Distal Radius
Authors: Koval, Kenneth J.; Zuckerman, Joseph D.
Title: Handbook of Fractures, 3rd Edition
Copyright ©2006 Lippincott Williams & Wilkins
> Table of Contents > III – Upper Extremity Fractures and Dislocations > 22 – Distal Radius
22
Distal Radius
EPIDEMIOLOGY
-
Distal radius fractures are among the most common fractures of the upper extremity.
-
More than 450,000 occur annually in the United States.
-
Fractures of the distal radius represent approximately one-sixth of all fractures treated in emergency departments.
-
The incidence of distal radius fractures
in the elderly correlates with osteopenia and rises in incidence with
increasing age, nearly in parallel with the increased incidence of hip
fractures. -
Risk factors for fractures of the distal
radius in the elderly include decreased bone mineral density, female
sex, white race, family history, and early menopause.
ANATOMY
-
The metaphysis of the distal radius is
composed primarily of cancellous bone. The articular surface has a
biconcave surface for articulation with the proximal carpal row
(scaphoid and lunate fossae), as well as a notch for articulation with
the distal ulna. -
80% of axial load is supported by the distal radius and 20% by the ulna and the triangular fibrocartilage complex (TFCC).
-
Reversal of the normal palmar tilt
results in load transfer onto the ulna and TFCC; the remaining load is
then borne eccentrically by the distal radius and is concentrated on
the dorsal aspect of the scaphoid fossa. -
Numerous ligamentous attachments exist to
the distal radius; these often remain intact during distal radius
fracture, facilitating reduction through “ligamentotaxis.” -
The volar ligaments are stronger and confer more stability to the radiocarpal articulation than the dorsal ligaments.
MECHANISM OF INJURY
-
Common mechanisms in younger individuals
include falls from a height, motor vehicle accident, or injuries
sustained during athletic participation. In elderly individuals, distal
radial fractures may arise from low-energy mechanisms, such as a simple
fall from a standing height. -
The most common mechanism of injury is a fall onto an outstretched hand with the wrist in dorsiflexion.
-
Fractures of the distal radius are
produced when the dorsiflexion of the wrist varies between 40 and 90
degrees, with lesser degrees of force required at smaller angles. -
The radius initially fails in tension on
the volar aspect, with the fracture propagating dorsally, whereas
bending moment forces induce compression stresses resulting in dorsal
comminution. Cancellous impaction of the metaphysis further compromises
P.227
dorsal stability. Additionally, shearing forces influence the injury pattern, often resulting in articular surface involvement. -
High-energy injuries (e.g., vehicular
trauma) may result in significantly displaced or highly comminuted
unstable fractures to the distal radius.
CLINICAL EVALUATION
-
Patients typically present with variable
wrist deformity and displacement of the hand in relation to the wrist
(dorsal in Colles or dorsal Barton fractures and volar in Smith-type
fractures). The wrist is typically swollen with ecchymosis, tenderness,
and painful range of motion. -
The ipsilateral elbow and shoulder should be examined for associated injuries.
-
A careful neurovascular assessment should
be performed, with particular attention to median nerve function.
Carpal tunnel compression symptoms are common (13% to 23%) owing to
traction during forced hyperextension of the wrist, direct trauma from
fracture fragments, hematoma formation, or increased compartment
pressure.
RADIOGRAPHIC EVALUATION
-
Posteroanterior and lateral views of the
wrist should be obtained, with oblique views for further fracture
definition, if necessary. Shoulder or elbow symptoms should be
evaluated radiographically. -
Contralateral wrist views may help to assess the patient’s normal ulnar variance and scapholunate angle.
-
Computed tomography scan may help to demonstrate the extent of intraarticular involvement.
-
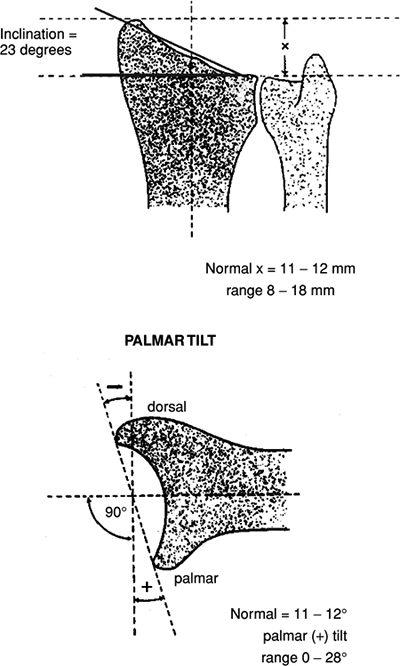
Normal radiographic relationships (Fig. 22.1).
-
Radial inclination: averages 23 degrees (range, 13 to 30 degrees)
-
Radial length: averages 11 mm (range, 8 to 18 mm).
-
Palmar (volar) tilt: averages 11 to 12 degrees (range, 0 to 28 degrees).
-
CLASSIFICATION
Descriptive
-
Open versus closed
-
Displacement
-
Angulation
-
Comminution
-
Loss of radial length
Frykman Classification of Colles Fractures
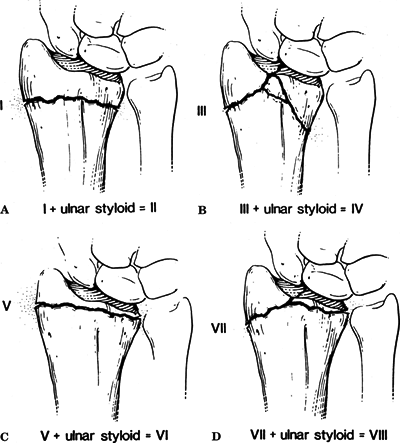
This is based on the pattern of intraarticular involvement (Fig. 22.2).
 |
|
Figure
22.1. The normal radiographic measurements of the distal radius. (Reproduced with permission from the Orthopaedic Trauma Association). |
 |
|
Figure
22.2. Frykman classification of distal radius fractures. (A) Frykman Type I/II, extraarticular. (B) Frykman Type III/IV, intraarticular radiocarpal joint. (C) Frykman Type V/VI, intraarticular distal radioulnar joint. (D) Frykman Type VII/VIII, intraarticular radiocarpal and distal radioulnar joints. (From Rockwood CA Jr, Green DP, Bucholz RW, Heckman JD, eds. Rockwood and Green’s Fractures in Adults, 4th ed, vol. 1. Philadelphia: Lippincott-Raven, 1996:771..)
|
| Distal Ulna Fracture | ||
|---|---|---|
| Fracture | Absent | Present |
| Extraarticular | I | II |
| Intraarticular involving radiocarpal joint | III | IV |
| Intraarticular involving distal radioulnar joint (DRUJ) | V | VI |
| Intraarticular involving radiocarpal and DRUJ | VII | VIII |
P.228
P.229
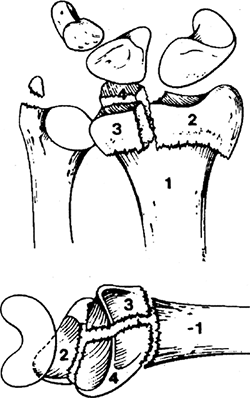
Melone Classification of Intraarticular Fractures
This is based on a consistent mechanism (lunate impaction injury) (Fig. 22.3).
P.230
| Type I: | Stable, without comminution |
| Type II: | Unstable die-punch, dorsal or volar |
| IIA: | Reducible |
| IIB: | Irreducible |
| Type III: | Spike fracture; contused volar structures |
| Type IV: | Split fracture; medial complex fractured with dorsal and palmar fragments displaced separately |
| Type V: | Explosion fracture; severe comminution with major soft tissue injury |
 |
|
Figure 22.3. Intraarticular distal radius fractures.
(From Melone CP Jr. Open treatment for displaced articular fractures of the distal radius. Clin Orthop 1986;202:103..)
|
Fernandez Classification
This is a mechanism-based classification system.
| Type I: | Metaphyseal bending fracture with the inherent problems of loss of palmar tilt and radial shortening relative to the ulna (DRUJ injury) |
| Type II: | Shearing fracture requiring reduction and often buttressing of the articular segment |
| Type III: | Compression of the articular surface without the characteristic fragmentation; also the potential for significant interosseous ligament injury |
| Type IV: | Avulsion fracture or radiocarpal fracture dislocation |
| Type V: | Combined injury with significant soft tissue involvement owing to high-energy injury |
P.231
OTA Classification of Fractures of the Distal Radius and Ulna
See Fracture and Dislocation Compendium at http://www.ota.org/compendium/index.htm.
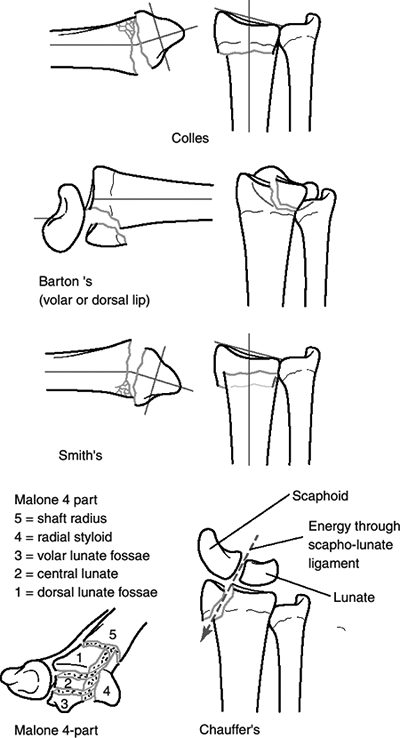
Eponyms (Fig. 22.4)
-
Colles fracture
-
The original description was for
extraarticular fractures. Present usage of eponym includes both
extraarticular and intraarticular distal radius fractures demonstrating
various combinations of dorsal angulation (apex volar), dorsal
displacement, radial shift, and radial shortening. -
Clinically, it has been described as a “dinner fork” deformity.
-
More than 90% of distal radius fractures are of this pattern.
-
The mechanism of injury is a fall onto a hyperextended, radially deviated wrist with the forearm in pronation.
-
Intraarticular fractures are generally
seen in the younger age group secondary to higher-energy forces;
concomitant injuries (i.e., to nerve, carpus, and distal ulna) are more
frequent, as is involvement of both the radiocarpal joint and the DRUJ.
-
-
Smith fracture (reverse Colles fracture)
-
This describes a fracture with volar
angulation (apex dorsal) of the distal radius with a “garden spade”
deformity or volar displacement of the hand and distal radius. -
The mechanism of injury is a fall onto a flexed wrist with the forearm fixed in supination.
-
This is a notoriously unstable fracture
pattern; it often requires open reduction and internal fixation because
of difficulty in maintaining adequate closed reduction.
-
-
Barton fracture
-
This is a fracture-dislocation or
subluxation of the wrist in which the dorsal or volar rim of the distal
radius is displaced with the hand and carpus. Volar involvement is more
common. -
The mechanism of injury is a fall onto a
dorsiflexed wrist with the forearm fixed in pronation. Fracture occurs
secondary to shear. -
Most fractures are unstable and require
open reduction and internal fixation with a buttress plate to achieve
stable, anatomic reduction.
-
-
Radial styloid fracture (chauffeur’s fracture, backfire fracture, Hutchinson fracture)
-
This is an avulsion fracture with extrinsic ligaments remaining attached to the styloid fragment.
-
The mechanism of injury is compression of the scaphoid against the styloid with the wrist in dorsiflexion and ulnar deviation.
-
It may involve the entire styloid or only the dorsal or volar portion.
-
It is often associated with intercarpal ligamentous injuries (i.e., scapholunate dissociation, perilunate dislocation).
-
Open reduction and internal fixation are often necessary.
-
 |
|
Figure 22.4. Eponymic classification of five basic types of distal radius fractures: four classic
(Colles,
Barton, Smith, and Chauffeur’s) fracture descriptions, and the Malone four-part fracture, which was described more recently and represents an increasing understanding of the importance of the distal radioulnar joint and the ulnar column of the radius. |
P.232
P.233
TREATMENT
-
Factors affecting treatment include:
-
Fracture pattern.
-
Local factors: bone quality, soft tissue injury, fracture comminution, fracture displacement, and energy of injury.
-
Patient factors: physiologic patient age,
lifestyle, occupation, hand dominance, associated medical conditions,
associated injuries, and compliance.
-
-
Acceptable radiographic parameters for a healed radius in an active, healthy patient include:
-
Radial length: within 2 to 3 mm of the contralateral wrist.
-
Palmar tilt: neutral tilt (0 degrees).
-
Intraarticular step-off: <2 mm.
-
Radial inclination: <5-degree loss.
-
McQueen has reported that the carpal alignment after distal radius fracture is the main influence on outcome.
-
Carpal alignment is measured by the
intersection of two lines on the lateral radiograph: one parallel and
through the middle of the radial shaft and the other through and
parallel to the capitate. If the two lines intersect within the carpus,
then the carpus is aligned. If the two lines intersect out with the
carpus, then the carpus is malaligned.
-
-
-
Several factors have been associated with redisplacement following closed manipulation of a distal radius fracture:
-
The initial displacement of the fracture:
The greater the degree of displacement (particularly radial
shortening), the more energy is imparted to the fracture resulting in a
higher likelihood that closed treatment will be unsuccessful. -
The age of the patient: Elderly patients with osteopenic bones tend to displace, particularly late.
-
The extent of metaphyseal comminution
(the metaphyseal defect), as evidenced by either plain radiograph or
computerized tomography. -
Displacement following closed treatment
is a predictor of instability, and repeat manipulation is unlikely to
result in a successful radiographic outcome.
-
Nonoperative
-
All fractures should undergo closed reduction, even if it is expected that surgical management will be needed.
-
Fracture reduction helps to limit postinjury swelling, provides pain relief, and relieves compression on the median nerve.
-
-
Cast immobilization is indicated for:
-
Nondisplaced or minimally displaced fractures.
-
Displaced fractures with a stable fracture pattern which can be expected to unite within acceptable radiographic parameters.
-
Low-demand elderly patients in whom
future functional impairment is less of a priority than immediate
health concerns and/or operative risks.
-
-
Hematoma block with supplemental
intravenous sedation, Bier block, or conscious sedation can be used to
provide analgesia for closed reduction. -
Technique of closed reduction (dorsally tilted fracture):
-
The distal fragment is hyperextended.
-
Traction is applied to reduce the distal to the proximal fragment with pressure applied to the distal radius.
-
A well-molded long arm (“sugar-tong”) splint is applied, with the wrist in neutral to slight flexion.
-
One must avoid extreme positions of the wrist and hand.
-
The cast should leave the metacarpophalangeal joints free.
-
-
Once swelling has subsided, a well-molded cast is applied.
-
The ideal forearm position, duration of
immobilization, and need for a long arm cast remain controversial; no
prospective study has demonstrated the superiority of one method over
another. -
Extreme wrist flexion should be avoided,
because it increases carpal canal pressure (and thus median nerve
compression) as well as digital stiffness. Fractures that require
extreme wrist flexion to maintain reduction may require operative
fixation. -
The cast should be worn for approximately 6 weeks or until radiographic evidence of union has occurred.
-
Frequent radiographic examination is necessary to detect loss of reduction.
P.234
Operative
-
Indications
-
High-energy injury
-
Secondary loss of reduction
-
Articular comminution, step-off, or gap
-
Metaphyseal comminution or bone loss
-
Loss of volar buttress with displacement
-
DRUJ incongruity
-
Operative Techniques
-
Percutaneous pinning: This is primarily used for extraarticular fractures or two-part intraarticular fractures.
-
It may be accomplished using two or three
Kirschner wires placed across the fracture site, generally from the
radial styloid, directed proximally and from the dorsoulnar side of the
distal radial fragment directed proximally. Transulnar pinning with
multiple pins has also been described. -
Percutaneous pinning is generally used to
supplement short arm casting or external fixation. The pins may be
removed 3 to 4 weeks postoperatively, with the cast maintained for an
additional 2 to 3 weeks.
-
-
Kapandji “Intrafocal” pinning.
-
This is a technique of trapping the distal fragment by buttressing to prevent displacement.
-
The wires are inserted both radially and
dorsally directly into the fracture site. The wires are then levered up
and then directed into the proximal intact opposite cortex. -
The fragments are thus buttressed from displacing dorsally or proximally.
-
In addition to being relatively simple
and inexpensive, this technique has been shown to be very effective,
particularly in elderly patients.
-
-
External fixation: Its use has grown in popularity based on studies yielding relatively low complication rates.
-
Spanning external fixation
-
Ligamentotaxis is used to restore radial length and radial inclination, but it rarely restores palmar tilt.
-
External fixation alone may not be
sufficiently stable to prevent some degree of collapse and loss of
palmar tilt during the course of healing. -
Overdistraction should be avoided because
it may result in finger stiffness and may be recognized by increased
intercarpal distance on intraoperative fluoroscopy. -
It may be supplemented with percutaneous pinning of comminuted or articular fragments.
-
Pins may be removed at 3 to 4 weeks, although most recommend 6 to 8 weeks of external fixation.
-
-
Nonspanning external fixation
-
A nonspanning fixator is one that
stabilizes the distal radius fracture by securing pins in the radius
alone, proximal to and distal to the fracture site. -
It requires a sufficiently large intact segment of intact distal radius.
-
McQueen reported that nonspanning better
preserved volar tilt, prevented carpal malalignment, and gave better
grip strength and hand function than spanning external fixation.
-
-
-
Open reduction and internal fixation
-
Dorsal plating: This has several theoretic advantages.
-
It is technically familiar to most surgeons, and the approach avoids the neurovascular structures on the palmar side.
-
The fixation is on the compression side of the fracture and provides a buttress against collapse.
-
Initial reports of the technique
demonstrated successful outcomes with the theoretic advantages of
earlier return of function and better restoration of radial anatomy
than seen with external fixation. -
Dorsal plating has been associated with extensor tendon complications.
-
-
Volar nonlocked plating
-
The primary indication is a shear fracture of the volar lip.
-
It may be unable to maintain fracture reduction in the presence of dorsal comminution.
-
-
Volar locked plating
-
Locked volar plating has increased in
popularity because this implant has been shown to stabilize distal
radius fractures with dorsal comminution. -
The interval is between the flexor carpi radialis and the radial artery.
-
-
-
Adjunctive fixation
-
Supplemental graft may be autograft, allograft, or synthetic graft.
-
Adjunctive Kirschner wire fixation may be helpful with smaller fragments.
-
-
Arthroscopically assisted intraarticular fracture reduction
-
Fractures that may benefit most from
adjunctive arthroscopy are: (1) complex articular fractures without
metaphyseal comminution, particularly those with central impaction
fragments; and (2) fractures with evidence of substantial interosseous
ligament or TFCC injury without large ulnar styloid base fracture.
-
Ulna styloid fractures: Indications for
fixation of ulna styloid are controversial. Some authors have advocated
fixation for displaced fractures at the base of the ulna styloid.
P.235
COMPLICATIONS
-
Median nerve dysfunction: Management is controversial, although there is general agreement about the following:
-
A complete median nerve lesion with no improvement following fracture reduction requires surgical exploration.
-
Median nerve dysfunction developing after
reduction mandates release of the splint and positioning of the wrist
in neutral position; if there is no improvement, exploration and
release of the carpal tunnel should be considered. -
An incomplete lesion in a fracture requiring operative intervention is a relative indication for carpal tunnel release.
-
-
Malunion or nonunion: This typically
results from inadequate fracture reduction or stabilization; it may
require internal fixation with or without osteotomy with bone graft. -
Complications of external fixation
include reflex sympathetic dystrophy, pin tract infection, wrist and
finger stiffness, fracture through a pin site, and radial sensory
neuritis. Open pin placement is advisable to allow visualization of the
superficial radial nerve. -
Posttraumatic osteoarthritis: This is a
consequence of radiocarpal and radioulnar articular injury, thus
emphasizing the need for anatomic restoration of the articular surface. -
Finger, wrist, and elbow stiffness: This
occurs especially with prolonged immobilization in a cast or with
external fixation; it emphasizes the need for aggressive occupational
therapy to mobilize the digits and elbow while wrist immobilization is
in place, as well as a possible supervised therapy regimen once
immobilization has been discontinued. -
Tendon rupture, most commonly extensor
pollicis longus, may occur as a late complication of distal radius
fractures, even in cases of minimally displaced injuries. Degeneration
of the tendon, owing to vascular disruption of the tendon sheath as
well as mechanical impingement on the callus, results in attrition of
tendon integrity. Dorsal plating has been most often associated with
extensor tendon complications. -
Midcarpal instability (i.e., dorsal or
volar intercalated segmental instability) may result from radiocarpal
ligamentous injury or a dorsal or volar rim distal radius disruption.
