Some type II and all type III are unstable.
|
tip of the coronoid and serve mainly as an indicator that the elbow has
dislocated or at least displaced sufficiently to have sustained an
injury of the collateral ligaments (7).
involved and the elbow is considered unstable unless proven otherwise.
If posterior displacement occurs with less than 40 to 45 degrees of
flexion, the residual articulation is considered inadequate and the
ulnohumeral joint must be stabilized. If the fracture fragment is large
enough for fixation, osteosynthesis through the anterior capsule is
performed. If the fragment is too small for fixation, then a heavy
number 5 suture is placed over the fragment (or fragments), which is
brought to its anatomic location and tied through drill holes placed in
the ulna. A threaded 0.045 or 0.062 Steinmann pin can be placed through
the ulna into the fragment to buttress it as well. In the latter
situation, or even if osteosynthesis has been carried out but there is
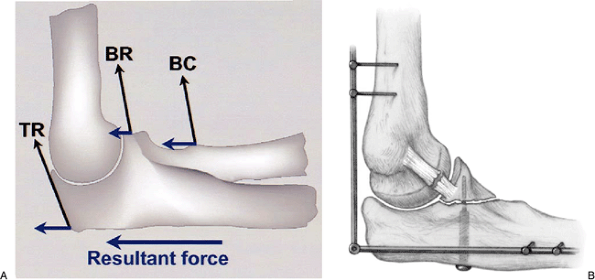
concern about stability and the rigidity of fixation, the system is
neutralized by the application of a hinged external fixator. The
external fixator eliminates or neutralizes the posteriorly directed
forces that are applied to the fracture site by the muscles that flex
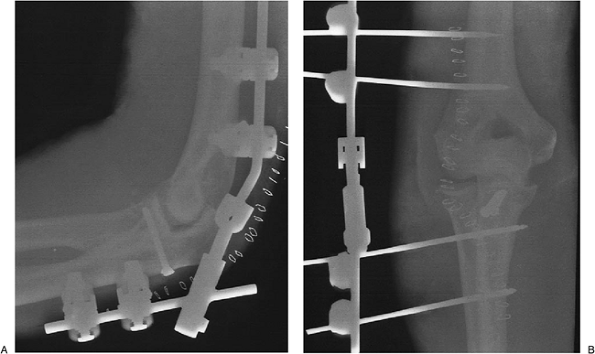
and extend the elbow joint (Fig. 7-4). The
device allows motion of the ulnohumeral joint while placing a distal
distraction force on the ulna, thus protecting the articulation. The
distraction device
is maintained for 3 to 6 weeks, depending upon the nature of the injury (1) (see Chapter 8).
 |
|
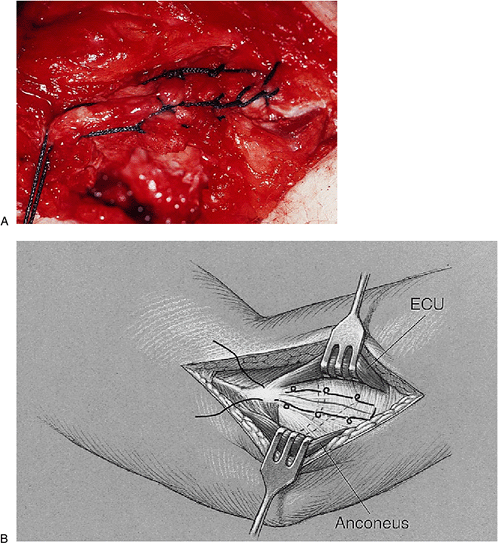
Figure 7-3.
A sagittal fracture occurs from varus axial load with or without comminution and usually involves attachment of the anterior medial collateral ligament. |
 |
|
Figure 7-4.
Complex instability of the elbow. Posterior directed forces occur from the posteriorly directed pull of the biceps, brachialis, and triceps (A). If fixation is inadequate, neutralization of coronoid fixation is carried out with an external fixator (B). |
since, by definition, the ulnohumeral joint is grossly unstable. If the
coronoid is a large fragment and has not been comminuted, it may be
fixed with a screw or plate, and screws and the joint will be stable.
-
Type II fractures with an intact radial head and in which the elbow is grossly unstable when flexed less than 50 or 60 degrees.
-
Type II coronoid fractures in which the
radial head has been fractured and the elbow has been dislocated
(“terrible triad” injury). -
All type III fractures.
-
Isolated anteromedial coronoid fractures, because of their propensity for slight articular incongruity and subluxation.
exposure of the coronoid if greater than 5 to 6 days after injury, but
only if the ulnohumeral joint is reduced. A persistently unstable joint
with articular incongruity is less successfully treated later than is
an elbow with heterotopic ossification.
coronoid is involved, a line from the tip of the olecranon through the
base of the fracture is parallel to or intersects the line of axis of
the ulna posterior to the olecranon. If greater than 50% has been
fractured, this line intersects the long axis distally.
The posterior skin incision affords medial or lateral deep exposure. If
a radial head fracture requires removal, a deep lateral approach may be
adequate. If the radial head is intact or the ulnar nerve is
symptomatic, the deep medial approach is used. Usually, the lateral
collateral ligament (LCL) is disrupted, so this is carefully repaired
along with the coronoid fixation.
posterior incision to allow medial exposure of the fracture as well as
lateral exposure of the lateral collateral ligament should this be
necessary. A 12-cm posterior incision is made just medial to the tip of
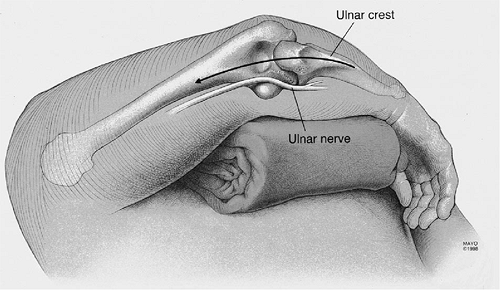
the olecranon (Fig. 7-5). A subcutaneous flap
is elevated medially, exposing the ulnar nerve posterior to the
intermuscular septum. The intermuscular septum is identified and
preserved or released from the medial epicondyle if ulnar nerve
transposition is anticipated (Fig. 7-6). The soft
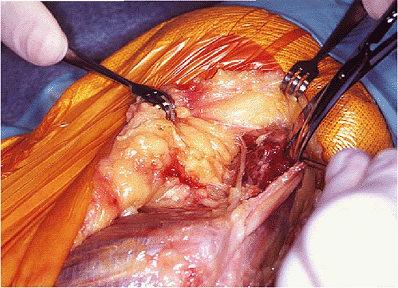
tissues are elevated from the anterior aspect of the septum and a
periosteal elevator elevates the brachialis from the anterior cortex of
the distal humerus. The pronator is elevated, leaving a portion of the
flexor carpi ulnaris (FCU) as a cuff for reattachment at closure. Take
care to preserve the medial collateral ligament. The muscle flap is
elevated from the capsule (Fig. 7-7).
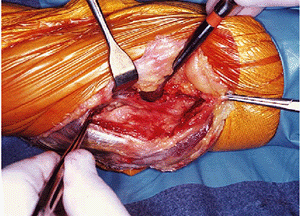
The fibers of the brachialis are swept from the anterior capsule, which
is divided for exposure of the joint surface with a longitudinal
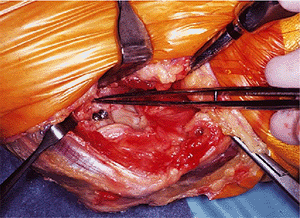
incision. The fracture is identified (Fig. 7-8)and reduced with a sharp tenaculum. A 0.045 or 0.062 K-wire stabilizes the fracture (Fig. 7-9). For some fractures (type II) fixation with a 2.7-mm screw is adequate (Figs. 7-10 and 7-11).
With type II or type III comminuted fractures not amenable to screw or
suture fixation, a carefully contoured plate may be used to buttress
the fixation construct. Exercise caution putting screws through the
fragments, as they may fragment.
 |
|
Figure 7-5. A posterior incision is preferred to expose the coronoid from the medial column.
|
 |
|
Figure 7-6. The intramuscular septum is identified. In this instance the ulnar nerve is identified and protected.
|
 |
|
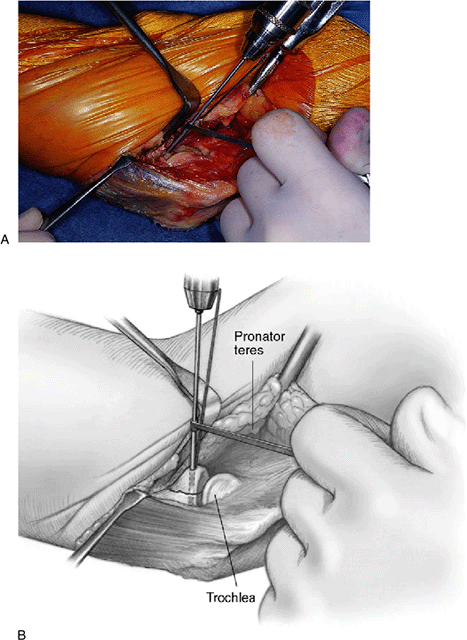
Figure 7-7. The brachialis and pronator teres muscles have been elevated from the anterior capsule.
|
 |
|
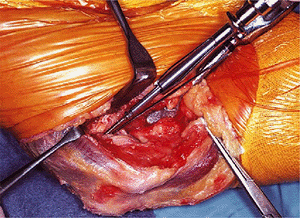
Figure 7-8. A,B: The anterior capsule is exposed and entered revealing a type II coronoid fracture.
|
or two no. 2 or no. 5 suture is passed over the fragment or through
drill holes if possible and through the capsule that is attached to it.
If possible, a Krachow suture is placed in the brachialis tendon at its
insertion (Fig. 7-12).
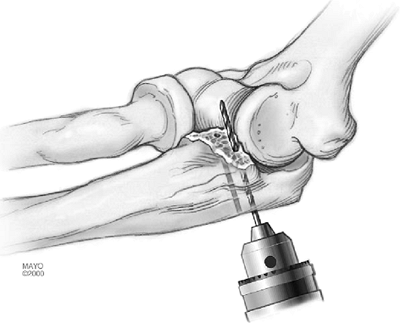
Two or three drill holes are placed retrograde from the subcutaneous
border of the ulna into the base of the fracture and close to the
articular surface (Fig. 7-13).
Care is taken to ensure that the fragments are pulled into place in a
fashion that places the bone fragment(s) close to the joint surface.
The sutures are then passed through the holes with a suture passer. The
fragment is reduced and the sutures are tied (Fig. 7-14).
 |
|
Figure 7-9. A,B:
The fracture is stabilized with a K-wire, and a 2.0 drill bit is used to drill coronoid fragment. The fragment is often too small to allow overdrilling. |
 |
|
Figure 7-10. The fracture is secured with a 2.7-mm screw.
|
 |
|
Figure 7-11. If a large enough fragment exists, two screws are preferable.
|
 |
|
Figure 7-12. Suture technique. Here a Krachow stitch is used to secure the brachialis muscle, capsule, and fractured fragments.
|
 |
|
Figure 7-13. The drill is directed retrograde from the dorsal aspect of the ulna into the bed of the fractured coronoid.
|
fractures of the coronoid are closed by repair of the disrupted
ligaments. Application of a hinged external fixator may be indicated as
well as needed (see Chapter 8).
the lateral collateral ligament and may involve an medial collateral
ligament (MCL) injury as well. Most have associated radial head
fractures. The combination of elbow dislocation and fractures of the
coronoid and radial head has been termed the terrible triad. With this injury we proceed with treatment of the coronoid, radial head and a careful ligamentous repair as described in Chapter 5.
 |
|
Figure 7-14. The suture is tied with the elbow in 90-degree flexion.
|
 |
|
Figure 7-15. A,B:
A disrupted lateral ulnar collateral ligament is stabilized with a running locked stitch (Krachow) that is secured to the humerus through drill holes. |
lateral collateral ligament complex. A heavy nonabsorbable suture is
passed through a drill hole exiting at the anatomic origin of the LUCL
at the humerus (Fig. 7-15). Using a Krachow
stitch, the suture passes along the length of the ligament, including
the ulnar insertion of the ligament at the tubercle of the supinator
crest. The stitch proceeds proximally and again passes through the
humeral origin and is tied with the elbow reduced, the forearm is in
neutral rotation, and the elbow is flexed 45 to 90 degrees. Medially,
the same technique is used if the medial collateral ligament has been
torn.
instructed in passive range-of-motion exercises with gravitational
varus stress eliminated (i.e., in vertical plane, which can also be
performed overhead while lying supine). The senior author prefers a
continuous passive motion (CPM) for this injury. Repeat radiographs are
taken after 7 to 10 days and at 6 weeks to ensure the maintenance of
reduction. If a contracture of 30 or more degrees is present at 6
weeks, a static adjustable splint program is commenced (see Chapter 9).
If the external fixator is applied, full motion is immediately allowed
and encouraged using a CPM machine for 21 hours a day for 3 to 4 weeks.
Active motion is allowed as tolerated when out of the CPM and while the
fixator is in place. The device is removed at 4 to 6 weeks.
 |
|
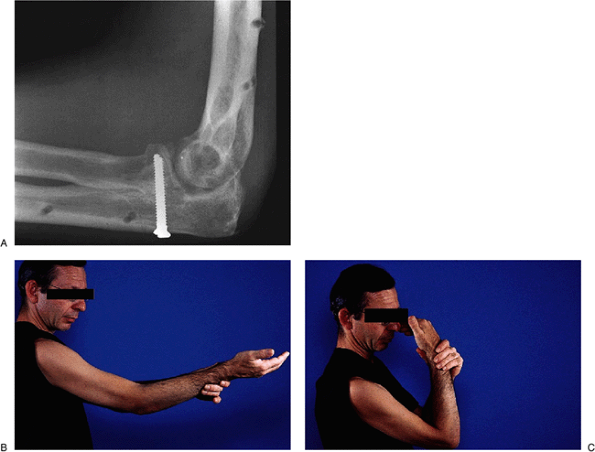
Figure 7-16. This 40-year-old thoracic surgeon sustained a type II coronoid fracture after a fall from a bike.
|
a fracture dislocation of the left elbow. A type III coronoid fracture
was observed (Fig. 7-16). This was reduced and fixed with two 3.0-mm AO screws applied with the lag technique. A DJD II external fixator was applied (Fig. 7-17). At 8 weeks he has an arc of 40 to 130 degrees (Fig. 7-18). He returned to surgery at 10 weeks.
 |
|
Figure 7-17. A,B: The fracture was fixed with two screws and stabilized with the half-pin configuration of the DJD II.
|
 |
|
Figure 7-18. A-C: Excellent function was restored by 10 weeks.
|
