Imaging of the Knee
most important instruments in evaluating joint pain, musculoskeletal
imaging remains an essential adjunct. Multiple imaging modalities are
available to confirm a provisional diagnosis or narrow the differential
diagnosis. Because many imaging techniques are costly and require
radiation exposure for the patient, they should be used judiciously.
Imaging should begin with a standard set of plain radiographs, with
special radiographic views and more elaborate modalities used if
indicated. Once a diagnosis is established and a treatment plan
initiated, imaging also can be used to monitor disease progression or
response to treatment.
confirmatory or screening imaging. Modern equipment and techniques have
reduced the amount of ionizing radiation required for routine
radiography. The equipment and processing are relatively inexpensive
and widely accessible compared with other modalities. The osseous
anatomy of the knee is simple and easily understood, making
interpretation of the images straightforward.
examination are a matter of preference and may even be tailored to
answer specific questions raised during the history and physical
examination. However, the initial radiographic examination should
include the least amount of radiation necessary to adequately visualize
the essential anatomic features of the knee:
-
Osseous structures of the distal femur, proximal tibia, and patella
-
Alignment of the knee joint
-
Joint space
-
Periarticular soft tissues
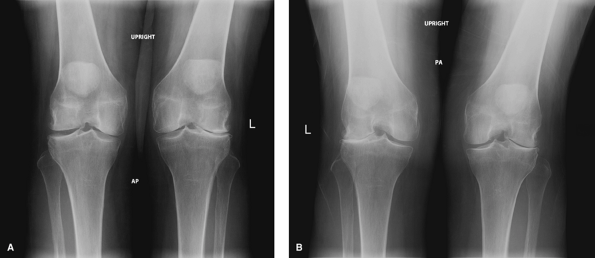
radiographic examination: (i) standing weight-bearing anteroposterior
(AP) view, (ii) standing weight-bearing posteroanterior (PA) flexion
view, (iii) lateral view, and (iv) axial view of the patella.
is obtained with the patient standing with equal weight on both lower
extremities, knees fully extended, and toes pointing straight ahead.
The beam is positioned horizontally at the level of the distal pole of
the patella. Inclusion of both knees on one image allows for careful
side-to-side comparison for subtle abnormalities. Like a standard
non–weight-bearing AP radiograph, the standing AP view allows
inspection of many osseous landmarks of the knee, including the distal
surfaces of the femoral condyles, medial and lateral epicondyles,
medial and lateral tibial plateaus, tibial spines, and the head of the
fibula. However, the weight-bearing radiograph more accurately
represents the condition of the articular surface and is more likely to
exhibit tibiofemoral joint space narrowing if pathology is present.
With no mechanical load through the knee, non–weight-bearing technique
allows relaxation through the joint and may project artificial widening
of the joint space. In addition, much like physical evaluation,
assessment of tibiofemoral alignment on a weight-bearing radiograph
better illustrates the functional alignment of the joint.
weight-bearing activities occur with the knee in full extension. In
addition, tibiofemoral contact area decreases and contact force
increases as the knee flexes, making the posterior weight-bearing
surfaces of the femoral condyles susceptible to early degeneration
under pathologic conditions. The addition of a weight-bearing 45-degree
PA flexion view allows for assessment of the posterior weight-bearing
surfaces of the femoral condyles and provides a tangential view of the
medial and lateral weight-bearing surfaces of the tibial plateau (Fig. 17-1B).
This view is also obtained with the patient standing with equal weight
on both lower extremities and toes pointing straight ahead, but the
knees are flexed 45 degrees with the patellae touching the vertically
oriented radiograph cassette. The beam is directed posteroanterior,
angled 10 degrees caudad, and centered at the level of the distal pole
of the patella. An additional advantage of this view is visualization
of the intercondylar notch of the femur, similar to that observed with
a traditional tunnel view.
 |
|
Figure 17-1 A:
Standing anteroposterior view of the knees demonstrates significant narrowing of the lateral compartment joint space in the left knee with a well-maintained joint space of the contralateral right knee. B: Weight-bearing 45-degree posteroanterior flexion view reveals complete loss of the lateral compartment joint space in both knees. |
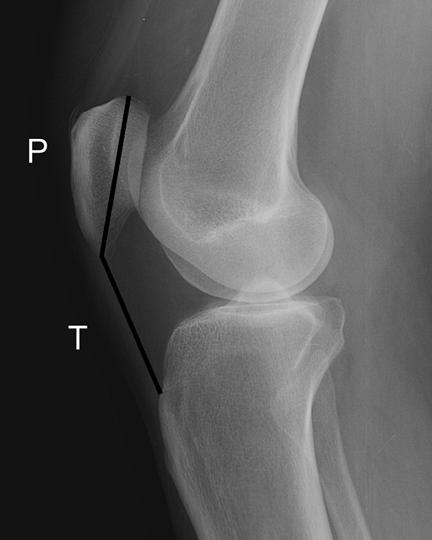
is obtained with the patient lying with the lateral aspect of the
affected knee against the radiograph table. With the knee flexed
approximately 30 degrees, the x-ray beam is directed tangential to the
surfaces of the tibial plateau, perpendicular to the radiograph
cassette under the lateral aspect of the knee. The lateral view also
visualizes most landmarks of the distal femur, proximal fibula, and
proximal tibia, adding an orthogonal view for complete evaluation of
osseous architecture. Additionally, the proximal and distal poles of
the patella and relationships of the patellofemoral articulation can be
assessed, as well as the soft tissues of the extensor mechanism.
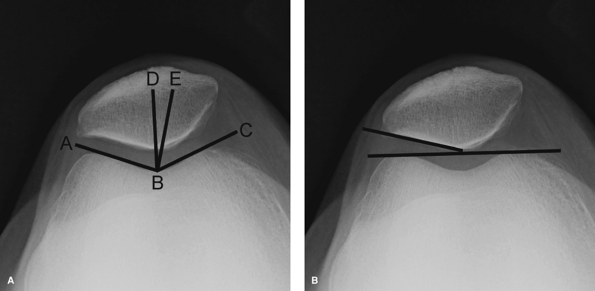
must be obtained to visualize the medial and lateral facets of the
patella, alignment of the patella within the femoral sulcus, and the
status of the patellofemoral joint space. Multiple techniques have been
described for obtaining the axial view, differing only by angle of knee
flexion at which the image is obtained. The Merchant view is probably
the most popular and widely used method, owing to its clear
representation of the medial and lateral patellar facets,
patellofemoral joint space, and alignment. The view is obtained with
patient’s knees flexed 45 degrees over the end of the exam table. The
x-ray beam is directed caudally through the patella, at an angle 30
degrees below horizontal, at a film cassette resting on the patient’s
shins in a position perpendicular to the x-ray beam.
 |
|
Figure 17-2
Lateral view of the knee. The Insall-Salvati ratio (T/P) can be used to determine the height of the patella relative to the sulcus of the distal femur. The ratio of the length of the patellar tendon (T) to the diagonal length of the patella (P) should differ by no more than 20%. |
a routine, systematic fashion. The patient’s name, date of examination,
and laterality (right versus left) of the image
must
be verified. The clinician should briefly review the image for quality
control to make sure all pertinent anatomy is visualized, paying
particular attention to image penetration, joint position, and
orientation of the x-ray beam.
 |
|
Figure 17-3 Merchant view of the knee. A:
To measure the congruence angle, line DB is established as a reference line that bisects the sulcus angle ABC. A second line is drawn from the apex (ridge) of the patella to the center of the sulcus. Congruence angle DBE is positive if it opens lateral to reference line DB, and measurements greater than approximately 15 degrees indicate lateral patellofemoral subluxation. B: The lateral patellofemoral angle is formed by a tangent across the medial and lateral condyles and a line parallel to the lateral facet of the patella. An angle that opens medially represents excessive lateral patellar tilt. |
soft tissue and osseous anatomy visible on an image. Like the
components of a thorough history, the findings peripheral to the knee
joint may provide valuable diagnostic clues and historical data that
could alter the diagnosis or treatment plan. The presence of
significant vascular calcification indicates the presence of peripheral
vascular disease and may preclude the use of a tourniquet should
surgical intervention be warranted. Evidence of posttraumatic or
postsurgical changes may be evident in the femoral or tibial diaphyses
near the margins of the image, requiring additional images for complete
evaluation. Rarely, occult soft tissue masses and neoplasms may be
identified as subtle soft tissue densities adjacent or peripheral to
the knee joint. Likewise, osseous neoplasms may be identified, either
as an incidental finding or as the primary source of the patient’s
symptoms.
and assessment of general architecture. The lateral femoral condyle is
normally smaller than the medial condyle and exhibits a more acute
radius of curvature posteriorly. The medial and lateral tibial plateaus
are also asymmetric, with the larger medial plateau demonstrating a
concave contour on the lateral projection and the lateral plateau
exhibiting slight convexity. Both tibial surfaces slope posteriorly
approximately 10 degrees. The patella, best visualized on the axial
view, consists of asymmetric medial and lateral facets.
The
medial facet is smaller and slightly convex, and the larger lateral
facet is concave in the coronal plane. Gross abnormalities in size,
shape, contour, or spatial relationships of major osseous structures
may indicate the presence of congenital, developmental, or
posttraumatic pathology.
|
TABLE 17-1 Radiographic Landmarks and Anatomy of the Knee
|
|
|---|---|
|
abnormalities indicative of metabolic or neoplastic processes. Bone
quality and mineralization can provide diagnostic clues, with
generalized osteopenia present in the setting of inflammatory
arthritides as a result of intense regional hyperemia. Conversely,
degenerative conditions are associated with increased mineralization in
the subchondral region as a result of increased local stresses. All
joint surfaces should be examined for focal defects, wear patterns, and
other signs of remodeling such as osteophyte formation.
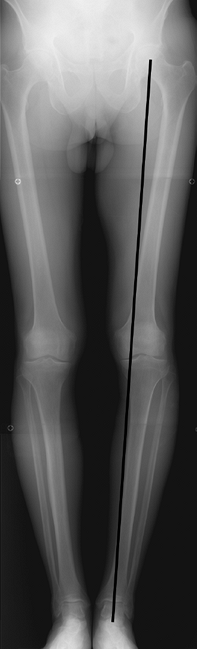
intersection of lines drawn parallel to the long axes of the femur and
tibia and is typically between five and seven degrees of valgus. In
most patients, the standing AP view allows for adequate assessment of
tibiofemoral alignment in the coronal plane. However, patients with
pre-existing congenital, posttraumatic, or postsurgical deformities of
the femur or tibia require an AP long-leg hip to ankle radiograph for
accurate assessment of the anatomic axis (Fig. 17-4).
The mechanical weight-bearing axis of the knee, illustrated by a
straight line drawn from the center of the femoral head to the center
of the ankle joint, can also be determined on the long-leg radiograph.
A line passing through the middle third of the proximal tibia
represents a neutral mechanical axis, whereas lines passing through the
medial third and lateral third represent varus and valgus mechanical
axes, respectively.
be evaluated on both the lateral and axial images of the knee. The
height of the patella relative to the distal femur is evaluated on the
lateral radiograph using the Insall-Salvati ratio (Fig. 17-2).
Normal patellar height is represented by a ratio of one, whereas ratios
of 0.8 and 1.2 represent patella baja and patella alta, respectively.
The relationship of the patella to the sulcus of the distal femur is
evaluated on the axial view of the patella. Patellofemoral subluxation
can be evaluated objectively by calculating the congruence angle (Fig. 17-3A).
When the apex of the patella lies lateral to the center of the femoral
sulcus and the congruence angle is >15 degrees, lateral
patellofemoral subluxation is present. The lateral patellofemoral angle
assesses patellar tilt (Fig. 17-3B) and opens medially in the presence of abnormal lateral tilt.
narrowing on plain radiographs, is the final common pathway for many
disease processes of the knee joint and must be accurately assessed in
the medial, lateral, and patellofemoral compartments. Many disease
processes produce predictable patterns of joint space narrowing. For
example, inflammatory conditions result in generalized enzymatic
destruction of articular cartilage and diffuse joint space narrowing on
plain radiographs. Conversely, osteoarthritis begins as a localized
mechanical process that leads to focal cartilage loss and joint space
narrowing.
 |
|
Figure 17-4
Anteroposterior long-leg hip-to-ankle radiograph. The mechanical axis of the limb is determined by a line between the center of the femoral head and the center of the ankle. |
predictive of tibiofemoral articular cartilage loss than a
non–weight-bearing view. However, the weightbearing 45-degree PA
flexion view is the most sensitive plain radiographic method for
detection of tibiofemoral joint space narrowing (Fig. 17-1).
With this technique, the x-ray beam is tangential to the weight-bearing
surfaces of the femoral condyles and tibial plateau and perpendicular
to the desired joint space measurement, therefore providing accurate
assessment of the actual joint space. Because the patella does not
enter the femoral sulcus until the knee is flexed 30 degrees, axial
views of the patellofemoral joint must be obtained at flexion angles
>30 degrees to visualize the patellofemoral articulation. The
traditional skyline view is obtained with the knee flexed >90
degrees, and in this degree of flexion the patella contacts the femur
distal to the femoral sulcus. The patellofemoral joint space is well
visualized on the Merchant view, obtained at 45 degrees of knee flexion
(Fig. 17-3).
tissues of varying composition allows visualization of many peripheral
soft tissue features. The extensor mechanism is the only normal
periarticular soft tissue structure routinely visualized on plain
radiographs. On the lateral view, adjacent adipose tissue delineates
the linear soft tissue densities of the quadriceps and patellar tendons
proximal and distal to the patella, respectively. Many pathologic
processes can be diagnosed by their characteristic appearance as soft
tissue densities. On the lateral image, joint effusion is an easily
identified soft tissue mass deep to the quadriceps tendon. Popliteal
cysts are also fluid-filled masses occasionally identified as soft
tissue densities on the lateral radiograph. Intra-articular and
extra-articular soft tissue structures are commonly visualized
secondary to calcification. Intra-articular findings include
chondrocalcinosis from deposition of calcium pyrophosphate dihydrate
crystals in articular cartilage and menisci. Osteocartilaginous loose
bodies are associated with many conditions affecting the articular
surface, including trauma, chondromalacia patella, osteochondritis
desiccans, and osteoarthritis. They may be identified anywhere within
the knee joint including the femoral notch, suprapatellar pouch, medial
and lateral gutters, and the posterior recesses of the knee.
Extra-articular soft tissue calcifications commonly occur in tendinous
and ligamentous structures. Calcification at the origin of the medial
collateral ligament (Pellegrini-Stieda sign) signifies prior injury to
the medial collateral ligament. Notable soft tissue calcifications in
the region of the popliteal vessels may suggest need for further
evaluation with ultrasonography to rule out aneurysm and pseudoaneurysm
of the popliteal artery.
 |
|
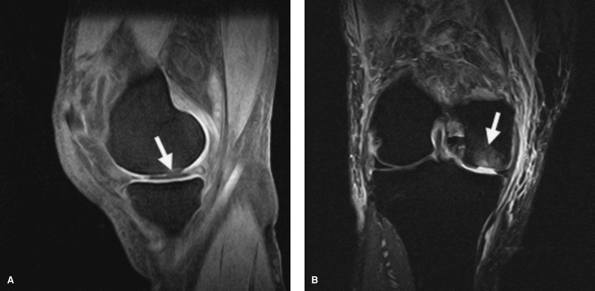
Figure 17-5 Images depicting a high-grade articular cartilage defect in the distal weight-bearing surface of the medial femoral condyle. A:
Sagittal fat-suppressed three-dimensional spoiled gradient-echo image demonstrating fluid, which is low signal intensity, within the lesion (arrow). B: Coronal short time inversion recovery (STIR) image of the same lesion. Note the adjacent edema in the subchondral bone (arrow). |
complement to plain radiography for evaluation of the painful knee.
Although costly, MRI has many advantages over other imaging modalities
and has supplanted many older imaging techniques. MRI provides
multiplanar capability and unrivaled image contrast with spatial
resolution comparable with that of computed tomography (CT). The
ability to enhance tissue contrast by variation of scanning parameters
allows for comprehensive evaluation of all osseous and soft tissue
structures of the knee, including articular cartilage, without exposing
the patient to ionizing radiation.
injuries to soft tissue structures of the knee, including tendons,
capsuloligamentous structures, and the menisci, is unrivaled and is
well documented in the orthopaedic and sports medicine literature. The
reader is referred to other sources for a comprehensive review of these
topics.
many pathologic processes of bone before they are detectable by plain
radiography. Osteonecrosis, stress fracture, osteomyelitis, and
neoplasm may all share a stage when patients present with significant
symptoms but normal plain
radiographs.
All of these conditions cause early accumulation of marrow edema at the
site of the lesion. MRI capitalizes on these early changes in local
tissue characteristics, which are manifested as areas of high signal on
T2-weighted images.
improved with the implementation of imaging sequences designed
specifically for articular cartilage. The two most commonly used
sequences are the T1 fat-suppressed three-dimensional (3D) spoiled
gradient-echo technique and the T2 fast spin echo technique. The 3D
gradient echo sequence displays articular cartilage as a smooth band of
hyperintense tissue along the cortical margin of the articular surface (Fig. 17-5A).
On the T2 fast spin echo sequence, articular cartilage is a smooth band
of intermediate signal intensity. Articular defects in this sequence
are visualized much as an arthrogram, with hyperintense fluid filling
the defect and interrupting the normally smooth contour. Both
techniques exhibit a high degree of accuracy, with the best results in
the patellofemoral joint where the hyaline cartilage is thickest. The
short time inversion recovery (STIR) sequence is also a commonly used
sequence and produces images similar to the fast spin echo technique (Fig. 17-5B).
knee has increased in recent years, mostly because of the development
of articular cartilage restoration procedures. The improved imaging
techniques help identify appropriate candidates for reconstruction, aid
in preoperative planning, and provide a reliable method for following
postoperative progress and response to treatment without the need for
repeat arthroscopy. Imaging of the articular surface can also help with
patient selection for corrective osteotomies about the knee, with or
without the need for cartilage restoration. Imaging can offer
preoperative prognostic information to patients undergoing arthroscopy
for other reasons, as the presence of articular surface defects has a
negative impact on clinical outcome.
KP, Schmid MR, Zanetti M, et al. Cartilaginous defects of the
femorotibial joint: accuracy of coronal short inversion time
inversion-recovery MR sequence. Radiology. 2006; 240:482-488.
