Physical Evaluation of the Elbow
IV – Elbow Reconstruction > Part A – Evaluation > 47 – Physical
Evaluation of the Elbow
can lead to the diagnosis in most cases. Before focusing on the main
complaint, it is important to determine some basic information about
your patient. With each piece of information obtained, the investigator
should always continually be triaging some differential diagnoses. The
patient’s age allows an early distinction
between possible congenital or developmental conditions when young,
e.g., congenitally dislocated radial head presenting in a child unable
to fully supinate the forearm in extension as compared with a greater
tendency for degenerative pathologies in the elderly. Some pathologies
(e.g., lateral epicondylitis) occur in the middle of an average life
span, between 20 and 60 years, but not at the extremes beyond this
range. The occupation may point toward
some obvious diagnoses—e.g., the baseball pitcher is more prone to
medial collateral ligament injury and valgus extension overload
syndrome, whereas a manual laborer may present with primary
degenerative arthrosis. Those in occupations involving a lot of weight
bearing on the elbows—e.g., plumbers, carpenters, and gardeners—may
show a tendency for olecranon bursitis. Which is the dominant arm (right, left, or ambidextrous), and is it the arm presenting with the current problem?
complaint, is pain. Also note any secondary complaints, which may or
may not be directly linked with the primary complaint; elbow pain with
numbness of the hand as occurs in median nerve entrapment at the elbow
is an example of linked symptoms. Which of the symptoms is most
troublesome to the patient, with respect to being most disabling to his
or her function? Ask for a subjective prioritization.
-
Location—Ask
the patient to be precise and delineate the painful area with a single
finger to map its extent where possible. Sometimes the pain is vague
and poorly defined, as in a rheumatoid elbow with articular and
periarticular pain (Table 47-1). -
Periodicity—Is the pain constant or intermittent, spontaneous or associated with specific activities?
-
Severity—Sometimes
sequential visual analogue scores are useful for tracking the
progression of pain on different office visits and after any
intervention. -
Quality—Pain
can be described in many ways, notably as sharp, dull, deep-seated,
aching, stabbing, locking with loose bodies, grating with a
degenerative joint, apprehension of an unstable joint, and so on. -
Timing—Is the
pain worse in the morning, suggestive of rheumatoid disease; in the
evening, suggestive of degenerative disease; or at night, which may
suggest chronic granulomatous or neoplastic pathologies. -
Radiation—Does
the pain radiate proximally or distally into the anatomically relevant
muscle groups (e.g., tennis elbow of ECRB degenerative cause can
radiate distally into the forearm to the distribution of the extensor
mass musculature), or does the pain radiate into a dermatomal
distribution? For example, ulnar nerve entrapment between the two heads
of flexor carpi ulnaris can cause radiating pain along the medial
forearm to the ring and little fingers, median nerve entrapment between
the two heads of pronator teres causes radiating pain into the radial
3.5 digits of the hand, and cervical osteoarthritis can cause radiating
pain or numbness into the whole hand. Also bear in mind that pain at
the elbow can originate from the neck, necessitating a cervical spine
examination. -
Duration—How long has the pain been present and troubling the patient?
-
Aggravating factors—Using
an osteoarthritic joint worsens the pain, wrist extension against
resistance aggravates tennis elbow, and wrist flexion against
resistance aggravates golfer’s elbow.
|
TABLE 47-1 Location of Pain in Relation to Common Differential Diagnoses
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
from the patient. This is often the most fruitful part of the history
taking. If there was a specific injury to account for the current
complaint, the direction, magnitude, and timing of the forces involved
should be examined. Distinguish between a single event (e.g., an
eccentric single contraction of the biceps during a football tackle
leading to an acute distal biceps rupture) or multiple events (e.g.,
multiple painful episodes during biceps curls while weight lifting,
leading to a partial biceps rupture). Some pathologies arise as a
result of overuse, which may seem unimportant to the patient—e.g., a
prolonged period of gardening or sports followed by tennis elbow after
2 days. During the time of injury or unusual event(s), did the patient
observe any noises or other symptoms—a pop suggestive of a ligament
sprain or rupture, a click as in an elbow instability, locking of the
joint owing to a trapped loose body or instability, immediate swelling
of a hematoma, or a delayed swelling of a traumatic or inflammatory
effusion?
concerning the complaint being presented? Although not all-inclusive,
pending litigation may adversely affect the patient’s perception of the
problem with an alteration of the portrayal of the clinical symptoms
and signs.
problem, what advice has been given previously, and what is the
patient’s perception of the final outcome? Understanding the patient’s
perception at the time of presentation gives valuable insight into the
potential for a good outcome.
standard algorithm: inspection, active motion, passive motion, and
relevant imaging. During the physical examination, the affected side
should be compared with the contralateral (normal) side.
angle of the forearm relative to the arm when the upper limb is in a
neutral position next to the body (fully extended and supinated). Age,
sex, and racial variations should be considered; normal is 5 to 10
degrees in males; 10 to 15 degrees in females.1
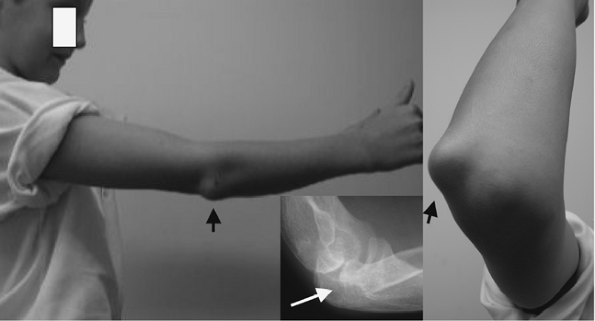
If the carrying angle is outside the normal range, the observable
deformity (posttraumatic or growth disturbance—cubitus varus or gun
stock deformity of <5 to 10 degrees [Fig. 47-1] or cubitus valgus >15 degrees), bearing in mind that all “deformity”
may not be pathologic (normal racial or sexual variation). The skin
color can be instructive in some conditions and should be compared with
the contralateral nonpathologic limb; for example, an anterior
ecchymosis as a result of a biceps rupture will be unilateral, and skin
changes as a result of chronic psoriasis can be bilateral. Some skin
changes can be nonpathologic but should be noted, e.g., port-wine
stains, strawberry nevi, grey slate marks, and so on. Following trauma
or some surgeries reflex sympathetic dystrophy can often lead to
reddened skin that is shiny and painful.
 |
|
Figure 47-1
An 18-year-old man with a 20-degree cubitus varus deformity following a childhood malunited supracondylar distal humeral fracture. |
|
TABLE 47-2 Location of Swelling in Relation To Common Differential Diagnoses
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
part of the elbow, and their fundamental characteristics help to
diagnose the underlying pathology. Basic characteristics to define are
the exact location and size. Other characteristics require palpation
and are outlined below. Scars can be
either traumatic or iatrogenic/surgical. The size and shape of the scar
is noteworthy and can be helpful for planning future surgeries. Also
note the quality of the scar, which can indicate the patient’s healing
response; for example, a keloid scar may indicate a vigorous scar
response and the potential for elbow capsular contracture, whereas a
paper-thin scar may indicate a poor healing response, of relevance to
ligamentous ruptures requiring repair. Finally note any muscle wasting.
In the forearm that has undergone a Volkman ischemic contracture, owing
to compartment syndrome, the forearm musculature can be markedly wasted
(Fig. 47-6). In the hand, the wasting of
interosseous muscles/hypothenar eminence may be indicative of ulnar
nerve compression in the cubital or Guyon tunnel; and wasting of the
thenar eminence may indicate median nerve entrapment between the two
heads of pronator teres (pronator syndrome) or may indicate nerve
compression in the carpal tunnel (carpal tunnel syndrome) (Table 47-2).
 |
|
Figure 47-2 Distal biceps tendon rupture with proximal migration of the muscle belly (Popeye sign).
|
 |
|
Figure 47-3 Proximal biceps tendon rupture with distal migration of the muscle belly with associated bruising (Popeye sign).
|
(full extension) to 145 degrees (full flexion). Loss of extension can
be a sensitive indicator of intra-articular pathology and can signal an
acute event (e.g., intra-articular effusion [synovial or hematoma] or a
chronic event (e.g., degenerative arthrosis with anterior capsular
contracture). Loss of flexion can be a consequence of posterior
capsular contracture.
to 90 degrees (pronation, palm down), 80 to 90 degrees (supination,
palm up). When assessing forearm rotation, the examiner should ensure
that the patient’s elbow is flexed to 90 degrees and positioned next to
the trunk, thereby avoiding shoulder abduction or adduction. These
latter motions can falsely alter forearm motion, with shoulder
abduction compensating for a restriction in pronation and shoulder
abduction compensating for supination restriction. Thumb and hand
motion relative to the distal radioulnar joint can also lead to a false
sense of motion of the forearm axis.
range of motion testing will highlight a difference since pain often
inhibits the active range. If active and passive ranges are
complete,
the latter can be used to gain information about both the midarc and
end-arc of the motion. The primary information that is sought regarding
the mid-arc of motion is whether or not there is crepitus, which is
suggestive of chondral degenerative pathology. This assessment can be
enhanced by asking the patient to actively resist the passive motion,
thereby increasing the joint reactive forces and accentuating signs
originating from the bearing surfaces.
 |
|
Figure 47-4 Developmental dislocation of the radial head, producing a lateral swelling and restriction of prosupination.
|
provide information about the restraint to greater motion, but this
test can be painful if done with excess zeal. During this assessment,
one should continually consider whether the end point to the passive
motion is rigid as in bony contact, or less rigid or soft implying a
soft tissue cause of the end point (Table 47-3).
With forced end-arc flexion, approximation of the forearm to arm
musculature prevents greater flexion, whereas in thin patients the
coronoid process may abut the coronoid fossa. In end-arc extension,
there is the bony abutment between the olecranon process and its
reciprocal fossa. In a normal joint such forced end-arc testing
is not painful, but pain may be encountered with pathologic changes in osteophytosis and loose bodies.
 |
|
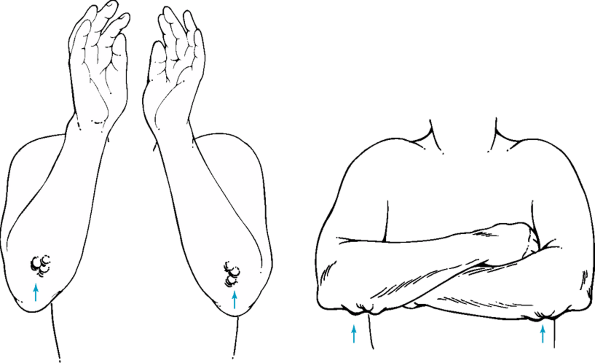
Figure 47-5 Typical position for rheumatoid nodules on the subcutaneous borders of the forearms (illustration), with a background photograph of severe rheumatoid swellings.
|
 |
|
Figure 47-6
Volkman ischemic contracture of left forearm after an elbow fracture dislocation, treated in plaster cast. Forearm muscles have necrosed, and fibrotic scar tissue remains. |
be immobilized and motion should be achieved by rotation of the forearm
at the distal radioulnar joint. A common mistake is to hold the
patient’s hand to test for forearm rotation, which serves to build in
an error to the rotation values so gained, since wrist joint laxity can
be ≤15 degrees and more in patients with rheumatoid arthritis. Forced
end-arc pronation and supination are normally resisted by forearm
muscular stretching, although in thin subjects bony abutment can occur
between the radius and ulna.
supported in 80 to 110 degrees of flexion with the forearm in neutral
rotation. If tested either in greater extension or greater flexion, the
maximum strength decreases to 75%.3
The examiner should support the flexed elbow in the cupped palm of one
hand with the other hand holding the distal forearm to produce
resistance to motion. When attempting to grade the power of muscles or
to longitudinally track changes in their strength, a grading system is
useful, notably the MRC muscle strength grading system (Table 47-4).
This method of testing is for isometric strength, but the clinical
history should guide the examiner to also test for eccentric and
concentric contractions where appropriate, first without resistance
then with resistance. The specific movements to be tested are elbow
flexion and extension, forearm pronation and supination, and wrist
flexion and extension. The latter two movements are relevant to the
examination of the elbow since most of the muscles driving these
actions cross the elbow joint and can be symptomatic at the elbow.
|
TABLE 47-3 Differential Diagnoses Associated with Passive Motion
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
TABLE 47-4 MRC Grading of Muscle Strength
|
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 |
|
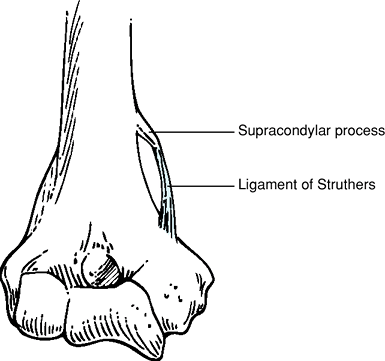
Figure 47-7 Medial supracondylar process and ligament of Struthers, sources of median nerve compression.
|
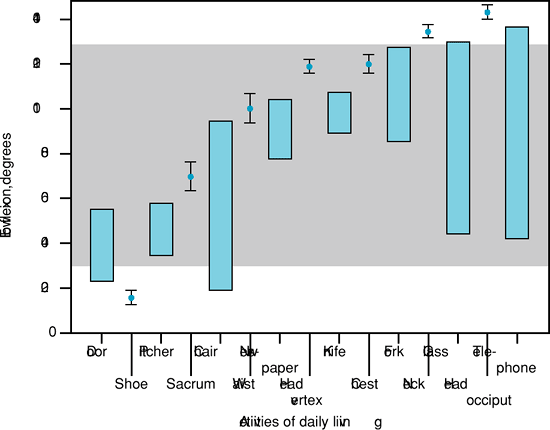
to place the hand where needed to manipulate the environment. Whereas
the shoulder motion defines a sphere centered on the glenohumeral
joint, the elbow allows the hand to move in and out to the extremity of
the sphere, along the radii of the sphere.4 To perform most activities of daily living, a full range of elbow motion is not
necessary, and this is possible with a sagittal flexion arc from 30 to
130 degrees and forearm rotational arc of 50 degrees pronation and 50
degrees supination. A comprehensive assessment should include 15
activities of daily living that primarily test the flexion arc and 15
activities that test the forearm rotational arc of motion (Fig. 47-11).
However, assessing the elbow function can be adequately and
consistently performed using an overall evaluation scoring system, the
Mayo Elbow Performance Score,4 in which five activities of daily living are addressed (Table 47-5).
 |
|
Figure 47-8
Cadaveric dissection demonstrating the origin of the anterior medial collateral ligament (AMCL) at the anteroinferior aspect of medial epicondyle and the insertion at the sublime tubercle of the proximal ulna. |
 |
|
Figure 47-9 Triceps rupture with a consequent inability to extend the elbow against gravity.
|
above will enable the examiner to decide whether specific pathology
related tests are required for further clarity of the presenting
complaint. The tests outlined below in this section are not mandatory
for all patients, but only for those about whom the examiner has a
level of suspicion regarding the diagnosis. These special and specific
tests fall broadly into three categories: (i) ligamentous instability
tests, (ii) inflammation tests, and (iii) neurology-based tests.
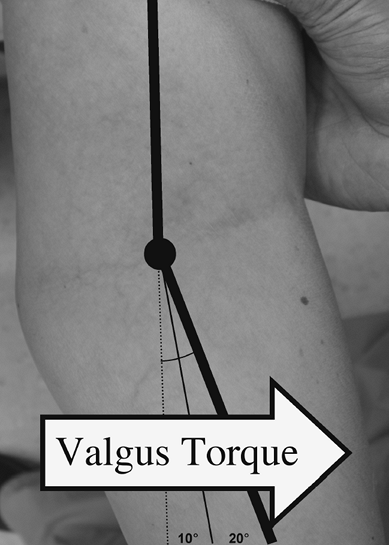
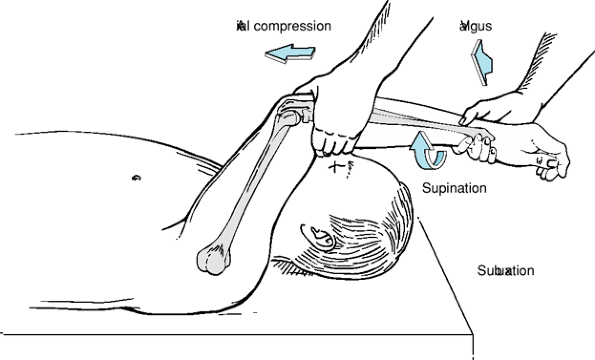
torque on the distal radioulnar joint. In this position the olecranon
process is closed packed in the reciprocal fossa and may conceal less
severe ligamentous injuries.
 |
|
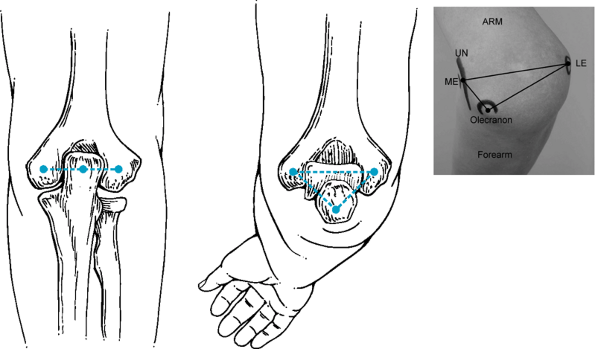
Figure 47-10
Normal posterior alignment is present when the olecranon forms a straight line with the two epicondyles with the elbow extended. An equilateral triangle is formed when the elbow is flexed to 90 degrees. Inset photograph demonstrates malalignment of these bony points owing to a malunited supracondylar humeral fracture. ARM, LE, lateral epicondyle; ME, medial epicondyle; UN, ulnar nerve. |
varus deformation, the elbow is flexed to 20 to 30 degrees, which
allows less severe ligamentous injuries to be uncovered. The difficulty
with testing valgus/varus stability in this position is that the
humerus rotates outside the examiner’s control, thereby introducing an
error to the extent of any instability detected. Hence when testing in
slight elbow flexion, the
effect
of the shoulder is minimized by placing it in either full external
rotation for valgus stress testing or full internal rotation for varus
stress testing5 (Fig. 47-12).
When considering what constitutes a positive test result, either
increases in laxity compared with the normal contralateral limb or an
increase in pain is a relevant finding. However, be wary of the
contralaterally lax “normal” elbow when comparing with the known
pathologic side.
 |
|
Figure 47-11
Fifteen activities of daily living. Those that can be achieved within a 100-degree arc of flexion (30 degrees–130 degrees) are in the central grey area. |
 |
|
Figure 47-12 Valgus stability testing in a fully extended elbow. The arm is stabilized, and the forearm is moved in the plane of testing.
|
|
TABLE 47-5 The Mayo Elbow Performance Score
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||
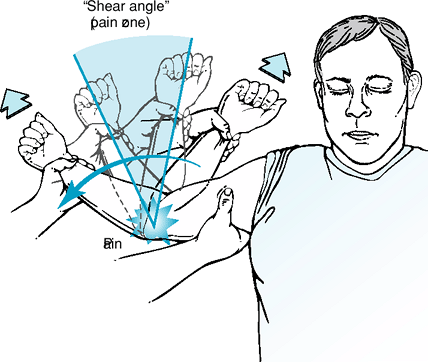
the examiner places, and maintains thoughout the test, a constant
valgus torque on a fully flexed elbow, which is then rapidly fully
extended (Fig. 47-13). This is essentially a motion version of the common
milking test. A positive finding consists of medial elbow pain
predominant in the flexion arc shear zone of between 120 and 70 degrees.6
 |
|
Figure 47-13 The moving valgus stress test for identifying medial collateral ligament (MCL) injuries.
|
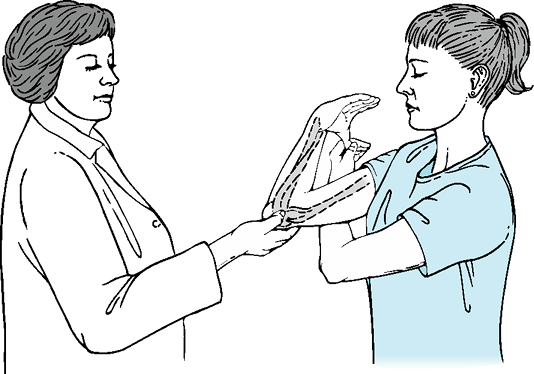 |
|
Figure 47-14 The milking test for identifying anterior medial collateral ligament (AMCL) injuries in continuity.
|
examiner or the patient pulls the thumb of the pathologic limb with a
valgus torque, with the elbow flexed between full 130 and 70 degrees7,8 (Fig. 47-14).
Pain is produced at the site of the medial collateral ligament,
anterior band. This test is especially sensitive when there is a medial
collateral ligament injury.
The radial head is seen to sublux/dislocate when the supinated forearm
is axially compressed and stressed with a valgus torque and passively
fully extended from 30-degree flexion. The radial head relocates with a
clunk with flexion from full extension to 30-degree flexion (Fig. 47-15).
This test is rarely positive in the awake patient but is quite helpful
to perform while the patient is under anesthesia. In the awake patient,
the push-up test may prove more patient friendly, with the patient
requested to push up from a seated position, with the hands firmly
pushing on the chair arms. The patient’s hands should be in full
supination. The patient will report pain or will not use the affected
side to push up from the chair.
 |
|
Figure 47-15 Posterolateral instability test-degree starting flexed position. The posterior subluxed radial head will reduce with a clunk.
|
(lateral epicondylitis), the examiner resists the patient’s effort to
extend a flexed wrist while maintaining an extended elbow, pronated
forearm, and radially deviated wrist. Pain originating from the lateral
epicondyle constitutes a positive test.
(lateral epicondylitis), the examiner fully flexes the patient’s wrist,
with a pronated forearm, and extends the elbow from a flexed starting
position.
A painful response can also emanate from radial nerve compression, requiring electrodiagnosis.
(lateral epicondylitis), resistance to the patient’s attempt to
maintain extension of the middle finger proximal interphalangeal joint
causes pain at the lateral epicondyle. This tests the involvement of
the extensor digitorum communis in the lateral epicondylar symptoms.
(medial epicondylitis), the examiner resists the patient’s attempt to
flex a fully extended wrist, with a supinated forearm and extended
elbow. A positive result constitutes pain at the medial epicondyle.
(medial epicondylitis), with the patient’s wrist flexed, the forearm
fully pronated, and the elbow flexed to 15 degrees, the examiner
performs wrist extension, forearm supination, and elbow extension
simultaneously. Pain emanating from the medial epicondyle constitutes a
positive result.
formal assessment, along with the dermatomal sensory distributions and
motor end organs. The sensation of these dermatomes and cutaneous
nerves should be performed as a matter of routine. The major mixed
nerves acting on the elbow are the ulnar, radial, and median nerves.
palpated behind the medial epicondyle, and any irritability should be
noted. A small percentage of normal subjects demonstrate subluxing
ulnar nerves, which can be felt to sublux over the medial epicondyle
during flexion and relocate during extension. In some, this finding is
associated with irritability and some degree of ulnar nerve
dysfunction. Sensation is tested with light touch and pin-prick testing
of the little finger and ulnar half of the ring finger. Motor function
is tested by the examiner, resisting the patient’s attempt to spread
apart the patient’s fully extended fingers, a function of the ulnar
nerve innervated interosseous muscles of the hand. However, Martin-Gruber anastomosis
may produce normal interosseous muscle function in the presence of an
ulnar nerve lesion at the elbow and should be borne in mind. This
anatomic anomaly provides motor fibers for interosseous muscle
innervation from the median nerve; these fibers enter the ulnar nerve
in the forearm, distal to the cubital tunnel. Normally the innervation
is entirely from the ulnar nerve, without interruption from the C8 and
T1 spinal origin.
tunnel syndrome), gentle tapping of the ulnar nerve, as it lies on the
posterior aspect of the medial epicondyle, should not cause a tingling
sensation in the forearm’s ulnar nerve innervated territory and the
little finger and ulnar half of the ring finger in the normal subject.
When this test is positive, the indication is that there is nerve
regenerative activity occurring at the test site, and hence, this is a
useful test for tracking the progress of a recovering nerve. Care
should be taken not to percuss the nerve too vigorously, since the
Tinel sign will be positive even in normal subjects, leading to
misdiagnosis. Another source of testing error can be a Guyon tunnel
compression of the ulnar nerve at the wrist, which should be sought
separately.
A positive finding constitutes pain, numbness, and ulnar nerve
distribution tingling owing to this positionally induced nerve ischemia
in the cubital tunnel.
of ulnar nerve motor dysfunction. The examiner pulls strongly on a
sheet of paper that the patient is asked to hold firmly between the
thumb and index finger. A positive test consists of the paper being
withdrawn by the examiner, since the ulnar nerve innervated adductor
pollicis and flexor pollicis brevis deep head are unable to maintain
good pinch strength with thumb metacarpophalangeal joint (MCPJ) flexion
and interphalangeal joint (IPJ) extension. With ulnar nerve (UN)
dysfunction, the thumb MCPJ becomes hyperextended and the IPJ flexes in
an attempt to maintain the pinch grip.
easily palpable nerve, but can be palpated 1 to 2 cm distal to the
anterior radiocapitellar joint while pronating and supinating the
forearm. This motion allows the nerve to pass under the examiner’s
digit and causes symptoms of pain when the nerve is pathologically
compressed. Sensory dysfunction of the main radial nerve trunk
(proximal to the elbow) or the superficial radial nerve (distal to the
elbow after bifurcation of the main nerve) leads to tingling or
paresthesia of the first dorsal web space. Motor dysfunction at the
elbow leads to a wrist drop owing to loss of innervation of the wrist
extensors in the forearm.
(radial tunnel syndrome), pain is reproduced when the examiner resists
the patient’s attempt at supinating the forearm. This is an important
test to carry out when one of the differential diagnoses is tennis
elbow because of the infrequent but recognized possibility that the two
pathologies coexist.
the cutaneous innervation to the radial three and a half digits, along
with the ulnar half of the volar forearm. It can be compressed by
anomalous anatomy, notably the ligament of Struthers, a ligament that
passes from the humeral shaft to the medial epicondyle in 1% of the
population.11 Since the brachial
artery accompanies the nerve on occasion, there may be concurrent
symptoms of vascular compromise. The lacertus fibrosus can also be a
source for median nerve compression, and resisted supination from a
starting position of supination can cause pain in the median nerve
distribution. The other common site for median nerve compression is the
carpal tunnel of the wrist, but this latter does not cause any
paresthesia of the forearm, as is the case with more proximal
compressions. Motor signs of median nerve compression include weakness
of forearm pronation (pronator teres), wrist flexion and abduction
(flexor carpi radialis), and flexion of the thumb IPJ (flexor pollicis
longus). Thenar eminence wasting may also be observed in long-standing
cases.
(pronator teres syndrome), the examiner resists the patient’s attempt
to pronate the forearm with a flexed and extended elbow. The
reproduction of tingling and paresthesia in the median nerve
distribution in the forearm and hand constitutes a positive result.
(FDS compression of Median nerve), when the examiner resists the
patient’s attempt to flex the middle finger from a starting position of
extension, a pathologic flexor digitorum superficialis fibrous arc can
cause compression and distal signs as above.
(anterior interosseous nerve syndrome), when the patient is asked to
form a tip-to-tip pinch with the thumb and index finger, making an O
sign, the patient can form only a pulp-to-pulp pinch, reminiscent of a
raindrop. The median nerve/anterior interosseous nerve, when compressed
between the two heads of pronator teres, interrupts the motor
innervation to the flexor pollicis longus and the radial half of the
flexor digitorum profundus, with the subsequent inability to flex the
terminal joints of the thumb and index finger.12
(LACN) is the sensory terminus of the musculocutaneous nerve. Its
sensory distribution is the radial half of the forearm between the
elbow and wrist. When pathologic, a Tinel sign can be elicited with
percussion of the nerve immediately lateral to the biceps tendon in the
elbow flexion crease.
-
AMCL – Anterior medial collateral ligament
-
DDRH – Developmental dislocation of radial head
-
DIY – Do it yourself
-
ECRB – Extensor carpi radialis brevis
-
EDC – Extensor digitorum communis
-
EMG – Electromyogram
-
GE – Golfer’s elbow
-
IA – Intra-articular
-
IPJ – Interphalangeal joint
-
LB – Loose body
-
LCL – Lateral collateral ligament
-
MCPJ – Metacarpophalangeal joint
-
MN – Median nerve
-
NCV – Nerve conduction study
-
OA – Osteoarthritis
-
PIN – Posterior interosseous nerve
-
RA – Rheumatoid arthritis
-
RCJ – Radiocapitellar joint
-
RSD – Reflex sympathetic dystrophy
-
TE – Tennis elbow
-
UN – Ulnar nerve
-
ΔΔ – Differential diagnosis
