The Forearm
differ significantly. The ulna has a subcutaneous border that extends
for its entire length; the bone can be reached simply and directly
without endangering other structures. In contrast, the upper two thirds
of the radius are enclosed by a sheath of muscles. All surgery in the
upper third of the radius is complicated further by the posterior
interosseous nerve, which winds spirally around the bone close to, if
not in contact with, its periosteum.
in this chapter, all of which allow for the complete exposure of bone.
In nearly every case, only part of the approach is required. The anterior approach to the radius
is one of the classic extensile approaches, relying on subperiosteal
dissection for protection of the posterior interosseous nerve. The posterior approach to the radius
also makes use of an internervous plane, but still requires
identification and preservation of the posterior interosseous nerve.
The approach to the ulna cuts directly
onto its subcutaneous border. The anatomy of the anterior approach to
the radius, the approach to the ulna, and the anatomy of the posterior
compartment of the forearm are considered separately. Because of the
critical importance of the posterior interosseous nerve, its course is
described in both anatomic sections.
of the radius, exposing the entire length of the bone. Exposing the
proximal third of the radius endangers the posterior interosseous
nerve. By stripping the supinator muscle off the radius subperiosteally
and using it to protect the nerve, however, the anterior approach
avoids this danger. Still, great care must be taken in positioning
retractors, because the nerve actually may touch the bone at the level
of the distal portion of the neck of the radius, opposite the bicipital
tuberosity, and posteriorly placed retractors can compress it against
the bone. The approach first was described by Henry, and his name
usually is associated with it.1
-
Open reduction and internal fixation of fractures2
-
Bone grafting and fixation of fracture nonunions
-
Radial osteotomy
-
Biopsy and treatment of bone tumors
-
Excision of sequestra in chronic osteomyelitis
-
Anterior exposure of the bicipital tuberosity
-
Treatment of compartment syndrome
entire length of the bone. Ordinarily, only a portion of the approach
is required.
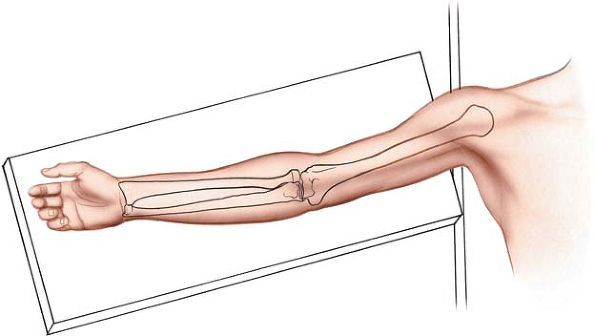
the arm on an arm board. Place a tourniquet on the arm, but do not
exsanguinate it fully before inflating the tourniquet. Venous blood
left in the arm makes the vascular structures easier to identify.
Finally, supinate the forearm (Fig. 4-1).
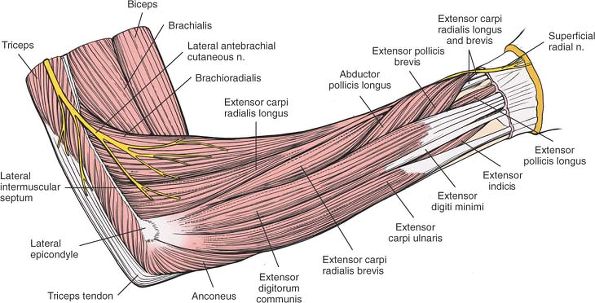
which is a fleshy muscle that arises with the extensor carpi radialis
longus and brevis muscles from the lateral epicondyle of the elbow. The
three muscles form a “mobile wad” of muscle that runs down the lateral
aspect of the supinated forearm.
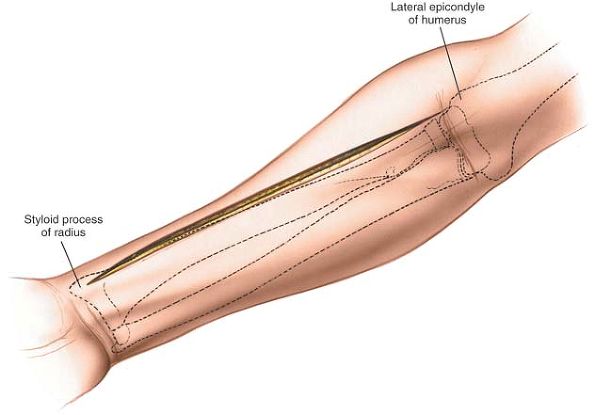
Note that this bony process is truly lateral when the hand is in the
anatomic (supinated) position. The styloid process is the most distal
part of the lateral side of the radius.
of the elbow just lateral to the biceps tendon down to the styloid
process of the radius. The length of the incision depends on the amount
of bone that needs to be exposed (Fig. 4-2).
 |
|
Figure 4-1 Position of the patient on the operating table, for the anterior approach to the radius.
|
 |
|
Figure 4-2
Make a straight incision on the anterior part of the forearm, from the flexor crease on the lateral side of the biceps down to the styloid process of the radius. |
 |
|
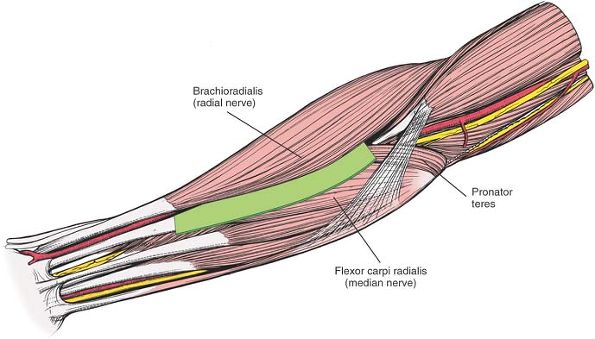
Figure 4-3 Internervous plane. The plane lies between the brachioradialis (radial nerve) and the flexor carpi radialis (median nerve).
|
Proximally, the internervous plane lies between the brachioradialis
muscle, which is innervated by the radial nerve, and the pronator teres
muscle, which is innervated by the median nerve.
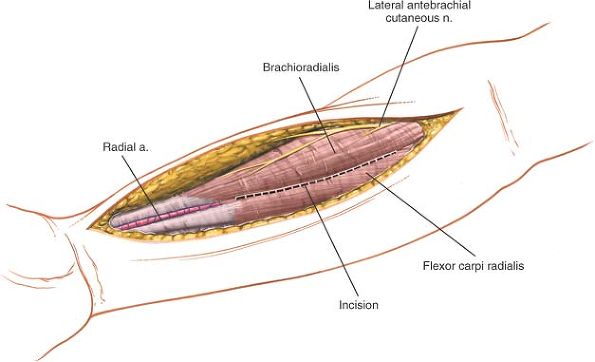
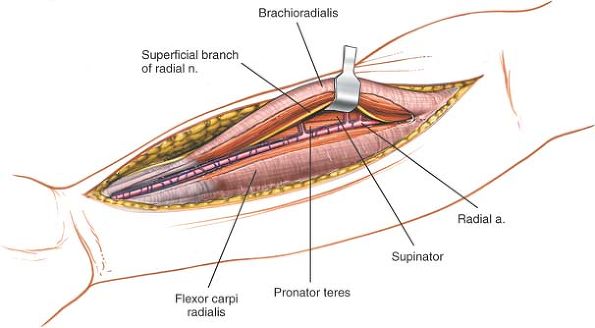
skin incision. Identify the medial border of the brachioradialis as it
runs down the forearm, and develop a plane between it and the flexor
carpi radialis distally. More proximally, the plane lies between the
pronator teres and brachioradialis muscles (Fig. 4-4).
Note that the medial border of the brachioradialis is surprisingly far
across the forearm. At the level of the elbow the brachioradialis
extends almost halfway across the forearm.
the superficial radial nerve running on the undersurface of the
brachioradialis and moving with it. The brachioradialis receives a
number of arterial branches from the radial artery (called the
recurrent radial artery) just below the elbow joint. Ligate this
recurrent leash of vessels (Fig. 4-5). Take
care to ligate these vessels and not avulse them, as avulsion is a
potent cause of postoperative hematoma formation. Many vessels are
present and all will need to be ligated and divided to allow the
brachioradialis to be mobilized laterally.
the middle part of the forearm; therefore, it is quite close to the
medial edge of the wound. It runs with its two venae comitantes, which
remain prominent if the limb is not exsanguinated before the tourniquet
is applied. Often, the artery may have to be mobilized and retracted
medially to achieve adequate exposure of the deeper muscular layer,
particularly at the upper and lower ends of the approach (see Fig. 4-5).
in the forearm, also runs under cover of the brachioradialis muscle.
Preserve the nerve, because damage to it may create a painful neuroma
at the operative site (see Fig. 4-5). It is retracted laterally with the brachioradialis muscle.
 |
|
Figure 4-4 Incise the fascia and develop the plane between the brachioradialis and the flexor carpi radialis.
|
 |
|
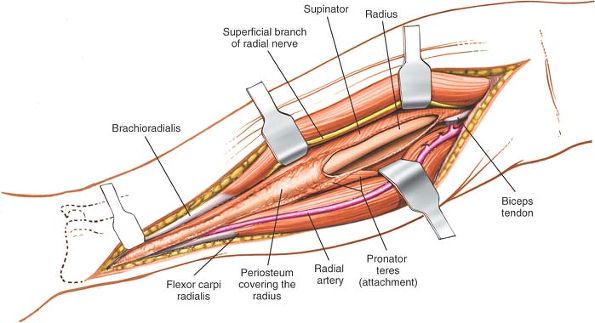
Figure 4-5
A leash of vessels from the radial artery supplies the brachioradialis. The vessels must be ligated to mobilize the brachioradialis laterally. Retract the superficial branch of the radial nerve with the brachioradialis muscle. |
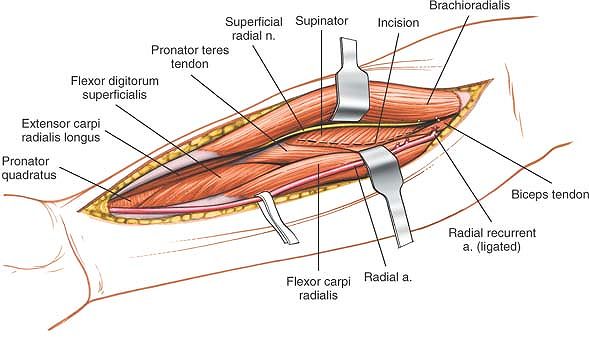
bicipital tuberosity of the radius. Just lateral to the tendon is a
small bursa; incise the bursa to gain access to the proximal part of
the shaft of the radius. Because the radial artery lies superficial and
just medial to the tendon at this point, deepen the wound on the lateral side of the biceps tendon (Fig. 4-6).
supinator muscle, through which the posterior interosseous nerve passes
on its way to the posterior compartment of the forearm.
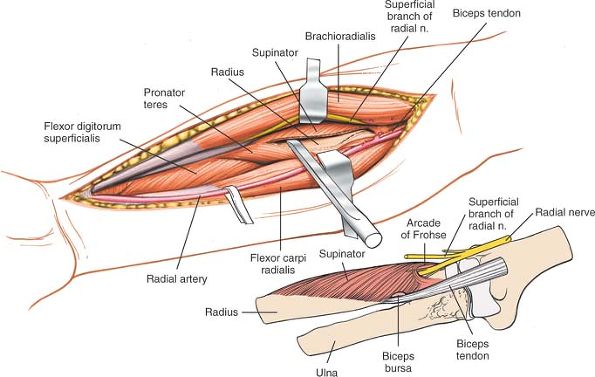
important structure left vulnerable by this approach. To displace the
nerve laterally and posteriorly (away from the surgical area), fully
supinate the forearm, exposing, at the same time, the insertion of the
supinator muscle into the anterior aspect of the radius (Fig. 4-7).
broad insertion. Ensure that the muscle is detached by dividing its
insertion and not by splitting the muscle. Continue subperiosteal
dissection laterally, stripping the muscle off the bone (see Fig. 4-7).
Lateral retraction of the muscle lifts the posterior interosseous nerve
clear of the operative field, but be careful! Excessive traction may
cause a neurapraxia of the nerve, and it recovers very slowly, taking
up to 6 to 9 months. Finally, do not place retractors on the posterior
surface of the radial neck, because they may compress the posterior
interosseous nerve against the bone in patients whose nerve comes into
direct contact with the posterior aspect of the radial neck (about 25%
of all patients).3
 |
|
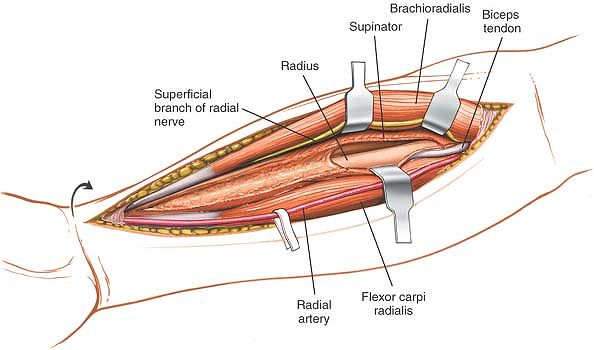
Figure 4-6
Deep to the brachioradialis and the flexor carpi radialis are the supinator muscle, the pronator teres, the flexor digitorum superficialis, and, most distally, the pronator quadratus. |
covered by the pronator teres and flexor digitorum superficialis
muscles. To reach the anterior surface of the bone, pronate the arm so
that the insertion of the pronator teres onto the lateral aspect of the
radius is exposed (Fig. 4-8; see Fig. 4-6).
Detach this insertion from the bone and strip the muscle off medially.
Preserve as much soft tissue as you can compatible with accurate
reduction and fixation of the fracture. This maneuver detaches the
origin of the flexor digitorum superficialis from the anterior aspect
of the radius as well (Fig. 4-9).
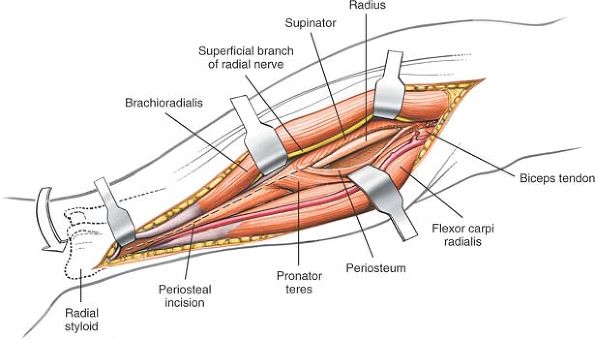
quadratus, arise from the anterior aspect of the distal third of the
radius. To reach bone, partially supinate the forearm and incise the
periosteum of the lateral aspect of the radius lateral to the pronator
quadratus and the flexor pollicis longus. Then, continue the dissection
distally, retracting the two muscles medially and lifting them off the
radius (Fig. 4-10).
 |
|
Figure 4-7
With the patient’s arm in the supinated position, resect the origin of the supinator. Reflect the muscle laterally. Leave the posterior interosseous nerve in the muscle’s substance. The radial nerve enters the supinator through the arcade of Frohse (inset). Turning the forearm upward moves the nerve laterally, away from the operative field. The origin of the supinator muscle is easier to identify if the surgeon stays lateral to the biceps tendon and locates the bursa between it and the supinator. |
 |
|
Figure 4-8 Turn the arm downward to identify the pronator teres muscle. Resect it along its insertion on the lateral aspect of the radius.
|
 |
|
Figure 4-9 Continue dissection distally to uncover the distal part of the radius. Leave the periosteum intact.
|
 |
|
Figure 4-10
With the arm in partial supination, remove the flexor pollicis longus and the pronator quadratus from the bone to expose the entire radius from its proximal to distal end. |
is vulnerable as it winds around the neck of the radius within the
substance of the supinator muscle. The key to ensuring its safety is to
detach correctly the insertion of the supinator muscle from the radius.
The insertion of the muscle is exposed completely only when the arm is
supinated fully. Once the subperiosteal dissection is begun, the nerve
is comparatively safe, but overzealous retraction still can lead to a
neurapraxia (see Figs. 4-7, inset, and 4-13).
runs down the forearm under the brachioradialis muscle. It becomes
vulnerable when the “mobile wad” of three muscles is mobilized and
retracted laterally (see Fig. 4-5). The
superficial radial nerve is vulnerable to neurapraxia if it is
retracted vigorously. Take great care, therefore, when retracting the
nerve and warn your patients preoperatively that temporary paresthesia
in the distribution of the superficial branch of the radial nerve may
occur in the early postoperative phase.
the middle of the forearm under the brachioradialis muscle. It is
vulnerable twice during the anterior approach to the radius:
-
During mobilization of the
brachioradialis. Protection depends on recognizing the artery. Its two
accompanying venae comitantes are the best surgical guide, because the
artery is surprisingly small after a tourniquet has been used (see Fig. 4-5). -
In the proximal end of the wound, as the
artery passes to the medial side of the biceps tendon. Damage to the
artery at that level can be avoided by remaining lateral to the tendon
(see Fig. 4-13).
are a leash of vessels that arise from the radial artery just below the
elbow joint. They consist of two groups, anterior and posterior, which
pass in front of and behind the superficial radial nerve, respectively,
before entering the brachioradialis muscle. They must be ligated to
allow mobilization of both the artery and the nerve (see Figs. 4-9 and 4-12).
entire length of the radius. The approach can be extended distally to
expose the wrist joint.4 Although it can be extended into an anterolateral approach to the elbow and humerus, such extension rarely is required.
(the brachioradialis, extensor carpi radialis longus, and extensor
carpi radialis brevis), which is supplied by the radial nerve, forms
the lateral border of the supinated forearm; and the flexor-pronator
muscles, which are supplied by the median and ulnar nerves, comprise
the rest.
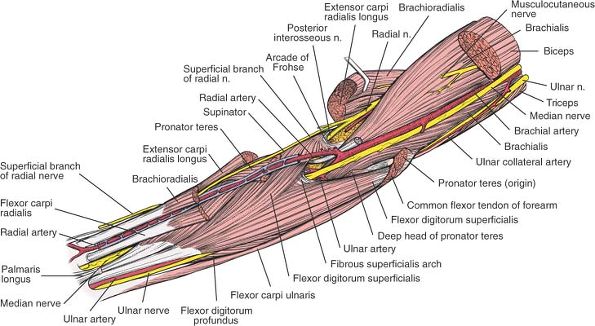
four muscles arise from the common flexor origin on the medial humeral
epicondyle and fan out across the forearm. They are easy to remember by
the following simple maneuver. Place the butt of the opposite hand over
the medial epicondyle, with the palm on the anterior surface of the
forearm: the thumb points in the direction of the pronator teres, the
index finger represents the flexor carpi radialis, the middle finger
represents the palmaris longus, and the ring finger represents the
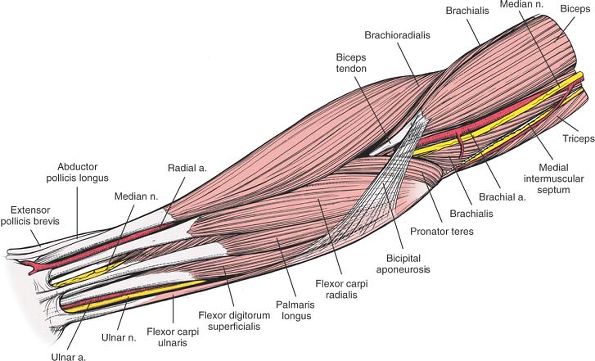
flexor carpi ulnaris (Figs. 4-11 and 4-12).
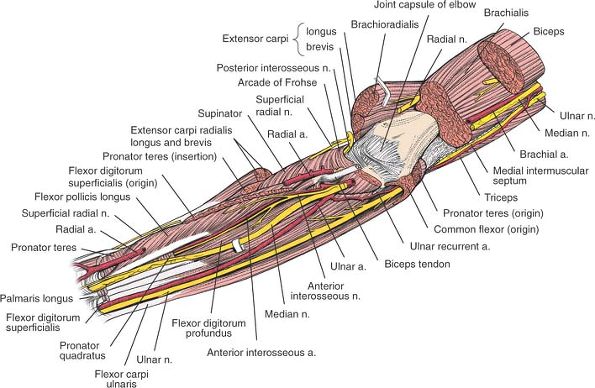
of three muscles: the flexor digitorum profundus, the flexor pollicis
longus, and the pronator quadratus. (A fourth deep muscle, the
supinator, is critical to the surgical anatomy of the area, but is not
strictly a flexor muscle [Fig. 4-14].)
internervous planes that are used in operative approaches:
 |
|
Figure 4-11 Superficial layer of the forearm muscles and vessels.
|
 |
|
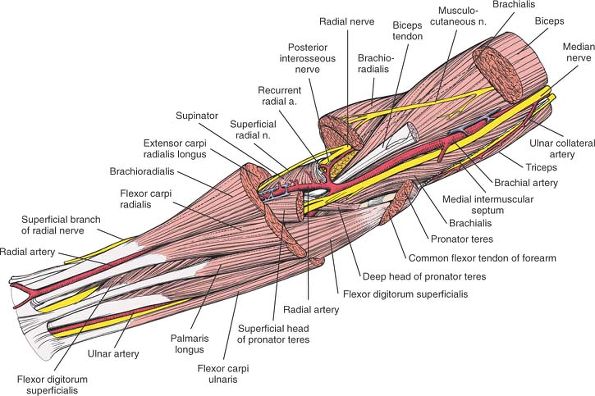
Figure 4-12
The superficial layer of the forearm has been resected, revealing the vessels and nerves. The median nerve pierces the gap between the two heads of the pronator teres. Note the leash of vessels of the radial artery and the recurrent radial artery. |
 |
|
Figure 4-13
The middle layer of the forearm, with the superficial branch of the radial nerve. In the proximal part of the wound, the median nerve enters the undersurface of the superficialis. Flexor Carpi Radialis. Origin. Common flexor origin on medial epicondyle of humerus. Insertion. Bases of second and third metacarpals. Action. Flexor and radial deviator of wrist. Nerve supply. Median nerve.
|
 |
|
Figure 4-14
The deep layer of the forearm. The ulnar nerve and artery and the median nerve lie on the flexor digitorum profundus. Note the position of the anterior interosseous nerve and artery. |
-
Between the radial and median nerves: a
dissection between the brachioradialis muscle, the most medial of the
three muscles forming the “mobile wad of three” (which is supplied by
the radial nerve), and the flexor carpi radialis and pronator teres
muscles, the most lateral of the flexor-pronator group (which are
supplied by the median nerve; see Fig. 4-3) -
Between the median and ulnar nerves: a
dissection between the flexor carpi ulnaris muscle (which is supplied
by the ulnar nerve) and the flexor digitorum superficialis muscle, the
most medial of the flexor muscles (which is supplied by the median
nerve; see Fig. 5-29) -
Between the ulnar and posterior
interosseous nerves: a dissection between the flexor carpi ulnaris
muscle (which is supplied by the ulnar nerve) and the extensor carpi
ulnaris muscle (which is supplied by the posterior interosseous nerve;
see Fig. 4-21)
approach to the radius, the second exposes the ulnar nerve in the
forearm, and the third is used for exposure of the ulna.
the forearm is relatively simple: the forearm is “framed” by its
nerves. The superficial radial nerve runs
down the radial aspect of the forearm, with the radial artery lying on
its medial side in the distal half of the forearm (see Fig. 4-13). The ulnar nerve
runs down the ulnar side of the forearm, with the ulnar artery lying on
its lateral side in the distal half of the forearm. The median nerve runs down the middle of the forearm (see Fig. 4-14).
are arteries of transit in the forearm; they both are branches of the
brachial artery. Because the brachial artery lies in the middle of the
anterior aspect of the elbow, with the median nerve lying on its medial
side, the ulnar artery and median nerve must cross in the upper
forearm, with the nerve superficial to the artery; this crossing occurs
at the level of the musculotendinous region of the pronator teres
muscle (see Fig. 4-13). The anterior
interosseous nerve (which is a branch of the median nerve) and the
anterior interosseous artery (which is a branch of the common
interosseous artery, which itself is a branch of the ulnar artery) also
run down the middle of the forearm, but deeper than the median nerve
(see Fig. 4-14).
of cleavage in the forearm, the resultant scar may be broad. Making the
incision as a series of gentle curves brings the skin incision closer
to the lines of cleavage in the forearm. Such an incision has the
effect of reducing tension on the subsequent skin repair.
the mobile wad of three muscles (the brachioradialis, extensor carpi
radialis longus, and extensor carpi radialis brevis) and the pronator
teres muscle proximally and flexor carpi radialis muscle distally (see Fig. 4-11).
the forearm, is supplied by the radial nerve. All three muscles take
some of their origin from the common extensor origin on the lateral
epicondyle of the humerus (see Fig. 4-13).
the forearm when it is supinated and supinates it when it is pronated.
Therefore, it may act as a deforming force in distal radial fractures
if the forearm is immobilized in either full pronation or full
supination after reduction of the fracture. Its action is one reason
for immobilizing distal radial fractures with the forearm in the
neutral position.
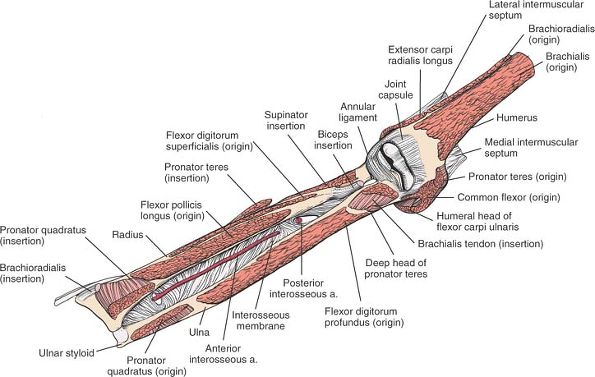
take origin from the distal end of one bone and insert onto the distal
end of another (Fig. 4-15; see Fig. 4-11).
is one of the first muscles to be reinnervated. If the patient
recovering from a high radial nerve palsy is asked to extend the wrist,
the muscle extends with radial deviation, because the balancing muscle,
the extensor carpi ulnaris, is supplied farther distally by a branch
from the posterior interosseous nerve. Reinnervation of the
brachioradialis, however, probably is the best way to diagnose both
clinically and electrically (by electromyographic studies) a recovering
high radial nerve palsy (see Figs. 4-12 and 4-24).
muscle is a wrist extensor that deviates the wrist neither toward the
radius nor toward the ulna. It may be involved in tennis elbow–lateral
epicondylitis.
the extensor carpi radialis brevis muscle have been described.
 |
|
Figure 4-15
The origins and insertions of the muscles of the forearm. Note the anterior interosseous artery lying on the interosseous membrane. Brachioradialis. Origin. Upper two thirds of lateral supracondylar ridge of humerus. Insertion. Styloid process of radius. Action. Flexor of elbow. Pronator and supinator of forearm. Nerve supply. Radial nerve.
Flexor Digitorum Superficialis. Origin.
Medial epicondyle of humerus, medial ligament of elbow, medial border of coronoid process of ulna, fibrous arch connecting coronoid process of ulna with anterior oblique line of radius. Insertion. Volar aspect of middle phalanges of fingers. Action. Flexor of proximal interphalangeal joints, metacarpophalangeal joints, and wrist joint. Nerve supply. Median nerve. Flexor Pollicis Longus. Origin. Middle part of anterior surface of radius. Insertion. Distal phalanx of thumb. Action. Main flexor of thumb. Nerve supply. Anterior interosseous nerve.
Pronator Quadratus. Origin. Lower fourth of volar surface of ulna. Insertion. Lower fourth of lateral aspect of radius. Action. Weak pronator of forearm. Nerve supply. Anterior interosseous nerve.
Palmaris Longus. Origin. Common flexor origin on humerus. Insertion. Palmar aponeurosis. Action. Weak flexor of wrist. Nerve supply. Median nerve.
Flexor Digitorum Profundus. Origin. Upper three fourths of anterior surface of ulna. Insertion. Distal phalanges of fingers. Action. Flexor of distal interphalangeal joints, proximal interphalangeal joints, metacarpophalangeal joints, and wrist joint. Nerve supply. Median and ulnar nerves.
Flexor Carpi Ulnaris. Origin.
From two heads. Humeral head: from common flexor origin on medial epicondyle of humerus. Ulnar head: from medial border of olecranon and upper three fourths of subcutaneous border of ulna. Insertion. Hamate and fifth metacarpal. Action. Flexor and ulnar deviator of wrist. Also weak flexor of elbow. Nerve supply. Ulnar nerve. |
-
The radial artery
originates from the brachial artery in the cubital fossa. Proximally,
it lies just medial to the biceps tendon in a somewhat superficial
position. The radial artery angles across the arm as it descends, lying
on the supinator, the pronator teres, the origin of the flexor pollicis
longus, and the lower part of the anterior surface of the radius, where
it can be palpated easily (see Fig. 4-13). -
The superficial radial nerve
is purely sensory in the forearm. It runs along the lateral side,
crossing the supinator, the pronator teres, and the flexor digitorum
superficialis. Damage to the nerve in the forearm produces an area of
diminished sensation on the dorsoradial aspect of the hand. The most
important problem associated with such damage is not the sensory loss,
however, but the painful neuroma that may result. The nerve runs
lateral to the radial artery when the two are together (see Figs. 4-13 and 4-34).
fully the anterior aspect of the bone. From proximal to distal, they
are as follows:
-
The supinator
-
The pronator teres
-
The flexor digitorum superficialis
-
The flexor pollicis longus
-
The pronator quadratus
muscle, the posterior interosseous nerve, passes through a fibrous arch
known as the arcade of Frohse as it enters the muscle (see Figs. 4-12 and 4-13).5
The arch is formed by the thickened edge of the superficial head of the
supinator. Compression of the nerve at that point produces paralysis or
dysfunction of all the extensor muscles of the forearm, fingers, and
thumb, a lesion that may be incomplete. Compression at the arcade of
Frohse is one of the causes of a posterior interosseous nerve
entrapment syndrome and can be relieved by incising the fibrous arch.6,7,8,9 It also is a cause of pain restricted to this area, which may present as a resistant “tennis elbow” (see Fig. 4-13).10
The great variations that occur in the site, size, and quality of the
ulnar head of the muscle sometimes cause the nerve to become trapped as
it traverses the muscle, producing the pronator syndrome, which mimics
the carpal tunnel syndrome, but includes pain and paresthesia to the
proximal end of the volar aspect of the forearm.11,12
Understandably, the syndrome occurs when the muscle contracts and
further compresses the nerve. In this syndrome, the intrinsic muscles
of the thumb become weak, but the muscles that are innervated by the
anterior interosseous nerve (the flexor pollicis longus, the flexor
profundus to the index and middle fingers, and the pronator quadratus)
are spared (see Fig. 4-12).
The tendons of the muscle form well above the wrist. Functionally, it
is four separate muscles; it can flex each finger independently, in
contrast to the mass action of the flexor digitorum profundus.
may have to be detached to expose the anterior part of the shaft of the
radius (see Figs. 4-13 and 4-15).
Because the muscle is relaxed totally when the forearm is pronated
fully, some authors suggest that distal radial fractures should be
immobilized in pronation. Clearly, however, the pronator quadratus is
not the only possible deforming force on the distal radius; the best
position for immobilizing reduced fractures of the distal radius still
is a matter of debate.
is the motor nerve of the extensor compartment of the forearm. A branch
of the radial nerve, it passes between the two heads of origin of the
supinator muscle and actually may come in direct contact with the
periosteum of the neck of the radius. At that point, it may be trapped
beneath incorrectly positioned plates or retractors. After emerging
from the supinator muscle,
the
nerve passes down over the origin of the abductor pollicis longus
muscle to reach the interosseous membrane. It continues distally on the
interosseous membrane to the wrist joint, which it supplies with some
sensory branches. The nerve supplies the muscles that arise from the
common extensor origin and the deep muscles of the extensor compartment
of the forearm.
 |
|
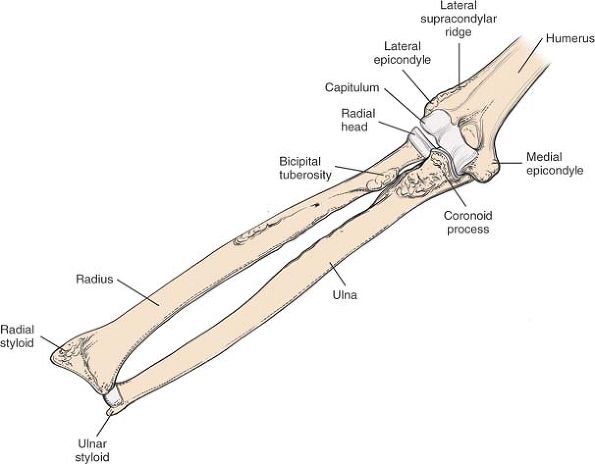
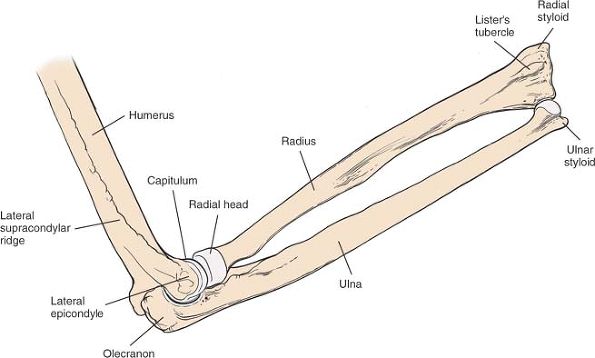
Figure 4-16 The bones of the forearm.
|
all approaches to the upper third of the radial shaft. Although the
nerve can be protected if the insertion of the supinator is detached
and the muscle is stripped off the bone subperiosteally, it can be
argued that the only certain protection as the upper third of the
radius is plated comes from identifying and preserving the nerve via a
posterior approach (see Figs. 4-34 and 4-35).
usually passes between the heads of the pronator teres muscle, whereas
the ulnar artery passes deep to both the heads. Distal to the pronator
teres, the median nerve joins the ulnar artery and passes beneath the
fibrous arch of origin of the flexor digitorum superficialis muscle.
Then, it runs down the flexor aspect of the forearm, roughly in the
midline (see Figs. 4-13 and 4-14).
superficialis muscle, the median nerve sometimes is mistaken for the
superficial tendon to the index finger. To differentiate nerve from
tendon, try to find an artery on the structure in question: the median
nerve has the median artery running along its surface. The artery,
derived from the anterior interosseous artery, is the original fetal
axial artery (see Fig. 4-14).
as a graft for tendon repairs. Because it is absent in 10% of the
population, it must be identified in the conscious patient before
surgery is undertaken. To find it, instruct the patient to touch the
thumb and little fingers together while flexing the wrist against
resistance. Then, palpate the tendon, which stands out prominently in
the forearm (see Fig. 4-11).
palmaris longus at the wrist. In the patient with an absent palmaris
longus, the nerve actually may be mistaken for the tendon (see Fig. 4-11).
four tendons, making it a mass action muscle that is used mainly for power grip.
nerve arises from the median nerve shortly after the median nerve
enters the forearm; the two lie under the tendinous origin of the deep
head of the pronator teres (see Figs. 4-11 and 4-13).
The anterior interosseous nerve may be compressed at this point,
producing the anterior interosseous nerve syndrome: paralysis of the
flexor pollicis longus and flexor profundus tendons to the index and
middle fingers, as well as of the pronator quadratus muscle.14,15,16
strong fascia. Fractures bleed, which increases the pressure within
these compartments. As the pressure increases, the venous return
decreases; in certain cases, the pressure becomes so high that it
reduces the arterial blood supply to the muscles and creates muscle
ischemia. Muscle ischemia in turn creates edema, further increasing
compartment pressure. This is known as a compartment syndrome. Muscle
ischemia produces pain disproportionate to the other injuries; if the
pressure within the compartment is not relieved within a short period
of time, permanent muscle necrosis will occur with associated damage to
the nerves traversing the affected compartment (Volkman’s ischemic
contracture). In extreme cases, arterial occlusion occurs, leading to
gangrene.
 |
|
Figure 4-17 (A)
To decompress the flexor compartments of the forearm begin by making a longitudinal incision extending for the lateral side of the elbow crease to the radial styloid process. (B) Deepen the skin incision to reveal the fascia covering the flexor muscles; the skin edges will spring apart. (C) Deepen the skin incision to reveal the fascia covering the flexor muscles; the skin edges will spring apart. |
the anterior forearm compartment. It can be decompressed by incising
the deep fascia that covers it along its entire length. In cases of
compartment syndrome, both the superficial and the deep compartments on
the volar side should be released along with the posterior compartment.
The incisions used may also be taken down to the wrist crease and into
the hand for release of the carpal tunnel and the deep palmar space.
Such incisions may also be extended proximally to the anterior lateral
approach to the humerus (Fig. 4-17 and 4-18).
 |
|
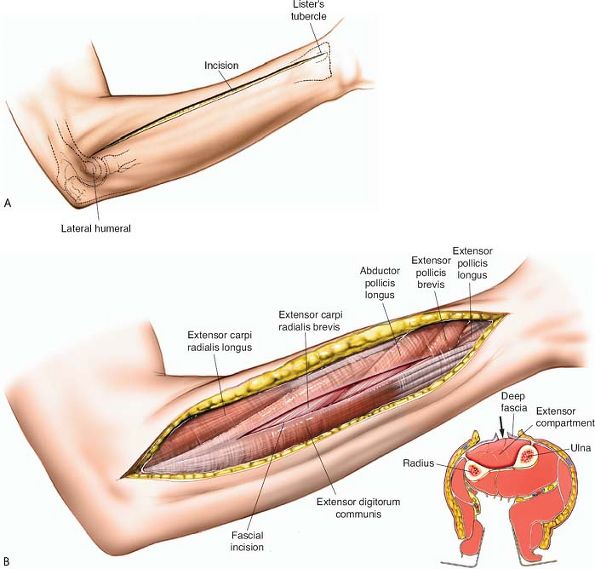
Figure 4-18 (A)
To decompress the posterior compartment, make a longitudinal incision overlying the posterior aspect of the forearm extending from the lateral humeral epicondyle to Lister’s tubercle. (B) Incise the fascia overlying the posterior muscle mass in the line of the skin incision. |
forearm approaches, uncovering the entire length of bone. The exposure
uses the internervous plane between the extensor carpi ulnaris and
flexor carpi ulnaris muscles. Both muscles attach by a shared
aponeurosis into the subcutaneous border of the ulna, the border of
bone that is exposed initially during the approach.
internervous plane share a common aponeurosis, they cannot be separated
at their origin, and the plane is difficult to define. Fibers of the
extensor carpi ulnaris usually have to be detached from the aponeurosis.
-
Open reduction and internal fixation of ulnar fractures
-
Treatment of delayed union or nonunion of ulnar fractures
-
Osteotomy of the ulna
-
Treatment of chronic osteomyelitis
-
Treatment of the fibrous anlage of the ulna in cases of ulnar clubhand2
-
Ulnar lengthening (in Kienböck’s disease)17
-
Ulnar shortening (in cases of distal radial malunion)
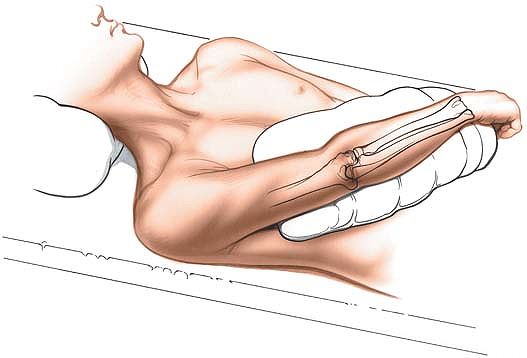
arm placed across the chest to expose the subcutaneous border of the
ulna. Exsanguinate the limb either by elevating it for 3 to 5 minutes
or by applying a soft rubber bandage and then a tourniquet (Fig. 4-19).
the operating table, and get the surgical assistant to hold the
patient’s hand so that the forearm is vertical.
 |
|
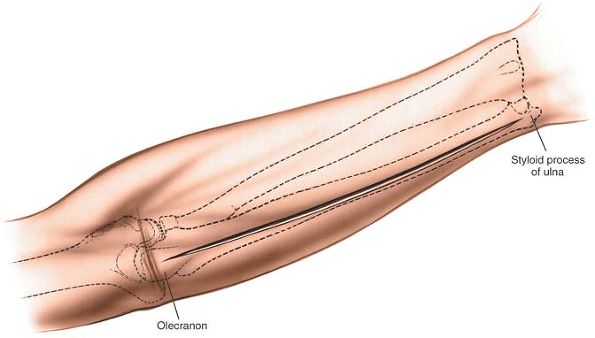
Figure 4-19 Position of the patient on the operating table, for exposure of the shaft of the ulna.
|
 |
|
Figure 4-20 Incision for ulnar exposure. Make a longitudinal incision over the subcutaneous border of the ulna.
|
 |
|
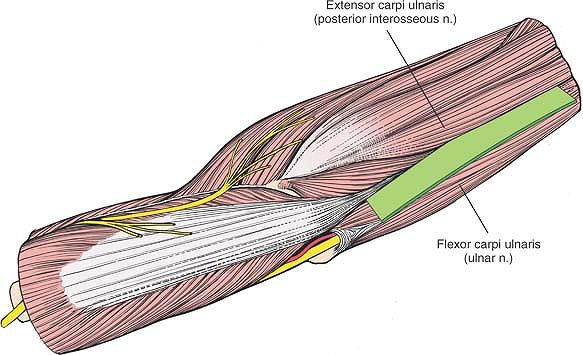
Figure 4-21
The internervous plane lies between the extensor carpi ulnaris (posterior interosseous nerve) and the flexor carpi ulnaris (ulnar nerve). |
subcutaneous border of the ulna. The length of the incision depends on
the amount of bone that is to be exposed. In cases of fracture, center
the incision over the fracture site (Fig. 4-20).
 |
|
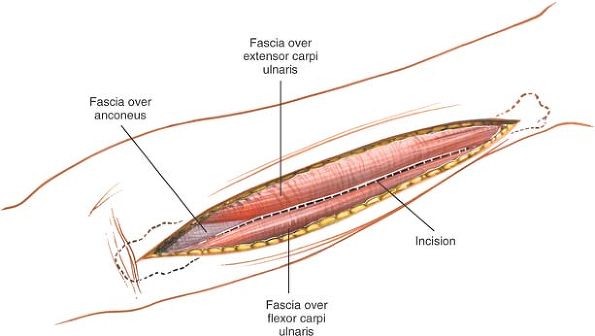
Figure 4-22 Make an incision through the fascia onto the subcutaneous border of the ulna.
|
deep fascia along the same line as the skin incision; continue the
dissection down to the subcutaneous border of the ulna (Fig. 4-22). Even though the bone feels subcutaneous in its middle third,
the fibers of the extensor carpi ulnaris muscle nearly always have to be divided to reach the bone.
 |
|
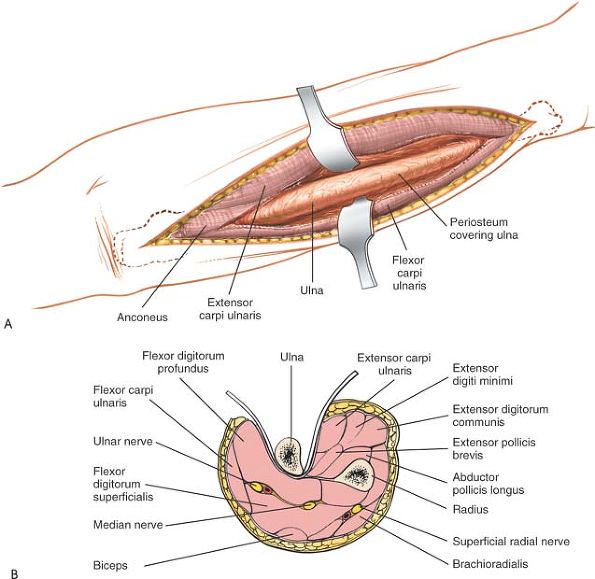
Figure 4-23 (A)
Lift the periosteum longitudinally on the posterior aspect of the ulna, both radially and medially, to expose the entire posterior length of the ulna. (B) Epi-periosteal dissection around the ulna is safe; the muscle masses on each side protect the vital structures. |
and anconeus muscles run along the plane of dissection. The plane still
is an internervous plane, because the anconeus is supplied by the
radial nerve and the flexor carpi ulnaris is supplied by the ulnar
nerve.
providing access to the fracture, continue the dissection in the
epi-periosteal plane to expose either the flexor or extensor aspects of
the bone as needed. Keep soft tissue stripping to a minimum to preserve
blood supply to the fracture (Fig. 4-23).
of the triceps tendon will need to be detached to gain access to the
bone. This insertion is very broad and long, and it blends in with the
periosteum of the subcutaneous surface of the olecranon.
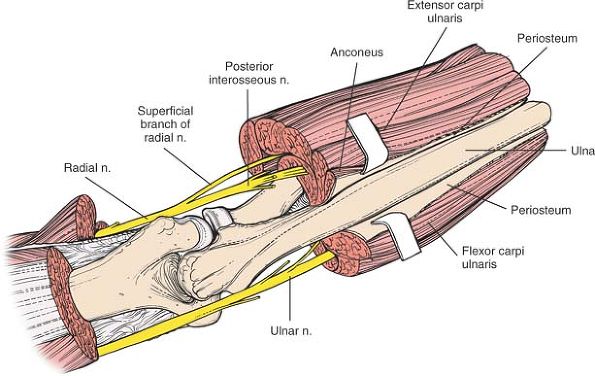
profundus. The nerve is safe as long as the flexor carpi ulnaris is
stripped off the ulna epi-periosteally. If the dissection strays into
the substance of the muscle, however, the nerve may be damaged. Because
the nerve is most vulnerable during very proximal dissections, it
should be identified as it passes through the two heads of the flexor
carpi ulnaris before the muscle is stripped off the proximal fifth of the bone (Fig. 4-24).
down the forearm with the ulnar nerve, lying on its radial side.
Therefore, it also is vulnerable when dissection of the flexor carpi
ulnaris is not carried out subperiosteally (see Fig. 4-23B).
 |
|
Figure 4-24
The ulnar nerve is vulnerable during the most proximal dissections of the ulna. It must be identified before muscle is stripped from bone in the proximal fifth. |
can be extended over the olecranon and up the back of the arm, however,
either to expose the elbow joint through an olecranon osteotomy or to
approach the posterior aspect of the distal two thirds of the humerus.
the flexor carpi ulnaris (which is supplied by the ulnar nerve) and the
extensor carpi ulnaris (which is supplied by the posterior interosseous
nerve; see Fig. 4-24).
the flexor carpi ulnaris, effectively tethers the nerve, preventing
further distal mobilization during decompression at the elbow.
Compression lesions of the nerve have been described (see Fig. 3-40).18,19
is the most medial of the muscles that are innervated by the posterior
interosseous nerve. Thus, it forms one border of the internervous plane
between the muscles that are innervated by the posterior interosseous
nerve and those that are innervated by the ulnar nerve, the most medial
of which is the flexor carpi ulnaris (see Fig. 4-21).
the medial side of the forearm between the flexor digitorum profundus
and the flexor digitorum superficialis, and under the flexor carpi
ulnaris. In the forearm, it supplies the flexor carpi ulnaris and the
ulnar half of the flexor digitorum profundus (see Figs. 3-40 and 4-14).
terminal branch of the brachial artery. It usually enters the forearm
deep to the deep head of the pronator teres before angling medially
across the forearm and passing under the fibrous arch of the flexor
digitorum superficialis, where it runs just deep to the median nerve
(see Figs. 4-12, 4-13 and 4-14).
In the distal two thirds of the forearm, the artery runs on the lateral
side of the ulnar nerve, lying on the flexor digitorum profundus and
under the flexor carpi ulnaris. The artery has one major branch in the
forearm, the common interosseous artery, which divides almost
immediately into two tributaries, the anterior interosseous artery
(which runs down the forearm in the midline, lying on the interosseous
membrane) and the posterior interosseous artery (which pierces the
interosseous membrane, running down the forearm in its posterior
compartment; see Fig. 4-14).
during superficial dissection if the dissection strays to the flexor
side of the bone.
The principal aim of the approach is to isolate and retract the
posterior interosseous nerve before exposing the most proximal parts of
the radial shaft, keeping the nerve under direct observation during all
stages of the subsequent procedure and protecting it from damage. The
uses of the posterior approach include the following:
-
Open reduction and internal fixation of
radial fractures (the approach provides access to the extensor side of
the bone; this is the tensile side of the bone, where plates should be
placed, if possible) -
Treatment of delayed union or nonunion of fractures of the radius
-
Access to the posterior interosseous
nerve; decompression of the nerve as it passes through the arcade of
Frohse for nerve paralysis or resistant tennis elbow9 -
Radial osteotomy
-
Treatment of chronic osteomyelitis of the radius
-
Biopsy and treatment of bone tumors
-
Place the patient supine on the operating
table, with the arm on an arm board. Pronate the patient’s arm to
expose the extensor compartment of the forearm. -
Place the patient’s arm across the chest. Supinate the forearm to expose its extensor compartment (Fig. 4-25).
If the ulna must be approached as well as the radius, this position
will allow easier access to the ulna through a separate incision.
 |
|
Figure 4-25 Position of the patient’s arm on the operating table, for the posterior approach to the radius.
|
the arm for 3 to 5 minutes or by applying a soft rubber bandage or
exsanguinator. Then, apply a tourniquet.
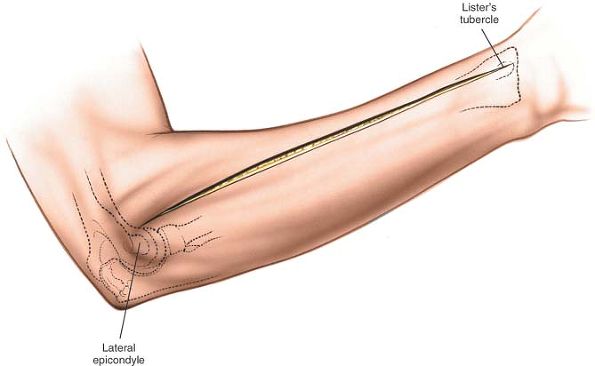
just lateral to the olecranon process on the distal humerus. It is a
prominent bony landmark, but is somewhat smaller and less defined than
the medial epicondyle of the humerus.
dorsoradial tubercle) lies about a third of the way across the dorsum
of the wrist from the styloid process of the radius. It feels like a
small, longitudinal bony prominence or nodule.
anterior to the lateral epicondyle of the humerus (along the dorsal
aspect of the forearm) to a point just distal to the ulnar side of
Lister’s tubercle at the wrist (Fig. 4-26).
given operation. In cases of fracture, the incision should be centered
over the fracture site. Use of an image intensifier may allow more
accurate placement of the incision.
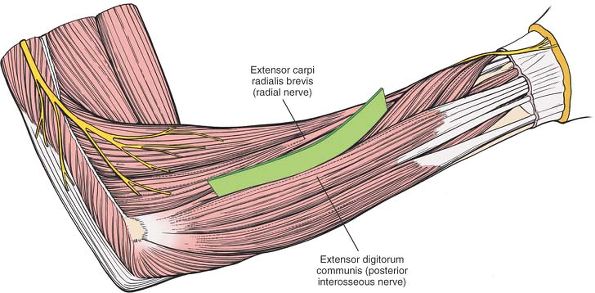
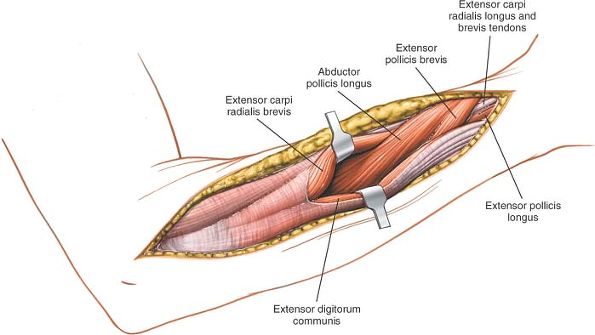
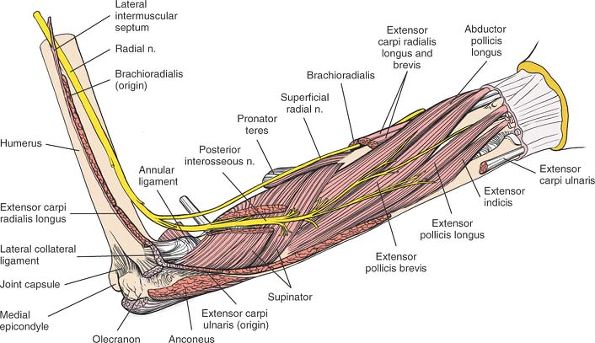
plane lies between the extensor carpi radialis brevis muscle (which is
supplied by the radial nerve) and the extensor digitorum communis
muscle (which is supplied by the posterior interosseous nerve; Fig. 4-27). The common aponeurosis of these muscles is the cleavage plane.
plane lies between the extensor carpi radialis brevis muscle (which is
supplied by the radial nerve) and the extensor pollicis longus muscle
(which is supplied by the posterior interosseous nerve).
 |
|
Figure 4-26
The long incision extends from just anterior to the lateral epicondyle of the humerus to just distal to the ulnar side of Lister’s tubercle at the wrist. |
 |
|
Figure 4-27
The internervous plane lies between the extensor carpi radialis brevis (radial nerve) and the extensor digitorum communis (posterior interosseous nerve). |
 |
|
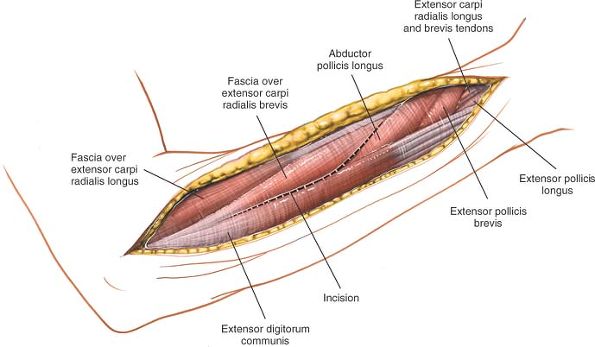
Figure 4-28
Incise the deep fascia and identify the space between the extensor carpi radialis brevis and the extensor digitorum communis. The identification is easier distally. |
and identify the space between the extensor carpi radialis brevis and
the extensor digitorum communis. This plane is more obvious distally,
where the abductor pollicis longus and the extensor pollicis brevis
emerge from between the two muscles. Proximally, the extensor carpi
radialis brevis and the extensor digitorum communis share a common
aponeurosis (Figs. 4-28 and 4-29).
 |
|
Figure 4-29 The interval between the extensor carpi radialis brevis and the extensor digitorum communis.
|
 |
|
Figure 4-30 The supinator muscle, beneath the extensor carpi radialis brevis and the extensor pollicis longus.
|
 |
|
Figure 4-31
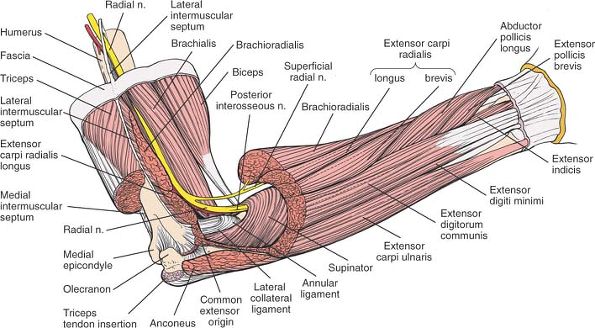
The supinator cloaks the upper third of the radius; the posterior interosseous nerve runs through its substance. The nerve must be protected and identified as it traverses the muscle. The interosseous nerve is seen in the substance of the supinator (inset). |
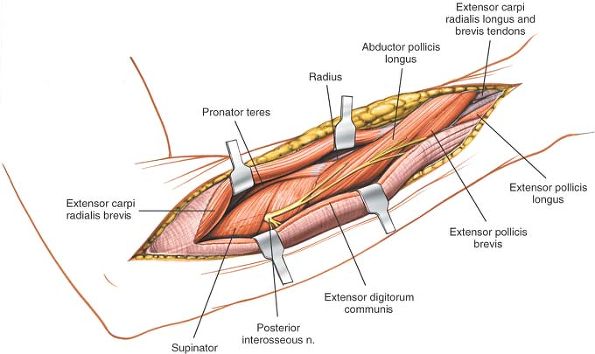
muscles to reveal the upper third of the shaft of the radius, which is
covered by the enveloping supinator muscle.
pollicis brevis, identify the intermuscular plane between the extensor
carpi radialis brevis and the extensor pollicis longus. Separating the
two muscles exposes the lateral aspect of the shaft of the radius (Figs. 4-30 and 4-31).
upper third of the radius; the posterior interosseous nerve runs within
its substance between the superficial and deep heads. The nerve emerges
from between the superficial and deep heads of the supinator muscle
about 1 cm proximal to the distal edge of the muscle. At this point, it
divides into branches that supply the extensors of the wrist, fingers,
and thumb (see Fig. 4-31).
 |
|
Figure 4-32
Detach the insertion of the supinator from the anterior aspect of the radius, with the arm in full supination to bring the origin of the supinator into view and to move the posterior interosseous nerve away from the area of incision. Along the distal third of the bone, the extensor carpi radialis brevis has been separated from the extensor pollicis longus, uncovering the lateral border of the radius. |
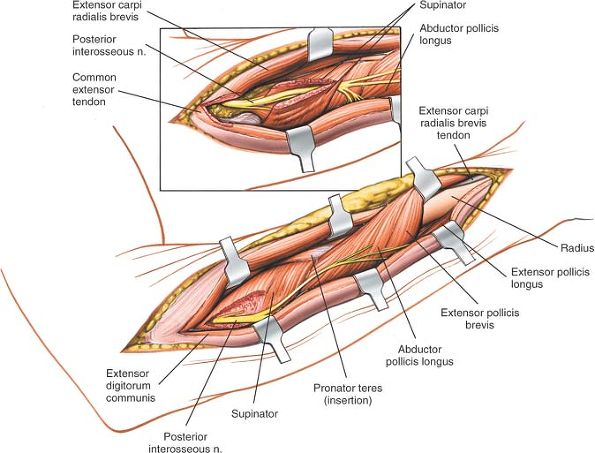
-
Proximal to distal (see Fig. 4-31 inset).
Detach the origin of the extensor carpi radialis brevis and part of the
origin of the extensor carpi radialis longus from the lateral
epicondyle and retract these two muscles laterally. Next, identify the
posterior interosseous nerve proximal to the proximal end of the
supinator muscle by palpating the nerve. Now, carefully dissect the
nerve out through the substance of the supinator, in a proximal to
distal direction, taking great care to preserve the multiple motor
branches to the muscle itself. -
Distal to proximal (see Fig. 4-31).
Identify the nerve as it emerges from the supinator. Note that it
emerges about 1 cm proximal to the distal end of the muscle. Now,
follow the nerve proximally through the substance of the muscle, taking
care to preserve all muscular branches.
successfully, fully supinate the arm to bring the anterior surface of
the radius into view. Detach the insertion of the supinator muscle from
the anterior aspect of the radius. Strip the supinator off the bone
subperiosteally to expose the proximal third of the shaft of the radius
(Fig. 4-32).
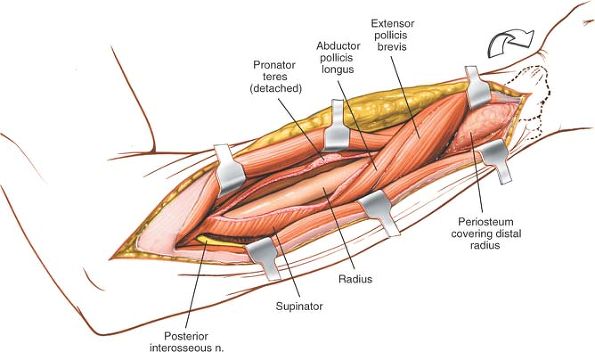
extensor pollicis brevis, blanket this approach as they cross the
dorsal aspect of the radius before heading distally and radially across
the middle third of the radius. To retract them off the bone, make an
incision along their superior and inferior borders. Then, they can be
separated easily from the underlying radius and retracted either
distally or proximally, depending on the exposure that is required (see
Fig. 4-32). Plates can be slid underneath these muscles if required for fixation.
extensor pollicis longus already has led directly onto the lateral
border of the radius (see Fig. 4-32).
-
Identification of the nerve.
In 25% of patients, the posterior interosseous nerve actually touches
the dorsal aspect of the radius opposite the bicipital tuberosity;
plates placed high on the dorsal surface of the radius may trap the
nerve underneath.21 Identifying and
preserving the nerve in the supinator muscle is the only means of
ensuring that it will not be trapped beneath any plate that is applied
for a radial fracture (see Fig. 4-31). -
Protecting the nerve with the supinator muscle.
Strip the supinator off the anterior aspect of the radius and retract
it radially, with the nerve still enclosed in its substance. This
technique often is used in the anterior approach to the radius,
exposing the anterior surface of the bone. The dorsal aspect of the
radius can be exposed in the same way, but because the posterior
interosseous nerve actually touches the periosteum in one of four
patients, the safest procedure is to dissect the nerve out fully before
stripping the muscle from the bone (see Fig. 4-32).
brevis and extensor digitorum communis muscles, detach the origin of
the extensor carpi radialis brevis from the common extensor origin on
the lateral epicondyle of the humerus.
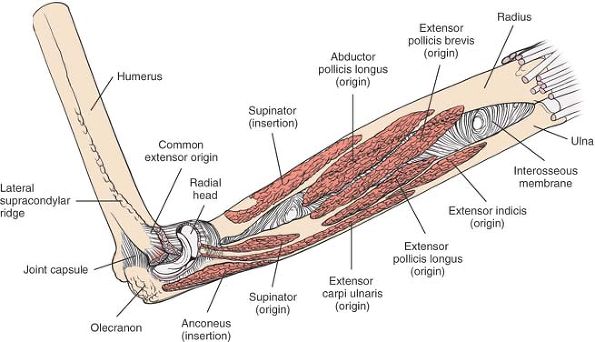
-
The mobile wad of three
(the brachioradialis, extensor carpi radialis longus, and extensor
carpi radialis brevis) runs along the lateral side of the forearm.
These three muscles arise from a continuous line on the lateral
supracondylar ridge and lateral epicondyle of the humerus. -
The four superficial extensor muscles
fan out from the lateral epicondyle of the humerus. From the ulnar to
the radial side of the forearm, they consist of the anconeus, the
extensor carpi ulnaris, the extensor digiti minimi, and the extensor
digitorum communis (Figs. 4-33 and 4-34).
Two internervous planes exist in this layer of musculature: between the
extensor carpi ulnaris muscle (which is supplied by the posterior
interosseous nerve) and the flexor carpi ulnaris muscle (which is
supplied by the ulnar nerve) on the ulnar side (see Fig. 4-21), and between the extensor carpi radialis brevis muscle22
(which is supplied by the radial nerve) and the extensor digitorum
communis muscle (which is supplied by the posterior interosseous nerve)
on the radial side (see Fig. 4-27). -
Of the five deep muscles,
three (the abductor pollicis longus, the extensor pollicis brevis, and
the extensor pollicis longus) supply the thumb. The three
P.177P.178
cross
the forearm obliquely from the ulnar to the radial side, and two of
them (the abductor pollicis longus and the extensor pollicis brevis)
wind around the dorsal and lateral aspects of the radius. The remaining
two muscles of the deep group are the supinator and the extensor
indicis (Fig. 4-35).
 |
|
Figure 4-33 Superficial muscles of the posterior aspect of the forearm.
|
 |
|
Figure 4-34
The superficial muscles have been removed to reveal the course of the posterior interosseous nerve as it enters the supinator muscle through the arcade of Frohse and the course of the superficial radial nerve, which is sensory and supplies no muscles of the forearm. |
interosseous nerve, innervates the muscles of the extensor compartment;
it is the key anatomic structure from an operative point of view. The
only major arterial supply of the compartment is the posterior
interosseous artery.
 |
|
Figure 4-35 The course of the posterior interosseous nerve through the supinator muscle, as it runs to supply muscles in the forearm.
Extensor Carpi Ulnaris. Origin.
Common extensor origin on lateral epicondyle of humerus and subcutaneous border of ulna. (Shared origin with flexor carpi ulnaris.) Insertion. Base of fifth metacarpal. Action. Extensor and ulnar deviator of wrist. Nerve supply. Posterior interosseous nerve. Extensor Digitorum Communis. Origin. Common extensor origin on lateral epicondyle of humerus. Insertion. Into extensor apparatus of fingers. Action. Extensor of wrist and fingers. Nerve supply. Posterior interosseous nerve.
|
lateral to the olecranon process, is smaller than the medial
epicondyle, but its lateral supracondylar line, which runs superiorly,
is longer than the medial supracondylar line, extending almost to the
deltoid tuberosity. The lateral epicondyle is the site of the common
origin of the superficial muscles of the extensor compartment of the
forearm. The extensor carpi radialis brevis, extensor digitorum
communis,
extensor
digiti minimi, and extensor carpi ulnaris all originate from fused
tendons that attach just anterior to the epicondyle. The
brachioradialis and extensor carpi radialis longus arise from the
lateral supracondylar ridge.
lateral epicondylitis; the pain that is characteristic of this
condition can be reproduced by providing resistance to extension of the
wrist.
arcade of Frohse may produce a syndrome similar to lateral
epicondylitis. In these cases, the tenderness usually is elicited more
distally in the course of the posterior interosseous nerve or
anteriorly over the arcade of Frohse. Both conditions can exist in a
single patient.23
forearm crosses the lines of cleavage of the skin at right angles and
often leaves a broad scar.
plane between the extensor carpi radialis brevis and the extensor
communis. In the distal third of the wound, the internervous plane lies
between the extensor carpi radialis brevis and the extensor pollicis
longus (see Fig. 4-33).
consists of detaching the insertion of the supinator muscle from the
radius while preserving the posterior interosseous nerve (see Fig. 4-32).
mobilizing and retracting two muscles, the abductor pollicis longus and
the extensor pollicis brevis (see Fig. 4-32).
internervous plane between the extensor pollicis longus and the
extensor carpi radialis brevis.
supinator muscle, through which the posterior interosseous nerve passes
on its way to the posterior compartment of the forearm (see Figs. 4-34 and 4-35). For additional information on the supinator muscle, see the section regarding the anterior approach to the radius.
is the motor nerve of the posterior compartment of the forearm. A
branch of the radial nerve, it passes between the two heads of the
supinator muscle and actually may come in direct contact with the neck
of the radius. At that point, it may be trapped beneath incorrectly
positioned plates. After emerging from the supinator muscle, the nerve
passes distally over the origin of the abductor pollicis longus muscle
to reach the interosseous membrane. It continues distally on the
interosseous membrane to the level of the wrist joint, which it
supplies with some sensory branches. The nerve supplies those muscles
that arise from the common extensor origin and the deep muscles of the
extensor compartment of the forearm (see Fig. 4-35).
important to remember that the posterior interosseous nerve is
vulnerable during all approaches to the proximal third of the radial
shaft. Although the nerve can be protected by detaching the insertion
of the supinator and stripping the muscle off the bone subperiosteally,
the only certain protection of the posterior interosseous nerve during
plating of the upper third of the radius may come with full dissection
via a posterior approach.
accompanies the posterior interosseous nerve as it runs along the
interosseous membrane in the proximal two thirds of the forearm. The
posterior interosseous artery enters the extensor compartment of the
forearm by passing between the radius and the ulna through the
interosseous membrane (Fig. 4-36). The artery then joins the posterior interosseous nerve distal to the distal edge of the deep head of the supinator muscle.
dissected easily down to the level of the wrist. Most of the blood
supply for the posterior area comes from an anterior interosseous
artery via branches that perforate the interosseous membrane. The
tendons running in this area may have a marginal blood supply.
approach to the radius, good collateral circulation appears to protect
the extremity from any functional deficits.
 |
|
Figure 4-36 The origins and insertions of the muscles of the posterior aspect of the forearm.
Extensor Carpi Radialis Longus. Origin. Lower third of lateral supracondylar ridge of humerus, lateral intermuscular septum of arm. Insertion. Base of second metacarpal. Action. Extensor and radial deviator of wrist. Nerve supply. Radial nerve.
Extensor Carpi Radialis Brevis. Origin. Common extensor origin on lateral epicondyle of humerus and radial collateral ligament of elbow. Insertion. Base of third metacarpal. Action. Extensor and radial deviator of wrist. Nerve supply. Radial nerve.
Supinator. Origin.
From two heads. Superficial head: from lateral epicondyle of humerus, lateral collateral ligament of elbow, and supinator crest of ulna. Deep head: from supinator crest and fossa of ulna. Insertion. Anterior aspect of radius. Action. Supinator of forearm. Weak flexor of elbow. Nerve supply. Posterior interosseous nerve. Extensor Pollicis Longus. Origin. Posterior surface of ulna in its middle third and from interosseous membrane. Insertion. Distal phalanx of thumb. Action. Extensor of thumb and wrist. Nerve supply. Posterior interosseous nerve.
Abductor Pollicis Longus. Origin. Posterior surface of ulna, posterior interosseous membrane, and middle third of posterior surface of radius. Insertion. Base of thumb metacarpal. Action. Abductor and extensor of thumb. Nerve supply. Posterior interosseous nerve.
Extensor Pollicis Brevis. Origin. Posterior surface of radius and interosseous membrane. Insertion. Base of proximal phalanx of thumb. Action. Extensor of proximal phalanx of thumb. Nerve supply. Posterior interosseous nerve.
Extensor Indicis. Origin. Posterior surface of ulnar shaft and interosseous membrane. Insertion. Extensor apparatus of index finger via ulnar side of tendon of extensor digitorum that runs to index finger. Action. Extensor of index finger. Nerve supply. Posterior interosseous nerve.
Extensor Digiti Minimi. Origin. Common extensor origin on lateral epicondyle of humerus. Insertion. Extensor apparatus of little finger. Action. Extensor of little finger. Nerve supply. Posterior interosseous nerve.
|
 |
|
Figure 4-37 The bones of the posterior aspect of the forearm.
|
F, Frankel M: Die muskeln des menschlichen armes. In: Bardelehen’s
handbuch der anatomie des menschlichen. Jena, Germany, Fisher, 1980
M: The arcade of Prohse and its relationship to posterior interosseous
nerve paralysis. J Bone Joint Surg [Br] 50:809, 1968
O: Pronator syndrome: compression neuropathy of the median nerve at
level of pronator teres muscle. Georgetown Med Bull 13:232, 1960
M: The anterior interosseous nerve syndrome, with special attention to
its variations. J Bone Joint Surg [Am] 54A:84, 1970
RB, Linscheid RL, Dobyns JH et al: Ulnar lengthening in the treatment
of Kienböck’s disease. J Bone Joint Surg [Am] 64:170, 1982
O: Management of peripheral nerve problems. In: Management of nerve
compression lesions of the upper extremity. Philadelphia, WB Saunders,
1980:569
