Management of Olecranon Fractures and Nonunion
two imperatives must be met if open reduction and internal fixation are
to be carried out:
-
Fixation must be stable enough to permit mobilization within 5 days.
-
Anatomic or essentially normal surface reduction (within 1 mm) and normal sigmoid notch contour must be achieved.
limited motion and a poorer result. Results of all elbow surgery are
based on pain, motion, strength, and stability.
relate more appropriately to the selection of fixation than to whether
or not to operate. The choice of one of several treatment options for
olecranon fractures is based entirely on fracture type. Various
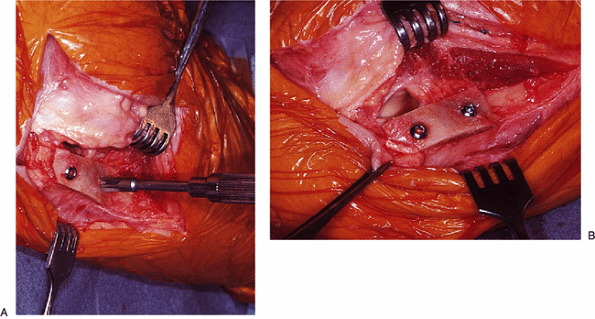
modifications of Colton’s (3) original classification of fracture types have been described. Morrey’s (12) classification based on displacement, comminution, and stability has been more workable in the authors’ hands (Fig. 6-1). Several treatment options are described, depending on the fracture type.
ruptures with attached large or small fragments that are best discussed
in the context of triceps mechanisms insufficiency (Chapter 11).
 |
|
Figure 6-1. The Mayo classification of olecranon fractures. (With permission, Mayo Foundation.)
|
is predicated on variable displacement, comminution, and joint
stability. These considerations are reflected in the Mayo
classification of olecranon fractures (Fig. 6-1).
tested by flexing and extending the elbow can be mobilized after 3 to 5
days of splinting for comfort (Fig. 6-2).
Questionably stable fractures, particularly when comminuted or with
some articular surface separation, even though less than 2 mm, may
require 3 to 4
weeks
of immobilization in midflexion. In such instances, the authors feel
immediate rigid internal fixation to permit mobilization within 5 days
is preferable to accepting the loss of motion usually accompanying
elbow injuries after longer immobilization.
 |
|
Figure 6-2.
Comminuted, undisplaced, and stable olecranon fracture in a 26-year-old man treated satisfactorily in a protective splint for 3 weeks but with range of motion daily after 5 days. |
that are transverse or oblique, involving less than 50% of the proximal
sigmoid notch, should probably be excised in the elderly patient (5,9). All others with sufficient bone stock are treated by an intramedullary screw or Kirschner wire and tension band fixation (9,13,19).
A large intramedullary screw with tension band is equal in energy to
failure to tension band wiring with two Kirschner wires by the AO
technique (18) and has fewer complications in
our hands. The following are examples of the preceding technique and
two alternate methods of fixation that are widely accepted for this
type of fracture:
-
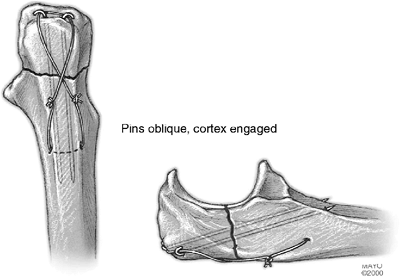
Tension band wiring with two Kirschner wires (9,13) (Fig. 6-3).
-
An obliquely placed cancellous bicortical
screw or an intramedullary screw with or without tension band wiring.
The former is best used with an oblique fracture (Fig. 6-4). -
Noncomminuted stable fractures involving
more than 50% of the sigmoid notch are best treated, in the authors’
hands, with a contoured plate, described later (9,13) (Fig. 6-5). -
Comminuted stable fractures of the
olecranon often involve central fragmentation. All fragments are
salvaged if at all possible and stabilized with an AO 3.5-mm DC,
one-third tubular, or reconstruction contoured plate (6,9,13),
using bone grafts from the iliac crest to fill or buttress defects
along with additional interfragmentary screw fixation. Comminuted
fractures involving less than 50% of the sigmoid notch can be safely
excised if ligamentous integrity is assured and is the treatment of
choice in the elderly patient (1,5,11).
uncommon, often comminuted, and unstable because of injury to the
collateral ligament that inserts at the medial aspect of the coronoid
process (16). Roentgenographic recognition of Regan-Morrey types II and III displaced coronoid fractures (15)
is sometimes difficult; however, the importance of restoring displaced
coronoid fractures both for the anterior buttress effect on the joint
and for the stabilizing effect of the anterior oblique ligament
insertion cannot be overstressed. With unstable elbow injuries,
fragment excision is contraindicated. Bone defects are buttressed with
iliac bone grafts.
Alternatively, the combination of a dorsally applied AO plate and
tension band with K-wires or intramedullary screw may be used.
 |
|
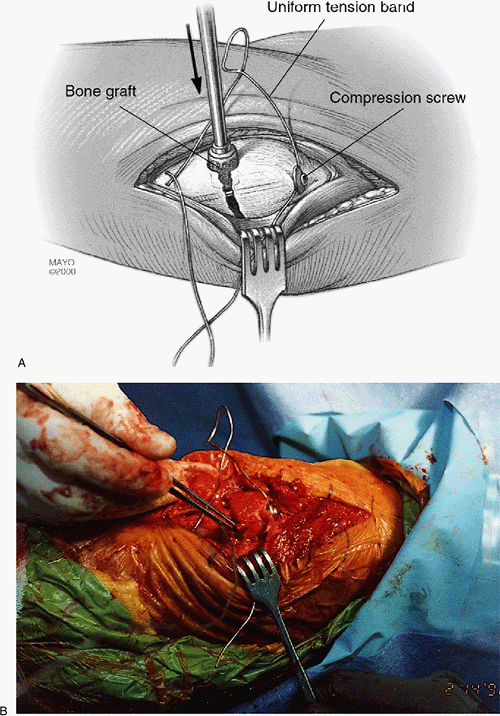
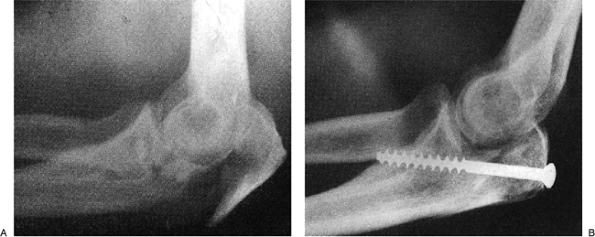
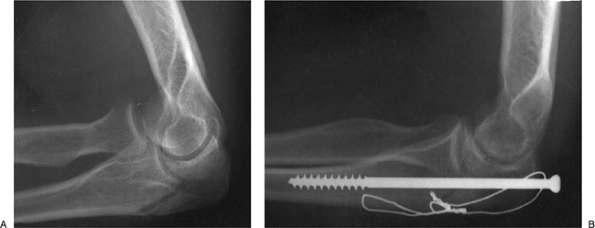
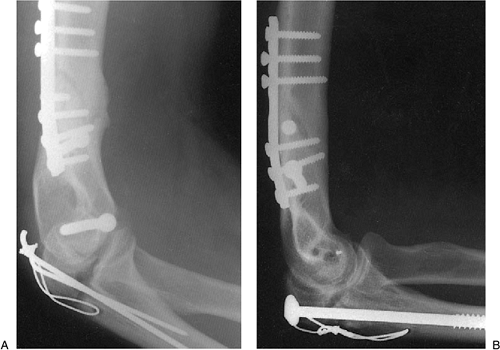
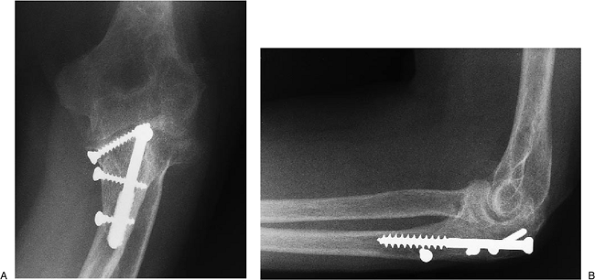
Figure 6-3. Pre- (A) and postoperative (B)
radiographs of a displaced, stable, Morrey type IIA olecranon fracture treated with Kirschner wires and tension band wire by the AO technique and mobilization at 5 days with satisfactory result; healing by 3 months. |
 |
|
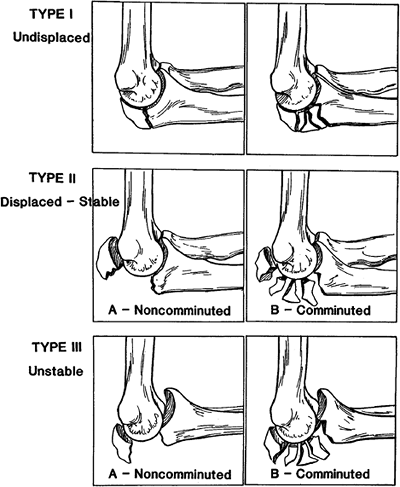
Figure 6-4. Pre- (A) and postoperative (B)
radiographs of a displaced, stable, Morrey type IIA comminuted olecranon fracture treated with bicortical oblique screw fixation with a range of motion result limited by only 5 degrees. (From Wadsworth TG. Adult trauma. In: Wadsworth TG, ed. The elbow. New York: Churchill Livingstone; 1982
.) |
questionable, as with severe comminution, an external fixator or
distraction device should be applied to compensate for the potential
instability and still permit early motion. The reader is referred to Chapter 8
for details of application and use of the distraction device. With
severe comminution and instability in the elderly patient, resection of
bone is likely to be disabling, and consideration may need to be given
to primary total elbow implant arthroplasty.
 |
|
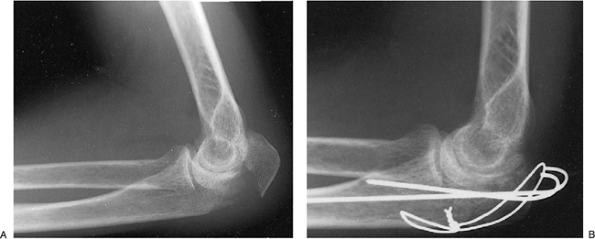
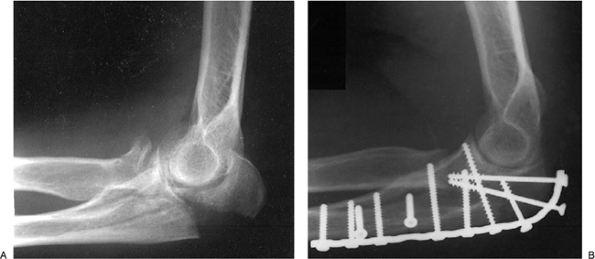
Figure 6-5. Pre- (A) and postoperative (B)
radiographs of a displaced, stable, Morrey type IIA olecranon fracture in a 46-year-old man treated with reconstruction plate and interfragmentary screws with excision of the comminuted radial head. Motion regained was from 10 to 135 degrees with full rotation. |
 |
|
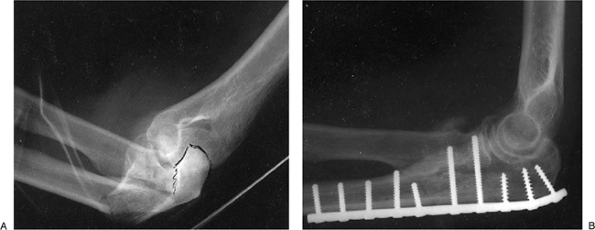
Figure 6-6. Preoperative radiograph (A)
of an open unstable, displaced, and comminuted olecranon fracture (type IIIB) in a 42-year-old woman treated with a plate and recovered 25 to 135 degrees of painless anteroposterior (AP) motion and 90 degrees of pronation with 75 degrees supination (B). |
consideration and is preferable in the elderly or osteopenic patient
with a noncomminuted or comminuted stable fracture involving 50% or
less of the proximal olecranon (1,5,10,11).
In all other instance, internal fixation should be used, with the
choice being determined by the type of fracture as classified earlier.
If instability is present the injury is considered one of complex
instability and managed as described in Chapter 7.
initial dose given at the time of the surgical procedure. A tourniquet
to 100 mm Hg above systolic pressure is checked before, during, and at
the end of the operative procedure. (Tourniquet calibration is checked
with each use.) Exsanguination before tourniquet inflation is by total
elevation of the extremity for 60 seconds, rather than with an Esmarch
bandage, to make visualization of the vascular structures easier.
tourniquet from seepage of prep solution beneath the tourniquet (burns
have been reported). Skin preparation is carried out with betadine
solution after a 5-minute scrub.
side of the involvement with the arm across the chest (authors’ choice)
or prone with the arm over a padded table. The arm can be extended from
either position away from the table for C-arm fluoroscopic use.
than 5 to 7 days of immobilization, treatment is the same as for type
II displaced stable fractures, described later.
less involvement of the sigmoid notch are treated with one of the three
following methods, listed in order of the authors’
preference: intramedullary screw, with wire technique; tension band technique; bicortical screw fixation.
 |
|
Figure 6-7. Approach to the proximal ulna and radial head through a posterior incision.
|
 |
|
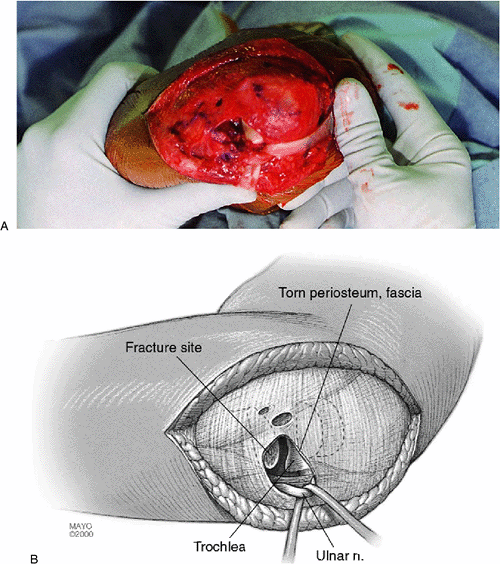
Figure 6-8. A,B: The ulnar nerve is routinely identified but transferred only if necessary. It is protected with a Penrose drain.
|
and extended proximally and distally if necessary, incising the
superficial fascia and elevating the anconeus from the lateral aspect
of the ulna (17). By reflecting the proximal fragment, sufficient visualization is available to perform anatomic reduction of the fragment (Fig. 6-8).
Care is taken to preserve and/or repair the radial ulnar collateral
ligament. Alternatively, if the radial head, anterior capsule, and
coronoid are to be visualized, the Kocher approach is used, developing
the interval between the anconeus and extensor carpi ulnaris as
described in Chapter 1.
with a 1/4-inch Penrose drain (wet and untied) around it, transferring
the nerve subcutaneously if necessary (Fig. 6-8).
proximal olecranon major fragment after identifying that the fracture
line is not already separated, and the soft tissue attached to the
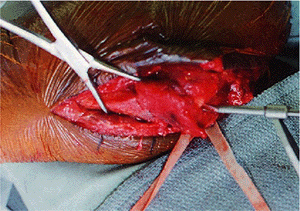
major fragments is disturbed as little as possible (Fig. 6-9). Laterally and medially,
the triceps retinaculum and the periosteum are incised and the
fracture(s) are identified and cleaned of hematoma; the fragments are
temporarily reduced and held in place with a ratcheted towel clip or
K-wire (Fig. 6-10).
Accurate approximation of the fracture surfaces dorsally, laterally,
and at the sigmoid notch level is achieved, and any defect of
buttressing of a central fragment is accomplished with bone graft from
the ilium.
 |
|
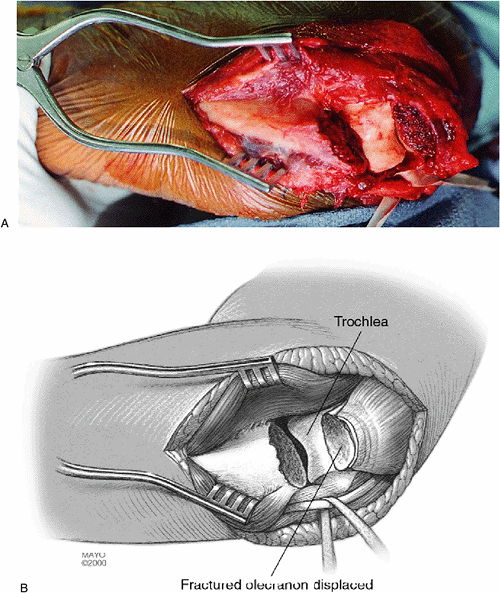
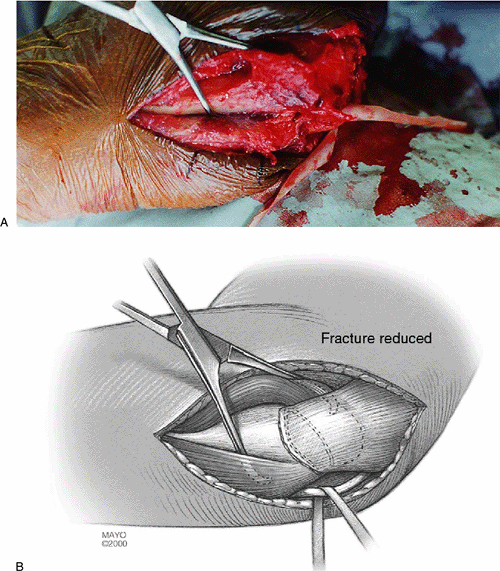
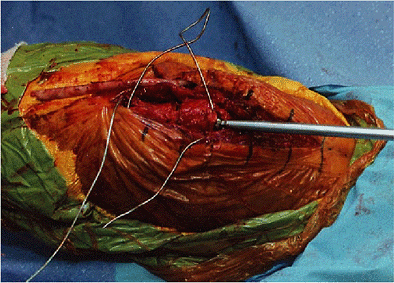
Figure 6-9. A,B: The fractured fragment is retracted by dissecting it free of the periosteum, which has usually been ruptured from the fracture.
|
intramedullary screw, and a drill hole at the level of and in line with
the medullary canal is made in the proximal fragment (Fig. 6-11).
The hole in the proximal fragment is enlarged by a 4.5-mm drill bit,
and a 6.5-mm tap is used in the cortex of the proximal fragment and
taken distally into the medullary canal of the distal segment for a
distance of 7 to 10 cm. Exposure for the tap, and subsequently for
screw placement, is made with a 1- to 2-cm longitudinal incision in the
triceps tendon in the midline over the posterior olecranon (Fig. 6-12). I also use fluoroscopic verification of the position of the fracture and fixation.
the proximal fragment is not proper to ensure anatomic reduction, it
may be enlarged to allow the proximal position of the screw to
accommodate the distal alignment. Further, the ulnar bow that occurs
about 7 cm distal to the fracture precludes the use of screws any
longer than 10 to 12 cm.
 |
|
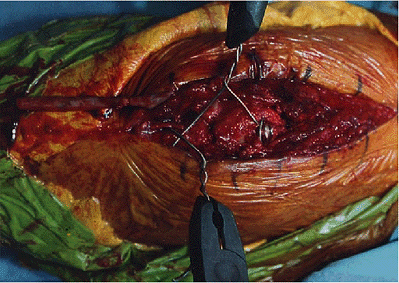
Figure 6-10. A,B: The fracture is reduced and stabilized with a bone holding forceps.
|
 |
|
Figure 6-11.
The proximal drill hole is very carefully made to ensure anatomic alignment of the fracture and correct orientation with the distal shaft fragment. |
 |
|
Figure 6-12. Intramedullary fixation should extend distally for approximately 7 cm; the proximal fragment is prepared with a 6.5-mm tap.
|
(unthreaded proximally and with 32-mm distal threads) is then inserted
over the washer and across the reduced fracture site, but incompletely
tightened (Fig. 6-14). The screw threads must achieve firm cortical fixation in the intramedullary canal. C-arm fluoroscopic verification is made.
made transversely through the distal fragment 3 mm anterior to the
dorsal cortex and 3 to 4 cm distal to the fracture, or more than equal
distance from the proximal tip of the olecranon to the fracture site (Fig. 6-15).
A 15-gauge tension band wire is passed beneath the triceps tendon and
under the washer and screw. This may be facilitated by a large-bore
intracatheter needle (Fig. 6-16), twisted in a
figure-eight fashion dorsally over the periosteal sleeve of the
olecranon, and threaded through the transverse hole in the distal
fragment. It is then twisted in a loop on each side by the AO method.
This will permit more uniform compression as the wire is tightened.
level while observing the sigmoid notch, with care taken to avoid any
collapse of its normal semicircular contour (Fig. 6-17).
 |
|
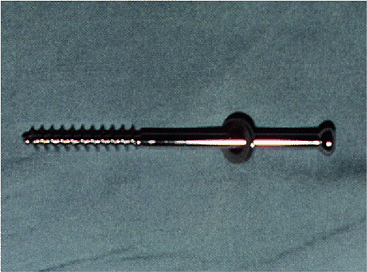
Figure 6-13.
A 6.5-mm cancellous screw 10 to 12 cm in length is introduced down the canal. This should cross the fracture site at least 7 cm. |
 |
|
Figure 6-14. A,B:
Exposure to insert the drill and screw is most readily obtained by a simple triceps splitting incision over the insertion at the posterior olecranon. |
 |
|
Figure 6-15. A transverse drill hole is made about 3 mm anterior to the dorsal cortex 3 or 4 cm distal to the fracture.
|
 |
|
Figure 6-16. A tension band is passed beneath the triceps tendon. This is facilitated by a large-bore needle to serve as a cannula.
|
 |
|
Figure 6-17.
The distance between the coronoid and the tip of the olecranon is directly observed as the screw is being tightened. This distance must not be narrowed. |
 |
|
Figure 6-18. Medial and lateral tightening of the tension band system is performed to apply uniform compression across the fracture site.
|
each side are repaired with 0 Vicryl interrupted sutures; the
subcutaneous tissue is closed with interrupted 2-0 Vicryl, and skin is
closed with 4-0 continuous Vicryl subcuticular suture. After using
Steri-strips for skin approximation, a dry dressing and skin adhesive
are applied and followed by six- to eight-thickness equally and snugly
applied sheet cotton beneath a light cast (two rolls of fiberglass
casting material) with the elbow in full extension.
operating and recovery room, and the patient is sent to the recovery
room with the extremity at 60 degrees of elevation, maintained with
pillows.
are identical to the intramedullary screw and band technique described
earlier.
medially, laterally, and dorsally, and with any central sigmoid notch
impaction reduced and buttressed with autogenous bone from the ileum or
lateral epicondyle, two 2-mm parallel Kirschner wires, to resist torque
and displacement forces, are inserted under C-arm fluoroscopic control
so that they extend from the posterior dorsal aspect of the olecranon,
traverse the fracture site obliquely, and
extend just through the anterior ulnar cortex distal to the coronoid process (Fig. 6-21). The wires are cut and bent toward the ulna.
 |
|
Figure 6-19. The wires are cut and bent to avoid irritation.
|
 |
|
Figure 6-20. A,B: Figure 6-20. Intramedullary screw and tension band technique for a Morrey type IA fracture.
|
the triceps tension and looped around the two bent Kirschner wires by
the AO technique directly over bone and brought out distally in a
figure-eight fashion and threaded transversely through a 2-mm drill
hole through the ulna as described earlier. The tension band
attachments to bone and K-wires are inserted dorsal to the midaxis of
the ulna, and with the elbow flexed serve to further compress the
fracture site. Radiographic verification of the construct and reduction
is made.
 |
|
Figure 6-21.
The tension band technique for which two pins are inserted down the midaxis of the ulna or obliquely to engage the anterior cortex. Radiographic verification is required to be sure the pins have not violated the sigmoid notch. |
orientation of the K-wires penetrating the anterior cortex has largely
eliminated the problem of K-wire back-out, requiring removal. Further,
although somewhat controversial, we are not convinced the cables offer
any advantages over simple 18-gauge wire (8).
or ratcheted towel clip, the 3.2-mm drill bit used as a guide is
removed and the hole is enlarged to 4.5 mm in the proximal fragment. A
6.5-mm tap is inserted through the ulnar cortex distal to the coronoid
and a 6.5-mm AO screw over a washer and of proper length to achieve
bicortical compression is inserted and tightened. Radiographic
verification of fixation and reduction is made. A tension band is
ordinarily unnecessary with oblique bicortical fixation.
displaced, unstable noncomminuted and comminuted fractures (type IIIA,
B) are treated by contoured plate technique if possible. The distractor
is applied if necessary (Chapter 7).
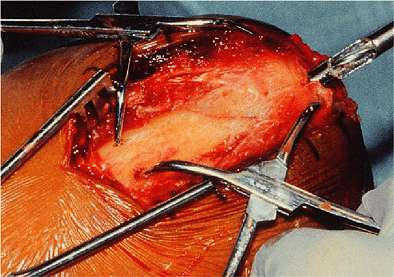
vision, and using C-arm fluoroscopic control, reduction is achieved and
maintained with temporary Kirschner wires and interfragmentary screw
fixation. The fracture reduction is visualized on each of the sigmoid
notch and dorsally.
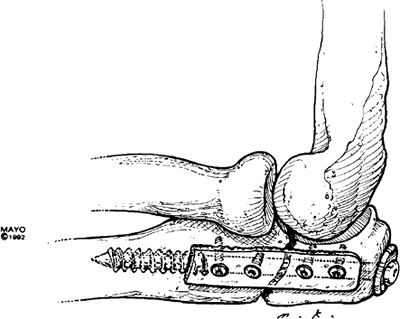
eight-hole AO plate (authors’ choice), a 3.5-mm DC, or a reconstruction
plate is contoured to permit 90-degree insertion of one screw at the
proximal end down the center of the olecranon, with the plate on the
dorsal surface (Fig. 6-22A). Contouring of the
plate is achieved with bending irons and the bending press. The next
two screws, if possible, are inserted in a divergent pattern and
pointing anteriorly within the proximal fragment. Subsequent screws are
placed in a compression mode, and any fracture of the coronoid process
is reduced and fixed with one of the screws. Visualization of the
coronoid can usually be made through the fracture site of the separated
olecranon fragments before reduction. Bicortical screw fixation is used
to ensure direction and length of the screws. The advantage of the LCDC
plate is that the screw heads are flush with the plate and are not
often prominent enough to require later removal. A compression device
is not typically necessary, as the plate is reserved for comminuted
fractures. If an intramedullary 6.5-mm or larger-caliber screw is to be
used with the construct,
the
proximal hole in the 3.5-mm LCDC plate must be enlarged preoperatively
or a 4.5-mm reconstruction plate must be used. The LCDC plate is less
likely to fracture than a tubular or reconstruction plate. Meticulous
care is taken to maintain the normal contour of the sigmoid notch (Fig. 6-23).
 |
|
Figure 6-22.
Contoured eight-hole 3.5-mm LCDC AO plate with three screws in the proximal larger fragment with bicortical screw fixation where possible, distal to the sigmoid notch. |
 |
|
Figure 6-23.
Contoured eight-hole reconstruction plate with bicortical screw fixation. Maintenance of the contour and width of the greater sigmoid notch is essential. |
testing after stabilization of the olecranon fracture, indicates the
need for medial or lateral collateral ligament repair (described in Chapter 14)
and, if medial, is followed by an application of a distractor device
for 4 weeks to prevent subluxation and permit active motion (described
in Chapter 8).
elevation for 2 to 3 days with pillow support and with the hand kept 1
foot above head height 100% of the time, whether recumbent, in a
recliner chair, or standing.
overhead is encouraged for another week. Because edema and swelling are
usually quite minimal at this time, the elbow can be taken through a
range of active assistive motion. Motion is increased by additional
sessions and by greater range each day thereafter.
usually unnecessary, and active assistive motion is carried out through
a full range at least four to six times daily.
even considered contraindicated by the authors. Carrying of weights is
also contraindicated.
motion exercise program with specific strengthening exercises added
when fracture healing is evident or at 12 weeks.
Satisfactory results in undisplaced fractures are obtained in 95% of
cases. In displaced stable noncomminuted and comminuted fractures
satisfactory results occur in 90% of patients. Poorer results in the
unstable displaced and comminuted fractures are to be expected, but the
outcomes are improving with current and improving treatment concepts (Chapter 7).
involving the proximal 50% of the sigmoid notch except in the elderly,
where excision is preferable. In most instances, a contoured plate with
screw fixation will adequately stabilize most comminuted fractures of
the olecranon, and fragment retention is important in the authors’
opinion, since even the proximal olecranon offers significant
architectural stability to the joint.
involving more than 60% of the sigmoid notch, with fractures of the
coronoid process, and with instability. This problem is discussed in
detail in Chapter 7. Problems include motion
loss, nonunion, ulnar neuropathy, malunion, and posttraumatic
arthrosis. Some motion loss occurred in 75% of fractures in a Mayo
Clinic series, with 50% having a loss of 20 to 60 degrees and 20%
having a loss of more than 60 degrees. If rigid fixation is achieved,
motion loss is almost directly proportional to the period of
immobilization and edema or swelling about the joint. With adherence to
a postoperative regimen of immobilization limited to 5 days with the
elbow in full extension and the strict elevation of the elbow above
shoulder height for 2 weeks, motion loss from swelling and edema can be
significantly minimized. Ulnar neuropathy has been reported from 3% to
10% and can be minimized or avoided with careful protection and
handling of the nerve, utilizing subcutaneous transposition if
necessary. Nonunion is most commonly a result of inadequate primary
fixation and has been reported in up to 5% of patients. Loss of blood
supply to the major fragments and excessive soft-tissue stripping often
play an important role in the incidence of nonunion. Malunion is
uncommon following open reduction but may occur with the more severely
comminuted open injuries delaying or excluding adequate reduction.
Posttraumatic arthrosis is more likely to develop in the unstable
comminuted fracture with coronoid and radial head fractures or with
failure of internal fixation requiring reoperation (10). Because of the significant impact of nonunion, we discuss this problem in detail.
earlier, nonunion may occur with a reported incidence of up to 5%.
There are two types of olecranon nonunions with significant difference
in management: undisplaced and displaced. The treatment of nonunion
follows principles of primary fracture treatment and therefore depends
entirely on the type as classified earlier. Although the blood supply
and vascularity of the cancellous olecranon are felt to be sufficient
without bone grafting when reconstruction for nonunion is carried out,
the authors use routine iliac inlay or onlay grafting.
-
When nonunion occurs in the proximal 50%
of the olecranon, excision is an acceptable alternative and is the
treatment of choice in the elderly or osteoporotic patient. -
If there is no gross deformity the inlay bone plug technique is used.
-
For gross deformity, rigid low-profile
dynamic compression plating (LDCP) plate fixation with or without an
intramedullary screw but always with an onlay corticocancellous “bone
plate” is the preferred strategy (14).
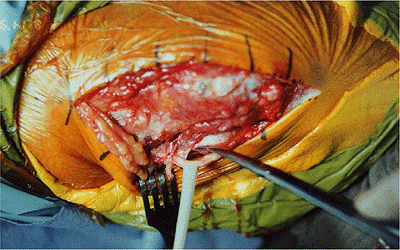
worked well. Incision and exposure are identical to those used for the
acute fracture, with the exception of the patient being positioned in
the prone posture with the arm over a padded armrest to permit use of a
fluoroscopic C-arm. This position is chosen to permit ease of obtaining
a better corticocancellous graft from the posterior rather than the
anterior iliac crest. Care should also be taken to carefully identify
and protect the ulnar nerve (Fig. 6-24). Any previously placed metal is removed and the area of pseudarthrosis is identified through the periosteum.
viable bone with a rongeur, curette, and motorized bur, avoiding the
removal of any vascularized bone (Fig. 25).
corticocancellous plugs of bone (additional in case of loss) are taken
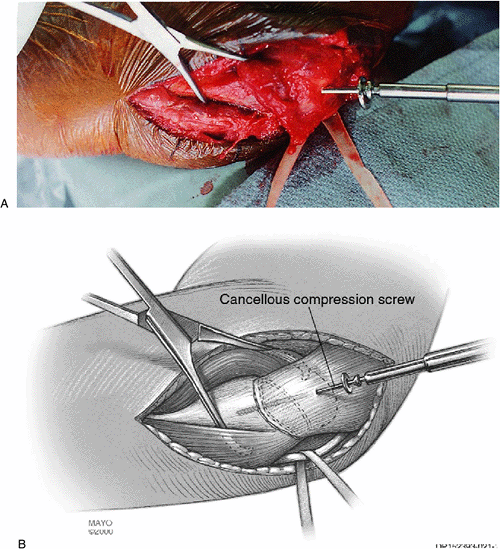
from the posterior iliac crest (Fig. 6-26), and an additional
piece of cancellous bone is cut to fit the pseudarthrosis defect in the olecranon at the site of nonunion.
wire fixation is carried out as described earlier. Particular care is
taken to avoid any change in the normal contour of the sigmoid notch as
compression is accomplished with the compression screw.
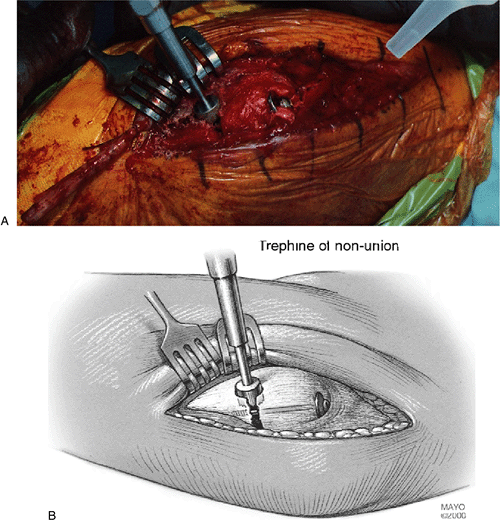
the site of olecranon pseudarthrosis laterally (Fig. 6-27), and the previously harvested plug of iliac graft is tapped into the prepared hole (Fig. 6-28). Additional small fragments of cancellous bone graft may be placed in any irregularity in the pseudarthrosis site.
 |
|
Figure 6-24.
Because exposing nonunions is typically more difficult, particular care should be made to identify the ulnar nerve to avoid injury. |
 |
|
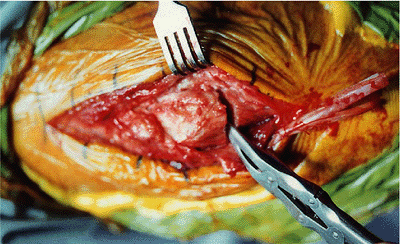
Figure 6-25.
The pseudarthrosis is debrided of fibrous tissue. If reasonable stability is present, the nonunion is not completely taken down. If it is grossly unstable, then both surfaces must be refashioned. |
 |
|
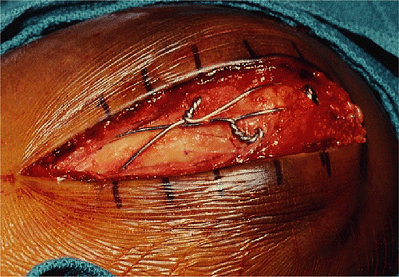
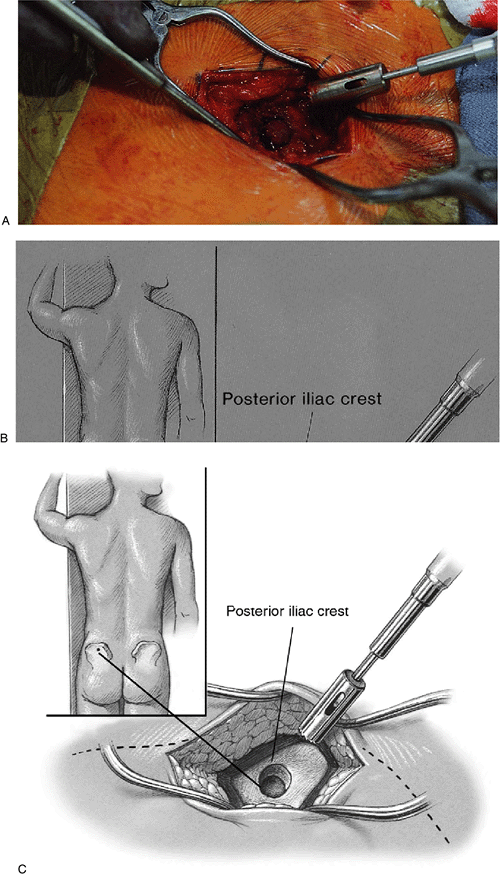
Figure 6-26. A,B:
A trephine (Cloward) is used to remove bone plugs from the posterior iliac crest. This can be done with a percutaneous technique. C: Several plugs may be removed. |
 |
|
Figure 6-27. A,B:
A circular trephine (Cloward) then is used to remove a plug of bone at the site of the pseudarthrosis allowing an effective bone graft site in the presence of an intramedullary fixation device. |
ulnohumeral articulation is required for joint function, then mobilize,
reduce, and fix.
-
The ulnar nerve is identified and protected in all instances.
-
The fracture is mobilized and reduced in such a way as to restore ulnohumeral function according to the principles described in Chapter 7.
-
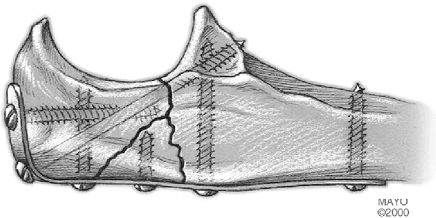
For bone grafting, one of us (BFM) always
employs structural differential cortical cancellous “bone plate”
harvested from the posterior iliac crest (Fig. 6-29). This may be applied
P.121P.122
to the medial or lateral face of the ulna. The plate is secured with
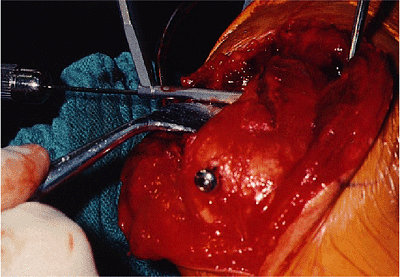
bone screws and the heads are countersunk to avoid irritation (Fig. 6-30).![]() Figure 6-28. A,B: The bone plugs are impacted into the circular defect created at the site of the pseudarthrosis.
Figure 6-28. A,B: The bone plugs are impacted into the circular defect created at the site of the pseudarthrosis.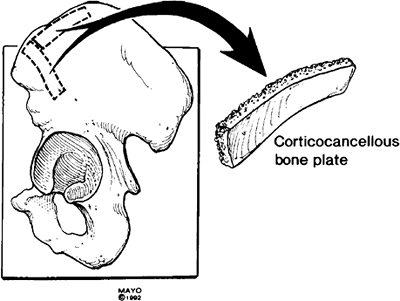 Figure 6-29. In all instances of displaced nonunion a 4- to 5-cm з 1.5-cm graft is harvested from the posterior iliac crest.
Figure 6-29. In all instances of displaced nonunion a 4- to 5-cm з 1.5-cm graft is harvested from the posterior iliac crest.![]() Figure 6-30. The plate of bone is secured with bone screws with the heads countersunk (A). At least one screw is placed on either side of the nonunion (B).
Figure 6-30. The plate of bone is secured with bone screws with the heads countersunk (A). At least one screw is placed on either side of the nonunion (B). -
Fixation.
-
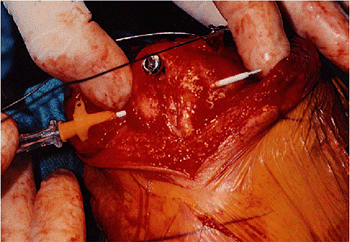
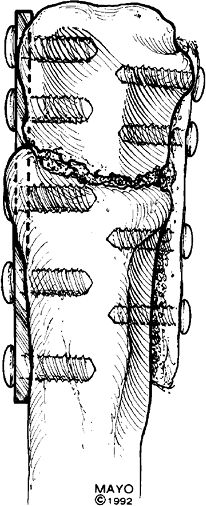
Compression. If adequate stock is present, we prefer axillary fixation with a threaded AO cancellous screw (Fig. 6-31).
-
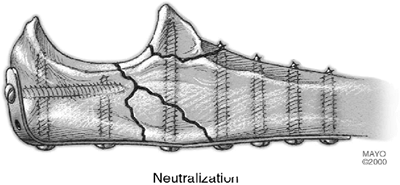
Neutralization. If the fracture does not
allow compression, an LDCP plate is applied either medially or
laterally, depending on the position of greatest rigidity. In all
instances, the essential component is the harvest and application of a
cortical/cancellous onlay “plate” 4.5 cm з 1.5 cm attached by screws to
the opposite ulnar cortex (Fig. 6-32) (14).
-
 |
|
Figure 6-31.
With adequate bone surface present, intramedullary fixation is effective treatment for olecranon nonunion supplemented by a cortical cancellous “bone plate” applied by screw fixation. |
 |
|
Figure 6-32.
With osseous deficiency, neutralization plate fixation is applied with the cortical cancellous “bone plate” applied to the opposite cortex. |
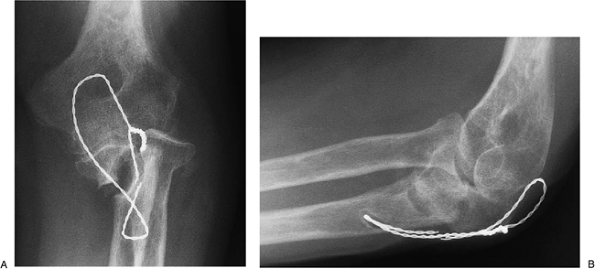
screw technique was successful in obtaining union (Fig. 6-33B) and a functional arc from 35 to 120 degrees.
 |
|
Figure 6-33. Pre- (A) and postoperative (B)
views of an olecranon nonunion at 9 months following a surgical osteotomy to repair a lower humeral fracture, and treated by bilateral iliac corticocancellous plug bone grafts with excision of the pseudarthrosis, cancellous grafting of the defect, and fixation with a 6.5-mm intramedullary bone screw and tension band wiring. Union was painless and solid at 9 months with 35 to 120 degrees of motion. |
 |
|
Figure 6-34. A,B: Established nonunion of olecranon with instability of the articulation.
|
 |
|
Figure 6-35. A,B: Excellent result with axial stability from AO cancellous screw and “bone plate” applied with three screws.
|
Displaced olecranon nonunion 2 years after injury in a 45-year-old
female. Mobilization of the fragment and rigid fixation with an
intramedullary screw and a “bone plate” graft resulted in healing at 6
months with an arc of 35 to 130 degrees flexion and minimal pain (Fig. 6-35).
S, Fay GD, MacAusland WR Jr. Treatment of olecranon fractures:
indications for excision of the olecranon fragment and repair of the
triceps tendon. J Trauma 1962;2:597.