Osteosarcoma
people. While relatively rare compared to other orthopaedic disorders,
an appropriate level of suspicion must be maintained for osteosarcoma
as a source of pain in this age group. When diagnosed early and treated
appropriately, survival with a highly functional limb can often be
achieved in this age group. Most osteosarcoma patients present with
pain as the initial symptom, but some patients first notice this after
an injury or falsely attribute their symptoms to a minor trauma.
Therefore, pain that does not improve in the expected time period, or
pain that is worsening despite treatment or rest, should raise a red
flag, and an appropriate work-up, starting with plain radiographs, must
be pursued. Osteosarcoma has a bimodal distribution with a second but
smaller peak in late adulthood. Adult osteosarcomas are often secondary
to conditions such as Paget’s disease or prior radiation (Table 6.1-1).
After biopsy, the standard treatment of osteosarcoma includes
preoperative chemotherapy, followed by resection, and postoperative
chemotherapy when appropriate.
-
Osteosarcoma is a tumor composed of a malignant spindle cell stroma (background) with malignant osteoblasts
P.178
that produce tumor osteoid (collagenous immature bone that appears pink on hematoxylin-and-eosin [H&E] staining) or bone (Fig. 6.1-1).Table 6.6-1 Comparison of Vascular Sarcomas of BoneSarcoma Type Age Gender Anatomic Distribution Gross Appearance Histologic Features Other Details Hemangioendothelioma First through ninth decades M > F (slightly) Half involve lower extremity; any bone affected Firm, friable, bloody Well-formed vascular spaces (“staghorn spaces”) lined by plump endothelial cells.
Intermixed with corded pattern mimicking carcinoma.Multicentricity common; one third of cases multifocal Epithelioid hemangioendothelioma Second through eighth decades; peaks in second and third decades M > F (slightly) Femur most common; any bone affected Firm, lobulated, tan Corded, nested, or stranded pattern of plump endothelial cells with eosinophilic cytoplasm within hyalinized stroma (see Fig. 6.6-1).
May form narrow vascular channels.
Occasional cytoplasmic vacuoles (represent primitive blood vessel lumina).
Signet ring-like appearance.Angiosarcoma Peaks in fourth decade M > F (slightly) Long tubular bones and spine most common; any bone affected Firm, bloody Less vasoformative than hemangioendotheliomas.
Regions with vascular differentiation and plump malignant endothelial cells.
Some areas may show epithelioid appearance. -
As is the case with most sporadic
occurring malignancies, the factors that lead to the development of an
osteosarcoma are largely unknown.-
Most likely, a mutation or group of mutations occurs that leads to uncontrolled growth of the mutant cells.
-
Evidence exists to support the role of
genetic abnormalities in patients with osteosarcoma, though these
abnormalities are not identified in most patients.
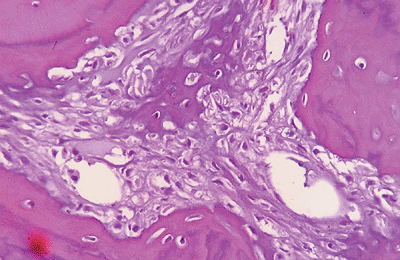 Figure 6.1-1
Figure 6.1-1
H&E stain shows a malignant spindle cell (osteoblast) stroma with
lace-like (pink) osteoid and calcified (darker) osteoid in center,
typical of a high-grade osteosarcoma. -
-
Two tumor suppressor genes may play a
significant part in tumorigenesis in osteosarcoma: p53 (chromosome 17)
and Rb (chromosome 13). -
Reported familial patterns of osteosarcoma
-
Chromosome 13:14 rearrangement in sisters
-
Deletion of part of chromosome 13 resulting in inactivation of the retinoblastoma (RB) gene in cousins
-
-
Two genetic conditions that predispose to development of osteosarcoma
-
Retinoblastoma patients
-
May have germline mutation of Rb gene
-
Increased risk of osteosarcoma
-
-
Li-Fraumeni syndrome (a familial cancer syndrome; p53 gene abnormalities)
-
Increased risk of osteosarcomas and other malignancies
-
Mothers of children with sarcomas have up to a three times increased risk of breast carcinoma.
-
-
is neither the most common primary bone malignancy nor the most common
malignancy affecting bone. The most common primary bone malignancy is
multiple myeloma, and the most common malignancy affecting bone is
metastatic carcinoma.
-
Bimodal peak age incidence
-
Crude incidence: 0.3 per 100,000 per year in United States (roughly 900 per year)
-
Majority occur within the second decade (~60%)
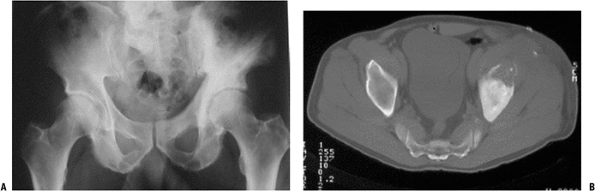
![]() Figure 6.1-2 (A)
Figure 6.1-2 (A)
Plain radiograph shows an area of bony destruction in the anterior left
iliac wing and pagetic changes throughout the left hemipelvis. (B)
Axial CT image shows lesion with soft tissue extension consistent with
an osteosarcoma secondary to Paget’s disease of the pelvis. -
Most occur at age <30 (~85%)
-
Second peak age >55; often secondary osteosarcomas (e.g., Paget’s sarcoma or postradiation sarcoma)
P.179 -
-
Classic secondary osteosarcomas represent 5% to 7% of all osteosarcomas; usually with worse prognosis.
-
Definition: osteosarcomas that occur in
relation to previous exposures or procedures as well as in the presence
of other primary diseases -
Paget’s osteosarcoma (Fig. 6.1-2)
-
Most common of the “secondary osteosarcomas”
-
Estimated 1% of Paget’s patients may develop osteosarcoma
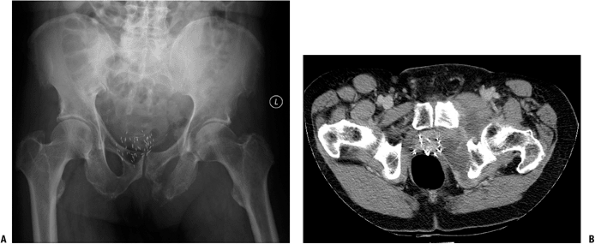 Figure 6.1-3 (A)
Figure 6.1-3 (A)
Plain anteroposterior radiograph of the pelvis shows a destructive
lesion of the left inferior pubic ramus. Note the metallic seeds
previously placed for treatment of prostate cancer in combination with
external-beam radiation 8 years prior. (B)
Axial CT image shows bony destruction and soft tissue mass extending
from pubic ramus. With the patient’s history, biopsy confirmed the
diagnosis of postradiation osteosarcoma. -
Majority in polyostotic Paget’s, although they do occur in monostotic disease
-
Reports as high as 5% of polyostotic symptomatic patients
-
-
Postradiation osteosarcomas occur in bone that is in a previously irradiated field (Fig. 6.1-3).
-
Usually >3 years after exposure
-
May occur decades after treatment for other malignancies or after high-dose exposure
-
-
-
Disease-associated osteosarcomas
region of long bones. They may be located within the bone or on the
surface of the bone. If untreated, osteosarcomas will continue to grow,
with local destruction of bone and extension outside the bone into the
surrounding soft tissues. The physis and articular cartilage may act as
a relative barrier to tumor extension, but epiphyseal or
intra-articular extension is still seen frequently.
-
Osteosarcomas, as with all sarcomas, usually metastasize hematogenously.
-
Lymph node metastases are not common and usually present only very late in the course of metastatic disease.
-
15% to 20% of patients present with metastases at time of diagnosis.
-
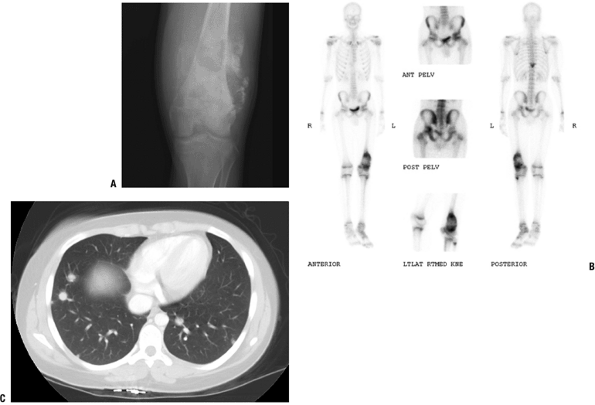
Most common site of metastasis: lungs (Fig. 6.1-4)
-
Second most common: bone
-
-
Skip lesions: distinct smaller areas apart from primary tumor within same bone
-
Prognosis: same as or worse than distant metastases (lung or bone)
-
-
Occurs most commonly due to respiratory
failure secondary to widespread pulmonary metastases, but also due to
other sequelae of tumor burden-
Superior vena cava obstruction
-
Pneumonia
-
Hemorrhage into tumor
-
Sepsis
-
Chemotoxicity (1% to 5%)
-
osteosarcoma, and central high-grade osteosarcoma represent the
majority of osteosarcomas (up to 75% in some series). Variants of
osteosarcomas exist that present differently, have unique radiographic
and histologic characteristics, may be treated differently, and may
convey a worse or better prognosis than conventional osteosarcoma. It
is important that these differences are identified and understood so
that correct diagnosis and treatment may be rendered.
 |
|
Figure 6.1-4 A 16-year-old boy with distal femoral lesion. (A) Plain radiograph shows abundant bone production and soft tissue extension strongly suggestive of an osteosarcoma. (B) Whole-body Tc-99 bone scan reveals a lesion of the ipsilateral acetabulum and thoracic spine. (C) CT axial image of the chest also reveals multiple pulmonary metastases.
|
spindle cell sarcomatous stroma with malignant osteoblasts that produce
malignant osteoid or bone. The tumor cells are typically anaplastic
(less differentiated), may show marked atypia and pleomorphic (widely
variable) nuclei, and may show many and/or bizarre mitoses. There may
be areas of osteoblastic (osseous), fibroblastic (fibrous), or
chondroblastic (cartilage) appearance, but if there is the presence of
malignant osteoid (wavy, lace-like, uncalcified bone matrix produced by
malignant osteoblasts), the diagnosis of osteosarcoma is made
regardless of the associated areas.
-
The grade of an osteosarcoma is used to:
-
Plan treatment: low-grade sarcomas are not treated with chemotherapy
-
Predict prognosis: low-grade osteosarcomas are less likely to develop metastases
-
-
Most osteosarcomas are high-grade tumors.
-
Low- and intermediate-grade osteosarcoma variants do exist (Box 6.1-1).
-
Most osteosarcomas are stage IIB
(high-grade and extracompartmental Enneking/Musculoskeletal Tumor
Society Staging System) at presentation. -
Patients with lung and/or bone metastases are considered MSTS stage III and have the worst prognosis.
-
15% to 20% of osteosarcomas have metastases (stage III) at presentation.
-
orthopaedic surgeon. The important factors to consider in making the
diagnosis of osteosarcoma follow.
-
Age
-
Most commonly occur in the second decade of life
-
Second peak in middle to late adulthood, usually from secondary osteosarcomas
-
-
Location
-
Distal femur (most common) > proximal tibia > proximal humerus
-
Metaphysis > diaphysis
-
Proximally in limb more common than distally
-
Pelvis and other flat bones (e.g., scapula) less frequently
-
Can occur in any bone
-
-
-
Symptoms
-
Pain is by far the most common complaint.
-
Pain gradually worsening, though may be intermittent or increase with activity
-
Pain is usually present for weeks to months, not acutely.
-
Red flags
-
Pain present or worse at night
-
Pain that is worsening despite treatment
-
Pain at rest
-
Pain without history of trauma
-
Antecedent pain, but worsened with minor injury
-
-
-
-
Low Grade
-
Parosteal
-
Low-grade central
-
Intermediate Grade
-
Periosteal
-
High Grade
-
Conventional
-
Telangiectatic
-
Small cell
-
Postradiation
-
Pagetoid
-
High-grade surface
-
Most common presentation is a tender mass about the knee.
-
Mass is firm and fixed to bone, nonmobile.
-
Warmth may be present.
-
Fusiform swelling of extremity
-
Dilated (ectatic) subcutaneous veins (large tumors)
-
Tenderness is usually present to palpation, with range of motion, and with weight bearing.
-
-
If pathologic fracture: antecedent pain is more worrisome for malignant pathologic fracture than if no prior pain.
-
There is no blood test for osteosarcoma.
-
Erythrocyte sedimentation rate (ESR) and
C-reactive protein (CRP) may be ordered to help distinguish from
osteomyelitis/infection. -
Calcium and alkaline phosphatase are usually normal.
-
Complete blood count usually normal, except with advancing disease
-
Elevated white count unusual, may suggest infection
-
Worse prognosis in osteosarcoma if elevated at time of diagnosis:
-
Serum lactate dehydrogenase (LDH)
-
Serum alkaline phosphatase
-
-
The typical findings seen on plain films
of an osteosarcoma are usually destructive lesions within the
metaphysis most common; surface osteosarcomas also occur. -
Evidence of malignant bone production, which appears as radiodensities within the lesion, adjacent to areas of lucency as well.
-
Usually cortical destruction with a soft tissue mass extending outside the normal contour of the cortexP.182
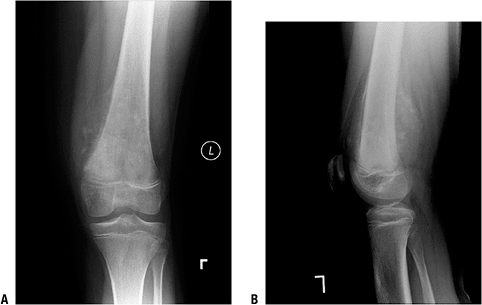 Figure 6.1-5 An 11-year-old girl with knee pain and distal femur mass. (A)
Figure 6.1-5 An 11-year-old girl with knee pain and distal femur mass. (A)
Anteroposterior radiograph shows the classic signs of an osteosarcoma.
Note the destructive, bone-forming lesion of the distal femoral
metaphysis. A Codman’s triangle is seen at the superior–medial
periosteal border. (B) In a lateral
radiograph of the distal femur lesion, the soft tissue extension is
more clearly seen, as is the bone formation within the tumor. -
“Codman’s triangle”: elevation of the
periosteum at the periphery of the soft tissue mass that forms a
radiodense triangle along the outer surface of the cortex (Fig. 6.1-5) -
“Sunburst pattern” seen with some osteosarcomas
-
Variants of osteosarcoma exist, each with typical plain radiographic findings.
-
-
Up to 75% of all osteosarcomas
-
Most common distal femur, proximal tibia
-
Typical findings of osteosarcoma
-
Malignant bone production within lesion
-
Destruction of cortex with soft tissue extension (extracompartmental) and Codman’s triangle
-
-
0.4% to 12% of all osteosarcomas
-
Typically a permeative, destructive radiolucent lesion with little if any bone production (see Fig. 6.1-6)
-
Can be confused radiographically with aneurysmal bone cyst or giant cell tumor of bone
-
Careful biopsy is important, as this variant consists of large blood pools within tumor with often scant cellular lining.
-
Histologically may also be confused with aneurysmal bone cyst
 |
|
Figure 6.1-6 A 16-year-old girl with 5-month history of thigh pain. (A)
Lateral radiograph shows a radiolucent, permeative lesion of the distal diaphysis of the femur. There is a Codman’s triangle superiorly, and the large soft tissue extension can be seen posterior to the femur. Note the lack of ossification radiographically within the lesion and soft tissue extension. (B) T2-weighted, fat-suppressed axial image through the femur at the level of the lesion reveals a large soft tissue mass and fluid–fluid level within the mass. Biopsy of this lesion confirmed a telangiectatic osteosarcoma. |
-
Rare; about 1% to 4% of all osteosarcomas
-
Controversy: Are these “atypical Ewing sarcoma”?P.183
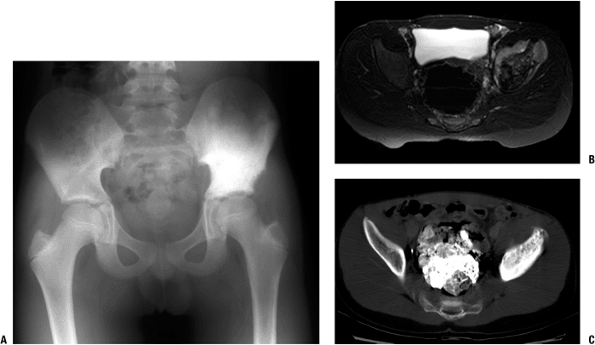 Figure 6.1-7 A 12-year-old boy with pain in the hip for 1 month. (A) Anteroposterior radiograph of the pelvis shows a radiodense supra-acetabular ilium on the left. (B) Axial T2-weighted, fat-suppressed MR image shows an infiltrative lesion with extension into the soft tissues. (C)
Figure 6.1-7 A 12-year-old boy with pain in the hip for 1 month. (A) Anteroposterior radiograph of the pelvis shows a radiodense supra-acetabular ilium on the left. (B) Axial T2-weighted, fat-suppressed MR image shows an infiltrative lesion with extension into the soft tissues. (C)
A CT axial image at the same level reveals a radiodense lesion. Biopsy
showed dense bone and nests of small, round blue cells. A diagnosis of
a small cell osteosarcoma was made. -
Age, location, and radiographic picture similar to conventional osteosarcoma
-
Typically has a destructive, permeative pattern, sometimes extends into diaphysis (Fig. 6.1-7)
-
On biopsy, there is often difficulty in
distinguishing this tumor from Ewing sarcoma and other small round cell
tumors if no osteoid is seen on biopsy. -
Usually has areas of osteoblastic activity, which helps distinguish it from Ewing sarcoma
-
1% to 2% of all osteosarcomas
-
Usually presents with pain
-
Older, typically third decade
-
Radiographic picture is variable, often radiodense (Fig. 6.1-8).
-
Often confused with fibrous dysplasia, or by progression or recurrence after treatment for suspected benign disease
-
Refers to osteosarcomas that occur in abnormal bone from other disease or after exposure to radiation
-
5% to 7% of all osteosarcomas
-
Many osteosarcoma case reports associated with other disease
-
Most common secondary osteosarcoma
-
Occurs in about 5% of patients with polyostotic Paget’s
-
Several thousand-fold increased risk of osteosarcoma in patients with Paget’s disease compared to the general population
-
Older patient population (55 to 85 years old)
-
Increasingly painful mass is most common presentation.
-
Flat bones; common, unlike conventional osteosarcoma due to frequent involvement of pelvis and scapula with Paget’s disease
-
Radiographs reveal destructive mass, usually with soft tissue extension in bone with Paget’s disease.
-
Usually 3 to 30 years after radiation
exposure most commonly from previous malignancy (e.g., breast cancer,
cervical cancer, Hodgkin’s, Ewing) -
Usually >4,000 cGy, with risk increasing as total radiation dose increases
-
Common in flat bones (scapula, pelvis, rib) as these more often exposed to radiation treatments for other malignancies
-
Radiographically similar to conventional osteosarcoma in a prior radiated bone
-
Multitude of case reports of osteosarcoma
diagnosed in the presence of other bone diseases, even in fracture site
or arthroplasty site. It is difficult to determine if these are
sporadic incidences (coincidences).-
Osteogenesis imperfecta
-
Fibrous dysplasiaP.184
![]() Figure 6.1-8 (A)
Figure 6.1-8 (A)
Anteroposterior radiograph of a 34-year-old woman with knee pain shows
a densely sclerotic lesion of the lateral femoral condyle. Biopsy
showed a low-grade central osteosarcoma. (B)
Anteroposterior radiograph of the distal femur of a 55-year-old woman
with a 1-year history of knee pain reveals a radiolucent, slightly
expansile, septated lesion. Biopsy also revealed a low-grade central
osteosarcoma. -
Chronic osteomyelitis
-
Osteopoikilosis
-
tumor that destroys cortical bone as it grows and extends into the
adjacent soft tissues. Osteosarcoma variants exist whose epicenter of
growth occurs at the surface of long bones. These surface sarcomas have
radiographic and clinical characteristics that can vary significantly
from those of conventional osteosarcoma. It is necessary to be aware of
these variants so that they are not confused with other bone tumors or
abnormalities.
-
Approximately 5% of all osteosarcomas
-
Most common surface osteosarcoma
-
Presents later than conventional: late second and third decades
-
Dull ache or pain may be present, but painless mass also may be presenting complaint.
-
Typically appears as a dense bony mass adjacent to the metaphyseal cortex of long bones (Fig. 6.1-9)
-
Distal posterior femur most common; proximal humerus second most common
-
Usually a “cleavage plane” between the
mass and the underlying cortex. Has a “stuck-on” appearance. It may
wrap around cortex, with invasion into bone only later. -
In contrast, the cortex of an
osteochondroma is continuous with the cortex of the involved bone and
the medullary canal of the bone is continuous with the medullary bone
of the stalk (pedunculated) or base (sessile) of the osteochondroma. -
Unlike conventional osteosarcoma, parosteal osteosarcomas are usually low grade, requiring surgery alone (no chemotherapy).
-
Dedifferentiated parosteal osteosarcoma
occurs when there is dedifferentiation of a portion of this tumor to a
high-grade sarcoma. In turn, the prognosis is worse if
dedifferentiation occurs.
-
-
1% to 2% of all osteosarcomas
-
Typically occurs on anterior surface of diaphysis of bone; tibia most common
-
Radiographically, a fusiform mass with lucency and ossification (Fig. 6.1-10)
-
“Sunburst pattern” of malignant bone can be seen.
-
Chondroblastic histology may predominate, but malignant osteoid is present.
-
Intermediate grade between parosteal and conventional
-
Up to 1% of osteosarcomas
-
Located on surface of bone
-
Otherwise identical to conventional osteosarcoma in histology, treatment, and prognosis
osteosarcoma, staging studies are required to determine the local and
distant extent of disease, prior to
biopsy. Biopsy of bone tumors without appropriate staging should not be
done, as it may jeopardize the ability to properly stage the
osteosarcoma.
 |
|
Figure 6.1-9 A 39-year-old woman with a several-year history of a slowly expanding mass in the popliteal fossa. (A)
Lateral radiograph shows a large ossified lesion at the posterior aspect of the distal femur. This was thought to be consistent with a parosteal osteosarcoma and was confirmed by biopsy. Resection of the distal femur was performed. (B) This lesion is adjacent to an intact posterior cortex. This can usually be distinguished from an osteochondroma as the cortices of the stalk of the osteochondroma are in continuity with the cortices of the bone itself. The medullary bone appears to flow out into the osteochondroma. |
-
Appropriate staging work-up must include:
-
History and physical
-
Plain radiographs (of entire bone with joint above and below)
-
Laboratory evaluation should include alkaline phosphatase and LDH.
-
Magnetic resonance imaging of entire bone is required to:
-
Determine the extent of the tumor intraosseously
-
Determine the anatomic relationship to adjacent structures
-
Nerves
-
Vessels
-
Joints
-
Soft tissue (e.g., muscles, skin)
-
-
At least one sequence of entire bone (preferably coronal T1 images) to rule out skip lesion in same bone (metastasis)
-
-
Whole-body bone scan
-
Uptake on scan of primary lesion is almost always present, but scan is to rule out other sites of disease.
-
May detect other sites of disease
-
May also show skip lesion in same bone
-
-
Computed tomographic (CT) scan of the chest
-
To evaluate for evidence of lung metastases
-
15% to 20% present with lung metastases
-
-
made, the grade and stage are determined. The grade and stage help to
direct treatment of patients with osteosarcoma. Current standard of
care involves the use of chemotherapy for high-grade osteosarcomas and
wide resection of the sarcoma in all patients. This resection can be
achieved by ablative surgery (amputation proximal to the extent of the
tumor) or with limb-sparing (limb salvage) surgery. When limb salvage
surgery is performed, skeletal defects must be reconstructed, unless
the tumor involves an expandable bone (e.g. the fibula).
staging studies, even with radical amputations, was in the range of 15%
to 20%. Without chemotherapy, it was likely that micrometastases not
detectable on routine imaging (chest CT scan, bone scan) progressed and
resulted in the later detection of disease despite the resection of the
tumor. Chemotherapy is used for the systemic treatment of patients with
osteosarcomas to eliminate these micrometastases. These patients are
treated in protocols that use multiagent therapies, which alone may
only slightly improve survival, but when used in combination have been
shown to significantly improve overall survival.
 |
|
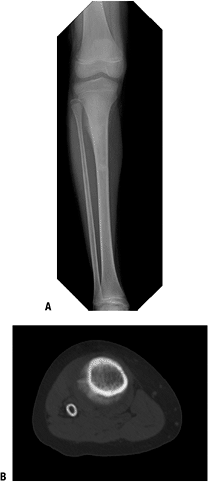
Figure 6.1-10 An 11-year-old boy with a 2-month history of pain. (A) Anteroposterior radiograph of the knee shows a lesion of the proximal metadiaphysis of the tibia. (B)
CT scan shows this periosteal lesion and bone production within the lesion. A biopsy of the lesion revealed a periosteal osteosarcoma. Approximately 60% of the lesion pathologically was chondroid, but areas of malignant cells producing osteoid were seen and the diagnosis of osteosarcoma was made. |
chemotherapy is given, followed by surgical treatment and then
postoperative chemotherapy to complete the protocol. The agents used
most commonly in the treatment of osteosarcomas and given in cycles
include doxorubicin (Adriamycin), cisplatin, high-dose methotrexate,
and ifosfamide.
usually involves preoperative chemotherapy, there has been no
randomized study that shows an increase in survival with neoadjuvant
chemotherapy followed by postoperative chemotherapy versus delivery of
all chemotherapy postoperatively.
toxicities can occur. These include mucositis, cardiomyopathy
(doxorubicin), alopecia, myelosuppression, nausea/vomiting, and
relative immunocompromise, sepsis, and rarely even death.
-
Medications used during chemotherapy treatment to minimize side effects
-
Granulocyte colony-stimulating factor (G-CSF; Neupogen)
-
Improves neutropenia by stimulating neutrophil production by marrow
-
Decreases infections and febrile neutropenias
-
-
Erythropoietin (Epogen) stimulates red blood cell production.
-
Dexrazoxane (Zinecard) protects against cardiomyopathy of doxorubicin.
-
Leucovorin rescues normal cells from effects of high-dose methotrexate and decreases myelosuppression and mucositis.
-
historical results of treatment of osteosarcoma by radiation therapy
were dismal. Currently radiation therapy should be reserved for
palliation only. Radiation therapy currently has no role in the
standard management of patients with nonmetastatic osteosarcoma.
agents in the treatment of osteosarcoma and its profound effect on
survival, complete surgical resection of the sarcoma is still required
for local control of the tumor. Historically, amputation was used for
the treatment of osteosarcoma. Currently 85% to 90% of osteosarcomas
are treated with limb salvage (limb-sparing) surgery. Current
literature does not demonstrate a difference in overall survival
between limb salvage versus amputation. However, an acceptable margin
of resection must be obtained, as incomplete excision will most likely
lead to recurrence, eventual metastasis, and death. The appropriate
margin for resection of an osteosarcoma is a wide (cuff of normal
tissue completely surrounds the tumor) margin. How thick the cuff of
normal tissue should be or how close the margins should be has not been
fully established. Tumor extending to the inked margin of resection
(positive margin) is not an adequate resection. Amputation may be the
safest oncologic treatment following initial resection with positive
margins.
limb salvage procedures. The most important goal of the surgical
treatment of osteosarcoma is complete (wide) resection of the tumor
with a wide margin.
-
For all nonmetastatic osteosarcomas, 60% to 70% 5-year survival rate
-
Important prognostic factors
-
Metastatic disease
-
Single most important factor in predicting survival
-
Patients who present with metastatic
disease, managed with chemotherapy and aggressive resection of distant
disease (i.e., thoracotomies), may have up to a 30% to 40% 5-year
survival rate. -
Patients who develop metastatic disease
after treatment also have a worse prognosis but with chemotherapy and
metastasectomy may achieve up to 15% to 20% survival rates.
-
-
Response to chemotherapy
-
Patients who have a good response to
chemo (>90% necrosis after examination of resected tumor) may have
up to a 90% 5-year survival rate. -
In high-grade osteosarcoma patients with no evidence of metastases, response to chemotherapy is the single most important predictor of prognosis.
-
-
Tumor grade
-
Patients with low-grade osteosarcomas
(parosteal and low-grade central) have a better prognosis than those
with high-grade osteosarcoma and approach a 90% survival rate with
appropriate management.
-
-
-
Subtypes of osteosarcomas also have a role in determining prognosis (Box 6.1-2).
-
Tumors with the poorest prognosis: chemotherapy is controversial as there is no documented benefit
-
Tumors with intermediate prognosis: controversies regarding chemotherapy exist, but most patients get chemotherapy
-
Better prognosis than conventional osteosarcoma: no chemotherapy used
-
-
Better Prognosis than Conventional Osteosarcoma
-
Parosteal
-
Low-grade central
-
Intermediate Prognosis (15% to 20% risk of metastases)
-
Periosteal
-
Equivalent Prognosis as Conventional Osteosarcoma
-
Telangiectatic
-
High-grade surface
-
Poorest Prognosis
-
Pagetoid
-
Postradiation
-
Small cell
-
Dedifferentiated