The Proprioceptive Sensations
sensations arise from the deeper tissues of the body, principally from
the muscles, ligaments, bones, tendons, and joints. Proprioception has
both a conscious and an unconscious component. The conscious component
travels with the fibers subserving fine, discriminative touch; the
unconscious component forms the spinocerebellar pathways. The conscious
proprioceptive sensations that can be tested clinically are motion,
position, vibration, and pressure.
of various parts of the body. The sense of position, or posture, is
awareness of the position of the body or its parts in space. These
sensations depend on impulses arising as a result of motion of the
joints and of lengthening and shortening of the muscles. Motion and
position sense are usually tested together, by passively moving a part
and noting the patient’s appreciation of the movement and recognition
of the direction, force, and range of movement; the minimum angle of
movement the patient can detect; and the ability to judge the position
of the part in space. In the lower extremity, testing usually begins at
the metatarsophalangeal joint of the great toe, in the upper extremity
at one of the distal interphalangeal joints. If these distal joints are
normal there is no need to test more proximally. Testing is done with
the patient’s eyes closed. It is extremely helpful to instruct the
patient, eyes open, about the responses expected before beginning the
testing. No matter the effort, nonsensical replies are frequent. The
examiner should hold the patient’s completely relaxed digit on the
sides, away from the neighboring digits, parallel to the plane of
movement, exerting as little pressure as possible to eliminate clues
from variations in pressure. If the digit is held dorsoventrally, the
grip must be firm and unwavering so that the pressure differential to
produce movement provides no directional clue. The patient must relax,
and not attempt any active movement of the digit that may help to judge
its position. The part is then passively moved up or down, and the
patient is instructed to indicate the direction of movement from the
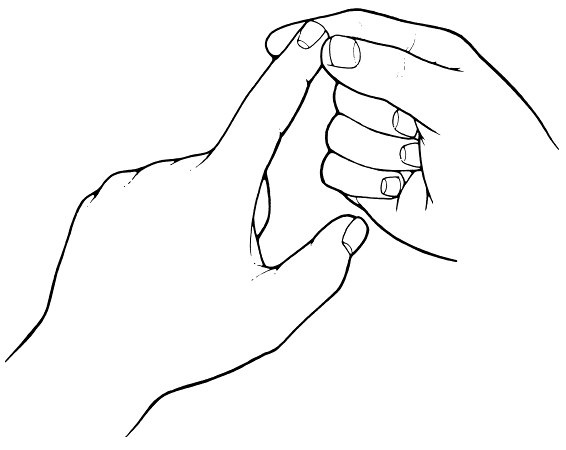
last position (Figure 24.1). Even when
instructed that the response is two alternatives, forced choice, up or
down, some patients cannot be dissuaded from reporting the absolute
position (e.g., down), even if the movement was up from a down
position; a surprising number insist on telling the examiner the digit
is “straight” when it is moved into that position. It is often useful
simply to ask the patient to report when he first detects movement,
then move the digit up and down in tiny increments, gradually
increasing the excursion until the patient is aware of the motion.
Quick movements are more easily detected than very slow ones. Healthy
young individuals
can
detect great toe movements of about 1 mm; in the fingers virtually
invisible movements at the distal interphalangeal joint are accurately
detected. There is some rise in the threshold for movement and position
sense with advancing age.
 |
|
FIGURE 24.1 • Method of testing position sense; done similarly with toe.
|
of the sense of position of the digits, then of motion. In the foot
these sensations are lost in the small toes before they disappear in
the great toe; in the hand involvement of the small finger may precede
involvement of the ring, middle, or index finger, or thumb. Loss of
small movements in the midrange is of dubious significance, especially
in an older person. Loss of ability to detect the extremes of motion of
the great toe is abnormal at any age. Errors between these two extremes
require clinical correlation. If the senses of motion and position are
lost in the digits, one should examine more proximal joints, such as
ankle, wrist, knee, or elbow. Abnormality at such large joints is
invariably accompanied by significant sensory ataxia and other
neurologic abnormalities.
of one of the patient’s hands in a certain position (e.g., the “OK”
sign) while his eyes are closed, and then asking him to describe the
position or to imitate it with the other hand. The foot may be
passively moved while the eyes are closed, and the patient asked to
point to the great toe or heel. With the hands outstretched and eyes
closed, loss of position sense may cause one hand to waver or droop.
One of the outstretched hands may be passively raised or lowered, and
the patient asked to place the other extremity at the same level. One
hand may be passively moved, with eyes closed, and the patient asked to
grasp the thumb or forefinger of that hand with the opposite hand.
Abnormal performance on these latter tests does not indicate the side
of involvement when a unilateral lesion is present. Loss of position
sense may cause involuntary, spontaneous movements (pseudoathetosis, Figure 21.3).
Reduction in the ability to perceive the direction of passive skin
movement may indicate impairment of position sense superficial to the
joint. Such impairment is usually associated with joint-sense deficit
as well. In the pinch-press test, the patient is asked to tell if the
examiner is lightly pinching or pressing the skin. Neither stimulus
should be sufficiently intense to cause pain. The methods available for
evaluating the senses of motion and position are all relatively crude,
and there may be functional impairment not adequately brought out by
the testing procedures.
sensory function in order to keep the nervous system informed about the
moment-to-moment position of the limbs and body in space. Patients with
severe proprioceptive deficits may have ataxia and incoordination which
closely resemble those seen in cerebellar disease, except that they are
much worse when the eyes are closed. The incoordination due to
proprioceptive loss is referred to as sensory ataxia. The ataxia and
incoordination are significantly influenced by vision. Visual input
allows for conscious correction of errors and permits the patient to
compensate to some degree for the proprioceptive loss. There may be
some degree of incoordination with eyes open, but performance is
significantly degraded with eyes closed. The incoordination may be
apparent on the tests usually employed for cerebellar function, such as
finger to nose and heel to shin. When trying to stand and walk, the
patient with sensory ataxia may not be aware of the position of his
feet or the posture of his body. He may walk fairly well with eyes
open, but with eyes closed he staggers and may fall. Although the
standing posture with eyes open is stable, with eyes closed there is a
tendency to sway and fall. The Romberg test explores for imbalance due
to proprioceptive sensory loss. The patient is able to stand with feet
together and eyes open but sways or falls with eyes closed; it is one
of the earliest signs of posterior column disease. The gait of sensory
ataxia and the Romberg sign are discussed in more detail in Chapter 44.
A classic disease causing sensory ataxia, now seldom seen, is tabes
dorsalis. Sensory ataxia is currently more likely to be encountered in
patients with severe peripheral neuropathy (especially if it involves
large fibers), dorsal root ganglionopathy, or vitamin B12 deficiency.
presence of vibration when an oscillating tuning fork is placed over
certain bony prominences. For clinical purposes, it can be considered a
specific type of sensation, but more probably results from a
combination of other sensations. Bone may act largely as a resonator.
The oscillations of the tuning fork invoke impulses that are coded so
that one cycle of the sinusoidal wave produces one action potential.
The frequency of action potentials in the afferent nerve fiber signals
the vibration frequency. The intensity of vibration is related to the
total number of sensory nerve fibers activated.
sensations through large, myelinated nerve fibers, and enter the spinal
cord through the medial division of the posterior root. Vibration has
been traditionally considered to ascend the spinal cord with other
proprioceptive impulses in the dorsal columns, but likely other
pathways are involved. Fibers in the dorsolateral funiculus may be the
most important pathway subserving vibratory sensation in man. Loss of
position sense and vibration sense do not always parallel one another,
and in some clinical conditions one is affected much more and much
earlier than the other. Divergence of the position sense and vibration
sense pathways may partially explain the occasional dissociation
between changes in position sense and vibration sense. In subacute
combined degeneration it is not uncommon for vibration loss to be much
worse than position sense loss, conversely for tabes dorsalis.
frequently used. Sensation may be tested on the great toes, the
metatarsal heads, the malleoli, the tibia, anterior superior iliac
spine, sacrum, spinous processes of the vertebrae, sternum, clavicle,
styloid processes of the radius and ulna, and the finger joints. It is
possible to test vibration perceived from the skin by testing on the
pads of the fingertips, or even on the skin overlying muscle and other
tissues. Both the intensity and duration of the vibration perceived
depend to a great extent on the force with which the fork is struck and
the interval between the time it is set in motion and the time of
application.
placed on a bony prominence, usually the dorsum of the great toe
interphalangeal joint initially, and held there until the patient no
longer feels the vibration. A frequent problem is failure to adequately
instruct the patient in the desired response. The novice examiner
strikes the tuning fork, touches it to the patient’s great toe, and
says,
“Do you feel that?” A deceptive problem lies in the definition of
“that.” A patient with absent vibratory sensation may feel the touch of
the handle of the tuning fork, misinterpret it as the “that” inquired
about, and respond affirmatively. Thus very gross defects in vibratory
sensibility may be completely missed. Always set the fork in motion,
touch it to some presumably normal body part and tell the patient “this
is vibrating or buzzing,” then dampen the tines, reapply the stimulus,
and tell the patient “this is just touching,” or something similar that
clearly differentiates the nature of the two stimuli, and then proceed
with the testing. With normal vibratory sensation, the patient can feel
the fork over the great toe until it has almost stopped vibrating. If
vibration is impaired, when the fork is no longer perceptible distally
it is moved to progressively more proximal locations until a level is
found that is normal. It is also important to compare vibratory
sensibility at homologous sites on the two sides. Sensing the vibration
briefly when moving to one side after vibration has ceased on the other
side is not abnormal; it probably has to do with sensory adaptation.
Consistent asymmetry of vibratory sensation is abnormal. It is
important to include occasional control applications, striking the fork
so the patient hears the hum, and then quickly grabbing and damping the
tines before applying the handle. The patient who then claims to feel
the vibration has not understood the instructions. Occasional
peripheral neuropathy patients with constant tingling in the feet may
think they feel a vibration even when the fork is silent.
somewhat higher in the lower than in the upper extremities. There is
progressive loss of vibratory sensibility with advancing age, and the
sensation may be entirely absent at the great toes in the elderly. The
best control is an approximately age-matched normal, such as the
patient’s spouse. If patient and examiner are about the same age, the
examiner can compare the patient’s perception of vibration with his own.
system must accurately perceive, transmit, and interpret a rapidly
changing stimulus. An early physiologic change due to demyelination is
prolongation of the nerve refractory period, which causes an inability
of the involved fiber to follow a train of impulses. An example is the
flicker fusion test, no longer used, in which a patient with optic
nerve demyelination perceives a strobe as a steady light on the
involved side at a frequency when it is still flickering on the normal
side. The ability to follow a train of stimuli is one of the first
functions impaired when there is demyelination in the nervous system,
either peripheral or central. Testing vibratory sensibility measures
this functional ability, and loss of vibratory sensation is a sensitive
indicator of dysfunction of the peripheral nervous system or the
posterior columns, especially when there is any degree of
demyelination. It is common for vibratory sensation to be impaired out
of proportion to other modalities in patients with multiple sclerosis.
noting where the patient can perceive it and for how long (e.g.,
“absent at the great toes and first metatarsal head, present for 5
seconds over the medial malleoli [128 Hz fork]”). If the patient
returns having lost vibration over the malleoli, then the condition is
progressing. If on follow-up, vibration is present for 12 seconds over
the malleoli and can now be perceived for 3 seconds over the metatarsal
heads, then the patient is improving.
of the peripheral nerves, nerve roots, dorsal root ganglia, posterior
columns, and lesions involving the medial lemniscus and other central
connections. In patients with posterior column or peripheral nerve
disease, vibratory sensation is lost in the lower extremities much
earlier than in the upper. The finding of a normal vibratory threshold
in the distal lower extremities usually obviates the need for testing
proximally or in the upper extremities, absent specific symptoms
involving these areas. A moderate decrease in vibratory perception in
the lower extremities or a difference between the lower and the upper
extremities may be clinically significant. Marked vibratory loss
distally (e.g., the toe), with a transition to normal more proximally
(e.g., the knee), is more consistent with peripheral neuropathy.
Impaired vibration from posterior column disease is more likely to be
uniform at all sites in the involved extremities. Occasionally, in
localized spinal cord lesions, a “level” of vibration sensory loss may
be found on
testing
over the spinous processes. Because bone is such an efficient
resonator, occasional patients with severe deficits to vibration in the
distal lower extremities may feel transmitted vibrations in the hip and
pelvis. When vibration seems more intact than it should, ask the
patient where he feels the sensation.
to tactile sense, but involves the perception of pressure from the
subcutaneous structures rather than light touch from the skin. It is
also closely related to position sense and is mediated via the
posterior columns. Pressure sense is tested by a firm touch on the skin
or by pressure on deep structures (muscle masses, tendons, nerves),
using finger pressure or a blunt object. The patient should both detect
and localize the pressure. Strong pressure over muscles, tendons, and
nerves tests deep pain sensibility.
more diffuse and less well localized than superficial pain. The
pathways for deep pain are the same as for superficial pain. Deep pain
may be tested by squeezing muscles, tendons, or the testicles; by
pressing on superficial nerves or on the eyeballs, or by pushing a
finger interphalangeal joint into extreme, forced hyperflexion. Firm
pressure on the base of a nail with a hammer or tuning fork handle also
hurts a great deal. Loss of deep pain sensibility is a classic finding
in tabes dorsalis. The response to superficial or deep pain stimulation
may be simply delayed before it is lost.
