Subtrochanteric Fractures
proximal femur between the inferior aspect of the lesser trochanter and
a distance of about 5 cm distally. These fractures generally occur in
two patient age distributions: the young, high-energy, often
polytraumatized population, and the elderly osteopenic population,
typically resulting from a low-energy fall from a standing height.2,9
Fractures in the subtrochanteric region present challenges to achieving
stable fixation and appropriate reduction regardless of age. The
subtrochanteric region of the femur is one of the highest stressed
zones in the human skeleton where tensile or compressive stresses can
exceed several multiples of body weight. Additional challenges include
short proximal fragments which are deformed by the hip flexors and
abductors which may make accurate reduction and fixation challenging.
There are several internal fixation options for managing these
fractures that generally fall into two categories: some form of
intramedullary fixation or some form of plating. There are many
specific technical hurdles that must be overcome to ensure stable
proximal fragment fixation performed in a biologically friendly manner
and with accurate alignment and implant position.
Prioritization of other life-threatening injuries should occur first,
and the subtrochanteric fracture should be stabilized as early as
possible after appropriate resuscitation of the patient in order to
allow early mobilization and avoid the complications of prolonged
recumbency. In the elderly population, medical optimization is
recommended; however, associated injuries are relatively uncommon as
these typically result from a fall from a standing height.
Subtrochanteric fractures are relatively rare compared to
intertrochanteric fractures in the elderly. A relatively unique
fracture
pattern has been associated with bisphosphonate therapy. It is
typically transverse; at the metadiaphyseal junction, there are signs
of lateral cortical thickening and a medial cortical spike. Prodromal
symptoms were often present.15
life-threatening injuries utilizing standard advance trauma life
support protocols. The fractured limb is then examined with careful
circumferential examination of the skin to rule out an open fracture.
The neurovascular status of the limb should be documented, and any
areas of abrasion or other skin compromise should be evaluated as this
may change one’s surgical incision. Elderly patients should be
evaluated for ipsilateral upper extremity fractures and any head injury
or loss of consciousness, since subdural hematomas can occur with
surprisingly little impact.
provide enough information to guide the treatment of the vast majority
of subtrochanteric fractures. The length of the proximal fragment and
the diameter of the diaphysis distally should be evaluated. A traction
view may be helpful in defining fracture geometry and location. Careful
attention to any proximal fracture extent into the piriformis fossa,
greater trochanter, or involvement of the lesser trochanter can
influence the surgeon’s choice of implant. If there is any concern
about fracture extension into the piriformis fossa or the greater
trochanter, a computed tomographic scan can be obtained, or if one was
obtained during the trauma workup, it can be reviewed for any proximal
fracture lines.
 |
|
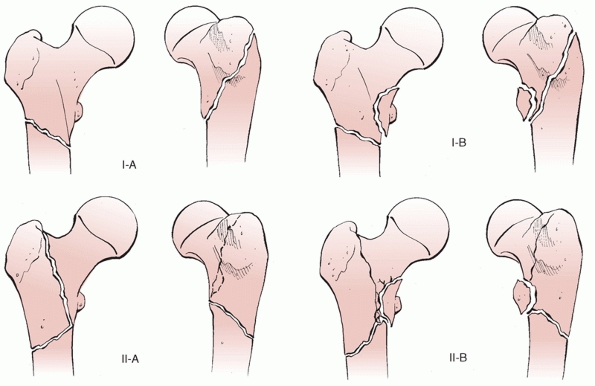
FIGURE 49-1
Russell-Taylor classification of subtrochanteric fractures. Note the emphasis on lesser trochanteric integrity and piriformis fossa extension. |
fractures. The authors find three to be generally useful in guiding
treatment. The Russell-Taylor classification38 (Fig. 49-1)
essentially guides the surgeon in determining the integrity of the
proximal fragment which historically has facilitated decision-making
regarding nail or plating choices. The classification is divided based
on whether the piriformis fossa is involved and whether the lesser
trochanter is involved. Previously, this information would guide
decision-making regarding standard locking of an intramedullary nail
from greater to lesser trochanter or the need for so-called
“reconstruction” nailing with cephalomedullary type fixation (Figs. 49-2 and 49-3).
Historically, with piriformis fossa extension proximally, plating
techniques were considered for fear of losing capture of the proximal
fragment with a piriformis fossa starting point nailing. Essentially,
the nail could “fall out the back” of the proximal fragment.2,13
With more contemporary nailing techniques that enter the tip of the
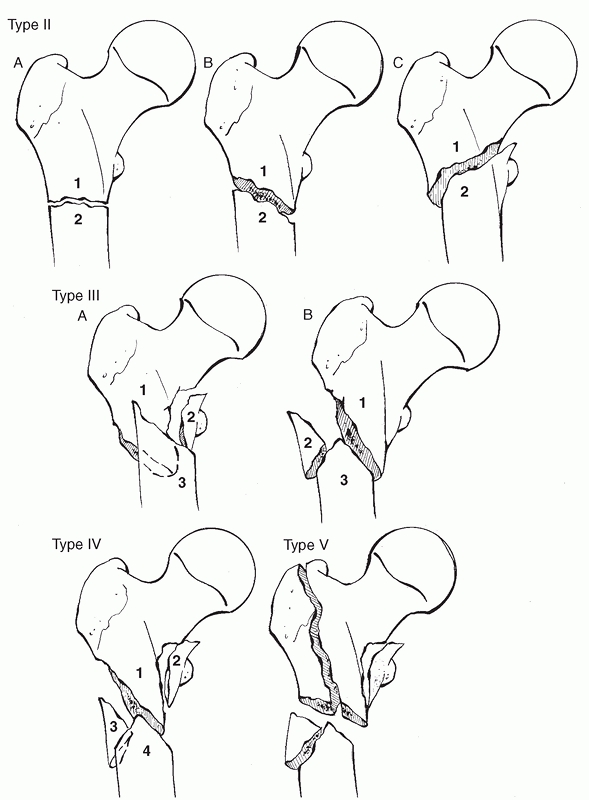
greater trochanter, these issues have become less problematic (see “Current Treatment Options”). The Seinsheimer classification40 (Fig. 49-4)
is more detailed but can also be useful as it grades fracture obliquity
and the extent of comminution in the subtrochanteric region. The
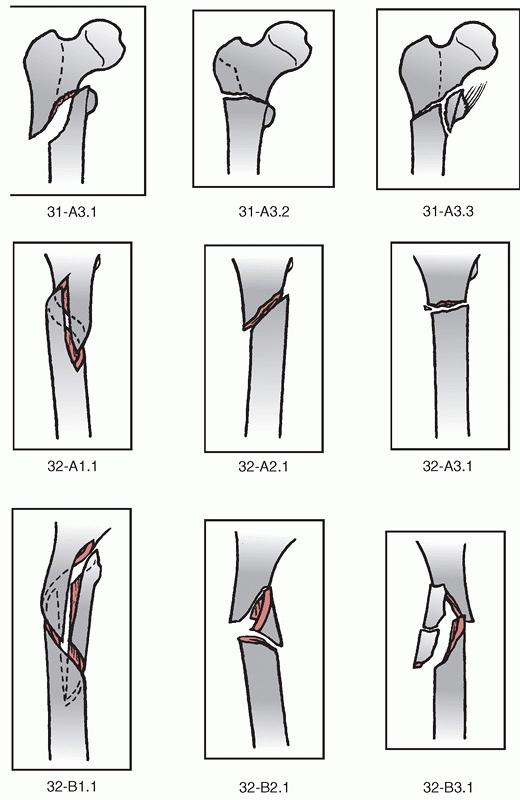
Orthopaedic Trauma Association classification11 (Fig. 49-5)
is also useful. The commonality to all classification schemes is that
they try to categorize fractures based on the integrity of the proximal
fragment, comminution, and fracture geometry to help the surgeon with
appropriate implant selection. With modern nailing techniques, however,
these classifications no longer influence a “nail versus plate”
decision, but may influence the locking configuration.
 |
|
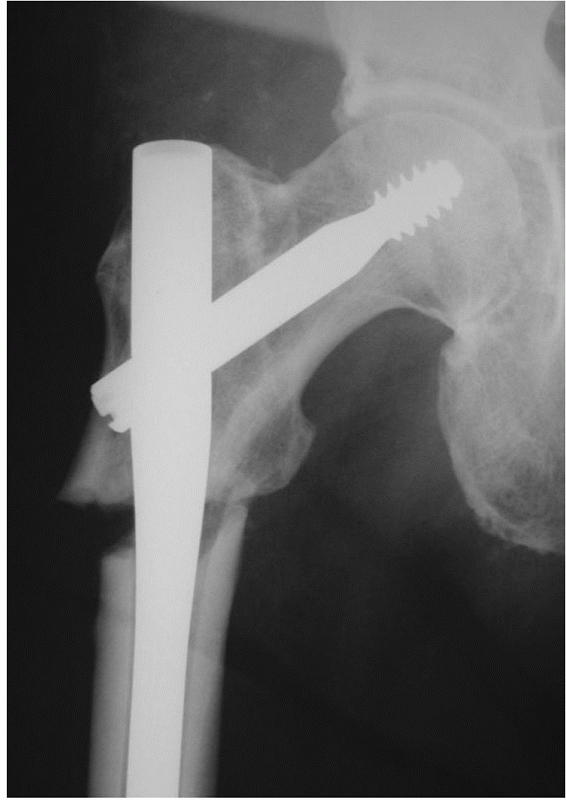
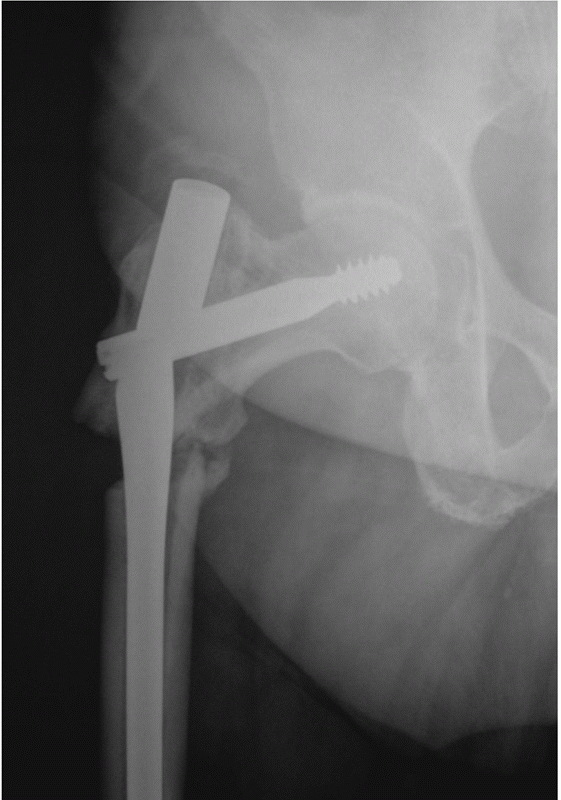
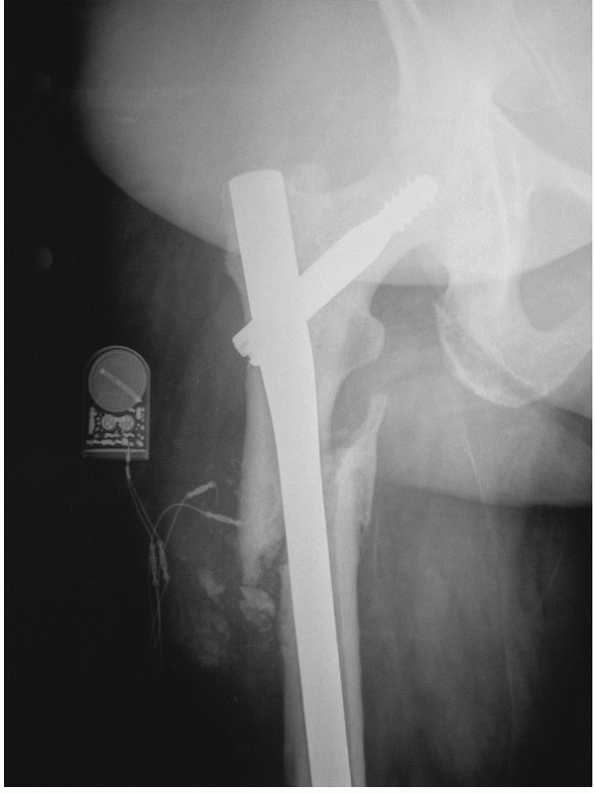
FIGURE 49-2
A segmental subtrochanteric fracture with an extremely short proximal fragment. Note the flexion, abduction, and external rotation of the proximal fragment. |
 |
|
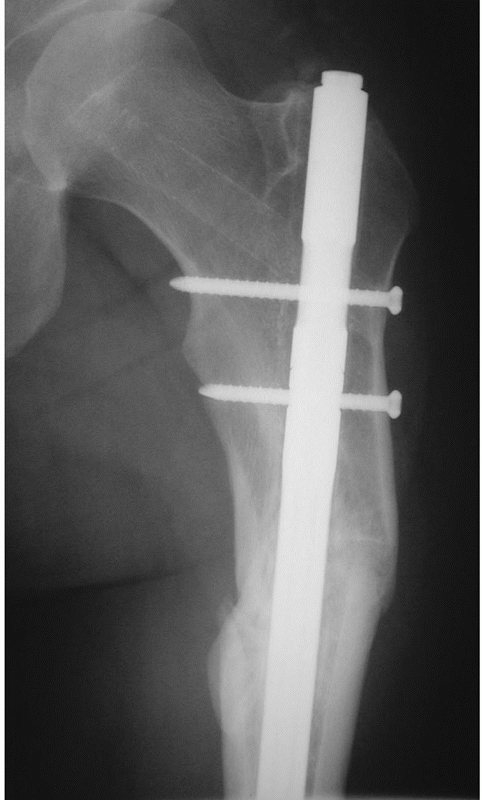
FIGURE 49-3
Postoperative radiograph demonstrating good reduction of both fractures. Due to the short proximal fragment a cephalomedullary device was chosen. |
 |
|
FIGURE 49-4
Seinsheimer classification of subtrochanteric fractures. Note the emphasis on fracture obliquity, comminution, and proximal extension. |
 |
|
FIGURE 49-5
Orthopedic Trauma Association classification of subtrochanteric fractures. (Redrawn from Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database, and outcomes committee. J Orthop Trauma 2007;21(10 Suppl):S32-36, with permission.) |
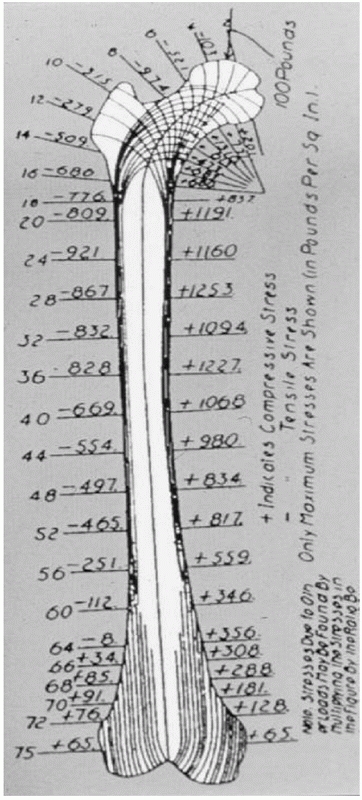
highest tensile and compressive stresses of any bone in the human
skeleton. Several multiples of body weight will challenge any fixation
construct (Fig. 49-6). Comminution in this area
often involves the medial cortex; therefore, the implant chosen must
withstand enormous compressive and tensile loads. Compressive forces in
the medial cortex can exceed 1200 lbs per square inch (in a 200-lb
person).22 The fixation constructs chosen, therefore, should be load-sharing and be able to withstand such multiples of body weight (Fig. 49-7).
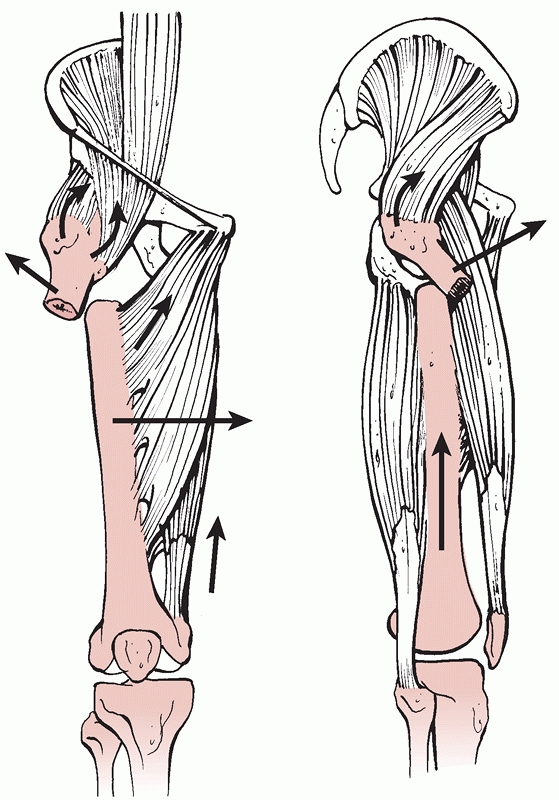
Additionally, the deforming muscular forces of short proximal fragments
can be problematic, especially when one is attempting either an
indirect reduction for a plating technique or a closed intramedullary
nailing technique. The proximal fragment is abducted by the abductor
mechanism, externally rotated and flexed by a combination of the short
external rotators and the iliopsoas tendon (Fig. 49-8).
Additionally, the femoral shaft distally is adducted and shortened by
the pull of the adductors and quadriceps mechanism. This essentially
moves the tip of the trochanter and the piriformis fossa away from the
surgeon and flexes the proximal fragment. These deformities must be
overcome and controlled in order to allow accurate reduction and avoid
varus. Varus alignment can increase the stresses in compression on any
internal fixation construct by changing the trajectory of
weight-bearing forces across the femoral neck. For example,
theoretically, a proximal fragment aligned with a neck shaft angle of
100 degrees will likely experience more compressive stresses on its
medial cortex than a proximal fragment aligned in 135 degrees. The
relationship between the tip of the greater trochanter and the center
of the femoral head should be evaluated during reduction and internal
fixation. If this relationship is coplanar, then in general the
neck-shaft angle will be in its normal anatomic location for that
particular patient, and varus can be
avoided.
An anteroposterior view of the pelvis will allow assessment of the
contralateral neck shaft relationship, which may assist evaluation of
appropriate alignment.
 |
|
FIGURE 49-6 Koch’s diagram showing the magnitude of the compressive stresses medially and the tensile stresses laterally.
|
formal surgical dissection is necessary. The technique is discussed in
the section below on intramedullary stabilization. With regard to
plating techniques, or if open reduction is necessary during
intramedullary nailing, the most common surgical approach is a direct
lateral approach to the proximal femur. A direct lateral incision is
made over the flare of the trochanter and deepened in through the
subcutaneous tissue and the fascia lata. The vastus lateralis is
elevated from its attachment on the lateral femur, and the
intermuscular septum and perforators are coagulated with
electrocautery. It is important to note that medial dissection over the
femoral shaft should be avoided as this is the main location of the
blood supply to the subtrochanteric region and devitalizing this area
by excessive dissection may contribute to delayed union or nonunion.
 |
|
FIGURE 49-7
A highly comminuted subtrochanteric fracture with a very short proximal fragment. Any implant chosen to stabilize this fracture must withstand substantial forces. |
 |
|
FIGURE 49-8
The typical deforming muscular forces cause the proximal fragment to be flexed by the iliopsoas, externally rotated by the short rotators, and abducted by the abductors. The femoral shaft is shortened and adducted by the adductors and quadriceps. |
indicated for the most infirm, moribund patients where surgical
intervention is impossible. For example, a nonambulatory demented
patient with fixed contractures and prohibitive medical comorbidity.
Again, the vast majority of cases should be treated with some form of
internal fixation to avoid the morbidity of prolonged recumbency.
of plating. Given an understanding of the substantial forces across any
fixation construct used to stabilize the subtrochanteric region of the
femur, it is clear that an intramedullary implant with a shorter lever
arm on the proximal fixation and load-sharing characteristics would be
the preferred implant in the vast majority of subtrochanteric
fractures. Plating techniques, however, can be useful for extremely
short proximal fragments and in certain situations such as delayed and
nonunion. Our discussion, therefore, will focus on these two general
categories of stabilization methods.
stabilization of polytraumatized patients, but it is generally not
recommended for definitive treatment.14
Arthroplasty may have a role in pathologic fractures due to neoplasm
with extensive proximal fragment involvement or for multiply operated
nonunions, but, in general, has no role in acute, nonpathologic
fractures.
techniques for the stabilization of subtrochanteric fractures have
already been discussed. A nailing technique should be chosen for the
overwhelming majority of subtrochanteric fractures for those reasons.
In general, the surgeon needs to make three major decisions when
nailing subtrochanteric fractures. The first decision is whether the
starting point should be in the piriformis fossa or in the tip of the
greater trochanter. Good results have been described with both
treatment techniques,35,42
and the quality of reduction is probably more important than whether a
trochanteric or piriformis starting point is chosen. It is far easier
to locate the starting point on the tip of the greater trochanter since
it is more lateral and the entry trajectory is more lateral as well.
Additionally, piriformis fossa involvement is not a contraindication
for greater trochanteric nailing. The starting point decision is based
on surgeon preference and accuracy of starting point placement;
regardless of philosophy it is critical to obtaining and maintaining
fixation and alignment of the proximal fragment.
locking in a standard “greater to lesser” trochanteric fashion with a
single locking screw or whether to place locking screws into the
femoral head and neck, the so-called “reconstruction” or
“cephalomedullary” nailing. The decision to use a single greater to
lesser locking screw or a cephalomedullary locking configuration should
be made based on the integrity of the proximal fragment (i.e.,
involvement of the lesser trochanter or extension of a fracture line
proximally) and bone quality. If the proximal fragment is intact and
the fracture is completely below the lesser trochanter, then a standard
antegrade nail with a greater to lesser trochanter single locking screw
will likely be adequate (in the authors’ experience, this situation is
quite rare). If comminution exists, if there is any concern about the
integrity of the proximal fragment (lesser trochanteric or proximal
involvement), or in elderly patients with osteopenic bone, the authors
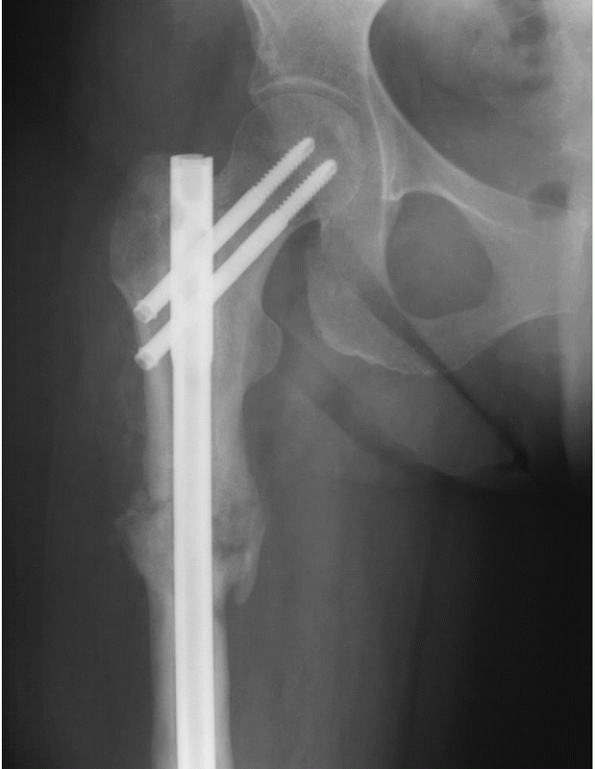
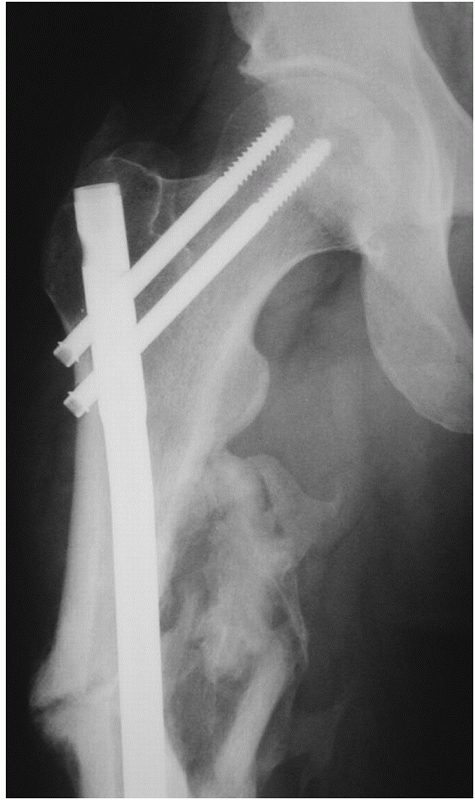
recommend cephalomedullary fixation (Fig. 49-9).
If cephalomedullary nailing is chosen, the third decision involves
whether a single large central lag screw (such as in a Gamma-type
nail), or two smaller diameter screws (such as in the standard
reconstruction type nail) should be selected. Most reconstructionnails
have a 13-mm proximal diameter, while Gamma-type devices are 16 to 17
mm in diameter. In general, for young patients with excellent bone
quality, the authors prefer two reconstruction type screws into the
femoral head since these nails have smaller proximal diameters and
probably cause less abductor damage.8
For older patients, one large central lag screw may provide better
purchase due to the larger surface area a large lag screw provides.
Also, this effectively “protects” the femoral neck as insufficiency
fractures after nailing have ben reported.21 A biomechanical study by Roberts et al.36
demonstrated that if comminution existed, then a single large lag screw
device was stiffer than a reconstruction type nail with two smaller
screws; however, the clinical performance of one versus two
cephalomedullary screws have not been studied in equivalent populations
(Figs. 49-10 and 49-11).10
 |
|
FIGURE 49-9 Intramedullary fixation of a subtrochanteric fracture with a so-called cephalomedullary or “reconstruction” nail.
|
 |
|
FIGURE 49-10 A comminuted reverse obliquity subtrochanteric fracture.
|
 |
|
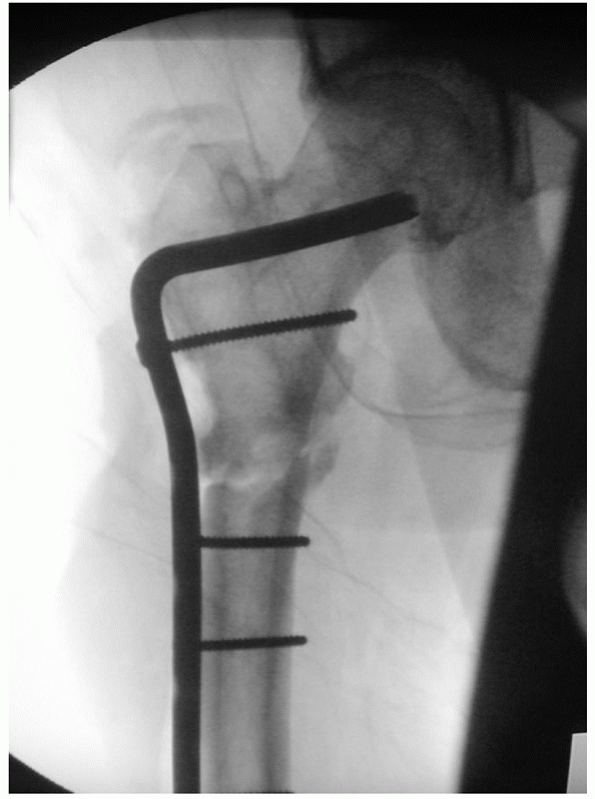
FIGURE 49-11
Fixation with a cephalomedullary device. Note the slight varus malalignment. This is common when the medial cortex below the lesser trochanter is comminuted since there is no surface to deflect and contain the nail. |
fractures, especially those with very short proximal fragments that can
be extremely difficult to nail due to limited nail containment and
difficulty with reduction. Several categories of plates can be useful
ranging from a traditional sliding hip screw or dynamic condylar screw
or 95-degree condylar blade plate. The obliquity of the fracture should
be evaluated carefully if a plating strategy is chosen. For so-called
reverse obliquity and transverse patterns, sliding hip screws should
not be used as proximal fragment lateralization is uncontrolled and
fixation failure has been reported. A 95-degree angled blade plate or a
locking plate are better choices as they resist these proximal
lateralizing forces. More recently, anatomically precontoured proximal
femoral locking plates have been developed to facilitate fixation of
such short fractures; however, limited data is available documenting
their efficacy to date. The common features of any plating technique
include the need for a relatively large dissection and the fact that
plating must be done in a biologically friendly manner (discussed
below) to allow relatively rapid healing.2,5,18,20,24,25,29,32,39
Plates are inherently biomechanically inferior to nails because of
their more lateral position (longer lever arm on the proximal fixation)
and their nonload-sharing characteristics, therefore it is critical
that a biologically friendly (indirect reduction) technique be chosen
for their implantation.
available of the entire length of the femur. The authors prefer to
carefully evaluate the integrity of the proximal fragment (proximal
fracture extension or lesser trochanteric involvement), the bone
quality of the proximal fragment, the obliquity of the fracture, and a
diameter of the femoral diaphysis distally since some cephalomedullary
devices come in certain minimum diameters. The lateral view can also
alert the surgeon to the degree of femoral bowing which may influence
device selection. In extremely osteopenic patients, the authors will
generally choose a cephalomedullary device with a single large lag
screw. In younger patients with short proximal fragments, a
reconstruction type nail with two smaller locking screws is chosen.
prefer to position patients supine on a fracture table with the
involved leg in a traction boot and the other leg carefully placed in
the lithotomy position. Although the procedure can be performed without
a fracture table if enough surgical assistants are available, the
authors have found that the use of a fracture table greatly facilitates
obtaining a clear proximal lateral fluoroscopic radiograph, especially
in heavy patients, and allows the surgeon to fine-tune the reduction,
leg length, and alignment and hold it in place during the nailing
procedure. Some have advocated the lateral position to facilitate
starting point location and reduction by flexing the distal fragment to
“match” the proximal deformity. This may be of benefit in heavier
patients. The lateral position, however, may not be practical in
polytraumatized patients with chest tubes, spine injuries, or other
extremity fractures.
nailing. The authors prefer to take a guide pin from the nail set
chosen and place this along the skin laterally, proximal to the greater
trochanter to determine the appropriate trajectory and skin entry site
in order to obtain entry into the tip of the greater trochanter. Once
this trajectory is known, then a stab incision is made in the proximal
gluteal area. The incisions required to get the appropriate trajectory
can be surprisingly proximal.
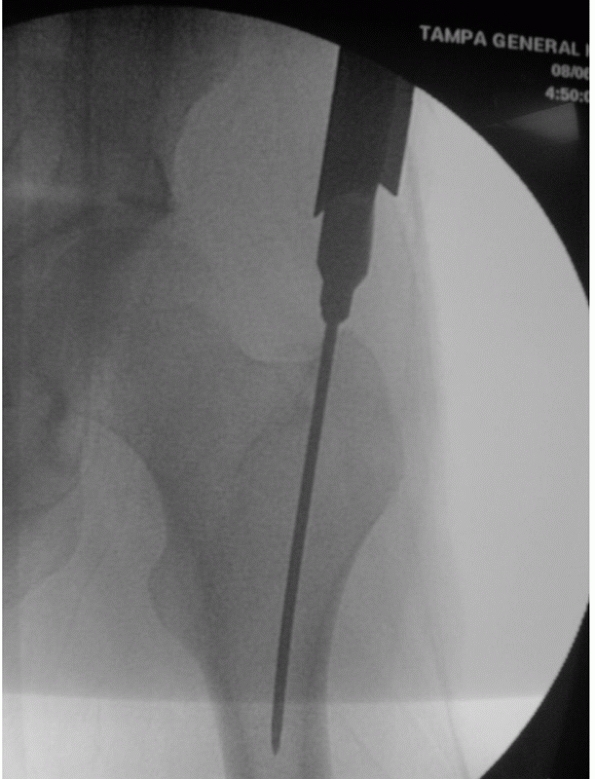
a guide pin is placed down to the tip of the trochanter. The authors
prefer to treat these fractures with a starting point in the tip of the
greater trochanter. The guide pin is placed into the tip of the
trochanter or just a few millimeters medial (Fig. 49-12).30
It is very important not to start even a tiny bit lateral to the tip of
the trochanter since this will generally tend to move the starting
point further laterally with canal preparation and may result in
excessive varus of the proximal fragment (Fig. 49-13).
The guide pin is placed in the proximal fragment, and the appropriate
starter reamer is passed using soft tissue protection sleeves. The
guide pin is placed across the fracture. For “low” subtrochanteric
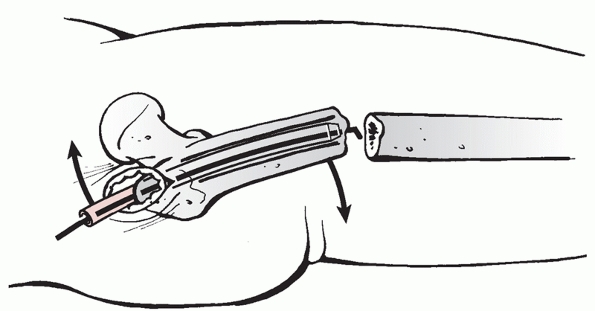
fractures that have some intact diaphysis, reduction tools (“fingers”)
can be used to assist with guide wire placement (Fig. 49-14).
These maneuvers are useless if the proximal fragments are short and
capacious. Appropriate measurements are taken. It is important not to
run the reamers until the reamer head is well inside the proximal
fragment. This will avoid excessive reaming of the starting hole, which
can lateralize the entry
angle
(essentially making the starting hole an oval). Reaming is performed
and a nail is inserted in the usual fashion. The authors select a nail
1 to 2 mm smaller than the reamer that provided first “chatter” in the
diaphysis. Nail length is chosen based on surgeon preference. The
authors routinely use long nails and lock them statically distally.
Locking screw fixation is placed into the femoral head or neck or into
the lesser trochanter based on the indications discussed above. True
lateral fluoroscopic projections are used to guide center placement of
cephalomedullary fixation. Practically speaking, the authors routinely
choose some form of cephalomedullary fixation for these fractures since
it is quite difficult to rule out any proximal fracture extensions and
fixation of the femoral head and neck essentially avoids any potential
problems with nail containment. Most modern nailing systems allows
standard (“greater to lesser”) or cephalomedullary locking with the
same implant (Fig. 49-15).
It should be carefully noted that a “high” subtrochanteric fracture
should never be reamed in an unreduced position. If the patient is
positioned on the fracture table, gentle traction is applied and
significant deformity is still noted in the proximal fragment, then the
author will typically attempt some simple percutaneous technique to try
to reduce the proximal fragment. This can involve either a ball spike
pusher placed from anterior to posterior, some form of joystick such as
a Shanz pin placed in the lateral cortex, or more commonly, a very
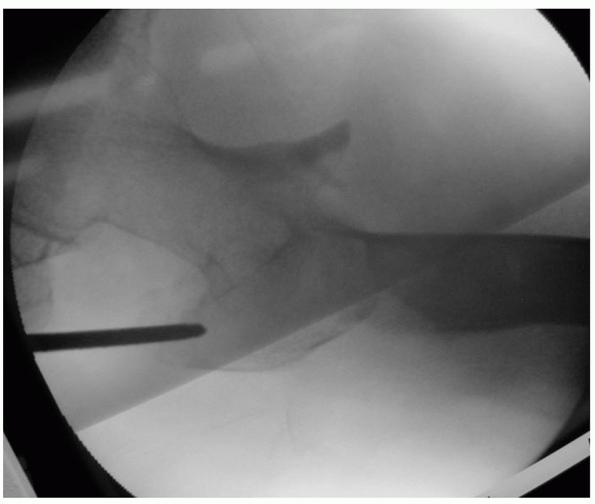
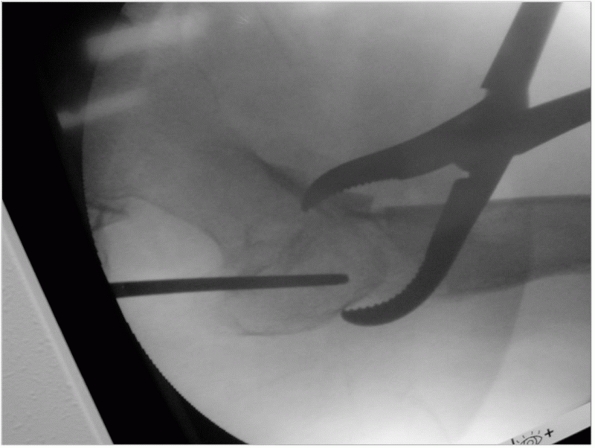
small incision placed over the lateral femur. A percutaneous clamp is
placed (Fig. 49-16). The proximal fragment is
then reduced, moving it into an extended and adducted position and an
internally rotation position. This “reversal” of the deforming forces
essentially moves the tip of the greater trochanter (or piriformis
fossa) into an ideal position for a starting point, and a starting
point can be made in an accurate fashion. Many different instruments
can achieve the reduction; however, the authors prefer a percutaneous
clamp since it can be repositioned easily (unlike a Shantz pin) and
typically will not slip easily (like a ball pike pusher). Additionally,
a clamp typically does not require an assistant to constantly hold it
in a reduced position. If one reams the fracture in an unreduced
position, it will remain unreduced after the nail is passed since there
is no “reducing effect” of passing the nail, unlike the situation when
reaming a diaphyseal femoral fracture. This typically results in a
proximal fragment that is left in varus, external rotation, and flexion
(Fig 49-17), which is a difficult deformity to
manage. One should remember that it is better to make a small incision,
use an adjunctive reduction maneuver, and nail the fracture in a well
aligned position than to perform a percutaneous malunion in a
biologically friendly manner (Figs. 49-18, 49-19, 49-20, 49-21, 49-22, 49-23 and 49-24).
It is also important to note that small incisions to improve reduction
should not be equated with large incisions with excessive stripping,
evacuation of the fracture hematoma, and broad blunt retractors used to
reduce the fracture under direct vision. This is not recommended since
it will devitalize the tissues and may contribute to delayed union and
nonunion. Cerclage cables should generally be discouraged; however,
they can occasionally be useful for supplemental fixation of long
spiral or long oblique patterns since nailing these patterns can often
leave them distracted (“sprung open”). The entire construct is checked
under fluoroscopic biplanar evaluation to ensure that excellent
fixation and appropriate implant position and length are achieved. The
distal femur is evaluated fluoroscopically, especially the lateral view
in elderly patients with osteopenia and bowed femoral shafts. The
wounds are then irrigated and closed in layers in the usual fashion.
The authors typically lock all nails distally with two distal locking
screws since the forces the implant will experience can be quite high.
 |
|
FIGURE 49-12
The ideal starting point for a trochanteric entry nail. Note the guide wire just slightly medial to the exact tip of the greater trochanter and the wire passing in the center of the femoral canal distally, not into the medial cortex. |
 |
|
FIGURE 49-13 Varus malreduction resulting from a starting point far too lateral on the greater trochanter.
|
 |
|
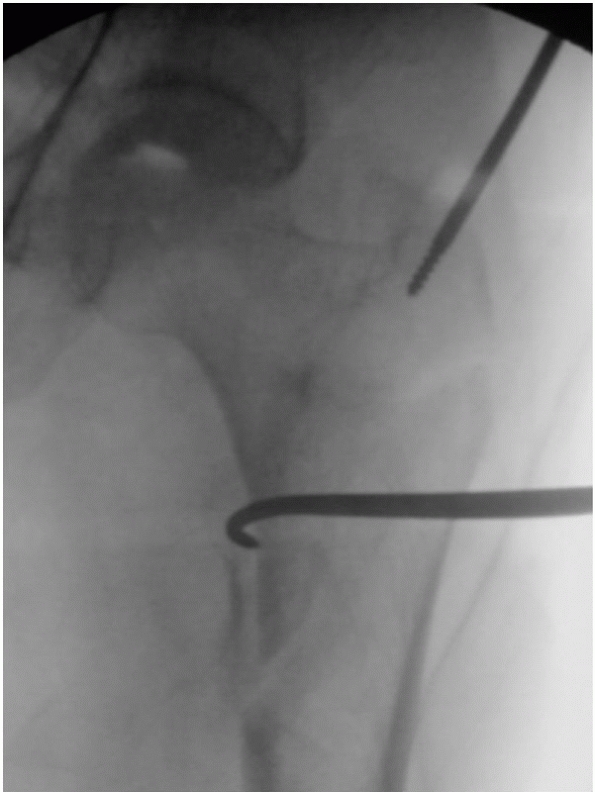
FIGURE 49-14
Küntscher technique to reduce the flexion deformity of proximal fragments. For this to be effective, there must be enough proximal fragment length to control the fragment with the reduction tool; therefore, it is primarily useful for relatively “low” subtrochanteric fractures. |
 |
|
FIGURE 49-15
Most modern nailing systems offer multiple locking options through the same nail so that the surgeon can decide after nail seating whether a standard greater to lesser trochanteric lock, a cephalomedullary lock, or some combination of the two is appropriate for the fracture pattern. |
 |
|
FIGURE 49-16
A clamp used to reduce and hold a short proximal fragment. Note the position of the greater trochanter and the slightly adducted proximal fragment. This maneuver greatly facilitates accurate starting point placement in very short, deformed proximal fragments. |
 |
|
FIGURE 49-17
The typical deformity noted when a subtrochanteric fracture is reamed and nailed without good reduction. The starting point is too lateral on the trochanter, the fragment is therefore in varus; the lesser trochanter is very visible indicating external rotational malalignment, therefore the fracture cannot “key in” and remains distracted. |
 |
|
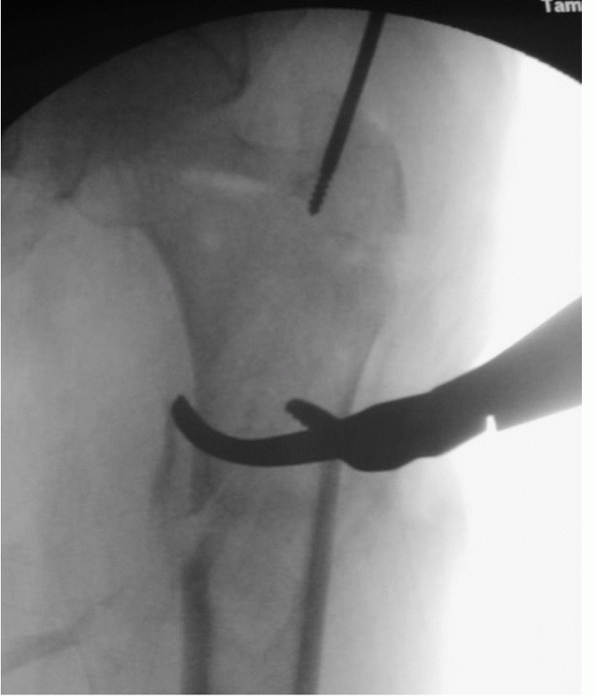
FIGURE 49-18
Lateral fluoroscopic view demonstrating persistent flexion deformity. Reaming a fracture in this position and passing a nail will not reduce the deformity. Intramedullary reduction maneuvers will also fail to control the capacious proximal fragment. |
 |
|
FIGURE 49-19 Note the improvement in the lateral plane reduction and the more accurate starting trajectory.
|
 |
|
FIGURE 49-20 A bone hook used to percutaneously reduce the residual flexion deformity.
|
 |
|
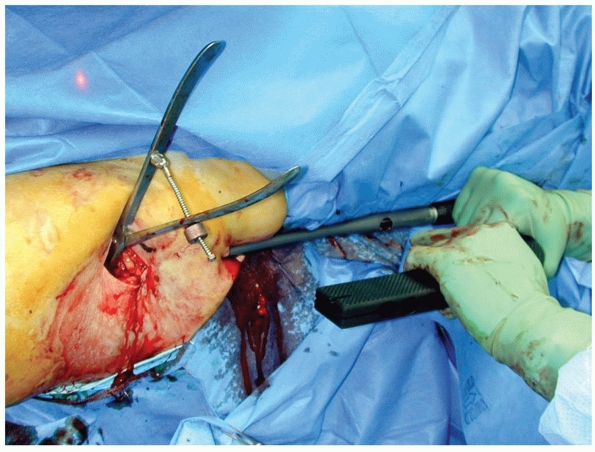
FIGURE 49-21 Alternatively, a percutaneously applied reduction clamp can hold the reduction during reaming and nail passage.
|
 |
|
FIGURE 49-22
A clinical photograph of the percutaneous clamp in place during nail passage. Note that this is not a large incision, and no deep retractors are used to avoid periosteal stripping. |
 |
|
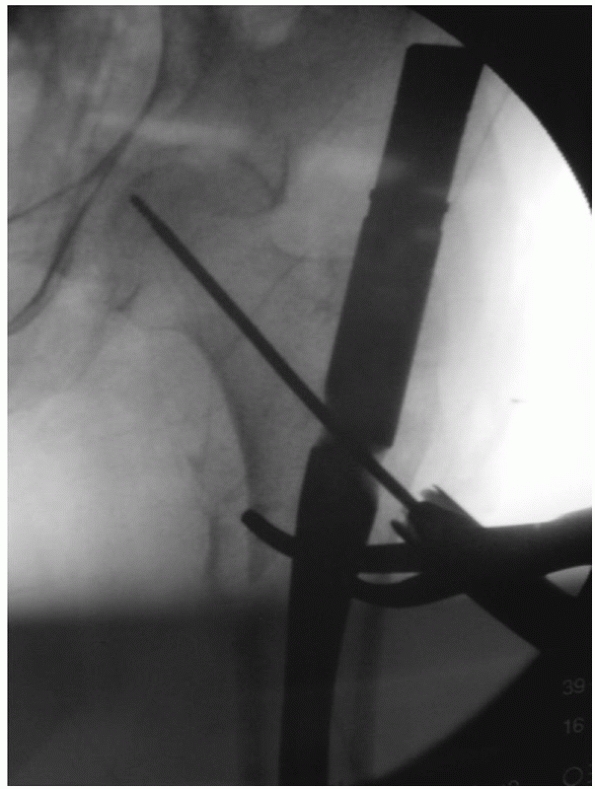
FIGURE 49-23 Nail passage with the reduction clamp in place.
|
antibiotics and thromboembolic prophylaxis per surgeon preference. The
patients are mobilized on the first postoperative day and allowed to
weight bear as tolerated with gait aids. The authors
recommend
two arm (crutches or a walker) support for 6 to 12 weeks, depending on
fracture geometry and bone quality. Radiographs are obtained at the 6-
and 12-week mark, and the patients are followed until union which
should be noted by the 4-month mark.
 |
|
FIGURE 49-24
Proximal fixation with excellent alignment of the neck shaft angle and good central guide pin placement. The reduction clamp is still in place. |
fractures with very short proximal fragments and for nonunions and
malunions.
fracture table as discussed previously. A direct lateral approach is
made over the flare of the trochanter deepened through the skin,
subcutaneous tissue, and fascia lata. The vastus lateralis is elevated
in a submuscular fashion from its origin on the vastus ridge and the
lateral femur. The surgeon should be careful to avoid any broad tipped
(Bennett type) retractors medially, and if possible, no medial
dissection should occur at all. It is important that any plating
technique involve as much “indirect” reduction as possible. Typically,
manipulation of the proximal fragment can be performed with simple
clamps or joysticks, avoiding large broad-based circumferential
clamping techniques which may further strip soft tissues. All modern
plating techniques share several common principles. The proximal
fixation must be placed accurately into the femoral head, for example,
when using a blade plate, a dynamic hip screw, a dynamic condylar
screw, or even a locking proximal femoral plate. The plate on the
proximal fragment is then reduced to the shaft and this should afford
an excellent reduction of the proximal fragment. This “self-aligning”
indirect reduction technique is predicated on absolutely accurate
positioning of the fixation in the proximal fragment (Fig. 49-25).
The neck shaft angle will be accurately restored only if the proximal
fixation is accurately placed. Preoperative templating can facilitate
accurate placement. Compression is then typically achieved with an
articulating tension device or other clamp-based techniques to avoid
distraction, and side plate screws are placed in the usual fashion. Due
to the inherently unfavorable biomechanics when using plates in this
anatomic region, it is important that compression be obtained so that
the bone can bear some load as well. Essentially, acute compression
makes the construct more “load sharing.” The specific surgical
techniques for implanting any plate such as a sliding hip screw,
dynamic condylar screw, blade plate, or locking proximal femoral plate
involve accurate biplanar fluoroscopic vigilance. The relationship of
the tip of the trochanter and the center of the femoral head should be
very carefully scrutinized to avoid any varus (Figs. 49-26 and 49-27).
After the plating is completed, the wound is irrigated and closed in
layers in the usual fashion over a suction drain. The patient is placed
in a lightly compressive dressing. When plating techniques are used,
the author typically recommends a limited weight-bearing protocol for 6
to 12 weeks until some radiographic healing is noted. At that point, a
gradual progression to weight-bearing is allowed; however, this
decision should be made primarily based on bone quality and the
fracture pattern, specifically whether any medial comminution exists.
 |
|
FIGURE 49-25 A 95-degree angled condylar blade plate used to treat a short, transverse subtrochanteric fracture.
|
fracture is to stabilize the fracture in an unreduced position
typically varus, flexion, and external rotation of the proximal
fragment with some distraction at the fracture site (Fig. 49-28 and Table 49-1).
Nails are often inserted too laterally as well. To avoid this, the
authors do not hesitate to perform a “mini open” nailing since recent
series have shown that this has no detrimental affect on union
rates and improves clinical alignment.48
Remember to never ream a fracture in an unreduced position since
passing the nail will have no reducing effect on the proximal fragment
with “high” subtrochanteric fractures. When plating techniques are
used, it is critical to perform these in a biologically friendly
fashion so that only the lateral aspect of the femur is visualized by
the surgical dissection. Plating techniques are biomechanically
inferior and, although they can be used effectively, they are very
dependent on indirect reduction (and bony contact to allow load
sharing) to allow rapid healing and avoid hardware failure.
 |
|
FIGURE 49-26 Hardware failure after the fracture was locked in distraction and varus malreduction.
|
 |
|
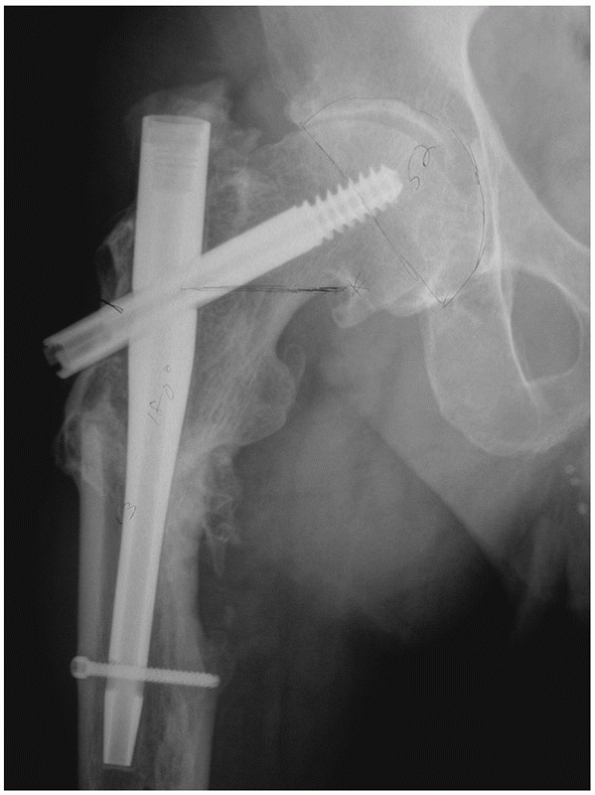
FIGURE 49-27
Salvage of a nonunion with a 95-degree condylar blade plate, note the anatomic neck shaft angle (the relationship of the tip of the trochanter and the center of the femoral head has been restored). Also, note the position of the blade in the inferior femoral head, below the defect from the previous lag screw. |
 |
|
FIGURE 49-28 Malreduced subtrochanteric fracture with supplemental cerclage cables.
|
|
TABLE 49-1 Pitfalls of Internal Fixation of Subtrochanteric Fractures
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|
|
reported. Malunion can result in a varus alignment to the proximal
femur which decreases abductor efficiency due to a more proximal
position of the greater trochanter (Fig. 49-29). This can also affect limb length and clinical rotation.16
The amount of deformity that is problematic remains undefined, so the
surgeon will have to individualize treatment decisions based on patient
complaints and physical examination. There are no large published
series
on the management of proximal subtrochanteric malunion; however,
corrective osteotomy may be indicated if the deformity is severe.
Implant choice for corrective osteotomy will depend on the previously
placed implants, available bone quality, and defects in the femoral
head. The author prefers to use a 95-degree angled blade plate in this
situation since the plate can be placed in the proximal fragment, a
corrective osteotomy performed at the apex of the deformity, and when
the plate is reduced to the femoral shaft, correct alignment is usually
obtained, similar to the technique used for indirect reduction of acute
fractures. The blade can typically be placed in the inferior femoral
head, an area unlikely to be violated by previous internal fixation
devices.
 |
|
FIGURE 49-29
Subtrochanteric malunion. Note the lateral starting point, the varus malalignment, and the very visible lesser trochanter which implies external rotational malreduction of the proximal fragment. |
The treatment of nonunion will vary; however, the surgeon must
determine whether the fracture is aligned in a suitable fashion and can
be treated with an exchange nailing or whether there is concomitant
malalignment that will require realignment via a full nonunion takedown
(the more common situation) (Fig. 49-30). In
general, if the nonunion is well aligned and was previously nailed,
then the authors prefer to perform an exchange nailing, with a larger
diameter nail, in a closed fashion. A nail with a different locking
screw configuration into the proximal fragment may provide better
fixation if bony defects from prior fixation are present (Fig. 49-31).
If there has been hardware failure, the proximal fragment is short or
there is problematic malalignment, then the author prefers an open
plating technique with a 95-degree blade plate. Usually a full nonunion
take-down—removing all fibrous tissue from the nonunion site—will be
required and compression must be achieved. Several studies have
demonstrated that successful union can be obtained as long as stable
proximal fragment fixation can be obtained.1,7,17
The authors prefer to use bone graft or a bone graft substitute for
atrophic nonunions or those with bony deficiency. Arthroplasty may have
a role in the multiply operated nonunion in the elderly patient,
especially if the proximal fragment has massive bone defects from prior
fixation attempts or articular damage from screw cut-out.
 |
|
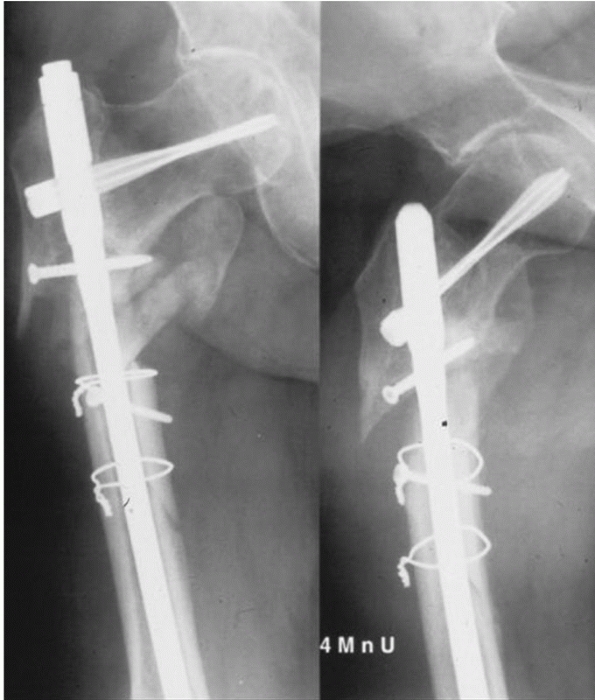
FIGURE 49-30
Subtrochanteric nonunion with varus, shortening, and external rotational malreduction of the proximal fragment. Such a situation will require open nonunion takedown and realignment probably with a blade plate. |
 |
|
FIGURE 49-31
A subtrochanteric nonunion after cephalomedullary nailing was treated with antegrade exchange nailing. A different proximal locking configuration was chosen to optimize fixation of the proximal fragment. |
complications to manage and is often associated with nonunion. Early
postoperative infection is managed with débridement, retention of
stable hardware, and a period of intravenous organism specific
antibiotics. For chronic infections or those with loose or broken
hardware, the authors prefer to remove all hardware, thoroughly
irrigate and débride the area (typically reaming the femoral canal),
and place the patient on a period of intravenous organism-specific
antibiotics. Intramedullary antibiotic spacers can be useful as well to
provisionally stabilize the subtrochanteric region. The authors use a
metal ball-tipped guide rod as an endoskeleton and surround the wire
with antibiotic loaded bone cement. The definitive fixation with or
without bone grafting is then performed after eradication of infection.
For extremely unstable fractures temporary external fixation can be
useful until definitive fixation can occur.
subtrochanteric fractures has generally been good with a high rate of
clinical union and a low rate of reoperation. Malalignments are common,
and these surgeries can be difficult with long operative times and
significant blood loss. Multiple studies support the superiority of
nailing techniques over plating techniques.2,3,4,6,12,23,26,27,28,31,33,34,37,41,43,44,45,46,47 Plating techniques can also be effective;
however, the best outcomes have been reported with fixed angle devices
implanted with technically demanding indirect reduction techniques.
Published data on management of nonunions have generally demonstrated
good outcomes if stable proximal fragment fixation can be obtained.
percutaneously applied locking plates, analogous to techniques utilized
for fractures of the distal femur. Nail developments will likely focus
on percutaneous reduction instruments and various proximal locking
options to optimize proximal fragment fixation. Computer-navigated
reduction of the proximal fragment may someday assist the surgeon in
avoiding varus and rotational malunions. It is likely that data will
emerge that routine “mini-open” nailing of the short, deformed,
so-called “high” subtrochanteric fracture will improve reduction
quality with no deleterious effects on union rates. Although
historically discouraged, it is likely that the judicious use of
cerclage in certain spiral and long oblique fracture patterns will play
an increasing role in minimizing malreduction and nonunion.
A. The treatment of subtrochanteric nonunions with the long gamma nail:
26 patients with a minimum 2-year follow-up. J Orthop Trauma
2005;19(4):294.
WW, Wiss DA, Becker V Jr, et al. Subtrochanteric femur fractures: a
comparison of the Zickel nail, 95 degrees blade plate, and interlocking
nail. J Orthop Trauma 1991; 5(4):458-464.
PL, Reynders P. The use of the unreamed AO femoral intramedullary nail
with spiral blade in nonpathologic fractures of the femur: experiences
with 80 consecutive cases. J Orthop Trauma 2002;16(3):150-154.
L, Cam M, Muratli HH, et al. Indirect reduction and biological internal
fixation of comminuted subtrochanteric fractures of the femur. Injury
2006;37(8):740-750.
F, Gamba D. Gamma nailing of pertrochanteric and subtrochanteric
fractures: clinical results of a series of 63 consecutive cases. J
Orthop Trauma 1997;11(6):412-415.
C, Leunig M, Beck M, et al. Entry point soft tissue damage in antegrade
femoral nailing: a cadaver study. J Orthop Trauma 2001;15(7):488-493.
B, Moed BR, Bledsoe JG. Biomechanical comparison of a 2 and 3 proximal
screw configured antegrade piriformis intramedullary nail with a
trochanteric reconstruction nail in an unstable subtrochanteric
fracture model. J Orthop Trauma 2008;22(5):337-341.
and Dislocation Compendium. Orthopaedic Trauma Association Committee
for Coding and Classification. J Orthop Trauma 1996;10(Suppl 1):v-ix,
1-154.
BG, Tornetta P. Use of an interlocked cephalomedullary nail for
subtrochanteric fracture stabilization. Clin Orthop 1998;348:95-100.
C, Peterman A, Howard PW. The treatment of difficult proximal femoral
fractures with the Russell-Taylor reconstruction nail. Injury
1999;30(6):407-415.
PV. Aspects of current management: Surgical priorities in damage
control in polytrauma. J Bone Joint Surg (Br) 2003;85B:478-483.
SK, Yang KY, Koh JS, et al. Subtrochanteric insufficiency fractures in
patients on alendronate therapy: a caution. J Bone Joint Surg
2007;89B(3):349-353.
JJ, Probe RA, Brinker MR. The effects of femoral shaft malrotation on
lower extremity anatomy. J Orthop Trauma 2004;18(10):658-664.
EA, Agudelo JF, Morgan SJ, et al. Treatment of complex proximal femoral
fractures with the proximal femur locking compression plate.
Orthopedics 2007;30(8): 618-623.
C, Bolhofner BR, Mast JW, et al. Subtrochanteric fractures of the
femur: results of treatment with the 95 condylar blade-plate. Clin
Orthop 1989;28:122-130.
I, Tachibana S, Mikama Y, et al. Insufficiency fracture of femoral neck
after intramedullary nailing. J Orthop Sci 1999;4:304-306.
WJ, Hearn TC, Powell JN, et al. Fixation of segmental subtrochanteric
fractures: a biomechanical study. Clin Orthop 1996;332:71-79.
C, Muller M, Miclau T. Evolution of minimally invasive plate
osteosynthesis (MIPO) in the femur. Injury 2001;32(Suppl 3):SC14-23.
C, Schandelmaier P, Miclau T, et al. Minimally invasive percutaneous
plate osteosynthesis (MIPPO) using the DCS in proximal and distal
femoral fractures. Injury 1997;28(Suppl 1):A20-30.
FJ, Olsson O, Pearlman CA, et al. Intramedullary versus extramedullary
fixation of subtrochanteric fractures. A biomechanical study. Acta
Orthop Scand 1998;69(6): 580-584.
PC, Hsieh PH, Yu SW, et al. Biologic plating versus intramedullary
nailing for comminuted subtrochanteric fractures in young adults: a
prospective, randomized study of 66 cases. J Trauma
2007;63(6):1283-1291.
C, Ostrum RF. Treatment of subtrochanteric femur fractures using a
submuscular fixed low-angle plate. Am J Orthop 2003;32(9 Suppl):29-33.
RF, Marcantonio A, Margurger R. A critical analysis of the eccentric
starting point for trochanteric intramedullary femoral nailing. J
Orthop Trauma 2005;19(10): 681-686.
C-H. Dynamic condylar screw for subtrochanteric femur fractures with
greater trochanteric extension. J Orthop Trauma 1996;10(5):317-322.
SM. Evolution of the internal fixation of long bone fractures. The
scientific basis of biological internal fixation: choosing a new
balance between stability and biology. J Bone Joint Surg Br
2002;84(8):1093-1110.
KJ, Morgan RA, Gorczyca JT, et al. A mechanical comparison of
subtrochanteric femur fracture fixation. J Orthop Trauma
1998;12(5):324-429.
J, Aro HT. Intramedullary fixation of high subtrochanteric femoral
fractures: a study comparing two implant designs, the Gamma nail, and
the intramedullary hip screw. J Orthop Trauma 1998;12(4):249-252.
WM, Schwappach J, Tucker M, et al. Trochanteric versus piriformis entry
portal for the treatment of femoral shaft fractures. J Orthop Trauma
2006;20(10):663-667.
CS, Nawab A, Wang M, et al Second-generation intramedullary nailing of
subtrochanteric femur fractures: a biomechanical study of fracture site
motion. J Orthop Trauma 2002;16(4):231-238.
CM, Houslian S, Khan LA. Trochanteric entry long cephalomedullary
nailing of subtrochanteric fractures caused by low-energy trauma. J
Bone Joint Surg Am 2005; 87(10):2217-2226.
R, Regazzoni P. Treatment of subtrochanteric femur fractures using the
dynamic condylar screw. J Orthop Trauma 1989;3(3):206-213.
S, Johnston P, Ahmad MA, et al. Outcome of traumatic subtrochanteric
femoral fractures fixed using cephalo-medullary nails. Injury
2007;38(11):1286-1293.
AJ, Hay MT, Reinert CM, et al. Cephalomedullary nails in the treatment
of high-energy proximal femur fractures in young patients: a
prospective, randomized comparison of trochanteric versus piriformis
fossa entry portal. J Orthop Trauma 2006;20(4): 240-246.
Doorn R, Stapert JW. The long gamma nail in the treatment of 329
subtrochanteric fractures with major extension into the femoral shaft.
Eur J Surg 2000;166(3):240-246.
DA, Brien WW. Subtrochanteric fractures of the femur: results of
treatment by interlocking nailing. Clin Orthop 1992;283:231-236.
A, Liporace F, Lindrall E, et al. Clamp assisted reduction of high
subtrochanteric fractures of the femure. J Bone Joint Surg Am
2009;91(8):1913-1918.
