The Elbow
collateral ligaments. The key neurovascular structures running down the
arm pass anterior and posterior to the joint. The medial and lateral
approaches, therefore, avoid the obvious neurovascular dangers, but
provide limited access to the elbow because of its bony configuration.
Anterior and posterior approaches provide better access to the joint,
but may endanger the key neurovascular structures.
provides the best possible exposure to all surfaces of the elbow and is
the approach used most often for the internal fixation of complex
fractures of this joint. The medial approach
provides good access to the medial side of the joint, but requires an
osteotomy of the medial epicondyle for best exposure. This osteotomy
does not involve any part of the articular surface, however. Although
the approach is extensile to the distal humerus, it is most useful in
dealing with local pathologies of the medial side of the joint. The
anterolateral approach exposes the lateral side of the joint; in
addition, it can be extended both proximally and distally to expose
both the humerus and the radius from the shoulder to the wrist. The anterior approach
to the cubital fossa is designed primarily for exploration of the
critical neurovascular structures that pass in front of the elbow
joint. The posterolateral approach to the radial head is designed exclusively for surgery on that structure.
single section of this chapter after the various surgical approaches
are described, mainly because the keys to the surgical anatomy are the
neurovascular bundles that pass across the elbow joint; their positions
are important in all the approaches. Separate subsections outline the
anatomy that applies to each particular approach.
Although it is basically a safe and reliable operative technique, it
does have one major drawback: it usually requires an osteotomy of the
olecranon on its articular surface, creating another “fracture” that
must be internally fixed. The uses of the posterior approach include
the following:
-
Open reduction and internal fixation of fractures of the distal humerus3,4
-
Removal of loose bodies within the elbow joint
-
Treatment of nonunions of the distal humerus
using some portions of this approach to lengthen the triceps muscle,
without performing an olecranon osteotomy.
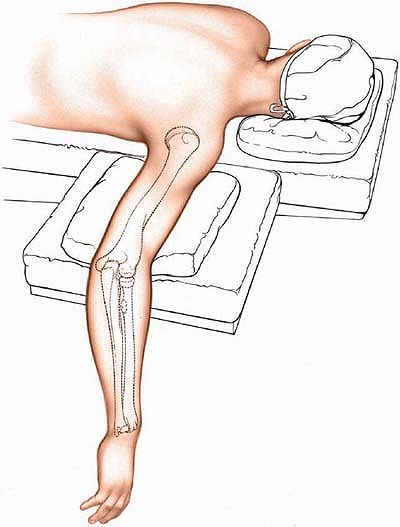
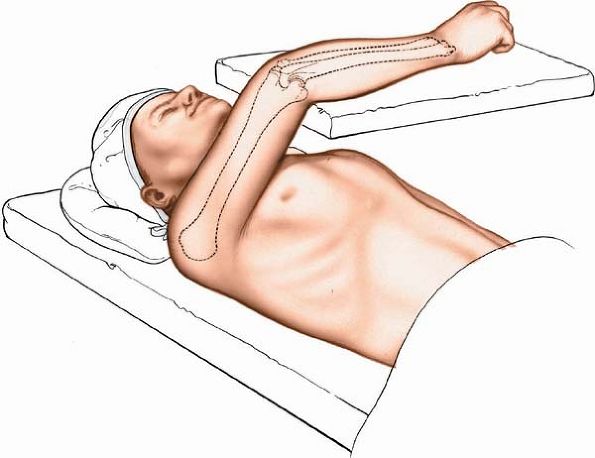
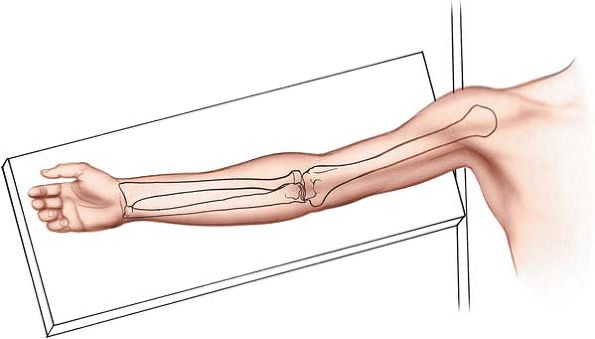
table, ensuring adequate padding for the chest and pelvis to allow free
movement of the abdomen during respiration. Exsanguinate the limb by
elevating it for 3 to 5 minutes and then apply a tourniquet as high up
on the arm as possible. Abduct the arm about 90° and place a small
sandbag underneath the tourniquet, elevating the upper arm from the
operating table. Allow
the elbow to flex and the forearm to hang over the side of the table (Fig. 3-1).
 |
|
Figure 3-1 Position of the patient on the operating table.
|
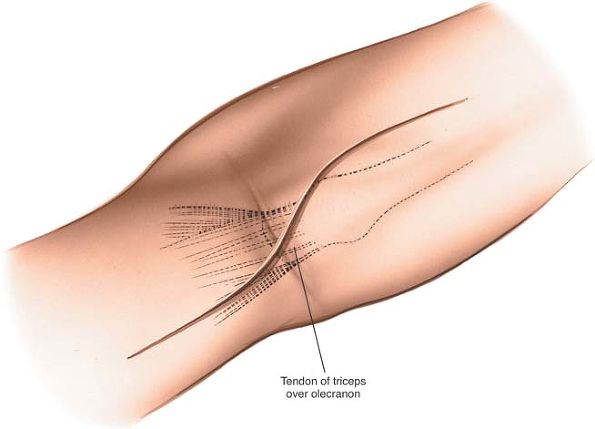
the elbow. Begin 5 cm above the olecranon in the midline of the
posterior aspect of the arm. Just above the tip of the olecranon, curve
the incision laterally so that it runs down the lateral side of the
process. To complete the incision, curve it medially again so that it
overlies the middle of the subcutaneous surface of the ulna. Running
the incision around the tip of the olecranon moves the suture line away
from devices that are used to fix the olecranon osteotomy and away from
the weight-bearing tip of the elbow (Fig. 3-2).
 |
|
Figure 3-2 Incision for the posterior approach to the elbow.
|
approach involves little more than detaching the extensor mechanism of
the elbow. The nerve supply of the triceps muscle (the radial nerve)
enters the muscle well proximal to the dissection.
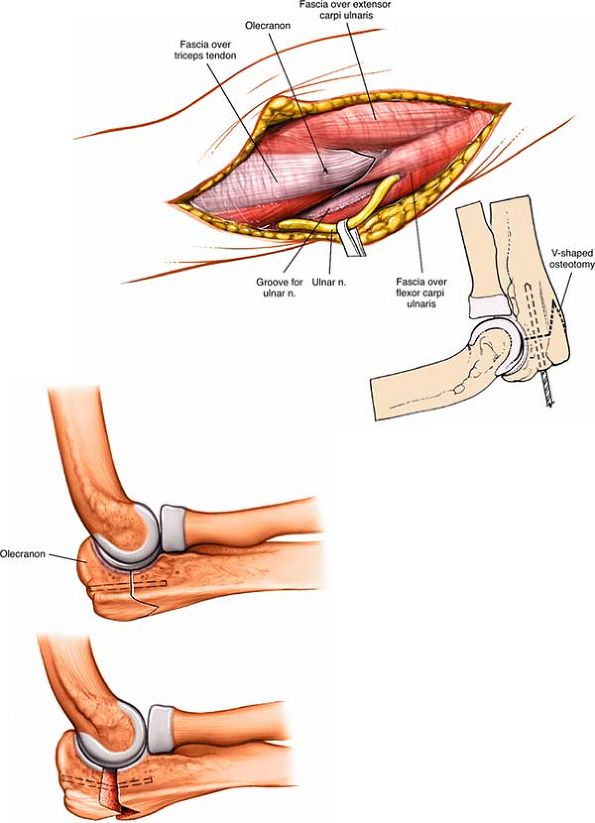
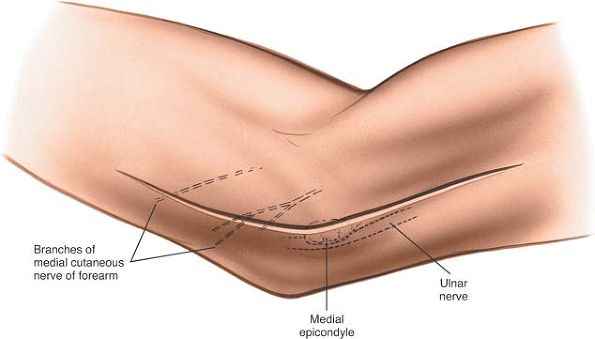
nerve as it lies in the bony groove on the back of the medial
epicondyle and incise the fascia overlying the nerve to expose it.
Fully dissect out the ulnar nerve and pass tapes around it so that it
can be identified at all times (Fig. 3-3). Do not use these tapes for retraction as this can create a traction lesion to the nerve.
the osteotomy is performed. Score the bone longitudinally with an
osteotome so that the pieces can be aligned correctly when the
osteotomy is repaired (see Fig. 3-3, inset).
 |
|
Figure 3-3
Dissect the ulnar nerve from its bed and hold it free with tape. Predrill the olecranon before performing an osteotomy for easy reattachment. A V-shaped osteotomy is inherently more stable than a transverse osteotomy. |
from its tip using an oscillating saw. The apex of the V is directed
distally. A V-shaped osteotomy gives greater stability than a
transverse osteotomy after fixation. Divide the bone until it is cut
through almost entirely. Snap the remaining cortex by wedging the two
cut surfaces apart with an osteotome. This will cause an irregularity
in the osteotomy, allowing it to key together better during
reconstruction (see Fig. 3-3, inset).
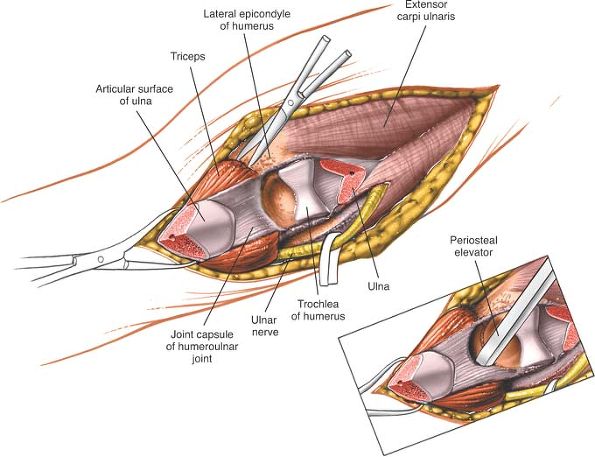
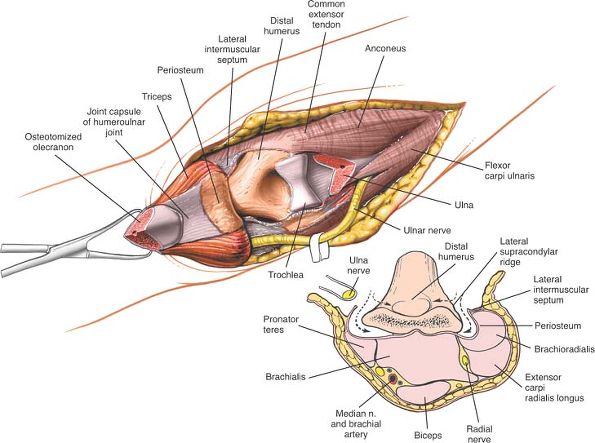
lateral sides of the portion of the olecranon that has been subjected
to osteotomy and retract it proximally, elevating the triceps from the
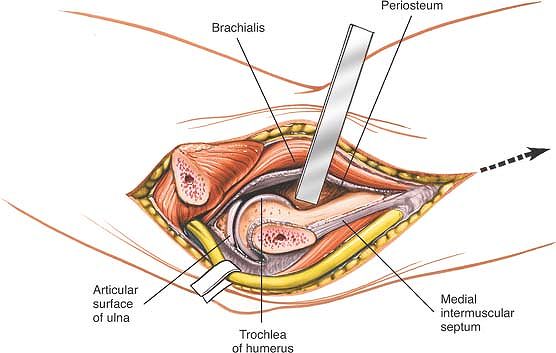
back of the humerus (Fig. 3-4). The posterior
aspect of the distal end of the humerus is directly underneath;
subperiosteal dissection around the medial and lateral borders of the
bone allows exposure of all surfaces of the distal fourth of the
humerus (Fig. 3-5). Note that full exposure
seldom will be needed. All the soft-tissue attachments to bone that can
be preserved should be, particularly in reductions of fractures.
Stripping excessive soft-tissue attachments off the bone leaves the
bone fragments without a vascular supply and jeopardizes healing.
 |
|
Figure 3-4
Perform a V-shaped osteotomy of the olecranon and retract it proximally, with the triceps muscle attached. Strip a portion of the joint capsule with an osteotome. |
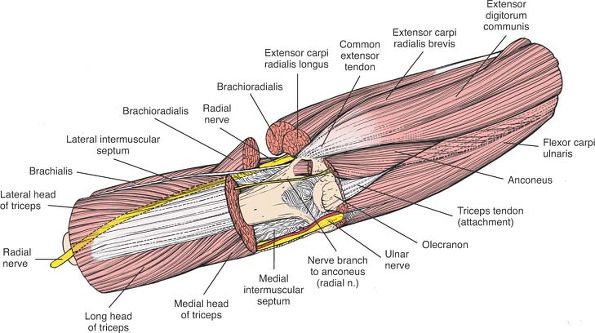
the distal fourth of the humerus, because the radial nerve, which
passes from the posterior to the anterior compartment of the arm
through the lateral intermuscular septum, may be damaged. Flex the
elbow to relax the anterior structures if they need to be elevated off
the front of the humerus (see Figs. 2-36 and 2-37).
field during all stages of the dissection. Some surgeons advise routine
anterior transposition of the nerve during closure, especially if
implant removal is anticipated in the future.
 |
|
Figure 3-5 Dissect around the medial and lateral borders of the bone to expose all the surfaces of the distal fourth of the humerus.
|
anterior to the distal humerus. It may be endangered if the anterior
structures are not stripped off the distal humerus. In cases of
fracture, this dissection has usually been done for you. In the
treatment of nonunions or when the approach is used for osteotomies, a
strictly subperiosteal plane must be used to avoid damage to the nerve
(see Fig. 3-5, inset).
if the dissection ventures farther proximally than the distal third of
the humerus, one handbreadth above the lateral epicondyle (see Fig. 2-36).
correctly during closure. Alignment after fractures is easy, because
the uneven ends of the bone usually fit snugly, like a jigsaw puzzle.
Osteotomies may result in flat surfaces, however, and can make accurate
reattachment difficult (see Fig. 3-3).
posterior approach cannot be extended more proximally than the distal
third of the humerus because of the danger to the radial nerve (see Fig. 2-36).
It also can be enlarged to expose the anterior surface of the distal
fourth of the humerus. The ulnar nerve (which runs across the operative
field), median nerve, and brachial artery may be at risk in this
exposure. The uses of the medial approach include the following:
-
Removal of loose bodies (now more commonly removed arthroscopically)
-
Open reduction and internal fixation of fractures of the coronoid process of the ulna (rarely indicated)
-
Open reduction and internal fixation of fractures of the medial humeral condyle and epicondyle
side of the joint and should not be used for routine exploration of the
elbow. The joint may be dislocated during the procedure, however, to
gain access to the lateral side of the elbow, if necessary.
 |
|
Figure 3-6 Position of the patient on the operating table.
|
the arm supported on an arm board or table. Abduct the arm and rotate
the shoulder fully externally so that the medial epicondyle of the
humerus faces anteriorly. Flex the elbow 90° (Fig. 3-6).
Alternatively, flex the patient’s shoulder and elbow such that the
forearm comes to lie over the front of the face. This allows easier
exposure of the medial side of the elbow, but requires an assistant to
hold the forearm to provide adequate exposure.
minutes or by applying a soft rubber bandage (or exsanguinator). Then,
inflate a tourniquet.
 |
|
Figure 3-7 Incision for the medial approach to the elbow, centered on the medial epicondyle.
|
 |
|
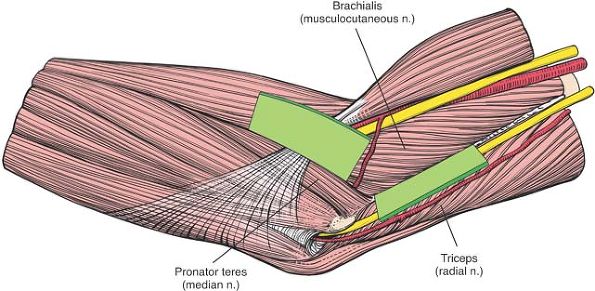
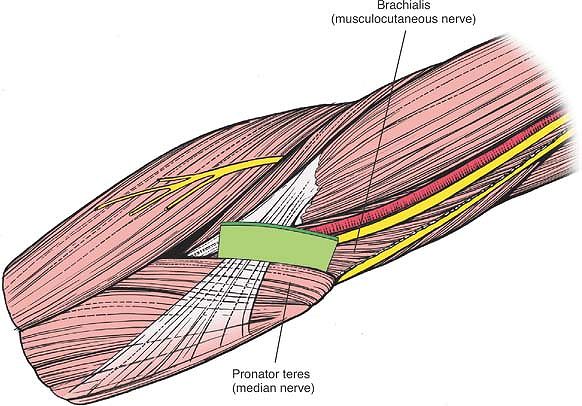
Figure 3-8
Internervous plane. Proximally, the plane is between the brachialis (musculocutaneous nerve) and the triceps (radial nerve); distally, it is between the brachialis and the pronator teres (median nerve). |
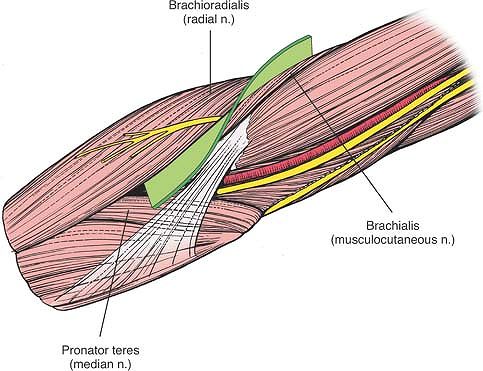
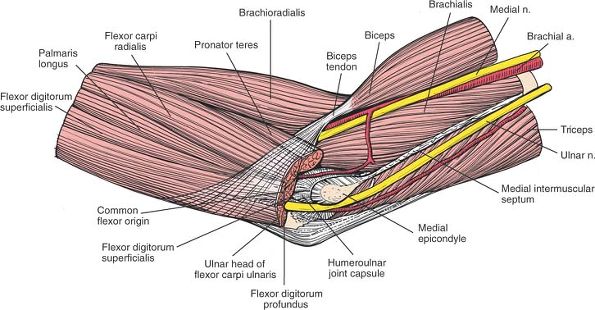
plane lies between the brachialis muscle (which is supplied by the
musculocutaneous nerve) and the triceps muscle (which is supplied by
the radial nerve) (Fig. 3-8).
between the brachialis muscle (which is supplied by the
musculocutaneous nerve) and the pronator teres muscle (which is
supplied by the median nerve; see Fig. 3-8).
 |
|
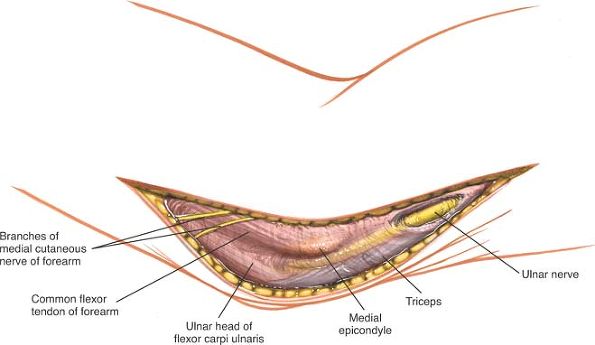
Figure 3-9 Superficial surgical dissection. Isolate the ulnar nerve along the length of the incision.
|
the medial condyle of the humerus. Incise the fascia over the nerve,
starting proximal to the medial epicondyle; then, isolate the nerve
along the length of the incision (Fig. 3-9).
overlying the pronator teres. The superficial flexor muscles of the
forearm now are visible as they pass directly from their common origin
on the medial epicondyle of the humerus (Fig. 3-10).
 |
|
Figure 3-10
Retract the skin anteriorly with the fascia to uncover the common origin of the superficial flexor muscles from the medial epicondyle. |
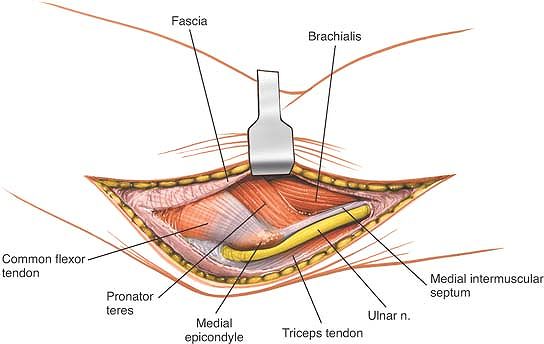
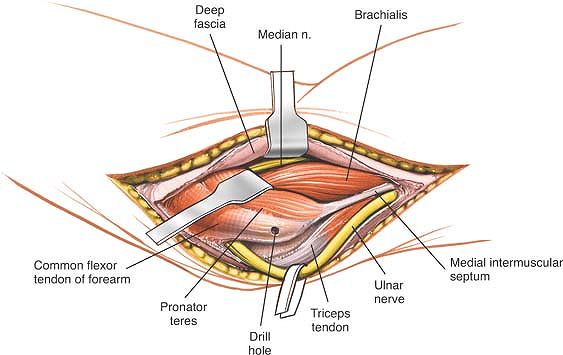
brachialis muscles, taking care not to damage the median nerve, which
enters the pronator teres near the midline. Gently retract the pronator
teres medially, lifting it off the brachialis (Fig. 3-11). Make sure that
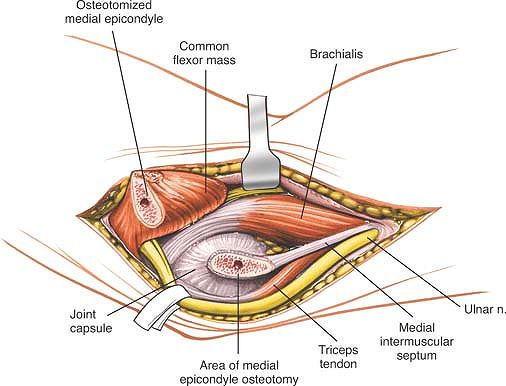
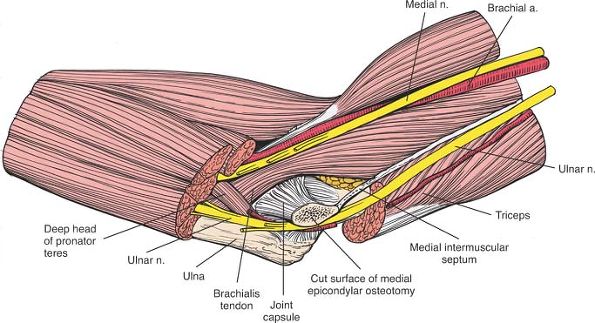
the ulnar nerve is retracted inferiorly; then, perform osteotomy of the
medial epicondyle. Place a periosteal elevator beneath the medial
collateral ligament in order to be certain that when the medial
epicondyle is osteotomized the ligament remains attached to the medial
epicondyle. Reflect the epicondyle with its attached flexors distally,
avoiding traction that might damage the median or anterior interosseous
nerves. Superiorly, continue the dissection between the brachialis,
retracting it anteriorly, and the triceps, retracting it posteriorly (Fig. 3-12).
The medial collateral ligaments must be preserved during osteotomy of
the medial epicondyle. Division of this ligament will result in valgus
instability of the elbow.
 |
|
Figure 3-11 Enter the interval between the pronator teres and the brachialis. Retract the pronator teres medially.
|
 |
|
Figure 3-12
Subject the medial epicondyle to osteotomy and retract it (gently) with its attached flexors. Vigorous retraction of the epicondyle and its attached muscles may stretch the branch of the median nerve to the flexors. |
a traction lesion, with special damage to its multiple branches to the
pronator teres muscle, if the medial epicondyle and its superficial
flexor muscles are retracted too vigorously in a distal direction. Its
major branch, the anterior interosseous nerve, also may suffer a
traction lesion (see Fig. 3-12).
 |
|
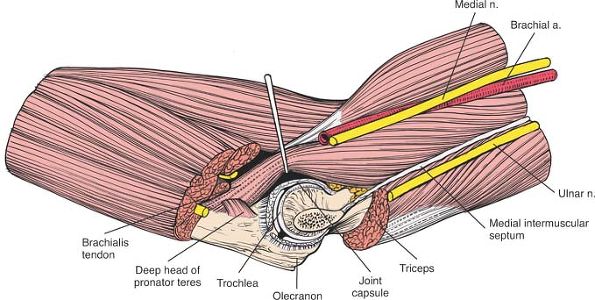
Figure 3-13 Incise the joint capsule and the medial collateral ligament to expose the joint.
|
can be abducted to open its medial side. To dislocate the elbow, the
joint capsule and periosteum should be stripped off the distal humerus,
working from within the joint. By this means, the mobility of the
proximal ulna will be increased significantly. This increased mobility
then will allow dislocation of the joint laterally, thereby opening all
the surfaces of the joint to inspection.
Enlarge the exposure proximally by developing the plane between the
triceps and brachialis muscles. Subperiosteal dissection and elevation
of the brachialis expose the anterior surface of the distal fourth of
the humerus (see Figs. 3-13 and 3-39).
medial epicondyle of the humerus, with its attached flexor muscles, can
be retracted only as far as the branches from the median nerve allow.
Thus, although the exposure provides an adequate view of the brachialis
inserting into the coronoid, it cannot offer a more distal exposure of
the ulna.
the elbow joint, especially the capitulum and the proximal third of the
anterior aspect of the radius. Its uses include the following:
-
Open reduction and internal fixation of fractures of the capitulum
-
Excision of tumors of the proximal radius
-
Treatment of aseptic necrosis of the capitulum
-
Drainage of infection from the elbow joint
-
Treatment of neural compression lesions
of the proximal half of the posterior interosseous nerve and of the
proximal part of the superficial radial nerve—access to the arcade of
Frohse, as well as treatment of radial head fractures with paralysis of
this nerve -
Treatment of biceps avulsion from the radial tuberosity
-
Total elbow replacements
approach to the humerus and a proximal extension of the anterior
approach to the radius. Theoretically, the approach can link the two
together to expose the entire upper extremity from shoulder to wrist.
the arm on an arm board. Exsanguinate the limb either by elevating it
for 3 to 5 minutes or by applying a soft rubber bandage or
exsanguinator. Then, inflate a tourniquet (Fig. 3-14).
 |
|
Figure 3-14 Position of the patient on the operating table.
|
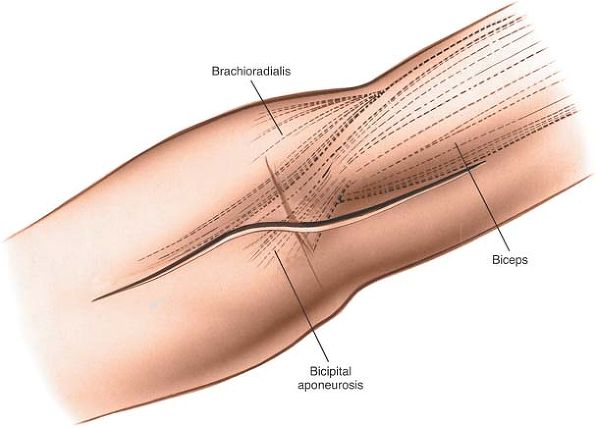
palpable as part of a thick wad of muscle on the anterolateral aspect
of the forearm. This “mobile wad” consists of three muscles; the
brachioradialis forms the medial border of the wad.
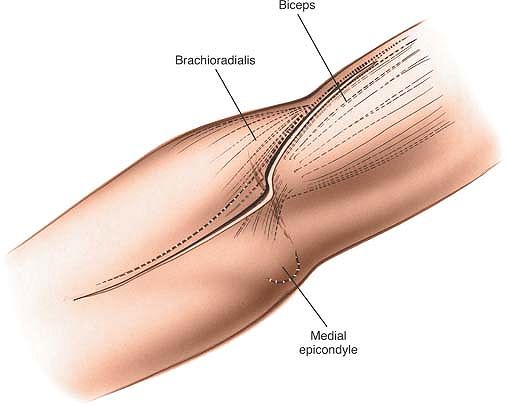
elbow joint. Begin 5 cm above the flexion crease of the elbow, over the
lateral border of the biceps muscle. Follow the lateral border of the
biceps distally, but curve the incision laterally at the level of the
elbow joint to avoid crossing a flexion crease at 90°. Then, continue
the incision inferiorly, curving medially and following the medial
border of the brachioradialis muscle. The lower limit of the extension
depends on the amount of the radius that must be exposed (Fig. 3-15).
 |
|
Figure 3-15
Incision for the anterolateral approach to the elbow. The upper portion of the incision follows the lateral border of the biceps muscle. The lower portion follows the medial border of the brachioradialis muscle. |
(which is supplied by the musculocutaneous nerve) and the
brachioradialis muscle (which is supplied by the radial nerve).
muscle (which is supplied by the radial nerve) and the pronator teres
muscle (which is supplied by the median nerve) (Fig. 3-16).
 |
|
Figure 3-16
Internervous plane. Proximally, the plane is between the brachialis (musculocutaneous nerve) and the brachioradialis (radial nerve); distally, it is between the brachioradialis and the pronator teres (median nerve). |
sensory branch of the musculocutaneous nerve) as it becomes superficial
to the deep fascia in
the
distal 2 in of the arm lateral to the biceps tendon in the interval
between it and the brachialis muscle. Retract it with the medial skin
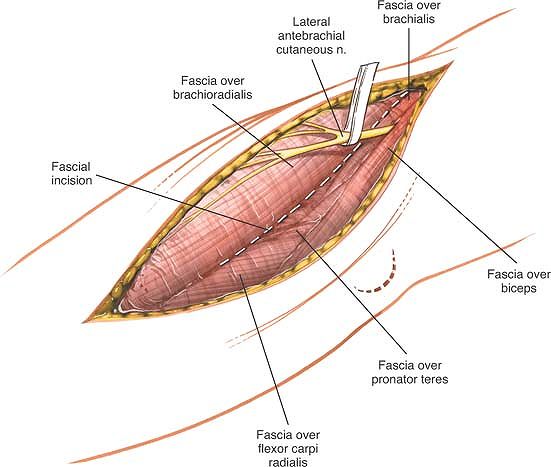
flap (Fig. 3-17).
It is more superficial than the superficial radial nerve, lying outside
the fascial compartment of the brachioradialis; the superficial radial
nerve still lies within the compartment at this level.
 |
|
Figure 3-17
Superficial surgical dissection. Incise the deep fascia along the medial border of the brachioradialis. Be careful to identify the lateral antebrachial cutaneous nerve and retract it. |
 |
|
Figure 3-18
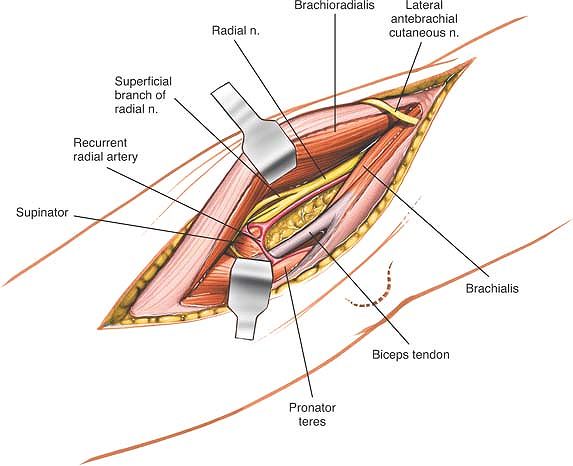
Identify the interval between the brachioradialis and brachialis muscles. Retract the brachioradialis laterally and the brachialis medially, and identify the radial nerve. |
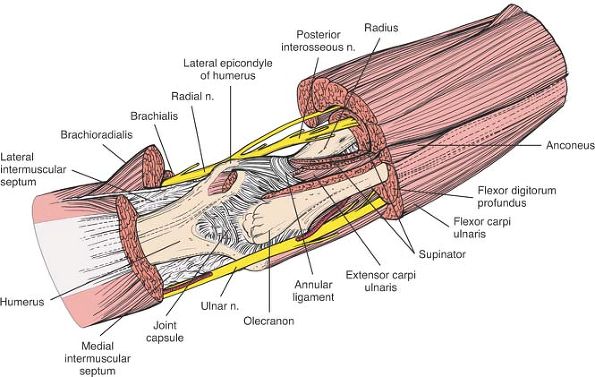
Identify the radial nerve proximally at the level of the elbow joint
between the brachialis and the brachioradialis. It lies deep between
the two muscles and cannot be seen fully until they are separated. The
intermuscular plane is oblique, with the brachioradialis overlying the
brachialis muscle. Develop the plane between the two muscles using your
finger, retracting the brachioradialis laterally and the brachialis and
the overlying biceps brachii medially (Fig. 3-18).
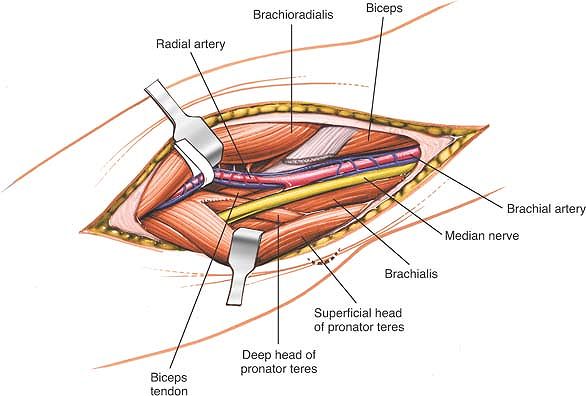
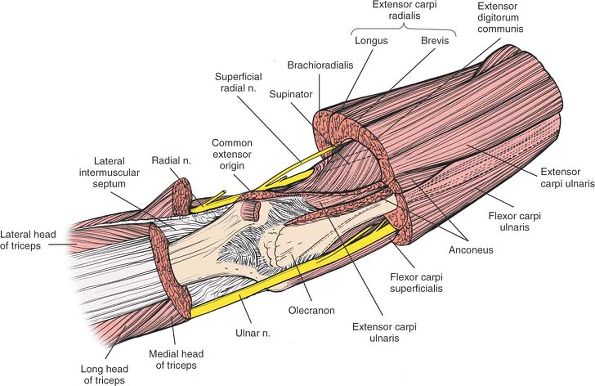
interval until it divides into its three terminal branches: the
posterior interosseous nerve enters the supinator muscle, the sensory
branch passes down the forearm behind the brachioradialis, and the
motor branch to the extensor carpi radialis brevis enters that muscle
almost immediately. Below the division of the nerve, develop a plane
between the brachioradialis on the lateral side and the pronator teres
on the medial side. Ligate the recurrent branches of the radial artery
and the muscular branches that enter the brachialis just below the
elbow so that the muscle can be retracted adequately. Ligation also
allows the radial artery, which runs down the proximal third of the
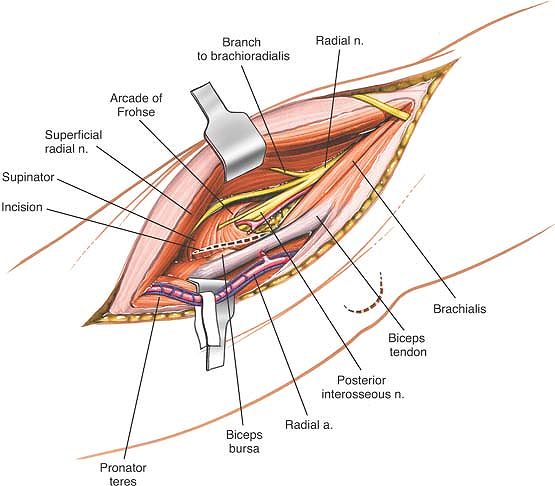
forearm on the pronator teres, to be retracted medially (Fig. 3-19).
 |
|
Figure 3-19
The radial nerve divides into its three terminal branches: the posterior interosseous nerve, the sensory branch (which appears under the brachioradialis), and a motor branch to the extensor carpi radialis brevis. Develop a plane between the brachioradialis and the pronator teres. |
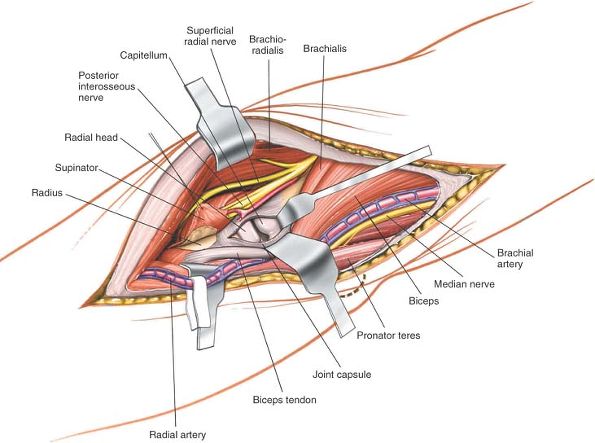
the elbow, make a longitudinal incision in the anterior capsule of the
joint between the radial nerve laterally and the brachialis medially (Fig. 3-20).
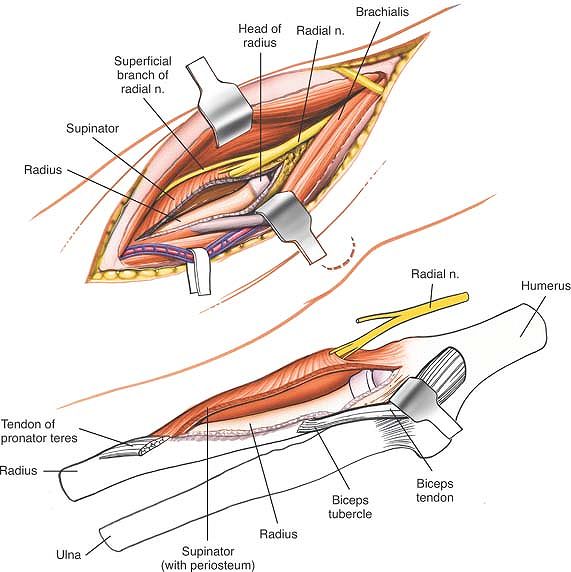
moves anteriorly. Incise the origin of the supinator down the bone,
staying just lateral to the insertion of the biceps tendon. Complete
the exposure of the proximal radius by circumferential subperiosteal
dissection (see Fig. 3-20, inset, and Anterior Approach to the Radius in Chapter 4).
 |
|
Figure 3-20
Deep surgical dissection. Make a longitudinal incision in the anterior capsule of the joint between the radial nerve and the brachialis muscle to expose the radial head and capitulum. To expose the radius further, remove the supinator muscle distally in a subperiosteal manner (inset). |
identified in the interval between the brachioradialis and brachialis
muscles before this interval is developed fully. Note that the nerve
lies anteromedial to the brachioradialis, within the fascial
compartment of that muscle. If it is being sought at the level of the
distal humerus or elbow, the intermuscular interval is the best place
to find it.
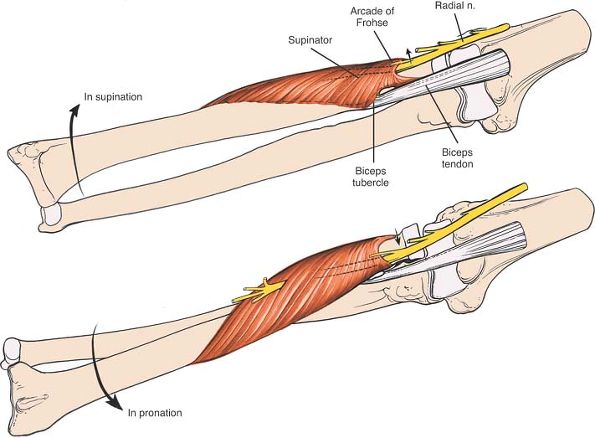
is vulnerable to injury as it winds around the neck of the radius
within the substance of the supinator muscle. To prevent damage to the
nerve, ensure that the supinator is detached from its insertion on the
radius with the forearm in supination. Do not cut through the muscle
body to expose the bone (see Anterior Approach to the Radius in Chapter 4; Fig. 3-21; see Fig. 3-33).
muscles; retract it with the medial skin flap (see Fig. 3-17).
 |
|
Figure 3-21
Place the forearm in supination to move the posterior interosseous nerve lateral to the incision into the radiohumeral joint and away from the incision into the origin of the supinator muscle, protecting it. |
must be ligated so that the brachioradialis can be mobilized fully.
Ligation also reduces postoperative bleeding and avoids the risk of an
ischemic contracture developing postoperatively as a result of the
pressure caused by a postoperative bleed (see Fig. 3-19).
anterolateral approach can be extended easily into an anterolateral
approach to the distal humerus by developing the plane between the
brachialis and triceps muscles. Remember that the radial nerve crosses
the lateral border of the humerus about one handbreadth above the
lateral epicondyle. (For details, see Anterolateral Approach to the Distal Humerus.)
anterolateral approach can be extended easily to expose the entire
anterior surface of the radius by developing the plane proximally
between the brachioradialis muscle (which is supplied by the radial
nerve) and the pronator teres muscle (which is supplied by the median
nerve), and distally between the brachioradialis muscle (which is
supplied by the radial nerve) and the flexor carpi radialis muscle
(which is supplied by the median nerve). (For details, see Anterior Approach to the Radius in Chapter 4.)
surgical approach to the elbow and provides access to the neurovascular
structures that are found in the cubital fossa. Its uses include the
following:
-
Repair of lacerations to the median nerve
-
Repair of lacerations to the brachial artery
-
Repair of lacerations to the radial nerve
-
Reinsertion of the biceps tendon
-
Repair of lacerations to the biceps tendon
-
Release of posttraumatic anterior capsular contractions
-
Excision of tumor
arm in the anatomic position. Exsanguinate the limb either by elevating
it for 3 to 5 minutes or by applying a soft rubber bandage or
exsanguinator. Then, apply a tourniquet (see Fig. 3-14).
 |
|
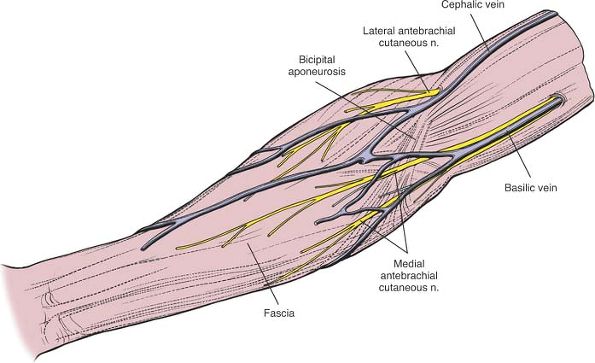
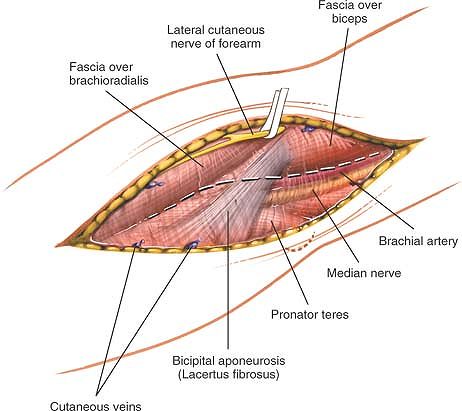
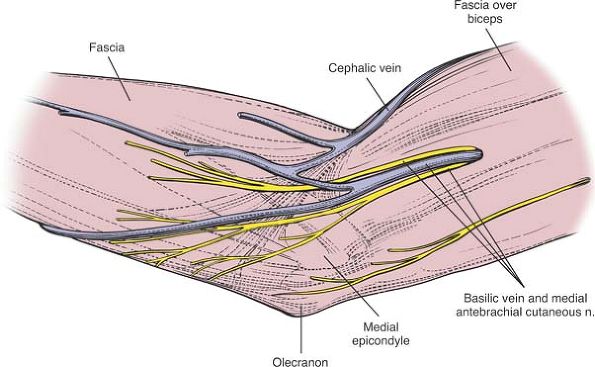
Figure 3-22 Superficial view of the elbow and forearm, showing superficial veins and nerves.
|
aspect of the elbow. Begin 5 cm above the flexion crease on the medial
side of the biceps. Curve the incision across the front of the elbow,
then complete it by incising the skin along the medial border of the
brachioradialis muscle. Curving the incision avoids crossing the
flexion crease at 90° (Figs. 3-22 and 3-23).
 |
|
Figure 3-23 Incision for the anterior approach to the cubital fossa.
|
 |
|
Figure 3-24
Internervous plane. Distally, the plane is between the brachioradialis (radial nerve) and the pronator teres (median nerve); proximally, it is between the brachioradialis (radial nerve) and brachialis (musculocutaneous nerve). |
plane lies between the brachioradialis muscle (which is supplied by the
radial nerve) and the pronator teres muscle (which is supplied by the
median nerve) (Fig. 3-24).
between the brachioradialis muscle (which is supplied by the radial
nerve) and the brachialis muscle (which is supplied by the
musculocutaneous nerve).
in line with the skin incision and ligate the numerous veins that cross
the elbow in this area.
branch of the musculocutaneous nerve) must be preserved. To find it,
locate the interval between the biceps tendon and the brachialis
muscle. The nerve emerges there to run down the lateral side of the
forearm subcutaneously (Fig. 3-25).
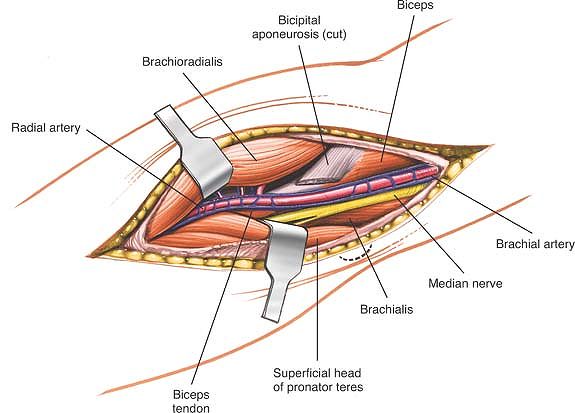
fibrosus), which is a band of fibrous tissue coming from the biceps
tendon and swinging medially across the forearm, running superficial to
the proximal part of the superficial flexor muscles (see Fig. 3-25).
Cut the aponeurosis close to its origin at the biceps tendon and
reflect it laterally. Be careful not to injure the brachial artery,
which runs immediately under the aponeurosis (Fig. 3-26).
 |
|
Figure 3-25
Superficial surgical dissection. Locate the lateral cutaneous nerve of the forearm in the interval between the biceps tendon and the brachialis, and preserve it. |
tendon and trace it proximally to its origin from the brachial artery.
Note that both the brachial vein and the median nerve lie medial to the
artery. To identify the radial nerve, look between the brachialis and
the brachioradialis; the nerve crosses in front of the elbow joint.
relationship are the keys to operating successfully in the cubital
fossa (see Fig. 3-26).
exploration of the neurovascular structures, deep dissection is not
required. If you require access to the anterior capsule of the elbow
joint, retract the biceps and brachialis muscle medially and the
brachioradialis muscle laterally. Fully supinate the forearm and
identify the origin of the supinator muscle from the anterior aspect of
the radius. Incise the origin of this muscle and dissect it off the
bone in a subperiosteal
plane,
carefully reflecting it laterally. Take care not to insert a retractor
on the lateral aspect of the proximal radius as this may compress the
posterior interosseous nerve. The anterior capsule of the elbow joint
is now exposed and may be incised to expose the anterior aspect of the
elbow joint (Fig. 3-28).
 |
|
Figure 3-26
After cutting the bicipital aponeurosis (lacertus fibrosus), identify the brachial artery. Note that the median nerve lies medial to the artery. The brachial vein, which accompanies the artery, consists of a series of small, fine vessels, the venae comitantes. |
-
The lateral cutaneous nerve of the
forearm (the sensory branch of the musculocutaneous nerve) is
vulnerable to injury in the distal fourth of the arm during incision of
the deep fascia. Pick it up in the interval between the biceps and
brachialis muscles in the arm, trace it downward, and preserve it (see Fig. 3-25). -
The radial artery lies immediately deep
to the bicipital aponeurosis; the aponeurosis must be incised carefully
to avoid damage to the artery (see Fig. 3-26). -
The posterior interosseous nerve is
vulnerable to injury as it winds round the neck of the radius within
the substance of the supinator muscle. To prevent damage to the nerve,
ensure that the supinator is detached from its insertion on the radius
with the forearm in supination (see Fig. 3-20).
the incision superiorly along the medial border of the biceps, and
incise the deep fascia in line with the incision. The brachial artery
lies immediately under the fascia, between the biceps muscle and the
underlying brachialis muscle. The medial nerve runs with the artery.
 |
|
Figure 3-27
Trace the median nerve distally into the pronator teres. Incise a portion of the muscle superficial to the nerve, if necessary, to expose the nerve. The incision lies between the humeral and ulnar heads of the pronator teres. |
 |
|
Figure 3-28
Retract the biceps tendon and carefully detach and retract the proximal supinator muscle to gain access to the anterior joint capsule, which may be incised to expose the elbow joint. |
median nerve as it disappears into the pronator teres muscle. Simple
retraction of the muscle may provide adequate exposure. Take care not
to cut any branches of the median nerve going to the flexor-pronator
group of muscles that pass from the medial side of the median nerve at
the level of the elbow joint. This incision lies between the humeral
and ulnar heads of the pronator teres and allows the plane between the
two heads to be developed for the distal exposure of the nerve (Fig. 3-27).
the radial artery, trace it distally as it crosses the surface of the
pronator teres, running toward the lateral side of the forearm.
Developing the plane proximally between the pronator teres and
brachioradialis muscles, and distally between the flexor carpi radialis
and brachioradialis muscles allows the artery to be followed to the
wrist.
is useful for all surgeries to the radial head, including excision of
the radial head and insertion of a prosthetic replacement.8,9
 |
|
Figure 3-29 Position of the patient on the operating table.
|
annular ligament without risking damage to the posterior interosseous
nerve, avoid extending the incision to the upper part of the radial
shaft.
Exsanguinate the limb either by applying a soft rubber bandage or an
exsanguinator or by elevating it for 3 to 5 minutes. Then, inflate a
tourniquet (Fig. 3-29).
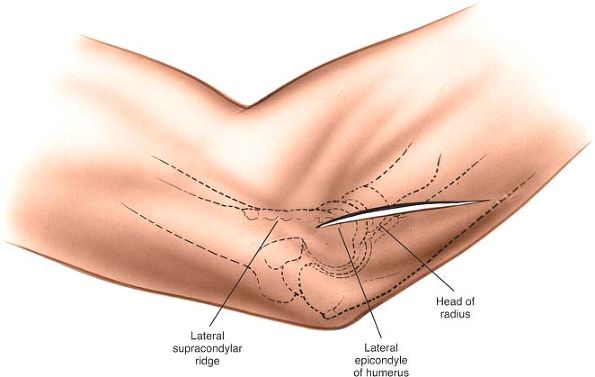
radial head lies deep within this depression. It is palpable through
the muscle mass of the wrist extensors. As the forearm is pronated and
supinated, movement of the radial head can be felt beneath the
surgeon’s fingers. In cases of fracture of the radial head, the normal
landmarks are lost because of hemorrhage and swelling. Crepitus at the
fracture site often is quite obvious and helpful in placing the
incision.
 |
|
Figure 3-30 Make a longitudinal incision based proximally on the lateral humeral epicondyle.
|
posterior surface of the lateral humeral epicondyle and continuing
downward and medially to a point over the posterior border of the ulna,
about 6 cm distal to the tip of the olecranon.
proximally on the lateral humeral epicondyle. This incision follows the
skin fold and lies directly over the radial head (Fig. 3-30).
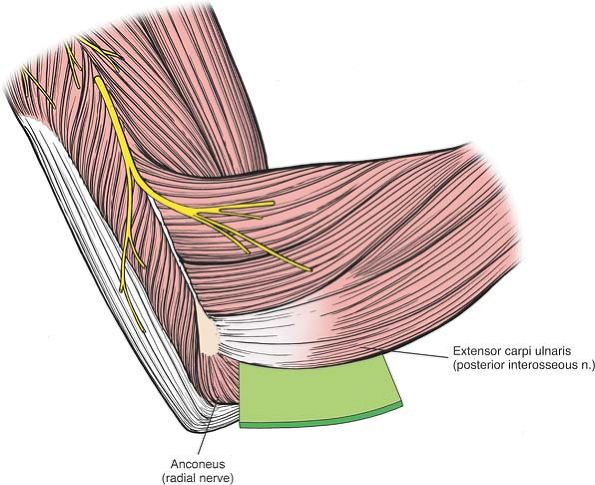
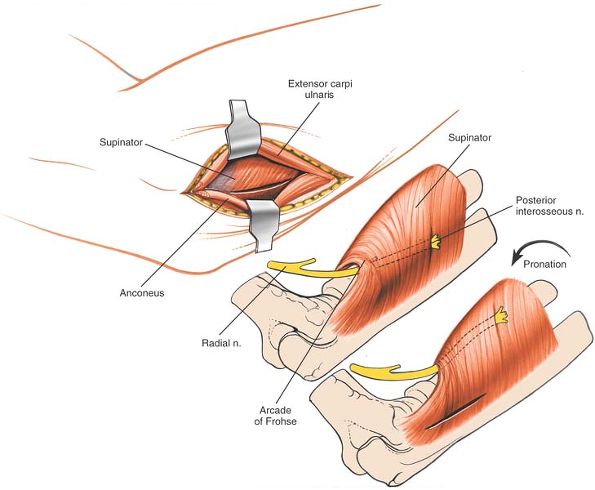
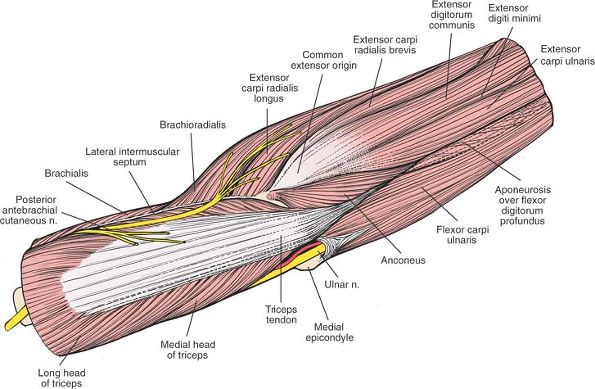
is supplied by the radial nerve, and the extensor carpi ulnaris, which
is supplied by the posterior interosseous nerve (Fig. 3-31).
To find the interval between the extensor carpi ulnaris and the
anconeus, look distally where the plane is easy to identify;
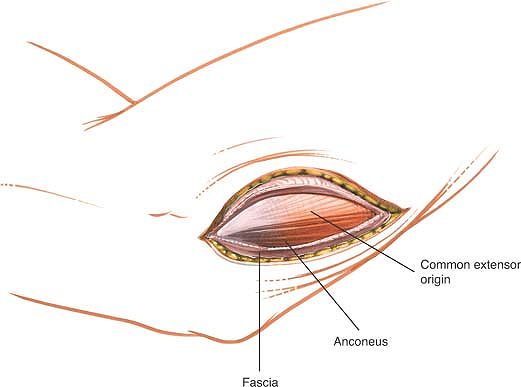
proximally, the two muscles share a common aponeurosis (Fig. 3-32).
Detach part of the superior origin of the anconeus as it arises from
the lateral epicondyle of the humerus. Then, separate the anconeus and
extensor carpi ulnaris muscles, using retractors (Fig. 3-33).
contusion in this area, and it is difficult to identify the interval
between the extensor carpi ulnaris and anconeus muscles. In this case,
it is safe to dissect straight down onto the lateral epicondyle of the
humerus, because this structure always can be palpated easily.
 |
|
Figure 3-31 The internervous plane lies between the anconeus (radial nerve) and the extensor carpi ulnaris (posterior interosseous nerve).
|
 |
|
Figure 3-32 Find the interval between the extensor carpi ulnaris and the anconeus distally. Proximally, the two muscles merge.
|
 |
|
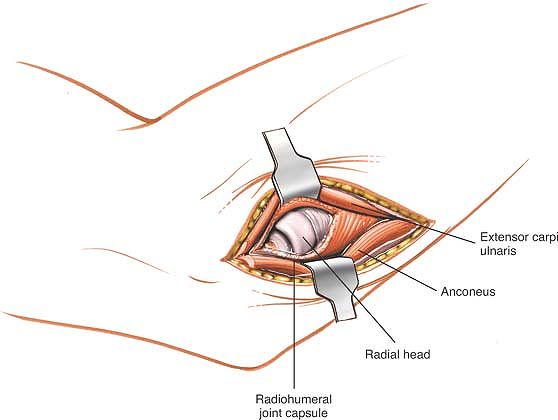
Figure 3-33
Detach the superior origin of the anconeus from the lateral epicondyle, and separate the anconeus and the extensor carpi ulnaris. Pronation of the forearm moves the posterior interosseous nerve medially away from the operative field (insets). |
reveal the underlying capitulum, the radial head, and the annular
ligament. Do not incise the capsule too far anteriorly; the radial
nerve runs over the front of the anterolateral portion of the elbow
capsule. Do not continue the dissection below the annular ligament or
retract vigorously, distally, or anteriorly, because the posterior
interosseous nerve lies within the substance of the supinator muscle
and is vulnerable to injury (Fig. 3-34).
is in no danger as long as the dissection remains proximal to the
annular ligament. Pronation of the forearm keeps the nerve as far from
the operative field as it possibly can be (see Fig. 3-33, inset).
To ensure the safety of the nerve, take great care to place the
retractors directly on bone and be careful in their placement. Because
the posterior interosseous nerve actually may touch the bone of the
radial neck, directly opposite the bicipital tuberosity, placing
retractors behind it poses a risk.11
cutting down on the lateral supracondylar ridge. Strip the tissues off
subperiosteally both anteriorly and posteriorly to gain access to the
distal humerus and to expose the capitellum. Apply a varus force to
open up the lateral compartment of the joint. The extension is most
useful for fixing fractures internally and for removing loose bodies in
the lateral compartment of the elbow (see Anterolateral Approach to the Distal Humerus in Chapter 2).
 |
|
Figure 3-34 Incise the joint capsule longitudinally to expose the capitulum and radial head.
|
lower end of the humerus and the upper end of the radius and ulna. It
communicates with the superior radioulnar joint.
-
The lateral capitulum articulates with the radial head. Its shape is reminiscent of a hemisphere.
-
The medial trochlea
articulates with the ulna. Its shape resembles a spool of thread. It
extends further distally than the capitulum, resulting in a
configuration that gives a tilt to the lower end of the humerus and
produces the “carrying angle” of the joint. The trochlea is grooved;
the groove’s boundaries are marked medially by a prominent, sharp ridge
and laterally by a lower, more blunted ridge.
collateral ligaments. The anterior and posterior ligaments are mainly
thickened sections in the capsule,
which
is exactly what would be expected from a hinge joint. The shape of the
bones that comprise the elbow joint and the presence of the strong
collateral ligaments make it difficult to explore the joint completely
without extensive dissection. Medial and lateral approaches to the
joint provide limited access unless they are extended. Complete
exposure is obtained most easily through a posterior approach, and then
only if an olecranon osteotomy is performed. Four groups of muscles
cross the elbow joint:
-
Anteriorly, the flexors of the elbow, which are supplied by the musculocutaneous nerve
-
Posteriorly, the extensor of the elbow, which is supplied by the radial nerve
-
Medially, the flexor-pronator group of
muscles (the flexors of the wrist and fingers, and the pronators of the
forearm), which are supplied by the median and ulnar nerves. They arise
from the medial epicondyle of the humerus. -
Laterally, the extensors of the wrist and
fingers, and the supinators of the forearm, which are supplied by the
radial and posterior interosseous nerves. They arise from the lateral
epicondyle of the humerus.
plane; two are internervous planes and can be explored. A third
internervous plane lies within the lateral group, as follows:
-
Between the anterior and lateral
muscle groups, which are supplied by the musculocutaneous and radial
nerves, respectively. The anterolateral approach uses the interval
between the brachialis and brachioradialis muscles (see Fig. 3-16). -
Between the anterior and medial
muscle groups, which are supplied by the musculocutaneous and median
nerves, respectively. The medial approach uses the interval between the
brachialis and pronator teres muscles (see Figs. 3-8 and 3-24). -
Between two members of the lateral group:
the anconeus muscle (which is supplied by the radial nerve) and the
extensor carpi ulnaris muscle (which is supplied by the posterior
interosseous nerve, a major branch of the radial nerve; see Fig. 3-31). The posterolateral approach to the radial head uses this plane.
posterior groups of muscles is not an internervous plane, because both
groups are supplied by the radial nerve. The plane is useful, though,
because the radial nerve gives off its branches well proximal to the
elbow. This pseudo-internervous plane, which is used in the lateral
approach, falls in the interval between the brachioradialis and triceps
muscles (see Fig. 2-24A).
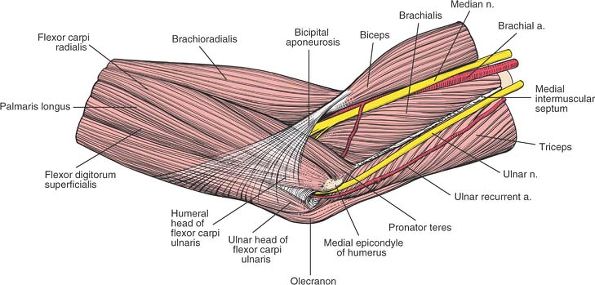
forearm, forming a triangular fossa known as the cubital fossa, which
is bordered by the pronator teres medially and the brachioradialis
laterally. The superior border of the triangle consists of an imaginary
line joining the medial and lateral epicondyle of the humerus.
front of the joint on its medial side and is covered by the bicipital
aponeurosis (lacertus fibrosus) in the cubital fossa. It disappears
between the two heads of the pronator teres muscle as it leaves the
fossa and runs down the forearm, adhering to the deep surface of the
flexor digitorum superficialis muscle (see Fig. 4-12).
front of the elbow joint in the interval between the brachialis and
brachioradialis muscles. It divides in the cubital fossa at the
radiohumeral joint line into the posterior interosseous nerve (which
enters the substance of the supinator muscle) and the superficial
radial nerve (which descends the lateral side of the forearm under
cover of the brachioradialis muscle; see Fig. 3-19).
joint in the groove on the back of the medial epicondyle, where it is
easy to palpate. The nerve enters the anterior compartment of the
forearm by passing between the two heads of the flexor carpi ulnaris
muscle, which it supplies and where it may be entrapped. It then runs
down the forearm on the anterior surface of the flexor digitorum
profundus (see Figs. 3-40 and 3-43). In the proximal third of the forearm, it supplies the ring and little fingers.
the cubital fossa, running on the lateral side of the median nerve and
lying on the brachialis muscle. The median nerve passes under the
bicipital aponeurosis, which separates it from the median basilic vein,
a frequent site of venous puncture (see Fig. 3-35).
In the days when bleeding was a recognized form of treatment and
venesection was done with lancets rather than with needles, this site
was a frequent one used by barber surgeons. The reason this site was
preferred is because the bicipital aponeurosis protects the vital
structures of the artery and nerve, which provided these early
practitioners with a margin of safety, because their patients often
moved on insertion of the lancet. Halfway down the
cubital
fossa, the artery divides into two terminal branches: the radial and
ulnar arteries. Similar to the median nerve, the artery may be damaged
in supracondylar fractures of the humerus (see Fig. 3-26).
medial to the biceps tendon before turning anteriorly, lying on the
supinator muscle and the insertion of the pronator teres muscle. In the
upper forearm, it lies under the brachioradialis muscle (see Fig. 4-11).
disappears from the cubital fossa by passing deep to the deep head of
the pronator teres, the muscle that separates it from the median nerve
(see Fig. 4-13).
-
The pronator teres
-
The flexor carpi radialis
-
The flexor digitorum superficialis
-
The palmaris longus
-
The flexor carpi ulnaris (Fig. 3-36)
the flexor carpi ulnaris is supplied by the ulnar nerve. The pronator
teres, the most proximal muscle, forms the medial border of the cubital
fossa.
 |
|
Figure 3-35 Medial view of the elbow. Note the sensory nerves and veins on the medial side of the elbow joint.
|
of the medial epicondyle. They can be retracted only a short distance
because the median nerve, passing through the pronator teres muscle,
“anchors” the group and prevents distal retraction (Figs. 3-35, 3-36, 3-37, 3-38 and 3-39).
-
The mobile wad of three muscles,
consisting of the brachioradialis, the extensor carpi radialis longus,
and the extensor carpi radialis brevis -
Four muscles arising from the common
extensor origin: the extensor digitorum communis, the extensor digiti
minimi, the extensor carpi ulnaris, and the anconeus
muscle of the elbow; its function is unclear. Its more distal fibers
run almost vertically and act as a weak extensor of the elbow, whereas
its proximal fibers are almost horizontal and
adduct
and rotate the ulna. This unlikely movement occurs to a slight degree
at the elbow. Electromyographic studies suggest that the muscle is most
active during extension,12
but it probably functions more as a stabilizer while other muscles act
on the elbow as prime movers, functioning in much the same way as does
the rotator cuff in the shoulder.
 |
|
Figure 3-36
The five muscles of the forearm have a common flexor origin on the medial epicondyle. All five are supplied by the median nerve. The ulnar nerve passes between the two heads of the flexor carpi ulnaris. The median nerve runs beneath the bicipital aponeurosis. |
 |
|
Figure 3-37
The flexor-pronator group has been resected, revealing the course of the ulnar nerve as it runs around the medial epicondyle, passing distally before entering the plane between the flexor carpi ulnaris and the flexor digitorum profundus. |
 |
|
Figure 3-38
The flexor muscles have been resected further. The medial epicondyle has been subjected to osteotomy. Distally, the ulnar nerve crosses the forearm between the flexor carpi ulnaris and the profundus. The median nerve enters the forearm between the two heads of the pronator teres, lying on the tendon of the brachialis. |
 |
|
Figure 3-39 The joint capsule has been opened. The brachialis is elevated from the capsule.
|
forms one boundary of the internervous plane that is used in the
posterolateral approach to the radial head.
cross the anterior aspect of the elbow joint. Both are supplied by the
musculocutaneous nerve, which runs between the biceps and the
brachialis in the upper arm. In front of the elbow, they diverge; the
biceps runs laterally to the bicipital tuberosity of the radius, and
the brachialis runs medially to the coronoid process of the ulna.
flat tendon, which also overlies the brachialis. The tendon rotates so
that its anterior surface faces laterally as it passes between the two
bones of the forearm before inserting into the back of the radius at
the bicipital tuberosity. A bursa separates the tendon from the
anterior part of the tuberosity.
 |
|
Figure 3-40
Superficial view of the posterior aspect of the elbow. The triangular aponeurosis of the triceps runs down to its triangular insertion into the ulna. The ulnar nerve lies in its groove on the posterior aspect of the elbow. The brachial cutaneous nerve crosses the intermuscular septum on the posterior aspect of the elbow. Anconeus. Origin. Lateral epicondyle of humerus and posterior joint capsule of elbow. Insertion. Lateral side of olecranon and posterior surface of ulna. Action. Extensor of elbow. Nerve supply. Radial nerve.
|
cubital fossa. It separates superficial nerves and vessels from deep
ones. Lying superficial are the median cephalic vein, the median
basilic vein, and the medial cutaneous nerve of the forearm. Lying deep
are the median nerve and the brachial artery.
and brachial vein can be remembered easily through the mnemonic “VAN”
(vein, artery, nerve), which labels the structures from the lateral to
the medial aspect. They all pass medial to the biceps tendon under the
lacertus fibrosus (see Fig. 3-27).
 |
|
Figure 3-41
The distal part of the triceps, the origins of the flexors and flexor carpi ulnaris, and the extensor tendons have been resected. The ulnar nerve enters the plane between the two heads of the flexor carpi ulnaris. On the radial side, the radial nerve lies anterior to the intermuscular septum, between the brachioradialis and brachialis muscles. |
 |
|
Figure 3-42
The insertion of the anconeus, the origin of the extensor carpi ulnaris, and the common extensor origin are revealed. The radial nerve divides into its main continuation, the posterior interosseous nerve, as it enters the supinator muscle through the arcade of Frohse. The superficial branch (sensory branch) of the radial nerve enters the undersurface of the brachioradialis. The ulnar nerve gives off its branches to the flexor carpi ulnaris immediately after it passes around the groove between the olecranon and the medial epicondyle. |
 |
|
Figure 3-43
The supinator muscle has been resected, revealing the distal course of the posterior interosseous nerve through its distal portion. The annular portion of the radiohumeral ligament is defined clearly. |
Boer P, Stanley D: Surgical approaches to the elbow. In: Stanley D, Kay
N, eds. Surgery of the elbow: practical and scientific aspects. London,
Arnold, 1998
AB, Jaeger SH, Larochelle D: Comminuted fractures of the radial head:
the role of silicone implant replacement arthroplasty. J Bone Joint
Surg [Am] 63:1039, 1981
JCH, Ellis BW: Vulnerability of the posterior interosseous nerve during
radial head excision. J Bone Joint Surg [Br] 53:320, 1971
